Abstract
Purpose
There is a growing concern about the COVID-19 epidemic intensifying in rural areas in the United States (U.S.). In this study, we described the dynamics of COVID-19 cases and deaths in rural and urban counties in the U.S.
Methods
Using data from April 1 to November 12, 2020, from Johns Hopkins University, we estimated COVID-19 incidence and mortality rates and conducted comparisons between urban and rural areas in three time periods at the national level, and in states with higher and lower COVID-19 incidence rates.
Results
Results at the national level showed greater COVID-19 incidence rates in urban compared to rural counties in the Northeast and Mid-Atlantic regions of the U.S. at the beginning of the epidemic. However, the intensity of the epidemic has shifted to a rapid surge in rural areas. In particular, high incidence states located in the Mid-west of the country had more than 3,400 COVID-19 cases per 100,000 people compared to 1,284 cases per 100,000 people in urban counties nationwide during the third period (August 30 to November 12).
Conclusions
Overall, the current epicenter of the epidemic is located in states with higher infection rates and mortality in rural areas. Infection prevention and control efforts including healthcare capacity should be scaled up in these vulnerable rural areas.
Keywords: Covid-19, United states: rural areas, Spatial epidemiology, Disease mapping
Introduction
The United States (U.S.) has the highest number of COVID-19 cases in the world, with 13,386,255 confirmed cases as of November 29, 2020. From the beginning of May to mid-November 2020, the number of confirmed COVID-19 cases in the U.S. has steadily increased, whereas the rate of COVID-19-related hospitalizations and mortality has declined[1]. However, there is substantial spatial and temporal variation in the dynamics of the epidemic within the U.S.[2], [3], [4], with New York, New Jersey and Maryland experiencing the highest burden of the infection early in the epidemic. The epicenter of the disease shifted to the southern U.S. from June to September of 2020, followed by a surge in the Midwest in late September. Furthermore, there is a growing concern about the epidemic worsening in rural areas, which are characterized by lower healthcare capacity, thus placing residents at higher risk of COVID-19 infection and death[4], [5], [6].
Rural areas in the United States face many challenges including lower healthcare resources compared to urban communities. For example, over 4.7 million people live in 460 rural counties across the nation where there are no general medical or surgical hospital beds. In addition, 16.4 million people live in rural areas with no medical/surgical intensive care unit (ICU) beds[7]. Rural residents have a shorter life expectancy than urban residents and rural households also report a lower median income[8]. According to the World Health Organization (WHO), older people are at the highest risk of COVID-19 morbidity and mortality[9]. In the 2016 U.S. Census, the median age of rural area residents was 51 years, whereas the median age in urban areas was 45[10]. Rural communities also have a larger proportion of residents 65 years and older (18.4% compared to 14.5%)[8]. The proportion of older adults is increasing more quickly in rural communities due to declining birth rates and migration patterns in younger adults[11].
With rural communities already at a disadvantage in terms of healthcare and population demographics, and with COVID-19 proving to be a more intense burden on older populations, rural areas are in greater danger compared to urban areas. In this study, we estimated COVID-19 incidence and mortality rates to compare urban and rural areas in the U.S. during three time periods in 2020.
Methods
COVID-19 data from April 1 to November 12, 2020, obtained from Johns Hopkins University[12] for 3108 counties in the 48 contiguous U.S. states, were used in our analyses. The study dataset contained records for 10,143,327 COVID-19 cases and 234,186 COVID-19 related deaths. We classified counties as rural or urban based on the 2013 National Center for Health Statistics urban classification methodology[13]. The criteria for metropolitan (urban) counties ranges from small metropolitan areas with population size less than 250,000 people to large metropolitan areas with more than one million people, and nonmetropolitan (rural) counties are those with population less than 50,000. We classified 1160 counties as urban (blue in Supplementary Fig. 1) and 1948 as rural counties (purple in Supplementary Fig. 1). Population density per county in 2019 was obtained from ESRI estimates derived from the 2010 U.S. Census population count[14].
We estimated temporal changes in COVID-19 incidence and mortality rates in urban and rural areas by evaluating three 75-day time intervals in 2020. The first-time interval from April 1 to June 15 included the time of initiation of intervention measures against the pandemic (i.e., lockdowns and stay home orders). Interventions were eased during the second time interval from June 16 to August 29, while the third interval from August 30 to November 12 corresponded to the surge of the third wave of the epidemic in the U.S. To illustrate temporal changes in both COVID-19 incidence and mortality rates, we generated choropleth maps at the county level to compare rates in each period. We also categorized states into two groups based on incidence rates. States in the highest quartile of COVID-19 incidence rates in the third period (that illustrates the current stage of the epidemic at the moment in which the study was conducted) were included in the “higher incidence rate states,” while the remaining states were included in the “lower incidence rate states,” and these groups were used as reference to retrospectively generate comparison between groups during the three periods.
To estimate the COVID-19 incidence and mortality rate for each period, we analyzed data on urban and rural cases at the national level as well as by high/low incidence states for each time interval. For example, we calculated the incidence rate in an urban area as the number of cases divided by the population size of the area (with the result reported per 100,000 people), and then calculated a 95% confidence interval for a Poisson rate using an exact method with the “pois.exact” function in the R environment[15]. We conducted comparisons of the COVID-19 incidence and mortality rates between urban and rural areas among the three different time intervals at the national level, and in the states with higher and lower COVID-19 incidence rates by computing Poisson rates of COVID-19 incidence (or mortality) for two different time periods. In this analysis it is assumed that (incidence or mortality) counts Y and X at two time periods vary according to Poisson distributions, and , and the parameter of interest is the rate ratio between the two time periods, . The values n and m are the number of persons at risk in each time period considered. We used the uniformly most powerful unbiased procedure for estimating rate ratios. This procedure is based on conditioning on the sum X + Y, yielding
where
Rate ratio analyses were conducted using the rateratio.test package in the R programming environment version 3.5.2[15]. This study followed the guidelines of the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE)[16].
Results
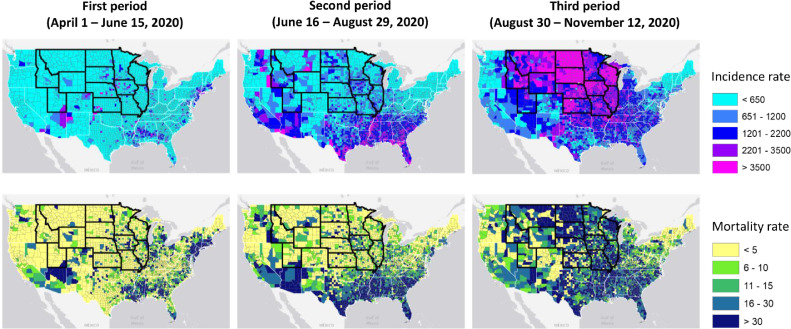
There was a total of 8613,630 cases and 204,873 deaths from COVID-19 in urban areas, and 1529,697 cases and 29,313 deaths in rural areas during the entire study period. North Dakota (ND; 6255 COVID-19 cases per 100,000 people), South Dakota (SD; 5400), Wisconsin (WI; 4032), Iowa (IA; 3384), Montana (MT; 3338), Nevada (NE; 3008), Wyoming (WY; 2884), Utah (UT; 2872), Idaho ID; (2607), Illinois (IL; 2407), Kansas (KS; 2394), and Missouri (MO; 2355) were states in the highest COVID-19 incidence rates quartile during the third period and were categorized as “higher incidence rate states”, with an average of 2946 cases per 100,000 people (95% confidence interval [CI]: 2940 – 2951). The remaining states were classified as “lower incidence rate states”, with an average of 1152 cases per 100,000 people (95% CI: 1151 – 1154) in the third time period (Fig. 1 ). We found that COVID-19 incidence rates were higher in rural counties, compared to urban counties, in the third period in 10 of the 12 higher incidence states (SD, WI, IA, MT, NE, WY, ID, IL, KS, MO; Supplementary Fig. 2).
Fig. 1.
Spatial distribution of COVID-19 incidence rates per 100,000 people (maps on the top), and spatial distribution of COVID-19 related mortality rates per 100,000 people (maps on the bottom) during the three time periods of the study. High incidence states are delineated with a thick dark line. Maps were created using ArcGIS by ESRI version 10.3 (http://www.esri.com)[29].
The Table 1 presents, estimates of COVID-19 incidence and mortality rates at the national level, as well as for higher and lower incidence rate states for the three periods. Nationally, the COVID-19 incidence rate was higher in urban counties compared to rural counties in the first two periods, but rural counties had the highest incidence rate in the third period. The COVID-19 incidence rate in rural counties increased by over 180% from the first to the second period (rate ratio [RR]: 2.86; 95% CI: 2.85 – 2.88; P < .001), and by over 80% from the second to the third period (RR: 1.88; 95% CI: 1.87–1.88; P < .001). In urban counties, the incidence rate increased by 90% from the first to the second period (RR: 1.92; 95% CI; 1.91 – 1.93; P < .001), but remained almost the same from the second to the third period, with a modest increase of only 9%. Among the higher incidence rate states, incidence rates were significantly higher during the first two periods in urban counties. In the third period, the incidence rate was more than 25% higher in rural compared to urban counties (RR: 1.27; 95% CI: 1.26 – 1.28; P < .001).
Table 1.
COVID-19 incidence and mortality rates in urban and rural counties at the national level, and in states with higher or lower incidence rates. Incidence and mortality rates are reported per 100,000 people with their corresponding confidence interval (CI)
| Area | Zone | Estimate | First period(April 1 - June 15)rate (95% CI) | Second period(June 16 - August 29)rate (95% CI) | Third period(August 30 – November 12)rate (95% CI) | Rate ratio (95% CI)Second period/first period | Rate ratio (95% CI)Third period/second period |
| Urbancounties | National | Incidence rate | 611.32 (610.41 – 612.23) | 1174.64 (1173.37 – 1175.91) | 1284 (1283.07 – 1285.72) | 1.92 (1.91 – 1.93) | 1.09 (1.09 – 1.10). |
| Mortality rate | 36.92 (36.74 – 37.19) | 20.37 (20.21 – 20.54) | 15.56 (15.42 – 15.71) | 0.55 (0.54 – 0.56) | 0.76 (0.75 – 0.77) | ||
| States withhigher incidence rate | Incidence rate | 657.45 (654.77 – 660.14) | 995.28 (991.98 – 998.58) | 2684.45 (2679.03 – 2689.87) | 1.51 (1.50 – 1.52) | 2.69 (2.68 – 2.70) | |
| Mortality rate | 27.73 (27.18 – 28.28) | 11.18 (10.83 – 11.53) | 18.06 (17.62 – 18.51) | 0.40 (0.38 – 0.41) | 1.61 (1.55 – 1.68) | ||
| States withlower incidence rate | Incidence rate | 604.71 (603.74 – 605.68) | 1200.35 (1198.98 – 1201.72) | 1083.75 (1082.45 – 1085.05) | 1.99 (1.98 – 2.00) | 0.90 (0.90–0.91) | |
| Mortality rate | 38.29 (38.05 – 38.54) | 21.69 (21.5 – 21.87) | 15.34 (15.18 – 15.49 | 0.57 (0.56 – 0.58) | 0.71 (0.69 – 0.72) | ||
| Ruralcounties | National | Incidence rate | 363.72 (361.72 – 365.22) | 1040.95 (1037.99 – 1043.92) | 1953.78 (1949.73 – 1957.85) | 2.86 (2.85 – 2.88) | 1.88 (1.87 – 1.88) |
| Mortality rate | 13.84 (13.51 – 14.19) | 19.79 (19.38 – 20.21) | 30.71 (30.21 – 31.29) | 1.43 (1.38 – 1.48) | 1.55 (1.51 – 1.59) | ||
| States withhigher incidence rate | Incidence rate | 332.68 (329.33 – 336.04) | 754.46 (749.42 – 759.52) | 3413.58 (3402.87 – 3424.32) | 2.26 (2.24 – 2.29) | 4.52 (4.49 – 4.55) | |
| Mortality rate | 6.42 (5.96 – 6.91) | 8.22 (7.71 – 8.77) | 35.52 (34.43 – 36.63) | 1.28 (1.16 – 1.41) | 4.32 (4.02 – 4.64) | ||
| States withlower incidence rate | Incidence rate | 363.01 (361.01 – 365.00) | 1103.89 (1107.37 – 1107.37) | 1424.58 (1420.64 – 1428.53) | 3.04 (3.02 – 3.06) | 1.29 (1.28 – 1.29) | |
| Mortality rate | 15.85 (15.44 – 16.27) | 22.97 (22.47 – 23.48) | 28.27 (27.72 – 28.83) | 1.45 (1.40 – 1.49) | 1.23 (1.19–1.27) |
Nationally, COVID-19 mortality rates sharply declined in urban areas over time, with the highest decline occurring between the first and second time periods (RR: 0.55; 95% CI: 0.54 - 0.56; P < .001), and then declined 30% from the second to the third period (RR: 0.76; 95% CI: 0.75 – 0.77). Conversely, COVID-19 related mortality across the nation significantly increased in rural areas from the first to the second period (RR: 1.43; 95% CI: 1.38 – 1.48; P < .001) and had the highest increase, with more than 50% increase in the mortality rate from the second to the third period (RR: 1.55; 95% CI: 1.51 – 1.59; P < .001). The highest mortality rate occurred in rural states with higher incidence rate during the third period, with a COVID-19 related mortality rate of 35.52 per 100,000 people (95% CI: 34.43 – 36.63).
Discussion
We assessed the patterns of COVID-19 incidence and mortality rates during intervention and post-intervention periods for rural and urban counties in the U.S. Our results suggest that the COVID-19 landscape in the U.S. is dynamic with substantial changes over time and space. Although results at the national level indicated greater COVID-19 incidence rates in urban compared to rural counties in the Northeast and Mid-Atlantic regions of the U.S. at the beginning of the epidemic, the intensity of the epidemic shifted to a rapid surge in rural areas, particularly in high incidence states located in the Mid-west of the country with more than 3400 cases per 100,000 people (compared to 1284 cases estimated for urban counties) during the third period. Urban counties experienced a rapid increase of COVID-19 infections after easing of lockdown restrictions in the second period (June 16 – August 29, 2020), but infection rates remained stable during the third period (August 30 – November 12). Conversely, there was a rapid surge of infections in rural areas with an incidence rate increasing from about 350 cases per 100,000 people in the first period to more than 1000 cases in the second period, and contrary to the pattern observed in urban areas, the infection rate continued increasing in rural counties, reaching almost 2000 cases in the third period.
Reasons for the differential temporal dynamics between urban and rural areas can be manifold. COVID-19 infection rates were lower on average in rural than in urban counties in the early stages of the epidemic. In large urban areas, the susceptibility driven by high population density and enhanced connectivity forced the implementation of strict non-pharmaceutical interventions such as lockdowns and social distancing practices, which reduced the community spread of infection in these areas. As a result, the pandemic may be showing signs of receding in large metropolitan areas, but continued to diffuse from cities to rural communities, which are communities that might have implemented less intensive interventions. For example, effective non-pharmaceutical measures such as face covering have been met with some resistance among rural communities in the U.S.[17]. With the slow rollout of vaccination in the country, masks remain one of the few control measures available for protection against the virus as they serve as a physical barrier for virus dispersion[18]. Although mask wearing has been found to be an effective and proactive public health tool against virus dispersion, some studies have identified lower frequency of mask use in public areas in rural compared to urban counties[17]. These studies found that the percentage of individuals wearing masks was about four times greater in urban than in rural areas, possibly reflecting a perception of lower risk of COVID-19 infection in rural communities.
Although COVID-19 mortality has declined nationally, this decline was only observed in urban areas, whereas the mortality rate has increased more than 100% from the first to the third period in the rural counties. COVID-19 mortality is steadily declining in urban areas, with the largest decline of 45% from the first to the second period, and with a smaller decline of 30% from the second to the third period. Conversely, mortality rate in rural areas is steadily increasing, with an increase of about 40% from the first to the second period, and with the largest increased occurring between the second to the third period, with about 55% increase in the COVID-19 mortality rate. Reasons for these disparities in the mortality rates between urban and rural areas can be linked to a shift in the demographic groups most affected by the epidemic. Younger populations in urban counties are currently experiencing the largest burden of infection. This demographic group has better infection outcomes, with lower infection complications, hospitalizations, and consequently COVID-19 related deaths[19]. Conversely, many of the risk factors for COVID-19 infection complications are exacerbated in rural areas, particularly in older adults. Rural areas have older populations[20], on average, with more underlying medical conditions than suburban and urban communities[21]. It is estimated that about 50% of rural residents are at high risk for hospitalization and COVID-19 related complications, compared to 40% in metropolitan areas. In addition, rural populations are older and have lower general health conditions than urban populations, and therefore they are vulnerable populations at higher risk of COVID-19 related hospitalization and deaths, with an estimated 10% higher hospitalization rate for COVID-19 per capita than urban residents given equal infection rates[22]. Additionally, major vulnerabilities in rural areas include fewer physicians and lack of access to intensive care and ventilators, which are key aspects of care needed for the at least 5% of critical COVID-19 infection related complications[23]. Health care facilities within rural communities are typically less well-resourced with reduced access to personal protective equipment, lower access to ICU beds, testing, and the necessary equipment to effectively treat people most severely affected by COVID-19 infection complications, which are commonly older adults[24]. As a result, many rural hospitals find themselves needing to transfer residents with more serious cases of COVID-19 to larger facilities in urban areas for treatment[25]. Hospital transfers require time and that can affect disease outcomes in critical situations, and relocating patients during the current wave of COVID- 19 to urban areas may present additional challenges if the receiving hospital is already overwhelmed[22].
As the U.S. begins its massive vaccine rollout, health departments across the country are scrambling to plan and adjust their vaccination plans, often while simultaneously managing a surge in new COVID-19 cases, particularly in rural areas. The geography can also compound disparities in access that affect rural clinics, which face unique challenges to provide vaccinations to residents who live many miles away. Rural communities often run short on resources including cold vaccine storage facilities or healthcare workers to administer vaccines.
Additionally, it has been shown that rural residents are less likely to receive flu shots than residents of urban areas[26]. This tendency combined with the hesitancy of rural communities to adopt other COVID-19 mitigation measures, can facilitate the surge of pockets of the virus in some rural areas of the country, from which it could reemerge into the broader population, compromising efforts to get the virus under control. Therefore, public information campaigns and vaccine promotions along with the setup of new sites for vaccinations in rural underserved areas become important strategies to target vulnerable populations in rural communities.
The COVID-19 pandemic has continued to spread, causing many deaths around the world. Analysis of setting-specific data is paramount in understanding local transmission dynamics of the disease and designing effective public health responses[2,27]. Our findings suggest that the pandemic in the U.S. is composed of sub-epidemics with different temporal dynamics and spatial patterns that could potentially present challenges in disease control within the country. The disease has manifested itself in different spatial and temporal ways in urban and rural areas. The current epicenter of the epidemic is located in states with higher infection intensity and mortality in rural areas, and higher incidence states are currently experiencing a significant increase in the rate of COVID-19 related deaths in both urban and rural areas.
Conclusions
A high burden of infection combined with lower healthcare capacity in rural areas implies that residents in these vulnerable areas are at higher risk of COVID-19 infection and related morbidity and mortality during the current stage of the epidemic in the U.S.[4,28]. Clinicians and public health policy makers must tailor intervention strategies to suit local needs. Public health policies should take into account county-level interventions and strategies specific to each type of community (urban or rural). When making public health policies, the local government should be aware of, and consider, the differences in COVID-19 spread between urban and rural areas, which will allow more effective disease control. With increasing incidence rates in rural areas, residents must be made aware of their increased risk of infection so they can take personal measures to protect themselves, and Critical Access Hospitals must continue to receive Federal funding, as they are crucial to treating patients in rural areas. Health partnerships must also be made to coordinate data and updates about COVID-19, and to share valuable resources, such as personal protective equipment. Efforts focused on decreasing disease spread and strengthening the healthcare capacity in the vulnerable rural areas would benefit rural communities and limit the spread of COVID-19 disease in the current geographical epicenter of the epidemic in the U.S.
Author statement
Dr. Cuadros had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Conceptualization: D.F.C, A.J.B., Z.M., F.DW.M, N.M.; methodology: D.F.C., A.J.B.; software: D.C.; validation: D.F.C., A.J.B.; writing—original draft preparation: D.F.C.,N.M., writing—review and editing: A.J.B., Z.M., F.DW.M,
Data availability
The data that support the findings of this study are openly available from the Johns Hopkins University Center for Systems Science and Engineering through a GitHub repository (https://github.com/CSSEGISandData/COVID-19).
Conflict of interest
The authors have no conflicts of interest to declare.
Ethics approval statement
The data that support the findings of this study are openly available from the Johns Hopkins University Center for Systems Science and Engineering through a GitHub repository (https://github.com/CSSEGISandData/COVID-19). Therefore, our study did not require an ethics approval because there were no human participants involved in this research, and it relies entirely on previously published data.
Acknowledgments
The authors thank the Johns Hopkins University Center for Systems Science and Engineering, and the Our World in Data project for releasing data on cases and testing for COVID-19.
Footnotes
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Appendix A. Supplementary materials
REFERENCES
- 1.Wu KJ.U.S. The New York Times; Manhattan, New York City: 2020. Coronavirus cases are rising sharply, but deaths are still down. https://www.nytimes.com/2020/07/03/health/coronavirus-mortality-testing.html, Accessed on November 15, 2020. [Google Scholar]
- 2.Cuadros D.F., Xiao Y., Mukandavire Z., Correa-Agudelo E., Hernández A., Kim H., et al. Spatiotemporal transmission dynamics of the COVID-19 pandemic and its impact on critical healthcare capacity. Health Place. 2020 doi: 10.1016/j.healthplace.2020.102404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bialek S., Bowen V., Chow N., Curns A., Gierke R., Hall A., et al. Centers for Disease Control and Prevention; Atlanta, Georgia: 2020. Geographic differences in COVID-19 cases, deaths, and incidence—United states. February 12–April 7, 2020. [Google Scholar]
- 4.Miller I.F., Becker A.D., Grenfell B.T., Metcalf C.J.E. Disease and healthcare burden of COVID-19 in the United States. Nat. Med. 2020:1–6. doi: 10.1038/s41591-020-0952-y. [DOI] [PubMed] [Google Scholar]
- 5.Paul R., Arif A.A., Adeyemi O., Ghosh S., Han D. Progression of COVID-19 from urban to rural areas in the United States: a spatiotemporal analysis of prevalence rates. The J Rural Health. 2020:591–601. doi: 10.1111/jrh.12486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Thebault R., Hauslohner A. The Washington Post; Washington, D.C.: 2020. A deadly ‘checkerboard’: covid-19’s new surge across rural america. https://www.washingtonpost.com/nation/2020/05/24/coronavirus-rural-america-outbreaks/?arc404=true, Access date: November 15, 2020. [Google Scholar]
- 7.Ullrich F., Mueller K. RUPRI Center for Rural Health Policy Analysis; 2020. Metropolitan/Nonmetropolitan COVID-19 confirmed cases and general and icu beds.” rupri center for rural health policy analysis. [Google Scholar]
- 8.Schroeder S. Rural Health Research RECAP; Grand Forks, North Dakota: 2018. Rural communities: age, income, and health status. [Google Scholar]
- 9.Kluge H. World Health Organization Regional Office for Europe, Copenhagen, Denmark; 2020. Statement–Older people are at highest risk from COVID-19, but all must act to prevent community spread. [Google Scholar]; Retrieved from World Health Organization website: http://wwweuro.who.int/en/health-topics/health-emergencies/coronavirus-covid-19/statements/statement-older-people-are-at-highest-risk-from-covid-19,-but-all-must-act-to-prevent-community-spread.
- 10.Bureau U.C. The United States Census Bureau, Suitland, Maryland; 2016. New census data show differences between urban and rural populations. [Google Scholar]
- 11.C T., J T., M L., J S., MS T., C H.-.S. The University of Minnesota Rural Health Research Center; 2020. Rural-Urban differences among older adults. [Google Scholar]
- 12.University J.H. University JH; Baltimore, Maryland: 2019. Novel coronavirus COVID-19 (2019-nCoV) data repository by johns hopkins csse. editor. [Google Scholar]
- 13.Ingram D.D., Franco S.J. 2013 NCHS urban-rural classification scheme for counties: US Department of Health and Human Services. Centers for Disease Control and …. 2014:1–65. [Google Scholar]
- 14.ESRI . 2020. 2019 USA population density. [Google Scholar]
- 15.Core Team R. R Foundation for Statistical Computing; Vienna, Austria: 2018. R: a language and environment for statistical computing. 3.5.2 ed. [Google Scholar]
- 16.von Elm E., Altman D.G., Egger M., Pocock S.J., Gotzche P.C., Vandenbroucke J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Epidemiology. 2007;18:800–804. doi: 10.1097/EDE.0b013e3181577654. [DOI] [PubMed] [Google Scholar]
- 17.Haischer M.H., Beilfuss R., Hart M.R., Opielinski L., Wrucke D., Zirgaitis G., et al. Who is wearing a mask? Gender-, age-, and location-related differences during the COVID-19 pandemic. PLoS ONE. 2020;15 doi: 10.1371/journal.pone.0240785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chu D.K., Akl E.A., Duda S., Solo K., Yaacoub S., Schünemann H.J., et al. Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: a systematic review and meta-analysis. The Lancet. 2020:1973–1987. doi: 10.1016/S0140-6736(20)31142-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zhang C.H., Schwartz G.G. Spatial disparities in coronavirus incidence and mortality in the United States: an ecological analysis as of May 2020. The J Rural Health. 2020;36:433–445. doi: 10.1111/jrh.12476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cromartie J. U.S. Department of Agriculture, Washington, D.C.; 2018. Rural america at a glance. 2018 Edition. [Google Scholar]
- 21.Statistics NCfH. Health, united states, 2018. National Center for Farmworker Health, Buda, Texas, 2019. [PubMed]
- 22.Kaufman B.G., Whitaker R., Pink G., Holmes G.M. Half of Rural Residents at High Risk of Serious Illness Due to COVID-19, Creating Stress on Rural Hospitals. The Journal of Rural Health. 2020;36:584–590. doi: 10.1111/jrh.12481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Schulte F., Lucas E., Rau J., Szabo L., Hancock J. Kaiser Health News; Washington, D.C.: 2020. Millions of older americans live in counties with no icu beds as pandemic intensifies. [Google Scholar]
- 24.Diaz A., Chhabra K., Scott J. Health Affairs Blog; Bethesda, Maryland: 2020. The COVID-19 pandemic and rural hospitals—adding insult to injury. [Google Scholar]
- 25.Henning-Smith C. The unique impact of COVID-19 on older adults in rural areas. J Aging Soc Policy. 2020:1–7. doi: 10.1080/08959420.2020.1770036. [DOI] [PubMed] [Google Scholar]
- 26.Bajak A. USA Today; McLean, Virginia: 2020. What vaccination rates in rural america tell us about the advent of COVID-19 vaccines. [Google Scholar]
- 27.Mukandavire Z., Nyabadza F., Malunguza N.J., Cuadros D.F., Shiri T., Musuka G. Quantifying early COVID-19 outbreak transmission in South Africa and exploring vaccine efficacy scenarios. PLoS ONE. 2020;15 doi: 10.1371/journal.pone.0236003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Davoodi N.M., Healy M., Goldberg E.M. Rural America's Hospitals are Not Prepared to Protect Older Adults From a Surge in COVID-19 Cases. Gerontology and Geriatric Medicine. 2020;6 doi: 10.1177/2333721420936168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.ESRI . ESRI; Redlands, CA, USA: 2004. ArcGIS 10.x. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data that support the findings of this study are openly available from the Johns Hopkins University Center for Systems Science and Engineering through a GitHub repository (https://github.com/CSSEGISandData/COVID-19).