Abstract
Aims:
The study compared changes in implant stability and bone loss of implants with different designs using early loading at 6 weeks.
Setting and Design:
In vivo-comparative study.
Materials and Methods:
Forty subjects were selected and divided randomly by sealed envelope method in Group X and Group A for early loading for missing single posterior tooth in mandible. Implants in Group X had flared crest module and buttress thread design, whereas implants in Group A had parallel crest module and V-shaped thread design. All subjects were evaluated by Ostell for implant stability at the interval of baseline, 6 weeks, 3 months, and 6 months. ImageJ software was used for measurement of crestal bone loss in intraoral periapical radiographs at the interval of 6 weeks, 3 months, and 6 months.
Statistical Analysis Used:
Unpaired t test, repeated ANOVA, Tukey post hoc test.
Results:
The mean bone loss values of Group X at predetermined interval were 1.51 ± 0.20 mm, 2.11 ± 0.21 mm and 2.13 ± 0.21 mm. The mean bone loss values of Group A were 1.79 ± 0.16 mm, 2.92 ± 0.23 mm and 2.95 ± 0.23 mm. The mean bone loss was statistical significant (P < 0.05) at 6 weeks, 3 months and 6 months. It was highly significant in Group A at 6 months (P < 0.001).
Conclusions:
It was concluded that Group X implants design showed better implant stability and less bone loss when compared to Group A implants design.
Keywords: Crestal bone loss, design, early loading, resonance frequency analyzer
INTRODUCTION
Delayed or conventional implant loading protocols were based on the achievement of submerged and prolonged healing duration from 3 to 6 months without loading.[1] The biggest drawbacks of the delayed loading protocol were the length of time required and the resultant patient inconvenience. Moreover, the bone density around the implant after the 6 months was found to be reduced due to the lack of functional stimulation during the healing period.[2]
Early loading of implants during the healing phase was found to be more favorable to osteogenesis rather than being harmful to bone growth or remodeling. Recent researches have also recommended a shorter healing duration by early loading of the dental implant.[3,4,5,6,7] Nowadays, edentulous areas with good bone quality, early loading of implants are preferred due to their high success rates.[8,9,10,11,12,13,14]
The stability of the peri-implant hard tissue was fundamental to success for early loading. Primary stability of the dental implant was achieved through a good mechanical fixation of the dental implant within the bone, whereas secondary stability was achieved due to biological integration.[15]
Various techniques for measuring the primary stability of a dental implant are radiographs, reverse torque analysis, percussion testing, periotest, and implant insertion torque values of a minimum of 35 Ncm and resonance frequency analyzer (RFA).[16,17]
The latest technique for measuring the primary stability by RFA was used in this study. RFA has a metal rod with magnet, which is activated by magnetic impulse from an electronic device. RFA assess implant stability and osseointegration noninvasively.[18,19,20,21]
Cochran et al., in their prospective human clinical trial, showed International team of implantology implants can be rehabilitated at 6 weeks with a success rate of 99% after 2 years.[11] To further contribute in this field, the present research was designed to compare implant stability and bone loss using early loading protocol in two implant systems with different designs.
MATERIALS AND METHODS
Source of data
The present study was done in the Department of Prosthodontics, Crown and Bridges, Faculty of Dental Sciences, King George's Medical University, Lucknow, U. P., after receiving ethical clearance from the Institutional Ethical Committee of the university (Letter No. 3151/ethics/R. cell-15 Dated 7/1/2015, Ref. Code. 70th ECM II-B/P50).
Sample size
It was calculated using the below formula:
n = 17 σ2/Δ2 + 1
For the power of 80% and the significance level of 5%
In the formula, n represents the required sample size per group, which was 20 samples, Δ represents the expected mean difference and σ was half of the confidence interval, which was 0.5.
Study design
This was a randomized, prospective, longitudinal, and in vivo-comparative study. Forty subjects out of sixty subjects who were partially edentulous in the posterior mandibular arch, fulfilling the following inclusion and exclusion criteria were enrolled in the research [Flow Chart 1]:
Flow Chart 1.
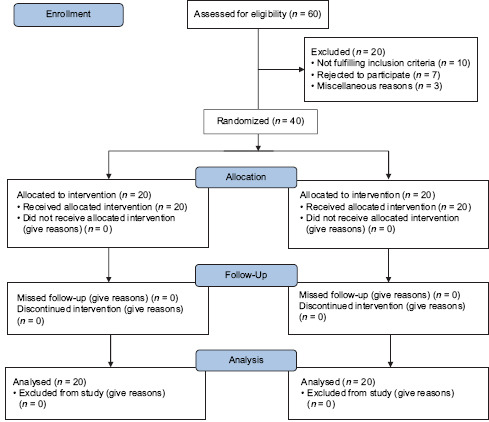
CONSORT 2010 flow chart
Inclusion criteria
Subjects who were having single missing posterior tooth in the mandible
Subjects having age between 18 and 65 years
Subjects having good general health with no systemic diseases
Extraction sites healed for at least 6 months
Patients with sufficient bone volume of more than 6.0 mm in width and 11.0 mm in height as evidenced on a pre-operative cone-beam computed tomography (CBCT) scan
Implant stability quotient (ISQ) value more than 60 during implant placement.
Exclusion criteria
Clinical sign of alveolar bone infection at the surgical area
Alcohol, drug, and medication dependent subjects
Subjects with underlying mental illness
Subjects with a previous history of radiotherapy or chemotherapy
Subjects with cigarette smoking and paan chewing habit.
The subjects fulfilling study criteria were randomly divided by sealed enveloped method into two groups, each consisting of twenty subjects:
Group X - Implants with flared crest module, buttress thread design, and 4.5 diameter
Group A - Implants with parallel crest module, V-shaped thread design, and 4.2 diameter.
Clinical procedure
For each group, dimensions of the edentulous bone to be restored were assessed using CBCT [Figure 1]. During surgery, mid-crestal incision was made and flap elevated, and the implant sequential osteotomy was done with bone drills of increasing diameter. A surgical template guided implant placement was done. The orientation of osteotomy was assessed by paralleling pin of 2 mm diameter and radiovisiography.
Figure 1.
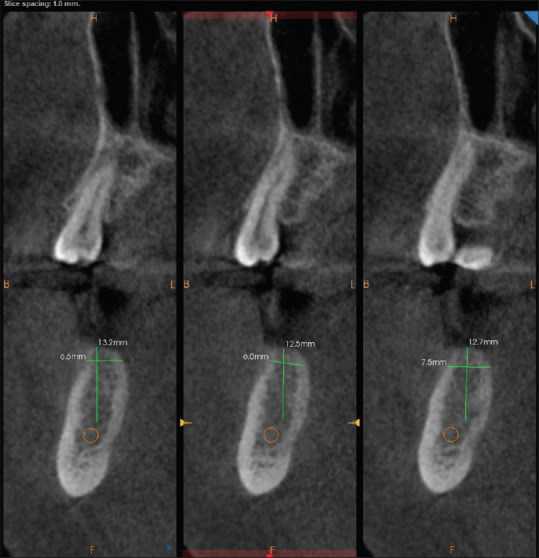
Preoperative assessment of bone by cone beam computed tomography
The implant was inserted at a torque 35 Ncm by a hand ratchet or a high torque low-speed handpiece. Subsequently, measurement of stability and level of crestal bone was determined. Silk suture was used to approximate the flaps, and postoperative instructions to maintain good oral hygiene were given. Postoperatively, oral hygiene instructions, antibiotic (amoxicillin 500 mg TDS for 5 days), and anti-inflammatory drugs (ibroprofen 200–400 mg orally as needed for 5 days) were prescribed. A follow-up appointment after a week was given for suture removal.
Six weeks after surgery, provisional crown was delivered with no occlusal interference in eccentric movement. At 3 months, porcelain fused metal crown was fabricated, which was cemented using noneugenol zinc oxide temporary cement, due to its property of easy removal after follow-up at 6 months [Figures 2–5].
Figure 2.

Preoperative of Group X
Figure 5.

Postoperative of Group A
Figure 3.

Postoperative of Group X
Figure 4.

Preoperative of Group A
Assessment of implant stability
Implant stability in each subject was assessed using RFA (OSTELL ISQ, Europe). SmartPeg™, a component of the RFA system, attached to the dental implant or abutment using an integrated screw, was activated by magnetic impulses generated by a handheld instrument with a measuring probe. ISQ value ranges from 1 to 100 as displayed on the Ostell instrument [Figure 6]. ISQ was measured, and the mean was recorded for each subject at baseline, 6 weeks, 3 months, and 6 months.
Figure 6.
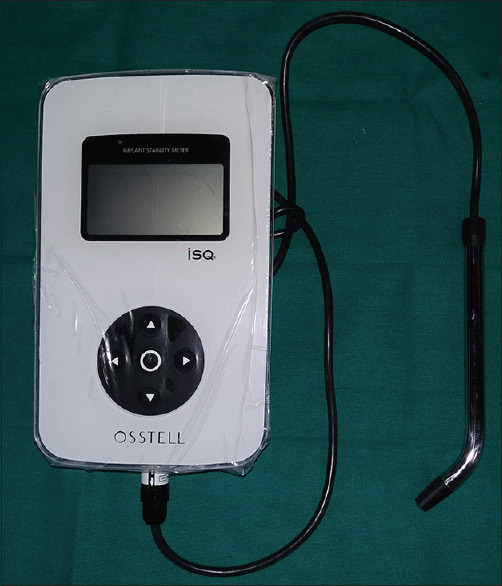
Resonance frequency analyzer
Assessment of crestal bone loss
ImageJ software (National institutes of health, Maryland, USA) was used for measurement of crestal bone in intraoral periapical radiographs taken at an interval of baseline, 6 weeks, 3 months, and 6 months recall. Standardization of radiograph was done with XCP (extension cone paralleling) extension cone. The implant-abutment junction was used as the reference point for all measurements. The linear measurement of the implant from the implant-abutment junction and linear measurement from the implant-abutment junction to crestal bone in IOPA X-ray was used to determine bone value on a computer by ImageJ software [Figure 7]. The crestal bone loss was calculated as the difference between the reading at the time of follow-up examination and the baseline value. The mean of mesial and distal bone value measurements was recorded for each implant at predetermined intervals.[22]
Figure 7.
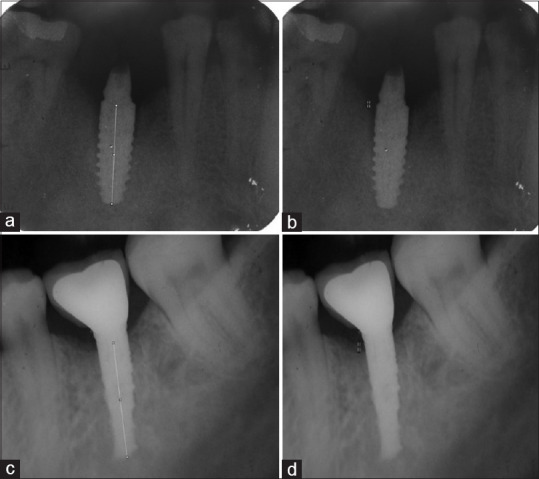
Bone loss calculated by linear measurements of implant and crestal bone from the implant-abutment junction as a reference using ImageJ software. ((a and b) shows bone loss measurement in Group X; (c and d) shows bone loss measurement in Group A)
RESULTS
Analyses were performed using SPSS software (PASW Statistics for Windows, Version 18.0. Chicago:SPSS Inc.). The data were analyzed and summarized as mean ± standard deviation. Table 1 shows the comparison of ISQ at baseline, 6 weeks, 3 months, and 6 months between Group X and Group A. There was a statistically significant (P ≤ 0.05) ISQ value at each four measured time periods in Group X. The ISQ value was highly significant (P ≤ 0.001) at 6 weeks in Group X.
Table 1.
Comparison of implant stability quotient at baseline, 6 weeks, 3 months, and 6 months in early loaded implants between Group X and Group A using unpaired t-test
| Timeline | Mean±SD | t | P | |
|---|---|---|---|---|
| Group X | Group A | |||
| Baseline | 85.45±0.55 | 79±1.49 | 10.1 | 0.02 |
| 6 weeks | 77.20±1.23 | 74.40±1.76 | 5.8 | 0.0001 |
| 3 months | 79.70±0.31 | 78.1±1.37 | 3.68 | 0.01 |
| 6 months | 83.20±0.29 | 81.25±1.37 | 4.65 | 0.03 |
SD: Standard deviation
Table 2 shows that there was statistically significant (P ≤ 0.05) bone loss in Group A as compared to Group X at 6 weeks, 3 months, and 6 months. The bone loss value was highly significant (P ≤ 0.001) at 6 months in Group A.
Table 2.
Comparison of bone loss at 6 weeks, 3 months, and 6 months in early loaded implants between Group X and Group A using unpaired t-test
| Timeline | Mean±SD | t | P | |
|---|---|---|---|---|
| Group X | Group A | |||
| 6 weeks | 1.51±0.20 | 1.79±0.16 | −4.63 | 0.01 |
| 3 months | 2.11±0.21 | 2.92±0.23 | −11.66 | 0.05 |
| 6 months | 2.13±0.21 | 2.95±0.23 | −11.74 | 0.001 |
SD: Standard deviation
DISCUSSION
With the recent advancement of implant design, surface modification and better surgical techniques in implant dentistry. The Branemark's protocol of implant of implant loading of 3–6 months has been reevaluated and modified significantly to 6–12 weeks with promising osseointegration and good clinical success rate.[4,5] The present randomized clinical study compared implant stability and crestal bone loss in two implant systems using early loading with the provisional crown at 6 weeks. Implants in Group X had flared crest module, buttress thread design and 4.5 diameter. Implants in Group A had parallel crest module, V-shaped thread design, and 4.2 diameter. The implant surface in both groups was sandblasted and acid-etched surface (SLA), which activates differentiation of bone cell, production of protein and improves bone-implant contact, which are favorable for shorter healing time.[11]
For standardization, single missing posterior tooth region in the mandible was chosen as it has bone density of generally D2 with 850–1250 Hounsfield unit, high elastic modulus, 65%–75% bone-implant contact percentage, which not only provides better primary stability but will also permit better stress distribution, lessening the chances of overload, thereby leading to better prognosis and ensuring uniformity among two groups.[9]
Implants with ISQ value above 60 may be suitable for early loading as supported by Meredith et al.[18] Other studies by Bornstein et al.,[9] Ganeles and Wismeijer,[23] Quinlan et al.,[24] Galli et al.,[25] and De Smet et al.,[26,27] proved that the early loading protocol has implant survival rate of >99%. The key determinant to achieve osseointegration was controlling micromotion at the initial stages of implant healing, which if not controlled leads to fibrous encapsulation formation.[28] In this study, micromotion <100 μm were achieved by removing all eccentric contact in the provisional crown at 6 weeks in both groups.
ISQ comparison of implant stability between Group X and Group A revealed greater stability of Group X at baseline, 6 weeks, 3 months, and 6 months, which was due to buttress thread design of Group X when compared to V thread design of Group A as supported by Rismanchian et al.[29] The decrease in the ISQ value from baseline to 6 weeks in both groups was due to the bone remodeling around the dental implant as supported by Huwiler et al. and Boronat López et al.[30,31]
Diameter of Group X implants used in the study was 4.5 mm, while it was 4.2 mm for Group A implants. As the width increases in increments of 0.5 mm, surface area increases by 10%–15%, and crestal strain decreases as much as a 3.5-fold.[32,33] An increase in diameter from 3.3 mm to 4.1 mm leads to decrease in maximum stress by 29.6% and an increase between 4.1 mm and 4.8 mm, leads to a maximum stress reduction of 34.1% for vertical forces.[34] Moreover, buccolingual forces were reduced with increasing diameter of implant.[35] Hence, the significantly reduced crestal bone loss around Group X implants may very well be a reflection of the greater reduction in crestal stress concentration attributable to the increased diameter.
Crest module of Group X implants was characterized by a flared crest module by 0.185 mm per side, whereas the Group A implants had a parallel-sided crest module. The flared crest module with smooth collar designs seals the coronal area preventing bacterial invasion; hence, the bone loss was less in Group X implants as supported by Misch et al.[36] The heights of the crest modules of the two implants used in this study also differed. Group A implants had a considerably longer collar (1.7 mm) than the Group X implants (1.5 mm). The greater crestal bone loss around Group A implants may also have been influenced by its longer collar length, as supported by Bordin et al. in their study.[37]
Thread design modifies the direction of occlusal load applied to the prosthesis at the implant-bone interface. Buttress threads design of Group X transmits compressive stress when compared to V-thread design of Group A, which transmits shear stress to the implant-bone interface.[38] Since bone was 65% weaker under shear stress than under compressive stresses, as supported by Reilly and Burstein and Oswal et al.,[39,40] implants with buttress thread design such as those used in Group X may had a beneficial effect in stress reduction at the crestal bone during early loading as compared to Group A.
Limitation
Interval of the investigation was of short duration
The sample size of the study was small.
The outcome of the present research should not be extrapolated to all dental implant systems.
CONCLUSIONS
Within the limitations of the study, we concluded that Group X implants design showed superior results in comparison to Group A implants design with respect to implant stability and crestal bone loss. Hence, early loading at 6 weeks may be considered as a promising option for missing single posterior tooth in the mandible. 41
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Brånemark PI, Hansson BO, Adell R, Breine U, Lindström J, Hallén O, et al. Osseointegrated implants in the treatment of the edentulous jaw. Experience from a 10-year period. Scand J Plast Reconstr Surg Suppl. 1977;16:1–32. [PubMed] [Google Scholar]
- 2.Roberts WE, Turley PK, Brezniak N, Fielder PJ. Implants: Bone physiology and metabolism. CDA J. 1987;15:54–61. [PubMed] [Google Scholar]
- 3.Fischer K, Stenberg T, Hedin M, Sennerby L. Five-year results from a randomized, controlled trial on early and delayed loading of implants supporting full-arch prosthesis in the edentulous maxilla. Clin Oral Implants Res. 2008;19:433–41. doi: 10.1111/j.1600-0501.2007.01510.x. [DOI] [PubMed] [Google Scholar]
- 4.Zhang XX, Shi JY, Gu YX, Lai HC. Long-term outcomes of early loading of straumann implant-supported fixed segmented bridgeworks in edentulous maxillae: A 10-year prospective study. Clin Implant Dent Relat Res. 2016;18:1227–37. doi: 10.1111/cid.12420. [DOI] [PubMed] [Google Scholar]
- 5.Han J, Tang Z, Zhang X, Meng H. A prospective, multi-center study assessing early loading with short implants in posterior regions. A 3-year post-loading follow-up study. Clin Implant Dent Relat Res. 2018;20:34–42. doi: 10.1111/cid.12568. [DOI] [PubMed] [Google Scholar]
- 6.Sekar S, Suthanthiran T, Thangavelu A, Karupannan SK, Prem F, Rajendran D. Clinical and radiological evaluation of delayed and early loading of single-tooth implant placement: A 6-month, prospective, randomized, follow-up clinical study. J Pharm Bioallied Sci. 2019;11(Suppl 2):S278–84. doi: 10.4103/JPBS.JPBS_12_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kreja L, Liedert A, Hasni S, Claes L, Ignatius A. Mechanical regulation of osteoclastic genes in human osteoblasts. Biochem Biophys Res Commun. 2008;368:582–7. doi: 10.1016/j.bbrc.2008.01.106. [DOI] [PubMed] [Google Scholar]
- 8.Esposito M, Grusovin MG, Tzanatea E, Coulthard P, Worthington HV. Interventions for replacing missing teeth: Different times for loading dental implants. Cochrane Database Syst Rev. 2007;16:CD003878. doi: 10.1002/14651858.CD003878.pub3. [DOI] [PubMed] [Google Scholar]
- 9.Bornstein MM, Lussi A, Schmid B, Belser UC, Buser D. Early loading of non-submerged titanium implants with a sandblasted and acid-etched (SLA) surface: 3 year result of a prospective study in partially edentulous patients. Int J Oral Maxillofac Implants. 2003;18:659–66. [PubMed] [Google Scholar]
- 10.Capelli M, Esposito M, Zuffetili F, Galli F, Del Fabbro M, Testori T. A 5 year report from a multicentre randomized clinical trial: Immediate non occlusal vs early loading of dental implants in partially edentulous patients. Eur J Oral Implantol. 2010;3:209–219. [PubMed] [Google Scholar]
- 11.Cochran DL, Buser D, ten Bruggenkate CM, Weingart D, Taylor TM, Bernard JP, et al. The use of reduced healing times on ITI implants with a sandblasted and acid-etched (SLA) surface: Early results from clinical trials on ITI SLA implants. Clin Oral Implants Res. 2002;13:144–53. doi: 10.1034/j.1600-0501.2002.130204.x. [DOI] [PubMed] [Google Scholar]
- 12.Grandi T, Garuti G, Giazzi P, Tarabini L, Forabosco A. Survival and success rates of immediately and early loaded implants: 12 month results from a multicentric randomized clinical study. J Oral Implantol. 2012;38:239–49. doi: 10.1563/AAID-JOI-D-10-00149. [DOI] [PubMed] [Google Scholar]
- 13.Roccuzzo M, Wilson TG. A prospective study of 3 weeks loading of chemically modified titanium implants in the maxillary molar region: 1 year results. Int J Oral Maxillofac Implants. 2009;24:65–72. [PubMed] [Google Scholar]
- 14.Testori T, Fabbro MD, Feldman S, Vincenzi G, Sullivan D, Rossi R, et al. A multicentre prospective evaluation of 2 months loaded Osseotite implants placed in the posterior jaws: 3 year follow up results. Clin Oral Implants Res. 2002;13:154–61. doi: 10.1034/j.1600-0501.2002.130205.x. [DOI] [PubMed] [Google Scholar]
- 15.Davies JE. Understanding periimplant endosseous healing. J Dent Educ. 2003;67:932–49. [PubMed] [Google Scholar]
- 16.Li D, Fergusson SJ, Beutler T. Biomechanical comparison of the sandblasted and acid etched and the machined and acid etched titanium surface for dental implants. J Biomed Mater Res. 2002 May;60(2):325–32. doi: 10.1002/jbm.10063. [DOI] [PubMed] [Google Scholar]
- 17.Sarfaraz H, Johri S, Sucheta P, Sripathi Rao S. Study to assess the relationship between insertion torque value and implant stability quotient and its influence on timing of functional implant loading. J Indian Prosthodont Soc. 2018;18:139–46. doi: 10.4103/jips.jips_203_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Meredith N, Friberg B, Sennerby L, Aparicio C. Relationship between contact time measurements and PTV values when using the periotest to measure implant stability. Int J Prosthodont. 1998;11:269–75. [PubMed] [Google Scholar]
- 19.Kim JM, Kim SJ, Han I, Shin SW, Ryu JJ. A comparison of implant stability among various implant systems: clinical study. J Adv Prosthodont. 2009;1:31–6. doi: 10.4047/jap.2009.1.1.31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Esposito M, Grusovin MG, Willings M, Coulthard P, Worthington HV. The effectiveness of Immediate, early and conventional loading of dental implants: A Cochrane systematic review of randomized controlled clinical trials. Int J Oral Maxillofac Implants. 2007;22:893–904. [PubMed] [Google Scholar]
- 21.Swami V, Vijayaraghavan V, Swami V. Current trends to measure implant stability. J Indian Prosthodont Soc. 2016;16:124–30. doi: 10.4103/0972-4052.176539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Makary C, Menhall A, Zammarie C, Lombardi T, Lee SY, Stacchi C, et al. Primary stability optimization by using fixtures with different thread depth according to bone density: A Clinical prospective study on early loaded implants. Materials (Basel) 2019;12:???. doi: 10.3390/ma12152398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ganeles SJ, Wismeijer D. Early immediately restored and loaded dental implant for single tooth and partial arch applications. Int J Oral Maxillofac Implants. 2004;19:92–102. [PubMed] [Google Scholar]
- 24.Quinlan P, Nummikoski P, Schenk R, Cagna D, Mellonig J, Higginbottom F, et al. Immediate and early loading of SLA ITI single-tooth implants: An in vivo study. Int J Oral Maxillofac Implants. 2005;20:360–70. [PubMed] [Google Scholar]
- 25.Galli F, Capelli M, Zuffetti F, Testori T, Esposito M. Immediate non-occlusal vs. Early loading of dental implants in partially edentulous patients: A multicentre randomized clinical trial. Peri-implant bone and soft-tissue levels. Clin Oral Implants Res. 2008;19:546–52. doi: 10.1111/j.1600-0501.2008.01530.x. [DOI] [PubMed] [Google Scholar]
- 26.De Smet E, Jaecques S, Vandamme K, Vander Sloten J, Naert I. Positive effect of early loading on implant stability in the bi-cortical guinea-pig model. Clin Oral Implants Res. 2005;16:402–7. doi: 10.1111/j.1600-0501.2005.01156.x. [DOI] [PubMed] [Google Scholar]
- 27.De Smet E, Duyck J, Vander Sloten J, Jacobs R, Naert I. Timing of loading –Immediate, early, or delayed – in the outcome of implants in the edentulous mandible: A prospective clinical trial. Int J Oral Maxillofac Implants. 2007;22:580–94. [PubMed] [Google Scholar]
- 28.Moncler SS, Salama H, Reingewirtz Y, Dubruille JH. Timing of loading and effect of micromotion on bone–dental implant interface: review of experimental literature. J Biomed Mater Res. 1998;43:192–203. doi: 10.1002/(sici)1097-4636(199822)43:2<192::aid-jbm14>3.0.co;2-k. [DOI] [PubMed] [Google Scholar]
- 29.Rismanchian M, Birang R, Shahmoradi M, Talebi H, Zare RJ. Developing a new dental implant design and comparing its biomechanical features with four designs. Dent Res J (Isfahan) 2010;7:70–5. [PMC free article] [PubMed] [Google Scholar]
- 30.Huwiler MA, Pjetursson BE, Bosshardt DD, Salvi GE, Lang NP. Resonance frequency analysis in relation to jawbone characteristics and during early healing of implant installation. Clin Oral Implants Res. 2007;18:275–80. doi: 10.1111/j.1600-0501.2007.01336.x. [DOI] [PubMed] [Google Scholar]
- 31.Boronat López A, Balaguer Martínez J, Lamas Pelayo J, Carrillo García C, Peñarrocha Diago M. Resonance frequency analysis of dental implant stability during the healing period. Med Oral Patol Oral Cir Bucal. 2008;13:E244–7. [PubMed] [Google Scholar]
- 32.Tada S, Stegaroiu R, Kitamura E, Miyakawa O, Kusakari H. Influence of implant design and bone quality on stress/strain distribution in bone around implants: A three dimensional finite element analysis. Int J Oral Maxillofac Implants. 2003;18:357–68. [PubMed] [Google Scholar]
- 33.Petrie CS, Williams JL. Comparative evaluation of implant designs: Influence of diameter, length, and taper on strains in the alveolar crest. A three-dimensional finite-element analysis. Clin Oral Implants Res. 2005;16:486–94. doi: 10.1111/j.1600-0501.2005.01132.x. [DOI] [PubMed] [Google Scholar]
- 34.Ding X, Zhu XH, Liao SH, Zhang XH, Chen H. Implant-bone interface stress distribution in immediately loaded implants of different diameters: A three dimensional finite element analysis. J Prosthodont. 2009;18:393–402. doi: 10.1111/j.1532-849X.2009.00453.x. [DOI] [PubMed] [Google Scholar]
- 35.Petrie CS, Williams JL. Shape optimization of dental implant designs under oblique loading using p-version finite element method. J Mech Med Biol. 2002;2:339–45. [Google Scholar]
- 36.Misch CE, Strong TD, Bidez MW. Scientific rationale for dental implant design. In: Misch CE, editor. Contemporary Implant Dentistry. 3rd ed. St. Louis: Mosby; 2008. pp. 200–32. [Google Scholar]
- 37.Bordin D, Cury AA, Faot F. Influence of abutment collar height and implant length on stress distribution in single crowns. Braz Dent J. 2019;30:238–43. doi: 10.1590/0103-6440201902533. [DOI] [PubMed] [Google Scholar]
- 38.Chun HJ, Cheong SY. Evaluation of design parameters of osseointegrated dental implants. J Oral Rehabil. 2002;29:565–74. doi: 10.1046/j.1365-2842.2002.00891.x. [DOI] [PubMed] [Google Scholar]
- 39.Reilly DT, Burstein AH. The elastic and ultimate properties of compact bone tissue. J Biomech. 1975;8:393–405. doi: 10.1016/0021-9290(75)90075-5. [DOI] [PubMed] [Google Scholar]
- 40.Fuller RW, Bromer WW, Snoddy HD, Baker JC. Regulation of enzyme activity by glucagon: Increased hormonal activity of iodinated glucagon. Adv Enzyme Regul. 1975;13:201–15. doi: 10.1016/0065-2571(75)90016-3. [DOI] [PubMed] [Google Scholar]
- 41.Oswal MM, Amasi UN, Oswal MS, Bhagat AS. Influence of three different implant thread designs on stress distribution: A three-dimensional finite element analysis. J Indian Prosthodont Soc. 2016;16:359–65. doi: 10.4103/0972-4052.191283. [DOI] [PMC free article] [PubMed] [Google Scholar]


