Abstract
Aims
Mental disorders in children are a significant and growing cause of morbidity worldwide. Although interventions to help overcome barriers along the pathway to accessing health care for children with mental disorders exist, there is no overview of randomised controlled trials (RCTs) on these interventions as yet. This study aimed to systematically identify RCTs of interventions to improve access to mental health care for children and synthesise them using a conceptual framework of access to health care.
Methods
This systematic review was performed following a predefined protocol registered with PROSPERO (ID: CRD42018081714). We searched the databases MEDLINE, EMBASE, PsycINFO and CENTRAL for RCTs up to 15 May 2019 using terms related to the concepts ‘young people,’ ‘mental disorders’ and ‘help-seeking interventions’ and scanned reference lists from relevant studies. Two reviewers independently screened all identified articles in a two-stage process, extracted results on outcomes of interest (knowledge, attitudes, intentions, help-seeking, accessing care, mental health outcomes and satisfaction), assessed the risk of bias and conducted meta-analyses where deemed appropriate.
Results
After screening 5641 identified articles, 34 RCTs were eligible for inclusion. Eighty per cent of universal school-based interventions measuring knowledge (n = 5) and 67% measuring attitudes (n = 6) reported significantly better results compared with controls on those outcomes, whereas 20% measuring access to care (n = 5) and none measuring mental health outcomes (n = 7) did. In contrast, 71% of interventions targeting at-risk individuals (n = 21) reported better access to care compared with controls, while just 33% (n = 6) did for mental health outcomes. For satisfaction with care, this proportion was 80% (n = 5). Meta-analyses of interventions measuring initial appointment attendance yielded combined odds ratios of 3.11 (2.07–4.67) for appointment reminder interventions and 3.51 (2.02–6.11) for treatment engagement interventions. The outcomes for universal school-based interventions were heterogeneous and could not be summarised quantitatively through meta-analysis.
Conclusions
To have a population-level effect on improving children's access to mental health care, two-stage interventions that identify those in need and then engage them in the health-care system may be necessary. We need more evidence on interventions to target contextual factors such as affordability and infrastructural barriers.
Key words: Children and adolescents, child psychiatry, children, health service research, mental health, pediatrics, systematic reviews
Introduction
Mental disorders are one of the most significant causes of disability-adjusted life-years worldwide, and they continue to grow in importance as a major contributor to the global burden of disease (GBD 2015 DALYs and HALE Collaborators, 2016). Because mental disorders usually first occur early in life (Kessler et al., 2005) and are characterised by recurrent episodes and symptoms that strongly affect work capacity (Simon et al., 2001), they have a significant impact on public health and society.
Childhood and adolescence are particularly critical periods for the identification and treatment of mental disorders. At 45% of the overall burden of disease in 15–19 year-olds, mental health issues are the leading cause of disability in adolescents (The Lancet, 2017). In addition, young patients with a mental disorder have a lower probability of receiving treatment and a longer delay between disease onset and first treatment compared with adults (Christiana et al., 2000; Wang et al., 2005; Iza et al., 2013). Despite the magnitude and importance of mental health problems in childhood and adolescence, international studies have consistently revealed a treatment gap: estimates of the gap between those in need of mental health care and those who access it exceed 50% (Saxena et al., 2007).
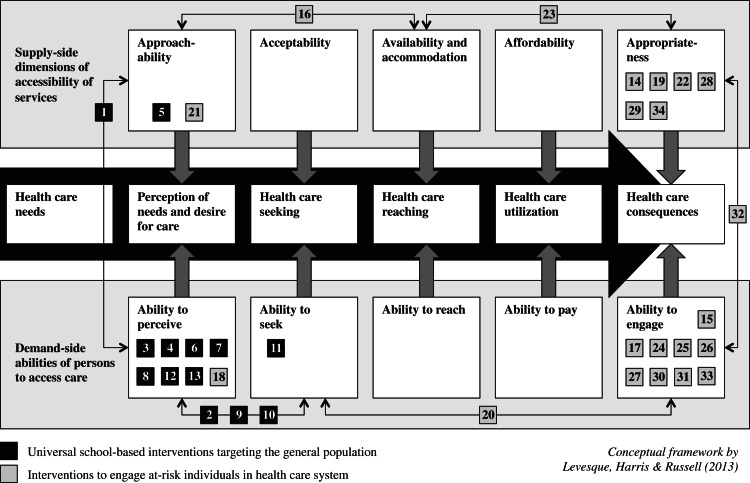
Levesque et al. (2013) define access to health care as ‘the opportunity to reach and obtain appropriate health-care services in situations of perceived need for care’ (Levesque et al., 2013). They have proposed a comprehensive conceptual framework describing accessing health care as a series of steps beginning with the opportunity to perceive health-care needs that can lead to opportunities to seek health care, reach health-care services, utilise health-care services and ultimately have health-care needs fulfilled (Levesque et al., 2013). At each stage, supply-side dimensions of accessibility of services (e.g., approachability, availability or affordability) interact with demand-side abilities of persons (e.g., abilities to perceive, pay or engage) to determine access to health care (see Appendix 1) (Levesque et al., 2013). In other words, the care that is obtained depends on the interplay of characteristics of individuals, such as their socio-economic status or where they live, and those of services and the environment, such as how much services cost and where they are located. Potential barriers that could explain the treatment gap can be found at each transition from step to step along this pathway to accessing care (Levesque et al., 2013). Barriers to mental health help-seeking in young people include lack of knowledge about services and stigma about mental health problems (Gulliver et al., 2010). As an example of barriers on the supply side, paediatricians perceive a wide variety of organizational hindrances, including inadequate reimbursement and lack of time and space, and many feel they lack the training and confidence to treat mental disorders (Horwitz et al., 2007).
To close the treatment gap, interventions targeting one or more dimensions of accessibility of services and/or abilities of persons have been designed to address the barriers along the pathway to accessing care (e.g., screenings, health literacy promotion); however, there is little high-quality evidence on these interventions (National Institute for Health and Clinical Excellence, 2011). Moreover, systematic reviews conducted in the past on interventions to improve access to mental health care for children and adolescents have limited searches to specific types of interventions and disorders (Ingoldsby, 2010; Gulliver et al., 2012; Lindsey et al., 2014; Anderson et al., 2017; Dunne et al., 2017; Richardson et al., 2017). This study thus aimed to systematically identify randomised controlled trials (RCTs) of all interventions designed to improve access to mental health care for children along the entire pathway to accessing care, describe them using Levesque et al. (2013)'s conceptual framework of access to health care (Levesque et al., 2013) and conduct meta-analyses for intervention types with comparable outcomes.
Methods
The methods used for this systematic review are based on the Centre for Reviews and Dissemination's guidance for undertaking reviews in health care (Centre for Reviews and Dissemination, 2009), and our reporting follows the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) (Moher et al., 2009). A PRISMA checklist can be found in Appendix 2. We registered our systematic review protocol with the International Prospective Register of Systematic Reviews (PROSPERO, ID: CRD42018081714).
Types of participants
We included interventions designed for children and adolescents <19 years old, both from the general population and vulnerable groups. If the age range exceeded 18 years old, the intervention was only included if more than 50% of the ages considered were under 19. Interventions that addressed the following disorders from the International Classification of Diseases, 10th Revision (ICD-10) (World Health Organization, 1992) as well as suicidal ideation were considered: F10–F59 and F90–99 (all mental disorders except for mental disorders due to known physiological conditions, disorders of adult personality and behaviour, intellectual disabilities and pervasive and specific developmental disorders including autism spectrum disorders). We also included studies that targeted children with emotional or behavioural problems since children are not always given a specific diagnosis.
Types of interventions
Any intervention designed to improve access to mental health was included; thus, the intervention could target any one of the five supply-side dimensions or five demand-side abilities included within the conceptual framework. Examples of specific intervention targets are listed next to each dimension or ability in Appendix 1. For example, an intervention could change where services are offered or deliver services via the Internet (National Institute for Health and Clinical Excellence, 2011). The interventions could target the child or adolescent directly or others, including parents/caregivers, teachers, friends or health-care professionals (potential helpers).
Types of outcome measures
We defined outcomes using the conceptual framework and expanded upon these using conceptualisations from previous systematic reviews on help-seeking and treatment engagement interventions (Gulliver et al., 2012; Lindsey et al., 2014). Outcomes at all steps in the process of accessing health care were included in the review: knowledge about accessing mental health care, changed attitudes or beliefs about seeking care, intentions to seek care, help-seeking attempts to access health-care services (successful or not) or action taken by a potential helper, mental health outcomes and satisfaction with health-care services. For a study with outcomes on health measures and satisfaction with care to be included in the analysis, the study also had to measure access to care as an outcome. We excluded studies for which it was not possible to calculate any effect sizes.
Search methods for identification of studies
We performed the literature search on 15 May 2019 in the following electronic databases: MEDLINE, EMBASE, PsycINFO and the Cochrane Central Register of Controlled Trials (CENTRAL). The search strategy included terms relating to the concepts ‘young people,’ ‘mental disorders’ and ‘help-seeking interventions.’ The full search strategy can be found in Appendix 3. Publications not originally published in English were excluded from the search. We enhanced our search by scanning the reference lists of papers (both primary studies and reviews) that were identified by the database search. Duplicates were removed during the title and abstract screening.
Selection of studies and data extraction
Two reviewers (LW, DG) independently assessed the title and abstract of all identified papers, recorded their decision about whether the paper should be included for full-text assessment and discussed discrepant decisions until a consensus was reached. All papers deemed potentially eligible by the reviewers were included in the full-text assessment, in which the two reviewers decided on study inclusion based on the inclusion criteria and discussed any discrepant decisions until they reached a consensus.
The two reviewers independently extracted data on the following study characteristics: title, first author, year, country, study design, age range, intervention setting, condition in focus, sample size, response rate, intervention condition, control condition, length of intervention, evaluation time points, method of outcome assessment and results.
Assessment of risk of bias in included studies
Two reviewers (LW, DG) assessed the risk of bias of each article using the Cochrane Collaboration's tool for assessing risk of bias in randomised trials (Higgins et al., 2011) and discussed discrepant evaluations until they reached a consensus. Because our review included a large variety of interventions and outcomes, we could rarely assess the heterogeneity, imprecision and indirectness beyond a single or a few studies and therefore decided against using the Grading of Recommendations Assessment, Development and Evaluation (GRADE) approach (Guyatt et al., 2011) to judge the overall quality of evidence. Instead, we used the risk of bias assessment as an indicator of the quality of evidence.
Data synthesis and measures of effect
We mapped the study results using the conceptual framework by Levesque et al. (2013) by target of intervention (Fig. 2) and by outcome (Fig. 3). For dichotomous outcomes, we extracted or calculated the odds ratio and 95% confidence interval, whereas, for continuous outcomes, we calculated the standardised mean difference and 95% confidence interval using Cohen's d with the package ‘esc’: Effect Size Computation for Meta Analysis in R (Lüdecke, 2017).
Fig. 2.
Target of interventions.
Fig. 3.
Significance of interventions' effect on targeted outcomes.
For intervention types with comparable outcomes, we conducted meta-analyses using the inverse variance method. We calculated a fixed-effects model if I2 was <30% and both fixed and random effects models if I2 was >30% using the package ‘meta’: General Package for Meta-Analysis in R (Schwarzer, 2007).
Results
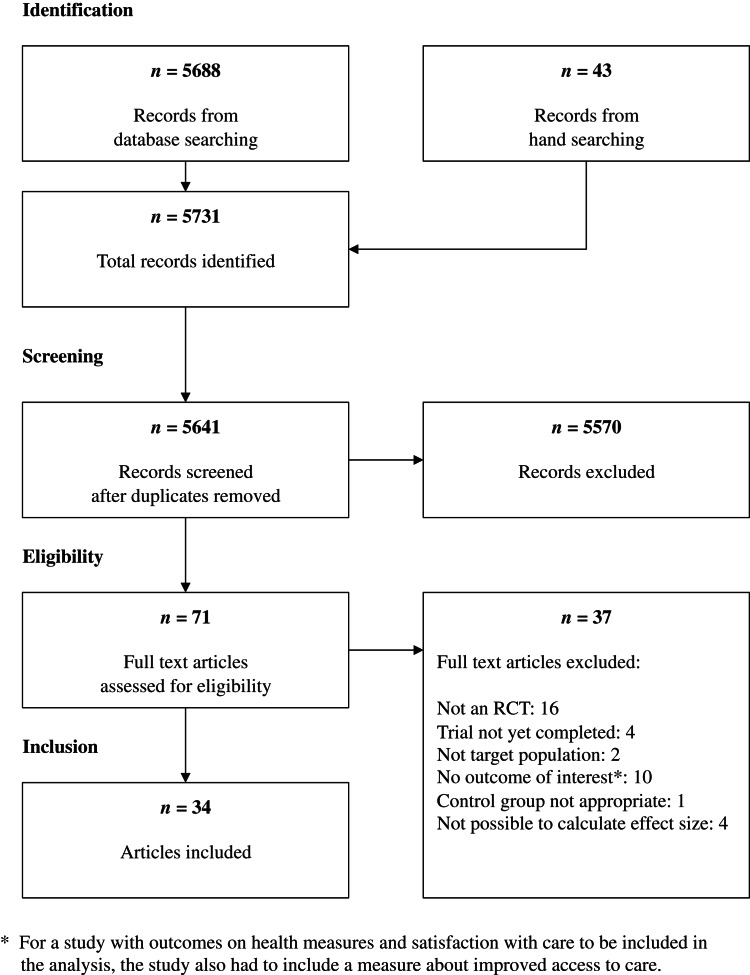
Results of the search and excluded studies
The electronic search yielded 5688 articles, and an additional 43 records were identified through hand searching. Of these 5731 records, 5641 unique studies remained after duplicates were removed. A total of 71 articles were considered eligible for full-text screening following the title and abstract screening. During the full-text screening process, 37 articles were excluded; the full list of articles excluded along with reason for exclusion can be found in Appendix 4. The remaining 34 articles were included in the systematic review. For an overview of the search and screening process, please see the study flow diagram (Fig. 1).
Fig. 1.
Study flow diagram.
Included studies
A summary of the characteristics of the 34 RCTs identified through the two-stage screening process can be found in Appendix 5. These studies fell into two main categories: (1) universal school-based interventions targeting the general population (13 studies) and (2) interventions to engage at-risk individuals who had already been identified by the health-care system (21 studies). The vast majority of these studies were conducted in the USA (22 studies); the rest were conducted in Australia (five studies), UK (three studies), Canada (two studies), Portugal (one study) and Israel (one study).
The interventions in the first study category were designed to improve outcomes for general mental health problems, mental distress, suicide, depression and attention-deficit hyperactivity disorder. All studies in the second category took place in health-care settings (e.g., primary care, emergency department, mental health agency) and targeted general mental health problems, behavioural health problems, suicide, depression, substance abuse and conduct disorder. Interventions designed to help younger children access care tended to be addressed towards caretakers, whereas interventions targeting older age groups tended to address the adolescent directly.
Figure 2 provides an overview of the step or steps along the pathway to accessing care that each intervention targeted. Interventions within the first category exclusively targeted service providers' approachability (i.e., service providers making their existence known to individuals) and the abilities of individuals to perceive a need for and to seek care. These interventions included educational curricula, live or virtual contact with a mentally ill person, screenings and helper training programs. The vast majority of engagement interventions from the second category mostly targeted service providers' appropriateness or individuals' ability to engage. Forty-eight per cent (10/21) of these interventions consisted of programs to engage and motivate patients or to improve service providers' communication skills (henceforth called treatment engagement interventions), while 24% (5/21) involved using a telephone or letter reminder mechanism to improve first appointment attendance (henceforth called appointment reminder interventions). Just one intervention was infrastructural in nature and involved providing onsite mental health services for primary care patients. None of the identified studies targeted the acceptability (cultural and social factors that make it possible for individuals to accept services) of service providers, affordability of care, or individuals' personal ability to reach (e.g., their personal mobility or support from their social network) or pay for care.
Risk of bias in included studies
The results of the risk of bias assessment can be found in Table 1. The randomisation procedure was not described in half of the studies, and two studies described a non-random sequence generation procedure. Details on allocation concealment were only provided in 21% of the studies. In all studies except for one, it was unclear whether a lack of blinding of participants and personnel would influence the outcome. However, we judged that a lack of blinding of outcome assessment would not have an impact on the outcome since most outcomes were evaluated either by questionnaire or service use records. All but one study had a low risk of bias for incomplete outcome data. Three studies did not report all outcomes and three studies had other sources of potential bias.
Table 1.
Risk of bias of included studies
| a. | b. | c. | d. | e. | f. | g.* | |
|---|---|---|---|---|---|---|---|
| 1. Aseltine et al. (2007) |  |
 |
 |
 |
 |
 |
 |
| 2. Campos et al. (2018) |  |
 |
 |
 |
 |
 |
 |
| 3. Hart et al. (2018) |  |
 |
 |
 |
 |
 |
 |
| 4. Howard et al. (2018) |  |
 |
 |
 |
 |
 |
 |
| 5. Husky et al. (2011) |  |
 |
 |
 |
 |
 |
 |
| 6. Jorm et al. (2010) |  |
 |
 |
 |
 |
 |
 |
| 7. Klingman and Hochdorf (1993) |  |
 |
 |
 |
 |
 |
 |
| 8. Morgan et al. (2019) |  |
 |
 |
 |
 |
 |
 |
| 9. Painter et al. (2017) |  |
 |
 |
 |
 |
 |
 |
| 10. Perry et al. (2014) |  |
 |
 |
 |
 |
 |
 |
| 11. Saporito et al. (2011) |  |
 |
 |
 |
 |
 |
 |
| 12. Sayal et al. (2010) |  |
 |
 |
 |
 |
 |
 |
| 13. Sharpe et al. (2017) |  |
 |
 |
 |
 |
 |
 |
| 14. Asarnow et al. (2005) |  |
 |
 |
 |
 |
 |
 |
| 15. Asarnow et al. (2011) |  |
 |
 |
 |
 |
 |
 |
| 16. Coker et al. (2019) |  |
 |
 |
 |
 |
 |
 |
| 17. Donohue et al. (1998) |  |
 |
 |
 |
 |
 |
 |
| 18. Fristad et al. (2003) |  |
 |
 |
 |
 |
 |
 |
| 19. Gadomski et al. (2010) |  |
 |
 |
 |
 |
 |
 |
| 20. Grupp-Phelan et al. (2012) |  |
 |
 |
 |
 |
 |
 |
| 21. Gully et al. (2008) |  |
 |
 |
 |
 |
 |
 |
| 22. Kourany et al. (1990) |  |
 |
 |
 |
 |
 |
 |
| 23. Lieberman et al. (2006) |  |
 |
 |
 |
 |
 |
 |
| 24. MacLean et al. (1989) |  |
 |
 |
 |
 |
 |
 |
| 25. McKay et al. (1996a) |  |
 |
 |
 |
 |
 |
 |
| 26. McKay et al. (1996b) |  |
 |
 |
 |
 |
 |
 |
| 27. McKay et al. (1998) |  |
 |
 |
 |
 |
 |
 |
| 28. Parrish et al. (1986) |  |
 |
 |
 |
 |
 |
 |
| 29. Planos and Glenwich (1986) |  |
 |
 |
 |
 |
 |
 |
| 30. Richardson et al. (2014) |  |
 |
 |
 |
 |
 |
 |
| 31. Stern et al. (2015) |  |
 |
 |
 |
 |
 |
 |
| 32. Stevens et al. (2009) |  |
 |
 |
 |
 |
 |
 |
| 33. Szapocznik et al. (1988) |  |
 |
 |
 |
 |
 |
 |
| 34. Wiseman and McBride (1998) |  |
 |
 |
 |
 |
 |
 |
a. Random sequence generation; b. Allocation concealment; c. Blinding of participants and personnel; d. Blinding of outcome assessment; e. Incomplete outcome data; f. Selective reporting; g. Other bias;  Low risk of bias;
Low risk of bias;  High risk of bias;
High risk of bias;  Unclear risk of bias.
Unclear risk of bias.
*Reasons for assessment of high risk of bias: Husky et al. (2011): Consent obtained after randomisation; Jorm et al. (2010): Some schools switched into another group and randomisation of schools did not occur after baseline assessment; Lieberman et al. (2006): procedure for outcome assessment was different for intervention and control groups.
Although we did not formally grade the quality of evidence using the GRADE approach (Guyatt et al., 2011), we considered the criteria heterogeneity, risk of bias and precision where appropriate when reporting the effects of interventions below.
Effects of interventions
Figure 3 provides a graphical overview of which outcomes were measured by which studies and whether or not the interventions had a significant effect on the outcome measures. The full report of intervention effects can be found in Table 2, and details on how outcomes were defined in each study can be found in Appendix 6.
| Interventions to engage at-risk individuals in health-care system | ||||||||
|---|---|---|---|---|---|---|---|---|
| Author(s) (year) | Intervention description | Outcomes studied and effect sizes* | ||||||
| Knowledge | Attitudes | Help-seeking | Accessing care | Health outcomes | Satisfaction | |||
| 14 | Asarnow et al. (2005) | 6-month health service quality improvement intervention through support and training for clinicians on treatment for people with mental disorders by expert leader teams and care managers | OR: 2.17 (1.31–3.62) | ES: −0.25 (−0.46–0.03) | ES: 0.32 (0.10–0.53)1 | |||
| 15 | Asarnow et al. (2011) | Brief family-based therapy session to increase motivation during emergency room visit by reframing the problem, educating families about the importance of treatment, obtaining commitment from youth, identifying triggers, and developing and practising a safety plan supplemented by care linkage telephone contacts within the first 48 h after discharge | OR: 3.65 (1.38–9.65) | OR: 0.88 (0.23–3.40) | ||||
| 16 | Coker et al. (2019) | A 5-min video on community mental health clinic and scheduled visit for a telehealth eligibility screening | OR: 0.80 (0.40–1.62) | ES: −0.01 (−0.24–0.23) | ES: 0.40 (0.17–0.64) | |||
| 17 | Donohue et al. (1998) | Telephone call by clinical psychology doctoral students to parents about treatment, intake session for parent and youth, motivational reminder calls, and incentives to participate in treatment | OR: 5.67 (1.02–31.54) | |||||
| 18 | Fristad et al. (2003) | Didactic and interactive multi-family psycho-education group program; parent sessions focused on providing social support, information and skills, while child sessions focused on feeling less alone, understanding symptoms and effects of treatment and building social skills | ES: 1.30 (0.45–2.16) | OR: 18.00 (2.47–131.29) | Not reported | |||
| 19 | Gadomski et al. (2010) | Three hour-long communication skills training sessions for primary care clinicians to engage parents and children in diagnosis and treatment and address barriers to treatment with group discussions and 10-min practice visits | ES: −0.03 (−0.23–0.16) | |||||
| 20 | Grupp-Phelan et al. (2012) | Discussion with a study social worker about screening results, patient concerns and available resources; designed to target various barriers and increase motivation for help-seeking behaviour | OR: 2.33 (0.42–43.20) | OR: 9.62 (1.38–67.25) | ES: 0.73 (−0.10–1.56) | OR: 48.0 (3.70–622.0) | ||
| 21 | Gully et al. (2008) | Educational booklet for parents on expectations and perceived value of treatment reviewed together with nurses | ES: 2.18 (1.49–2.88) | ES: 0.06 (−0.49–0.61) | ES: 1.46 (0.84–2.07) | ES: 0.90 (0.32–1.47) | ||
| 22 | Kourany et al. (1990) | Reminder telephone call, letter describing what would happen on the first clinic visit or both the call and the letter | OR: 3.56 (1.28–9.94) | |||||
| 23 | Lieberman et al. (2006) | Provision of on-site mental health services (usual care was a referral to an off-site mental health provider) | OR: 74.0 (8.94–612.84) | |||||
| 24 | MacLean et al. (1989) | One of four experimental letters (systematic appointment reminders, change slips requesting if appointment time should be changed, warnings and change slips combined with warnings) | OR: 3.64 (1.40–9.48) | |||||
| 25 | McKay et al. (1996a) | Intensive 30-min telephone intervention with a social worker to engage caretaker in help-seeking process by identifying child's problem, framing caretaker actions as having potential to impact the situation and exploring barriers to help-seeking | OR: 3.22 (1.44–7.19) | |||||
| 26 | McKay et al. (1996b) | Telephone intake with therapists trained in specific engagement skills, i.e., informing clients about the process of obtaining mental health services, responding to concrete concerns or crisis situations and exploring potential barriers to obtaining services | OR: 4.16 (1.32–13.12) | |||||
| 27 | McKay et al. (1998) | Thirty-minute telephone and in-person engagement intervention by master's level clinicians to clarify the need for mental health care, increase the caretaker's investment in help-seeking, identify attitudes about and previous experiences with mental health care and over concrete barriers to accessing services | OR: 8.77 (3.41–22.54) | |||||
| 28 | Parrish et al. (1986) | Letter informing parents that children would be moved to the bottom of the waiting list if three appointments were missed or letter informing parents that attending appointments would earn a coupon for winning a prize | OR: 3.36 (1.40–8.03) | |||||
| 29 | Planos and Glenwich (1986) | Appointment reminder (telephone or letter prompt) | OR: 3.06 (1.33–7.05) | |||||
| 30 | Richardson et al. (2014) | A 12-month collaborative care intervention delivered by master's-level clinicians involving initial in-person education engagement session, choice of treatment and regular follow-up | OR: 1.03 (0.42–2.51) | ES: −0.57 (−1.02– −0.12) | OR: 2.1 (0.7–6.1) | |||
| 31 | Stern et al. (2015) | A 10–15 min enhanced engagement phone intake to develop rapport with parents, identify and address likely barriers to treatment, increase parental self-efficacy, hope and treatment motivation | OR: 2.30 (0.97–5.46) | |||||
| 32 | Stevens et al. (2009) | Three phone calls in the first weeks after the first visit to the adolescent management clinic to assess youth's understanding of recommendations, address youth's struggles through case management and use motivational interviewing techniques if youth was ambivalent about treatment | OR: 1.10 (0.51–2.38) | |||||
| 33 | Szapocznik et al. (1988) | Engagement intervention during intake interview to overcome family's resistance to treatment by identifying family patterns that interfere with entry into treatment | OR: 17.73 (5.58–56.34) | ES: −0.62 (−1.01– −0.24) | ||||
| 34 | Wiseman and McBride (1998) | A letter stating that confirmation from parents was required if they still wanted an appointment | OR: 2.30 (0.94–5.61) | |||||
ES, effect size; OR, odds ratio.
Significant/not significant at 95% confidence level.
Table 2.
Summary of findings
| Universal school-based interventions targeting the general population | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Author(s) (year) | Intervention description | Outcomes studied and effect sizes* | |||||||
| Knowledge | Attitudes | Intensions | Help-seeking | Action taken | Accessing care | Health outcomes | |||
| 1 | Aseltine et al. (2007) | Two-part suicide prevention program: (1) curriculum via video with dramatisations, interviews and guidelines including discussion guide over half of the school year; (2) screening on depression and suicidality symptoms | OR: 0.96 (0.82–1.12) | OR: 0.99 (0.78–1.25) | OR: 0.84 (0.69–1.02) | ||||
| 2 | Campos et al. (2018) | Interactive two-session educational curriculum that explored students' knowledge and beliefs about physical and mental health and illness, identified risk factors and symptoms of mental disorders as well as help-seeking options, promoted non-stigmatised behaviours and inadequate beliefs related to mental disorders and addressed self-help strategies and mental health-promoting behaviour | ES: −0.06 (−0.26–0.14) | ||||||
| 3 | Hart et al. (2018) | Three standardised pyschoeducation sessions via program booklet, presentations, videos, role-plays, group and workbook activities and final certificate for peer training to help adolescents with a mental health problem | ES: 0.35 (0.23–0.47) | ES: 0.27 (0.15–0.38) | ES: 0.68 (0.56–0.80) | ||||
| 4 | Howard et al. (2018) | Two brief online educational interventions consisting of one page of a vignette about a person with depression: a biological condition describing the biological causes of depression and a psychosocial condition describing the psychosocial causes of depression | Biological intervention ES: 0.25 (−0.26–0.76) Psychosocial intervention ES: 0.30 (−0.26–0.85) |
||||||
| 5 | Husky et al. (2011) | Brief, two-stage mental health screening via questionnaire and structured interview; referrals to mental health care were provided for those who screened positive | OR: 21.64 (6.66–70.36) | OR: 11.34 (3.41–37.69) | |||||
| 6 | Jorm et al. (2010) | Two day-long teacher training sessions on common mental health disorders, school policy on mental health issues and how to assist students in need | ES: 0.36 (0.14–0.58)a | OR: 2.56 (1.44–4.57)a | OR: 1.27 (0.89–1.79)b | OR: 1.30 (0.82–2.08)a | OR: 1.08 (0.78–1.51) | ||
| 7 | Klingman and Hochdorf (1993) | Twelve weekly sessions delivering an educational curriculum on mental distress and disorders, help-seeking and prevention via theoretical component, role-playing and rehearsing new skills | ES: 0.96 (0.48–1.43) | ||||||
| 8 | Morgan et al. (2019) | A 14-h standardised pyschoeducation and training program for parents of adolescents to learn to recognise early signs of a mental health problem or crisis and to assist adolescents to access appropriate professional help as early as possible | ES: 0.23 (−0.06–0.53)b | ES: −0.15 (−0.48–0.18)b | OR: 4.52 (0.57–35.75) | ES: 0.16 (−0.41–0.73)b | OR: 0.62 (0.16–2.34) | ||
| 9 | Painter et al. (2017) | Three-hour educational curriculum on stigma, mental illness and barriers to help-seeking via presentation, class discussion and video and presentation and discussion with a mentally ill college student | ES: 0.31 (0.09–0.53) | ES: 0.42 (0.20–0.65) | |||||
| 10 | Perry et al. (2014) | 10 h of educational curriculum delivered over 5–8 weeks; resources for teachers delivering intervention included a booklet, slideshow and appendices on mental health, mood disorders and on helping others and oneself | ES: −0.02 (−0.29–0.26) | ES: −0.07 (−0.35–0.20) | |||||
| 11 | Saporito et al. (2011) | A 35-min presentation on mental illness and its treatment plus video on an adolescent with a mental illness | ES: 0.71 (0.39–1.04) | ES: −0.31 (−0.63–0.00) | |||||
| 12 | Sayal et al. (2010) | School-based screening to identify children with high ADHD rating scale scores and a book about ADHD and how to manage and work with affected children | OR: 1.22 (0.61–2.46) | OR: 1.12 (0.60–2.08) | |||||
| 13 | Sharpe et al. (2017) | Booklets on mental health and disorders and help-seeking for students | ES: −0.02 (−0.01–0.05)c | ES: 0.01 (−0.03–0.04)c | |||||
Teacher.
Parent.
Estimate for older age group (12–13 years).
Among the studies on universal school-based interventions targeting the general population, 80% (4/5) of those that assessed knowledge about accessing mental health care, 67% (4/6) of those that assessed attitudes or beliefs about seeking care, 22% (2/9) of those that assessed help-seeking or intentions, 20% (1/5) of those that assessed accessing care or taking action and none (0/7) of those that assessed mental health outcomes had a significant impact on the respective outcome. Thus, universal school-based interventions targeting individuals from the general population tended to have a significant impact on steps earlier on the pathway to accessing care, especially knowledge and attitudes, but not on later steps, such as actually accessing care or mental health outcomes. The risk of bias for studies on these interventions ranged from low to high (see Table 1). The effect sizes ranged from −0.06 to 0.96 for knowledge about seeking health care, −0.02 to 2.56 for attitudes about seeking health care and −0.15 to 0.30 for intensions to seek health care or help others seek health care. Both odds ratios and effect sizes were calculated for the outcomes help-seeking, action taken and health outcomes. The odds ratios ranged from 0.96 to 21.64 for help-seeking, 0.99 to 11.34 for accessing care and 0.62 to 1.12 for health outcomes.
The pattern of significant outcomes found for universal interventions differed from that observed for interventions targeting at-risk individuals who had already been identified by the health-care system. Among studies on these interventions, all assessed accessing care (e.g., the proportion of study subjects who attended the first appointment or number of appointments attended) as an outcome, and 71% (15/21) of these interventions had a significant impact on that outcome. Eighty per cent (8/10) of studies on treatment engagement interventions (e.g., a family-based session to increase motivation during an emergency room or motivational telephone calls with trained staff) and 80% (4/5) of studies on appointment reminder interventions had a significant effect on accessing care. Just three interventions targeting at-risk individuals assessed outcomes that preceded accessing care. The effects on knowledge about accessing mental health care, attitudes or beliefs about seeking care and help-seeking were thus unclear due to the limited number of studies measuring these outcomes. Of the seven interventions that assessed the remaining two outcomes along the pathway to accessing care, 33% (2/6) of those that assessed mental health outcomes and 80% (4/5) of those that assessed satisfaction with care were significantly better as compared with controls on the respective outcome. Interventions targeting at-risk children who had already been identified by the health-care system therefore generally yielded more access to care and satisfaction with care as compared with controls, but not necessarily improved mental health outcomes. The risk of bias found for appointment reminder and treatment engagement interventions ranged from low to high (see Table 1). The most important outcome comparisons for these types of interventions are summarised in the meta-analyses below.
Meta-analyses
We conducted meta-analyses for two types of interventions that measured the same outcome (accessing care) using the binary measure first appointment attendance (yes/no): (1) appointment reminder interventions (five studies) and (2) treatment engagement interventions (10 studies). For the appointment reminder interventions, we only calculated a fixed-effects model since heterogeneity was low (I2 = 0%). For the treatment engagement interventions, heterogeneity was substantial (I2 = 70%), so we calculated fixed effects and random-effects models. Forest plots for each of these two types of interventions can be found in Fig. 4. The combined odds ratio of the appointment reminder interventions was 3.11 (2.07–4.67), and the combined odds ratio calculated using the random-effects model for the treatment engagement interventions was 3.51 (2.02–6.11). In other words, the odds of attending an initial appointment were 3.11 times higher for those who received an appointment reminder as compared with controls and 3.51 higher for those who participated in a treatment engagement intervention as compared with controls, indicating that overall, both types of interventions yielded significantly higher first appointment attendance in the target population as compared with controls.
Fig. 4.
Forest plots of appointment reminder and treatment engagement interventions measuring first appointment attendance.
Discussion
Summary of main results
This systematic review identified 34 RCTs of interventions that fell into two main categories: universal school-based interventions targeting the general population and interventions to engage at-risk individuals who had already been identified by the health-care system. Interventions in the first category generally yielded significantly better knowledge and attitudes about accessing care as compared with controls, but did not have an impact on actually accessing care or on mental health outcomes. Most interventions targeting at-risk children who had already been identified by the health-care system yielded significantly better access to care and satisfaction with care as compared with controls, but did not seem to have a significant impact on mental health outcomes. Meta-analyses of appointment reminder interventions and treatment engagement interventions measuring the outcome accessing care using the binary measure first appointment attendance found that both types of interventions yielded significantly more access to care as compared with controls. We did not identify studies that targeted the domains of acceptability and affordability or individuals' ability to reach or pay for care.
Comparison with other reviews
In our study, we used Levesque et al.'s conceptual framework of access to health care to design a systematic review of RCTs of interventions to improve access to mental health care for children (Levesque et al., 2013). This approach enabled us to provide a broad overview of RCTs of interventions that was not limited to particular types of interventions or disorders by structuring our findings along the entire pathway to accessing care. Our results on the effects of universal interventions targeting individuals from the general population were similar to those from a previous systematic review on help-seeking interventions for depression, anxiety and general psychological distress in adults that found that mental health literacy content significantly improved help-seeking attitudes, but did not have an effect on help-seeking behaviour (Gulliver et al., 2012). Another systematic review on interventions to promote help-seeking for mental health problems found that interventions increased formal help-seeking behaviours when targeting affected or at-risk people with mental disorders, but not the general population (Xu et al., 2018). This is the same pattern that we found for the outcome of accessing care.
Strengths and limitations
This systematic review provided an overview of interventions to improve access to mental health care along the entire pathway to accessing care using a conceptual framework, which allowed us to assess where evidence for effective interventions lies and where evidence is missing. However, taking a broad approach to the search necessitated restricting the search to the title field and English language only. We attempted to address this by hand searching reference lists and key articles. In addition, we did not include retention in treatment as an outcome in this review since we were interested in gaining access to treatment.
Implications for practice and research
Both the results of this systematic review and previous research have shown that interventions can improve knowledge and attitudes about mental disorders and their treatment (Lo et al., 2017); however, there is evidence that such interventions do not necessarily have an impact on health behaviours, such as help-seeking (Kelly and Barker, 2016; Laverack, 2017). Interventions to engage and motivate an at-risk population, on the other hand, have been shown to significantly change health behaviours (Ingoldsby, 2010). From a public health perspective, the problem with this finding is that existing interventions do not improve access to care for people in need from the general population, leaving a large treatment gap.
In order to have a population-level effect on improving access to care, it may be necessary to introduce two-stage interventions, i.e., ones that first identify those in need from the general population and then engage them in the health-care system. In this systematic review, the only study in that targeted the general population, yet had a significant impact on accessing care was Husky et al. (2011), which tested systematic referral to mental health services using a brief mental health screening in a school setting (Husky et al., 2011). Additionally, five of the six studies targeting at-risk children that took place in a primary care setting used a screening procedure to identify these at-risk children; however, only two of these five studies had a significant effect on access to care as compared with controls. Since the evidence to recommend screening the general population of children for mental disorders is currently insufficient (Lenzer, 2017), it is imperative to rigorously test screening procedures using RCTs giving careful consideration to the benefits and harms that would result from such screenings (Wissow et al., 2013).
There is growing evidence that changing environmental factors, including policies, infrastructure and health-care financing (Hodgkinson et al., 2017; So et al., 2019), can have a larger impact on health behaviours such as help-seeking than health literacy education (Kelly and Barker, 2016). Integrating mental health services into existing service settings is considered a promising means of improving access to care (Anderson et al., 2017; Hodgkinson et al., 2017; Richardson et al., 2017); however, we identified just one infrastructural intervention that involved providing onsite mental health services for primary care patients (Lieberman et al., 2006). In light of this and the fact that our systematic review revealed gaps in the research on interventions to improve acceptability, affordability and individuals' ability to reach and pay, it seems that more research on interventions that address contextual factors such as these is warranted, although it may be difficult to test some of these interventions via RCT. In addition, targeting individual barriers in isolation, such as cost or insurance coverage, without addressing other barriers like accessibility, acceptability and availability may not improve service utilisation (So et al., 2019). It is possible that interventions that address multiple barriers simultaneously are more likely to have a population-level effect on improving children's access to mental health care, but this must be tested in future research.
Future studies on interventions to improve access to mental health care for young people should attempt to coordinate and standardise the outcomes assessed so that more quantitative comparison among studies via meta-analysis is possible. We especially need more studies testing the effects on mental health care outcomes since this is the ultimate purpose of improving access to care. In addition, longer follow-up periods are required to gain information about the longer-term effects of interventions to improve access to care (Salerno, 2016; Anderson et al., 2017). Finally, none of the studies identified in this systematic review took place in low- or middle-income countries. Due to a shortage of mental health professionals, the fact that detection rates of mental disorders are much lower in many of these countries, less developed infrastructure and potentially more stigma surrounding mental health disorders, different interventions than those that are effective in high-income countries may be required (Patel et al., 2013). More research is therefore needed to draw conclusions about improving access to care in these settings.
Conclusion
In order to bridge the existing treatment gap in mental health care for children, interventions that aim to improve knowledge and attitudes about mental health care in the general population are not sufficient. Instead, a two-stage approach that first identifies young people in need of care from the general population and then engages them in the health-care system should be tested in high quality studies. In addition, we need high quality research on the impact of interventions addressing contextual factors such as affordability and individuals' ability to reach care.
Acknowledgements
Thank you to Sabine Klein for her help in designing and executing the systematic search, to Diego Morosoli for obtaining every difficult-to-locate article, to Julia Braun and Sarah Haile for their statistical support, and to Anja Frei for her input on the figures.
Appendix 1
A conceptual framework of access to health care (Levesque et al., 2013)
Appendix 2
PRISMA checklist (Moher et al., 2009)
| Section/topic | # | Checklist item | Reported on page # |
|---|---|---|---|
| Title | |||
| Title | 1 | Identify the report as a systematic review, meta-analysis or both. | 1 |
| Abstract | |||
| Structured summary | 2 | Provide a structured summary including as applicable: background; objectives; data sources; study eligibility criteria, participants and interventions; study appraisal and synthesis methods; results; limitations; conclusions and implications of key findings; systematic review registration number. | 1 |
| Introduction | |||
| Rationale | 3 | Describe the rationale for the review in the context of what is already known. | 1–2 |
| Objectives | 4 | Provide an explicit statement of questions being addressed with reference to participants, interventions, comparisons, outcomes and study design (PICOS). | 2 |
| Methods | |||
| Protocol and registration | 5 | Indicate if a review protocol exists, if and where it can be accessed (e.g., Web address) and, if available, provide registration information including registration number. | 2 |
| Eligibility criteria | 6 | Specify study characteristics (e.g., PICOS, length of follow-up) and report characteristics (e.g., years considered, language, publication status) used as criteria for eligibility, giving rationale. | 2 |
| Information sources | 7 | Describe all information sources (e.g., databases with dates of coverage, contact with study authors to identify additional studies) in the search and date last searched. | 2 |
| Search | 8 | Present full electronic search strategy for at least one database, including any limits used, such that it could be repeated. | Appendix 3 |
| Study selection | 9 | State the process for selecting studies (i.e., screening, eligibility, included in systematic review and, if applicable, included in the meta-analysis). | 2–3 |
| Data collection process | 10 | Describe the method of data extraction from reports (e.g., piloted forms, independently, in duplicate) and any processes for obtaining and confirming data from investigators. | 2–3 |
| Data items | 11 | List and define all variables for which data were sought (e.g., PICOS, funding sources) and any assumptions and simplifications made. | 2 |
| Risk of bias in individual studies | 12 | Describe methods used for assessing risk of bias of individual studies (including specification of whether this was done at the study or outcome level), and how this information is to be used in any data synthesis. | 3, 5 |
| Summary measures | 13 | State the principal summary measures (e.g., risk ratio, difference in means). | 3–4 |
| Synthesis of results | 14 | Describe the methods of handling data and combining results of studies, if done, including measures of consistency (e.g., I2) for each meta-analysis. | 3–4 |
| Risk of bias across studies | 15 | Specify any assessment of risk of bias that may affect the cumulative evidence (e.g., publication bias, selective reporting within studies). | N/A |
| Additional analyses | 16 | Describe methods of additional analyses (e.g., sensitivity or subgroup analyses, meta-regression), if done, indicating which were pre-specified. | 3–4 |
| Results | |||
| Study selection | 17 | Give numbers of studies screened, assessed for eligibility and included in the review, with reasons for exclusions at each stage, ideally with a flow diagram. | 4–5, Fig. 1 |
| Study characteristics | 18 | For each study, present characteristics for which data were extracted (e.g., study size, PICOS, follow-up period) and provide the citations. | 4–5, Table 2, Appendix 5 |
| Risk of bias within studies | 19 | Present data on risk of bias of each study and, if available, any outcome level assessment (see item 12). | 5, Table 1 |
| Results of individual studies | 20 | For all outcomes considered (benefits or harms), present, for each study: (a) simple summary data for each intervention group (b) effect estimates and confidence intervals, ideally with a forest plot. | Table 2, Fig. 4 |
| Synthesis of results | 21 | Present results of each meta-analysis done, including confidence intervals and measures of consistency. | 7 |
| Risk of bias across studies | 22 | Present results of any assessment of risk of bias across studies (see Item 15). | N/A |
| Additional analysis | 23 | Give results of additional analyses, if done (e.g., sensitivity or subgroup analyses, meta-regression [see Item 16]). | Figures 2 and 3 |
| Discussion | |||
| Summary of evidence | 24 | Summarise the main findings including the strength of evidence for each main outcome; consider their relevance to key groups (e.g., healthcare providers, users and policymakers). | 7–12 |
| Limitations | 25 | Discuss limitations at study and outcome level (e.g., risk of bias), and at review-level (e.g., incomplete retrieval of identified research, reporting bias). | 8 |
| Conclusions | 26 | Provide a general interpretation of the results in the context of other evidence and implications for future research. | 7–12 |
| Funding | |||
| Funding | 27 | Describe sources of funding for the systematic review and other support (e.g., supply of data); role of funders for the systematic review. | N/A |
Appendix 3
Search strategy
| Search in EMBASE Date of search: 15 May 2019 | ||
|---|---|---|
| No. | Query | Results |
| # 1 | ‘mental disease'/exp OR 'mental health’/exp OR (((mental OR mentally OR psychiatric OR psychological OR psychosocial OR behavioural OR behavioural OR emotional) NEAR/3 (health OR disease OR diseases OR disorder OR disorders OR ill OR illness OR illnesses OR insanity OR insanities OR abnormality OR abnormalities OR disturbance OR disturbances OR confusion OR confusions OR symptom OR symptoms OR health OR problem OR problems)):ti) OR depression:ti OR depressive:ti | 2269428 |
| # 2 | ‘adolescent’/exp OR ‘child’/exp OR child:ti OR children:ti OR adolescent:ti OR adolescents:ti OR juvenile:ti OR juveniles:ti OR young:ti OR youth:ti OR pediatric*:ti OR paediatric*:ti OR teen*:ti OR ‘young people’:ti OR ‘young person*’:ti OR minor*:ti | 3820655 |
| # 3 | ‘help seeking behavior’/exp OR (((help OR treatment OR treatments) NEAR/5 (seek* OR behavior OR behaviour)):ti) OR helpseeking:ti OR ‘mental health literacy’:ti OR (((screening* OR intervention* OR communica* OR utili?ation OR access OR attitude*) NEAR/5 (mental OR psych*)):ti) | 31782 |
| # 4 | #1 AND #2 AND #3 | 4583 |
| # 5 | #1 AND #2 AND #3 NOT ([animals]/lim NOT [humans]/lim) AND [english]/lim NOT [conference abstract]/lim | 3676 |
Note: This search strategy was adapted to search MEDLINE, PsycINFO and the Cochrane Central Register of Controlled Trials (CENTRAL)
Appendix 4
List of studies excluded from the review by primary reason for exclusion
Reason 1. Not an RCT (n = 16)
Battaglia J, Coverdale JH and Bushong CP (1990) Evaluation of a Mental Illness Awareness Week program in public schools. American Journal of Psychiatry 147, 324.
Contreras S, Porras-Javier L, Zima BT, Soares N, Park C, Patel A, Chung PJ and Coker TR (2018) Development of a telehealth-coordinated intervention to improve access to community-based mental health. Ethnicity & Disease 28(Supp), 457–466.
Cynthia Logsdon M, Myers J, Rushton J, Gregg JL, Josephson AM, Davis DW, Brothers K, Baisch K, Carabello A, Vogt K, Jones K and Angermeier J (2018) Efficacy of an Internet-based depression intervention to improve rates of treatment in adolescent mothers. Archives of Women's Mental Health 21, 273–285.
Elliott DJ, Koroloff NM, Koren PE and Friesen BJ (1998) Improving access to children's mental health services: the Family Associate approach. In Epstein MH et al. (eds), Outcomes for Children and Youth with Emotional and Behavioral Disorders and their Families: Programs and Evaluation Best Practices. pp. 581–609.
Esters IG, Cooker PG and Ittenbach RF (1998) Effects of a unit of instruction in mental health on rural adolescents' conceptions of mental illness and attitudes about seeking help. Adolescence 33, 469–476.
Grimes KE, Creedon TB, Webster CR, Coffey SM, Hagan GN and Chow CM (2018) Enhanced child psychiatry access and engagement via integrated care: A collaborative practice model with pediatrics. Psychiatric Services 69, 986–992.
Jonovich SJ and Alpert-Gillis LJ (2014) Impact of pediatric mental health screening on clinical discussion and referral for services. Clinical Pediatrics 53, 364–371.
Lubman DI, Cheetham A, Berridge BJ and McKay-Brown L (2018) MAKINGtheLINK: A school-based intervention to improve help-seeking for substance use problems. Early Intervention in Psychiatry 12, 915–921.
McKay MM, Hibbert R, Hoagwood K, Rodriguez J, Murray L, Legerski J and Fernandez D (2004) Integrating evidence-based engagement interventions into ‘real world' child mental health settings. Brief Treatment and Crisis Intervention 4, 177–186.
-
10.
Rotheram-Borus MJ, Piacentini J, Van Rossem R, Graae F, Cantwell C, Castro-Blanco D, Miller S and Feldman J (1996) Enhancing treatment adherence with a specialized emergency room program for adolescent suicide attempters. Journal of the American Academy of Child and Adolescent Psychiatry 35, 654–663.
Ruble AE, Leon PJ, Gilley-Hensley L, Hess SG and Swartz KL (2013) Depression knowledge in high school students: Effectiveness of the adolescent depression awareness program. Journal of Affective Disorders 150, 1025–1030.
Shaffer D, Garland ANN, Vieland V, Underwood M and Busner C (1991) The impact of curriculum-based suicide prevention programs for teenagers. Journal of the American Academy of Child & Adolescent Psychiatry 30, 588–596.
Smalec JL and Klingle RS (2000) Bulimia interventions via interpersonal influence: The role of threat and efficacy in persuading bulimics to seek help. Journal of Behavioral Medicine 23, 37–57.
Spirito A, Overholser J, Ashworth S, Morgan J and Benedict-Drew C (1988) Evaluation of a suicide awareness curriculum for high school students. Journal of the American Academy of Child & Adolescent Psychiatry 27, 705–711.
Swartz KL, Kastelic EA, Hess SG, Cox TS, Gonzales LC, Mink SP and Raymond DePaulo J (2010) The effectiveness of a school-based adolescent depression education program. Health Education & Behavior 37, 11–22.
Ventieri D, Clarke DM and Hay M (2011) The effects of a school-based educational intervention on pre-adolescents' knowledge of and attitudes towards mental illness. Advances in School Mental Health Promotion 4, 5–17.
Reason 2. Trial not yet completed (n = 4)
Bauer S, Bilić S, Reetz C, Ozer F, Becker K, Eschenbeck H, Kaess M, Rummel-Kluge C, Salize HJ, Diestelkamp S and Moessner M (2019) Efficacy and cost-effectiveness of Internet-based selective eating disorder prevention: study protocol for a randomized controlled trial within the ProHEAD Consortium. Trials 20.
Calear AL, Banfield M, Batterham PJ, Morse AR, Forbes O, Carron-Arthur B and Fisk M (2017) Silence is deadly: a cluster-randomised controlled trial of a mental health help-seeking intervention for young men. BMC Public Health 17, 834.
Darraj H, Mahfouz MS, Al Sanosi R, Badedi M and Sabai A (2018) The effects of an educational program on depression literacy and stigma among students of secondary schools in Jazan city, 2016. Medicine 97, e9433.
Kilbourne AM, Smith SN, Choi SY, Koschmann E, Liebrecht C, Rusch A, Abelson JL, Eisenberg D, Himle JA, Fitzgerald K and Almirall D (2018) Adaptive School-based Implementation of CBT (ASIC): clustered-SMART for building an optimized adaptive implementation intervention to improve uptake of mental health interventions in schools. Implementation Science 13, 119.
Reason 3. Did not target population of interest (n = 2)
Weinstein M (1988) Preparation of children for psychotherapy through videotaped modeling. Journal of Clinical Child Psychology 17, 131–136.
Winkler P, Janoušková M, Kožený J, Pasz J, Mladá K, Weissová A, Tušková E and Evans-Lacko S (2017) Short video interventions to reduce mental health stigma: a multi-centre randomised controlled trial in nursing high schools. Social Psychiatry and Psychiatric Epidemiology 52, 1549–1557.
Reason 4. Did not include outcome of interest (n = 10)*
Baer JS, Garrett SB, Beadnell B, Wells EA and Peterson PL (2007) Brief motivational intervention with homeless adolescents: evaluating effects on substance use and service utilization. Psychology of Addictive Behaviors 21, 582–586.
Burns BJ, Farmer EMZ, Angold A, Costello EJ and Behar L (1996) A randomized trial of case management for youths with serious emotional disturbance. Journal of Clincial Child Psychology 25, 376–387.
Fristad MA (2006) Psychoeducational treatment for school-aged children with bipolar disorder. Development and Psychopathology 18.
Nock MK and Kazdin AE (2005) Randomized controlled trial of a brief intervention for increasing participation in parent management training. Journal of Consulting and Clinical Psychology 73, 872–879.
Pinto-Foltz MD, Logsdon MC and Myers JA (2011) Feasibility, acceptability, and initial efficacy of a knowledge-contact program to reduce mental illness stigma and improve mental health literacy in adolescents. Social Science and Medicine 72, 2011–2019.
Rahman A, Mubbashar MH, Gater R and Goldberg D (1998) Randomised trial of impact of school mental-health programme in rural Rawalpindi, Pakistan. Lancet 352, 1022–1025.
Sakellari E, Sourander A, Kalokerinou-Anagnostopoulou A and Leino-Kilpi H (2016) Opinions about mental illness among adolescents: the impact of a mental health educational intervention. School Mental Health 8, 268–277.
Vila-Badia R, Martínez-Zambrano F, Arenas O, Casas-Anguera E, García-Morales E, Villellas R, Martín JR, Pérez-Franco MB, Valduciel T, Casellas D, García-Franco M, Miguel J, Balsera J, Pascual G, Julia E and Ochoa S (2016) Effectiveness of an intervention for reducing social stigma towards mental illness in adolescents. World Journal of Psychiatry 6, 239–247.
Wagner V, Sy J, Weeden K, Blanchard T, Cauce AM, Morgan CJ, Moore E, Wurzbacher K and Tomlin S (1994) Effectiveness of intensive case management for homeless adolescents: results of a 3-month follow-up. Journal of Emotional and Behavioral Disorders 2, 219–227.
-
10.
Wissow LS, Gadomski A, Roter D, Larson S, Brown J, Zachary C, Bartlett E, Horn I, Luo X and Wang M-C (2008) Improving child and parent mental health in primary care: a cluster-randomized trial of communication skills training. Pediatrics 121, 266–275.
Reason 5. Control group not appropriate (n = 1)
Chisholm K, Patterson P, Torgerson C, Turner E, Jenkinson D and Birchwood M (2016) Impact of contact on adolescents' mental health literacy and stigma: the SchoolSpace cluster randomised controlled trial. BMJ Open 6, e009435.
Reason 6. Not possible to calculate effect size (n = 4)
Beaudry MB, Swartz K, Miller L, Schweizer B, Glazer K and Wilcox H (2019) Effectiveness of the Adolescent Depression Awareness Program (ADAP) on depression literacy and mental health treatment. Journal of School Health 89, 165–172.
Poland AL (2010) Got Training? The Effect of Mental Health Training on the Attitudes and Behaviors of Direct Care Workers in a Residential Facility for Juvenile Offenders. Ipswich, MA: ProQuest Information & Learning.
Warzak WJ, Parrish JM and Handen BL (1987) Effects of telephone intake procedures on initial appointment keeping in a child behavior management clinic. Journal of Compliance in Health Care 2, 143–154.
Watt BD, Hoyland M, Best D and Dadds MR (2007) Treatment participation among children with conduct problems and the role of telephone reminders. Journal of Child and Family Studies 16, 522–530.
*For a study with outcomes on health measures and satisfaction with care to be included in the analysis, the study also had to include a measure about improved access to care.
Appendix 5
Characteristics of included studies by intervention type
| Universal school-based interventions targeting the general population | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| No. | First author, year/country | N enrolled/analysed | Age | Setting | Targeted population | Target condition | Intervention description | Intervention duration | Assessment time point(s) | Outcomes studied |
| 1 | Aseltine, 2007/USA | 4491/3837–3899 | 14–18 | School | Students | Suicide | Two-part suicide prevention program: (1) curriculum via video with dramatisations, interviews and guidelines including discussion guide over half of the school year; (2) screening on depression and suicidality symptoms | 2 days | 3 months |
|
| 2 | Campos, 2018/Portugal | 543/387 | 12–14 | School | Students | General mental health problems | Interactive two-session educational curriculum that explored students' knowledge and beliefs about physical and mental health and illness, identified risk factors and symptoms of mental disorders as well as help-seeking options, promoted non-stigmatised behaviours and inadequate beliefs related to mental disorders and addressed self-help strategies and mental health-promoting behaviour | Two 90-min sessions (1 week apart) |
|
|
| 3 | Hart, 2018/Australia | 1942/1116 | 15–18 | School | Student peers, parents and teachers | General mental health problems | Three standardised pyschoeducation sessions via program booklet, presentations, videos, role-plays, group and workbook activities and final certificate for peer training to help adolescents with a mental health problem | 3 weeks | 1 week |
|
| 4 | Howard, 2018/Australia | 350/327 | 16–19 | School | Students | Depression | Two brief online educational interventions consisting of one page of a vignette about a person with depression: a biological condition describing the biological causes of depression and a psychosocial condition describing the psychosocial causes of depression | Single time point | Directly post-intervention |
|
| 5 | Husky, 2011/USA | 890/656 | 14–15 | School | Students | General mental health problems | Brief, two-stage mental health screening via questionnaire and structured interview; referrals to mental health care were provided for those who screened positive | Single time point | 3–5 months |
|
| 6 | Jorm, 2010/Australia | 423/327 | 12–15 | School | Teachers | General mental health problems | Two day-long teacher training sessions on common mental health disorders, school policy on mental health issues and how to assist students in need | Two days |
|
|
| 7 | Klingman, 1993/Israel | 237/76 | 12–13 | School | Student peers | Mental distress and suicide | Twelve weekly sessions delivering an educational curriculum on mental distress and disorders, help-seeking and prevention via theoretical component, role-playing and rehearsing new skills | 12 weeks | 2 weeks |
|
| 8 | Morgan, 2019/Australia | 384/322 | 12–15 | School | Parents of adolescents | General mental health problems | A 14-h standardised pyschoeducation and training program for parents of adolescents to learn to recognise early signs of a mental health problem or crisis and to assist adolescents to access appropriate professional help as early as possible | Two sessions over four months |
|
|
| 9 | Painter, 2017/USA | 751/721 | 10–13 | School | Students | General mental health problems | Three-hour educational curriculum on stigma, mental illness and barriers to help-seeking via presentation, class discussion and video and presentation and discussion with a mentally ill college student | ⩽1 week | 1 week |
|
| 10 | Perry, 2014/Australia | 380/208 | 13–16 | School | Students | General mental health problems | Ten hour of educational curriculum delivered over 5–8 weeks; resources for teachers delivering intervention included a booklet, slideshow and appendices on mental health, mood disorders and on helping others and oneself | 5–8 weeks |
|
|
| 11 | Saporito, 2011/USA | 159/156 | 15–19 | School | Students | General mental health problems | A35-min presentation on mental illness and its treatment plus video on an adolescent with a mental illness | Single time point | Directly post-intervention |
|
| 12 | Sayal, 2010/UK | 1662/487 | 4–5 | School | Students and teachers | Attention-deficit hyperactivity disorder | School-based screening to identify children with high ADHD rating scale scores and a book about ADHD and how to manage and work with affected children | Single time point | 5 years |
|
| 13 | Sharpe, 2017/UK | 27▫885/ 14▫690 | 10–13 | School | Students | General mental health problems | Booklets on mental health and disorders and help-seeking for students | Single time point | 12 months |
|
| Interventions to engage at-risk individuals within health-care system | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| No. | First author, year/country | N enrolled/analysed | Age | Setting | Targeted population | Target condition | Intervention description | Intervention duration | Assessment time point(s) | Outcomes studied |
| 14 | Asarnow, 2005/USA | 418/344 | 13–21 | Primary care | Patients with depressive symptoms and their parents (when appropriate) | Depression | 6-month health service quality improvement intervention through support and training for clinicians on treatment for people with mental disorders by expert leader teams and care managers | 6 months | 6 months |
|
| 15 | Asarnow, 2011/USA | 181/160 | 10–18 | Emergency department | Suicidal youths and their families | Suicide | Brief family-based therapy session to increase motivation during emergency room visit by reframing the problem, educating families about the importance of treatment, obtaining commitment from youth, identifying triggers and developing and practising a safety plan supplemented by care linkage telephone contacts within the first 48 h after discharge | Single time point with follow-up phone calls after 48 h and additional contacts as needed (usually 1, 2 and 4 weeks post-discharge) | 2 months |
|
| 16 | Coker, 2019/USA | 342/342 | 5–12 | Primary care | Parents of children referred to community mental health clinics | General mental health problems | A 5-min video on community mental health clinic and scheduled visit for a telehealth eligibility screening | Single time point | 6 months |
|
| 17 | Donohue, 1998/USA | 39/39 | Not stated (ca. 12–18) | Outpatient cognitive-behavioural treatment program specialising in adolescent substance dependence and conduct disorder | Adolescents referred as prospective clients and their parents | Conduct disorder and substance abuse | Telephone call by clinical psychology doctoral students to parents about treatment, intake session for parent and youth, motivational reminder calls and incentives to participate in treatment | Single time point | Directly post-intervention |
|
| 18 | Fristad, 2003/USA | 52/42 | 8–11 | Clinical research group | Children with mood disorders and their parents | Mood disorders | Didactic and interactive multi-family psycho-education group program; parent sessions focused on providing social support, information and skills, while child sessions focused on feeling less alone, understanding symptoms and effects of treatment and building social skills | 6 sessions over 6 weeks |
|
|
| 19 | Gadomski, 2010/USA | 397/397 | 5–16 | Primary care | Primary care providers who treat children with possible or probable mental health problems | General mental health problems | Three hour-long communication skills training sessions for primary care clinicians to engage parents and children in diagnosis and treatment and address barriers to treatment with group discussions and 10-min practice visits | Single time point |
|
|
| 20 | Grupp-Phelan, 2012/USA | 24/24 | 12–17 | Emergency department | Patients with suicide-related risk factors | Suicide | Discussion with a study social worker about screening results, patient concerns and available resources; designed to target various barriers and increase motivation for help-seeking behaviour | Single time point | 2 months |
|
| 21 | Gully, 2008/USA | 87/51 | 2–17 | Child advocacy centres and outpatient program at hospital | Parents of children who are suspected victims of abuse | General mental health problems | Educational booklet for parents on expectations and perceived value of treatment reviewed together with nurses | Single time point | 1 month |
|
| 22 | Kourany, 1989/USA | 111/111 | 2–17 | Outpatient child psychiatry clinic | Parents of prospective clients | General mental health problems | Reminder telephone call, letter describing what would happen on the first clinic visit, or both the call and the letter | Single time point | Directly post-intervention |
|
| 23 | Lieberman, 2006/USA | 71/71 | 13–22 | Primary care | Adolescents with psychosocial issues | General mental health problems | Provision of on-site mental health services (usual care was a referral to an off-site mental health provider) | Single time point | 3 months |
|
| 24 | MacLean, 1989/Canada | 327/327 | <12 | Child community mental health centre | Parents of prospective clients | Non-emergency general mental health problems | One of four experimental letters (systematic appointment reminders, change slips requesting if appointment time should be changed, warnings and change slips combined with warnings) | Single time point | Directly post-intervention |
|
| 25 | McKay, 1996a/USA | 108/108 | Not stated | Child mental health agency | Caretakers requesting mental health services | General mental health problems | Intensive 30-min telephone intervention with a social worker to engage caretaker in help-seeking process by identifying child's problem, framing caretaker actions as having potential to impact the situation, and exploring barriers to help-seeking | Single time point | Directly post-intervention |
|
| 26 | McKay, 1996b/USA | 107/107 | Not stated | Urban child mental health agency | Parents of prospective clients | Non-emergency general mental health problems | Telephone intake with therapists trained in specific engagement skills, i.e., informing clients about the process of obtaining mental health services, responding to concrete concerns or crisis situations and exploring potential barriers to obtaining services | Single time point | Directly post-intervention |
|
| 27 | McKay, 1998/USA | 109/109 | 1–14 | Child mental health agency | Caregivers of urban children who requested services at the mental health agency | General mental health problems | Thirty-minute telephone and in-person engagement intervention by master's level clinicians to clarify the need for mental health care, increase the caretaker's investment in help-seeking, identify attitudes about and previous experiences with mental health care, and over concrete barriers to accessing services | Single time point | 18 weeks |
|
| 28 | Parrish, 1986/USA | 99/99 | 2–20 | Outpatient behavioural paediatrics clinic | Parents of children referred as prospective clients | Behavioural health problems | Letter informing parents that children would be moved to the bottom of the waiting list if three appointments were missed or letter informing parents that attending appointments would earn a coupon for winning a prize | Single time point | Directly post-intervention |
|
| 29 | Planos, 1986/USA | 274/274 | <18 | Children's mental health centre | Parents of children referred as prospective clients | General mental health problems | Appointment reminder (telephone or letter prompt) | Single time point | 1 month |
|
| 30 | Richardson, 2014/USA | 101/101 | 13–17 | Primary care | Adolescents who screened positive for depression and their parents | Depression | A 12-month collaborative care intervention delivered by master's-level clinicians involving initial in-person education engagement session, choice of treatment and regular follow-up | 12 months | 12 months |
|
| 31 | Stern, 2015/Canada | 117/99 | 5–12 | Children's mental health centre | Parents of children with mental health problems | General mental health problems | A 10–15 min enhanced engagement phone intake to develop rapport with parents, identify and address likely barriers to treatment, increase parental self-efficacy, hope and treatment motivation | Single time point | Not standardised – several weeks to months |
|
| 32 | Stevens, 2009/USA | 179/179 | 11–20 | Primary care | Adolescents who screened positive for at least one of depressive symptoms, suicidal ideation or substance abuse | Depression, suicide and substance abuse | Three phone calls in the first weeks after the first visit to the adolescent management clinic to assess youth's understanding of recommendations, address youth's struggles through case management and use motivational interviewing techniques if youth was ambivalent about treatment | Several weeks to months | 6 months |
|
| 33 | Szapocznik, 1988/USA | 108/108 | 12–21 | Mental health centre | Adolescent drug abusers and their families | Substance abuse | Engagement intervention during intake interview to overcome family's resistance to treatment by identifying family patterns that interfere with entry into treatment | As many contacts as necessary within 3-week period | 3 weeks |
|
| 34 | Wiseman, 1998/UK | 128/128 | Not stated | Child mental health clinic | Parents of prospective clients | Non-emergency general mental health problems | Didactic and interactive multi-family psycho-education group program; parent sessions focused on providing social support, information, skills, while children sessions focused on feeling less alone, understanding symptoms and effects of treatment, and building social skills | Single time point | Directly post-intervention |
|
Appendix 6
How outcomes were measured in each study
| Universal school-based interventions targeting the general population | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| First author (year) | Intervention description | Outcomes studied | |||||||
| Knowledge | Attitudes | Intensions | Help-seeking | Action taken | Accessing care | Health outcomes | |||
| 1 | Aseltine (2007) | Two-part suicide prevention program: (1) curriculum via video with dramatisations, interviews and guidelines including discussion guide over half of the school year; (2) screening on depression and suicidality symptoms | Talking to an adult due to feeling depressed or suicidal | Receiving specialist care | Suicidal ideation (suicide attempts also measured as an outcome) | ||||
| 2 | Campos (2018) | Interactive two-session educational curriculum that explored students' knowledge and beliefs about physical and mental health and illness, identified risk factors and symptoms of mental disorders as well as help-seeking options, promoted non-stigmatised behaviours and inadequate beliefs related to mental disorders and addressed self-help strategies and mental health-promoting behaviour | Knowledge about first aid skills and help-seeking | ||||||
| 3 | Hart (2018) | Three standardised pyschoeducation sessions via program booklet, presentations, videos, role-plays, group and workbook activities, and final certificate for peer training to help adolescents with a mental health problem | Knowledge about when to recommend that another person seek help | Confidence in supporting a peer | Endorsing intentions to help a peer to seek help | ||||
| 4 | Howard (2018) | Two brief online educational interventions consisting of one page of a vignette about a person with depression: a biological condition describing the biological causes of depression and a psychosocial condition describing the psychosocial causes of depression | Help-seeking intentions | ||||||
| 5 | Husky (2011) | Brief, two-stage mental health screening via questionnaire and structured interview; referrals to mental health care were provided for those who screened positive | Any student assistance contact | Any access to community-based services (any access to school-based services also measured) | |||||
| 6 | Jorm (2010) | Two day-long teacher training sessions on common mental health disorders, school policy on mental health issues and how to assist students in need | Beliefs about treatment for depressiona | Confidence to talk with students about mental health problemsa | Help-seeking intentionsb | Spoke to students about mental health problems occasionally or morea | Mental health (abnormal SDQ score) | ||
| 7 | Klingman (1993) | Twelve weekly sessions delivering an educational curriculum on mental distress and disorders, help-seeking, and prevention via theoretical component, role-playing and rehearsing new skills | Knowledge of facts about help resources | ||||||
| 8 | Morgan (2019) | A 14-h standardised pyschoeducation and training program for parents of adolescents to learn to recognise early signs of a mental health problem or crisis and to assist adolescents to access appropriate professional help as early as possible | Parental confidence to help adolescentb | Parental intensions to help adolescentb | Help-seeking by adolescent | Quality of parental supportb | Adolescent mental health | ||
| 9 | Painter (2017) | Three-hour educational curriculum on stigma, mental illness and barriers to help-seeking via presentation, class discussion and video and presentation and discussion with a mentally ill college student | Knowledge about when to recommend that another person seek help | Personal willingness to seek help | |||||
| 10 | Perry (2014) |
A 10 h of educational curriculum delivered over 5–8 weeks; resources for teachers delivering intervention included a booklet, slideshow and appendices on mental health, mood disorders and on helping others and oneself | Explicit attitudes toward seeking help | Psychological distress (suicidal ideation also measured as an outcome) | |||||
| 11 | Saporito (2011) | 35-min presentation on mental illness and its treatment plus video on an adolescent with a mental illness | Explicit attitudes toward seeking professional help | Emotional health (change in negative affect measured by PANAS) | |||||
| 12 | Sayal (2010) |
School-based screening to identify children with high ADHD rating scale scores and a book about ADHD and how to manage and work with affected children | Specialist service use | Symptoms of hyperactivity and inattention | |||||
| 13 | Sharpe (2017) | Booklets on mental health and disorders and help-seeking for students | Frequency of seeking help from counsellor | Mental health (measured by Me and My School Questionnaire) | |||||
| Interventions to engage individuals in health-care system | ||||||||
|---|---|---|---|---|---|---|---|---|
| First author (year) | Intervention description | Outcomes studied | ||||||
| Knowledge | Attitudes | Help-seeking | Accessing care | Health outcomes | Satisfaction | |||
| 14 | Asarnow (2005) | A 6-month health service quality improvement intervention through support and training for clinicians on treatment for people with mental disorders by expert leader teams and care managers | Proportion of subjects who accessed any speciality mental health care | Depressive symptoms (measured by CES-D) | Satisfaction with mental health care | |||
| 15 | Asarnow (2011) |
Brief family-based therapy session to increase motivation during emergency room visit by reframing the problem, educating families about the importance of treatment, obtaining commitment from youth, identifying triggers and developing and practising a safety plan supplemented by care linkage telephone contacts within the first 48 h after discharge | Outpatient mental health treatment | Suicide attempts | ||||
| 16 | Coker (2019) |
A 5-min video on community mental health clinic and scheduled visit for a telehealth eligibility screening | Community mental health clinic screening visit | Health-related quality of life (measured by the Pediatric Quality of Life Inventory) | Satisfaction with the referral process | |||
| 17 | Donohue (1998) | Telephone call by clinical psychology doctoral students to parents about treatment, intake session for parent and youth, motivational reminder calls and incentives to participate in treatment | Proportion of subjects who attended the first appointment | |||||
| 18 | Fristad (2003) | Didactic and interactive multi-family psycho-education group program; parent sessions focused on providing social support, information and skills, while child sessions focused on feeling less alone, understanding symptoms and effects of treatment and building social skills | Perceived social support from parents | Ability to obtain appropriate services | Illness severity (measured by CDRS-R, MRS) | |||
| 19 | Gadomski (2010) | Three hour-long communication skills training sessions for primary care clinicians to engage parents and children in diagnosis and treatment and address barriers to treatment with group discussions and 10-min practice visits | Number of primary care visits | |||||
| 20 | Grupp-Phelan (2012) | Discussion with a study social worker about screening results, patient concerns and available resources; designed to target various barriers and increase motivation for help-seeking behaviour | Proportion of subjects who scheduled the first appointment | Proportion of subjects who attended the first appointment | Depressive symptoms (measured by CES-D) | Screening found to be helpful | ||
| 21 | Gully (2008) | Educational booklet for parents on expectations and perceived value of treatment reviewed together with nurses | Knowledge about evidence-based treatment | Belief that evidence-based treatment is helpful | Proportion of subjects who attended the first appointment and discussed evidence-based treatment during appointment | Satisfaction with services | ||
| 22 | Kourany (1989) | Reminder telephone call, letter describing what would happen on the first clinic visit, or both the call and the letter | Proportion of subjects who attended the first appointment | |||||
| 23 | Lieberman (2006) | Provision of on-site mental health services (usual care was a referral to an off-site mental health provider) | Meeting with a counsellor at least once | |||||
| 24 | MacLean (1989) | One of four experimental letters (systematic appointment reminders, change slips requesting if appointment time should be changed, warnings and change slips combined with warnings) | Proportion of subjects who attended the first appointment | |||||
| 25 | McKay (1996a) | Intensive 30-minute telephone intervention with a social worker to engage caretaker in help-seeking process by identifying child's problem, framing caretaker actions as having potential to impact the situation and exploring barriers to help-seeking | Proportion of subjects who attended the first appointment | |||||
| 26 | McKay (1996b) | Telephone intake with therapists trained in specific engagement skills, i.e., informing clients about the process of obtaining mental health services, responding to concrete concerns or crisis situations and exploring potential barriers to obtaining services | Proportion of subjects who attended the first appointment | |||||
| 27 | McKay (1998) | Thirty-minute telephone and in-person engagement intervention by master's level clinicians to clarify the need for mental health care, increase the caretaker's investment in help-seeking, identify attitudes about and previous experiences with mental health care and over concrete barriers to accessing services | Proportion of subjects who attended the first appointment (proportion of sessions attended v. scheduled was also measured) | |||||
| 28 | Parrish (1986) | Letter informing parents that children would be moved to the bottom of the waiting list if three appointments were missed or letter informing parents that attending appointments would earn a coupon for winning a prize | Proportion of subjects who attended the first appointment | |||||
| 29 | Planos (1986) | Appointment reminder (telephone or letter prompt) | Proportion of subjects who attended screening appointments | |||||
| 30 | Richardson (2014) | A 12-month collaborative care intervention delivered by master's-level clinicians involving initial in-person education engagement session, choice of treatment and regular follow-up | Proportion of subjects with any specialty mental health visits according to administrative data | Depressive symptoms (measured by CDRS-R) | Satisfaction with treatment | |||
| 31 | Stern (2015) | A 10–15 min enhanced engagement phone intake to develop rapport with parents, identify and address likely barriers to treatment, increase parental self-efficacy, hope and treatment motivation | Attendance of first face-to-face interview | |||||
| 32 | Stevens (2009) | Three phone calls in the first weeks after the first visit to the adolescent management clinic to assess youth's understanding of recommendations, address youth's struggles through case management and use motivational interviewing techniques if youth was ambivalent about treatment | Any mental health service use | |||||
| 33 | Szapocznik (1988) | Engagement intervention during intake interview to overcome family's resistance to treatment by identifying family patterns that interfere with entry into treatment | Proportion of subjects visiting centre for intake appointment | Psychiatric and psychosocial functioning (measured by PSS) | ||||
| 34 | Wiseman (1998) | Didactic and interactive multi-family psycho-education group program; parent sessions focused on providing social support, information, skills, while children sessions focused on feeling less alone, understanding symptoms and effects of treatment and building social skills | Proportion of subjects who attended the first appointment | |||||
aTeacher.
bParent.
Data
The protocol for this systematic review has been registered with the International Prospective Register of Systematic Reviews (PROSPERO, ID: CRD42018081714). The publication details for the studies included in this systematic review have been included in the reference list.
Financial support
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Ethical standards
This research did not involve human and/or animal experimentation.
Conflict of interest
None.
References
- Anderson JK, Howarth E, Vainre M, Jones PB and Humphrey A (2017) A scoping literature review of service-level barriers for access and engagement with mental health services for children and young people. Children and Youth Services Review 77, 164–176. [Google Scholar]
- Asarnow JR, Jaycox LH, Duan N, LaBorde AP, Rea MM, Murray P, Anderson M, Landon C, Tang L and Wells KB (2005) Effectiveness of a quality improvement intervention for adolescent depression in primary care clinics: a randomized controlled trial. Journal of the American Medical Association 293, 311–319. [DOI] [PubMed] [Google Scholar]
- Asarnow JR, Baraff LJ, Berk M, Grob CS, Devich-Navarro M, Suddath R, Piacentini JC, Rotheram-Borus MJ, Cohen D and Tang L (2011) An emergency department intervention for linking pediatric suicidal patients to follow-up mental health treatment. Psychiatric Services 62, 1303–1309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aseltine RH, James A, Schilling EA and Glanovsky J (2007) Evaluating the SOS suicide prevention program: a replication and extension. BMC Public Health 7, 161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campos L, Dias P, Duarte A, Veiga E, Dias CC and Palha F (2018) Is it possible to “find space for mental health” in young people? Effectiveness of a school-based mental health literacy promotion program. International Journal of Environmental Research and Public Health 15, 1426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centre for Reviews and Dissemination (2009) Systematic Reviews: CRD's Guidance for Undertaking Reviews in Health Care. Centre for Reviews and Dissemination, York, UK. [Google Scholar]
- Christiana JM, Gilman SE, Guardino M, Mickelson K, Morselli PL, Olfson M and Kessler RC (2000) Duration between onset and time of obtaining initial treatment among people with anxiety and mood disorders: an international survey of members of mental health patient advocate groups. Psychological Medicine 30, 693–703. [DOI] [PubMed] [Google Scholar]
- Coker TR, Porras-Javier L, Zhang L, Soares N, Park C, Patel A, Tang L, Chung P and Zima BT (2019) A telehealth-enhanced referral process in pediatric primary care: a cluster randomized trial. Pediatrics 143, e20182738. [DOI] [PubMed] [Google Scholar]
- Donohue B, Azrin NH, Lawson H, Friedlander J, Teichner G and Rindsberg J (1998) Improving initial session attendance of substance abusing and conduct disordered adolescents: a controlled study. Journal of Child & Adolescent Substance Abuse 8, 1–13. [Google Scholar]
- Dunne T, Bishop L, Avery S and Darcy S (2017) A review of effective youth engagement strategies for mental health and substance use interventions. Journal of Adolescent Health 60, 487–512. [DOI] [PubMed] [Google Scholar]
- Fristad MA, Goldberg-Arnold JS and Gavazzi SM (2003) Multi-family psychoeducation groups in the treatment of children with mood disorders. Journal of Marital and Family Therapy 29, 491–504. [DOI] [PubMed] [Google Scholar]
- Gadomski A, Wissow LS, Slade E and Jenkins P (2010) Training clinicians in mental health communication skills: impact on primary care utilization. Academic Pediatrics 10, 346–352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grupp-Phelan J, McGuire L, Husky MM and Olfson M (2012) A randomized controlled trial to engage in care of adolescent emergency department patients with mental health problems that increase suicide risk. Pediatric Emergency Care 28, 1263–1268. [DOI] [PubMed] [Google Scholar]
- Gulliver A, Griffiths KM and Christensen H (2010) Perceived barriers and facilitators to mental health help-seeking in young people: a systematic review. BMC Psychiatry 10, 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gulliver A, Griffiths KM, Christensen H and Brewer JL (2012) A systematic review of help-seeking interventions for depression, anxiety and general psychological distress. BMC Psychiatry 12, 81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gully KJ, Price BL and Johnson MK (2008) Increasing abused children's access to evidence-based treatment: diffusion via parents as consumers. Child Maltreatment 13, 280–288. [DOI] [PubMed] [Google Scholar]
- Guyatt GH, Oxman AD, Schünemann HJ, Tugwell P and Knottnerus A (2011) GRADE guidelines: a new series of articles in the Journal of Clinical Epidemiology. Journal of Clinical Epidemiology 64, 380–382. [DOI] [PubMed] [Google Scholar]
- Hart LM, Morgan AJ, Rossetto A, Kelly CM, Mackinnon A and Jorm AF (2018) Helping adolescents to better support their peers with a mental health problem: a cluster-randomised crossover trial of teen Mental Health First Aid. Australian & New Zealand Journal of Psychiatry 52, 638–651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higgins JPT, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, Savovic J, Schulz KF, Weeks L, Sterne JAC and Cochrane Bias Methods Group and Cochrane Statistical Methods Group (2011) The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ (Clinical research ed.), 343, d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hodgkinson S, Godoy L, Beers LS and Lewin A (2017) Improving mental health access for low-income children and families in the primary care setting. Pediatrics 139, e20151175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horwitz SM, Kelleher KJ, Stein REK, Storfer-Isser A, Youngstrom EA, Park ER, Heneghan AM, Jensen PS, O'Connor KG and Hoagwood KE (2007) Barriers to the identification and management of psychosocial issues in children and maternal depression. Pediatrics 119, e208–e218. [DOI] [PubMed] [Google Scholar]
- Howard KA, Griffiths KM, McKetin R and Ma J (2018) Can a brief biologically-based psychoeducational intervention reduce stigma and increase help-seeking intentions for depression in young people? A randomised controlled trial. Journal of Child & Adolescent Mental Health 30, 27–39. [DOI] [PubMed] [Google Scholar]
- Husky MM, Kaplan A, McGuire L, Flynn L, Chrostowski C, Olfson M, McGuirea L, Flynna L, Chrostowski C and Olfson M (2011) Identifying adolescents at risk through voluntary school-based mental health screening. Journal of Adolescence 34, 505–511. [DOI] [PubMed] [Google Scholar]
- Ingoldsby EM (2010) Review of interventions to improve family engagement and retention in parent and Child Mental Health Programs. Journal of Child and Family Studies 19, 629–645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iza M, Olfson M, Vermes D, Hoffer M, Wang S and Blanco C (2013) Probability and predictors of first treatment contact for anxiety disorders in the United States: analysis of data from the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC). The Journal of Clinical Psychiatry 74, 1093–1100. [DOI] [PubMed] [Google Scholar]
- Jorm AF, Kitchener BA, Sawyer MG, Scales H and Cvetkovski S (2010) Mental health first aid training for high school teachers: a cluster randomized trial. BMC Psychiatry 10, 51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- GBD 2015 DALYs and HALE Collaborators (2016) Global, regional, and national disability-adjusted life-years (DALYs) for 315 diseases and injuries and healthy life expectancy (HALE), 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. The Lancet 388(10053), 1603–1658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly MP and Barker M (2016) Why is changing health-related behaviour so difficult? Public Health 136, 109–116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR and Walters EE (2005) Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry 62, 593–602. [DOI] [PubMed] [Google Scholar]
- Klingman A and Hochdorf Z (1993) Coping with distress and self harm: the impact of a primary prevention program among adolescents. Journal of Adolescence 16, 121–140. [DOI] [PubMed] [Google Scholar]
- Kourany RF, Garber J and Tornusciolo G (1990) Improving first appointment attendance rates in child psychiatry outpatient clinics. Journal of the American Academy of Child & Adolescent Psychiatry 29, 657–660. [DOI] [PubMed] [Google Scholar]
- Laverack G (2017) The challenge of behaviour change and health promotion. Challenges 8, 25. [Google Scholar]
- Lenzer J (2017) Is the United States preventive services task force still a voice of caution? BMJ: British Medical Journal (Online) 356. [DOI] [PubMed] [Google Scholar]
- Levesque J-F, Harris MF and Russell G (2013) Patient-centred access to health care: conceptualising access at the interface of health systems and populations. International Journal for Equity in Health 12, 18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lieberman A, Adalist-Estrin A, Erinle O and Sloan N (2006) On-site mental health care: a route to improving access to mental health services in an inner-city, adolescent medicine clinic. Child: Care, Health and Development 32, 407–413. [DOI] [PubMed] [Google Scholar]
- Lindsey MA, Brandt NE, Becker KD, Lee BR, Barth RP, Daleiden EL and Chorpita BF (2014) Identifying the common elements of treatment engagement interventions in children's mental health services. Clinical Child and Family Psychology Review 17, 283–298. [DOI] [PubMed] [Google Scholar]
- Lo K, Gupta T and Keating JL (2017) Interventions to promote mental health literacy in university students and their clinical educators. A systematic review of randomised control trials. Health Professions Education 4, 161–175. [Google Scholar]
- Lüdecke D (2019). esc: Effect Size Computation for Meta Analysis (Version 0.5.0). doi: 10.5281/zenodo.1249218, https://CRAN.R-project.org/package=esc [DOI]
- MacLean LM, Greenough T, Jorgenson V and Couldwell M (1989) Getting through the front door: improving initial appointment attendance at a mental-health clinic. Canadian Journal of Community Mental Health 8, 123–133. [Google Scholar]
- McKay MM, McCadam K and Gonzales JJ (1996a) Addressing the barriers to mental health services for inner city children and their caretakers. Community Mental Health Journal 32, 353–361. [DOI] [PubMed] [Google Scholar]
- McKay MM, Nudelman R, McCadam K and Gonzales J (1996b) Evaluating a social work engagement approach to involving inner-city children and their families in mental health care. Research on Social Work Practice 6, 462–472. [Google Scholar]
- McKay MM, Stoewe J, McCadam K and Gonzales J (1998) Increasing access to child mental health services for urban children and their caregivers. Health & Social Work 23, 9–15. [DOI] [PubMed] [Google Scholar]
- Moher D, Liberati A, Tetzlaff J and Altman DG (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Medicine 6, e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morgan AJ, Fischer J-AA, Hart LM, Kelly CM, Kitchener BA, Reavley NJ, Yap MBH, Cvetkovski S and Jorm AF (2019) Does mental health first Aid training improve the mental health of aid recipients? The training for parents of teenagers randomised controlled trial. BMC Psychiatry 19, 99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institute for Health and Clinical Excellence (2011) Common Mental Health Disorders: The NICE Guideline on Identification and Pathways to Care. The British Psychological Society and The Royal College of Psychiatrists. [Google Scholar]
- Painter K, Phelan JC, DuPont-Reyes MJ, Barkin KF, Villatoro AP and Link BG (2017) Evaluation of antistigma interventions with sixth-grade students: a school-based field experiment. Psychiatric Services 68, 345–352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parrish JM, Charlop MH and Fenton LR (1986) Use of a stated waiting list contingency and reward opportunity to increase appointment keeping in an outpatient pediatric psychology clinic. Journal of Pediatric Psychology 11, 81–89. [DOI] [PubMed] [Google Scholar]
- Patel V, Kieling C, Maulik PK and Divan G (2013) Improving access to care for children with mental disorders: a global perspective. Archives of Disease in Childhood 98, 323–327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perry Y, Petrie K, Buckley H, Cavanagh L, Clarke D, Winslade M, Hadzi-Pavlovic D, Manicavasagar V and Christensen H (2014) Effects of a classroom-based educational resource on adolescent mental health literacy: a cluster randomised controlled trial. Journal of Adolescence 37, 1143–1151. [DOI] [PubMed] [Google Scholar]
- Planos R and Glenwich DS (1986) The effects of prompts on minority children's screening attendance at a community mental health center. Child and Family Behavior Therapy 8, 5–14. [Google Scholar]
- Richardson LP, Ludman E, McCauley E, Lindenbaum J, Larison C, Zhou C, Clarke G, Brent D and Katon W (2014) Collaborative care for adolescents With depression in primary care. JAMA 312, 809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richardson LP, McCarty CA, Radovic A and Suleiman AB (2017) Research in the integration of behavioral health for adolescents and young adults in primary care settings: a systematic review. Journal of Adolescent Health 60, 261–269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salerno JP (2016) Effectiveness of universal school-based mental health awareness programs among youth in the United States: a systematic review. Journal of School Health 86, 922–931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saporito JM, Ryan C and Teachman BA (2011) Reducing stigma toward seeking mental health treatment among adolescents. Stigma Research And Action 1, 9–21. [PMC free article] [PubMed] [Google Scholar]
- Saxena S, Thornicroft G, Knapp M and Whiteford H (2007) Resources for mental health: scarcity, inequity, and inefficiency. The Lancet 370, 878–889. [DOI] [PubMed] [Google Scholar]
- Sayal K, Owen V, White K, Merrell C, Tymms P and Taylor E (2010) Impact of early school-based screening and intervention programs for ADHD on children's outcomes and access to services. Archives of Pediatrics & Adolescent Medicine 164, 462–469. [DOI] [PubMed] [Google Scholar]
- Schwarzer G (2007) Meta: an R package for meta-analysis. R News 7, 40–45. [Google Scholar]
- Sharpe H, Patalay P, Vostanis P, Belsky J, Humphrey N and Wolpert M (2017) Use, acceptability and impact of booklets designed to support mental health self-management and help seeking in schools: results of a large randomised controlled trial in England. European Child & Adolescent Psychiatry 26, 315–324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simon GE, Barber C, Birnbaum HG, Frank RG, Greenberg PE, Rose RM, Wang PS and Kessler RC (2001) Depression and work productivity: the comparative costs of treatment versus nontreatment. Journal of Occupational and Environmental Medicine 43, 2–9. [DOI] [PubMed] [Google Scholar]
- So M, McCord RF and Kaminski JW (2019) Policy levers to promote access to and utilization of children's mental health services: a systematic review. Administration and Policy in Mental Health and Mental Health Services Research 46, 334–351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stern SB, Walsh M, Mercado M, Levene K, Pepler DJ, Carr A, Heppell A and Lowe E (2015) When they call, will they come? A contextually responsive approach for engaging multistressed families in an urban child mental health center: a randomized clinical trial. Research on Social Work Practice 25, 549–563. [Google Scholar]
- Stevens J, Klima J, Chisolm D and Kelleher KJ (2009) A trial of telephone services to increase adolescent utilization of health care for psychosocial problems. Journal of Adolescent Health 45, 564–570. [DOI] [PubMed] [Google Scholar]
- Szapocznik J, Perez-Vidal A, Brickman AL, Foote FH, Santisteban D, Hervis O and Kurtines WM (1988) Engaging adolescent drug abusers and their families in treatment: a strategic structural systems approach. Journal of Consulting and Clinical Psychology 56, 552–557. [DOI] [PubMed] [Google Scholar]
- The Lancet (2017) Better understanding of youth mental health. The Lancet 389, 1670. [DOI] [PubMed] [Google Scholar]
- Wang PS, Berglund P, Olfson M, Pincus HA, Wells KB and Kessler RC (2005) Failure and delay in initial treatment contact after first onset of mental disorders in the national comorbidity survey replication. Archives of General Psychiatry 62, 603–613. [DOI] [PubMed] [Google Scholar]
- Wiseman M and McBride M (1998) Increasing the attendance rate for first appointments at child and family psychiatry clinics: an opt-in system. Child Psychology & Psychiatry Review 3, 68–71. [Google Scholar]
- Wissow LS, Brown J, Fothergill KE, Gadomski A, Hacker K, Salmon P and Zelkowitz R (2013) Universal mental health screening in pediatric primary care: a systematic review. Journal of the American Academy of Child and Adolescent Psychiatry 52, 1134–1147.e23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization (1992) The ICD-10 classification of mental and behavioural disorders: Clinical descriptions and diagnostic guidelines.
- Xu Z, Huang F, Kösters M, Staiger T, Becker T, Thornicroft G and Rüsch N (2018) Effectiveness of interventions to promote help-seeking for mental health problems: systematic review and meta-analysis. Psychological Medicine 48, 2658–2667. [DOI] [PubMed] [Google Scholar]