Abstract
Aim:
To evaluate the microleakage of metallic copings luted with three different commercially available luting cements.
Setting and Design:
Comparative evaluation in vitro study.
Materials and Methods:
Thirty replicas of abutment analog were milled and divided into 3 groups. Nickel chromium copings were fabricated; marginal gap was evaluated with optical microscope and luted with Zinc Oxide Non Eugenol cement, Zinc Polycarboxylate cement and Zinc Phosphate cement. After Thermocycling, cemented specimens were placed into 0.5% aqueous solution of basic fuchsin solution for 24 hours for dye penetration. Copings were longitudinally sectioned and microleakage scores were evaluated.
Statistical Analysis Used:
Kruskal-Wallis analysis of variance (ANOVA) followed by Chi-Square test. Pairwise comparison of groups with Mann Whitney U test.
Result:
Mean microleakage score was least for Zinc Phosphate cement (1.075 ± 0.85) followed by Zinc Polycarboxylate cement (1.80± 0.23) and most for Zinc Oxide Non Eugenol (2.1± 0.37). The results of the study were statistically significant, P < 0.05.
Conclusions:
Within the limitations of the study, it was found that all cements exhibited certain amount of microleakage. Zinc Phosphate cement exhibited a mean microleakage score that was significantly lower than Zinc Oxide Non Eugenol cement and Zinc Polycarboxylate cement. When microleakage scores of Zinc Oxide Non Eugenol cement and Zinc Polycarboxylate cement were compared, the difference was found to be insignificant indicating that microleakage in these cements is similar.
Keywords: Cement solubility, implant abutments, luting cements, microleakage
INTRODUCTION
Dental implants have an important role in mainstream dental practice today to restore esthetics, contour, occlusion, function, comfort, speech, and health. From 1980s to early 1990s, there was a strong preference for screw-retained restorations, which subsequently changed to cement-retained restorations.[1] In screw-retained restorations, fastening screws are the main form of retention, which fixes the prosthesis to abutment and, therefore, the abutment to implant. These are mainly indicated in the cases with restricted interarch space that limits the specified height of the axial wall for retention of cement-retained prosthesis. The benefits of screw-retained prosthesis are satisfactory crown retention, cement free gingival sulcus area, and crown retrievability. There are some complications which include abutment screw loosening, fracture of fastening screw, optimum location of the access hole for precise placement, ceramic chip off around access hole, fracture of the abutment, etc.[2,3] The incidence of abutment screw loosening has been reported in 2%–45% of cases in the review of 17 studies.[4,5]
With the recent development in techniques, the survival rate of implants progressed rapidly from 50% to 90%. Due to this increased survival rate, the matter of retrievability has not been clinically significant.[6] It is usually troublesome to achieve a passive fit coping for screw-retained implant prosthesis due to which popularity of cement retained prosthesis became very high. The minor discrepancies for the fit of the prosthesis can be compensated with the cement space present between the abutment and the prosthesis. Cement retained implant prosthesis provides optimum occlusion, esthetics, less ceramic fracture, easier axial loading, use of conventional prosthetic technique, less appointments, simple and lower cost.[2,3,6]
Retrievability is the main disadvantage of cement-retained prosthesis.[1,2,3,4,5,6,7,8] The selection of cements for an implant-supported restorations should be based on the desire of retrievability, the anticipated amount of retention required and the ease of cement removal. According to literature, in implant dentistry most commonly used cements for luting of the final prosthesis are zinc oxide eugenol with or without ethoxy benzoic acid, zinc phosphate cement and zinc polycarboxylate cement. After the retrieval of the prosthesis, the removal of the remaining Glass Ionomer Cement from abutment becomes very difficult because of its property of adhesion. The high tensile strength of composite resin cement makes the prosthesis difficult to retrieve.[1,2,3,7]
Other issues encountered with the cement-retained prosthesis are microleakage and inflammation of gingiva around the implant site. Microleakage is crucial consideration while selecting luting cements. Leakage around crown margins are directly proportional to cement solubility, film thickness, adherence to substrate, dimensional changes, and poor adaptation of the prosthesis with abutment.[2,7]
Microleakage results from dead spaces formed by luting cement dissolution. Peri-implantitis can occur especially in subgingival areas due to the accumulation of toxins in these dead spaces resulting in bone loss around the implants.[1,8] This bone loss could be stress induced, microorganism induced or combination of both. The oxygen tension reduction takes place when the bone loss from stress and microorganisms deepens the sulcular crevice. Furthermore, the anaerobic bacteria act as primary promoters of continued bone loss, resulting implant failure. Keller et al. considered that this effect could be associated with marginal gap width and the inability of cement to prevent leakage at the interface.[9] Thus an ideal cement for implant-supported restorations should have properties of minimal microleakage, adequate retention, and easy retrieval.[1,2,3,6]
Various studies have been conducted in the past to study microleakage at tooth- prosthesis interface.[10,11,12,13,14] Very little literature is available on microleakage at implant-abutment- prosthesis interface.[15,16,17] Hence, a study was conducted to evaluate the microleakage at implant abutment and prosthesis interface in cemented implant-supported prosthesis which were cemented with three different commercially available luting cements.
MATERIALS AND METHODS
The study has been approved by institutional review board. Thirty replicas of abutment analog having length 5 mm, width of platform 4.8 mm, taper 6°, broad chamfer finish line and three anti-rotation grooves over it which end 1 mm above finish line were milled from titanium rods [Figures 1 and 2].
Figure 1.

Abutment analog used in the study
Figure 2.
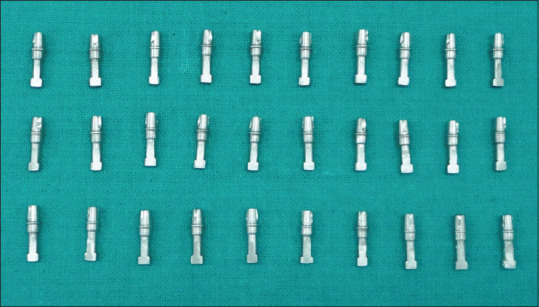
Thirty abutment analog samples
Fabrication of metal copings
Each abutment analog was mounted in dental plaster along the long axis for stabilization. Two layers of die spacer were applied on abutments analogs 1mm short of margin. Two different colored die spacers were used to ensure even thickness of the die spacer on the abutment. A die lubricant was applied over abutments to help easy separation of the pattern. Wax pattern was prepared using type II inlay wax having uniform thickness of 0.5 mm. For even thickness of wax pattern for other abutment analogs, a putty index was prepared from this wax pattern. The remaining wax patterns were prepared using the putty index. Wax near the margin was scraped off and readapted for marginal refinement. A sprue former was made of wax, and a reservoir was attached to the sprue. The length of the sprue was adjusted so that the wax pattern was approximately ¼ inch from the casting ring. A non-asbestos ring liner was applied inside the casting ring. Wetting agent was applied over the wax pattern to prevent any bubble formation. Wax patterns were invested into phosphate bonded investment, burnout procedure was carried out, and casting was done using Ni-Cr alloy in induction casting machine. Castings were divested, desprued and sandblasted with aluminum oxide particles of 110–125 micron under 2 bar pressure to remove residual investment material. Nodules were removed from the fitting surface with the help of rotary instrument. Copings were finished and polished using polishing burs. Each coping was checked under optical microscope for marginal discrepancy [Figure 3] and the specimens with marginal discrepancy <40 μm were selected for the study.
Figure 3.

Evaluation of marginal discrepancy under optical microscope
Cementation
The copings with their respective abutment analog were randomly divided into three groups having 10 samples in each. Cementation was done with three luting agents commonly used in cementation of implant-supported prosthesis. The cements were:
Zinc oxide non-eugenol luting cement (3M)
Zinc polycarboxylate cement (Dentsply)
Zinc phosphate luting cement (GC).
Cementation was done in accordance with the manufacturer's instructions for mixing time, mixing conditions, and powder: liquid ratio. Luting agent was applied completely on all internal walls of copings and was then seated onto abutment analog with firm figure pressure for 10 s followed by 2 kg axial load for 5 min with the help of the customized holding device. For equal distribution of load on metallic coping, the customized holding device was designed in such a way that the circumference of the head of weight was 1 mm short of circumference of occlusal surface of coping [Figure 4]. After setting, excess cement was removed with the help of hollenback carver. Specimens were examined visually to confirm complete seating of copings onto abutment analogs and allowed to set for 24 h.
Figure 4.
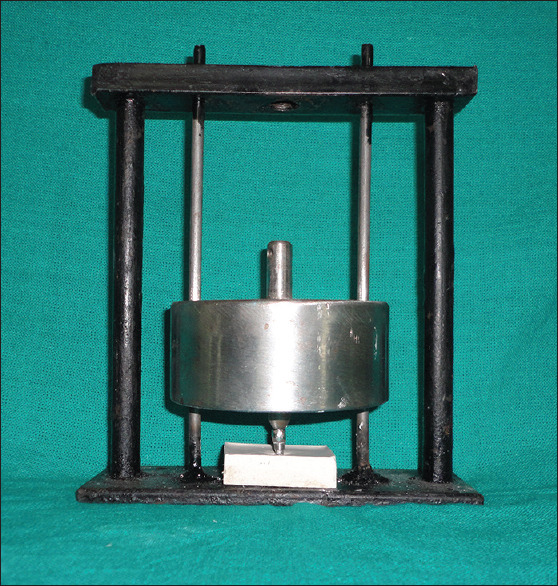
Customized holding device used for cementation
Thermocycling
After 24 h, the cemented specimens were removed from plaster blocks and subjected to 5000 cycles of thermocycling between 5° and 55° C with dwell time of 10 s and transfer time of 5 s in the thermocycling unit.
Dye penetration
After thermocycling, cemented specimens were placed into 0.5% aqueous solution of basic fuchsin solution for 24 h for dye penetration.
Evaluation of microleakage
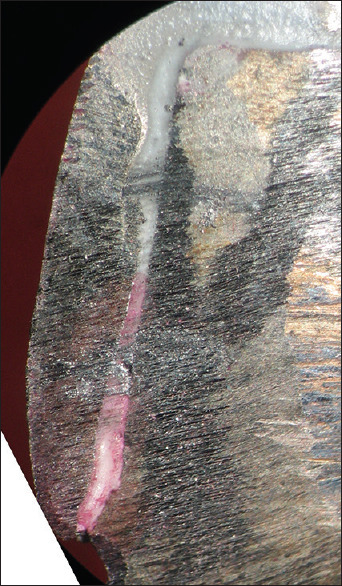
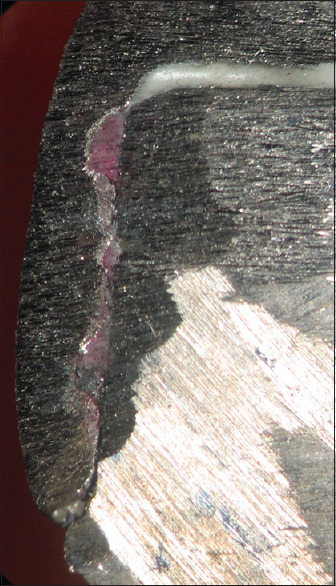
Microleakage was evaluated by using multiple surface scoring methods for each specimen. After keeping the cemented specimen in dye solution for 24 h, the specimens were sectioned longitudinally in bucco-lingual axis with the help of carborundum disc [Figures 5 and 6]. Microleakage score was recorded at two abutment-coping interfaces of each section, thus making a total of four scores for each specimen. Two markings were made on the axial walls, which were at 1/3rd and 2/3rd of the length of abutment analog. The sectioned specimens were placed under stereomicroscope under ×40 for the evaluation of microleakage [Figure 7]. Microleakage was scored by the method used by Tjan et al. Microleakage scores used were:
Figure 5.

Sectioned specimen
Figure 6.

Thirty sectioned specimen samples
Figure 7.

Stereomicroscope used for evaluation of microleakage
0 No microleakage seen on the axial wall of the sectioned specimen
1 Microleakage seen up to 1/3rd the length on the axial wall of the sectioned specimen [Figure 8]
Figure 8.

Microleakage score 1 (upto 1/3rd the length of axial wall)
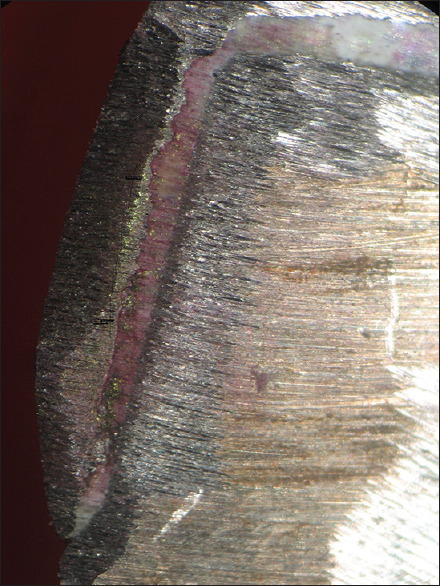
2 Microleakage seen up to 2/3rd the length on the axial wall of the sectioned specimen [Figure 9]
Figure 9.
Microleakage score 2 (upto 2/3rd the length of axial wall)
3 Microleakage seen along the full length of the axial wall of the sectioned specimen [Figure 10]
Figure 10.
Microleakage score 3 (along full length of axial wall)
4 Microleakage seen on the occlusal surface of the sectioned specimen [Figure 11].
Figure 11.
Microleakage score 4 (microleakage seen on occlusion surface)
RESULTS
Microleakage scores were recorded for each group. Data were tabulated and analyzed using Kruskal–Wallis analysis of variance (ANOVA) followed by Chi-square test. Pairwise comparison of groups was made with Mann–Whitney U-test. Statistical significance was set at P < 0.05.
Tables 1–3 show microleakage scores for specimens cemented with zinc oxide non-eugenol, zinc polycarboxylate and zinc phosphate luting cements, respectively. All specimens exhibited microleakage to different degrees. Mean microleakage score was least for Zinc Phosphate cement (1.075 ± 0.85), followed by Zinc Polycarboxylate cement (1.80 ± 0.23) and most for zinc oxide non-eugenol (2.1 ± 0.37) [Graph 1].
Table 1.
Microleakage scores in specimens cemented with zinc oxide noneugenol luting cement (Group I)
| Specimen number | Microleakage scores | ||||
|---|---|---|---|---|---|
| Buccal 1 | Buccal 2 | Lingual 1 | Lingual 2 | Mean score | |
| 1 | 2 | 2 | 1 | 1 | 1.50 |
| 2 | 2 | 1 | 1 | 1 | 1.25 |
| 3 | 2 | 2 | 1 | 1 | 1.50 |
| 4 | 2 | 2 | 3 | 3 | 2.50 |
| 5 | 3 | 4 | 2 | 2 | 2.75 |
| 6 | 2 | 2 | 1 | 1 | 1.50 |
| 7 | 3 | 3 | 2 | 2 | 2.50 |
| 8 | 1 | 1 | 2 | 2 | 1.50 |
| 9 | 4 | 4 | 4 | 4 | 4.00 |
| 10 | 2 | 2 | 2 | 2 | 2.00 |
| Total mean score | 2.1±0.85 | ||||
Table 3.
Microleakage scores in specimens cemented with zinc phosphate luting cement (Group III)
| Specimen number | Microleakage scores | ||||
|---|---|---|---|---|---|
| Buccal 1 | Buccal 2 | Lingual 1 | Lingual 2 | Mean score | |
| 1 | 1 | 2 | 1 | 1 | 1.25 |
| 2 | 1 | 1 | 2 | 2 | 1.50 |
| 3 | 1 | 1 | 0 | 0 | 0.50 |
| 4 | 1 | 1 | 1 | 1 | 1.00 |
| 5 | 0 | 0 | 1 | 1 | 0.50 |
| 6 | 2 | 2 | 1 | 1 | 1.50 |
| 7 | 1 | 1 | 2 | 2 | 1.50 |
| 8 | 1 | 1 | 1 | 1 | 1.00 |
| 9 | 1 | 1 | 1 | 1 | 1.00 |
| 10 | 1 | 1 | 1 | 1 | 1.00 |
| Total mean score | 1.075±0.37 | ||||
Graph 1.
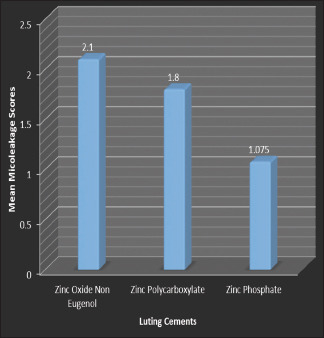
The mean microleakage scores of Group I (zinc oxide noneugenol luting cement), Group II (zinc polycarboxylate luting cement) and Group III (zinc phosphate luting cement)
Table 2.
Microleakage scores in specimens cemented with zinc polycarboxylate luting cement (Group II)
| Specimen number | Microleakage scores | ||||
|---|---|---|---|---|---|
| Buccal 1 | Buccal 2 | Lingual 1 | Lingual 2 | Mean score | |
| 1 | 1 | 1 | 2 | 2 | 1.50 |
| 2 | 2 | 1 | 2 | 2 | 1.75 |
| 3 | 1 | 2 | 2 | 2 | 1.75 |
| 4 | 2 | 2 | 2 | 2 | 2.00 |
| 5 | 2 | 2 | 2 | 2 | 2.00 |
| 6 | 1 | 1 | 2 | 2 | 1.50 |
| 7 | 1 | 1 | 2 | 2 | 1.50 |
| 8 | 2 | 2 | 2 | 2 | 2.00 |
| 9 | 2 | 2 | 2 | 2 | 2.00 |
| 10 | 2 | 2 | 2 | 2 | 2.00 |
| Total mean score | 1.8±0.23 | ||||
Table 4 shows descriptive statistics for the microleakage scores. On subjecting the values of mean microleakage scores to Kruskal–Wallis ANOVA followed by Chi-square test, the value of P = 0.001 indicating that there was significant difference in mean microleakage scores of the groups tested (P < 0.05) [Table 5].
Table 4.
Descriptive statistics
| NPar tests | |||||
|---|---|---|---|---|---|
| n | Mean | SD | Minimum | Maximum | |
| Total | 30 | 1.6583 | 0.69009 | 0.50 | 4.00 |
| Cement | 30 | 2.00 | 0.830 | 1 | 3 |
SD: Standard deviation
Table 5.
Statistical analysis for microleakage with all luting cements using Kruskal–Wallis test
| Ranks | ||||
|---|---|---|---|---|
| Cement | n | Mean rank | ||
| Group I | 10 | 19.90 | ||
| Group II | 10 | 19.70 | ||
| Group III | 10 | 6.90 | ||
| Total | 30 | |||
| Test statisticsa, b | Difference_score | |||
| χ2 | 15.033 | |||
| df | 2 | |||
| Asymptotic significant | 0.001 | |||
aKruskal–Wallis test,
bGrouping variable: Group
Tables 6–8 show the pairwise comparison of microleakage scores of the three cements by Mann–Whitney U-test. On comparing microleakage scores of zinc oxide non-eugenol luting cement with zinc polycarboxylate luting cement, the value of P = 0.796 (>0.05), indicating that the difference in the mean microleakage scores of both the cements is insignificant [Table 6]. On comparing microleakage scores of zinc polycarboxylate luting cement with Zinc Phosphate luting cement, the value of P = 0.000 (P < 0.05), indicating that the difference in the mean microleakage scores of both the cements is significant [Table 7]. On comparing microleakage scores of zinc oxide non-eugenol luting cement with Zinc Phosphate luting cement, the value of P = 0.001 (P < 0.05), indicating that the difference in the mean microleakage scores of both the cements is significant [Table 7].
Table 6.
Pairwise comparison of Group I (zinc oxide noneugenol luting cement) and Group II (zinc polycarboxylate luting cement) using Mann–Whitney U-test
| Ranks | ||||
|---|---|---|---|---|
| Cement | n | Mean rank | Sum of ranks | |
| Total | Group I | 10 | 10.85 | 108.50 |
| Group II | 10 | 10.15 | 101.50 | |
| Total | 20 | |||
| Test statisticsb | Difference_score | |||
| Mann–Whitney U | 46.500 | |||
| Wilcoxon W | 101.500 | |||
| Z | −0.274 | |||
| Asymptotic significant (two-tailed) | 0.784 | |||
| Exact significant (two×[one-tailed significant]) | 0.796a | |||
aNot corrected for ties,
bGrouping variable: Group
Table 8.
Pairwise comparison of Group I (zinc oxide noneugenol luting cement) and Group III (zinc phosphate luting cement) using Mann–Whitney U-test
| Ranks | |||
|---|---|---|---|
| Cement | n | Mean rank | Sum of ranks |
| Group I | 10 | 14.55 | 145.50 |
| Group III | 10 | 6.45 | 64.50 |
| Total | 20 | ||
| Test statisticsb | Difference_score | ||
| Mann–Whitney U | 9.500 | ||
| Wilcoxon W | 64.500 | ||
| Z | −3.144 | ||
| Asymptotic significant (two-tailed) | 0.002 | ||
| Exact significant (two×[one-tailed significant]) | 0.001a | ||
aNot corrected for ties,
bGrouping variable: Group
Table 7.
Pairwise comparison of Group II (zinc polycarboxylate luting cement) and Group III (zinc phosphate luting cement) using Mann–Whitney U-test
| Ranks | ||||
|---|---|---|---|---|
| Cement | n | Mean rank | Sum of ranks | |
| Total | Group II | 10 | 15.05 | 150.50 |
| Group III | 10 | 5.95 | 59.50 | |
| Total | 20 | |||
| Test statisticsb | Difference_score | |||
| Mann–Whitney U | 4.500 | |||
| Wilcoxon W | 59.500 | |||
| Z | −3.530 | |||
| Asymptotic significant (two-tailed) | 0.000 | |||
| Exact significant (two×[one-tailed significant]) | 0.000a | |||
aNot corrected for ties,
bGrouping variable: Cement
DISCUSSION
In implant dentistry, there is adhesion between two metallic components instead of the tooth to the metal as in conventional fixed prosthodontics. Thus the selection of luting cements is more diverse and extensive than natural teeth. Additionally, the resistance and retention form of implant abutments is much more favorable than natural tooth preparations.[1] This allows the use of lower strength cements in retaining implant-supported restorations and also permits retrieval when required.
The major problem encountered with cement-retained implant prosthesis is microleakage. Microleakage is defined as the movement of bacteria, fluid molecules, or ions between abutment and prosthesis. It has been well known that luting agents do not form a perfect seal between abutment and prosthesis and have numerous micro spaces present which allow passage for solutes and solvents, resulting in the growth of bacteria and their by-products. Thus causing peri-implantitis, which results in bone loss and may lead to implant failure.[15]
Various principles, including biological, chemical, electrical, physical, or radioactive components, have been utilized by contemporary methods to evaluate microleakage. These include the use of dyes, bacteria, neuron activation analysis, radioactive isotopes, artificial caries, air pressure, scanning electron microscope, and calcium hydroxide.[18] Organic dyes are widely used and one of the most popular and older methods for the evaluation of microleakage. Various organic dyes are basic fuchsin, methylene blue, eosin, aniline blue, crystal violet, and erythrosine B.[19,20,21] Among these dyes, basic fuchsin (0.5%–2%) is most commonly used.[11,12,15,16]
Wenner et al. found that microleakage studies have the probability of finding false negative in 33% cases if only single section is evaluated.[22] Therefore multiple surface scoring methodology is preferred in microleakage studies.[10,11,12,13,14] Nonparametric scoring methods are widely used in microleakage studies. Linear dye penetration expressed in millimeters may have different significance, depending on the variation in the teeth size and shape. The best method to evaluate microleakage is nonparametric scoring method in fixed prosthesis.[11]
In the present study, zinc phosphate cement exhibited the least microleakage. This can be attributed to its high compressive and tensile strengths coupled with excellent retention properties. The mean microleakage score in zinc polycarboxylate cement was less than zinc oxide noneugenol cement. Although both the cements have similar compressive strengths, the difference in microleakage can be attributed to better retentive properties of polycarboxylate cement. The difference in the microleakage for these two cements was insignificant. In the present study, Zinc oxide non-eugenol cement was selected because zinc oxide non-eugenol cement showed less microleakage than Zinc oxide eugenol cement.[23]
The factors which make an impact on microleakage are solubility, set cement structure, film thickness, thermal changes, sealing ability, resistance of stresses, etc.[12,24]
Solubility is an important criterion in selecting luting cements in fixed prosthesis. Cement dissolution can promote microleakage. Water sorption and solubility may cause further degradation of cement, leading to the formation of microgaps in the cement. The microgaps formed inside the set matrix are invaded by the bacteria and their by-products.[25] The set cement of zinc oxide non-eugenol has solubility (0.4 wt%), which is higher when compared to zinc polycarboxylate cement (0.06 wt%) and zinc phosphate cement (0.06 wt%) in water. The solubility of zinc polycarboxylate cement is increased markedly when exposed to organic acids having pH <4.5.[26] The residual spaces are formed in the matrix of both to zinc phosphate cement and zinc polycarboxylate cement due to the leaching of unreacted zinc and magnesium particles during dissolution resulting in an increase in microleakage. These unreacted particles in the matrix have diameter of nearly 2–8 μm.[27]
The other major factor in microleakage is the amount of marginal gap present between the abutment and the prosthesis. Various researchers stated that there is an increase in the rate of cement dissolution if the marginal gap exceeds 75 μm.[28] According to Fick's Law, the rate of cement dissolution due to diffusion is independent of the degree of exposed luting cement. Jacobs and Windeler evaluated that marginal gap of more than 150 μm demonstrated slight but statistically significant increase in cement dissolution.[14,27,29]
Mechanical stresses and thermal changes produce stresses in luting agents which, when exceed the cohesive and adhesive strength of the material, result in the appearance of microcracks and leads to microleakage. In in vitro studies the expansion and contraction of luting agents in response to thermal cycling subjects the cement to mechanical stresses, leading to the formation of microcracks, causing microleakage.[19,20]
The most common soft access cement used in implant dentistry is zinc oxide eugenol with o-ethoxybenzoic acid (EBA). It is suggested by manufacturers that the bonding capacity of eugenol-free cement is higher than other conventional provisional agents.[21] The compressive strength is increased by the addition of EBA modifier comparable to zinc polycarboxylate cement but is less than zinc phosphate cement. This results in prosthesis that can be easily removed but remains in place during normal functions.[7]
The tensile strength of zinc polycarboxylate cement is higher than zinc phosphate cement, but it is not commonly used as definitive cement in implant dentistry. This can be attributed to its inferior compressive strength and retentive properties. This cement is commonly used in cases with the presence of less than six abutments, no cantilever or offset loads are present and soft access cement is desired. Zinc polycarboxylate cement can also be used as provisional cement when zinc oxide eugenol cement appears insufficient.[1,26,30]
The selection of each cement depends upon its various properties. It is important for the clinician to self-analyze the selection of the certain type of cement based upon various clinical conditions.[10]
In vitro microleakage tests carried out with dyes are more sensitive than those carried out in oral cavity. This is probably because the dye is more easily diffused than bacteria and their by-products and secondly, the build-up of proteins and debris that calcify in the marginal opening may improve the seal.[31] In vivo results still may differ due to many other factors like saliva, altered pH of the oral environment, masticatory load, etc. This study was taken up to provide information about microleakage in cemented copings on implant abutments, which would be helpful in predicting their values in the oral environment. A long-term clinical study would be required further for the final evaluation of these materials.
CONCLUSION
Within the limitations of this study, the following conclusions can be drawn:
Zinc phosphate cement, when used as luting agent for metallic copings in cement-retained implant prosthesis, exhibited the least microleakage and the difference is statistically significant than zinc polycarboxylate cement and zinc oxide non-eugenol cement
Zinc Polycarboxylate cement resulted in less microleakage than Zinc oxide Non-eugenol cement, but the result is not statistically significant.
Hence, the cementation of cement-retained implant prosthesis should be done progressively. If the failure occurs using provisional cement, definitive cement should be considered. The final decision to use various luting cements should be based on clinician's judgment and different clinical circumstances.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Misch CE. Dental Implant Prosthetics. 1st ed. Philadelphia: Elsevier Mosby; 2005. [Google Scholar]
- 2.Uludamar A, Ozkan YK. Cement selection of cemented implant supported restorations. Cumhuriyet Dent J. 2012;15:166–74. [Google Scholar]
- 3.Hebel KS, Gajjar RC. Cement-retained versus screw-retained implant restorations: Achieving optimal occlusion and esthetics in implant dentistry. J Prosthet Dent. 1997;77:28–35. doi: 10.1016/s0022-3913(97)70203-8. [DOI] [PubMed] [Google Scholar]
- 4.Goodacre CJ, Kan JY, Rungcharassaeng K. Clinical complications of Osseo integrated implants. J Prosthet Dent. 1999;81:537–52. doi: 10.1016/s0022-3913(99)70208-8. [DOI] [PubMed] [Google Scholar]
- 5.Becker W, Becker BE. Replacement of maxillary and mandibular molars with single endosseous implant restorations: A retrospective study. J Prosthet Dent. 1995;74:51–5. doi: 10.1016/s0022-3913(05)80229-x. [DOI] [PubMed] [Google Scholar]
- 6.Michalakis KX, Pissiotis AL, Hirayama H. Cement failure loads of 4 provisional luting agents used for the cementation of implant-supported fixed partial dentures. Int J Oral Maxillofac Implants. 2000;15:545–9. [PubMed] [Google Scholar]
- 7.Michalakis KX, Hirayama H, Garefis PD. Cement-retained versus screw-retained implant restorations: A critical review. Int J Oral Maxillofac Implants. 2003;18:719–28. [PubMed] [Google Scholar]
- 8.Jokstad A. Osseointegration and Dental Implants. Hoboken: Wiley-Blackwell Publication; 2008. [Google Scholar]
- 9.Keller W, Bragger U, Mombelli A. Peri-implant micro flora of implants with cemented and screw retained suprastructures. Clin Oral Impl Res. 1998;9:209–17. doi: 10.1034/j.1600-0501.1998.090401.x. [DOI] [PubMed] [Google Scholar]
- 10.Bhatnagar V, Sardar CS, Ram SM, Mehta A. An evaluation of microleakage of metallic copings cemented with three luting agents: A stereomicroscopic study. J Indian Prosthodont Soc. 2007;7:81–4. [Google Scholar]
- 11.Baldissara P, Comin G, Scotti FM. Comparative study of the marginal microleakage of six cements in fixed provisional crowns. J Prosthet Dent. 1998;80:417–22. doi: 10.1016/s0022-3913(98)70005-8. [DOI] [PubMed] [Google Scholar]
- 12.Yüksel E, Zaimoğlu A. Influence of marginal fit and cement types on microleakage of all-ceramic crown systems. Braz Oral Res. 2011;25:261–6. doi: 10.1590/s1806-83242011000300012. [DOI] [PubMed] [Google Scholar]
- 13.Shiva Kumar K, Boris Bhim A, Shankar S. Microleakage of two systems of glass ionomer luting agents – In vitro study. JIADS. 2010;1:1–4. [Google Scholar]
- 14.Rossetti PH, Do Valle AL, De Carvalho RM, De Goes MF, Pegoraro LF. Correlation between marginal fit and microleakage in complete crowns cemented with three luting agents. J Appl Oral Sci. 2008;16:64–9. doi: 10.1590/S1678-77572008000100013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pan YH, Ramp LC, Lin CK, Liu PR. Retention and leakage of implant-supported restorations luted with provisional cement: A pilot study. J Oral Rehabil. 2007;34:206–12. doi: 10.1111/j.1365-2842.2006.01673.x. [DOI] [PubMed] [Google Scholar]
- 16.Pan YH, Ramp LC, Lin CK, Liu PR. Comparison of 7 luting protocols and their effect on the retention and marginal leakage of a cement-retained dental implant restoration. Int J Oral Maxillofac Implants. 2006;21:587–92. [PubMed] [Google Scholar]
- 17.Oyague RC, Turrion AS, Lozano JF, Suarez-Garcia MJ. Vertical discrepancy and microleakage of laser sintered and vacuum cast implant supported structures luted with different cements. J Dent. 2012;40:123–30. doi: 10.1016/j.jdent.2011.11.007. [DOI] [PubMed] [Google Scholar]
- 18.Bhandari S, Aras M, Chitre V. An in vitro evaluation of the microleakage under complete metal crowns using three adhesive luting cements. J Indian Prosthodont Soc. 2012;12:65–71. doi: 10.1007/s13191-011-0109-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Piwowarczyk A, Lauer HC, Sorensen JA. Microleakage of various cementing agents for full cast crowns. Dent Mater. 2005;21:445–53. doi: 10.1016/j.dental.2004.07.009. [DOI] [PubMed] [Google Scholar]
- 20.Nascimento CD, Barbosa RE, Issa JP, Watanabe E, Ito IY, Albuquerque RF. Bacterial leakage along the implant abutment interface of pre-machined or cast components. Int J Oral Maxillofac Implants. 2008;37:177–80. doi: 10.1016/j.ijom.2007.07.026. [DOI] [PubMed] [Google Scholar]
- 21.Gonzalez NA, Kasim NH, Aziz RD. Microleakage testing. Annals Dent Univ Malaya. 1997;4:31–7. [Google Scholar]
- 22.Wenner KK, Fairhurst CW, Morris CF, Hawkins IK, Ringle RD. Microleakage of root resorations. J Am Dent Assoc. 1988;117:825–28. doi: 10.14219/jada.archive.1988.0127. [DOI] [PubMed] [Google Scholar]
- 23.Arora SJ, Arora A, Upadhyaya V, Jain S. Comparative evaluation of marginal leakage of provisional crowns cemented with different temporary luting cements: In vitro study. J Indian Prosthodont Soc. 2016;16:42–8. doi: 10.4103/0972-4052.164911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tjan AH, Dunn JR, Grant BE. Marginal leakage of cast gold crowns luted with an adhesive resin cement. J Prosthet Dent. 1992;67:11–5. doi: 10.1016/0022-3913(92)90039-d. [DOI] [PubMed] [Google Scholar]
- 25.Mash LK, Beninger CK, Bullard JT, Staffanou RS. Leakage of various types of luting agents. J Prosthet Dent. 1991;66:763–6. doi: 10.1016/0022-3913(91)90411-o. [DOI] [PubMed] [Google Scholar]
- 26.Philips science of dental materials. 11th ed. Philadelphia: Elsevier; 2003. Anusavice. [Google Scholar]
- 27.Hajmiragha H, Nokar S, Alikhasi M, Nikzad S, Dorriz H. Solubility of three luting cements in dynamic artificial saliva. J Dent. 2008;5:95–8. [Google Scholar]
- 28.Rosenstiel SF, Bruce MF, Crispin J. Dental luting agents: A review of current literature. J Prosthet Dent. 1998;80:280–01. doi: 10.1016/s0022-3913(98)70128-3. [DOI] [PubMed] [Google Scholar]
- 29.Jacobs MS, Windeler AS. An investigation of dental luting cement solubility as a function of the marginal gap. J Prosthet Dent. 1991;65:436–42. doi: 10.1016/0022-3913(91)90239-s. [DOI] [PubMed] [Google Scholar]
- 30.Li ZC, White SN. Mechanical properties of dental luting cements. J Prosthet Dent. 1999;81:597–609. doi: 10.1016/s0022-3913(99)70216-7. [DOI] [PubMed] [Google Scholar]
- 31.Bandgar S, Nagra SJ. Evaluation of marginal microleakage of three zinc oxide based non eugenol temporary luting agents: An in vitro study. J Indian Prosthodont Soc. 2007;7:132–36. [Google Scholar]


