Abstract
Aim:
Recording the maxillomandibular relationship is important in various prosthodontic treatments. Evidence of face-bow transfer resulting in improved outcome is conflicting. Hence the objective of this study is to determine the use of face-bow transfer in prosthodontics.
Settings and Design::
Systematic review based on PRISMA guidelines.
Materials and Methods:
A protocol was developed prior, which covered all aspects of the review. The databases explored were MEDLINE database, ScienceDirect, and Cochrane collaboration library. The PICO model included participants who received a complete denture/partial denture prosthesis. Intervention was the use of the face-bow device. Comparator was prosthesis made with a simple procedure of not using a face-bow device for prosthodontic rehabilitation. Outcomes were patient satisfaction with dentures, the stability of the dentures, esthetics, and time taken for clinical and laboratory procedures. Only randomized clinical trials were included in this study. The methodological quality of the studies was assessed according to the Cochrane risk of bias tool.
Statistical Analysis Used:
Qualitative analysis.
Results:
A total of 144 articles were identified. On excluding 4 duplicates and screening the title and abstracts of the rest of the records based on exclusion criteria only 15 studies were selected for review.
Conclusions:
The use of the face-bow did not yield superior results for the quality of the prosthesis. Therefore, there is no evidence for the utility of face-bow transfer in complete denture treatment. However, no inference could be drawn for its utility in partial denture prosthodontics as there was no study to draw an inference.
Keywords: Arbitrary face-bow, complete denture, face-bow, face-bow transfer
INTRODUCTION
Prosthodontic rehabilitation with indirect restorations that are in harmony with the patients' masticatory system in a minimum amount of time and effort is very crucial.[1] Indirect restorations without any occlusal errors can be achieved with the proper location of the hinge axis.[2] Face-bow is an instrument used to record the spatial relationship of the maxillary arch to some anatomic reference point or points and then transfer this relationship to an articulator; it orients the dental cast in the same relationship to the opening axis of the articulator.[3] Face-bow is regarded as a convenient instrument to transfer maxillary cast to semi-adjustable articulators, also to support the casts while they are being attached to an articulator.[3]
As mentioned in the literature, many authors suggest face-bow transfer is essential for avoiding errors in occlusion of any prosthesis and it is widely followed in most dental colleges worldwide.[4,5,6,7] However, results of clinical studies made to compare the patient response to variations in denture techniques failed to show any significant differences between a complex technique involving hinge axis location, for a face-bow transfer to the articulator, and a standard technique without face-bow and with an arbitrary mounting.[8,9] The argument that the face-bow helps support the maxillary cast while it is being mounted may be true.[1] However, an arbitrary mounting of the maxillary cast can be accomplished with any convenient support material. Studies have shown that there was no difference found for patients, overall satisfaction, and prosthodontists rating of denture quality without using face-bow or with it.[8,9]
As the merit of face-bow usage in prosthodontics remains questionable, the aim of this systematic review is to evaluate the effect of face-bow transfer on the outcome of a dental prosthesis fabricated using it in the available randomized clinical trials available in the literature.
MATERIALS AND METHODS
The primary protocol of this systematic review is in accordance with PRISMA-P statements.[10] Before the start of the review, a review methodology was established based on the recommendations of the Cochrane Handbook for Systematic Reviews of Interventions.[11]
Focused question
The focused question was whether the use of face-bow for the fabrication of prostheses in prosthodontics is better than not using the face-bow.
Outcome measures
The primary outcome variable measured was patient satisfaction (comfort, denture quality, and mastication) with a dental prosthesis made with or without face-bow transfer. The secondary outcome variable was, time duration required for fabrication of the prosthesis, postinsertion occlusal adjustments required, production cost, reliability in transfer, and validity with or without face-bow transfer.
Search strategy
The literature search for articles published up to and including October 2019 in English literature, was performed using the MEDLINE (via PubMed), Cochrane library, and ScienceDirect databases.
The search strategy was based on the PICOS tool [Table 1]. A combination of MeSH terms, and search terms were used to identify the relevant literature [Table 2]. Furthermore, manual search was performed in the reference sections of studies included studies, previous review articles, and relevant texts (Cross-referencing).
Table 1.
Systematic search strategy (patient, intervention, comparison, outcome search strategy)
| Search strategy |
|---|
| Population - Complete/partial removable denture patients, fixed prosthesis patients, occlusal splint patient |
| Intervention - Face-bow transfer |
| Comparison - Prosthesis fabricated with and without face-bow transfer |
| Outcome - Patient satisfaction, time duration required for fabrication of the prosthesis, post-insertion occlusal adjustments required, production cost, reliability in transfer and validity |
| Study design - Randomized control trials |
Table 2.
Systematic search strategy and algorithms for different electronic database search
| MEDLINE (via PubMed) | |
|---|---|
| #1 (population) | (((((((((((((dental prostheses[MeSH Terms]) OR (dental prostheses[Title/Abstract])) OR (complete denture[MeSH Terms])) OR (complete denture[Title/Abstract])) OR (fixed prostheses[Title/Abstract])) OR (denture, removable partial[MeSH Terms])) OR (removable prostheses[Title/Abstract])) OR (occlusal splints[MeSH Terms])) OR (occlusal splint[Title/Abstract])) OR (dental occlusion[MeSH Terms])) OR (record, jaw relation[MeSH Terms])) |
| #2 (intervention) | (((Face-bow[Title/Abstract]) OR (virtual face-bow[Title/Abstract])) OR (extraoral traction appliance[MeSH Terms]))) |
| #3 (comparison) | ((((Conventional techniques[Title/Abstract]) OR (Simpler approach[Title/Abstract])) OR (Without face-bow[Title/Abstract])) OR (simplified[Title/Abstract]))) |
| #4 (outcome) | (((((((treatment outcome[MeSH Terms]) OR (occlusal adjustments[MeSH Terms])) OR (Occlusal contact points[Title/Abstract])) OR (patient satisfaction[MeSH Terms])) OR (patient satisfaction[Title/Abstract])) OR (Reliability[Title/Abstract])) OR (validity[Title/Abstract])) |
| Final search | #1 AND #2 AND #3 AND #4 |
| The COCHRANE Library | |
| #1 | MeSH descriptor: [Dental Prosthesis] explode all trees |
| #2 | (Dental protheses) |
| #3 | MeSH descriptor: [Denture, Complete] explode all trees |
| #4 | (complete denture) |
| #5 | (Fixed prostheses) |
| #6 | (Removable prostheses) |
| #7 | MeSH descriptor: [Occlusal Splints] explode all trees |
| #8 | (Occlusal splint):ti, ab, kw (Title, Abstract, Keyword) |
| #9 | MeSH descriptor: [Dental Occlusion] explode all trees |
| #10 | MeSH descriptor: [Jaw Relation Record] explode all trees |
| #11 | (Facebow):ti, ab, kw |
| #12 | (Virtual facebow):ti, ab, kw |
| #13 | MeSH descriptor: [Extraoral Traction Appliances] explode all trees |
| #14 | (“simplified”):ti, ab, kw |
| #15 | (simpler approach):ti, ab, kw |
| #16 | (conventional technique):ti, ab, kw |
| #17 | (without facebow):ti, ab, kw |
| #18 | MeSH descriptor: [Treatment Outcome] explode all trees |
| #19 | MeSH descriptor: [Occlusal Adjustment] explode all trees |
| #20 | (occlusal contact points):ti, ab, kw |
| #21 | MeSH descriptor: [Patient Satisfaction] explode all trees |
| #22 | (patient satisfaction):ti, ab, kw |
| #23 | (reliability):ti, ab, kw |
| #24 | (validity):ti, ab, kw |
| Final search | (#1 or #2 or #3 or #4 or #5 or #7 or #8 or #9 or #10) AND (#11 or #12 or #13) AND (#14 or #15 or #16 or #17) AND (#18 or #19 or #20 or #21 or #22 or #23 or #24) |
| Science direct | |
| Final search | (“Dental Prostheses” OR “complete denture” OR “fixed prostheses” OR “occlusal splints”) AND (“Facebow”) AND (“Simpler approach” OR “Without facebow”) AND (“occlusal adjustments” OR “patient satisfaction” OR “Reliability”) |
Selection criteria
The present systematic review included only the randomized control trials (RCTs), which analyzed the denture quality, comfort, patient satisfaction, esthetics, and time required to fabricate a dental prosthesis with or without the use of face-bow.
Inclusion criteria
Clinical studies involving patient of any age
Comparison between dental prostheses made with and without face-bow transfer
Assessment of the number of occlusal contacts, patient's satisfaction, masticatory function
Virtual face-bow used in prosthodontics
New or old denture assessment.
Exclusion criteria
Review articles
Articles including face-bow used in orthodontic treatments
Case series and case reports
Techniques reported were excluded from this systematic review.
Screening process
The titles and abstracts were independently screened by two reviewers (VS, NKS), and the articles differences in reviewers was discussed with the third senior author (RC) and appropriate decision was taken. Titles/abstract screening was based on the following questions:
Was the study conducted on patients included prosthodontic rehabilitation?
Were the studies included intervention using a face-bow device?
Was a control group included in the study, treated without using a face-bow device?
Was the treatment outcomes evaluated?
The full text of an article was obtained whether the response was “yes” or “uncertain” to the screening questions. Disagreement regarding inclusion was resolved by discussion with the third author and thus, the studies were finalized to include in the review.
Data extraction
Data were extracted on the general characteristics of the studies (authors; source and year of publication); clinical issues (number, age, gender; intervention strategies; and outcome measures); methodological characteristics (study design and methodological quality); and conclusions. Data entry into the computer was performed by one reviewer.
Assessment of risk of bias and quality
The risk of bias and quality of studies included were analyzed independently by two reviewing authors (VS, NKS). The assessment of RCTs was based on the recommendations given by Cochrane Collaboration tool for assessing risk of bias.[9] Studies were identified as low risk when all the six criteria were met, medium risk when all but one criterion was missing, and high risk, when all but two or more criteria were missing.
RESULTS
Literature search
The database search identified, a total of 140 records of which 25 were from PubMed/Medline, 113 were from ScienceDirect and 2 was from the COCHRANE library. Four records were identified through manual search of previous systematic reviews.[14,17,18,22] Four duplicate records were removed. After removing duplicate, titles and abstracts of remaining 140 records were screened for eligibility. One hundred twenty six records were excluded after title and abstract screening which did not meet the eligibility criteria. Two records were identified through cross referencing of included studies.[12,13] A total of 16 full-text articles were screened for inclusion.[8,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26] One articles was excluded after full-text reading because in which face-bow procedure evaluation was not done.[26] Therefore, a total of 15 articles were included in qualitative analysis [Figure 1].[8,12,13,14,15,16,17,18,19,20,21,22,23,24,25]
Figure 1.
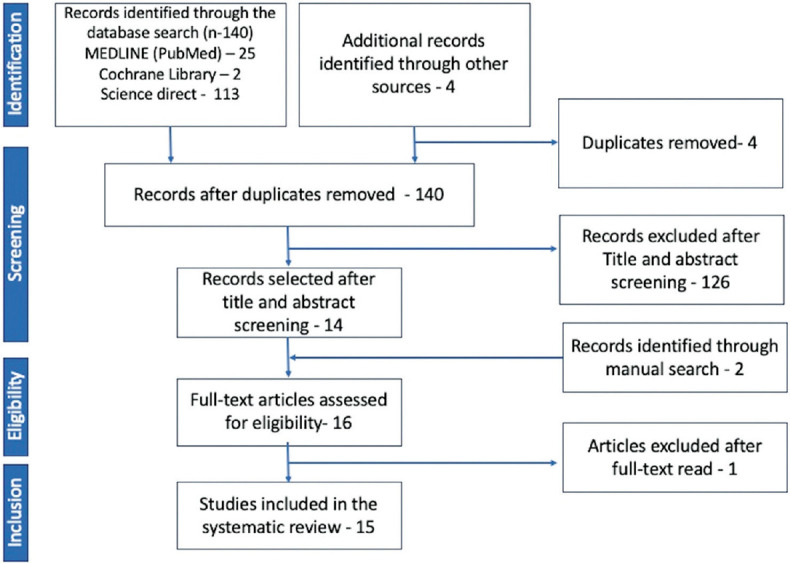
PRISMA flow chart of literature search
Study characteristics
Fifteen studies included were randomized controlled trials. Out of those, 15 included studies, four were double-blinded randomized controlled trials,[14,21,23,24] nine were single-blinded randomized controlled trials,[8,13,15,16,17,18,19,20,22] and two studies did not give information about blinding.[12,25] A total of 406 patients, 196 males and 210 females, in the age group of 21–98 years participated in the studies. A total of 469 pairs of complete Dentures (both maxilla and mandible) were fabricated. One study used a patient simulator and 38 undergraduate students as observers.[25] Of 15 studies included, two studies measured the coincidence of centric relation and centric occlusion on 74 patients,[12,13] five studies used 100 mm visual analogue scale to measure patients' ratings of several denture related factors,[8,15,16,19,21] one study used colorimetric method to check for the masticatory performance.[20]
The outcome measures considered for the systematic review were patient's satisfaction, time duration required for fabrication of the prosthesis, postinsertion occlusal adjustments required, production cost, reliability in transfer and validity. Of the 15 studies included, 9 studies evaluated patient's satisfaction,[8,13,14,15,16,18,20,21,23] three studies evaluated the time taken for fabrication,[18,19,22] three studies evaluated the postinsertion occlusal adjustment required,[8,17,22] 2 studies evaluated production cost.[19,22] Only one study evaluated the reliability in transfer and validity on using face-bow[25] [Table 3].
Table 3.
Randomized clinical trials evaluating the influence of face-bow transfer on prosthodontic work
| Author and year | Type of study | Number of patients | Age (years) | Technique of prosthesis fabrication | Parameters evaluated | Conclusion |
|---|---|---|---|---|---|---|
| Thorp et al., 1978[12] | RCT | 10 | N/A | Recently constructed dentures were duplicated, hinge axis location and transfer using face-bow | Coincidence of CR and CO | No difference |
| Ellinger et al., 1979[13] | Single blinded RCT | 64 | <65 | Group I - standard technique (no face-bow transfer) Group II - complex technique (face-bow transfer) |
Coincidence of CR and CO, denture stability, denture retention and condition of supporting tissues | No difference |
| Nascimento et al., 2004[14] | Double-blinded RCT crossover design | 5 | N/A | Casts of patients duplicated and divided into two groups Group A - mounted using face-bow Group B - mounted without using facebow |
Number of occlusal contacts and patient satisfaction | Better comfort, stability, and lesser stress to supporting tissue without the face-bow transfer |
| Kawai et al., 2005[8] | Single-blinded RCT | 122 | 45–75 | Patients were divided into two groups, each received dentures made by either T or S methods T - with facebow transfer S - without face-bow transfer |
Patient satisfaction, comfort, function of the denture at 3 and 6 months following delivery measured on 100 mm VAS and visual quantitative scale | No significant difference between two groups |
| Heydecke et al., 2007[15] | Single-blinded RCT crossover trial | 22 | 50–85 | Each patient received 2 sets of dentures, one pair manufactured by intraoral tracing and face-bow transfer, another pair without face-bow transfer | Patient satisfaction regarding aesthetic, appearance, ability to chew, ability to speak and retention of the denture patients’ ratings recorded on VAS after 3 months of delivery | Comprehensive method of denture fabrication does not influence chewing ability and patient satisfaction |
| Heydecke et al., 2008[16] | Single blinded RCT crossover trial | 20 | 50–85 | Each patient received 2 sets of dentures, one pair manufactured by intraoral tracing and face-bow transfer, another pair without facebow transfer | General satisfaction, comfort, ability to speak, stability, aesthetics, ease of cleaning and ability to chew | Patients rated their general satisfaction, denture stability and aesthetic significantly better without face-bow |
| Vivell et al., 2009[17] | Single-blinded RCT | 12 | 21–73 | Group I - arbitrary mounting Group II - hinge axis location, face-bow transfer and mounting |
Occlusal adjustments required | No difference |
| Kumar and d’souza 2010[18] | Single-blinded RCT | 20 | 58–64 | Single-blinded RCT Two sets of dentures for each subject, Technique I – face-bow transfer was done Technique II - without face-bow transfer |
Number of occlusal contacts, time taken, aesthetics, comfort and stability | Better results without face bow balanced occlusion was provided without face-bow |
| Kawai et al., 2010[19] | Single-blinded RCT | 122 | 45–75 | Patients were divided into two groups, each received dentures made by either T or S methods T - with face-bow transfer S - without face-bow transfer |
Production cost and clinician’s labor time | Mean total cost of fabrication of denture was significantly higher and clinician’s spent 90 min longer on clinical care with the face-bow transfers |
| Cunha et al., 2013[20] | Single-blinded RCT | 42 | 46–57 | Group S - patient’s receiving dentures fabricated by simplified method without using face-bow Group C - patients receiving conventionally fabricated denture by using face-bow Group DN - external comparator |
Masticatory performance (colorimetric method) | Better masticatory ability without face-bow use |
| Omar et al., 2013[21] | Double-blinded RCT | 43 | 35–78 | Group I - omission of secondary cast fabrication Group II - omission of secondary cast and face-bow articulator mounting Group III - omission of face-bow mounting Group IV - no steps omitted (control group) |
General satisfaction with new denture, ability to chew | No significant differences within groups |
| Vecchia et al., 2014[22] | Single-blinded RCT | 42 | 57–74 | Group C - denture were fabricated by conventional methods using face-bow Group S - dentures were fabricated by simplified method without using face-bow |
Production cost, clinician’s and dental assistant’s labor time, postinsertion adjustments | Simplified method was found to be less costly for patients, more time efficient for clinicians, assistants and patients |
| von Stein-Lausnitz et al., 2017[23] | Double-blinded RCT | 32 | 44–98 | Group I - mean setting for the transfer of CDs into semi adjustable articulator Group II – face-bow transfer into articulator according to arbitrary hinge axis |
Laboratory and clinical occlusal contact points, extent of vertical shift in relation to the number of laboratory occlusal contacts | No substantial difference by the use of arbitrary face-bow compared to mean setting |
| von Stein-Lausnitz et al., 2018[24] | Double-blinded RCT | 32 | 44–98 | Group I - mean setting for the transfer of CD’s into semi-adjustable articulator Group II – face-bow transfer into articulator according to arbitrary hinge axis |
Oral health index, amount of physical pain, number of sore spots | Face-bow registration has no positive effect on OHRqOL |
| Ahlers et al., 2018[25] | RCT | N/A | N/A | Group I - operators using face-bow transfer to mount casts Group II - operators using average values to mount casts |
Reliability in transfer and validity | Use of an arbitrary face-bow significantly improves transfer reliability and validity |
CR: Centric relation, CO: Centric occlusion, CD: Complete denture, RCT: Randomized controlled trial, VAS: Visual analog scale, OHRqOL: Oral health-related quality of life
No clinical trials were identified comparing the construction of removable partial dentures or fixed prostheses with or without face-bow transfer.
Assessment of risk of bias and quality
Risk of bias and quality assessment of RCTs was conducted using Cochrane Collaboration tool for assessing risk of bias [Table 4]. Five studies showed a high risk of bias (Agency for Healthcare Research and Quality [AHRQ] score-Poor).[12,13,17,18,22] six studies showed medium risk of bias (AHRQ score-Fair).[14,15,16,19,20,21] four studies showed low risk of bias (AHRQ score-Good).[8,23,24,25]
Table 4.
Cochrane risk of bias tool for randomized controlled trials
| Selected studies | Adequate sequence generation | Allocation concealment | Selective reporting | Blinding of participants and personnel | Blinding of outcome assessment | Incomplete outcome data | Other bias | AHRQ score |
|---|---|---|---|---|---|---|---|---|
| Thorp et al., 1978[12] | Unclear | Unclear | Yes | No | No | No | Unclear | Poor |
| Ellinger et al., 1979[13] | Unclear | Yes | Unclear | Yes | Unclear | Unclear | Unclear | Poor |
| Nascimento et al., 2004[14] | Yes | Yes | No | Yes | Yes | Yes | Unclear | Fair |
| Kawai et al., 2005[8] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Good |
| Heydecke et al., 2007[15] | Yes | Yes | Yes | Yes | Yes | Yes | Unclear | Fair |
| Heydecke et al., 2008[16] | Yes | Yes | Yes | Yes | Yes | Yes | Unclear | Fair |
| Vivell et al., 2009[17] | Yes | Yes | Unclear | Unclear | Yes | Unclear | Unclear | Poor |
| Kumar and D’souza 2010[18] | Unclear | Yes | Yes | Unclear | Yes | Yes | Unclear | Poor |
| Kawai et al., 2010[19] | Yes | Yes | Yes | Unclear | Yes | Yes | Unclear | Fair |
| Cunha et al., 2013[20] | Yes | Yes | Yes | Yes | Yes | Yes | Unclear | Fair |
| Omar et al., 2013[21] | Yes | Yes | Yes | Yes | Yes | Yes | Unclear | Fair |
| Vecchia et al., 2014[22] | Yes | Yes | Yes | Unclear | Yes | Yes | Unclear | Poor |
| von Stein-Lausnitz et al., 2017[23] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Good |
| von Stein-Lausnitz et al., 2018[24] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Good |
| Ahlers et al., 2018[25] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Good |
AHRQ: Agency for Healthcare Research and Quality
DISCUSSION
In various prosthodontic procedures, recording the maxillomandibular relationship becomes important. Orientation jaw relation establishes the reference in the cranium and orients the casts of the edentulous jaws to the articulator, usually by using some type of a face-bow record.[27] Conventionally, face-bow can be classified into two basic types: Arbitrary or kinematic axis types. Face-bow can be configured to locate and transfer the mandibular transverse horizontal axis points to an articulator.[28] However, the axis of rotation belongs to the movable mandible and many rotational centers are possible. To determine the validity of the face-bow use in prosthodontic rehabilitation, occlusion, esthetics, and overall patient satisfaction with the prosthesis are considered to be the appropriate outcome measures. For aesthetics, there would be variations in the anteroposterior plane and/or the mediolateral plane. For occlusion, given that the horizontal axis of the articulator may not be the same as the horizontal axis of the mandible, errors would occur at the insertion.[29]
The results of this review study do not support the null hypothesis that the construction of dental prostheses with face-bow transfer may present better clinical results than simpler approaches. The use of face-bow device in prosthodontic rehabilitation does not yield better results when compared to a simplified technique of not using a face-bow device. If data from reviewed studies comparing the use of face-bow device versus not using it, is compared, the evidence base indicates either no significant difference,[8,12,13,15,17,21,23,24] or better results without the face-bow transfer.[14,16,18,19,20,22,25]
During the last many now, several studies have confirmed that face-bow transfer does not offer clinically significant advantages compared to an average mounting according to the Scandinavian approach.[30,31,32] Most of the studies included measured patient's satisfaction in terms of aesthetics, retention, stability, ability to chew, and the speech by documenting patients' ratings on the 100 mm visual analogue scale and concluded as no significant difference between the technique following face-bow transfer and technique not using the face-bow transfer.[8,13,15,17,21] some studies found better results in terms of patients' satisfaction with the dentures fabricated by a simplified technique of not using the face-bow device.[14,16,18,20]
It is been documented that, a quality denture in terms of occlusal contacts in centric relation and esthetics can be achieved better without the use of face-bow.[14,18] In addition, there was no significant difference in the coincidence of centric relation and centric occlusion with and without the face-bow transfer.[12,13] In terms of the oral health-related quality of life for the patients receiving dentures fabricated using the face-bow device has no positive effect when compared with the dentures fabricated by not using the face-bow device.[24] Moreover, the complex method of denture fabrication which uses face-bow transfer is 24.5% costlier in terms of materials and labor cost, taking 36% more time for the whole procedure of fabricating denture when compared to the simplified method where face-bow is not used.[19]
In contrast, only one randomized control trial reported that, the use of an arbitrary face-bow significantly improves transfer reliability and validity of the maxillary cast when compared to the transfer method relying only on the average values.[25] However, this study was carried on a jaw of the dummy model, where in the assessment of the operators who transferred the face-bow information to the articulator was assessed and not the patient outcome. However, ultimately, patient satisfaction and oral health related quality of patient life with dentures determine the success of the denture.
As a clinician, the cost of providing prosthodontic rehabilitation is a major concern while deciding between the various treatment modalities and alternatives as the most appropriate treatment modality chosen should be cost-effective, time efficient for both clinician and dental assistants and at the same time provide utmost care to the patient in terms of the satisfaction as well as aesthetics. The studies included in this review establish that a simplified method of not using the face-bow device in denture fabrication is more cost effective, time efficient as well as provide equal or sometimes better satisfaction to the patients in terms of denture stability, retention, comfort, and aesthetics. However, in all the randomized controlled trials included in this systematic review, complete dentures were fabricated by experienced specialists and prosthodontists, hence to generalize the result of this study and infer whether an inexperienced undergraduate student or a clinician would be able to achieve the same results without using a face-bow device, is not possible. To add a note on teaching and use of face-bow, in Scandinavian countries, the teaching and use of face-bows have been abandoned, and in china, where 97% of Prosthodontists reported that they seldom used face-bows.[9] In United states use of face-bow is taught in 75% of U.S. dental schools. It is difficult to change the mindset of the many professional colleagues, even after having so much of documented evidence favoring no scientific evidence in using face-bow, with manufacturers providing new face-bow designs, teaching curriculums of universities recommend its usage. It would make more viable that these researchers produce more clinical evidence published with scientific reasoning of use of face-bow in prosthodontics.
CONCLUSIONS
There is no clinical evidence which can be drawn in favour of the use of Facebow to be essential in construction of complete denture, which enhances the denture performance.
Simpler approaches for the construction of complete denture may present similar results to more complex techniques.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.George A Zarb, Hobkirk J, Eckert S, Jacob R. Prosthodontic Treatment for Edentulous Patients: Complete Denture and Implant Supported Prostheses. South Asia Edition: Elsevier; 2015. [Google Scholar]
- 2.Brotman DN. Hinge axes Part II. Geometric significance of the transverse axis. J Prosthet Dent. 1960;10:436–40. [Google Scholar]
- 3.Driscoll CF, Freilich MA, Guckes AD, Knoernschild KL, McGarry TJ. The glossary of prosthodontic terms, GPT-9. J Prosthet Dent. 2017;117:E1–105. [Google Scholar]
- 4.Carlsson GE. Critical review of some dogmas in prosthodontics. J Prosthodont Res. 2009;53:3–10. doi: 10.1016/j.jpor.2008.08.003. [DOI] [PubMed] [Google Scholar]
- 5.Rashedi B, Petropoulos VC. Preclinical complete dentures curriculum survey. J Prosthodont. 2003;12:37–46. doi: 10.1053/jpro.2003.1. [DOI] [PubMed] [Google Scholar]
- 6.Lynch CD, Singhrao H, Addy LD, Gilmour AS. The teaching of fixed partial dentures in undergraduate dental schools in Ireland and the United Kingdom. J Oral Rehabil. 2010;37:908–15. doi: 10.1111/j.1365-2842.2010.02106.x. [DOI] [PubMed] [Google Scholar]
- 7.Farias-Neto A, Dias AH, de Miranda BF, de Oliveira AR. Face-bow transfer in prosthodontics: A systematic review of the literature. J Oral Rehabil. 2013;40:686–92. doi: 10.1111/joor.12081. [DOI] [PubMed] [Google Scholar]
- 8.Kawai Y, Murakami H, Shariati B, Klemetti E, Blomfield JV, Billette L, et al. Do traditional techniques produce better conventional complete dentures than simplified techniques? J Dent. 2005;33:659–68. doi: 10.1016/j.jdent.2005.01.005. [DOI] [PubMed] [Google Scholar]
- 9.Wang MQ, Xue F, Chen J, Fu K, Cao Y, Raustia A. Evaluation of the use of and attitudes towards a face-bow in complete denture fabrication: A pilot questionnaire investigation in Chinese prosthodontists. J Oral Rehabil. 2008;35:677–81. doi: 10.1111/j.1365-2842.2007.01835.x. [DOI] [PubMed] [Google Scholar]
- 10.Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4:1. doi: 10.1186/2046-4053-4-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Higgins JP, Green S. Cochrane handbook for systematic reviews of interventions 4.2.6 [updated September 2006] Cochrane Lib. 2016;2006:4. [Google Scholar]
- 12.Thorp ER, Smith DE, Nicholls JI. Evaluation of the use of a face-bow in complete denture occlusion. J Prosthet Dent. 1978;39:5–15. doi: 10.1016/s0022-3913(78)80039-0. [DOI] [PubMed] [Google Scholar]
- 13.Ellinger CW, Somes GW, Nicol BR, Unger JW, Wesley RC. Patient response to variations in denture technique. Part III: Five-year subjective evaluation. J Prosthet Dent. 1979;42:127–30. doi: 10.1016/0022-3913(79)90160-4. [DOI] [PubMed] [Google Scholar]
- 14.Nascimento DF, Patto RB, Marchini L, da Cunha VP. Double-blind study for evaluation of complete dentures made by two techniques with and without face-bow. Braz J Oral Sci. 2004;3:439–45. [Google Scholar]
- 15.Heydecke G, Akkad AS, Wolkewitz M, Vogeler M, Türp JC, Strub JR. Patient ratings of chewing ability from a randomised crossover trial: Lingualised vs. first premolar/canine-guided occlusion for complete dentures. Gerodontology. 2007;24:77–86. doi: 10.1111/j.1741-2358.2007.00153.x. [DOI] [PubMed] [Google Scholar]
- 16.Heydecke G, Vogeler M, Wolkewitz M, Türp JC, Strub JR. Simplified versus comprehensive fabrication of complete dentures: Patient ratings of denture satisfaction from a randomized crossover trial. Quintessence Int. 2008;39:107–16. [PubMed] [Google Scholar]
- 17.Vivell C, Slavicek G, Slavicek R. Arbitrary versus exact mounting procedure during fabrication of intraoral splints: An exploratory randomized controlled clinical trial. Int J Stomatol Occl Med. 2009;2:99–105. [Google Scholar]
- 18.Kumar M, D'Souza D. Comparative evaluation of two techniques in achieving balanced occlusion in complete dentures. Med J Armed Forces India. 2010;66:362–6. doi: 10.1016/S0377-1237(10)80019-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kawai Y, Murakami H, Takanashi Y, Lund JP, Feine JS. Efficient resource use in simplified complete denture fabrication. J Prosthodont. 2010;19:512–6. doi: 10.1111/j.1532-849X.2010.00628.x. [DOI] [PubMed] [Google Scholar]
- 20.Cunha TR, Della Vecchia MP, Regis RR, Ribeiro AB, Muglia VA, Mestriner W, Jr, et al. A randomised trial on simplified and conventional methods for complete denture fabrication: Masticatory performance and ability. J Dent. 2013;41:133–42. doi: 10.1016/j.jdent.2012.09.008. [DOI] [PubMed] [Google Scholar]
- 21.Omar R, Al-Tarakemah Y, Akbar J, Al-Awadhi S, Behbehani Y, Lamontagne P. Influence of procedural variations during the laboratory phase of complete denture fabrication on patient satisfaction and denture quality. J Dent. 2013;41:852–60. doi: 10.1016/j.jdent.2013.07.013. [DOI] [PubMed] [Google Scholar]
- 22.Vecchia MP, Regi RR, Cunha TR, de Andrade IM, da Matta JC, de Souza RF. Randomized trial on simplified and conventional methods for complete denture fabrication: Cost analysis. J Prosthodont. 2014;23:182–91. doi: 10.1111/jopr.12090. [DOI] [PubMed] [Google Scholar]
- 23.von Stein-Lausnitz M, Schmid S, Blankenstein FH, Peroz I, Beuer F, Sterzenbach G. Influence of a face-bow on oral health-related quality of life after changing the vertical dimension in the articulator: A randomized controlled trial. Part II. Clin Oral Investig. 2017;22:433–42. doi: 10.1007/s00784-017-2130-2. [DOI] [PubMed] [Google Scholar]
- 24.von Stein-Lausnitz M, Sterzenbach G, Helm I, Zorn A, Blankenstein FH, Ruge S, et al. Does a face-bow lead to better occlusion in complete dentures? A randomized controlled trial: Part I. Clin Oral Investig. 2018;22:773–82. doi: 10.1007/s00784-017-2152-9. [DOI] [PubMed] [Google Scholar]
- 25.Ahlers MO, Edelhoff D, Jakstat HA. Reproduction accuracy of articulator mounting with an arbitrary face-bow vs. average values-a controlled, randomized, blinded patient simulator study. Clin Oral Investig. 2019;23:1007–14. doi: 10.1007/s00784-018-2499-6. [DOI] [PubMed] [Google Scholar]
- 26.Ceruti P, Mobilio N, Bellia E, Borracchini A, Catapano S, Gassino G. Simplified edentulous treatment: A multi-center randomized controlled trial to evaluate the timing and clinical outcomes of the technique. J Prosthet Dent. 2017;118:462–7. doi: 10.1016/j.prosdent.2017.01.024. [DOI] [PubMed] [Google Scholar]
- 27.Carlsson GE. Facts and fallacies: An evidence base for complete dentures. Dent Update. 2006;33:134. doi: 10.12968/denu.2006.33.3.134. [DOI] [PubMed] [Google Scholar]
- 28.Preston JD. A reassessment of the mandibular transverse horizontal axis therory. J Prosthet Dent. 1979;41:605–13. doi: 10.1016/0022-3913(79)90054-4. [DOI] [PubMed] [Google Scholar]
- 29.Nagy WW, Goldstein GR. Facebow use in clinical prosthodontic practice. J Prosthodont. 2019;28:772–4. doi: 10.1111/jopr.12944. [DOI] [PubMed] [Google Scholar]
- 30.Pröschel PA, Maul T, Morneburg T. Predicted incidence of excursive occlusal errors in common modes of articulator adjustment. Int J Prosthodont. 2000;13:303–10. [PubMed] [Google Scholar]
- 31.Shodadai SP, Türp JC, Gerds T, Strub JR. Is there a benefit of using an arbitrary facebow for the fabrication of a stabilization appliance? Int J Prosthodont. 2001;14:517–22. [PubMed] [Google Scholar]
- 32.Petropoulos VC, Rashedi B. Complete denture education in U.S. dental schools. J Prosthodont. 2005;14:191–7. doi: 10.1111/j.1532-849X.2005.03043.x. [DOI] [PubMed] [Google Scholar]


