Abstract
Background
Regular stair climbing has the potential to lower the risk of premature death, but current evidence is scarce. We aimed to examine whether daily stair climbing is associated with lower risk of all‐cause, cancer, and cardiovascular disease (CVD) mortality.
Methods
Using the UK Biobank cohort, we extracted information of self‐reported daily flights of stairs climbed at home, categorized as none, 1 to 5, 6 to 10, 11 to 15, and ≥16 flights per day. Associations between flights of stair climbed per day and mortality were examined as hazard ratios (HRs) from Cox proportional hazards models adjusted for demographic, clinical, and behavioural covariates including time spent in other physical activities. We calculated the restricted mean survival time as an absolute measure of association. The risk of residual confounding was examined using propensity score matching and by using lung cancer as negative control outcome. Participants were followed from baseline (2006–2010) through 31 March 2020.
Results
A total of 280 423 participants (median follow‐up 11.1 years, during which 9445 deaths occurred) were included. Compared with not climbing any stairs, climbing more than five flights of stairs at home per day was associated with lower risk of premature mortality. The lowest risk was found for those climbing 6–10 flights per day: 0.91; 95% confidence interval (CI): 0.85, 0.98, translated to approximately 44 to 55 days of additional survival. A similar pattern was found after applying propensity score matching and for cancer mortality (6–10 flights per day HR: 0.88; 95% CI: 0.80, 0.97), but not for CVD mortality (6–10 flights per day HR: 1.08; 95% CI: 0.91, 1.29). The association between stair climbing and lung cancer was similar to that of all‐cause mortality.
Conclusions
Climbing more than five flights of stairs at home per day was associated with a lower risk of all‐cause and cancer mortality, but not CVD mortality, compared with those who did not take the stairs. The magnitude of the association was small and appeared susceptible to residual confounding. It is unlikely that at‐home stair climbing is sufficient physical activity stimuli to lower the risk of premature mortality.
Keywords: stair walking, physical activity, mortality, epidemiology
Introduction
Worldwide, one in four adults does not meet the recommended level of physical activity. 1 This is problematic as insufficient physical activity is a major cause of non‐communicable chronic disease, responsible for more than three million premature deaths per year worldwide in addition to enormous economic cost for societies. 2 , 3
High intensity physical activity has unique health benefits over and above lighter intensities 4 and is a time‐efficient way to improve vital cardiometabolic health outcomes. 5 As such, integration of small bursts of high‐intensity physical activity into daily life may provide a feasible and effective opportunity to improve population health, particularly among those unable to achieve the current physical activity recommendations.
To many people, stair climbing is a common incidental physical activity. In older or inactive individuals, stair climbing may require a substantial effort and can also be considered a muscle‐strengthening activity. 6 There is evidence that structured relatively short bouts of stair climbing (as few as three 20 s long bouts reaching >85% of maximal heart rate on 3 days per week) may be sufficient stimuli to improve markers of cardiometabolic risk, including cardiorespiratory fitness and aerobic power, in sedentary young adults, within only 6 weeks. 7 , 8 , 9 , 10 Such effects are promising, considering that as little as 10% increase in cardiorespiratory fitness is associated with up to 25% reduction in incident cardiovascular disease (CVD) risk in people with low cardiorespiratory fitness. 11 Unfortunately, compared with other types of physical activity, the association of stair climbing with mortality risk has been less explored. 6 Results from previous studies suggest that regular stair climbing is associated with lower risk of death. 12 , 13 , 14 Nevertheless, previous body of evidence are either based on small and selected samples of highly educated men from higher socioeconomic backgrounds, which may have limited generalisability, or have included people with chronic diseases, which may introduce reverse causality bias. 15 Therefore, studies that include larger and demographically diverse samples with rigorous procedures to account for confounding and other biases are needed to determine if stair climbing as a form of physical activity is a sufficient stimulus to lower the risk of premature death. Further, it is unknown if stair climbing lowers the risk of cause specific death, such as cancer and CVD mortality.
To address the above‐identified gaps, we leveraged the potential of the UK Biobank study, a large population‐based cohort. The purpose of this study is to examine whether daily stair climbing is associated with lower risk of all‐cause, cancer, and CVD mortality.
Methods
Data source and study population
We used data from the UK Biobank, a population‐based cohort study designed to investigate the interrelations between environment, lifestyle and genes, and to improve the prevention, diagnosis and treatment of chronic diseases (application number 29717). 16 A total of 502 493 participants (about 5.5% of those invited), aged 37–82 years, were recruited between 2006 and 2010 via 22 assessment centres across England, Wales and Scotland. Participants gave written informed consent in the assessment centres prior to data collection, which included a touch‐screen questionnaire, a large array of physical measurements, biological sampling and linkage with electronic registries. Ethical approval was obtained by the North‐West Research Ethics Committee. The full details of the protocol are available elsewhere. 17
Measures
Stair climbing
Stair climbing was assessed by asking the participants the following question (touchscreen questionnaire): ‘At home, during the last 4 weeks, about how many times a DAY do you climb a flight of stairs? (approximately 10 steps)’. Possible answers were none, 1–5 times a day, 6–10 times a day, 11–15 times a day, 16–20 times a day, or more than 20 times a day. Due to few cases in the upper response options, we combined ≥16 times a day into one category. All individuals with no information on stair climbing (n = 9598) were excluded. Detailed information of the inclusion and exclusion process is shown in the supporting information Figure S1. Long‐term reliability of stair climbing was assessed in a sub‐sample with data from the UK Biobank repeated assessment (mean 4.2 years after baseline). Using a quadratic weighed kappa, we estimated low‐to‐moderate reliability (kappa coefficient of 0.62; refer to Table S2 for cross‐tabulation).
Outcome
Date of death was obtained from death certificates held by the National Health Service Information Centre for participants (England and Wales) and the National Health Service Central Register Scotland (Scotland). Person‐years were calculated from the date attending the assessment centre to the date of death, emigration, loss to follow‐up, or 31 March 2020, whichever came first.
Covariates
Height and weight were measured during the initial visit to the assessment centre by trained clinical staff following standardized protocols. Thereafter, body mass index (BMI) was calculated as weight (kg)/height(m)2 and categorized following the World Health Organization's criteria 18 into underweight (<18.5 kg/m2), normal weight (18.5–24.9 kg/m2), overweight (25.0–29.9 kg/m2), and obese (≥30 kg/m2).
Self‐reported sociodemographic characteristics included ethnicity (White, Asian, Black, others, or mixed background), education (no qualifications, qualification apart from college or university degree, or college or university degree), marital status (living with partner or not living with partner), employment status (employed or not employed), type of accommodation (living in house/bungalow or flat/maisonette/apartment), and average annual household income before tax (<£18 000, £18 000–51 999, >£52 000, or missing). The Townsend score was used as a marker of area‐based socioeconomic status 19 and analysed as a continuous variable.
Lifestyle covariates were also self‐reported. Physical activity was assessed using an adapted version of the International Physical Activity Short Form questionnaire. 20 The participants reported the frequency and duration of walking, moderate, and vigorous intensity physical activity lasting for more than 10 min in a typical week. Therefore, the information contained in this covariate did not overlap daily at‐home stair climbing (more detailed information is shown in the supporting information). A dietary pattern covariate was created based on meeting at least two out of three healthy eating targets: (i) ≤ 3 weekly servings of red meat and ≤1 servings per week of processed meat; (ii) ≥2 servings per week of fish including at least one with oily fish; (iii) ≥5 servings per day of fruits and vegetables. 21 In addition, we adjusted for frequency of adding salt after cooking (never, sometimes, usually, and always) as another marker for healthy eating habits, alcohol intake (never, previous, current and <3 times per week, and current and ≥3 times per week) and smoking (never, previous, and current smoker). We also adjusted for leisure‐time screen use by summing the reported time spent watching TV and using a computer outside of work (<2, 2–3, 3–4, 4–5, and >5 h/day), 22 and for self‐reported walking pace (<3 miles/h defined as slow; 3 to 4 miles/h as average, and >4 miles/h as brisk) as a marker for fragility.
Baseline health status (presence of longstanding illness, disability or infirmity, history of depression, diabetes, hypertension, and statins medication) was extracted from a combination of self‐report, verbal interview with a trained nurse, and hospital records. 17 We used clinical measurements of blood pressure (systolic blood pressure ≥140 or diastolic blood pressure ≥90) and HbA1c (≥48 mmol/L) in combination with the hospital records to identify potentially undiagnosed hypertensive and diabetic patients, respectively.
Individuals with missing covariates were excluded from the analysis, as well as those reporting >24 h/day of the combination of walking, moderate‐to‐vigorous physical activity, sleep time (missing values replaced with 8 h/day) and total screen time (n = 136 645). Detailed information regarding variable extraction and recoding is given in Table S1.
Statistical analyses
We analysed the associations between categories of daily stair climbing at home and all‐cause mortality using Cox‐proportional hazard regression model adjusted for the covariates described above. We verified the proportional hazards assumption of the models by visual inspection of log–log plots. Associations between stair climbing and all‐cause mortality were also analysed by calculating the restricted mean survival time (RMST), using flexible parametric survival models (Royston–Parmar models, stpm2 package for Stata 16 (StataCorp LP, College Station, TX, USA), adjusted for the same set of covariates. In addition, we used propensity score matching as an alternative to the multivariable adjustment. Propensity score matching can reduce bias by creating a sample in which confounding factors are balanced between ‘treatment groups’. 23 This was performed by creating two categories of stair climbing (less or ≥6 flights per day) and using propensity score matching to exclude non‐matched participants based on the set of covariates, applying a 1‐to‐2 ratio and a calliper of 0.2 24 (excluding n = 9096 participants and 406 deaths). Thereafter, we used Cox's regression to analyse the hazard ratios (HRs) using <6 flights per day as the referent category.
To minimize potential influence of reverse causality (i.e. cases in which inability to take the stairs may represent disease severity), we excluded participants reporting poor self‐perceived health, those who were unable to walk, or required attendance, disability, or mobility allowance and those who lived in mobile or temporary structures, sheltered accommodation, or care homes (n = 23 667). We also excluded all participants reporting any prevalent chronic neurological degenerative problems, chronic widespread pain, chronic respiratory diseases (including chronic obstructive pulmonary disease), liver failure or cirrhosis, psychological or psychiatric problems, substance abuse or dependency and eating disorders, as well as those with a BMI < 18.5 kg/m2 and pregnant women at baseline (n = 14 290). Additionally, participants with prevalent cancer (excluding non‐melanoma skin cancer) or CVD, identified from self‐report or flagged in hospital records, were excluded prior to analysis (n = 37 182). Finally, follow‐up was commenced 2 years after baseline (excluding 688 participants).
To examine the robustness of the results, we repeated the analysis stratified by sex, age (under and over 60 years old), BMI, walking pace (as a potential marker of frailty not accounted for through restrictions or multivariable‐adjustment), 25 education, employment, and type of accommodation. In addition, we examined interactions between flights per day and these subgroups using a likelihood‐ratio test.
The association between frequency of stair climbing and cause‐specific mortality (CVD and cancer) was also analysed accounting for competing risks using the sub‐distribution method of Fine and Gray. 26 For CVD mortality, we treated all other causes of death as competing events with all non‐cancer deaths treated as competing events when cancer‐related mortality was the outcome.
Finally, in order to examine possible residual confounding, we repeated the analysis using lung‐cancer mortality as a negative control outcome (i.e. an outcome that is not plausibly affected by stair climbing, but shares the same confounding structure or sources of bias). 27 We consider lung cancer an appropriate negative control outcome based on the following reasons: (i) the association with physical activity appears highly susceptible to smoking‐related confounding 28 ; (ii) there is no evidence of an association in never smokers 29 ; (iii) the associations in previous research between physical activity and lung cancer is established at much higher physical activity contrasts (e.g. 10th vs. 90th percentiles of leisure‐time physical activity) 30 than those produced by the stair‐climbing categories; and (iv) because lung cancer and stair climbing may share a similar confounding structure with socioeconomic factors (i.e. at‐home stair climbing being a marker of living circumstances).
We performed all analyses using statistical software Stata 16 (StataCorp LP).
Results
A total of 280 423 participants (mean age ± SD = 56.0 ± 8.1; range 38.9–73.7; 51.7% women) were included in the analysis (Table 1). Median follow‐up time was 11.1 years, during which 9445 deaths occurred (3 090 104 person‐years).
Table 1.
Characteristics of included participants (n = 280 423) by strata of flights of stairs climbed per day
| None (n = 20 226) | 1–5 (n = 52 190) | 6–10 (n = 106 396) | 11–15 (n = 56 001) | ≥16 (n = 45 610) | |
|---|---|---|---|---|---|
| Age (years), mean (SD) | 58.8 (7.8) | 55.5 (7.9) | 55.9 (8.0) | 55.9 (8.2) | 55.7 (8.2) |
| Age sub‐groups (years old) | |||||
| <60 | 46.1 | 66.2 | 63.0 | 61.6 | 62.2 |
| ≥60 | 53.9 | 33.8 | 37.0 | 38.4 | 37.8 |
| Sociodemographic variables | |||||
| Ethnicity | |||||
| White | 96.4 | 93.8 | 96.0 | 96.5 | 95.6 |
| Asian | 1.1 | 2.6 | 1.7 | 1.4 | 1.8 |
| Black | 1.2 | 1.9 | 1.2 | 1.0 | 1.2 |
| Others/mixed background | 1.3 | 1.7 | 1.1 | 1.1 | 1.3 |
| Townsend Deprivation Index, mean (SD) | 2.1 (1.4) | 1.9 (1.4) | 2.2 (1.4) | 2.2 (1.4) | 2.2 (1.4) |
| Education | |||||
| No qualifications | 19.9 | 12.7 | 10.5 | 9.2 | 9.3 |
| Not college/university degree | 52.1 | 50.9 | 50.9 | 49.3 | 47.7 |
| University degree | 28.0 | 36.4 | 38.5 | 41.5 | 42.9 |
| Marital status, living with partner | 65.5 | 68.3 | 77.5 | 79.4 | 80.1 |
| Currently employed | 50.4 | 72.7 | 67.9 | 62.7 | 60.5 |
| Type of accommodation lived in | |||||
| House or bungalow | 71.7 | 79.2 | 95.7 | 97.4 | 97.0 |
| Flat, maisonette, or apartment | 28.3 | 20.8 | 4.3 | 2.6 | 3.0 |
| Household income before tax | |||||
| <£18 000 | 25.6 | 16.1 | 13.1 | 12.6 | 13.0 |
| £18 000–51 999 | 47.9 | 47.6 | 47.9 | 48.3 | 46.1 |
| >£52 000 | 15.3 | 27.7 | 30.1 | 30.3 | 31.0 |
| Those with missing data | 11.3 | 8.6 | 8.8 | 8.9 | 10.0 |
| Lifestyle covariates | |||||
| Total PA (MET‐minutes/week), mean (SD) | 2782.4 (2711.0) | 2380.7 (2531.7) | 2540.7 (2519.7) | 2748.8 (2584.4) | 3245.9 (2874.2) |
| Diet pattern, meeting 2 targets | 70.0 | 65.2 | 68.8 | 72.2 | 74.4 |
| Salt intake | |||||
| Never/rarely | 56.3 | 55.3 | 57.2 | 58.3 | 59.1 |
| Sometimes | 27.0 | 28.3 | 27.8 | 27.5 | 26.8 |
| Usually | 12.0 | 11.9 | 11.2 | 10.8 | 10.3 |
| Always | 4.7 | 4.6 | 3.8 | 3.3 | 3.8 |
| Alcohol intake | |||||
| Never | 4.1 | 3.9 | 3.0 | 2.9 | 3.2 |
| Previous | 3.2 | 2.7 | 2.2 | 2.1 | 2.5 |
| Current, <3 times per week | 48.3 | 49.4 | 46.4 | 44.7 | 43.9 |
| Current, ≥3 times per week | 44.4 | 44.0 | 48.4 | 50.3 | 50.4 |
| Smoking status | |||||
| Never | 53.3 | 55.1 | 57.8 | 58.8 | 60.2 |
| Previous | 36.4 | 34.1 | 33.7 | 33.4 | 32.2 |
| Current | 10.2 | 10.8 | 8.6 | 7.8 | 7.7 |
| Screen time (h/day) | |||||
| <2 | 9.8 | 12.0 | 12.2 | 12.8 | 14.1 |
| 2–3 | 17.1 | 18.9 | 19.9 | 19.8 | 20.3 |
| 3–4 | 21.8 | 22.8 | 23.3 | 23.3 | 22.3 |
| 4–5 | 20.7 | 19.3 | 18.9 | 18.8 | 18.2 |
| >5 | 30.6 | 27.0 | 25.6 | 25.3 | 25.2 |
| Health‐related covariates | |||||
| BMI (kg/m2), mean (SD) | 27.4 (4.5) | 27.8 (4.8) | 27.1 (4.4) | 26.6 (4.1) | 26.2 (4.0) |
| BMI categories (kg/m2) | |||||
| 18.5–24.9 | 31.9 | 30.0 | 34.1 | 38.5 | 42.5 |
| 25–29.9 | 44.8 | 43.4 | 44.4 | 43.9 | 42.3 |
| ≥30 | 23.3 | 26.6 | 21.5 | 17.6 | 15.2 |
| Usual walking pace | |||||
| Slow | 4.4 | 5.0 | 2.9 | 2.1 | 1.7 |
| Steady average | 54.3 | 55.9 | 52.8 | 48.5 | 43.5 |
| Fast | 41.2 | 39.1 | 44.3 | 49.5 | 54.7 |
| History of depression | 4.8 | 4.9 | 4.3 | 4.1 | 4.1 |
| Diabetes | 5.4 | 5.1 | 3.9 | 3.3 | 3.0 |
| Hypertension | 58.5 | 52.4 | 51.4 | 49.4 | 48.7 |
| Taking statins medication | 14.8 | 11.4 | 10.8 | 10.3 | 9.5 |
| Longstanding illness, disability, or infirmity | 26.0 | 24.1 | 21.8 | 21.1 | 20.5 |
BMI, body mass index; MET, metabolic equivalent; PA, physical activity.
Values are percentages unless stated otherwise. Dietary pattern is based on meeting at least two out of three healthy eating targets related to food types: (i) ≤3 weekly servings of red meat and ≤1 servings per week of processed meat; (ii) ≥2 servings per week of fish including at least one with oily fish; (iii) ≥5 servings per day of fruits and vegetables.
Table 2 shows the associations between stair climbing and all‐cause, cancer, and CVD mortality. Compared with the reference (no stair climbing), no association was found for climbing 1–5 flights of stairs/day but climbing more than 5 flights/day was associated with a 10 to 12% lower risk of all‐cause mortality. In analyses of RMST differences, this translated to approximately 44 to 55 days of additional survival. Results were consistent for cancer‐related mortality, but stair climbing was not associated with lower risk of CVD mortality. We show the analysis with adjustment for only age and sex in Table S3. After excluding non‐matched participants based on propensity score matching, a 9% risk reduction was still found for all‐cause mortality (HR = 0.91; 95% CI: 0.87, 0.95) for those climbing more than five flights per day compared with those climbing less.
Table 2.
Associations of all‐cause, cancer, and cardiovascular disease mortality with flights of stairs climbed per day
| Flights of stairs (around 10) climbed per day | |||||
|---|---|---|---|---|---|
| None (n = 20 226) | 1–5 (n = 52 190) | 6–10 (n = 106 396) | 11–15 (n = 56 001) | ≥16 (n = 45 610) | |
| All‐cause mortality | |||||
| Hazard ratio (95% CI) | 1 (reference) | 1.01 (0.94, 1.10) | 0.91 (0.85, 0.98) | 0.92 (0.85, 0.99) | 0.93 (0.86, 1.02) |
| RMSTD, days (95% CI) | (reference) | −27.43 (−97.14, 42.28) | 45.73 (−0.62, 92.08) | 55.79 (−8.54, 120.12) | 41.77 (−30.30, 113.85) |
| Deaths | 1018 | 1967 | 3385 | 1714 | 1361 |
| Cancer mortality | |||||
| Hazard ratio (95% CI) | 1 (reference) | 0.99 (0.90, 1.10) | 0.88 (0.80, 0.97) | 0.91 (0.82, 1.01) | 0.92 (0.82, 1.02) |
| RMSTD, days (95% CI) | (reference) | −25.47 (−76.90, 25.95) | 19.93 (−14.94, 54.80) | 22.52 (−25.77, 70.82) | 8.14 (−46.26, 62.53) |
| Deaths | 590 | 1158 | 2039 | 1068 | 848 |
| CVD mortality | |||||
| Hazard ratio (95% CI) | 1 (reference) | 1.14 (0.95, 1.37) | 1.08 (0.91, 1.29) | 1.05 (0.86, 1.28) | 1.04 (0.84, 1.28) |
| RMSTD, days (95% CI) | (reference) | −11.21 (−47.09, 24.67) | −1.29 (−27.72, 25.14) | −8.04 (−46.84, 30.75) | −1.04 (−42.71, 40.62) |
| Deaths | 167 | 365 | 622 | 295 | 228 |
CI, confidence Interval; CVD, cardiovascular disease; RMSTD, restricted mean survival time difference.
The analysis was adjusted for age, sex, ethnicity, type of accommodation (house/flat), Townsend deprivation index, education, marital status, employment, total annual income before tax, physical activity, diet pattern, salt consumption, screen time, smoking, alcohol, body mass index, walking pace, depression, diabetes, hypertension, use of statins and longstanding illness, disability, or infirmity.
The associations between flights of stairs climbed per day and all‐cause mortality in strata of sex, age, BMI and walking pace are presented in Figure 1. The results stratified by education, employment status, and type of accommodation are presented in Figure 2. Sex stratified analyses showed that the association did not reach statistical significance in women, albeit associations were similar in magnitude as those observed when restricted to men. The pattern of associations was broadly similar across strata of BMI, age‐category (refer to Table S4 for the results of the analysis stratified by 35–49, 50–59, and ≥60 age categories), and walking pace with maximal risk reductions of about 10–15%, albeit with some variation. No association was observed with 1–5 flights per day, and generally, there was no further risk reduction above 6–10 flights per day. A particularly strong association was observed within the strata reporting slow usual walking pace. A similar pattern of the association was found for those living in houses, but it was not present in those living in flats. The likelihood ratio tests provided no evidence for an interaction in any of these subgroups (P values ≥0.23).
Figure 1.
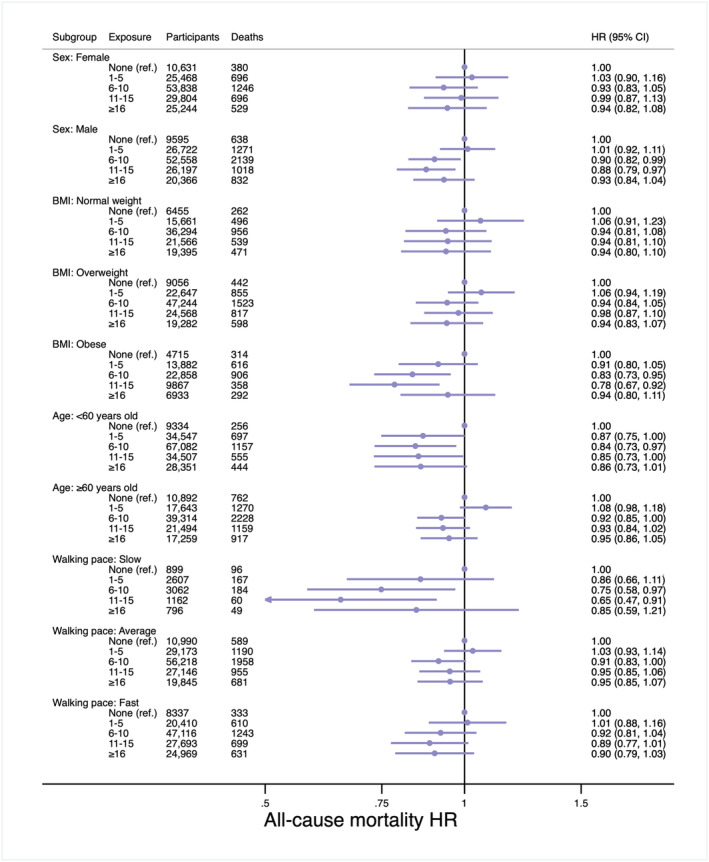
Hazard ratios of all‐cause mortality for categories of flights of stairs climbed per day by sex, body mass index, age and walking pace subgroups. CI, confidence interval; HR, hazard ratio; Ref, reference. The analysis was adjusted for age, sex, ethnicity, type of accommodation (house/flat), Townsend deprivation index, education, marital status, employment, total annual income before tax, physical activity, diet pattern, salt consumption, screen time, smoking, alcohol, body mass index, walking pace, depression, diabetes, hypertension, use of statins and longstanding illness, disability, or infirmity.
Figure 2.
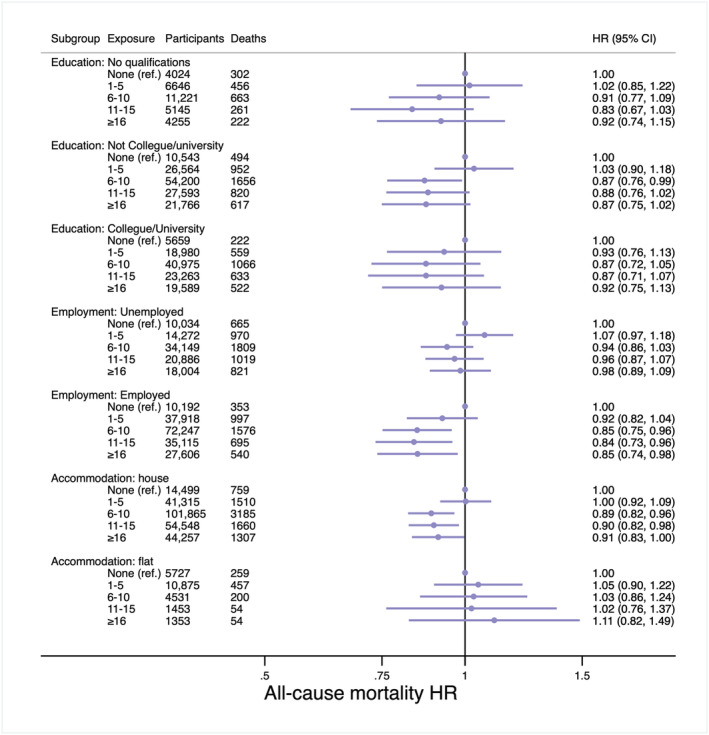
Hazard ratios of all‐cause mortality for categories of flights of stairs climbed per day by education, employment, and accommodation subgroups. CI, confidence interval; HR, hazard ratio; Ref, reference. The analysis was adjusted for age, sex, ethnicity, type of accommodation (house/flat), Townsend deprivation index, education, marital status, employment, total annual income before tax, physical activity, diet pattern, salt consumption, screen time, smoking, alcohol, body mass index, walking pace, depression, diabetes, hypertension, use of statins and longstanding illness, disability, or infirmity.
A total of 842 lung cancer deaths (14.8% of cancer deaths) were included in the negative control analysis (Table S5). The confounding structure of the covariates for all‐cause and lung cancer mortality was similar, as was the associations between stair climbing and the two outcomes [for lung cancer mortality, 1–5 flights per day HR = 0.97 (95% CI: 0.76, 1.23), 6–10 flights per day HR = 0.81 (95% CI: 0.65, 1.02), 11–15 flights per day HR = 0.69 (95% CI: 0.53, 0.91), ≥16 flights/day HR = 0.91 (95% CI: 0.70, 1.19)].
Discussion
Climbing more than five flights of stairs per day at home (around 50 stairs) was associated with a 7% to 9% lower risk of all‐cause mortality compared with no stair climbs per day. There appeared to be a threshold with lower risk above five flights per day and no further risk reduction at higher levels of stair climbing. Climbing between 6 and 10 flights was associated with lower risk of cancer but not CVD mortality. The results were consistent across subgroups, with markedly stronger associations in those reporting slow average walking pace.
Our findings are in accordance with previous research from the Harvard Alumni Health Study, which found significant 9–18% 14 risk reductions in all‐cause mortality from stair climbing, although these reductions were weaker in our study. There could be several reasons for this discrepancy. For example, the Harvard Study used total stair climbing while we could only consider at‐home stair walking. We extended previous research in several aspects, which may also explain the differences in the findings. First, we included women in the analysis. Indeed, our sex‐stratified results showed a stronger association in men, compared with the whole sample, while the opposite occurred for women. Second, we controlled for many different sociodemographic variables in addition to health and behavioural factors. Third, we carefully excluded participants with low physical mobility in addition to those with prevalent chronic diseases and deaths occurring within 2 years of follow‐up as measures to reduce the impact of reverse causation bias. Fourth, we were able to stratify the analysis by different covariates, including some socioeconomic (i.e. education, employment status, and type of accommodation lived in) and some related to frailty and mobility (i.e. walking pace), in an effort to account for potential residual confounding from socioeconomic status or poor physical mobility, respectively. Fifth, we aimed to account for potential residual confounding by applying different statistical methods (i.e. exclusions based on propensity score matching and the use of a negative control).
While higher levels of stair climbing were associated with lower risk of mortality across strata of socioeconomic status and self‐reported walking pace as a marker of frailty, we are cautious interpreting our data as a causal effect of at‐home stair climbing on mortality. It is unclear why the association between stair climbing and mortality was only apparent for all‐cause and cancer mortality, but not CVD mortality. This seems contradictory with the current evidence indicating the benefits of physical activity on the cardiovascular system. 5 In the Harvard Alumni Health Study, both total and CVD mortality was inversely associated with stair walking, but the association was weaker for CVD (6% lower at >35 floors/week against the reference) than for total mortality (16% lower). We used lung‐cancer as a negative control outcome and observed a similar magnitude of association as with total mortality. While the association between physical activity and lung cancer is rated as ‘Limited–suggestive’ by the World Cancer Research Fund, 31 these associations are observed at much higher physical activity levels than is elicited by walking up and down a flight of stairs 5–10 times perday. 30 Further, there is a substantial risk of residual confounding from smoking in current data from observational analyses as physical activity–lung cancer associations were not present among never smokers. 28 , 32 Finally, it is unclear why a threshold effects should be observed if stair climbing is sufficient stimuli to lower mortality. This observation may be biased by frailty or other unmeasured or poorly measured confounders. Taken together, we consider the risk of residual confounding bias from socioeconomic factors, such as living conditions, or from unaccounted frailty, as more plausible explanations for the observed associations rather than the amount of physical activity induced by stair walking being sufficient to prevent mortality. Importantly, this does not mean that promoting stair walking through nudges or by design features of the environment cannot make a meaningful contribution towards an overall active lifestyle, but our results does not show that at‐home stair climbing, in isolation, is enough to prevent early mortality.
Our study should be interpreted in light of several limitations. First, the stair climbing variable was collected through questionnaire, so it is susceptible to reporting bias. Second, we controlled for self‐reported moderate, vigorous, and walking activity, but this adjustment is also susceptible to cognitive biases. Third, the participants from the UK Biobank are not representative of the entire UK population, and a healthy volunteer selection bias has been previously reported, 33 and there is evidence that some exposure‐outcome associations may be susceptible to bias from selection mechanisms. 34 Fourth, we only had information on at‐home stair climbing, which misses stair climbing in other localities, where interventions are feasible. Finally, we used lung cancer as negative control outcome to identify possible residual confounding from socioeconomic status, as the main causes of lung cancer are smoking, second‐hand smoking, air pollution, and occupational exposures. Still, lung cancer may not represent a perfect negative control outcome as we cannot completely refute high levels of physical activity as a protective factor for lung cancer. 29
Our study is relevant for public health because interventions aimed at increasing stair climbing appears effective, both in the public space and workplace. 35 , 36 We did not find convincing evidence that taking the stairs for activities of the daily living at home will be sufficient physical activity stimuli to lower the risk of premature death. Previous randomized controlled trials in sedentary young women 10 and office workers 9 reported health benefits (e.g. increased maximum oxygen consumption) after 8 week stair‐climbing interventions, while other CVD‐related parameters (e.g. lipid profile or adiposity) where unaltered. It should be highlighted that these two studies involved structured stair climbing programmes, with protocols characterized by a specific weekly frequency (five times per day), a specific intensity (climbing at comfortable but brisk rate, about 90 steps a minute) and increasing volume (i.e. from climbing once a day 145 and 199 stairs to climbing those five times per day). Therefore, the benefits of increasing physical activity through replacing the use of elevators or escalators with stair taking in everyday life, which differs from prescribing stair climbing programmes, should be further investigated.
In conclusion, climbing more than five flights of stairs per day was associated with a lower risk of all‐cause and cancer mortality, but not CVD mortality, compared with those who did not take the stairs. The magnitude of the association was small and appeared susceptible to residual confounding. It is unlikely that at‐home stair climbing is sufficient physical activity stimuli to lower the risk of premature mortality.
Conflict of interest
Miguel A. Sanchez‐Lastra, Ding Ding, Knut‐Eirik Dalene, Borja del Pozo Cruz, Ulf Ekelund, and Jakob Tarp declare that they have no conflict of interest.
Supporting information
Table S1. Description of variables included from UK Biobank Data Showcase.
Table S2. Cross‐tabulation of stair climbing categories at baseline and the repeated assessment.
Table S3. Results from the age and sex‐adjusted model for the associations of all‐cause, cancer and cardiovascular disease mortality with flights of stairs climbed per day.
Table S4. Associations of all‐cause mortality with flights of stairs climbed per day by ten‐year age subgroups.
Table S5. Confounding structure of all‐cause mortality and negative control outcomes.
Figure S1. Number of participants in each step of the inclusion and exclusion process.
Acknowledgements
The authors of this manuscript certify that they comply with the ethical guidelines for authorship and publishing in the Journal of Cachexia, Sarcopenia and Muscle. 37
Sanchez‐Lastra M. A., Ding D., Dalene K.‐E., del Pozo Cruz B., Ekelund U., and Tarp J. (2021) Stair climbing and mortality: a prospective cohort study from the UK Biobank, Journal of Cachexia, Sarcopenia and Muscle, 12, 298–307, 10.1002/jcsm.12679.
References
- 1. World Health Organization (WHO) . Global action plan on physical activity 2018–2030: more active people for a healthier world. WHO 2019. http://www.who.int/ncds/prevention/physical-activity/global-action-plan-2018-2030/en/. Accessed 19 June 2020.
- 2. Lim SS, Vos T, Flaxman AD, Danaei G, Shibuya K, Adair‐Rohani H, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012;380:2224–2260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Lee I‐MM, Shiroma EJ, Lobelo F, Puska P, Blair SN, Katzmarzyk PT, et al. Effect of physical inactivity on major non‐communicable diseases worldwide: an analysis of burden of disease and life expectancy. Lancet (London, England) 2012;380:219–229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Strain T, Wijndaele K, Dempsey PC, Sharp SJ, Pearce M, Jeon J, et al. Wearable‐device‐measured physical activity and future health risk. Nat Med 2020;26:1385–1391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. U.S. Department of Health and Human Services . Physical Activity Guidelines for Americans, 2nd ed. Washington, DC: U.S. Department of Health and Human Services; 2018. [Google Scholar]
- 6. Physical Activity Guidelines Advisory Comittee . Physical Activity Guidelines Advisory Committee Scientific Report, Vol. 2018. Washington, DC: US Department of Health and Human Services; 2018. https://health.gov/sites/default/files/2019-09/PAG_Advisory_Committee_Report.pdf [Google Scholar]
- 7. Allison MK, Baglole JH, Martin BJ, MacInnis MJ, Gurd BJ, Gibala MJ. Brief intense stair climbing improves cardiorespiratory fitness. Med Sci Sports Exerc 2017;49:298–307. [DOI] [PubMed] [Google Scholar]
- 8. Jenkins EM, Nairn LN, Skelly LE, Little JP, Gibala MJ. Do stair climbing exercise “snacks” improve cardiorespiratory fitness?. Applied Physiology, Nutrition, and Metabolism. 2019;44(6):681–684. 10.1139/apnm-2018-0675. [DOI] [PubMed] [Google Scholar]
- 9. Kennedy RA, Boreham CAG, Murphy MH, Young IS, Mutrie N. Evaluating the effects of a low volume stairclimbing programme on measures of health‐related fitness in sedentary office workers. J Sports Sci Med 2007;6:448–454. [PMC free article] [PubMed] [Google Scholar]
- 10. Boreham CAG, Kennedy RA, Murphy MH, Tully M, Wallace WFM, Young I. Training effects of short bouts of stair climbing on cardiorespiratory fitness, blood lipids, and homocysteine in sedentary young women. Br J Sports Med 2005;39:590–593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Ross R, Blair SN, Arena R, Church TS, Després JP, Franklin BA, et al. Importance of assessing cardiorespiratory fitness in clinical practice: a case for fitness as a clinical vital sign: a scientific statement from the American Heart Association. Circulation 2016;134:e653–e699. [DOI] [PubMed] [Google Scholar]
- 12. Lee IM, Paffenbarger RS. Associations of light, moderate, and vigorous intensity physical activity with longevity: the Harvard Alumni Health Study. Am J Epidemiol 2000;151:293–299. [DOI] [PubMed] [Google Scholar]
- 13. Paffenbarger RS, Lee IM. A natural history of athleticism, health and longevity. In: Journal of Sports Sciences. Taylor & Francis; 1998. [DOI] [PubMed] [Google Scholar]
- 14. Rey‐Lopez JP, Stamatakis E, Mackey M, Sesso HD, Lee IM. Associations of self‐reported stair climbing with all‐cause and cardiovascular mortality: the Harvard Alumni Health Study. Prev Med Rep 2019;15:100938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Strain T, Wijndaele K, Sharp SJ, Dempsey PC, Wareham N, Brage S. Impact of follow‐up time and analytical approaches to account for reverse causality on the association between physical activity and health outcomes in UK Biobank. Int J Epidemiol 2020;49:162–172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. The UK Biobank . About UK Biobank. https://www.ukbiobank.ac.uk/about-biobank-uk/. Accessed 27 January 2020.
- 17. The UK Biobank. UK Biobank : Protocol for a large‐scale prospective epidemiological resource. 2007. https://www.ukbiobank.ac.uk/wp-content/uploads/2011/11/UK-Biobank-Protocol.pdf. Accessed 23 September 2019.
- 18. World Health Organization . Obesity: preventing and managing the global epidemic: report of a WHO consultation. In World Health Organization; 2000. [PubMed] [Google Scholar]
- 19. Townsend P, Phillimore P, Beattie A. Health and deprivation: inequality and the North Croom Helm: London; 1988.
- 20. Lee PH, Macfarlane DJ, Lam TH, Stewart SM. Validity of the international physical activity questionnaire short form (IPAQ‐SF): a systematic review. Int J Behav Nutr Phys Act 2011;8:115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. NHS . 8 tips for healthy eating. https://www.nhs.uk/live-well/eat-well/eight-tips-for-healthy-eating/. Accessed 14 August 2019.
- 22. Celis‐Morales CA, Lyall DM, Steell L, Gray SR, Iliodromiti S, Anderson J, et al. Associations of discretionary screen time with mortality, cardiovascular disease and cancer are attenuated by strength, fitness and physical activity: findings from the UK Biobank study. BMC Med 2018;16:77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Morgan CJ. Reducing bias using propensity score matching. J Nucl Cardiol 2018;25:404–406. [DOI] [PubMed] [Google Scholar]
- 24. Austin PC. Statistical criteria for selecting the optimal number of untreated subjects matched to each treated subject when using many‐to‐one matching on the propensity score. Am J Epidemiol 2010;172:1092–1097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Woo J. Walking speed: a summary indicator of frailty? J Am Med Dir Assoc 2015;16:635–637. [DOI] [PubMed] [Google Scholar]
- 26. Fine JP, Gray RJ. A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc 1999;94:496–509. [Google Scholar]
- 27. Hamer M, Ding D, Chau J, Duncan MJ, Stamatakis E. Association between TV viewing and heart disease mortality: observational study using negative control outcome. J Epidemiol Community Health 2020;74:391–394. [DOI] [PubMed] [Google Scholar]
- 28. Matthews CE, Moore SC, Arem H, Cook MB, Trabert B, Hakansson N, et al. Amount and intensity of leisure‐time physical activity and lower cancer risk. J Clin Oncol 2020;38:686–698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Baumeister S‐E, Leitzmann M, Bahls M, Meisinger C, Amos C, Hung R, et al. Physical activity does not lower the risk of lung cancer. Cancer Res 2020;80: canres.1127.2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Moore SC, Lee IM, Weiderpass E, Campbell PT, Sampson JN, Kitahara CM, et al. Association of leisure‐time physical activity with risk of 26 types of cancer in 1.44 million adults. JAMA Intern Med 2016;176:816–825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. World Cancer Research Fund International . Physical activity & cancer. https://www.wcrf.org/dietandcancer/exposures/physical-activity. Accessed 5 August 2020.
- 32. Patel AV, Friedenreich CM, Moore SC, Hayes SC, Silver JK, Campbell KL, et al. American College of Sports Medicine Roundtable report on physical activity, sedentary behavior, and cancer prevention and control. Med Sci Sports Exerc 2019;51:2391–2402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Fry A, Littlejohns T, Sudlow C, Doherty N, Allen N. The representativeness of the UK Biobank cohort on a range of sociodemographic, physical, lifestyle and health‐related characteristics. J Epidemiol Community Health 2016;70:A26.1–A26. [Google Scholar]
- 34. Stamatakis M, Shepherd L, Drayton B, Hamer M, Bauman A. Is cohort study representativeness passé? Matching the UK Biobank sample to target population characteristics and recalculating the associations between lifestyle risk factors and mortality. SSRN Electron J 2020; 10.2139/ssrn.3572906. [DOI] [Google Scholar]
- 35. Jennings CA, Yun L, Loitz CC, Lee EY, Mummery WK. a systematic review of interventions to increase stair use. Am J Prev Med 2017;52:106–114. [DOI] [PubMed] [Google Scholar]
- 36. Bellicha A, Kieusseian A, Fontvieille AM, Tataranni A, Charreire H, Oppert JM. Stair‐use interventions in worksites and public settings—a systematic review of effectiveness and external validity. Prev Med (Baltim) 2015;70:3–13. [DOI] [PubMed] [Google Scholar]
- 37. von Haehling S, Morley JE, Coats AJS, Anker SD. Ethical guidelines for publishing in the Journal of Cachexia, Sarcopenia and Muscle: update 2019. J Cachexia Sarcopenia Muscle 2020;10:1143–1145. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Description of variables included from UK Biobank Data Showcase.
Table S2. Cross‐tabulation of stair climbing categories at baseline and the repeated assessment.
Table S3. Results from the age and sex‐adjusted model for the associations of all‐cause, cancer and cardiovascular disease mortality with flights of stairs climbed per day.
Table S4. Associations of all‐cause mortality with flights of stairs climbed per day by ten‐year age subgroups.
Table S5. Confounding structure of all‐cause mortality and negative control outcomes.
Figure S1. Number of participants in each step of the inclusion and exclusion process.


