Abstract
Aims
Unmet needs for mental health treatment are large and widespread, and periods of economic crisis may increase the need for care and the treatment gap, with serious consequences for individuals and society. The aim of this systematic review was to summarise the empirical evidence on the association between periods of economic crisis and the use of mental health care.
Methods
Following the PRISMA statement, MEDLINE, Embase, Scopus, Open Grey and Cochrane Database were searched for relevant publications, published between 1990 and 2018, from inception to June 2018. Search terms included (1) economic crisis, (2) use of mental health services and (3) mental health problems. Study selection, data extraction and the assessment of study quality were performed in duplicate.
Results
Seventeen studies from different countries met the inclusion criteria. The results from the included articles suggest that periods of economic crisis might be linked to an increase of general help sought for mental health problems, with conflicting results regarding the changes in the use of specialised psychiatric care. The evidence on the use of mental health care specifically due to suicide behaviour is mixed. The results also suggest that economic crises might be associated with a higher use of prescription drugs and an increase in hospital admissions for mental disorders.
Conclusions
Research on the impact of economic crises on the use of mental health care is scarce, and methodologies of the included papers are prone to substantial bias. More empirical and long-term studies on this topic are needed, in order to adapt mental health care systems to the specific needs of the population in times of economic crisis.
Key words: Economic crisis, mental health care, systematic review, use of service
Introduction
The financial crisis that hit the global economy in 2008 led to the deepest recession since the 1930s (European Commission, 2009), possibly longer, wider and deeper than the Great Depression (Bambra et al., 2016). The crisis had a varied impact across countries, resulting in a decline in gross domestic product (GDP), a rise in unemployment rates and severe fiscal pressure (Thomson et al., 2014). Many countries adopted austerity policies, with substantial reductions in public spending affecting health and social care budgets, and many citizens faced growing insecurity and social exclusion (Thomson et al., 2014).
Research on the social determinants of mental health has shown that health is shaped by social and economic conditions, as well as by health and welfare systems (World Health Organization and Calouste Gulbenkian Foundation, 2014). Economic crises may affect mental health either by increasing risk factors, such as unemployment, indebtedness and loss of socioeconomic status, or by weakening protective factors, such as job security and welfare protection programmes (Caldas de Almeida et al., 2017). Indeed, recent reviews assessing the health consequences of economic crises have revealed a significant relationship between these periods and psychopathology including suicide, onset or exacerbation of mood and anxiety disorders, heavy drinking, and psychological distress (Frasquilho et al., 2016; Martin-Carrasco et al., 2016). These results would make expectable an increased search for mental health treatment. However, barriers to access to mental health care may be exacerbated during economic crises, due to changes in the availability (e.g., cuts in human resources) and affordability (e.g., out-of-pocket payments) of services (Wahlbeck and McDaid, 2012; Maresso et al., 2015; Antunes et al., 2017). Literature on how the use of mental health care varies in times of economic crisis is scarce, and recent reviews found mixed evidence (Zivin et al., 2011; Cheung and Marriott, 2015; Martin-Carrasco et al., 2016). Zivin et al. (2011) concluded that economic downturns might be associated with increased first admissions to mental health services. Cheung and Marriott (2015) found a decline in the use of mental health services in the USA, likely due to a lack of access to insurance, and an increase in the use of prescription medication. Martin-Carrasco et al. (2016) concluded that the treatment gap increases in times of economic crisis, probably due to the lack of accessibility to services, the austerity measures, and the increased stigma towards people with mental illness. However, these reviews had some limitations: (a) only one of them followed the PRISMA guidelines (Martin-Carrasco et al., 2016); (b) one of the systematic reviews did not focus specifically on the use of mental health care (Martin-Carrasco et al., 2016); and (c) one did not include data from the 2008 Great Recession (Zivin et al., 2011).
The aim of this study was to systematically review the available literature on the impact of economic crises on the use of mental health care, information that might contribute to the design of strategies, policies and programmes to promote equitable access to care in times of economic crisis.
Methods
Search strategy and selection of articles
The PRISMA guidelines for reporting systematic reviews were followed (Moher et al., 2009). The protocol was registered in the International Prospective Register of Systematic Reviews on 28 June 2017 (PROSPERO, registration No.: CRD42017069284). Comprehensive literature searches of MedLine (through Ovid and Pubmed), Scopus, Cochrane Database and Open Grey Repository databases were conducted, from inception to 20 June 2017 and last updated on 25 June 2018. Databases were searched separately by two reviewers (DMR and MS).
Three sets of keywords were combined in the search strategy: (1) economic crisis; (2) use of mental health; (3) mental health problems. Searches were piloted in Ovid and then adapted to run across the other databases (see Supplementary Table S1). The reference lists of the primary studies selected as well as recent reviews in the field were checked. In addition, we contacted expert authors to identify any additional articles.
Study selection was done in duplicate (DMR and MS), and a third reviewer participated where disagreements arose (GC) over the three phases. First, duplicate studies were deleted. Second, a selection of potentially relevant articles was made based on the title and abstract. Third, after reading the full text, a final selection was made. The inter-agreement between reviewers measured with the κ statistic was excellent (κ = 0.81; 95% CI 0.65–0.97).
The studies selected had to meet specific inclusion criteria (see Table 1). We focused on countries that faced crises since the 1990s as this would allow the inclusion of the available research on the impact of the main economic crises on health, namely the Post-Communist Depression in the early 1990s, the East Asian financial crisis in the late 1990s, and the Great Recession in 2008. We selected only studies with a predominantly adult population, excluding those focusing on children and adolescents, as differences in psychopathology, clinical and social characteristics between children/adolescents and adults would make it difficult to draw conclusions. We excluded studies focusing on residential care, due to the fact that during economic crises the population living in residential care, although vulnerable, were likely to be less exposed to factors affecting an individual's search for mental health treatment (social determinants of mental health and barriers to treatment) compared with those residing in permanent private dwellings, and it would be difficult to make comparisons between the two populations. Only observational studies, including ecological, cross-sectional, case–control and longitudinal studies, were selected. We included all health settings which were accessed with mental health problems as the main complaint.
Table 1.
Inclusion and exclusion criteria for the studies included in the systematic review
| Aspects considered | Inclusion criteria | Exclusion criteria |
|---|---|---|
| Population | Adult population with any mental health problem/disorder; countries that faced crises since the 90s | Population not accessing health care for mental health problems; population with a specific medical condition |
| Outcome | Access/use of mental health care (visits, admissions, lengths of stay, emergencies); use of psychotropic medication; referral to specialised psychiatric care | Impact on services (budget, organisational, financial); focused on cost; impact only on mental health prevalence |
| Design | Observational studies, including ecological, cross-sectional, case–control and longitudinal studies | Randomised controlled trials, systematic reviews, meta-analysis, editors’ letters, clinical cases, protocols, qualitative studies |
| Language | All | None |
| Setting | Primary care; psychiatric/mental health outpatient services; psychiatric/mental health inpatient services | Non-psychiatric care; residential care |
Summary measures
The summary of measures included in the selected studies were relative risk (RR), adjusted relative risk (ARR), adjusted incidence rates (AIR) and incidence risk ratio (IRR).
Data synthesis
We developed a data extraction sheet, pilot tested it on three randomly selected studies that had been included and refined herein. The main characteristics of these studies were rigorously extracted by MS and verified by a second reviewer (DMR). Any discrepancies were resolved by discussion between the two reviewers. In the event of disagreement, a third reviewer (GC) was consulted.
For each study, information was collected about the author(s), year of publication, study country, setting, sample size, time period of crisis, study design, purpose of the study, outcome variable (indicator), procedure for data collection and main results (see Table 2).
Table 2.
Details of studies included in this systematic review
| Author, year, country | Setting/population | Time period considered | Study design | Purpose of the study | Indicator/outcome considered | Procedure for data collection | Main results |
|---|---|---|---|---|---|---|---|
| Ásgeirsdóttir et al., 2017
Iceland |
National population sample, general hospital, n = 2548 (41% men, 59% women) | 2003–12 | Repeated cross-sectional study | To examine potential changes in suicide attempts and self-harm in Iceland during a period of major economic transition | Incidence of attendance rates due to suicidal behaviour | Hospital records | Risk of attendance post-collapse compared with pre-collapse (95% CI):
|
| Bidargaddi et al., 2015
Australia |
Regional population sample, emergency services, n = from 978 to 1421 per month (mean 1226.5; s.e. 10.11) | 2004–11 | Time series | To analyse the effects of changes in rates of unemployment on numbers of Emergency Department Mental Health presentations | Use of emergency department due to mental health problems | Hospital records | Cross-correlation between unemployment and mental health presentations to emergency departments:
|
| Bonnie Lee et al., 2017
Taiwan, Republic of China |
National population sample, hospitals, n = 11 643 417 (53% men and 47% women) | 2007–2012 | Time series | To evaluate the impacts of the 2008 financial crisis on different socioeconomic subgroups in Taiwan | Monthly adjusted incidence rates of hospitalisation | Hospital records | Effects of economic recession in change (in percent) on incidence rates of hospitalisation due to depressive illnesses (per 1 000 000 persons): Men Low income: AIR = 18.01 (95% CI 14.53–21.48) Middle income: AIR = −3.56 (−1.93 to –5.18) High income: AIR = 2.76 (−7.56 to 13.09) Women Low income: AIR = 14.23 (8.46–19.99) Middle income: AIR = −0.28 (−4.95 to 4.39) High income: AIR = 5.02 (4.05–6.00) |
| Buffel et al., 2015
European countries |
National population samples, general and mental health outpatient visits, n = 52 216 (45% men, 55% women) | 2002, 2005–2006, and 2010 | Repeated cross-sectional study | To examine whether the macro-economic context and changes therein are related to mental health care use, via their impact on mental health, or more directly, irrespective of mental health | Use of mental health care | Structured interviews | General practitioner consultations1:
1Adjusted for the interaction effects with the non-employed |
| Burgard and Hawkins, 2014
USA |
National population sample, all settings, n = 73 403 | 2006–2010 | Repeated cross-sectional study | To examine the consequences of the Great Recession for disparities in foregone care in the USA | Foregone use of mental health care | Structured interviews | Predicted percent reporting foregone mental health care by recessionary period:
|
| Chen and Dagher, 2016 USA |
National population sample, primary care and hospital outpatient visits, n = 23 317 (29% men, 71% women) | 2007–2009 | Longitudinal study (panel study) | To examine the changes in health care utilisation for mental health disorders among patients who were diagnosed with depressive and/or anxiety disorders during the Great Recession in the USA | Utilisation of prescription drugs. Use of mental health care | Medical records | Negative binomial results of differences in prescription drug use and physician visits before and during the recession: Women Prescription drug use
Prescription drug use
|
| Córdoba-Doña et al., 2014 Spain |
Regional population sample, emergency services, n = 24 380 (47% men, 53% women) | 2003–2012 | Ecological study | To examine the impact of the economic crisis on suicide attempts, and its relation to unemployment, age and sex | Use of emergency departments due to suicide behaviour | Hospital records | Linear regression fixed-effects models for suicide attempt rates (×105) regressed on unemployment rates1: Men β = 1.08, p = 0.04 (95% CI 0.06–2.09) Women β = 0.49, p = 0.52 (−1.23 to 2.21) 1Adjusted for yearly trends |
| Dunlap et al., 2016
USA |
National population sample, outpatient or inpatient mental health treatment, n = 21 100 (49% men, 51% women) | 2008–2010 | Repeated cross-sectional study | To examine the relationship between state and local economic conditions and serious psychological distress, substance use disorders, and mental health service utilisation | Mental health service utilisation | Structured interviews | Predictors of mental health service utilisation: Serious mortgage delinquency rate (quartile) (reference: quartile 1)
|
| Gotsens et al., 2015
Spain |
National population sample, all settings, n = 23 760 in 2006 and n = 16 616 in 2012 | 2006 and 2012 | Repeated cross-sectional study | To analyse health inequalities between immigrants born in middle- or low-income countries and natives in Spain, in 2006 and 2012 | Utilisation of prescription drugs | Structured interviews | Use of psychotropic drugs: PR 2006 = 0.22 (95% CI 0.11–0.43) PR 2012 = 1.20 (0.73–2.01) |
| Hawton et al., 2016
UK |
Regional population sample, general hospitals, n = 35 951 (40% men, 60% women) | 2008–2010 | Ecological study | To investigate the impact of the recent recession on rates of self-harm in England and problems faced by patients who self-harm | Use of emergency departments due to suicide behaviour | Hospital records | Estimates of changes in rates of self-harm in 2008–2010 relative to expected rates based on trends in 2001–2007: Self-harm Oxford
|
| Iglesias García, 2014
Spain |
Regional population sample, general hospitals and mental health outpatient visits, n = 1 078 406 (48% men, 52% women) | 2000–2010 | Ecological study | To study the association between socioeconomic status and number of people demanding mental health services | Annual incidence and prevalence demand for mental illness | Hospital records | Administrative incidence of mental disease per 1000 inhabitants: Z = −1.863; p = 0.03 |
| Korkeila et al., 1998
Finland |
National population, psychiatric hospitals, n = 24 546 and n = 24 909 (53% men, 47% women) | 1900–1993 | Retrospective cohort study | To study the changes in psychiatric inpatient population after (1) the rapid reduction in the number of beds in psychiatric hospitals, (2) the amendment of the mental health legislation and (3) the economic recession | Discharges from psychiatric hospitals | Hospital records | Readmissions to psychiatric hospitals (Poisson regression analysis) First-timers: N° readmissions: 9616 (1991), 9361 (1994); p = 0.003 3 or more readmissions: 267 (1991), 402 (1994); p < 0.001 All patients: N° readmissions: 15 964 (1991), 15 715 (1994); p = 0.005 3 or more readmissions: 1407 (1991), 1796 (1994); p < 0.001 Total: 24 546 (1991), 24 909 (1994); NS |
| Modrek et al., 2015
USA |
National population sample, outpatient physician visits (including emergency room visits) and inpatient hospitalisations, n = 11 625 (80% men, 20% women) and n = 10 242 (81% men, 19% women) | 2007–2012 | Cohort study | To examine the mental health effects of the Great Recession of 2008–2009 on workers who remained continuously employed and insured | Use of mental health care. Utilisation of prescription drugs | Medical records | Mental health inpatient utilisation: β = 0.002; p = 0.078 Mental health outpatient utilisation: β = 0.019; p < 0.001 Mental health medication supply (in 2007/2010):
|
| Ostamo and Lönnqvist, 2001, Finland | Regional population sample, general hospitals, n = 3100 | 1989–1997 | Time series | To investigate the rates and trends of attempted suicide treated in health care during a period of severe economic recession | Use of health care due to suicide behaviour | Structured interviews and medical records | Trends of attempted suicide:
|
| Petrou, 2017, Cyprus | Regional population sample, primary care and hospital outpatient visits | 2011–2014 | Time series | To elucidate the impact of crisis and introduction of copayment in the utilisation of mental health services in Cyprus primary public health care sector | Use of mental health care | Medical records | Visits to mental health services: Non-significant increase during the early phases of the financial crisis; p = 0.978. Introduction of copayment: No impact on mental health services utilisation rate, up to 9 months following its inception; p = 0.097 |
| Sicras-Mainar and Navarro-Artieda, 2015
Spain |
Regional population sample, primary care and hospital outpatient visits, n = 3662 and n = 5722 | 2008–2009 and 2012–2013 | Retrospective, observational study | To describe antidepressant use in the treatment of major depressive disorder during a period of economic crisis | Utilisation of prescription drugs. Use of mental health care | Medical records | Total pharmaceutical spending and consumption of antidepressants during the two study periods: Precrisis period (2008–2009)/period of economic crisis (2012–2013)
Precrisis period/period of economic crisis Number of patients
|
| Wong et al., 2014, USA | National population sample, primary care and outpatient visits, n = 11 041 855 | 2004–2012 | Longitudinal study | To examine whether local unemployment was associated with utilisation of Veterans Affairs Health Care System primary care, specialty care and mental health services during 2004–2012 | Use of mental health care | Medical records | Mental health visits at baseline and study end:
Fiscal year 2012–quarter 4: mean 3073.44, s.d. 4886.73; p < 0.001
Fiscal year 2012–quarter 4: mean 743.89, s.d. 1040.69; p < 0.001 Association between local area unemployment rates and outpatient utilisation, by copayment status and age group:
|
AIR, adjusted incidence rates; CC, cross-correlation coefficient; PR, prevalence ratio; s.e., standard error.
Risk of bias in individual studies
Quality assessment was performed independently in duplicate (DMR and MS), and a third reviewer participated in cases of disagreement (GC). The quality of the studies was assessed using the Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies (NHLBI, 2017), which assesses 14 items, rating quality as poor, fair or good.
Results
Search results
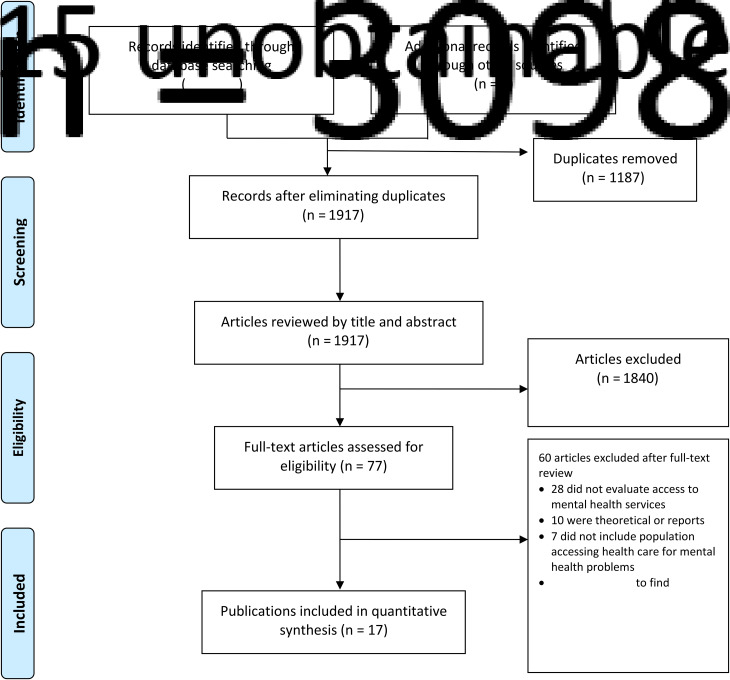
The search strategy produced 3098 potentially relevant studies (see Fig. 1 PRISMA flow diagram). Further six articles were identified from the references of the articles selected. Of these, 1187 were duplicates. Of those remaining, 1840 were excluded after reviewing the title and abstract. After reviewing the full text of the remaining articles, 60 were excluded for the following main reasons: 28 did not evaluate access or use of mental health services, ten were reports or theoretical articles, and seven did not include population accessing health care for mental health problems. Finally, 17 articles were selected.
Fig. 1.
Flow chart of articles included and excluded after the systematic review.
The data of the included studies were extracted and summarised (see Table 2). Five were repeated cross-sectional studies, as well as four time series studies, three ecological studies, three cohorts, one panel study and one longitudinal study. Eleven studies employed national population samples and six employed regional samples. The studies were based on samples from European countries (58.82%), USA (29.41%), Australia (5.88%) and Republic of China (5.88%).
Study quality
The results of the quality assessment of the included studies are presented in Supplementary Table S2. All studies have an objective clearly stated and a study population prespecified. Only two studies provided a sample size justification (Buffel et al., 2015; Chen and Dagher, 2016). Nine studies measured the exposure of interest prior to the outcome (Córdoba-Doña et al., 2014; Wong et al., 2014; Bidargaddi et al., 2015; Gotsens et al., 2015; Modrek et al., 2015; Chen and Dagher, 2016; Dunlap et al., 2016; Hawton et al., 2016; Petrou, 2017). Seven studies did not provide adjustment for confounding variables (Ostamo and Lönnqvist, 2001; Iglesias García et al., 2014; Bidargaddi et al., 2015; Sicras-Mainar and Navarro-Artieda, 2015; Ásgeirsdóttir et al., 2017; Hawton et al., 2016; Petrou, 2017).
Impact of the economic crisis on the use of health facilities
Use of general and specialised care for mental health problems
Periods of economic crisis appeared linked to an increase of general help seeking for mental health problems (Bidargaddi et al., 2015; Buffel et al., 2015; Sicras-Mainar and Navarro-Artieda, 2015), with mixed patterns for the use of specialised psychiatric care (Iglesias García et al., 2014; Wong et al., 2014; Buffel et al., 2015; Modrek et al., 2015; Chen and Dagher, 2016; Petrou, 2017). Two studies conducted in European Union countries found that a significantly increased contact with a general practitioner for mental health problems occurred during the period of economic crisis (Buffel et al., 2015; Sicras-Mainar and Navarro-Artieda, 2015), but a significantly decreased contact with a psychiatrist (Buffel et al., 2015) or no change in the use of specialist care occurred despite the higher proportion of referrals (Sicras-Mainar and Navarro-Artieda, 2015). Bidargaddi et al. (2015) found a higher number of visits to the medical emergency room for reasons of mental health during economic slow-down. Two studies in the USA found a significant increase in the utilisation of mental health services during the Great Recession (Wong et al., 2014; Modrek et al., 2015), whereas two others found a significant decrease in the use of mental health services in this period (Iglesias García et al., 2014; Chen and Dagher, 2016), and one found no impact of the crisis on the utilisation rate (Petrou, 2017).
Hospitalisations for mental health problems
Several studies found an increase of hospital admissions for mental disorders during periods of economic crisis (Korkeila et al., 1998; Modrek et al., 2015; Bonnie Lee et al., 2017). In Finland (Korkeila et al., 1998), the increase of admissions was particularly significant in multiple readmissions among new inpatients (from 0.05 to 0.08, p < 0.001), and in the diagnostic group of mood disorders among first-timers (by 60%) and among patients with previous admissions (by 39%). In the USA (Modrek et al., 2015), a marginally significant increase in the postrecession trend in inpatient utilisation compared with prerecession trend (b = 0.002; p = 0.078) was found. In Taiwan, Bonnie Lee et al. (2017) found increased rates of hospitalisation for depressive illnesses. Specifically, the AIR of hospital admissions among the low-income group were ten times higher than those of the high-income group.
Use of health facilities due to suicide behaviour
The studies included found mixed results regarding the use of mental health care due to suicide behaviour (Ostamo and Lönnqvist, 2001; Córdoba-Doña et al., 2014; Hawton et al., 2016; Ásgeirsdóttir et al., 2017). Studies conducted in Nordic countries (Finland and Iceland) showed no overall increase in attendance rates due to suicide attempts and self-harm following economic crises (Ostamo and Lönnqvist, 2001; Ásgeirsdóttir et al., 2017). On the contrary, an increase in the use of health facilities for suicide attempt and self-harm after the onset of the 2008 crisis was found in other European countries (Spain and England) (Córdoba-Doña et al., 2014; Hawton et al., 2016), with authors proposing that the increase may be related to changes in unemployment.
Impact of the economic crisis on the use of prescription drugs
Different studies found an increase in the use of psychotropic drugs during the period of an economic crisis, including psychotropic medications to treat depressive and anxiety disorders (Gotsens et al., 2015; Modrek et al., 2015; Sicras-Mainar and Navarro-Artieda, 2015; Chen and Dagher, 2016). Gotsens et al. (2015) compared the use of psychotropic drugs between natives and immigrants who arrived in Spain before 2006 and found that the increase in the use of psychotropic drugs was higher among immigrant men.
Impact of macroeconomic indicators on the use of mental health care
Several articles included in this review found that unemployment rates were associated with changes in help-seeking behaviour for mental health problems (Córdoba-Doña et al., 2014; Iglesias García et al., 2014; Wong et al., 2014; Bidargaddi et al., 2015; Buffel et al., 2015; Modrek et al., 2015; Dunlap et al., 2016; Ásgeirsdóttir et al., 2017). The likelihood of men contacting a general practitioner for mental health problems was found to be higher in countries experiencing an increase in the unemployment rate (OR = 1.031, 95% CI) (Buffel et al., 2015). Studies in the USA found significant associations between higher local unemployment and increased outpatient visits, use of opiates and sleep aids (Modrek et al., 2015), as well as increased outpatient utilisation among veterans exempt from copayments (Wong et al., 2014). However, a third study in the USA (Dunlap et al., 2016) found that individuals who resided in counties with higher unemployment rates were less likely to use mental health services compared with individuals who resided in counties with the lowest unemployment rates (ARR = 0.58, 0.62 and 0.71). Similarly, in Spain, the increase in the unemployment rate was associated with a clear decrease in mental health demand (Iglesias García et al., 2014). Unemployment rates were also associated with the use of mental health care due to suicide attempts in men, accounting for almost half of the cases during the five initial years of the crisis in Spain (Córdoba-Doña et al., 2014). However, Ásgeirsdóttir et al. (2017) found that a 1% increase in unemployment rate was significantly associated with reduced attendance rates due to suicide attempts among men in Iceland (RR = 0.84; 0.76–0.93), but not among women.
Buffel et al. (2015) found that, in countries with a decline in the GDP growth rate, employed men were less likely to contact a psychiatrist (OR = 0.966, 95% CI) compared with those in countries with an increase in the GDP growth rate, while Iglesias García et al. (2014) found that GDP increase was strongly associated with an increased demand for mental health care.
Finally, Dunlap et al. (2016) found that individuals who resided in states with higher rates of serious mortgage delinquency were less likely to use mental health services (ARR = 0.54, 0.52 and 0.73, respectively).
Impact of individual indicators on the use of mental health care
Several studies included showed a higher utilisation of mental health care by women (such as access to outpatient visits, emergency department, prescription drugs and hospitalisation) compared with men during the crisis (Buffel et al., 2015; Chen and Dagher, 2016; Bonnie Lee et al., 2017). Regarding the risk of attendance of health facilities due to suicidal behaviour, Ostamo and Lönnqvist (2001) showed that there was a convergence of rates between genders, with the men's rates decreasing 15% (trend test χ2 = 10.45, p ⩽ 0.001) and the women's rates increasing 8% (trend test χ2 = 2.55, p = 0.11). Other studies showed that socioeconomic factors were more strongly associated with suicidal behaviour care in men than in women (Córdoba-Doña et al., 2014; Ásgeirsdóttir et al., 2017).
Two studies found that adults aged 35–54 years were the risk group for the use of care due to suicidal behaviour (Córdoba-Doña et al., 2014; Hawton et al., 2016).
Bonnie Lee et al. (2017) suggested low income to be a risk factor for hospitalisation for depressive disorders.
Gotsens et al. (2015) found that, in Spain, the 2008 economic crisis may have had a worse impact on the health status of immigrants, as shown by the loss of the ‘healthy immigrant effect’ and the equalisation of the previously lower use of psychotropic drugs among immigrants compared with natives. Chen and Dagher (2016) found that ethnic minorities presented lower rates of health care use during the 2008 Great Recession. Specifically, compared with white women, African American women had significantly fewer physician visits (IRR = 0.71, p = 0.01), and Latinas and African American women used significantly fewer prescription drugs (IRR = 0.75, p < 0.001; IRR = 0.71, p < 0.001). Compared with white men, Latino men had significantly lower rates of physician visits (IRR = 0.72, p < 0.05), and lower rates of prescription drug utilisation (IRR = 0.72, p < 0.001). Burgard and Hawkins (2014) found that levels of foregone mental health care rose in the Great Recession of 2007–2009, but that disparities between ethnic groups in foregone mental care were stable during the recession.
Discussion
To our knowledge, this is the first systematic review to specifically study the impact of the economic crisis on the utilisation of mental health care following PRISMA guidelines. This study is relevant for systematising the scarce literature available, and for highlighting the risk of a growing treatment gap, particularly among the most vulnerable groups.
Our results suggest an increase of general help-seeking behaviour for mental health problems, with more contradictory results in relation to the use of specialised psychiatric care. There may be several explanations for these findings. First, in times of economic crisis, more accessible and affordable general health care might be the preferred pathway to care, with the subsequent increase in unmet need for specialised care (Buffel et al., 2015). In these periods, reduced mental health budgets may decrease availability of mental health services and/or they may be unaffordable because of the reduction of households’ disposable income, lack of health insurance coverage or the introduction of copayment in the public health care sector (Dunlap et al., 2016). Second, decreased motivation to demand specialised care may be due to possible negative consequences, such as fear of losing a job due to work disability or treatment stigma (Iglesias García et al., 2014). Lastly, the adverse social circumstances that occur in periods of economic crisis might cause health expectations to decrease and induce more personal efforts to be taken on to achieve these expectations (Iglesias García et al., 2014).
The review conducted by Martin-Carrasco et al. (2016) had already described an increase in the treatment gap during times of economic crisis, pointing out the lack of accessibility to services, the austerity measures and the increased stigma as probable explanations.
Our review found different trends in relation to the use of mental health care due to suicide behaviour between the Nordic countries and other European countries. Possible factors explaining these findings might be Nordic countries’ relatively high levels of social capital and strong welfare systems, possibly mitigating the adverse consequences of unemployment on suicidal outcomes (Ostamo and Lönnqvist, 2001; Ásgeirsdóttir et al., 2017).
Our results also suggest that economic crises might be associated with a higher use of prescription drugs and an increase in hospital admissions for mental disorders, as had been found in previous reviews (Zivin et al., 2011; Cheung and Marriott, 2015).
The results provide information on the patterns of demand for care of different groups defined by an axis of inequality during economic crises. The groups of people most susceptible to the effects of crises were not consistently those that most accessed mental health care (Burgard and Hawkins, 2014; Córdoba-Doña et al., 2014; Iglesias García et al., 2014; Wong et al., 2014; Bidargaddi et al., 2015; Buffel et al., 2015; Gotsens et al., 2015; Modrek et al., 2015; Dunlap et al., 2016; Chen and Dagher, 2016; Ásgeirsdóttir et al., 2017; Bonnie Lee et al., 2017). Mental health care utilisation patterns depend on the recognition that help is needed (Andrade et al., 2008; Mojtabai et al., 2002), on structural factors including financial costs (Mojtabai, 2009), and availability of services (Wells et al., 2002; Saxena et al., 2003), and on attitudinal factors (Sareen et al., 2007; Mojtabai, 2010). These factors might change during economic crises and affect differently the various socioeconomic groups, possibly exacerbating systemic problems in access to care and widening social inequalities in mental health. The reasons for the increased treatment gap among vulnerable groups might include a disproportionate worsening of socioeconomic conditions, the impact of austerity measures, and subsequent reduced available income, lack of social protection and a reduction in available health care, but also worse perceived need for care, reluctance to seek services and/or cultural or linguistic barriers.
In the studies included, during periods of crisis, women used mental health care more frequently than men (Bidargaddi et al., 2015; Buffel et al., 2015; Chen and Dagher, 2016; Bonnie Lee et al., 2017). This might reflect women's relatively worse mental health status and higher need for care or gender differences in healthcare-seeking behaviour. Reasons for gender differences in healthcare-seeking behaviour could be greater stigma among men, a greater ability of women to identify their mental health problems or differences in health insurance coverage. Some of the studies reviewed suggest that socioeconomic factors may be more strongly associated with suicidal behaviour in men than in women (Córdoba-Doña et al., 2014; Hawton et al., 2016; Ásgeirsdóttir et al., 2017). One possible explanation to this finding is that men are subjected to more pressure from their working role and relative expectations of socioeconomic success, thereby sensitised to unmet expectations. Related to this, mild-adulthood seemed to be the most consistent risk group for the use of care due to suicidal behaviour (Córdoba-Doña et al., 2014; Hawton et al., 2016). This finding could be attributed to the fact that it is a period of pressure to the main earners, and during which financial crisis-related events most frequently occur.
Policy implications
The results of this systematic review highlight the need for health services to be particularly attentive and responsive to changes in patients’ socioeconomic status, especially to the needs of the most vulnerable groups.
Models of care that are closer to the population, that facilitate the early identification of mental health problems and the implementation of integrated interventions, and that have a focus on prevention of mental health problems and disorders are particularly useful.
It is crucial to maintain universal, accessible and affordable health care of good quality to avoid increasing the treatment gap.
Additionally, reforms of social welfare to maintain or strengthen safety nets and interventions across several sectors beyond the mental health sector are fundamental to minimise increasing social inequalities in mental health during economic crises.
Strengths and limitations
This review provides updated evidence about the impact of economic crises on the use of mental health care, and it is the first systematic review following the PRISMA statement in this field.
The results give us some information on the patterns of demand for care of different socioeconomic groups during these periods, and we propose some insights for these findings.
However, results should be taken with caution due to several aspects.
First, studies from some of the most severely affected countries by economic crises were not available, and this low representation of geographical and health systems limits the interpretation of our results. The scarce variety of a study's origin may reflect different levels of cross-country research or a publication bias, due to financial constraints, methodological difficulties or language barriers. It would be highly beneficial if this gap in the existing literature could be improved.
Second, the diversified designs of the included studies make it difficult to derive more homogeneous and robust conclusions, and to ascertain causality. Future studies should combine both aggregate-level and individual-level research, and longitudinal studies are needed. Measurement error may have occurred for some of the indicators. Service indicators are dependent on the nature and structure of the services, many are clinical and not based on standardised interviews and have limitations such as potential variations in the registry. Most of the studies reported that, during the period studied, there was no variation in the organisation of mental health services or registration process, in addition to those resulting from the austerity measures. Due to the special features of economic crises in each country, the specific national welfare and health systems and the countries’ policies adopted to deal with the crisis, external validity may be limited, and further research is needed to confirm the results obtained.
Third, the literature included results linked to different economic crises worldwide. Different types of economic crises will influence the length, depth and effects of the recession.
Conclusions
Research is scarce on the impact of economic crises on the use of mental health care, and methodologies used in these papers were prone to substantial bias. However, the evidence suggests that periods of economic crisis might be linked to an increase of demand for care at the general care level, an increase of hospital admissions for mental disorders and a significant higher use of prescription drugs, with more conflicting results in the use of specialised psychiatric care.
Other crises will occur in the future, and more empirical and long-term studies are needed in order to adapt mental health care systems to the needs of the populations, especially in times of economic crisis.
Financial support
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Availability of data and materials
The data regarding the process of screening and selection of the articles included in this systematic review are available in an online Supplementary material.
Conflict of interest
None.
Supplementary material
For supplementary material accompanying this paper visit http://dx.doi.org/10.1017/S2045796018000641.
click here to view supplementary material
References
- Andrade LH, Viana MC, Tófoli LF and Wang YP (2008) Influence of psychiatric morbidity and sociodemographic determinants on use of service in a catchment area in the city of São Paulo, Brazil. Social Psychiatry and Psychiatric Epidemiology 43, 45–53. [DOI] [PubMed] [Google Scholar]
- Antunes A, Frasquilho D, Cardoso G, Pereira N, Silva M, Caldas-de-Almeida JM and Ferrão J (2017) Perceived effects of the economic recession on population mental health, well-being and provision of care by primary care users and professionals: a qualitative study protocol in Portugal. BMJ Open 7, e017032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ásgeirsdóttir HG, Ásgeirsdóttir TL, Nyberg U, Thorsteinsdottir TK, Mogensen B, Matthíasson P, Lund SH, Valdimarsdóttir UA and Hauksdóttir A (2017) Suicide attempts and self-harm during a dramatic national economic transition: a population-based study in Iceland. European Journal of Public Health 27, 339–345. [DOI] [PubMed] [Google Scholar]
- Bambra C, Garthwaite K, Copeland A and Barr B (2016). All in it together? Health inequalities, austerity, and the ‘Great Recession’. In Smith KE, Hill S and Bambra C (eds), Health Inequalities, Critical Perspectives. Oxford: Oxford University Press, pp. 164–176. [Google Scholar]
- Bidargaddi N, Bastiampillai T, Schrader G, Adams R, Piantadosi C, Strobel J, Tucker G and Allison S (2015) Changes in monthly unemployment rates may predict changes in the number of psychiatric presentations to emergency services in South Australia. BMC Emergency Medicine 15, 16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonnie Lee C, Liao CM and Lin CM (2017) The impacts of the global financial crisis on hospitalizations due to depressive illnesses in Taiwan: a prospective nationwide population-based study. Journal of Affective Disorders 221, 65–71. [DOI] [PubMed] [Google Scholar]
- Buffel V, van de Straat V and Bracke P (2015) Employment status and mental health care use in times of economic contraction: a repeated cross-sectional study in Europe, using a three-level model. International Journal for Equity in Health 14, 29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burgard SA and Hawkins JM (2014) Race/ethnicity, educational attainment, and foregone health care in the United States in the 2007-2009 recession. American Journal of Public Health 104, e134–e140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caldas-de-Almeida JM, Cardoso G, Antunes A, Frasquilho D, Silva M, Neto D, Santana P, Ferrão J and Saraceno B (2017). Epidemiological Study and Qualitative Study Results – Report 1. MH Crisis Impact Study. Lisbon: Nova Medical School. [Google Scholar]
- Chen J and Dagher RK (2016) Gender and race/ethnicity differences in mental health care use before and during the Great Recession. The Journal of Behavioral Health Services & Research 43, 187–199. [DOI] [PubMed] [Google Scholar]
- Cheung S and Marriott B (2015). Impact of an economic downturn on addiction and mental health service utilization: a review of the literature. Alberta Health Services, Knowledge notes num.12. Available at (https://www.albertahealthservices.ca/assets/info/res/mhr/if-res-mhr-kn-12-economic-downturn.pdf) (Accessed 7 December 2017).
- Córdoba-Doña JA, San Sebastián M, Escolar-Pujolar A, Martínez-Faure JE and Gustafsson PE (2014) Economic crisis and suicidal behaviour: the role of unemployment, sex and age in Andalusia, southern Spain. International Journal for Equity in Health 13, 55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunlap LJ, Han B, Dowd WN, Cowell AJ, Forman-Hoffman VL, Davies MC and Colpe LJ (2016) Behavioral health outcomes among adults: associations with individual and community-level economic conditions. Psychiatric Services 67, 71–77. [DOI] [PubMed] [Google Scholar]
- European Commission (2009). Economic Crisis in Europe: Causes, Consequences and Responses. Luxembourg: European Economy. [Google Scholar]
- Frasquilho D, Matos MG, Salonna F, Guerreiro D, Storti CC, Gaspar T and Caldas-de-Almeida JM (2016) Mental health outcomes in times of economic recession: a systematic literature review. BMC Public Health 16, 115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gotsens M, Malmusi D, Villarroel N, Vives-Cases C, Garcia-Subirats I, Hernando C and Borrell C (2015) Health inequality between immigrants and natives in Spain: the loss of the healthy immigrant effect in times of economic crisis. European Journal of Public Health 25, 923–929. [DOI] [PubMed] [Google Scholar]
- Hawton K, Bergen H, Geulayov G, Waters K, Ness J, Cooper J and Kapur N (2016) Impact of the recent recession on self-harm: longitudinal ecological and patient-level investigation from the Multicentre Study of Self-harm in England. Journal of Affective Disorders 191, 132–138. [DOI] [PubMed] [Google Scholar]
- Iglesias García C, Sáiz Martinez P, García-Portilla González MP, Bousoño García M, Jiménez Treviño L, Sánchez Lasheras F and Bobes J (2014) Effects of the economic crisis on demand due to mental disorders in Asturias: data from the Asturias Cumulative Psychiatric Case Register (2000-2010). Actas Españolas de Psiquiatría 42, 108–115. [PubMed] [Google Scholar]
- Korkeila JA, Lehtinen V, Tuori T and Helenius H (1998) Patterns of psychiatric hospital service use in Finland: a national register study of hospital discharges in the early 1990s. Social Psychiatry and Psychiatric Epidemiology 33, 218–223. [DOI] [PubMed] [Google Scholar]
- Maresso A, Mladovsky P, Thomson S, Sagan A, Karanikolos M, Richardson E, Cylus J, Evetovits T, Jowett M, Figueras J and Kluge H (2015). Economic Crisis, Health Systems and Health in Europe: Country Experience. Copenhagen: WHO Regional Office for Europe/European Observatory on Health Systems and Policies. [PubMed] [Google Scholar]
- Martin-Carrasco M, Evans-Lacko S, Dom G, Christodoulou NG, Samochowiec J, González-Fraile E, Bienkowski P, Gómez-Beneyto M, Dos Santos MJ and Wasserman D (2016) EPA guidance on mental health and economic crises in Europe. European Archives of Psychiatry and Clinical Neuroscience 266, 89–124. [DOI] [PubMed] [Google Scholar]
- Modrek S, Hamad R and Cullen MR (2015) Psychological well-being during the Great Recession: changes in mental health care utilization in an occupational cohort. American Journal of Public Health 105, 304–310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moher D, Liberati A, Tetzlaff J, Altman DG, and The PRISMA Group (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Annals of Internal Medicine 151, 264–269. [DOI] [PubMed] [Google Scholar]
- Mojtabai R (2009) Unmet need for treatment of major depression in the United States. Psychiatric Services 60, 297–305. [DOI] [PubMed] [Google Scholar]
- Mojtabai R (2010) Mental illness stigma and willingness to seek mental health care in the European Union. Social Psychiatry and Psychiatric Epidemiology 45, 705–712. [DOI] [PubMed] [Google Scholar]
- Mojtabai R, Olfson M and Mechanic D (2002) Perceived need and help-seeking in adults with mood, anxiety, or substance use disorders. Archives of General Psychiatry 59, 77–84. [DOI] [PubMed] [Google Scholar]
- Ostamo A and Lönnqvist J (2001) Attempted suicide rates and trends during a period of severe economic recession in Helsinki, 1989-1997. Social Psychiatry and Psychiatric Epidemiology 36, 354–360. [DOI] [PubMed] [Google Scholar]
- Petrou P (2017) Financial crisis hangover in Cyprus: tracking the demand for utilization of mental health services. Public Health 142, 4–6. [DOI] [PubMed] [Google Scholar]
- Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies (2017) Available at (https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools) (Accessed 17 November 2017).
- Sareen J, Jagdeo A, Cox BJ, Clara I, ten Have M, Belik SL, de Graaf R and Stein MB (2007) Perceived barriers to mental health service utilization in the United States, Ontario, and the Netherlands. Psychiatric Services 58, 357–364. [DOI] [PubMed] [Google Scholar]
- Saxena S, Sharan P and Saraceno B (2003) Budget and financing of mental health services: baseline information on 89 countries from WHO's project atlas. The Journal of Mental Health Policy and Economics 6, 135–143. [PubMed] [Google Scholar]
- Sicras-Mainar A and Navarro-Artieda R (2015) Use of antidepressants in the treatment of major depressive disorder in primary care during a period of economic crisis. Neuropsychiatric Disease and Treatment 12, 29–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomson S, Figueras J, Evetovits T, Jowett M, Mladovsky P, Maresso A, Cylus J, Karanikolos M and Kluge H (2014) Economic Crisis, Health Systems and Health in Europe: Impact and Implications for Policy. Copenhagen: WHO Regional Office for Europe/European Observatory on Health Systems and Policies; (Policy Summary 12). [PubMed] [Google Scholar]
- Wahlbeck K and McDaid D (2012) Actions to alleviate the mental health impact of the economic crisis. World Psychiatry 11, 139–145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wells KB, Miranda J, Bauer MS, Bruce ML, Durham M, Escobar J, Ford D, Gonzalez J, Hoagwood K, Horwitz SM, Lawson W, Lewis L, McGuire T, Pincus H, Scheffler R, Smith WA and Unützer J (2002) Overcoming barriers to reducing the burden of affective disorders. Biological Psychiatry 52, 655–675. [DOI] [PubMed] [Google Scholar]
- Wong ES, Hebert PL, Hernandez SE, Batten A, Lo S, Lemon JM, Fihn SD and Liu CF (2014) Association between local area unemployment rates and use of Veterans Affairs outpatient health services. Medical Care 52, 137–143. [DOI] [PubMed] [Google Scholar]
- World Health Organization and Calouste Gulbenkian Foundation (2014) Social Determinants of Mental Health. Geneva: World Health Organization. [Google Scholar]
- Zivin K, Paczkowski M and Galea S (2011) Economic downturns and population mental health: research findings, gaps, challenges and priorities. Psychological Medicine 41, 1343–1348. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
For supplementary material accompanying this paper visit http://dx.doi.org/10.1017/S2045796018000641.
click here to view supplementary material
Data Availability Statement
The data regarding the process of screening and selection of the articles included in this systematic review are available in an online Supplementary material.