Abstract
Aims
A complex interaction exists between age, body mass index, medical conditions, polypharmacotherapy, smoking, alcohol use, education, nutrition, depressive symptoms, functioning and quality of life (QoL). We aimed to examine the inter-relationships among these variables, test whether depressive symptomology plays a central role in a large sample of adults, and determine the degree of association with life-style and health variables.
Methods
Regularised network analysis was applied to 3532 North-American adults aged ⩾45 years drawn from the Osteoarthritis Initiative. Network stability (autocorrelation after case-dropping), centrality of nodes (strength, M, the sum of weight of the connections for each node), and edges/regularised partial correlations connecting the nodes were assessed.
Results
Physical and mental health-related QoL (M = 1.681; M = 1.342), income (M = 1.891), age (M = 1.416), depressive symptoms (M = 1.214) and education (M = 1.173) were central nodes. Depressive symptoms’ stronger negative connections were found with mental health-related QoL (−0.702), income (−0.090), education (−0.068) and physical health-related QoL (−0.354). This latter was a ‘bridge node’ that connected depressive symptoms with Charlson comorbidity index, and number of medications. Physical activity and Mediterranean diet adherence were associated with income and physical health-related QoL. This latter was a ‘bridge node’ between the former two and depressive symptoms. The network was stable (stability coefficient = 0.75, i.e. highest possible value) for all centrality measures.
Conclusions
A stable network exists between life-style behaviors and social, environmental, medical and psychiatric variables. QoL, income, age and depressive symptoms were central in the multidimensional network. Physical health-related QoL seems to be a ‘bridge node’ connecting depressive symptoms with several life-style and health variables. Further studies should assess such interactions in the general population.
Key words: Depressive symptoms, elderly, functioning, income, network analysis, quality of life
Introduction
Psychiatric conditions manifest via signs and symptoms (American Psychiatric Association, 2000, 2013) that are closely connected to alterations of functioning (Galderisi et al., 2018), quality of life (QoL) (Hofer et al., 2017), medical comorbidities (Vancampfort et al., 2015, 2016; Stubbs et al., 2016b, 2017a; Correll et al., 2017) and life-style/behavioural habits, including nutrition, physical activity and substance abuse (Schuch et al., 2016; Stubbs et al., 2016a, 2018a, 2018b; Shivappa et al., 2018).
Several lines of evidence have implicated significant associations between functioning and QoL on the one hand and demographic, social, environmental, medical and psychiatric variables. For example, depressive symptoms have been associated with impaired functioning (Licht-Strunk et al., 2009), particularly in older populations (Ellervik et al., 2014), and with lower QoL (Lin et al., 2014). Also QoL appears to be associated with depression, ranging on a continuum from individuals without depression with higher QoL and functioning to patients with severe depression and lower QoL and functioning (Cotrena et al., 2016).
Additionally, a link has also been suggested between depression and multiple medical conditions. Several putative pathways have been proposed underlying this connection. For example, a bidirectional link has been described with obesity, with the two conditions possibly having a shared underlying biological pathway (Milaneschi et al., 2018; Vittengl, 2018). Among others, inflammatory cytokines and gut-hyperpermeability may be involved (Slyepchenko et al., 2016; Milaneschi et al., 2018). A higher prevalence of diabetes has been observed compared with the general population in patients with severe mental illness (SMI) (R1.85, 95% CI 1.45–2.37) (Vancampfort et al., 2016). The same is true for the metabolic syndrome (RR = 1.58; 95% CI 1.35–1.86) (Vancampfort et al., 2015), as well as ultimately cardiovascular disease prevalence (O1.53, 95% CI 1.27–1.83) and incidence (H1.78, 95% CI 1.60–1.98) (Correll et al., 2017). Such high comorbidity figures often complicate medication prescriptions, ultimately resulting in polypharmacotherapy, with related drug–drug interactions and safety or tolerability issues (Ban et al., 1984; Frye et al., 2000).
In addition, life-style/behavioural habits play a relevant role in the onset and maintenance of both depression and medical comorbidities. Poor nutrition, among others, has been associated with depressive symptoms. While adherence to the Mediterranean diet is associated with better QoL (Veronese et al., 2016a), food habits with a higher dietary inflammatory index (DII®) are associated with an increased risk of depression (Shivappa et al., 2018). In addition to the already complex set of putative factors associated with depression, the educational level has also been associated with depression, or suicide attempts (Rahman et al., 2018). Moreover, substance use or abuse have also been associated with depression. For example, a robust association was observed between smoking and depression both in cross-sectional and prospective studies (Luger et al., 2014; Tjora et al., 2014; Stubbs et al., 2018b). Additionally, smoking was associated with increased stress levels(Stubbs et al., 2017c). However, despite the well-replicated direct association between smoking and depression and a negative association between depression and QoL, it has been reported that patients with SMI who smoke appear to have better mental QoL (Li et al., 2017). Such a paradox represents the complexity of the relationships among psychiatric symptoms, QoL and smoking, among other variables. Moreover, beyond smoking, an association between alcohol and depressive symptoms has also been described consistently (Choi et al., 2018; Hogarth et al., 2018).
Aforementioned associations are clinically relevant in particular in the population with or at risk of osteoarthritis, given the association between osteoarthritis and pain, osteoarthritis and depression(Veronese et al., 2017c), pain and depression (Stubbs et al., 2017b), in addition to the association between osteoarthritis and several other variables (Veronese et al., 2016b; Shivappa et al., 2018). Osteoarthritis associates with high social and health costs (Chen et al., 2012), and has led the World Health Organization to proclaim the past decade as the Bone and Joint Decade (2000–2010) (Woolf and Pfleger, 2003). Among comorbid conditions, depression brings huge costs (Chiu et al., 2017; Hsieh and Qin, 2018) also. Part of the costs of treatment of chronic conditions such as osteoarthritis and depression is also on patients’ shoulders, with a crucial role of income in determining treatment, outcome (Kemp et al., 2013) and ultimately additional costs related to poor outcome of osteoarthritis and depression. Research and prevention has been proposed as targets to tackle osteoarthritis-related burden (Chen et al., 2012). Indeed, understanding the relationship among factors that share common and reciprocal associations, such as depression, sedentary behaviour, smoking and alcohol consumption and other life-style parameters could allow to better understand where most efforts in prevention of several frequently comorbid disorders, or promotion of healthy life-style campaigns may be directed.
Given the aforementioned complex associations between depressive symptoms and other multidimensional factors, alternative statistical methods, such as network analysis, may better describe the reciprocal relationships among several variables, compared with standard statistical procedures. A network meta-analysis allows the simultaneous analysis of all relationships that may be important to a network of connected phenomena. Therefore, this approach has the advantage of providing a big picture of how several variables directly or indirectly interact in the whole person's clinical and non-clinical characteristics as well as absence of any a priori hypothesis, different from structural equation modelling. Network analysis models individual variables as nodes within a network, and correlations among variables that connect each node. For example, network analysis has been used to describe the reciprocal connections among positive and negative symptoms in schizophrenia, and functioning (Galderisi et al., 2018). Also, network analysis can individuate ‘bridging’ nodes that may connect other nodes within a network.
Based on the above, we aimed employing a network analysis to describe the complex interaction between age, body mass index (BMI), medical conditions, polypharmacotherapy, smoking and alcohol use, education, nutrition, depressive symptoms, functioning and QoL. We hypothesised that among all examined variables, depressive symptoms will play a central role in the studied networks. We further hypothesised that an aggregated measure of proneness to medical comorbidity will capture the relationship between physical and mental health.
Methods
Data source and subjects
Data were extracted from the freely available Osteoarthritis Initiative (OAI) database (http://www.oai.ucsf.edu/).
Within the OAI, potential participants were recruited across four clinical sites in the USA (Baltimore, MD; Pittsburgh, PA; Pawtucket, RI; and Columbus, OH) between February 2004 and May 2006. Inclusion and exclusion criteria of OAI are reported elsewhere (Eby and Eby, 2006; Shivappa et al., 2018). In brief, patients owith or at risk of knee osteoarthritis (but without end-state bilateral knee osteoarthritis), older than 45 years, with no ethnicity restriction, without inflammatory arthritis were included.
Variable definitions
The variables included in the network were defined as follows:
Age (years) and BMI (kg/m2) (both continuous).
Charlson comorbidity index (continuous). Validated general health measures of self-reported comorbidities were assessed through a modified Charlson comorbidity score, with higher scores indicating an increased severity of conditions (Katz et al., 1996). Individual medical conditions used to build the Charlson comorbidity index were cerebrovascular disease, chronic obstructive pulmonary disease, gastro-intestinal ulcers, diabetes mellitus, asthma, heart failure, heart attack or to have undergone either percutaneous transluminal coronary angioplasty or coronary artery bypass, to have had bone fractures, knee osteoarthritis or cancer.
Number of medications (continuous). Number of medications was calculated based on the self-reported ongoing pharmacologic treatment.
Alcohol (continuous). Alcohol use was measured with the self-reported average number of drinks per week.
Education (binary). Education was categorised as having completed college, or not.
Smoking (binary). Smoking was categorised as having ever smoked, or not.
Income (binary). Income was categorised as having an income >US$50 000 per year, or not/not declared. Income was considered as a proxy of occupational functioning.
Depressive symptoms (continuous). Depressive symptoms were measured with the 20-item Center for Epidemiologic Studies-Depression (CES-D) self-rated instrument (Radloff, 1977). The range of possible values for this scores is 0–60, where higher scores indicate more depressive symptoms. We did not consider full-criteria depressive disorder or episode.
Mediterranean diet adherence (continuous). Adherence to Mediterranean diet was measured with the score proposed by Panagiotakos et al. (Panagiotakos et al., 2006; Veronese et al., 2016a, 2016b, 2017a).
Physical activity (continuous). Physical activity was evaluated using the validated Physical Activity Scale for the Elderly (PASE). This scale covers 12 physical activities, scoring from 0 without a cut-off score.
Health-related QoL (continuous). Health-related QoL was measured with the Short-Form Health Survey 12 (SF-12) (McHorney et al., 1994; Burdine et al., 2000), and in particular two separate scores were considered in the network: physical SF-12, namely the QoL related to physical health, and mental SF-12, namely the QoL related to mental health.
Network estimation
All codes used for the present analyses are described in the online Supplementary Material.
The network was estimated with RStudio (R_Core_Team, 2013) using mgm and qgraph package according to the methods described by Borsboom and Cramer (2013), Costantini et al. (2014), Haslbeck and Waldorp (2015) and Epskamp et al. (2017).
Within the networks (Cuthbert, 2014; Insel, 2014; Wildes and Marcus, 2015; Patrick and Hajcak, 2016; Epskamp et al., 2017), variables are represented as nodes, connected by edges. Namely, edges are the regularised partial correlations between the nodes. Nodes are reciprocally connected creating a network of interacting self-reinforcing pools of variables. In the present network analysis, a pairwise mixed graphical model was estimated (Haslbeck and Waldorp, 2015) and several properties of the estimated network were measured (Epskamp et al., 2012). This method allows to estimate undirected associations, called edges, among variables, called nodes, without implying any directionality, and allowing to pool together categorical and continuous variables. Biological variables and other conditions are often interconnected, and an excess of sparse correlations may add confusion without adding information to a network interpretation. As a consequence, we applied a penalty to correlations close to zero, to retain only meaningful associations. Such operation is also defined as a ‘least absolute shrinkage and selection operator’ (LASSO) (Friedman et al., 2014) regularisation (a sort of shrinkage of small edges to zero), which was applied in order to only retain more solid edges (regularised partial correlations). Using LASSO, we aimed for a conservative approach that makes results more interpretable. Also, the Extended Bayesian Information Criterion (EBIC) (Chen and Chen, 2008; Foygel and Drton, 2010), a parameter that sets the degree of regularisation/penalty applied to sparse correlations, was set to 0.5 (BIC = 0 would allow sparse and meaningless correlations to survive regularisation, while BIC = 0.5 applies a conservative approach).
Network inference
Analyses also assessed the centrality indices of nodes, namely how strongly the nodes were interconnected with several other nodes of the network. Centrality indices (node strength, closeness, betweenness) measure how important a node is in a given network. Centrality of nodes was estimated with node strength (i.e. the absolute sum of edge weights), closeness (i.e. the inverse of the sum of the distances of the focal node from all the other nodes in the network) (Costantini et al., 2014) and betweenness indices (i.e. the number of shortest paths between any two nodes that pass through the node of interest) (Costantini et al., 2014). This approach allows circularity of regularised partial correlations. Such methodology is considered an alternative approach to generalised linear modelling, or latent component analysis. No a priori direction or causal modelling is assumed, also because data used in the model were observational and cross-sectional.
Network stability
The stability of the network after removing increasing percentages of patients was measured as well, by means of a case-dropping subset bootstrapping, namely the re-calculation of centrality indices after dropping growing percentages of the included participants (Epskamp et al., 2017). To quantify stability of the centrality indices, the correlation stability coefficient (CS) was calculated. CS represents the maximum proportion of population that can be dropped with re-calculated indices correlating at least 0.7 with indices of the original full sample (auto-correlation). Networks with reliable centrality should have a CS ≥0.25, ideally higher than 0.5 for centrality estimates, being optimal if 0.75. In addition, to measure edges’ accuracy, an estimated 95% confidence interval of the range containing the true regularised partial correlations (edge) was calculated by means of ‘non-parametric’ bootstrapping (n boots = 1000).
Results
Characteristics of the included sample
Characteristics of the included sample are reported in Table 1. Out of 4796 individuals potentially eligible, we ultimately included 3532 North-American adults with or at risk for osteoarthritis. Excluded were subjects with missing values of at least one of the variables included in the network. Mean age of participants was 62.2 (9.0) years, and the average number of medications was 3.68 (2.55). Cases included in the present analysis had significantly higher Charlson comorbidity score (p < 0.001), more depressive symptoms (p = 0.043), were more frequently smokers (p < 0.001), lower physical and mental health-related QoL (p = 0.007; p = 0.047, respectively), lower physical activity levels (p = 0.013), lower income (p < 0.001) and slightly higher adherence to Mediterranean diet (p < 0.001), compared with those excluded for missing values. No difference emerged with respect to age, education, BMI, alcohol intake, number of medications.
Table 1.
Characteristics of multidimensional network in a sample of 3532 North-American adults
| Continuous variables | Mean | s.d. | Continuous variables | Mean | s.d. | Categorical variable | % |
|---|---|---|---|---|---|---|---|
| Age (years) | 62.15 | 9.01 | SF-12 physical (range: 13–68) | 48.20 | 9.16 | Education (college graduate) | 30.18 |
| Body mass index (kg/m2) | 28.91 | 4.84 | SF-12 mental (range: 10–73) | 53.56 | 8.22 | Lifetime smoking (yes) | 48.50 |
| CES-D (range: 0–57) | 6.82 | 7.07 | PASE (range: 0–531) | 155.08 | 80.71 | Income >US$50 000/year | 60.11 |
| Alcohol (number of drinks/week) | 1.71 | 1.48 | Number of medications | 3.68 | 2.54 | ||
| Charlson index (range: 0–10) | 0.45 | 0.89 | Mediterranean diet adherence score (range: 0–44) | 28.09 | 5.01 |
CES-D, Center for Epidemiologic Studies-Depression Scale; COPD, chronic obstructive pulmonary disease; Education, completed college; Functioning, income >US$50 000; PASE, Physical activity Scale for the Elderly; SF-12, Short-Form Health Survey 12 items
Network description
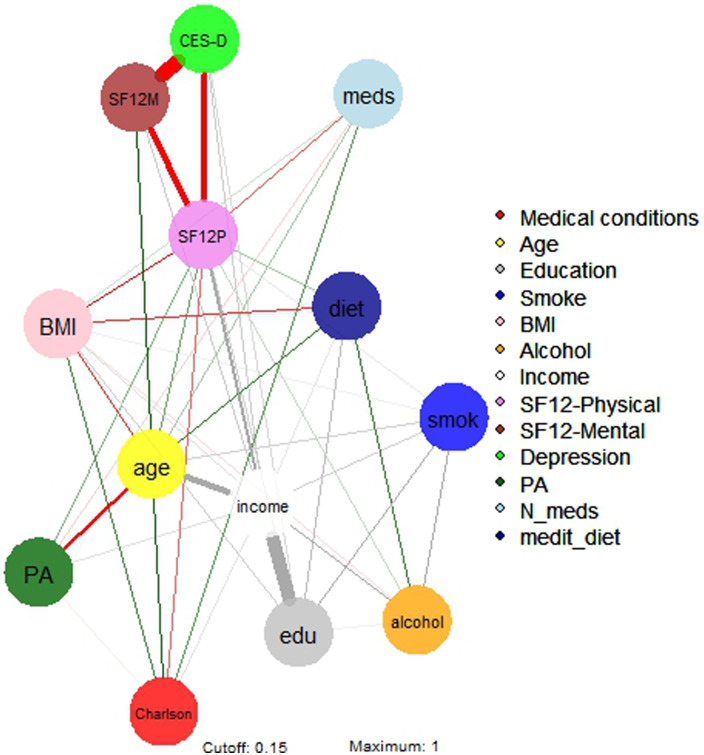
The regularised partial correlations matrix is reported in online Supplementary Table S1, and the network is represented in Figure 1.
Fig. 1.
Network 1 of multidimensional variables in a sample of 3532 North-American adults aged >45 years old. BMI, body mass index; Depression, Center for Epidemiologic Studies – Depression score; drinkweek, drinks per week; education, college completers; Income, yearly income >US$50 000; Medical conditions, Charlson comorbidity index; N_meds, number of medications; medit_diet, adherence to Mediterranean diet; Physical activity, PASE – Physical activity Scale for the Elderly; SF12 phys/ment, Short-Form Health Survey 12 physical/mental score; Smoking, life-time smokers.
Income
The strongest regularised partial correlations were observed between income and education (0.652), alcohol (0.186) and physical health-related QoL (0.232). Income also correlated with physical activity (0.056) and adherence to Mediterranean diet (0.041). Negative connections were found between income and age (−0.356), depressive symptoms (−0.091), Charlson comorbidity score (−0.049) and BMI (−0.056).
Physical health-related QoL
The strongest direct regularised partial correlations were observed between physical health-related QoL and income (0.232), followed by education and age (0.087), physical activity (0.073), Mediterranean diet (0.054) and alcohol (0.034). Negative connections were found between physical health-related QoL and depressive symptoms (−0.354), BMI (−0.146), number of medications (−0.104) and Charlson comorbidity index (−0.095).
Age
The strongest regularised partial correlations were observed between age and mental health-related QoL (0.173), Charlson comorbidity index (0.146), adherence to Mediterranean diet (0.126), smoking (0.081) and polypharmacotherapy (0.052). Negative connections were found between age and income (−0.355), physical activity (−0.263) and BMI (−0.129).
Mental health-related QoL
The strongest regularised partial correlations were between mental health-related QoL and age (0.173), and income (0.090). Negative connections were found between mental health-related QoL and depressive symptoms (−0.702).
Depressive symptoms
Negative connections were found between depressive symptoms and mental health-related QoL (−0.702), physical health-related QoL (−0.354), income (−0.090) and education (−0.068).
Education
The strongest regularised partial correlations were observed between education and income (0.652), smoking (0.142) and adherence to Mediterranean diet (0.116). A negative connection was found between education and depressive symptoms (−0.068).
To be noted, physical health-related QoL was a ‘bridge node’ among depressive symptoms and several other nodes, including Charlson comorbidity index, polypharmacotherapy, BMI, physical activity and adherence to Mediterranean diet.
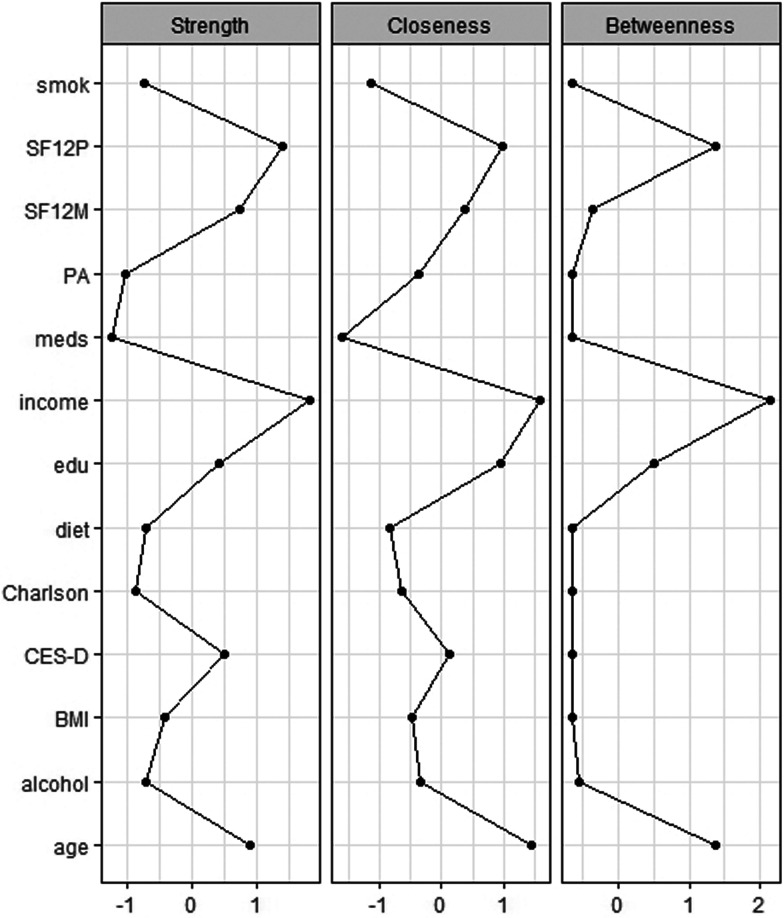
Network inference
The network's representation is summarised in Fig. 2. Strengths of the multidimensional nodes are reported in Table 2, and figures of centrality indices are reported in Fig. 2. Among nodes with higher centrality indices (higher than M = 1), the most central node was income (M = 1.891), followed by physical health-related QoL (M = 1.681), age (M = 1.416), mental health-related QoL (M = 1.342), depressive symptoms (M = 1.214) and education (M = 1.173). Lower centrality indices between 0.5 and 0.8 were found for BMI (M = 0.733), alcohol use (M = 0.590), adherence to Mediterranean diet (M = 0.587), smoking (M = 0.571) and Charlson comorbidity index (M = 0.512).
Fig. 2.
Centrality indices of multidimensional variables in a sample of 3532 North-American adults aged >45 years old. BMI, body mass index; Ch_, Charlson comorbiditiy index; cll, college completers; CES, Center for Epidemiologic Studies-Depression; drn, drinks per week; i > 5, yearly income >US$50 000; mds, number of medications; md_, adherence to Mediterranean diet; PAS, PASE – Physical activity Scale for the Elderly; SF12p/SF12m, Short-Form Health Survey 12 physical/mental score, smk, life-time smokers.
Table 2.
Strength of nodes of multidimensional networks in a sample of 3532 North-American adults years old
| Nodes | Strength |
|---|---|
| Income >US$50 000 | 1.891 |
| Short-Form Health Survey 12 items (SF-12) physical health score | 1.681 |
| Age | 1.416 |
| Short-Form Health Survey 12 items (SF-12) mental health score | 1.342 |
| Center for Epidemiologic Studies-Depression (CES-D) score | 1.214 |
| College graduate | 1.173 |
| Body mass index | 0.733 |
| Mean alcoholic drinks per week | 0.590 |
| Mediterranean diet adherence score | 0.587 |
| Lifetime smoking status | 0.571 |
| Charlson comorbidity index | 0.512 |
| Physical activity Scale for the Elderly (PASE) score | 0.431 |
| Number of medications | 0.311 |
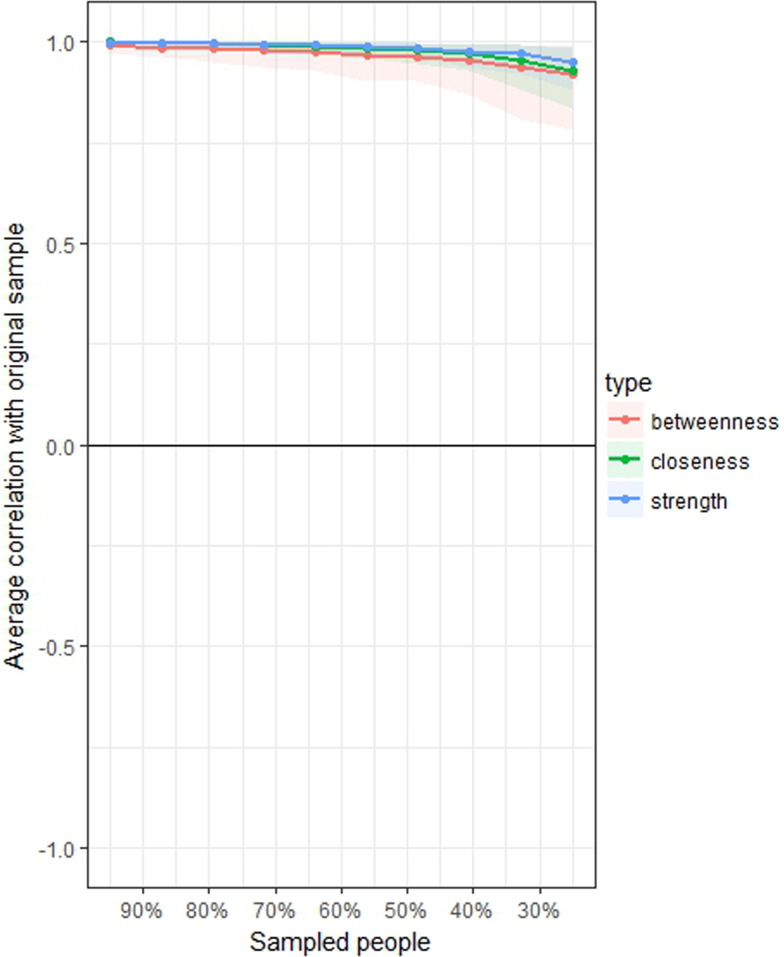
Network stability
Stability of the network 2, measured with the central stability coefficient (maximum drop proportions to retain correlation of 0.7 in at least 95% of the sample) was 0.75 or above for strength, 0.75 or above for closeness and 0.75 or above for betweenness (Fig. 3). Accuracy of the estimated edges among nodes is represented in online Supplementary Fig. S1.
Fig. 3.
Average correlations between centrality indices of networks sampled with persons dropped and in the original sample of 3532 North-American adults aged >45 years old. Lines indicate the means and areas indicate the range from the 2.5th quantile to the 97.5th quantile.
Discussion
The aim of this study was to describe the complex interactions of a multidimensional set of variables in a population of North-American adults with or at risk for knee osteoarthritis. A further aim was to test whether depressive symptoms had a central role in this network, and whether depressive symptoms had a regularised partial correlation with life-style and health variables. Importantly, all associations reported in results and discussed below in this section have no direction, and preclude any causal inference.
Physical and mental health-related QoL, age, income, education and depressive symptoms were the variables with higher centrality. Nodes with higher centrality are those that maintain the status of the network, and those whose modification is expected to influence the whole network (Costantini et al., 2014).
Physical health-related QoL was associated with both physical activity and Mediterranean diet, as well as with income and education. These associations may support the central role of policies investing in education to reduce health-related costs in later stages of life (AHRQ, 2015; Hahn and Truman, 2015). Furthermore, this result confirms previous findings supporting the role of physical activity in improving QoL (Rejeski and Mihalko, 2001; Penedo and Dahn, 2005), and the role of exercise in improving QoL even in people affected by depression (Schuch et al., 2016). Moreover, the positive association between Mediterranean diet and QoL is in line with results from several large cohort studies (Henriquez Sanchez et al., 2012; Costarelli et al., 2013; Milte et al., 2015; Veronese et al., 2016a). The association between income and higher physical health-related QoL is also in line with previous evidence from clinical and general populations (Costa and Nogueira, 2014; Wyshak, 2016).
Mental health-related QoL was higher in older patients, again being consistent with previous findings in the general population (Bell, 2014). Reduced life expectancy in people with SMI (Chang et al., 2011; Laursen et al., 2013; Correll et al., 2017) might have also played a role in decreasing the rates of subjects with mental illness among elderly subjects. Additionally, the direct association between income and mental health-related QoL is also consistent with previous findings(Cao et al., 2016).
Income in the analysed sample was associated with a large set of favourable health and life-style outcomes, namely education, QoL, physical activity and adherence to Mediterranean diet. Replication of this association may differ across countries other than USA, given the different welfare organisations that may influence general well-being, access to health-care and QoL. However, to the best of our knowledge, we are not aware of any other study applying the same analysis to samples from different countries. Also, the direction of such associations remains to be elucidated.
As hypothesised, depressive symptoms played a central role in the analysed networks. In particular, CES-D score was indirectly correlated with Charlson comorbidity index, polypharmacotherapy and BMI. These three regularised partial correlations strongly support the proneness of individuals with depressive symptoms to be affected by medical illnesses or vice versa, and in particular suggest that mental health-related QoL may play a role in bridging mental and medical illness. These results are consistent with the large body of research supporting an increased medical burden in patients with SMI (Vancampfort et al., 2015; Vancampfort et al., 2016; Correll et al., 2017; Stubbs et al., 2017a), possibly extending it to sub-clinical populations. According to this network analysis, the association (yet indirect) between physical illness and depressive symptoms holds true in the elderly OAI population as well, in addition to clinical populations with full-criteria diagnosed depressive disorder. In other words, it appears that the association between depressive symptoms and medical comorbidity may already exist in the presence of sub-clinical depressive symptoms, and that it may be mediated by QoL.
Furthermore, this network analysis observed an indirect association between depressive symptoms and a general proneness to medical comorbidity. Several reasons may explain why a cumulative index of medical comorbidities was indirectly associated with depressive symptoms. First, common pathways have been described among depression and medical conditions, such as a pro-inflammatory state (Slyepchenko et al., 2016; Kohler et al., 2017; Milaneschi et al., 2018). Also, unhealthy life-style behaviours are common/non-specific risk factors for both depression and several medical conditions (Stubbs et al., 2016a; Veronese et al., 2016a, 2017b, 2017d; Soysal et al., 2017; Shivappa et al., 2018). Clinical implications of the close connection between depressive symptoms and greater morbidity and mortality from medical illnesses may exist (Vancampfort et al., 2015, 2016; Correll et al., 2017; Stubbs et al., 2017a).
These findings are relevant for several reasons. First, screening and early interventions for both depressive symptoms and medical conditions should be considered in health-care services (Mitchell et al., 2014; Mitchell et al., 2015). Second, should mental illness occur, it has been proposed that higher levels of physical comorbidity complicate the successful treatment of patients with depression (Sato and Yeh, 2013), given the additional safety and tolerability issues of psychopharmacologic agents in case of comorbid diabetes, cardiovascular disease, arthritis or chronic obstructive pulmonary disease (Stubbs et al., 2016b; Solmi et al., 2017). Third, in case of medical comorbidity, polypharmacotherapy is the rule rather than an exception, with drug–drug interactions further complicating the efficacy and safety scenario. Also, a finer grained description of the complex interaction among variables included in the network could help in better understanding what ongoing associations are there when designing specific interventions. This could be relevant in particular in the case of patients with osteoarthritis. People with osteoarthritis often suffer from chronic pain (Ho-Pham et al., 2014), which limits physical activity and increases sedentary behaviour. Low physical activity is associated with weight gain, which in turn is associated with a large set of unfavourable health outcomes. Also, depression itself is associated with low levels of physical activity and multimorbidity (Stubbs et al., 2017a). Hence, understanding the complex interaction among such variables, and showing that they are interconnected in a stable network, may suggest to design future interventions which ideally should not scotomise such a complex scenario. Moreover, the bridging role of physical health-related QoL may be targeted by specific interventions to potentially weaken the apparently indirect association among depressive symptoms and medical comorbidities, polypharmacotherapy, BMI, physical activity and adherence to Mediterranean diet. Of course, studies with a longitudinal, ideally prospective design are needed to better characterise the direction of aforementioned associations, which remain unknown based on this network analysis.
The study has several strengths. First the network proved to be stable as measured by CS > 0.25; actually results yielded the highest possible stability coefficient (CS = 0.75 for all centrality indices). This finding supports the reliability of the estimates of the multidimensional network among the variables included in the analysis, and should encourage the application of network analysis to other multidimensional sets of variables in future projects. Network analysis provides a valuable tool to investigate and describe how life-style, social, environmental, medical and psychiatric variables are closely connected. Second, the study had a large sample. Third, the network provides insight into a multidimensional set of variables in North-American elderly adults with or at risk for knee osteoarthritis who were not selected for mental health issues, providing insights into the connection between nutrition, social/occupational status functioning, depressive symptoms and other clinical and non-clinical variables.
The study has also some limitations that need to be considered when interpreting the results. First, several variables included in the network were self-reported (individual comorbidities that are summarised by the Charlson comorbidity index). Second, only depressive symptoms were measured, limiting any further consideration on other mental health burden, such as anxiety, bipolar disorder or psychosis spectrum symptoms. Third, depressive symptoms were measured with a rating scale, but no full-criteria diagnosis of depressive disorder was available. Fourth, data were cross-sectional, and therefore no causal inference can be made. Fifth, OAI includes adults aged >45 years old with knee osteoarthritis or at high risk of this condition. Finally, by excluding subjects with missing data, we selected a population with unfavourable medical and mental health status, which furtherly precludes any inference of present results to general population. Even if knee OA and its risk factors are very common also in the general population, other studies are needed to apply our results to the general population or different subpopulations of interest.
In conclusion, in elderly North-American adults with or at risk for osteoarthritis depressive symptoms play a central role in a multidimensional network, including QoL, income, age and medical comorbidities. The indirect association between the Charlson comorbidity index and polypharmacotherapy with depressive symptoms which are connected by a bridging node, namely health-related QoL, support the close interplay between these important variables that are each amenable to therapeutic action. QoL, income and age also play a central role. Finally, physical activity and adherence to Mediterranean diet were significantly associated with physical health-related QoL and with income. Future studies may address whether the same associations hold true in general population.
Acknowledgements
None.
Availability of data and materials
The original data set for the OAI is available from the OAI website (https://oai.epi-ucsf.org/datarelease/).
Financial support
None.
Ethical standards
All participants provided informed written consent, and the OAI study received ethical approval by the institutional review board of the OAI Coordinating Center, at the University of California, San Francisco.
Supplementary material
For supplementary material accompanying this paper visit http://dx.doi.org/10.1017/S204579601800077X.
click here to view supplementary material
Conflict of interest
Dr Correll has been a consultant and/or advisor to or has received honoraria from: Alkermes, Allergan, Angelini, Gerson Lehrman Group, IntraCellular Therapies, Janssen/J&J, LB Pharma, Lundbeck, Medavante, Medscape, Merck, Neurocrine, Otsuka, Pfizer, ROVI, Servier, Sunovion, Takeda and Teva. He has provided expert testimony for Bristol-Myers Squibb, Janssen and Otsuka. He served on a Data Safety Monitoring Board for Lundbeck, ROVI and Teva. He received royalties from UpToDate and grant support from Janssen and Takeda. He is also a shareholder of LB Pharma. No conflict of interest is reported for all other authors.
References
- AHRQ (2015) Understanding the Relationship Between Education and Health: A Review of the Evidence and an Examination of Community Perspectives. Agency for Healthcare Research and Quality, Rockville, MD. Available at http://www.ahrq.gov/professionals/education/curriculum-tools/population-health/zimmerman.html (Accessed 12 July 2018).
- American Psychiatric Association (2000) Diagnostic and Statistical Manual of Mental Disorders, 4th Edn. Text Revision. Washington, DC: Author. [Google Scholar]
- American Psychiatric Association (2013) Diagnostic and Statistical Manual of Mental Disorders, 5th Edn. Washington, DC: Author. [Google Scholar]
- Ban TA, Guy W and Wilson WH (1984) The psychopharmacological treatment of depression in the medically ill patient. Canadian Journal of Psychiatry 29, 461–466. [DOI] [PubMed] [Google Scholar]
- Bell A (2014) Life-course and cohort trajectories of mental health in the UK, 1991–2008 – a multilevel age-period-cohort analysis. Social Science and Medicine 120, 21–30. [DOI] [PubMed] [Google Scholar]
- Borsboom D and Cramer AO (2013) Network analysis: an integrative approach to the structure of psychopathology. Annual Review of Clinical Psychology 9, 91–121. [DOI] [PubMed] [Google Scholar]
- Burdine JN, Felix MR, Abel AL, Wiltraut CJ and Musselman YJ (2000) The SF-12 as a population health measure: an exploratory examination of potential for application. Health Services Research Journal 35, 885–904. [PMC free article] [PubMed] [Google Scholar]
- Cao W, Guo C, Ping W, Tan Z, Guo Y and Zheng J (2016) A community-based study of quality of life and depression among older adults. International Journal of Environmental Research and Public Health 13, 693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang CK, Hayes RD, Perera G, Broadbent MT, Fernandes AC, Lee WE, Hotopf M and Stewart R (2011) Life expectancy at birth for people with serious mental illness and other major disorders from a secondary mental health care case register in London. PLoS ONE 6, e19590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen J and Chen Z (2008) Extended Bayesian information criteria for model selection with large model spaces. Biometrika 95, 759–771. [Google Scholar]
- Chen A, Gupte C, Akhtar K, Smith P and Cobb J (2012) The global economic cost of osteoarthritis: how the UK compares. Arthritis 698709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chiu M, Lebenbaum M, Cheng J, de Oliveira C and Kurdyak P (2017) The direct healthcare costs associated with psychological distress and major depression: a population-based cohort study in Ontario, Canada. PLoS ONE 12, e0184268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi KW, Na EJ, Hong JP, Cho MJ, Fava M, Mischoulon D, Cho H and Jeon HJ (2018) Alcohol-induced disinhibition is associated with impulsivity, depression, and suicide attempt: a nationwide community sample of Korean adults. Journal of Affective Disorders 227, 323–329. [DOI] [PubMed] [Google Scholar]
- Correll CU, Solmi M, Veronese N, Bortolato B, Rosson S, Santonastaso P, Thapa-Chhetri N, Fornaro M, Gallicchio D, Collantoni E, Pigato G, Favaro A, Monaco F, Kohler C, Vancampfort D, Ward PB, Gaughran F, Carvalho AF and Stubbs B (2017) Prevalence, incidence and mortality from cardiovascular disease in patients with pooled and specific severe mental illness: a large-scale meta-analysis of 3,211,768 patients and 113,383,368 controls. World Psychiatry 16, 163–180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costa JM and Nogueira LT (2014) Association between work, income and quality of life of kidney transplant recipient the municipality of Teresina, PI, Brazil. Journal of Brazilian Nephrology 36, 332–338. [DOI] [PubMed] [Google Scholar]
- Costantini G, Epskamp S, Borsboom D, Perugini M, Mottus R, Waldorp L and Cramer AOJ (2014) State of the aRt personality research: a tutorial on network analysis of personality data in R. Journal of Research in Personality 54, 13–29. [Google Scholar]
- Costarelli V, Koretsi E and Georgitsogianni E (2013) Health-related quality of life of Greek adolescents: the role of the Mediterranean diet. Quality of Life Research 22, 951–956. [DOI] [PubMed] [Google Scholar]
- Cotrena C, Branco LD, Kochhann R, Shansis FM and Fonseca RP (2016) Quality of life, functioning and cognition in bipolar disorder and major depression: a latent profile analysis. Psychiatry Research 241, 289–296. [DOI] [PubMed] [Google Scholar]
- Cuthbert BN (2014) The RDoC framework: facilitating transition from ICD/DSM to dimensional approaches that integrate neuroscience and psychopathology. World Psychiatry 13, 28–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eby GA and Eby KL (2006) Rapid recovery from major depression using magnesium treatment. Medical Hypotheses 67, 362–370. [DOI] [PubMed] [Google Scholar]
- Ellervik C, Kvetny J, Christensen KS, Vestergaard M and Bech P (2014) Prevalence of depression, quality of life and antidepressant treatment in the Danish General Suburban Population Study. Nordic Journal of Psychiatry 68, 507–512. [DOI] [PubMed] [Google Scholar]
- Epskamp S, Cramer AOJ, Waldorp LJ, Schmittmann VD and Borsboom D (2012) Graph: network visualizations of relationships in psychometric. Data Journal of Statistical Software 48, 1–18, doi: 10.18637/jss.v048.i04. [DOI] [Google Scholar]
- Epskamp S, Borsboom D and Fried EI (2017) Estimating psychological networks and their accuracy: a tutorial paper. Behavior Research Methods 50, 195–212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foygel R and Drton M (2010) Extended Bayesian information criteria for Gaussian graphical models. Advances in Neural Information Processing Systems 23, 2020–2028. [Google Scholar]
- Friedman J, Hastie T and Tibshirani R (2014) Glasso: Graphical lasso estimation of Gaussian graphical models. R package version 1.8. Available at http://CRAN.R-project.org/package=glasso. (Accessed 12 July 2018).
- Frye MA, Ketter TA, Leverich GS, Huggins T, Lantz C, Denicoff KD and Post RM (2000) The increasing use of polypharmacotherapy for refractory mood disorders: 22 years of study. Journal of Clinical Psychiatry 61, 9–15. [DOI] [PubMed] [Google Scholar]
- Galderisi S, Rucci P, Kirkpatrick B, Mucci A, Gibertoni D, Rocca P, Rossi A, Bertolino A, Strauss GP, Aguglia E, Bellomo A, Murri MB, Bucci P, Carpiniello B, Comparelli A, Cuomo A, De Berardis D, Dell'Osso L, Di Fabio F, Gelao B, Marchesi C, Monteleone P, Montemagni C, Orsenigo G, Pacitti F, Roncone R, Santonastaso P, Siracusano A, Vignapiano A, Vita A, Zeppegno P, Maj M and Italian Network for Research on, P. (2018) Interplay among psychopathologic variables, personal resources, context-related factors, and real-life functioning in individuals with schizophrenia: a network analysis. JAMA Psychiatry 75, 396–404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hahn RA and Truman BI (2015) Education improves public health and promotes health equity. International Journal of Health Services 45, 657–678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haslbeck J and Waldorp L (2015) Mgm: estimating time-varying mixed graphical models in high-dimensional data. Journal of Statistical Software arXiv151006871H [Google Scholar]
- Henriquez Sanchez P, Ruano C, de Irala J, Ruiz-Canela M, Martinez-Gonzalez MA and Sanchez-Villegas A (2012) Adherence to the Mediterranean diet and quality of life in the SUN Project. European Journal of Clinical Nutrition 66, 360–368. [DOI] [PubMed] [Google Scholar]
- Ho-Pham LT, Lai TQ, Mai LD, Doan MC, Pham HN and Nguyen TV (2014) Prevalence of radiographic osteoarthritis of the knee and its relationship to self-reported pain. PLoS ONE 9, e94563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hofer A, Mizuno Y, Wartelsteiner F, Wolfgang Fleischhacker W, Frajo-Apor B, Kemmler G, Mimura M, Pardeller S, Sondermann C, Suzuki T, Welte A and Uchida H (2017) Quality of life in schizophrenia and bipolar disorder: the impact of symptomatic remission and resilience. European Psychiatry 46, 42–47. [DOI] [PubMed] [Google Scholar]
- Hogarth L, Hardy L, Mathew AR and Hitsman B (2018) Negative mood-induced alcohol-seeking is greater in young adults who report depression symptoms, drinking to cope, and subjective reactivity. Experimental and Clinical Psychopharmacology 26, 138–146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hsieh CR and Qin X (2018) Depression hurts, depression costs: the medical spending attributable to depression and depressive symptoms in China. Health Economics 27, 525–544. [DOI] [PubMed] [Google Scholar]
- Insel TR (2014) The NIMH Research Domain Criteria (RDoC) Project: precision medicine for psychiatry. American Journal of Psychiatry 171, 395–397. [DOI] [PubMed] [Google Scholar]
- Katz JN, Chang LC, Sangha O, Fossel AH and Bates DW (1996) Can comorbidity be measured by questionnaire rather than medical record review? Medical Care 34, 73–84. [DOI] [PubMed] [Google Scholar]
- Kemp A, Preen DB, Glover J, Semmens J and Roughead EE (2013) Impact of cost of medicines for chronic conditions on low income households in Australia. Journal of Health Service Research & Policy 18, 21–27. [DOI] [PubMed] [Google Scholar]
- Kohler CA, Freitas TH, Maes M, de Andrade NQ, Liu CS, Fernandes BS, Stubbs B, Solmi M, Veronese N, Herrmann N, Raison CL, Miller BJ, Lanctot KL and Carvalho AF (2017) Peripheral cytokine and chemokine alterations in depression: a meta-analysis of 82 studies. Acta Psychiatrica Scandinavica 135, 373–387. [DOI] [PubMed] [Google Scholar]
- Laursen TM, Wahlbeck K, Hallgren J, Westman J, Osby U, Alinaghizadeh H, Gissler M and Nordentoft M (2013) Life expectancy and death by diseases of the circulatory system in patients with bipolar disorder or schizophrenia in the Nordic countries. PLoS ONE 8, e67133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li XH, An FR, Ungvari GS, Ng CH, Chiu HFK, Wu PP, Jin X and Xiang YT (2017) Prevalence of smoking in patients with bipolar disorder, major depressive disorder and schizophrenia and their relationships with quality of life. Science Reports 7, 8430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Licht-Strunk E, Van Marwijk HW, Hoekstra T, Twisk JW, De Haan M and Beekman AT (2009) Outcome of depression in later life in primary care: longitudinal cohort study with three years’ follow-up. British Medical Journal 338, a3079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin CH, Yen YC, Chen MC and Chen CC (2014) Depression and pain impair daily functioning and quality of life in patients with major depressive disorder. Journal of Affective Disorders 166, 173–178. [DOI] [PubMed] [Google Scholar]
- Luger TM, Suls J and Vander Weg MW (2014) How robust is the association between smoking and depression in adults? A meta-analysis using linear mixed-effects models. Addictive Behaviors 39, 1418–1429. [DOI] [PubMed] [Google Scholar]
- McHorney CA, Kosinski M and Ware JE Jr (1994) Comparisons of the costs and quality of norms for the SF-36 health survey collected by mail versus telephone interview: results from a national survey. Medical Care 32, 551–567. [DOI] [PubMed] [Google Scholar]
- Milaneschi Y, Simmons WK, van Rossum EFC and Penninx BW (2018) Depression and obesity: evidence of shared biological mechanisms. Molecular Psychiatry. doi: 10.1038/s41380-018-0017-5. Epub ahead of print. https://www.nature.com/articles/s41380-018-0017-5#rightslink. [DOI] [PubMed] [Google Scholar]
- Milte CM, Thorpe MG, Crawford D, Ball K and McNaughton SA (2015) Associations of diet quality with health-related quality of life in older Australian men and women. Experimental Gerontology 64, 8–16. [DOI] [PubMed] [Google Scholar]
- Mitchell AJ, Pereira IE, Yadegarfar M, Pepereke S, Mugadza V and Stubbs B (2014) Breast cancer screening in women with mental illness: comparative meta-analysis of mammography uptake. British Journal of Psychiatry 205, 428–435. [DOI] [PubMed] [Google Scholar]
- Mitchell AJ, Vancampfort D, De Hert M and Stubbs B (2015) Do people with mental illness receive adequate smoking cessation advice? A systematic review and meta-analysis. General Hospital Psychiatry 37, 14–23. [DOI] [PubMed] [Google Scholar]
- Panagiotakos DB, Pitsavos C and Stefanadis C (2006) Dietary patterns: a Mediterranean diet score and its relation to clinical and biological markers of cardiovascular disease risk. Nutrition, Metabolism, and Cardiovascular Diseases Nutrition, Metabolism and Cardiovascular Diseases 16, 559–568. [DOI] [PubMed] [Google Scholar]
- Patrick CJ and Hajcak G (2016) RDoc: translating promise into progress. Psychophysiology 53, 415–424. [DOI] [PubMed] [Google Scholar]
- Penedo FJ and Dahn JR (2005) Exercise and well-being: a review of mental and physical health benefits associated with physical activity. Current Opinions in Psychiatry 18, 189–193. [DOI] [PubMed] [Google Scholar]
- R_Core_Team (2013) R: A Language and Environment for Statistical Computing. Vienna, Austria: R Foundation for Statistical Computing. [Google Scholar]
- Radloff LS (1977) The CES-D scale: a self-report depression scale for research in the general population. Applied Psychological Measurement 1, 385–401. [Google Scholar]
- Rahman MA, Todd C, John A, Tan J, Kerr M, Potter R, Kennedy J, Rice F and Brophy S (2018) School achievement as a predictor of depression and self-harm in adolescence: linked education and health record study. British Journal of Psychiatry 212, 215–221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rejeski WJ and Mihalko SL (2001) Physical activity and quality of life in older adults. The Journals of Gerontology. Series A, Biological Sciences and Medical Sciences 56 Spec No 2, 23–35. [DOI] [PubMed] [Google Scholar]
- Sato S and Yeh TL (2013) Challenges in treating patients with major depressive disorder: the impact of biological and social factors. Central Nervous System Drugs 27(suppl. 1), S5–10. [DOI] [PubMed] [Google Scholar]
- Schuch FB, Vancampfort D, Rosenbaum S, Richards J, Ward PB and Stubbs B (2016) Exercise improves physical and psychological quality of life in people with depression: a meta-analysis including the evaluation of control group response. Psychiatry Research 241, 47–54. [DOI] [PubMed] [Google Scholar]
- Shivappa N, Hebert JR, Veronese N, Caruso MG, Notarnicola M, Maggi S, Stubbs B, Firth J, Fornaro M and Solmi M (2018). The relationship between the dietary inflammatory index (DII((R))) and incident depressive symptoms: a longitudinal cohort study. Journal of Affective Disorders 235, 39–44. [DOI] [PubMed] [Google Scholar]
- Slyepchenko A, Maes M, Machado-Vieira R, Anderson G, Solmi M, Sanz Y, Berk M, Kohler CA and Carvalho AF (2016) Intestinal dysbiosis, gut hyperpermeability and bacterial translocation: missing links between depression, obesity and type 2 diabetes. Current Pharmaceutical Designs 22, 6087–6106. [DOI] [PubMed] [Google Scholar]
- Solmi M, Murru A, Pacchiarotti I, Undurraga J, Veronese N, Fornaro M, Stubbs B, Monaco F, Vieta E, Seeman MV, Correll CU and Carvalho AF (2017) Safety, tolerability, and risks associated with first- and second-generation antipsychotics: a state-of-the-art clinical review. Therapeutic and Clinical Risk Management 13, 757–777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soysal P, Veronese N, Thompson T, Kahl KG, Fernandes BS, Prina AM, Solmi M, Schofield P, Koyanagi A, Tseng PT, Lin PY, Chu CS, Cosco TD, Cesari M, Carvalho AF and Stubbs B (2017) Relationship between depression and frailty in older adults: a systematic review and meta-analysis. Ageing Research Reviews 36, 78–87. [DOI] [PubMed] [Google Scholar]
- Stubbs B, Koyanagi A, Schuch FB, Firth J, Rosenbaum S, Veronese N, Solmi M, Mugisha J and Vancampfort D (2016a) Physical activity and depression: a large cross-sectional, population-based study across 36 low- and middle-income countries. Acta Psychiatrica Scandinavica 134, 546–556. [DOI] [PubMed] [Google Scholar]
- Stubbs B, Vancampfort D, Veronese N, Solmi M, Gaughran F, Manu P, Rosenbaum S, De Hert M and Fornaro M (2016b) The prevalence and predictors of obstructive sleep apnea in major depressive disorder, bipolar disorder and schizophrenia: a systematic review and meta-analysis. Journal of Affective Disorders 197, 259–267. [DOI] [PubMed] [Google Scholar]
- Stubbs B, Vancampfort D, Veronese N, Kahl KG, Mitchell AJ, Lin PY, Tseng PT, Mugisha J, Solmi M, Carvalho AF and Koyanagi A (2017a) Depression and physical health multimorbidity: primary data and country-wide meta-analysis of population data from 190 593 people across 43 low- and middle-income countries. Psychological Medicine 47, 2107–2117. [DOI] [PubMed] [Google Scholar]
- Stubbs B, Vancampfort D, Veronese N, Thompson T, Fornaro M, Schofield P, Solmi M, Mugisha J, Carvalho AF and Koyanagi A (2017b) Depression and pain: primary data and meta-analysis among 237 952 people across 47 low- and middle-income countries. Psychological Medicine 47, 2906–2917. [DOI] [PubMed] [Google Scholar]
- Stubbs B, Veronese N, Vancampfort D, Prina AM, Lin PY, Tseng PT, Evangelou E, Solmi M, Kohler C, Carvalho AF and Koyanagi A (2017c) Perceived stress and smoking across 41 countries: a global perspective across Europe, Africa, Asia and the Americas. Science Reports 7, 7597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stubbs B, Vancampfort D, Firth J, Schuch FB, Hallgren M, Smith L, Gardner B, Kahl KG, Veronese N, Solmi M, Carvalho AF and Koyanagi A (2018a) Relationship between sedentary behavior and depression: a mediation analysis of influential factors across the lifespan among 42,469 people in low- and middle-income countries. Journal of Affective Disorders 229, 231–238. [DOI] [PubMed] [Google Scholar]
- Stubbs B, Vancampfort D, Firth J, Solmi M, Siddiqi N, Smith L, Carvalho A and Koyanagi A (2018b) Association between depression and smoking: a global perspective from 48 low- and middle-income countries. Journal of Psychiatric Research 103, 142–149. [DOI] [PubMed] [Google Scholar]
- Tjora T, Hetland J, Aaro LE, Wold B, Wiium N and Overland S (2014) The association between smoking and depression from adolescence to adulthood. Addiction 109, 1022–1030. [DOI] [PubMed] [Google Scholar]
- Vancampfort D, Stubbs B, Mitchell AJ, De Hert M, Wampers M, Ward PB, Rosenbaum S and Correll CU (2015) Risk of metabolic syndrome and its components in people with schizophrenia and related psychotic disorders, bipolar disorder and major depressive disorder: a systematic review and meta-analysis. World Psychiatry 14, 339–347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vancampfort D, Correll CU, Galling B, Probst M, De Hert M, Ward PB, Rosenbaum S, Gaughran F, Lally J and Stubbs B (2016) Diabetes mellitus in people with schizophrenia, bipolar disorder and major depressive disorder: a systematic review and large scale meta-analysis. World Psychiatry 15, 166–174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Veronese N, Stubbs B, Noale M, Solmi M, Luchini C and Maggi S (2016a) Adherence to the Mediterranean diet is associated with better quality of life: data from the Osteoarthritis Initiative. American Journal of Clinical Nutrition 104, 1403–1409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Veronese N, Stubbs B, Noale M, Solmi M, Luchini C, Smith TO, Cooper C, Guglielmi G, Reginster JY, Rizzoli R and Maggi S (2016b) Adherence to a Mediterranean diet is associated with lower prevalence of osteoarthritis: data from the osteoarthritis initiative. Clinical Nutrition 36, 1609–1614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Veronese N, Stubbs B, Noale M, Solmi M, Rizzoli R, Vaona A, Demurtas J, Crepaldi G and Maggi S (2017a) Adherence to a Mediterranean diet is associated with lower incidence of frailty: a longitudinal cohort study. Clinical Nutrition 37, 1492–1497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Veronese N, Stubbs B, Noale M, Solmi M, Vaona A, Demurtas J, Nicetto D, Crepaldi G, Schofield P, Koyanagi A, Maggi S and Fontana L (2017b) Fried potato consumption is associated with elevated mortality: an 8-y longitudinal cohort study. American Journal of Clinical Nutrition 106, 162–167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Veronese N, Stubbs B, Solmi M, Smith TO, Noale M, Cooper C and Maggi S (2017c) Association between lower limb osteoarthritis and incidence of depressive symptoms: data from the osteoarthritis initiative. Age and Ageing 46, 470–476. [DOI] [PubMed] [Google Scholar]
- Veronese N, Stubbs B, Trevisan C, Bolzetta F, De Rui M, Solmi M, Sartori L, Musacchio E, Zambon S, Perissinotto E, Baggio G, Crepaldi G, Manzato E, Maggi S and Sergi G (2017d) Poor physical performance predicts future onset of depression in elderly people: Progetto Veneto Anziani Longitudinal Study. Physical Therapy 97, 659–668. [DOI] [PubMed] [Google Scholar]
- Vittengl JR (2018) Mediation of the bidirectional relations between obesity and depression among women. Psychiatry Research 264, 254–259. [DOI] [PubMed] [Google Scholar]
- Wildes JE and Marcus MD (2015) Application of the Research Domain Criteria (RDoC) framework to eating disorders: emerging concepts and research. Current Psychiatry Reports 17, 30. [DOI] [PubMed] [Google Scholar]
- Woolf AD and Pfleger B (2003) Burden of major musculoskeletal conditions. Bulletin of World Health Organization 81, 646–656. [PMC free article] [PubMed] [Google Scholar]
- Wyshak G (2016) Income and subjective well-being: new insights from relatively healthy American women, ages 49–79. PLoS ONE 11, e0146303. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
For supplementary material accompanying this paper visit http://dx.doi.org/10.1017/S204579601800077X.
click here to view supplementary material
Data Availability Statement
The original data set for the OAI is available from the OAI website (https://oai.epi-ucsf.org/datarelease/).