The primary objective of preparticipation cardiovascular evaluation (PPCE) in young athletes is to detect asymptomatic individuals with cardiovascular disease (CVD) at risk of sudden cardiac death (SCD).1 The optimal protocol, including the ideal age to start screening and whether PPCE should be repeated on a regular basis, remains unclear and lacks evidence. The current study was designed to evaluate the diagnostic yield and outcomes of serial (annual) versus single (initial) PPCE to screen adolescent athletes for CVDs at risk of SCD. The study was approved by the local ethics committee, and no consent was required because of the observational study design. The study data are available from the corresponding author on reasonable request.
The study population included a consecutive series of competitive athletes age 12 to 18 years who underwent PPCE, which according to Italian law is mandatory and based on yearly evaluations, at the Center for Sports Medicine of Treviso (Veneto region of Italy), from 2009 to 2019. The screening protocol included personal and family history questionnaire, physical examination, resting 12-lead ECG, and limited stress testing for evaluation of exertional ventricular arrhythmias.2,3 This latter test was performed using a bicycle with constant-load increases (ie, 2 W/Kg in female participants and 3 W/Kg in male participants) for 3 minutes or until 85% or more of maximal heart rate was achieved, plus 3 minutes of postexercise monitoring.3 Athletes with a positive medical history and abnormal physical examination, ECG, or stress test underwent further investigations. The diagnostic yield of the initial screening session was compared with that of repeat PPCEs. Athletes with a definitive diagnosis of CVD at risk of SCD were considered ineligible for competitive sports, although they received a tailored program for leisure physical activity and were enrolled in a yearly follow-up program. Outcome data of screened athletes, either eligible or ineligible to play competitive sports, were obtained from office visits, hospital records, or interrogation of the Registry of Juvenile SCD of the Veneto region.
The study population included 15 127 consecutive athletes (64% male, 96% White) who underwent a total of 53 396 annual PPCEs (mean 3.7 per athlete) over the 11-year study period. The median age at first screening was 13 years (interquartile range [IQR], 12 to 14). Additional investigations were prescribed after 5389 (10.1%) first-line evaluations and mainly included echocardiography (n=5042 [9.4%]), 24-hour Holter monitoring (n=4463 [8.4%]), maximal exercise testing (n=2460 [4.6%]), and cardiac magnetic resonance (n=115 [0.2%]). Reasons for additional investigations included positive family history (2.4%), abnormal physical examination (0.9%), ECG abnormalities (3.1%), or exertional arrhythmias (5.5%). Sixty-three athletes (65% male) were diagnosed with a CVD at risk of SCD such as congenital heart disease (n=17), ion channel disease (n=11), inherited cardiomyopathy (n=13), isolated nonischemic left ventricular scar (NLVS) with ventricular arrhythmias (n=18), or other (n=4); 266 athletes had cardiac conditions not associated with SCD (Figure [A] and [B]). Seventeen of the 63 athletes (27%) with at-risk CVD had a positive family history, symptoms, or abnormal physical examination, 38 (60%) had ECG abnormalities, and 32 (51%) developed arrhythmias on limited exercise testing. The median age at diagnosis of cardiomyopathies and isolated NLVS with ventricular arrhythmias was significantly higher (15 years [IQR, 14 to 17]) than that of congenital heart diseases and long QT syndrome (14 years [IQR, 12–15]; P=0.016) (Figure [C]). At-risk CVDs were diagnosed at the initial screening evaluation in 22 (35%) athletes (68% male; median age 15 years [IQR, 13 to 15]) and on repeat cardiovascular evaluations in 41 (65% [61% male]; median age 15 years [IQR, 14 to 17]; Figure [D]). CVDs more frequently identified on repeat evaluation included inherited cardiomyopathies (7/11 [64%]), NLVS with ventricular arrhythmias (15/18 [83%]), and long QT syndrome (7/11 [64%]). All athletes with at-risk CVD were judged ineligible to play competitive sports. During a mean follow-up of 6.7±3.5 years, 1 athlete with a negative PPCE experienced an episode of aborted SCD attributable to ventricular fibrillation that remained unexplained after a comprehensive diagnostic workup (event rate, 0.98/100 000 athletes per year).
Figure.
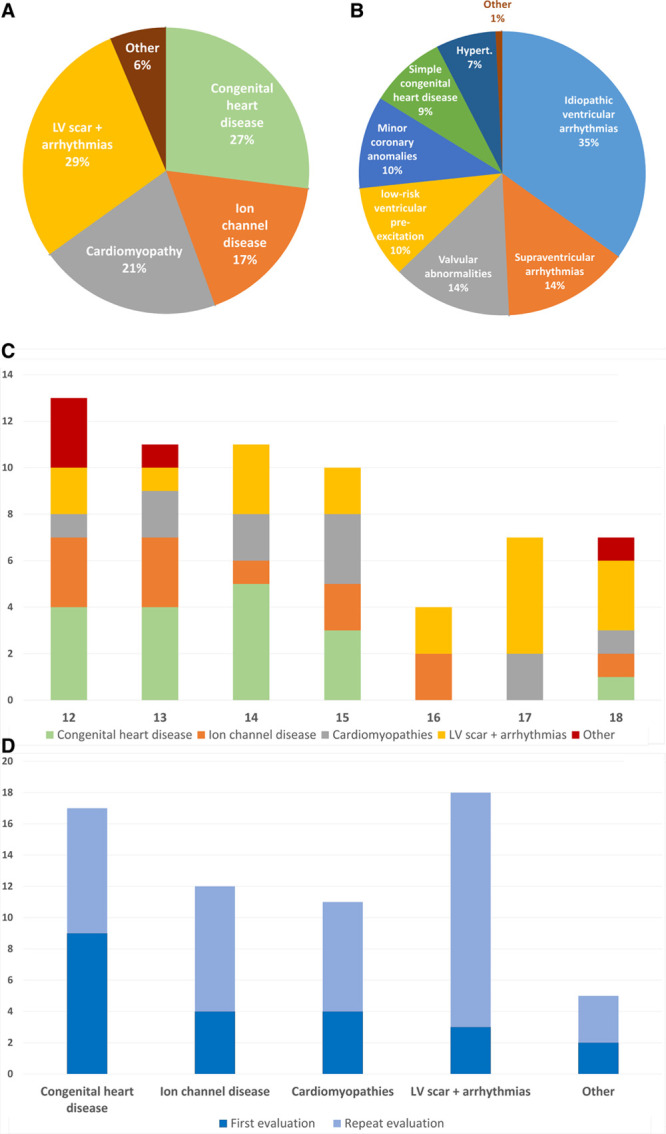
Diagnoses of cardiovascular diseases at preparticipation cardiovascular screening. A, Pie chart shows the distribution of the 63 diagnoses of cardiovascular diseases at risk of sudden cardiac death (SCD). B, Pie chart shows the distribution of the 266 diagnoses of cardiac conditions not associated with SCD. C, Bar graph shows the distribution of diagnoses of cardiovascular diseases at risk of SCD according to the athlete’s age. Athletes with inherited cardiomyopathies and isolated nonischemic left ventricular scar with ventricular arrhythmias were significantly older at the time of diagnosis by preparticipation screening than those with congenital heart diseases and long QT syndrome. D, Bar graph shows the distribution of diagnoses of cardiovascular diseases at risk of SCD according to the preparticipation cardiovascular evaluations. Sixty-five percent of diagnoses of a cardiovascular disease at risk of SCD were made on repeat screening. More frequently identified by serial evaluations were inherited cardiomyopathies (64%) with a late phenotypic expression and acquired nonischemic left ventricular scar with ventricular arrhythmias (83%) that newly developed over follow-up. LV indicates left ventricular.
These results show that annual cardiovascular screening of adolescent athletes increased by 3 times the diagnostic yield of CVD at risk of SCD compared with a once-only (initial) evaluation. Inherited cardiomyopathies and isolated NLVS with ventricular arrhythmias were the CVDs more frequently identified on repeat evaluation. The study findings demonstrate that more CVDs at risk of SCD will be diagnosed with serial screening in young athletes. Serial PPCEs increase the detection of both genetic cardiomyopathies with a late-onset phenotype during adolescence and newly acquired heart muscle diseases, such as isolated NLVS, whose clinical features are absent at the initial screening and develop over follow-up. A NLVS was most frequently suspected in asymptomatic adolescents on the basis of ventricular arrhythmias induced by limited exercise testing, which led to a deeper investigation by cardiac magnetic resonance.3,4 The low incidence of cardiac arrest during follow-up is in agreement with the substantially reduced SCD rate (<1/100 000 athletes per year) that was reported previously among competitive athletes of the Veneto region after 2 decades (1982 through 2004) of systematic screening.5
Disclosures
None.
Footnotes
Contributor Information
Patrizio Sarto, Email: patrizio.sarto@aulss2.veneto.it.
Alessandro Zorzi, Email: alessandropatti88@gmail.com.
Laura Merlo, Email: laura.merlo@aulss2.veneto.it.
Teresina Vessella, Email: teresina.vessella@aulss2.veneto.it.
Cinzia Pegoraro, Email: cinzia.pegoraro1@aulss2.veneto.it.
Flaviano Giorgiano, Email: flaviano.giorgiano@aulss2.veneto.it.
Alessandro Patti, Email: alessandropatti88@gmail.com.
Martino Crosato, Email: martino.crosato@aulss2.veneto.it.
Gaetano Thiene, Email: gaetano.thiene@unipd.it.
Jonathan A. Drezner, Email: jdrezner@uw.edu.
Cristina Basso, Email: cristina.basso@unipd.it.
References
- 1.Corrado D, Basso C, Schiavon M, Thiene G. Screening for hypertrophic cardiomyopathy in young athletes. N Engl J Med. 1998; 339:364–369. doi: 10.1056/NEJM199808063390602 [DOI] [PubMed] [Google Scholar]
- 2.Corrado D, Pelliccia A, Bjørnstad HH, Vanhees L, Biffi A, Borjesson M, Panhuyzen-Goedkoop N, Deligiannis A, Solberg E, Dugmore D, et al. ; Study Group of Sport Cardiology of the Working Group of Cardiac Rehabilitation and Exercise Physiology and the Working Group of Myocardial and Pericardial Diseases of the European Society of Cardiology. Cardiovascular pre-participation screening of young competitive athletes for prevention of sudden death: proposal for a common European protocol: consensus statement of the study group of sport cardiology of the working group of cardiac rehabilitation and exercise physiology and the working group of myocardial and pericardial diseases of the European Society of Cardiology. Eur Heart J. 2005; 26:516–524. doi: 10.1093/eurheartj/ehi108 [DOI] [PubMed] [Google Scholar]
- 3.Zorzi A, Vessella T, De Lazzari M, Cipriani A, Menegon V, Sarto G, Spagnol R, Merlo L, Pegoraro C, Marra MP, et al. Screening young athletes for diseases at risk of sudden cardiac death: role of stress testing for ventricular arrhythmias. Eur J Prev Cardiol. 2020; 27:311–320. doi: 10.1177/2047487319890973 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zorzi A, Perazzolo Marra M, Rigato I, De Lazzari M, Susana A, Niero A, Pilichou K, Migliore F, Rizzo S, Giorgi B, et al. Nonischemic left ventricular scar as a substrate of life-threatening ventricular arrhythmias and sudden cardiac death in competitive athletes. Circ Arrhythm Electrophysiol. 2016; 9:e004229. doi: 10.1161/CIRCEP.116.004229 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Corrado D, Basso C, Pavei A, Michieli P, Schiavon M, Thiene G. Trends in sudden cardiovascular death in young competitive athletes after implementation of a preparticipation screening program. JAMA. 2006; 296:1593–1601. doi: 10.1001/jama.296.13.1593 [DOI] [PubMed] [Google Scholar]


