Abstract
Background/Objective:
Advance care planning (ACP) is associated with improved patient and caregiver outcomes, but is underutilized. To encourage ACP the Centers for Medicare & Medicaid Services (CMS) implemented specific ACP visit reimbursement codes in 2016. To better understand the utilization of these ACP reimbursement codes, we explored regional variation in billed ACP visits.
Design:
We performed a retrospective cross-sectional analysis using a randomly-sampled 5% cohort of Medicare fee-for-service (FFS) beneficiaries’ claims files from 2017. Region was defined by Hospital Referral Region (HRR).
Setting:
National Medicare fee-for-service (FFS)
Participants:
1.3 million Medicare beneficiaries aged 65 and older.
Measurement:
Receipt of billed ACP service, identified through Current Procedural Terminology codes 99497 or 99498. Proportion of beneficiaries who received billed ACP service(s) by region was calculated. We fit a multi-level logistic regression model with a random regional intercept to determine the variation in billed ACP visits attributable to the region after accounting for patient (demographics, comorbidities and medical care utilization) and regional factors (hospital size, Emergency Department visits, hospice utilization and costs).
Results:
The study population included about 1.3 million beneficiaries of which 32,137 (2.4%) had at least one billed ACP visit in 2017. There was substantial regional variation in the percentage of beneficiaries with billed ACP visits; lowest quintile region <0.83%, subsequent regions <1.6%, <2.4%, <3.3% to <8.4% in the highest quintile regions. 15.4% of the variance in whether an older adult had a billed ACP visit was explained by the region. While numerous regional factors were associated with billed ACP visits, none were strong predictors.
Conclusion:
In 2017, we found wide regional variation in the use of billed ACP visits although use overall was low in all regions. Increasing the understanding of the drivers and the effects of billed ACP visits could inform strategies for increasing ACP.
Background
Advance care planning (ACP) is a process intended to ensure that people receive end of life medical care that is consistent with their values, goals and preferences.1 ACP is critical given that many adults do not have decision making capacity near the end of life, and because ACP results in more value concordant care and better patient and caregiver outcomes.2–6 However, ACP is underutilized; over 25% of older adults have not engaged in any form of ACP (i.e. advance directive, durable power of attorney or discussed their preferred medical treatment if they were to become seriously ill).7
Recognizing ACP underutilization despite the well-described benefits of this guideline concordant process, in January of 2016, the Centers for Medicare & Medicaid Services (CMS) introduced Current Procedural Terminology (CPT) reimbursement codes for ACP visits (99497 and 99498) to encourage ACP. The CPT code 99497 is used for the first 30 minutes, allowing for reimbursement of approximately $86 in the outpatient setting and $80 in the inpatient setting. The CPT code 99498 can be used for each additional 30-minute period with a reimbursement of $75.8 There is no cost to the beneficiary if ACP occurs as part of the annual wellness visit.9 While there are many approaches to increasing ACP, CMS incentivizing ACP visits is an at-scale approach.
One approach to better understand ACP visit utilization is to explore regional variation in billed ACP visits.10, 11 Quantifying regional variation in billed ACP visits may provide a lens into understanding how patients and providers perceive the necessity of ACP. In addition, exploring regional factors that are associated with billed ACP visits may suggest strategies to increase ACP visits. Overall, a better understanding of regional differences in billed ACP visits and the drivers of those differences could permit public health officials to target regions of the country that are in the greatest need for improvement and may suggest strategies for such improvement. In this context, we explored regional variation in billed ACP visits and the extent to which regional variation in billed ACP visits is accounted for by patient demographics, comorbidities, health care utilization and regional factors.
Methods
Data Source
We performed a retrospective cross-sectional analysis using a randomly-sampled 5% cohort of Medicare fee-for-service (FFS) beneficiaries’ files. Medicare FFS claim files included medpar (inpatient, SNF), outpatient, carrier, home health, hospice claims and the Medicare Beneficiary Summary File (MBSF). Medicare includes data on demographics, eligibility, residence, medical services (diagnosis codes and procedures) and provider information (provider’s identifier and practice location). For regional characteristics, we obtained regional demographic (number of beneficiaries), medical care utilization (percent of beneficiaries use hospice and emergency department visits), and spending (standardize per capita total medical care cost) through the CMS geographic variation public use file12 for Medicare beneficiaries aged 65+ and hospital bed sizes through the hospital tracking files created by the Dartmouth Atlas.13 This study was approved by the institutional review board of University of Michigan.
Study Population
We included all Medicare beneficiaries aged 65 and older who were continuously enrolled in Medicare Part A/Part B programs in 2017. Beneficiaries who died during 2017 were included until their death. Since the study looked into beneficiaries’ comorbidities and their prior medical utilization, beneficiaries who did not have 24-month continuous enrollment in Medicare Part A/Part B prior to 2017 (N=314,861) were excluded. Beneficiaries who utilized hospice services (N=27,238) or had a billed ACP visit (s) (N=21,987) in 2016, or resided in unknown HRRs (N=10,362) were excluded (Figure 1).
Figure 1.
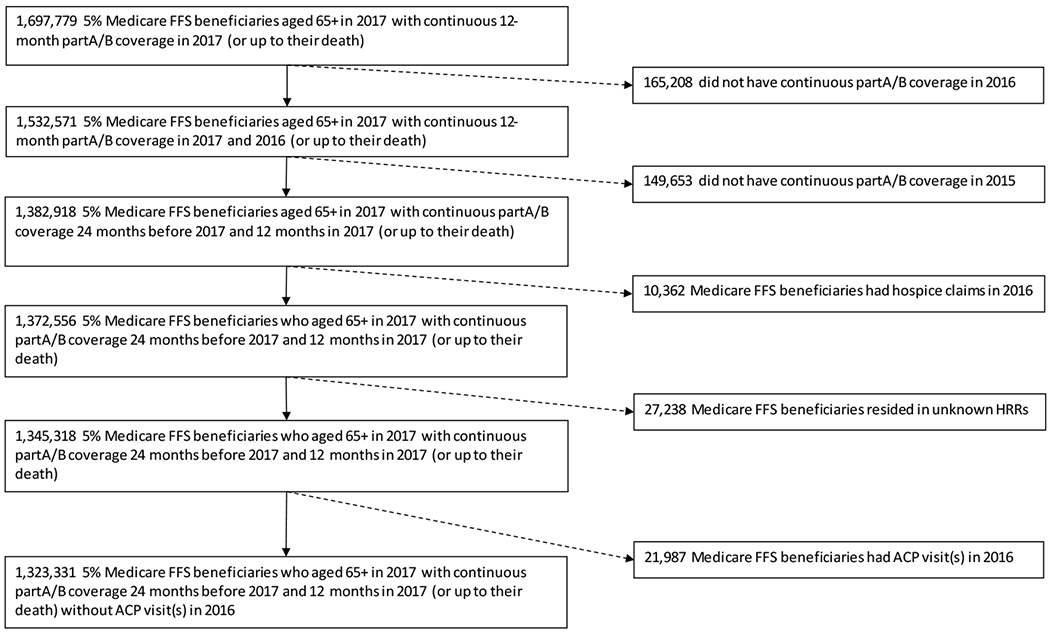
Cohort selection diagram
Outcome Measures
The primary outcome was receipt of a billed ACP visit in 2017, identified through Current Procedural Terminology codes 99497 or 99498 through Medicare carrier files, as a binary variable (Yes/No). Proportion of beneficiaries who had a billed ACP visit(s) by region was calculated.
Covariates
Covariates were selected based on the prior theoretical and empirical evidence for predicting ACP engagement (Supplementary Table S1).7 Patient-level factors included age, sex, race/ethnicity, dual eligibility, original reason for eligibility, comorbidities and medical care utilization in 2016. Medicare care utilization included number of hospitalizations, emergency department visits, ICU stays, home health service episodes, skilled nursing home (SNF) stays, and home-away days (number of inpatient days and SNF days) within 12-month time period prior to January 1, 2017.
Regional-level factors included measures to account for possible volume-outcome associations including, hospital beds per 1,000 beneficiaries, emergency department visits per 1,000 beneficiaries, percent of beneficiaries using hospice. We also included standardized total Medicare reimbursements per capita in hospital referral region (HRR)-level as a measure of overall levels of healthcare utilization in HRR.14 While a large number of regional factors may contribute to ACP, we focused on these variables to focus on the extent to which ACP visits are explained by general variation in regional intensity of care. HRRs, developed by the Dartmouth Atlas of Health Care to represent regional health care markets, were used to assess geographic variation across 306 regions in the US. We characterized region factors by quintiles. Beneficiaries’ region factors were determined by zip code of their residence.
Statistical Analysis
We conducted descriptive statistics to compare beneficiaries’ characteristics between those who underwent a billed ACP visit in 2017 and those who did not, using chi-square tests for categorical variables and t-test for continuous variables. To characterize billed ACP visits at the HRR level, we examined the proportion of beneficiaries who underwent billed ACP visits and characterized regions by quintiles of ACP use. To determine whether regional variation was associated with billed ACP visits, we fit a multi-level logistic regression model with a random regional intercept. The multilevel model included level-1 personal factors, level-2 regional factors, and a random intercept of HRR to account for correlated observations within region. We performed the analyses using PROC GLIMMIX procedure in SAS. The interclass correlation coefficient (ICC) was used to quantify the ratio of the between-region variance to the total variance, ranged from 0 (no variance between regions) to 1 (all variance was regional variance). We calculated the ICC initially using an unconditional model with a random intercept of HRR to estimate the variance in receiving billed ACP visits due to between-region differences which was compared to subsequent models that added covariate groups.15 All p values were two-sided and were determined statistically significant if p<0.05. We created maps using ArcGIS Pro (version 2.4.2; Esri). Map files containing HRR shape files were accessed from the Dartmouth Atlas Data. 16
After completing our primary analyses, we then performed a post-hoc set of analyses to try to explore the unique role of providers. In the optimal scenario we would fit a 3-level model nesting patients within providers within regions. However, given that numerous different provider types provide ACP visits and that there is no clear strategy for assigning patients to providers, we instead performed descriptive analyses to inform the general importance of providers on billed ACP visits and attempt to clarify the relative contributions of provider variation to regional variation. Thus we explored the distribution of billed ACP visits across providers and the proportion of physicians within each HRR who submitted an ACP claim. We then qualitatively compared, regional variation in billed ACP visits and regional variation in providers who perform billed ACP visits. For beneficiaries who died early in 2017, defined as died within first three months of 2017, it is possible that they might undergo ACP for different reasons than those who do not die or their underutilization of billed ACP visits might be less as the use of the ACP codes increases over time. Thus, we conducted a sensitivity analysis excluding beneficiaries who died in the first three months of 2017. All statistical analyses were performed with SAS version 9.4 (SAS Institute, Inc., Caray, NC).
Results
The study population consisted of about 1.3 million beneficiaries of which 32,137 (2.4%) received at least one billed ACP visit in 2017. Table 1 shows the demographic, clinical and regional characteristics of the population and of those who did and did not have a billed ACP visit. Mean (SD) age was 76.1 (7.7) years, 54.5% were women, 81.5% were non-Hispanic white, and 7.4% were Black. Over one-tenth (11.7%) were dual-eligible for Medicare and Medicaid.
Table 1.
Demographic, clinical and regional characteristics of the population and of those with and without an ACP visit
| Total | ACP | No ACP | ||
|---|---|---|---|---|
| N (row%) | N (row%) | N (row%) | ||
| N=1323331 (100) | N=32137 (2.4) | N=1291194 (97.6) | ||
| Patient Level | Mean (SD) | Mean (SD) | Mean (SD) | T test p value |
| Age | 76.1 (7.7) | 78.4 (8.1) | 76.04 (7.7) | <.0001 |
| Sex | N (col%) | N (col%) | N (col%) | Chi-square p value |
| Male | 602695 (45.5) | 13077 (40.7) | 589618 (45.7) | <.0001 |
| Female | 720636 (54.5) | 19060 (59.3) | 701576 (54.3) | |
| Race/Ethnicity | ||||
| Non-Hispanic White | 1078540 (81.5) | 25946 (80.7) | 1052594 (81.5) | <.0001 |
| Black | 97517 (7.4) | 2542 (7.9) | 94975 (7.4) | |
| Hispanics | 69602 (5.3) | 1813 (5.6) | 67789 (5.3) | |
| Others | 56818 (4.3) | 1537 (4.8) | 55281 (4.3) | |
| Unknown | 20854 (1.6) | 299 (0.9) | 20555 (1.6) | |
| Dual Eligibility | 155091 (11.7) | 5339 (16.6) | 149752 (11.6) | <.0001 |
| Original Medicare Eligible Reason | ||||
| old age | 1207753 (91.3) | 28949 (90.1) | 1178804 (91.3) | <.0001 |
| disability | 113342 (8.6) | 3101 (9.7) | 110241 (8.5) | |
| ESRD | 1286 (0.1) | 50 (0.2) | 1236 (0.1) | |
| both disability and ESRD | 950 (0.1) | 37 (0.1) | 913 (0.1) | |
| Medical Care Utilization in 2016 | Mean (SD) | Mean (SD) | Mean (SD) | T test p value |
| # Hospitalization | 0.22 (0.7) | 0.39 (1) | 0.21 (0.7) | <.0001 |
| # ED visits | 0.34 (1) | 0.51 (1.2) | 0.33 (1) | <.0001 |
| # ICU visits | 0.06 (0.3) | 0.11 (0.4) | 0.05 (0.3) | <.0001 |
| # HHA episode | 0.15 (0.7) | 0.34 (1) | 0.15 (0.7) | <.0001 |
| # SNF stays | 0.05 (0.3) | 0.11 (0.5) | 0.05 (0.3) | <.0001 |
| # Home-away days | 1.54 (15.3) | 3.09 (13.2) | 1.51 (15.3) | <.0001 |
| Charlson Comorbidity Scores | N (col%) | N (col%) | N (col%) | Chi-square p value |
| 0 | 738947 (55.8) | 12149 (37.8) | 726798 (56.3) | <.0001 |
| 1 | 205813 (15.6) | 5621 (17.5) | 200192 (15.5) | |
| 2+ | 378571 (28.6) | 14367 (44.7) | 364204 (28.2) | |
| Comorbid conditions in 2016 | ||||
| Acute MI (w/ or w/o history of MI) | 12243 (1) | 503 (1.6) | 11740 (0.9) | <.0001 |
| History of MI (no Acute MI in 2016) | 22136 (1.7) | 929 (2.9) | 21207 (1.6) | <.0001 |
| CHF | 92797 (7.0) | 4245 (13.2) | 88552 (6.9) | <.0001 |
| PVD | 109231 (8.3) | 4636 (14.4) | 104595 (8.1) | <.0001 |
| CVD | 66671 (5.0) | 2763 (8.6) | 63908 (5) | <.0001 |
| COPD | 137676 (10.4) | 5500 (17.1) | 132176 (10.2) | <.0001 |
| Dementia | 59253 (4.5) | 2731 (8.5) | 56522 (4.4) | <.0001 |
| Paralysis | 7935 (0.6) | 355 (1.1) | 7580 (0.6) | <.0001 |
| Diabetes | 138793 (10.5) | 3983 (12.4) | 134810 (10.4) | <.0001 |
| Diabetes w/ complications | 130621 (9.9) | 5274 (16.4) | 125347 (9.7) | <.0001 |
| renal disease | 116441 (8.8) | 5037 (15.7) | 111404 (8.6) | <.0001 |
| mild liver disease | 15591 (1.2) | 585 (1.8) | 15006 (1.2) | <.0001 |
| moderate/severe liver disease | 2311 (0.2) | 128 (0.4) | 2183 (0.2) | <.0001 |
| ulcers | 7480 (0.6) | 293 (0.9) | 7187 (0.6) | <.0001 |
| rheumatic disease | 43288 (3.3) | 1465(4.6) | 41823 (3.2) | <.0001 |
| aids | 955 (0.1) | 26 (0.1) | 929 (0.1) | 0.5549 |
| Metastatic solid tumor | 11848 (0.9) | 584 (1.8) | 11264 (0.9) | <.0001 |
| Other cancer | 90042 (6.8) | 3170 (9.9) | 86872 (6.7) | <.0001 |
| Regional Level | Mean (SD) | Mean (SD) | Mean (SD) | T test p value |
| # Hospital beds per 1000 65+ Medicare beneficiaries | 15.8 (4.2) | 15.86 (4.3) | 15.85 (4.2) | <.0001 |
| # Emergency Department visits per 1000 65+ Medicare beneficiaries | 589.7 (64.5) | 585.5 (62.6) | 589.8 (64.5) | <.0001 |
| % beneficiaries using hospice | 2.48 (1.5) | 2.45 (1.5) | 2.48 (1.5) | <.0001 |
| Standardized Per Capita Costs | 9553.5 (1158.8) |
9719.9 (1170.9) |
9549.3 (1158.1) | <.0001 |
| # Hospital beds per 1000 65+ Medicare beneficiaries | N (col%) | N (col%) | N (col%) | Chi-square p value |
| 1st quintile (≤11.9) | 223318 (16.9) | 5600 (17.4) | 217718 (16.9) | <.0001 |
| 2nd quintile (11.91-14.3) | 313197 (23.7) | 7820 (24.3) | 305377 (23.7) | |
| 3rd quintile (14.31-16.2) | 258217 (19.5) | 6140 (19.1) | 252077 (19.5) | |
| 4th quintile (16.21-19.5) | 306093 (23.1) | 7061 (22) | 299032 (23.2) | |
| 5th quintile (>19.5) | 222506 (16.8) | 5516 (17.2) | 216990 (16.8) | |
| # Emergency Department visits per 1000 65+ Medicare beneficiaries | ||||
| 1st quintile (≤533) | 303613 (22.9) | 7774 (24.2) | 295839 (22.9) | <.0001 |
| 2nd quintile (534-578) | 287426 (21.7) | 7271 (22.6) | 290155 (21.7) | |
| 3rd quintile (579-620) | 314874 (23.8) | 7789 (24.2) | 307085 (23.8) | |
| 4th quintile (621-655) | 232302 (17.6) | 5742 (17.9) | 226560 (17.6) | |
| 5th quintile (>655) | 185116 (14) | 3561 (11.1) | 181555 (14.1) | |
| % beneficiaries using hospice | ||||
| 1st quintile (≤0.0385) | 291819 (22.1) | 7386 (23) | 284433 (22.0) | <.0001 |
| 2nd quintile (0.0386-2.81999) | 244764 (18.5) | 5800 (18.15) | 238964 (18.5) | |
| 3rd quintile (2.82-3.25) | 318635 (24.1) | 8290 (25.8) | 310345 (24.0) | |
| 4th quintile (3.26-3.74) | 267588 (20.2) | 6216 (19.3) | 261372 (20.2) | |
| 5th quintile (>3.74) | 200525 (15.2) | 4445 (13.8) | 196080 (15.2) | |
| Standardized Per Capita Costs | ||||
| 1st quintile (≤$8319.23) | 199767 (15.1) | 3811 (11.9) | 195956 (15.2) | <.0001 |
| 2nd quintile ($8319.24-$9102.01) | 246970 (18.7) | 5365 (16.7) | 241605 (18.7) | |
| 3rd quintile ($9102.02-$9768.95) | 283258 (21.4) | 6760 (21.0) | 276498 (21.4) | |
| 4th quintile ($9768.96-$10464.18) | 306669 (23.2) | 7342 (22.9) | 299327 (23.2) | |
| 5th quintile (>$10464.18) | 286667 (21.7) | 8859 (27.6) | 277808 (21.5) |
Overall, a higher proportion of beneficiaries who were older and those with more comorbidities were more likely to have a billed ACP visit compared with beneficiaries who did not have a billed ACP visit (Table 1). A higher proportions of women compared to men and dual-eligible beneficiaries compared to non dual-eligible beneficiaries had an ACP visit. Very small difference in regional variables were noted, with the largest difference in per capita costs. The regional mean per capita cost was $9720 among beneficiaries who had a billed ACP visit compared to $9549 among beneficiaries without a billed ACP visit.
Among those with a billed ACP visit, 29,496 (92%) had ACP visit(s) on one claim date and mostly with one ACP session only. The majority of billed ACP visits were provided by primary care physicians (70%: including general practice [1.2%], family practice [25.1%], and internal medicine [43.9%]) and nurse practitioners (16.9%).
There was substantial regional variation in billed ACP visits; lowest quintile region <0.83%, subsequent regions <1.6%, <2.4%, <3.3% to <8.4% in the highest quintile regions (Figure 2). The ICC for the unconditional model (i.e., only HRR as the random intercept) was 15.4%, indicating that 15.4% of the variance in whether an older adult had a billed ACP visit was explained by the region (HRR). After including patient and regional predictors of billed ACP visits, the ICC decreased to 13.2%.
Figure 2.
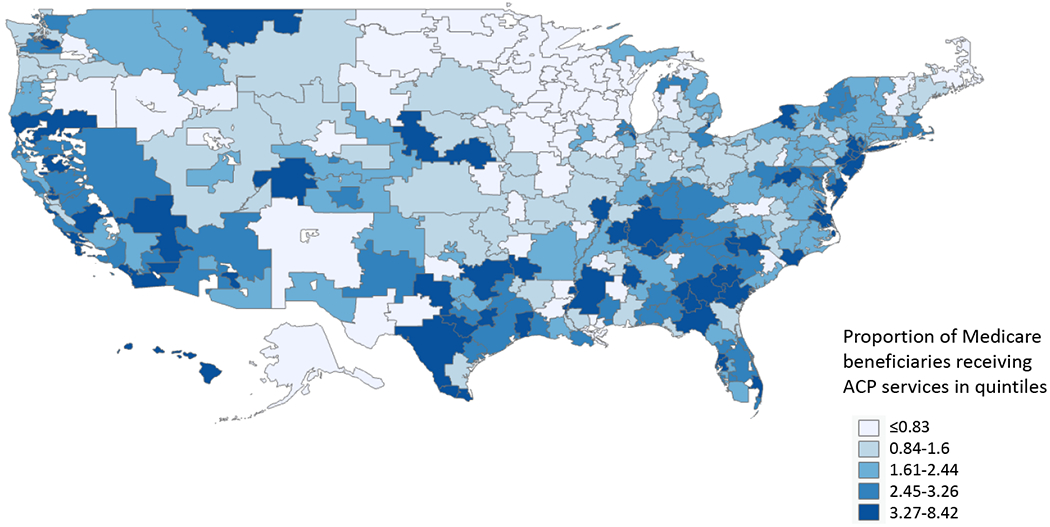
Geographic variation in proportion of Medicare beneficiaries receiving billed ACP visits in 2017 Proportion of Medicare beneficiaries receiving ACP visits in quintiles
≤0.83
0.84-1.60
1.61-2.44
2.45-3.26
3.27-8.42
In the fully adjusted model accounting for patient and regional factors (C-statistic: 0.7063) (Supplementary Figure S1), age was the factor that explained the most variance in ACP visits (Table 2). For every year increase, the odds of a billed ACP visit increased by 1.027 (95% CI,1.025-1.028). Women (OR 1.17 [95% CI 1.15-1.2]), dual eligible beneficiaries (OR 1.15 [95% CI 1.11-1.19]), and those with comorbidities were more likely to have a billed ACP visit. Racial/ethnic minorities were less likely to have a billed ACP visit (black vs. white: OR 0.85 [95% CI 0.81-0.88]; Hispanics vs white: OR 0.84 [95% CI 0.8-0.89]). Overall, the magnitude of the associations between medical care utilization and ACP were small. ED visits (OR 1.03 [95% CI 1.03-1.04]) and HHA episodes (OR 1.09 [95% CI 1.07-1.1]) were associated with higher odds of an ACP visits, while ICU visits (OR 0.97 [95% CI 0.93-1]) decreased the odd of a billed ACP visit.
Table 2.
Multivariate logistic regression predicting receipt of ACP visits among Medicare beneficiaries
| OR (95% CI) | p value | |
|---|---|---|
| Patient Level | ||
| Age | 1.027 (1.025-1.028) | <.0001 |
| Sex | ||
| Male | 1 (reference) | |
| Female | 1.17 (1.15-1.2) | <.0001 |
| Race/Ethnicity | ||
| NH White | 1 (reference) | |
| Black | 0.85 (0.81-0.88) | <.0001 |
| Hispanics | 0.84 (0.8-0.89) | <.0001 |
| Others | 0.96 (0.91-1.02) | 0.2076 |
| Unknown | 0.79 (0.7-0.89) | <.0001 |
| Dual Eligibility | ||
| No | 1 (reference) | |
| Yes | 1.15 (1.11-1.19) | <.0001 |
| Original Medicare Eligible Reason | ||
| old age | 1 (reference) | |
| disability | 1.09 (1.05-1.13) | <.0001 |
| ESRD | 1.27 (0.95-1.69) | 0.1098 |
| both disability and ESRD | 1.22 (0.87-1.71) | 0.2585 |
| Medical care utilization in 2016 | ||
| # Hospitalization | 1.01 (0.99-1.03) | 0.4224 |
| # ED visits | 1.03 (1.03-1.04) | <.0001 |
| # ICU visits | 0.97 (0.93-1) | 0.0482 |
| # HHA episode | 1.09 (1.07-1.1) | <.0001 |
| # SNF stays | 1.03 (1-1.06) | 0.0615 |
| # Home away days | 1 (0.999-1) | 0.6616 |
| Comorbid conditions in 2016 | ||
| Acute MI (w/ or w/o history of MI) | 1 (0.91-1.1) | 0.9809 |
| History of MI (no Acute MI in 2016) | 1.05 (0.98-1.13) | 0.1828 |
| CHF | 1.19 (1.14-1.24) | <.0001 |
| PVD | 1.2 (1.16-1.24) | <.0001 |
| CVD | 1.16 (1.11-1.21) | <.0001 |
| COPD | 1.33 (1.28-1.37) | <.0001 |
| Dementia | 1.15 (1.1-1.2) | <.0001 |
| Paralysis | 1.08 (0.97-1.21) | 0.1705 |
| Diabetes | 1.22 (1.18-1.26) | <.0001 |
| Diabetes w/ complications | 1.4 (1.36-1.45) | <.0001 |
| renal disease | 1.24 (1.2-1.29) | <.0001 |
| mild liver disease | 1.17 (1.08-1.28) | 0.0003 |
| moderate/severe liver disease | 1.64 (1.36-1.97) | <.0001 |
| ulcers | 1.03 (0.91-1.16) | 0.6704 |
| rheum disease | 1.16 (1.1-1.22) | <.0001 |
| aids | 1.05 (0.71-1.54) | 0.8161 |
| Metastatic solid tumor | 1.88 (1.72-2.04) | <.0001 |
| Other cancer | 1.34 (1.29-1.4) | <.0001 |
| Regional Level | ||
| # Hospital beds per 1000 65+ Medicare beneficiaries | ||
| 1st quintile (low) | 1 (reference) | |
| 2nd quintile | 0.82 (0.63-1.07) | 0.1459 |
| 3rd quintile | 0.77 (0.58-1.02) | 0.0692 |
| 4th quintile | 0.77 (0.57-1.03) | 0.0812 |
| 5th quintile (high) | 0.74 (0.54-1.01) | 0.0548 |
| # Emergency Department visits per 1000 65+ Medicare beneficiaries | ||
| 1st quintile (low) | 1 (reference) | |
| 2nd quintile | 0.92 (0.7-1.2) | 0.5138 |
| 3rd quintile | 0.8 (0.61-1.06) | 0.117 |
| 4th quintile | 1 (0.76-1.33) | 0.9887 |
| 5th quintile (high) | 0.64 (0.47-0.87) | 0.0038 |
| % beneficiaries using hospice | ||
| 1st quintile (low) | 1 (reference) | |
| 2nd quintile | 0.97 (0.75-1.25) | 0.8004 |
| 3rd quintile | 0.97 (0.75-1.27) | 0.8444 |
| 4th quintile | 0.75 (0.58-0.98) | 0.0363 |
| 5th quintile (high) | 0.74 (0.56-0.98) | 0.0328 |
| Standardized Per Capita Costs | ||
| 1st quintile (low) | 1 (reference) | |
| 2nd quintile | 1.11 (0.84-1.47) | 0.4529 |
| 3rd quintile | 1.49 (1.1-2.02) | 0.01 |
| 4th quintile | 1.73 (1.26-2.38) | 0.0006 |
| 5th quintile (high) | 2.1 (1.5-2.95) | <.0001 |
Regarding regional factors, beneficiaries who resided in regions with highest quintile number of hospital beds was associated with a non-significant lower odds of a billed ACP visit (OR 0.74 [95% CI 0.54-1.01]) than those who resided in regions with the lowest quintile number of hospital beds (Table 2). Beneficiaries who resided in regions with highest quintile number of ED visits was associated with a lower odds of a billed ACP visit (OR 0.64 [95% CI 0.47-0.87]) than those who resided in regions with the lowest quintile number of ED visits, although there was not a clear dose-effect across quintiles. Regions with the highest hospice utilization (top utilizing quintile) were associated with a lower odds of a billed beneficiary ACP visit compared to the lowest quintile of hospice utilization (OR 0.74 [95% CI 0.56-0.98]) while regions with the highest quintile per capita costs were associate with the greater odds of a billed ACP visit (OR 2.1 [95% CI 1.5-2.95]) compared to the lowest quintile per capita regions.
In post-hoc analyses of regional variation of provider performance of billed ACP visits, we found significant variation (Figure 3) by region although overall there was low utilization of billed ACP visits by providers. On average only 2.2% of providers per region performed billed ACP visits. This varied from 0.7% (IQR, 0.38-0.87%) of providers in the lowest use quintiles to 5.1% (IQR, 4.3-6.6%) of providers in the regions with the highest visit quintile. The median number of billed ACP visits per provider was also low (2.2; IQR, 1.1-2.5).
Figure 3.
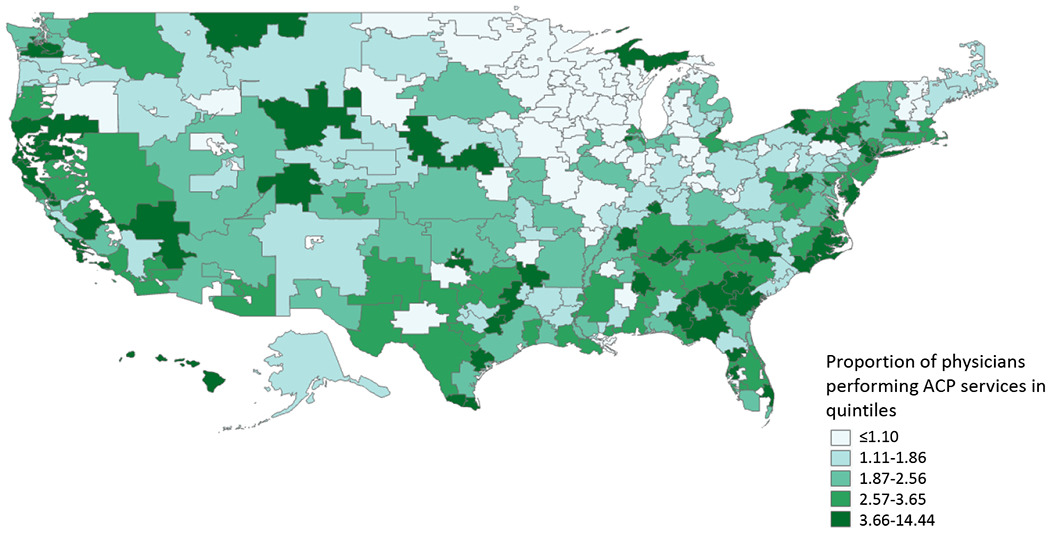
Geographic variation in proportion of providers performing billed ACP visits in 2017 Proportion of providers performing ACP visits in quintiles
≤1.10
1.11-1.86
1.87-2.56
2.57-3.65
3.66-14.44
In 2017, 13,970 (1.06%) beneficiaries died in the first three months. Those who died were more likely to have a billed ACP visit than those who did not (3.84% vs. 2.41%, p<.0001) and were more likely to be older, dual-eligible, utilize more medical care services in 2016, and have more comorbid conditions (Supplementary Table S2). In the sensitivity analysis excluding beneficiaries who died early in 2017, our findings were similar to the primary analyses (Supplementary Table S3).
Discussion
In this 2017 national sample of older Americans, we found that 2.4% had a billed ACP visit and that the use of billed ACP visits varied substantially by region. Most of the regional variation was not explained by patient and regional medical care factors indicating the need for additional research to understand the drivers of regional variation of ACP visits. ACP comes in many forms including advance directives, durable power of attorney and family discussions in addition to formal ACP visits.17 Thus, increasing billed ACP visits is not the only strategy to increase ACP. However, to the extent billed ACP visits increase ACP, they have the virtue of being potentially scalable to the magnitude of the challenge. By identifying the high and low performing regions, researchers can begin to explore barriers and facilitators to billed ACP visits.
The 2016 CMS reimbursement for ACP visits was in response to the commonly identified ACP barriers of lack of provider time and reimbursement for ACP.18 Yet, we found that billed ACP visits were infrequently used even in the second year of availability. The reasons for this low use are not clear but could relate to insufficient patient and provider knowledge about the code, insufficient financial incentive, or a lack of interest or medical engagement by the estimated 27% of older adults without prior ACP.9 In addition, provider discussions about ACP do not require an ACP code – these discussions can still take place without submitting a claim or by using typical evaluation and management codes as was done prior to 2016.
We found that at most about 8.4% of beneficiaries in a region had a ACP claim one year after the roll out. These early adopting regions may be a forecast of the volume of visits that can be expected as billed ACP visits continue to increase over time and inform goal setting of billed ACP visit rates. Several regional factors were associated with billed ACP visits that may inform efforts to increase ACP visits. Beneficiaries in regions with greater hospice utilization were less likely to have a billed ACP visit. This may be because beneficiaries in these regions had already established their ACP and thus further discussions to update their ACP were not thought to warrant an ACP claim. It will be important to test this hypothesis overtime as more beneficiaries enter Medicare in the time of ACP claim availability. Billed ACP visits were associated with higher per capita spending suggesting that more ACP visits are billed in higher billing regions. Overall inclusion of regional variables accounted for a small proportion of the variation in the models. These variables focused on regional intensity of overall medical care. This suggests that further work is needed to understand the more complex interplay of regional level factors on regional differences in ACP.
Future work could determine whether billed ACP visits are associated with health care utilization outcomes. While the association between ACP and patient centered and health care utilization outcomes is well established,2, 5 less is known about the impact specifically of billed ACP visits on outcomes. For example, billed ACP visits are associated with healthcare utilization among seriously ill Medicare Advantage Beneficiaries, whether this association extends to older adults outside this population is unknown.19 Similarly, exploring the association of billed ACP visits and concordance with care received at the end of life is also important. Future research could consider using regional variation in billed ACP visits as an instrumental variable to explore outcomes such as ICU, life prolonging treatment, and hospice utilization and how these align with individual preferences. We anticipate that over time as ACP claims increase so will the strength of ACP visits as an instrumental variable, strengthening these future analyses.
Our study has limitations. First, it is likely that ACP occurred outside of these billed ACP visits such that our measures are likely an underestimate of ACP. Similarly, it is impossible to know whether regions with high billing of ACP visits perform more ACP or have better optimized coding systems. Second, data on the quality of the ACP visit is not available. However, specifically ACP visits can include a discussion and are not predicated on completion of an advance directive. Early data suggests that ACP visits are not limited to only completion of advance directives.20 Third, although the primary focus of our study was regional factors that relate to ACP visits, our models predicting ACP visits are limited by not having provider level data. However, individual providers seem unlikely to be a major driver of ACP claim use in 2017 since both the number of providers using ACP claims and the number of claims per provider were low even in high use regions. In addition, inclusion of additional regional variables could be included in future studies. Finally, our findings are limited to older adults, given the sample was drawn from Medicare.
In conclusion, 2.4% of beneficiaries had a billed ACP visit in 2017 and this proportion varied by region. Additional work is needed to understand regional drivers of ACP visits in order to inform regions with low utilization of ACP visits.
Supplementary Material
Supplementary Table S1. Definition of covariates
Supplementary Table S2. Demographic, clinical and regional characteristics of the total population and of those who died within the first three months of 2017 and those who did not die within the first three months of 2017
Supplementary Table S3. Multivariate logistic regression predicting receipt of ACP visits among Medicare beneficiaries who did not die within the first three months of 2017
Supplementary Figure 1. ROC curve for model predicting the odds of receiving ACP services in 2017
Acknowledgements
Sponsors role: Funding was provided by the NIH NIA R01AG059733
Funding:
NIH/NIA R01AG059733
Footnotes
Paper presentation: None
Conflict of interest: none
References
- [1].Sudore RL, Lum HD, You JJ, et al. Defining Advance Care Planning for Adults: A Consensus Definition From a Multidisciplinary Delphi Panel. Journal of Pain and Symptom Management. 2017;53: 821–832.e821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Silveira MJ, Kim SY, Langa KM. Advance directives and outcomes of surrogate decision making before death. New England Journal of Medicine. 2010;362: 1211–1218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Houben CHM, Spruit MA, Groenen MTJ, Wouters EFM, Janssen DJA. Efficacy of Advance Care Planning: A Systematic Review and Meta-Analysis. Journal of the American Medical Directors Association. 2014;15: 477–489. [DOI] [PubMed] [Google Scholar]
- [4].Wright AA, Zhang B, Ray A, et al. Associations Between End-of-Life Discussions, Patient Mental Health, Medical Care Near Death, and Caregiver Bereavement Adjustment. JAMA. 2008;300: 1665–1673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Bischoff KE, Sudore R, Miao Y, Boscardin WJ, Smith AK. Advance Care Planning and the Quality of End-of-Life Care in Older Adults. Journal of the American Geriatrics Society. 2013;61: 209–214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Detering KM, Hancock AD, Reade MC, Silvester W. The impact of advance care planning on end of life care in elderly patients: randomised controlled trial. The BMJ. 2010;340: c1345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Harrison KL, Adrion ER, Ritchie CS, Sudore RL, Smith AK. Low Completion and Disparities in Advance Care Planning Activities Among Older Medicare Beneficiaries. JAMA Internal Medicine. 2016;176: 1872–1875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Mehta A, Kelley AS. Advance Care Planning Codes—Getting Paid for Quality Care. JAMA Internal Medicine. 2019;179: 830–831. [DOI] [PubMed] [Google Scholar]
- [9].Wright MS. Change without Change? Assessing Medicare Reimbursement for Advance Care Planning. Hastings Center Report. 2018;48: 8–9. [DOI] [PubMed] [Google Scholar]
- [10].Belanger E, Loomer L, Teno JM, Mitchell SL, Adhikari D, Gozalo PL. Early utilization patterns of the new Medicare procedure codes for advance care planning. JAMA internal medicine. 2019;179: 829–830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Pelland K, Morphis B, Harris D, Gardner R. Assessment of first-year use of Medicare’s advance care planning billing codes. JAMA internal medicine. 2019;179: 827–829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].CMS Public Use File. https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/Medicare-Geographic-Variation/GV_PUF. Accessed February 17, 2020.
- [13].Dartmouth Data Atlas. https://atlasdata.dartmouth.edu/static/supp_research_data#hospital-research-data. Accessed February 17, 2020. [Google Scholar]
- [14].Newhouse JP, Garber AM. Geographic variation in Medicare services. N Engl J Med. 2013;368: 1465–1468. [DOI] [PubMed] [Google Scholar]
- [15].Multilevel Models for Categorical Data Using SAS® PROC GLIMMIX: The Basics https://support.sas.com/resources/papers/proceedings15/3430-2015.pdf. Accessed April 16, 2020.
- [16].Dartmouth Atlas Data. https://atlasdata.dartmouth.edu/static/suppresearchdata 16, 2020. [Google Scholar]
- [17].Sudore RL, Fried TR. Redefining the “planning” in advance care planning: preparing for end-of-life decision making. Annals of internal medicine. 2010;153: 256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Issues IoMCoADAKE-o-L. Dying in America: Improving Quality and Honoring Individual Preferences Near the End of Life, 2015. [PubMed] [Google Scholar]
- [19].Ashana DC, Chen X, Agiro A, et al. Advance Care Planning Claims and Health Care Utilization Among Seriously Ill Patients Near the End of Life. JAMA Network Open. 2019;2: e1914471–e1914471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Kim K, Lehning AJ, Sacco P. Assessing the factor structure of well-being in older adults: findings from the National Health and Aging Trends Study. Aging & mental health. 2015: 1–9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Table S1. Definition of covariates
Supplementary Table S2. Demographic, clinical and regional characteristics of the total population and of those who died within the first three months of 2017 and those who did not die within the first three months of 2017
Supplementary Table S3. Multivariate logistic regression predicting receipt of ACP visits among Medicare beneficiaries who did not die within the first three months of 2017
Supplementary Figure 1. ROC curve for model predicting the odds of receiving ACP services in 2017


