Abstract
Aims
This review aims to understand the scope of the literature regarding mental health-related microaggressions towards people affected by mental health problems.
Methods
A scoping review was conducted to explore this question. Four electronic health-oriented databases were searched alongside Google Scholar. As per scoping review principles, the inclusion criteria were developed iteratively. The results of included studies were synthesised using a basic narrative synthesis approach, utilising principles of thematic analysis and thematic synthesis where appropriate.
Results
A total of 1196 records were identified, of which 17 met inclusion criteria. Of these, 12 were peer-reviewed journal articles, three were research degree theses and two were book chapters. Six included empirical studies were qualitative, four were quantitative and two employed a mixed-methods design. Within these, five qualitative studies aimed to describe the nature of mental health microaggressions experienced by people with mental health problems. Themes identified in a thematic synthesis of these five studies included stereotypes about mental illness, invalidating peoples' experience and blaming people with mental illness for their condition. The included publications informed on the perpetration of mental health microaggressions by family, friends, health professionals and social workers. In addition, two studies created scales, which were then used in cross-sectional surveys of the general public and community members to assess characteristics, such as right-wing political views, associated with endorsement of mental health microaggressions. A consensus definition of microaggressions emerged from the included studies: microaggressions are brief, everyday slights, snubs or insults, that may be subtle or ambiguous, but communicate a negative message to a target person based on their membership of a marginalised group, in this case, people affected by mental illness.
Conclusions
The study of mental health microaggressions is an emerging, heterogeneous field, embedded in the wider stigma and discrimination literature. It has been influenced by earlier work on racial microaggressions. Both can be ambiguous and contradictory, which creates difficulty defining the boundaries of the concept, but also underpins the key theoretical basis for the negative impact of microaggressions. Mental illness is a more concealable potential type of identity, so it follows that the reported perpetrators of microaggressions are largely friends, family and professionals. This has implications for intervening to reduce the impact of microaggressions. There are several challenges facing research in this area, and further work is needed to understand the impact of mental health microaggressions on people affected by mental health problems.
Key words: Community mental health, discrimination, mental health, mental illness stigma
Introduction
The term ‘microaggression’ was coined in 1970 to describe subtle dismissals and insults towards Black Americans (Pierce, 1970). The word remained largely in obscurity until the late 2000s, when a paper exploring ‘subtle and contemporary’ forms of racism in the context of therapy gained widespread public attention (Sue et al., 2007). Based on the analysis of personal narratives and the social and counselling psychology literature, Sue et al. defined microaggressions as ‘brief and commonplace daily verbal, behavioural or environmental indignities, whether intentional or unintentional, that communicate hostile, derogatory, or negative racial slights and insults towards people of color’ (Sue et al., 2007, p. 271). They describe three distinct forms of microaggressions: microassault, microinsult and microinvalidation. A microassault is the most overt form, for example, intentionally calling a person of colour a derogatory term. Microinsults are more subtle and convey rudeness or insensitivity, for example, clutching one's purse more tightly when in the presence of a person of colour. Finally, microinvalidations negate or nullify the feelings or experiences of a person, by saying, for example, ‘Don't be so oversensitive’ (Sue et al., 2007, p. 275).
The concept of subtle, contemporary forms of racism has captured the attention of wide audiences, not least because these researchers argue that microaggressions have a powerful, negative cumulative effect on the mental health of people of colour (Sue et al., 2007; Sue, 2010). The theoretical basis of this assertion is grounded in ‘minority stress theory’ (Meyer, 1995) which states that a hostile social environment demands heightened vigilance to protect oneself from discrimination and violence. It is also argued that the subtle nature of microaggressions creates a ‘catch-22’ (or ‘no win’) situation, in which an individual is left questioning the validity of his or her experience (‘Did what I think happened, really happen?’). This concept has been described as attributional ambiguity in the wider stigma literature and is argued to pose a particular threat to self-esteem and lead to suspicion and mistrust (Crocker et al., 1998).
Numerous studies have reported a significant correlation between reported experiences of microaggressions and self-reported negative mental health outcomes (e.g. Nadal et al., 2014; Gattis and Larson, 2017; Reid, 2017). Whilst most studies have been cross-sectional, a study using a longitudinal design has shown that microaggressions in the form of ‘underestimation of personal ability’ significantly predicted self-rated depression symptoms 1 year later – providing some indication of potential causation (Torres et al., 2010).
Research on microaggression is not without its critics. Some argue that a microaggression is an open concept with ‘fuzzy’ boundaries, full of contradictions and ambiguities – for example, both ignoring and attending to minority students in classrooms have been listed as microaggressions (Lilienfeld, 2017). It is apparent that microaggressions are ambiguous and ‘lie in the eye of the beholder’, and so, variations in responses by targets of microaggressions may be a function of an individual's personality dispositions, a key confounder when asserting a causal association between microaggressions and adverse mental health outcomes (Lilienfeld, 2017). Indeed, once accounting for scores of ‘perceived stress’ (feeling life is unpredictable, uncontrollable and overloaded), Torres et al. found that the predictive effect of microaggressions on depression symptoms was non-significant (Torres et al., 2010).
Nevertheless, the use of the term ‘microaggression’ is expanding. It is now used to describe snubs, slights and insults towards members of other marginalised social groups including women, sexual minorities and people with disabilities (Sue, 2010). There is a growing literature on the experience of people affected by mental health problems, arguably a marginalised social group in its own right. This emerging field can be seen to fit into the wider literature on stigma towards mental illness – a broad concept that encompasses ignorance, prejudice and discrimination (Thornicroft, 2006).
The purpose of this scoping review was to answer the following research question: ‘What is the scope of the literature regarding mental health-related microaggressions towards people affected by mental health problems?’. We aimed to characterise the literature in this area (e.g. who is conducting this research, and from what discipline?), elucidate the purpose of research on this topic for this population (e.g. to describe the experiences of people with mental health problems or to measure the effect) and describe and synthesise the current evidence base. In doing so, we planned to clarify the definition of the term microaggression as it is used in relation to people with mental health problems. In addition, we aimed to identify the problematic areas of this research topic (e.g. varying definitions, the distinction between a microaggression and other forms of subtle discrimination) and propose the next steps for researchers in this field.
Methods
A scoping review approach was used to answer the research question. Like a systematic review, a scoping review is informed by an a priori protocol, involves systematic and exhaustive searching, must be transparent and reproducible, includes steps to reduce error and increase reliability, and presents data in a structured way (Munn et al., 2018). However, in contrast to the systematic review method which is guided by a highly focussed research question, the scoping review method is guided by a requirement to identify all relevant literature, and as such it allows for procedural flexibility during the conduct of the review to achieve this aim (Arksey and O'Malley, 2005). A scoping review methodology was therefore considered highly appropriate for our research aim to characterise and synthesise the current literature. We followed the procedure outlined by Arksey and O'Malley (2005) and further developed by Levac et al. (2010).
This review complies with the preferred reporting items for systematic reviews and meta-analyses (PRISMA) statement (Moher et al., 2009). It follows an a priori developed review protocol, registered at the Open Science Framework platform (Barber et al., 2019).
Identifying the review question and aims
The research question was formulated through consideration of the concept and target population, using aspects of the SPIDER question format tool (i.e. examining Sample, Phenomenon of Interest, Design, Evaluation, and Research type) (Cooke et al., 2012). For this review, we specified only the ‘sample’ and ‘phenomenon of interest’ aspects, to fulfil the aim of characterising the literature in this area.
In line with the iterative, flexible nature of the scoping review process (Levac et al., 2010), the ‘sample’ was revised during the study selection process. Initially defined as ‘people with mental health problems’, this was refined to ‘people whose defining characteristic, in the study, is being affected by a mental health problem or disability’.
The ‘phenomenon of interest’ was mental health-related microaggressions specifically. This was specified as microaggressions attributed to a mental health problem or mental health-related disability. We did not include papers which addressed racial or other microaggressions directed towards people with mental health problems. Unless otherwise stated, the term microaggression in this manuscript refers to this narrow definition.
Identifying relevant studies
The search strategy was designed to identify formally published, peer-reviewed articles and selected grey literature, including research degree theses and book chapters but not ‘grey data’ (e.g. websites, tweets and blog posts). Four electronic health-oriented databases were searched in July 2019: Medline, EMBASE, PsycINFO and WorldCat Dissertation database. We also searched Google Scholar, identified as a powerful addition to traditional search methods (Haddaway et al., 2015). The first 300 results of a search on ‘Incognito mode’ (used to improve replicability) were screened.
The search strategies consisted of keywords and subject headings related to ‘mental health’ and ‘microaggressions’. For Google Scholar the following search strategy was used: ‘(Mental* or Psych*) AND microaggress*’. Appendix 1 gives full search strategies for each database.
We supplemented the database and search engine searches by conducting backwards and forwards citation checking and contacting authors and experts in the field.
Study selection
Study selection followed a two-step approach: (1) title, abstract, key word screening, (2) full-text screening. In both stages, SB and SA independently screened a proportion of results (25 and 40%, respectively), with PCG acting as an arbitrator. Interrator reliability was calculated and exceeded 80%. SB screened the remainder of the results. In line with scoping review principles, inclusion criteria were developed iteratively through discussion between authors.
Data extraction and management
Data from the included full texts were extracted onto a ‘Characteristics of Included Studies’ table, including country, department/institution (lead author), publication type, study design, population of interest (sample size) and purpose (e.g. to describe the experience of microaggressions, or to validate a scale).
Qualitative synthesis and analysis
The results of included studies were synthesised using a basic narrative synthesis approach, applying principles of thematic analysis (Braun and Clarke, 2006) and thematic synthesis (Thomas and Harden, 2008) where appropriate, given the available data and how it could best be examined to answer the review questions.
Quality of included studies assessment
We used the Mixed Methods Appraisal Tool (MMAT) (Hong et al., 2018) to assess the quality of included empirical studies. This tool is designed for quality assessment in systematic reviews that include quantitative, qualitative and mixed-method studies. Articles were assigned one point for each criterion that was fulfilled, and half a point for each partially met the criterion. These points were summed to produce an index based on the proportion of total criteria met. No studies were excluded from the synthesis due to low-quality score.
Results
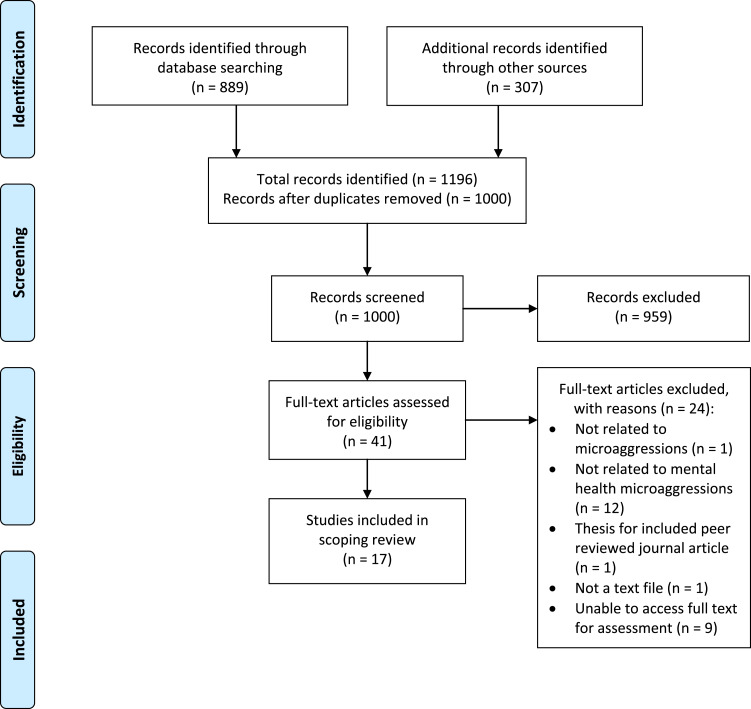
In total, 1196 records were identified: 889 records from database searching, and 307 through other sources (300 from Google Scholar, five through communication with authors, two through consultation with experts). After duplicates were removed, 1000 records remained for title, abstract and key word screening. In total, 959 records were excluded at this stage, leaving 41 records for full-text assessment for eligibility, of which 17 met inclusion criteria for this review. This study selection procedure is illustrated in the PRISMA flow diagram (see Fig. 1).
Fig. 1.
PRISMA flow diagram. Adapted from Moher et al. (2009).
Characterising the literature
The characteristics of included studies are summarised in Table 1.
Table 1.
Characteristics of included studies
| Study | Country | Department/institution (of lead author) | Publication type | Study design | Population of interest (sample size) | Purpose | MMAT Index score |
|---|---|---|---|---|---|---|---|
| Gonzales et al. (2015a) | USA | Department of Psychology, City University of New York | Peer-reviewed journal article | Qualitative (focus groups) | People with mental health problems (21) | To describe the nature of mental health microaggressions from the perspective of people affected by mental health problems | 100% |
| Peters et al. (2016) | USA | Department of Psychology, University of South Dakota | Peer-reviewed journal article | Qualitative (focus groups) | People with mental health problems (18) | To describe the nature of mental health microaggressions from the perspective of people affected by mental health problems | 100% |
| Holley et al. (2016a) | USA | School of Social Work Arizona State University | Peer-reviewed journal article | Qualitative (1:1 interview) | People with mental health problem (or their family) who also identify as of colour or LGBTQ or both (20) | To examine the experience of mental illness discrimination in the mental health system | 100% |
| McCue (2016) | USA | Unknown, Michigan State University | PhD thesis | Qualitative (1:1 interview) | Law students with mental health problems (11) | To examine the lived experiences of law students with mental health problems | 100% |
| Zenga (2018) | USA | Faculty of the California School of Professional Psychology, Alliant International University San Diego | PhD thesis | Mixed methods: qualitative (focus groups) and cross-sectional survey | Mental health peer support specialists (16) | To examine how peer support specialists experience microaggressions | 90% |
| Charles et al. (2017) | USA | School of Social Work, University of Indianapolis | Peer-reviewed journal article | Qualitative component (open text questions) of cross-sectional survey | Social work educators (246) | To determine whether social work educators report microaggressions towards students with mental illnesses, and if educators practice cultural humility | 90% |
| Gonzales et al. (2015b) | USA | Department of Psychology, City University of New York | Peer-reviewed journal article | Validation of a scale | General public (505) | To develop and validate a scale for measuring microaggression behaviours as endorsed among the general population | Not applicable |
| Ezell et al. (2018) | USA | Department of Sociology, University of Chicago | Peer-reviewed journal article | Validation of a scale | People with mental health problems (65) | To develop and validate a scale for measuring the daily indignities of mental illness | Not applicable |
| DeLuca et al. (2018) | USA | Department of Psychology, City University of New York | Peer-reviewed journal article | Cross-sectional survey | General public (518) | To determine the relationship between political attitudes to multidimensional components of mental health stigma | 80% |
| Gonzales et al. (2018) | USA | Department of Psychology, City University of New York | Peer-reviewed journal article | Cross-sectional survey | Community members (606), people with mental health problems (343) | To determine the relationship between microaggressions perceived by persons with disabilities and the self-reported attitudes and behaviours by community members | 60% |
| Zurick (2016) | USA | Department of Psychology, Southern Illinois University | Masters thesis | Cross-sectional survey | General public (222) | To examine the role of specific prejudicial beliefs and intimacy of interpersonal contact in relation to mental health microaggressions | 50% |
| DeLuca et al. (2017) | USA | Department of Psychology, City University of New York | Peer-reviewed journal article | Cross-sectional survey | General public (951) | To examine the influence of individual- and societal-level characteristics, including endorsement of microaggressions, on mental health funding decisions | 70% |
| Harper et al. (2017) | USA | Department of Psychiatry, Yale University | Peer-reviewed journal article | Qualitative (1:1 interview) | People with mental health problems (8) | To examine the community integration experiences of people with severe mental illness | 100% |
| Borg et al. (2009) | Norway | Department of Health Sciences, Buskerud University College | Peer-reviewed journal article | (Conceptual paper) | People with mental health problems in the community | To raise fundamental questions associated with user involvement in community mental health practices | Not applicable |
| Holley et al. (2016b) | USA | School of Social Work, Arizona State University | Peer-reviewed journal article | Mixed methods: qualitative (1:1 interview) and cross-sectional survey | People with mental health problems (or their family) who also identify as of colour or LGBTQ or both (20) | To examine the perceptions of similarities and differences between mental illness discrimination and racism and/or heterosexism | 60% |
| Yanos (2017) | USA | Not stated | Book chapter | (Synthesis of literature and commentary) | People with mental health problems | To describe forms of stigmatising behaviour towards people with mental health problems | Not applicable |
| Holley and Thomas (2018) | Not stated | Not stated | Book chapter | (Synthesis of literature and commentary) | People with intersecting identities including mental health problems | To discuss effective social work practice | Not applicable |
All papers and chapters were published in the last decade (16 in the last 4 years), 15 are from the USA (five from authors associated with the City University of New York) and most papers originated from departments of Psychology (n = 8), followed by Social Work (n = 3).
Six included empirical studies were qualitative in nature, using focus group (Gonzales et al., 2015a; Peters et al., 2016), one-to-one semi-structured interviews (Holley et al., 2016a; McCue, 2016; Harper et al., 2017) and analysis of free-text survey questions (Charles et al., 2017). Four were cross-sectional surveys (Zurick, 2016; DeLuca et al., 2017; DeLuca et al., 2018; Gonzales et al., 2018), with sample sizes from 222 to 951 participants. Four of these studies employed convenience sampling of the US public using online survey platforms. Two studies adopted a mixed-methods design (Holley et al., 2016b; Zenga, 2018). Two included publications aimed to validate a scale (Gonzales et al., 2015b; Ezell et al., 2018). The remaining three papers and chapters (Borg et al., 2009; Yanos, 2017; Holley and Thomas, 2018) were not research studies, but still met inclusion criteria and offered an insight into the scope of the literature.
Characterising the purpose of research on this topic for this population
Five studies aimed to elucidate the nature of mental health microaggressions from the perspective of people affected by mental health problems (Gonzales et al., 2015a; Holley et al., 2016a; McCue, 2016; Peters et al., 2016; Zenga, 2018). In three, the participants had intersecting identities as racial and/or sexual orientation minority group members (Holley et al., 2016a), law students (McCue, 2016) and peer support specialists (Zenga, 2018). We synthesised the experiences of microaggressions described in these studies (see Table 2).
Table 2.
A thematic synthesis of experiences described as mental health microaggressions
| Theme (sub-theme) | Supporting quote (source) |
|---|---|
| Stereotypes about mental illness | |
| People with mental illness lack intelligence | ‘you are not as smart or as capable to succeed or to be in like leadership positions’ (Peters et al., 2016, p. 93) |
| People with mental illness are incapable | ‘because you're mentally ill, they think all you can do is just scrub floors’ (Gonzales et al., 2015a, p. 237) |
| People with mental illness are weak | ‘You'll do things because someone tells you to… that you're weak.’ (Gonzales et al., 2015a, p. 237) |
| People with mental illness are dangerous | ‘Well, he does have a mental illness… he tends to be violent’ (Gonzales et al., 2015a, p. 237) |
| People with mental illness are cold | ‘You aren't in like this deep dark void where you don't even care about everyone else?’ (Peters et al., 2016, p. 96) |
| Treating people with mental illness differently | |
| Treating people with mental illness like children | ‘non-[peer support specialist]staff spoke in an overly gushy tone, like to a child, I felt she was fake’ (Zenga 2018, p. 56) |
| Patronising people with mental illness | ‘They often try to intercede on my behalf and do things for me’ (Holley et al., 2016a, p. 316) |
| Giving fake compliments to people with mental illness | ‘They were trying to by nice but they weren't, pretty much. Saying like, “Wow, that's really brave of you”’ (Gonzales et al., 2015a, p. 237) |
| Ignoring people with mental illness | ‘Ann described a psychiatrist's attitude during an appointment with her partner as: “I just want to ask the questions and you're going to answer [them] and that's it”’ (Holley et al., 2016a, p. 314) |
| Increasing distance from people with mental illness | ‘… and they take a second look and start moving away from me, and sit somewhere else’ (Gonzales et al., 2015a, p. 238) |
| Devaluing people with mental illness | ‘well we are viewed as professionals, but not quite professional’ (Zenga, 2018, p. 58) |
| Defining people with mental illness by their diagnosis | |
| Labelling people with mental illness | ‘Gerard explained that staff “gear” PWMI to say “I am bipolar” rather than “I have bipolar disorder”’ (Holley et al., 2016a, p. 315) |
| Not treating people as complex individuals | ‘We have thoughts, feelings, and emotions just like everyone else does’ (Holley et al., 2016a, p. 316) |
| Assuming behaviour is a symptom of mental illness | ‘Or if I do a lot of activities or stay up late I'll have people call me up and say ‘Maybe you're manic, you stayed up really late. You've done a lot more things than you usually do’ (Gonzales et al., 2015a, p. 237) |
| Invalidating peoples experience of mental illness | |
| Doubting existence of mental illness | ‘You have PTSD? Well you are acting normal’ (Zenga, 2018, p. 57) |
| Doubting severity of mental illness | ‘You'll be fine. Just get over it’ (McCue, 2016, p. 85) |
| Minimizing experiences of people with mental illness | ‘Oh I sometimes get sad, too’ (McCue, 2016, p. 85) |
| Comparing peoples' experiences of mental illness | ‘I have another client who did this when they were depressed. So you're not actually that depressed’ (Gonzales et al., 2015a, p. 236) |
| Blaming people with mental illness for their condition | |
| People with mental illness bring it upon themselves | ‘you did something to cause this to happen’ (Peters et al., 2016, p. 96) |
| Accusing people with mental illness of ulterior motives | |
| People use mental illness as an excuse | ‘You're using it as an excuse not to do your work’ (Peters et al., 2016, p. 96) |
| People use mental illness to seek attention | ‘… people treat you like you're just being dramatic’ (Peters et al., 2016, p. 96) |
| Shaming people with mental illness | |
| Shaming people who disclose their mental illness | ‘That's okay that you're telling me but that's not appropriate to say in an interview’ (Gonzales et al., 2015a, p. 238) |
| Not acknowledging mental illness | ‘I saw a picture of a relative and no one talked about her’ (Zenga, 2018, p. 55) |
| Misusing terminology | |
| Using mental health terms inappropriately | ‘The weather is bipolar’ (McCue, 2016, p. 85) |
| Using mental health terms flippantly | ‘“I feel like killing myself today” and you're like dude, no you don't’ (Peters et al., 2016, p. 99) |
These five papers also provide data on the perpetrators of mental health microaggressions, which included family, friends and health professionals. For example, a participant in Gonzales et al. (2015a) stated: ‘People in my family, if I actually starting being happy they're like, “Are you sure you're okay?”’ (p. 237). Similarly, Peters et al. (2016) provided an example of friends misusing terminology ‘I even have friends that say it… they're just like, “But oh man they were so bipolar”’ (p. 100). Additionally, a participant in McCue (2016) described an experience where a fellow student said ‘that he has depression’ and that ‘he could go out and get that extra time but he has dignity’ (p. 85), consistent with perpetration of a microaggression by a peer (by shaming mental illness). One further paper aimed to describe mental health microaggressions from the perspective of potential perpetrators (Charles et al., 2017). They demonstrated that social work educators report personal reactions that reflect microaggressions.
Two papers aimed to create scales, one measuring the experience of microaggressions (Ezell et al., 2018) and one measuring endorsement of microaggressions by possible perpetrators (Gonzales et al., 2015b). The latter was used in three studies aiming to identify individual characteristics associated with endorsement of mental health microaggressions by the general public. Broadly, endorsement of microaggressions was positively associated with right-wing political views (DeLuca et al., 2018), suburban values and socio-economic disadvantage (Gonzales et al., 2018), authoritarianism (the attitude that people with serious mental illness cannot care for themselves and require coercion) and social restrictiveness (the belief that people with mental illness should be feared and excluded) (Zurick, 2016). Endorsement was negatively associated with benevolence (the belief that people with mental illness are innocent and naïve) (Zurick, 2016).
Two studies considered the impact of microaggressions. One qualitative study described a ‘negative outcome’ theme that included frustration, loss of self-esteem and alienation (Gonzales et al., 2015a). One quantitative study assessed the impact of endorsing microaggressions on preferences for mental health funding allocation by the general public and found a weak but significant negative correlation (DeLuca et al., 2017).
Defining the term microaggression as it is used in relation to people with mental health problems
We found that the majority (11/17) of papers directly or indirectly referenced a definition of microaggressions from the work of Sue et al. (e.g. Sue, 2010; Sue et al., 2007), and eight listed the three types of microaggression described by Sue et al.: microassaults, microinsults and microinvalidations. Ezell et al. (2018) referenced Pierce et al. (1977) and described a ‘nexus of recurrent, daily indignities, both overt and non-overt, that are directed at historically marginalised populations… which insult, degrade or otherwise demoralize their recipients’ (p. 28). Borg et al. (2009) describe ‘the things you experience every day that then add up and take their toll’ (p. 290). Three papers provided no reference but emphasised the ‘everyday’ (Harper et al., 2017) or ‘subtle’ (DeLuca et al., 2017; DeLuca et al., 2018) nature of microaggressions. There is an apparent consensus across all included studies that microaggressions are brief, everyday slights, snubs or insults, which may be subtle or ambiguous, but communicate a negative message to a target person based on their membership of a marginalised group, in this case, people with experience of mental illness.
Quality of included studies
The 12 empirical studies included in the review were assessed using the MMAT tool. Index scores are presented in Table 1. All of the qualitative studies (Gonzales et al., 2015a; Holley et al., 2016a; McCue, 2016; Peters et al., 2016; Charles et al., 2017; Harper et al., 2017) used an appropriate approach (interpretive or critical) and methods of data collection and analysis were well described and adequate. Overall, conclusions were well substantiated by data and the author's arguments were coherent. Of note, Charles et al. (2017) included a clear discussion of neutral and ambiguous findings. In general, there was an absence of reflexivity (with McCue (2016) a notable exception) or respondent validation. Three of the cross-sectional surveys used online convenience methods to sample US residents (Zurick, 2016; DeLuca et al., 2017, 2018). In one study, the recruitment system stratified based on demographic attributes resulting in gender balance and equal numbers of four age groups and regions (DeLuca et al., 2018). The other two were biased, for example, towards females. Zurick (2016) found that 36.9% of their sample reported they had a mental illness, a limitation to the study of general attitudes. All three of these surveys used validated measures and appropriate statistical techniques. One cross-sectional study used an unvalidated perceived microaggression scale (Gonzales et al., 2018). Two studies employed mixed methods (Zenga, 2018; Holley et al., 2016b), both using quantitative measures to triangulate the qualitative analyses. In both cases, there were weaknesses in the interpretation and integration of the quantitative findings, due to small sample size, reducing the quality of the study.
Discussion
The results of this scoping review have demonstrated an emerging field that is highly heterogenous methodologically. Largely in the last five years, researchers have described mental health-related microaggressions, operationalised them into scales, examined the characteristics associated with perpetration and begun to study the impact. By synthesising the results of four good quality qualitative studies and one mixed-method study, we provide an overview of the experiences people with mental illness have described as microaggressions in the literature to date.
The influence of Sue et al. from the racial microaggression field is evident; the majority of studies directly cite their definition and some authors framed their results in terms of microassualts, microinsults and microinvalidations (Peters et al., 2016; McCue, 2016; Holley et al., 2016a; Zenga, 2018). There are similarities between racial and mental health microaggressions, such as the assumption of inferiority or dangerousness (Sue et al., 2007) and the notion of questioning the validity of the perceived microaggressions. For example, one focus group participant felt a false sense of support when she won an award (Gonzales et al., 2015a). This is an example of attributional ambiguity, arguably a threat to self-esteem by making it difficult to assess one's abilities (Crocker et al., 1998).
However, the mental health literature has key differences to the wider microaggression work. The ‘perpetrators’ of microaggressions towards people with mental illness are largely family and friends and health professionals, rather than strangers or acquaintances. This follows from mental illness being an arguably more concealable potential identity compared to race, but this has particular implications for intervening to reduce mental health microaggressions. In addition, certain experiences are unique to mental illness, such as symptomizing – where ‘emotions and behaviours considered “normal” for people without mental illness are assumed to be a symptom of their mental illness’ (Gonzales et al., 2015a, p. 236).
Criticism of the wider microaggression literature has focused on boundaries of the concept, the ambiguous and contradictory nature of microaggressions and role of unexplored confounders such as personality traits (Lilienfeld, 2017). These challenges and problems are evident in the mental health literature too. Firstly, in synthesising the experiences described as microaggressions by people affected by mental health problems, we found examples that do not fit with the apparent consensus definition of microaggressions as brief, everyday forms of discrimination. For example, ‘I was arrested, I spent 8 months of my life in a cage for something I did not do’ (Gonzales et al., 2015a, p. 237). If this incarceration had anything to do with stigma or discrimination, it might be more helpfully considered an example of structural discrimination within the legal system than a microaggression. Similarly, ‘shortly before going back to work, they informed her that someone with more experience was hired’ (Zenga, 2018, p. 59) is not consistent with a subtle slight, snub or insult.
Defining what is, and what is not, a microaggression will be critical to distinguishing microaggressions from other described forms of discrimination. Currently, authors appear to be at odds as to whether the microaggression concept is new and ‘scarcely… studied or discussed’ (Gonzales et al., 2015a, p. 234), or an extension or rebranding of previously described forms of covert discrimination or forms of oppression (e.g. Holley et al., 2016a). In his book chapter, Yanos (2017) explores the relationship between microaggressions and other forms of stigmatising behaviour. To distinguish a microaggression from a ‘social rejection’ experience, Yanos describes ‘the difference between situations in which others avoid initiating a relationship with someone and situations in which others actively end a relationship’ (p. 46). He places microaggressions on a spectrum of stigmatising behaviour, at ‘the lowest level of severity’ (p. 41).
Several papers discuss the changing, contradictory and ambiguous nature of microaggressions. For example, Charles et al. (2017) reflect that ‘the nature of language and what is not recognised as a microaggression is always in flux’ (p. 420) and that ‘reaching out’ to students who disclose their mental illness could be seen as either supportive or a microaggression. ‘Symptomizing’ also presents a ‘catch-22’ situation to friends, family members and health professionals. Sleep disturbances are well recognised to be manic prodromes (Sierra et al., 2007), and a psychoeducational family intervention (including early warning signs) has been shown to improve the level of disability of patients with bipolar disorder (Fiorillo et al., 2015). Yet, one participant in Gonzales et al. (2015a) gives the following example of a microaggression: ‘…if I do a lot of activities or stay up late I'll have people call me up and say “Maybe you're manic, you stayed up really late…”’ (p. 237).
The authors of a number of the included studies suggest strategies to reduce perpetration of microaggressions and their impact. They focus on health professionals (Borg et al., 2009; Peters et al., 2016; Charles et al., 2017), institutions (Holley et al., 2016a; McCue, 2016) and the general public (DeLuca et al., 2017; DeLuca et al., 2018), and consider training and awareness campaigns. However, given the evidence that family and friends often perpetrate microaggressions, it may be useful to target interventions to closer acquaintances, for example, in family therapy. Another paper included in this study highlighted resilience as a key theme in the experience of microaggressions by peer support specialists (Zenga, 2018). Having gained confidence through recovery, one participant explained ‘she has developed empathy and compassion because she believes that they are “trying to be supportive”’ (p. 62). Given the changing, ambiguous nature of microaggressions, supporting people with mental health problems to cope with these slights, snubs and insults may be critical to reducing the impact of microaggressions. This could be done, for example, by focusing on strategies that improve self-esteem.
Limitations
There are several limitations to this scoping review. Firstly, our search strategy extended to grey literature but not grey data, which may have contained important perspectives. Secondly, we identified several studies in the screening stages that we were unable to access, despite attempts to contact the authors, which may represent a loss of valuable data.
We adopted a narrow focus for this scoping review for reasons of feasibility, including only papers that referenced mental health-related microaggressions explicitly. Widening the search to include terms such as subtle and covert discrimination might have enabled us to comment on distinguishing features (if they exist) of microaggressions in particular.
Conclusions
This scoping review has revealed a highly heterogenous body of work relating to microaggressions towards people with mental illness. The research has been heavily influenced by the work of Sue et al. in the wider microaggression literature. However, it is also embedded in the broader field of discrimination towards people with mental illness, with apparent similarities to previously described forms of subtle discrimination such as social rejection.
We have identified many challenges in this field of research, not least issues with the definition and boundaries of the concept: what is, and what is not, a microaggression needs to be clear and distinct to other forms of discriminatory behaviour. Also, some authors have asserted that the experience of microaggressions has a negative impact on people with mental illness, with little empirical evidence. Further work, including a careful examination of potential confounding personality traits, is required (as has been done in the wider mental health stigma literature, see Schibalski et al. (2017)). Indeed, placing the experience of microaggressions at the ‘lowest level of severity’ (Yanos, 2017, p. 41) of stigmatising experiences may be premature. Daily exposure to subtle forms of discrimination may, paradoxically, have a greater cumulative negative effect than other forms of blatant, unambiguous discrimination (Crocker et al., 1998).
Acknowledgements
At the time of starting this review, SB was supported by the National Institute for Health Research (NIHR) Integrated Academic Training Programme as an Academic Foundation Programme Trainee. GT is supported by the National Institute for Health Research (NIHR) Collaboration for Leadership in Applied Health Research and Care (CLAHRC) South London and by the NIHR Applied Research Centre (ARC) at King's College London NHS Foundation Trust, and the NIHR Applied Research and the NIHR Asset Global Health Unit award. The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR or the Department of Health and Social Care. GT receives support from the National Institute of Mental Health of the National Institutes of Health under award number R01MH100470 (Cobalt study). GT is supported by the UK Medical Research Council in relation to the Emilia (MR/S001255/1) and Indigo Partnership (MR/R023697/1) awards. PCG is supported by the UK Medical Research Council in relation to the Indigo Partnership (MR/R023697/1) award. SA receives support from the Economic and Social Research Council (ESRC) through the ASPIRES research project.
Appendix 1
Appendix 1.
Full search strategy
| Database | Search strategy |
|---|---|
| Medline | 1. (mental* adj5 (health* or illness* or condition* or disabilit* or disorder* or disease* or impair* or problem* or stress* or wellbeing or ‘well being’)).mp. [mp = title, abstract, original title, name of substance word, subject heading word, floating sub-heading word, keyword heading word, organism supplementary concept word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier, synonyms] 2. (psych* adj5 (health* or illness* or condition* or disabilit* or disorder* or disease* or impair* or problem* or stress* or wellbeing or ‘well being’)).mp. [mp = title, abstract, original title, name of substance word, subject heading word, floating sub-heading word, keyword heading word, organism supplementary concept word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier, synonyms] 3. exp Mental Health/ 4. exp Mental Disorders/ 5. 1 or 2 or 3 or 4 6. microaggress*.mp. [mp = title, abstract, original title, name of substance word, subject heading word, floating sub-heading word, keyword heading word, organism supplementary concept word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier, synonyms] 7. 5 and 6 |
| EMBASE | 1. (mental* adj5 (health* or illness* or condition* or disabilit* or disorder* or disease* or impair* or problem* or stress* or wellbeing or ‘well being’)).mp. [mp = title, abstract, heading word, drug trade name, original title, device manufacturer, drug manufacturer, device trade name, keyword, floating subheading word, candidate term word] 2. (psych* adj5 (health* or illness* or condition* or disabilit* or disorder* or disease* or impair* or problem* or stress* or wellbeing or ‘well being’)).mp. [mp = title, abstract, heading word, drug trade name, original title, device manufacturer, drug manufacturer, device trade name, keyword, floating subheading word, candidate term word] 3. exp mental health/ 4. exp mental disease/ 5. 1 or 2 or 3 or 4 6. microaggress*.mp. [mp = title, abstract, heading word, drug trade name, original title, device manufacturer, drug manufacturer, device trade name, keyword, floating subheading word, candidate term word] 7. 5 and 6 |
| PsycINFO | 1. (mental* adj5 (health* or illness* or condition* or disabilit* or disorder* or disease* or impair* or problem* or stress* or wellbeing or ‘well being’)).mp. [mp = title, abstract, heading word, table of contents, key concepts, original title, tests & measures, mesh] 2. (psych* adj5 (health* or illness* or condition* or disabilit* or disorder* or disease* or impair* or problem* or stress* or wellbeing or ‘well being’)).mp. [mp = title, abstract, heading word, table of contents, key concepts, original title, tests & measures, mesh] 3. exp Mental Health/ 4. exp Mental Disorders/ 5. 1 or 2 or 3 or 4 6. microaggress*.mp. [mp = title, abstract, heading word, table of contents, key concepts, original title, tests & measures, mesh] 7. 5 and 6 |
| WorldCat Dissertation database | kw: mental* and kw: adj5 and kw: health* or kw: illness* or kw: condition* or kw: disabilit* or kw: disorder* or kw: disease* or kw: impair* or kw: problem* or kw: stress* or kw: wellbeing or kw: well w being) OR (kw: psych* and kw: adj5 and kw: health* or kw: illness* or kw: condition* or kw: disabilit* or kw: disorder* or kw: disease* or kw: impair* or kw: problem* or kw: stress* or kw: wellbeing or kw: well w being) AND kw: microaggress* |
Financial support
None.
Ethical standards
We have adhered to the principles of open and transparent reporting.
Conflict of interest
None.
References
- Arksey H and O'Malley L (2005) Scoping studies: towards a methodological framework. International Journal of Social Research Methodology: Theory and Practice 8, 19–32. [Google Scholar]
- Barber S, Gronholm P, Ahuja S, Rüsch N and Thornicroft G (2019) What types of experiences are described as micro-aggressions in the literature concerning people with mental health problems? (osf.io/fstcp) (Accessed 1 August 2019).
- Borg M, Karlsson B and Kim HS (2009) User involvement in community mental health services - principles and practices. Journal of Psychiatric and Mental Health Nursing 16, 285–292. [DOI] [PubMed] [Google Scholar]
- Braun V and Clarke V (2006) Using thematic analysis in psychology. Qualitative Research in Psychology 2, 77–101. [Google Scholar]
- Charles JLK, Holley LC and Kondrat DC (2017) Addressing our own biases: social work educators’ experiences with students with mental illnesses. Social Work Education 36, 414–429. [Google Scholar]
- Cooke A, Smith D and Booth A (2012) Beyond PICO. Qualitative Health Research 22, 1435–1443. [DOI] [PubMed] [Google Scholar]
- Crocker J, Major B and Steele C (1998) Social stigma. In Gilbert DT, Fiske ST and Lindzey G (eds), The Handbook of Social Psychology, 4th Edn. New York, USA: McGraw-Hill, pp. 504–553. [Google Scholar]
- DeLuca JS, Clement T and Yanos PT (2017) Does individual stigma predict mental health funding attitudes? Toward an understanding of resource allocation and social climate. Israel Journal of Psychiatry and Related Sciences 54, 6–17. [PubMed] [Google Scholar]
- DeLuca JS, Vaccaro J, Seda J and Yanos PT (2018) Political attitudes as predictors of the multiple dimensions of mental health stigma. International Journal of Social Psychiatry 64, 459–469. [DOI] [PubMed] [Google Scholar]
- Ezell JM, Chien-Wen JC, Wall MM and Link BG (2018) Measuring recurring stigma in the lives of individuals with mental illness. Community Mental Health Journal 54, 27–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fiorillo A, Del Vecchio V, Luciano M, Sampogna G, De Rosa C, Malangone C, Volpe U, Bardicchia F, Ciampini G, Crocamo C, Iapichino S, Lampis D, Moroni A, Orlandi E, Piselli M, Pompili E, Veltro F, Carrà G and Maj M (2015) Efficacy of psychoeducational family intervention for bipolar I disorder: a controlled, multicentric, real-world study. Journal of Affective Disorders 172, 291–299. [DOI] [PubMed] [Google Scholar]
- Gattis MN and Larson A (2017) Perceived microaggressions and mental health in a sample of black youths experiencing homelessness. Social Work Research 41, 7–17. [Google Scholar]
- Gonzales L, Davidoff KC, Nadal K and Yanos PT (2015a) Microaggressions experienced by persons with mental illnesses: an exploratory study. Psychiatric Rehabilitation Journal 38, 234–241. [DOI] [PubMed] [Google Scholar]
- Gonzales L, Davidoff KC, Deluca JS and Yanos PT (2015b) The Mental Illness Microaggressions Scale-Perpetrator version (MIMS-P): reliability and validity. Psychiatry Research 229, 120–125. [DOI] [PubMed] [Google Scholar]
- Gonzales L, Yanos PT, Stefancic A, Alexander MJ and Harney-Delehanty B (2018) The role of neighborhood factors and community stigma in predicting community participation among persons with psychiatric disabilities. Psychiatric Services 69, 76–83. [DOI] [PubMed] [Google Scholar]
- Haddaway NR, Collins AM, Coughlin D and Kirk S (2015) The role of google scholar in evidence reviews and its applicability to grey literature searching. PLoS ONE 10, e0138237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harper A, Kriegel L, Morris C, Hamer HP and Gambino M (2017) Finding citizenship: what works? American Journal of Psychiatric Rehabilitation 20, 200–217. [Google Scholar]
- Holley LC and Thomas D (2018) LGBTQ people of colour with mental health conditions. In Dentato MP (ed.), Social Work Practice with the LGBTQ Community: The Intersection of History, Health, Mental Health and Policy Factors. Oxford, UK: Oxford University Press, pp. 430–451. [Google Scholar]
- Holley LC, Mendoza NS, Del-Colle MM and Bernard ML (2016a) Heterosexism, racism, and mental illness discrimination: experiences of people with mental health conditions and their families. Journal of Gay & Lesbian Social Services 22, 93–116. [Google Scholar]
- Holley LC, Tavassoli KY and Stromwall LK (2016b) Mental illness discrimination in mental health treatment programs: intersections of race, ethnicity, and sexual orientation. Community Mental Health Journal 52, 311–322. [DOI] [PubMed] [Google Scholar]
- Hong QN, Pluye P, Fàbregues S, Bartlett G, Boardman F, Cargo M, Dagenais P, Gagnon M-P, Griffiths F, Nicolau B, O'Cathain A, Rousseau M-C and Vedel I (2018) Mixed Methods Appraisal Tool (MMAT), version 2018. Registration of Copyright (#1148552), Canadian Intellectual Property Office, Industry Canada.
- Levac D, Colquhoun H and O'Brien KK (2010) Scoping studies: advancing the methodology. Implementation Science 5, 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lilienfeld SO (2017) Microaggressions: strong claims, inadequate evidence. Perspectives on Psychological Science 12, 138–169. [DOI] [PubMed] [Google Scholar]
- McCue MJ (2016) An Ecological Systems Approach to Understanding The Lived Experience of Law Students with Mental Illness. Michigan, USA: Michigan State University. [Google Scholar]
- Meyer I (1995) Minority stress and mental health in gay men. Journal of Health and Social Behaviour 36, 38–56. [PubMed] [Google Scholar]
- Moher D, Liberati A, Tetzlaff J and Altman DG (2009) Preferred Reporting Items for Systematic Reviews and Meta-Analyses: the PRISMA statement. Annals of Internal Medicine 151, 264–269. [DOI] [PubMed] [Google Scholar]
- Munn Z, Peters MDJ, Stern C, Tufanaru C, McArthur A and Aromataris E (2018) Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Medical Research Methodology 18, 1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nadal KL, Griffin KE, Wong Y, Hamit S and Rasmus M (2014) The impact of racial microaggressions on mental health: counseling implications for clients of color. Journal of Counseling and Development 92, 57–66. [Google Scholar]
- Peters HJ, Schwenk HN, Ahlstrom ZR and Mcialwain LN (2016) Microaggressions: the experience of individuals with mental illness. Counselling Psychology Quarterly 30, 86–112. [Google Scholar]
- Pierce CM (1970) Black psychiatry one year after Miami. Journal of the National Medical Association 62, 461–473. [PMC free article] [PubMed] [Google Scholar]
- Pierce CM, Carew JV, Pierce-Gonzalez D and Wills D (1977) An experiment in racism: TV commercials. Education and Urban Society 10, 61–87. [Google Scholar]
- Reid E (2017) How Racial Microaggressions Impact the Mental Health of Black Women of Different Occupational Prestige. Boston, USA: University of Massachusetts. [Google Scholar]
- Schibalski JV, Müller M, Ajdacic-Gross V, Vetter S, Rodgers S, Oexle N, Corrigan PW, Rössler W and Rüsch N (2017) Stigma-related stress, shame and avoidant coping reactions among members of the general population with elevated symptom levels. Comprehensive Psychiatry 74, 224–230. [DOI] [PubMed] [Google Scholar]
- Sierra P, Livianos L, Arques S, Castelló J and Rojo L (2007) Prodromal symptoms to relapse in bipolar disorder. Australian & New Zealand Journal of Psychiatry 41, 385–391. [DOI] [PubMed] [Google Scholar]
- Sue DW (2010) Microaggressions and Marginality: Manifestation, Dynamics, and Impact. New Jersey, USA: John Wiley & Sons. [Google Scholar]
- Sue D, Capodilupo CM, Torino GC, Bucceri JM, Holder AMB, Nadal KL and Esquilin M (2007) Racial microaggressions in everyday life implications for clinical practice. American Psychologist 62, 271–286. [DOI] [PubMed] [Google Scholar]
- Thomas J and Harden A (2008) Methods for the thematic synthesis of qualitative research in systematic reviews. BMC Medical Research Methodology 8, 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thornicroft G (2006) Shunned: Discrimination Against People with Mental Illness. Oxford, UK: Oxford University Press. [Google Scholar]
- Torres L, Driscoll MW and Burrow AL (2010) Microaggressions and psychological functioning among high achieving African-Americans: a mixed-methods approach. Journal of Social and Clinical Psychology 29, 1074–1099. [Google Scholar]
- Yanos PT (2017) Written Off: Mental Health Stigma and the Loss of Human Potential. Cambridge, UK: Cambridge University Press. [Google Scholar]
- Zenga D (2018) Perceived Effects of Microaggressions on Peer Support Workers in Mental Health Recovery. San Diego, USA: Alliant International University. [Google Scholar]
- Zurick S (2016) The Relationship Among Mental Illness Microaggressions, Level of Contact, and Prejudicial Beliefs. Edwardsville, USA: Southern Illinois University. [Google Scholar]