Abstract
The ongoing COVID-19 pandemic has precipitated a global health crisis. Non-COVID diseases across specialties have been significantly compromised. The greatest challenge has been to continue providing care to non-COVID cases with minimum transmission risk to health care workers, patients, and caregivers. In this specter, better described as a medical holocaust, we present our experiences of dealing with acute neurological patients who could access our facility. We attempted to work on three key areas – initial screening using a more inclusive, dynamic checklist for COVID suspicion over and above the emergency triage, a mandatory initial holding on a separate floor of our inpatient service equipped with infection control strategies similar to a COVID-designated area, and daily screening of health care workers and caregivers for symptoms and possible exposures. It was a steep learning curve, a couple of close shaves, and many more lessons that went into the development of an algorithm that seems to be working well.
Keywords: Access to care, acute neurology, COVID-19, models of care, underserved populations
During the ongoing COVID-19 (coronavirus disease-2019) pandemic, management of non-COVID diseases across specialties is likely to suffer. In-spite of lockdowns and restrictions, emergency triage continues to be overwhelmed with COVID suspect cases, making it difficult for non-COVID patients to gain access. Amidst this crisis, how can the heavily exhausted health infrastructure best accommodate non-COVID disorders without compromising on the safety of health care workers (HCWs), patients, and caregivers? In this context, we present our experience of managing an in-patient service catering to acute neurology admissions.
In mid-March, when COVID-19 surfaced in India, two centers of our institute were designated as COVID-care areas. Suspected cases were triaged and tested in emergency, and positive cases were admitted to these centers. In April 2020, two patients with acute intracerebral hemorrhage were admitted to our non-COVID neurology ward in quick succession. These patients had no symptoms suggestive of SARS-Cov2 infection at presentation [1] and tested positive when they developed symptoms consistent with COVID-19 after admission. More than 50 health care workers (HCWs) were quarantined because of the exposure. It was a wake-up call to reorganize our system and to continue providing care with minimum transmission risk. We considered the following options:
Liberal testing (test all patients before transfer to neurology ward): Around mid-March, India was in a limited local transmission stage; hence, indications for testing were stringent [Table 1]. Atypical presentations with extrapulmonary manifestations alone would be missed by screening criteria targeted at capturing a febrile, respiratory illness. But there were practical difficulties in liberal testing due to the limited availability of test kits at the time.
Table 1.
Evolution of testing strategy based on Advisory by Indian Council of Medical Research in India (https://www.icmr.gov.in/cteststrat.html, accessed on June 12, 2020)
| Date | Indication of testing |
|---|---|
| 17th March 2020 | Symptomatic (ILI* symptoms) individuals who have taken international travel in the last 14 days |
| All symptomatic (ILI symptoms) contacts of laboratory-confirmed cases | |
| All symptomatic (ILI symptoms) health care workers managing respiratory distress or SARI** | |
| 20th March 2020 | Addition |
| All hospitalized patients with SARI | |
| Asymptomatic direct and high-risk contacts of a confirmed case | |
| 9th April 2020 | Addition |
| All symptomatic ILI in hotspots/clusters and large migration gatherings/evacuee centers | |
| 18th May 2020 | Addition |
| All hospitalized patients who develop ILI symptoms | |
| All symptomatic ILI among returnees and migrants within 7 days of illness |
*ILI (influenza-like illness) - acute respiratory infection with fever ≥38°C AND cough. **SARI (Severe acute respiratory illness) - acute respiratory infection with fever ≥38°C AND cough AND requiring hospitalization
Identify specific neurological presentations of COVID-19 for directed testing: Initially, the impact of COVID-19 on the nervous system was not considered to be significant. The first study on 41 patients with COVID-19 did not mention significant neurological symptoms.[2] Headache and myalgias/fatigue were reported in 8% and 44% cases, respectively, but were nonspecific symptoms. In April 2020, a retrospective case series of 214 patients from Wuhan, China reported neurologic manifestations in 36.4% of the cases.[3] Strokes, impaired consciousness, and skeletal muscle injury were found to be more common in severe cases, later in the course of illness. Now it is being recognized that in some patients with stroke,[4] Guillain Barre syndrome, and cranial neuropathies (anosmia, ageusia), the neurological manifestations can precede typical features such as fever and cough.[5] Recently, the Indian health authorities have included anosmia and ageusia in the list of clinical features of COVID-19, though these and other neurological presentations are yet to be included in the criteria for testing.
Provide appropriate personal protective equipment (PPE) to all HCWs in the clinical area, and develop a working structure similar to a COVID-designated area: With PPE availability being a major limitation worldwide, this was not a viable option initially.
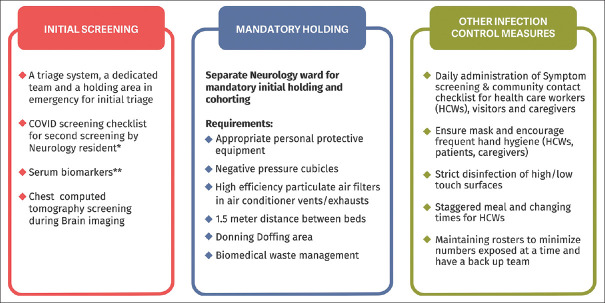
Considering our limitations, we trod a middle path and tried working out a pragmatic strategy as detailed below [Figure 1]:
Figure 1.
NON-COVID INPATIENT MANAGEMENT STRATEGY. Summary of Management Strategies of a non-COVID In-Patient Neurology Service in COVID era. *Febrile/Respiratory illness-related – fever, sore throat, running nose, recurrent sneezing, difficulty breathing, pneumonia, severe acute respiratory illness in the past 14 days. Other parameters – anosmia, loss of taste, diarrhea, anorexia, fatigue, myalgias, conjunctivitis, acute confusion, any family member or close contact with the above symptoms in the past 14 days, history of travel to a hot spot (personal or of a close contact) in the past 14 days, residence in community hot spots irrespective of influenza-like illness symptoms. **Lymphocytopenia, a raised serum lactate dehydrogenase, total and direct serum bilirubin, aminotransferase, Trop T, D-dimer, PT-INR, C-reactive protein
Clinical: A COVID screening checklist was formulated (more inclusive with lowered testing threshold) for the screening of patients being admitted through emergency and updated as per experience gained over time. After the initial triage by the emergency team (largely based on Indian Council of Medical Research Advisory for testing, Table 1), the neurology resident administered this checklist, which included additional parameters such as anosmia, ageusia, diarrhea, anorexia, fatigue, myalgias, conjunctivitis, acute confusion, any family member or close contact with above symptoms, history of travel to an area reporting community transmission, and residence in community hot spots irrespective of the presence of influenza-like illness (ILI) symptoms. Patients having suspicious symptoms underwent COVID testing in liaison with the emergency team and isolation in a COVID suspect- designated area in the emergency room. They were shifted to the neurology ward once the COVID test was negative. Few laboratory investigations were added as potential biomarkers for COVID infection (lymphocyte counts, serum lactate dehydrogenase, serum bilirubin, serum alanine and aspartate aminotransferase, troponin T, D-dimer, prothrombin time expressed as an international normalized ratio (PT-INR), C-reactive protein). Chest screening computed tomography (CT) was made mandatory while undergoing CT head among our patients.
Logistics: Despite having a checklist, initially high testing threshold made it difficult to test all patients failing the second triage. Moreover, COVID-19 prediction cannot be simplified as there are caveats to it. A large number of patients may be asymptomatic, and the sensitivity of reverse transcription-polymerase chain reaction (RT-PCR) from the upper respiratory tract is not 100%, creating a possibility of missing positive cases. So, we designated one floor of our neurology inpatient unit as a COVID-suspect holding area. All admitted patients irrespective of testing status were now kept for 5 days (from symptom onset) in the designated area (mandatory holding) and observed for the development of clinical or radiological features suggestive of COVID-19. If negative at the end of 5 days (median incubation period of SARS-Cov 2), they were transferred to the nondesignated neurology ward [Figure 2]. Staff rosters were changed to minimize numbers exposed at a time and to ensure a back-up team.
Figure 2.
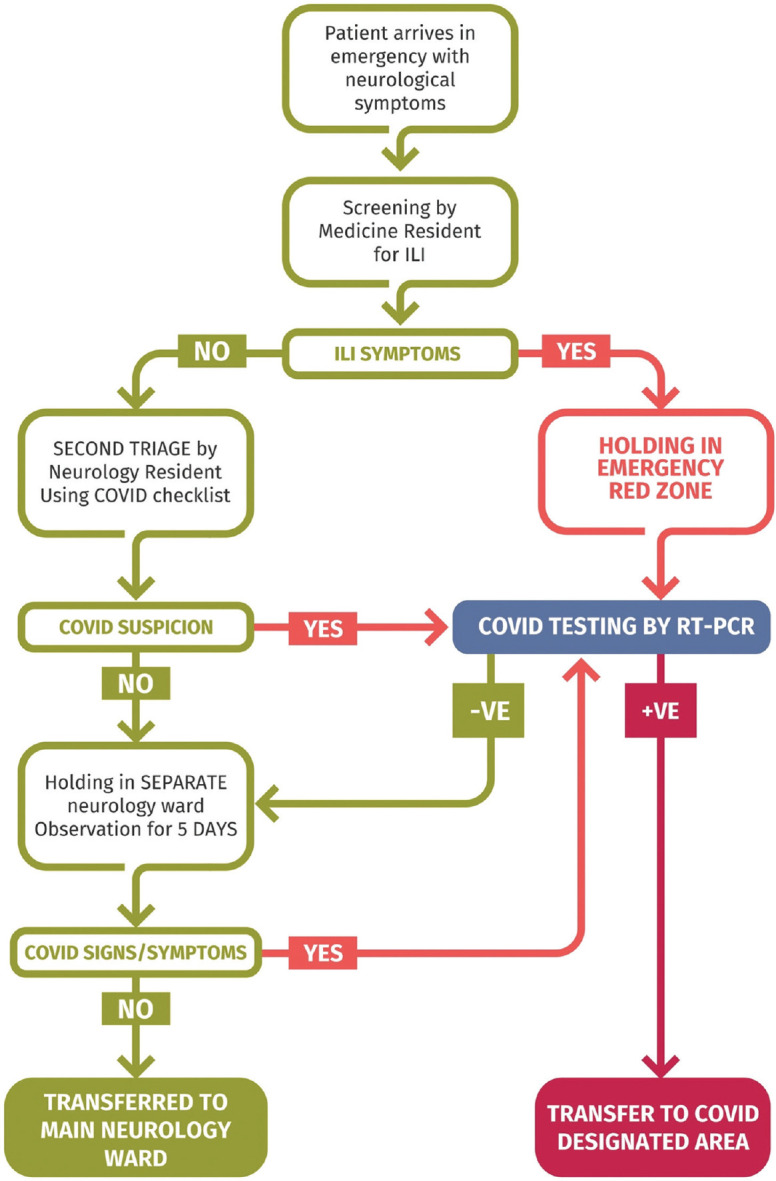
PATIENT FLOW ALGORITHM. Algorithm depicting patient flow once the patient arrives in an emergency with neurological complaints. The initial screening in the emergency was largely based on a history of recent respiratory illness – fever, sore throat, running nose, recurrent sneezing, difficulty breathing, pneumonia, severe acute respiratory illness in the past 14 days. The second triage included other parameters like – anosmia, loss of taste, diarrhea, anorexia, fatigue, myalgias, conjunctivitis, acute confusion, any family member or close contact with the above symptoms in the past 14 days, history of travel to a hot spot (personal or of a close contact) in the past 14 days, residence in community hot spots irrespective of influenza-like illness (ILI) symptoms
Infection control measures: Appropriate PPE were provided to the HCWs in the COVID- suspect designated area; their numbers and shifts adjusted to rationalize PPE utilization. Separate donning/doffing rooms were designated, training was provided, and appropriate protocols were exhibited. High-efficiency particulate air filters were placed over exhausts and air conditioner vents, and negative pressure functioning was ensured in the patient cubicles. Adequate spacing between patients was maintained (≥1.5 m between beds) by leaving alternate beds vacant. A separate patient transport lift was designated for suspect cases. Frequent disinfection of high and low touch surfaces was performed as per the institutional protocol. Symptom screening and community contact checklists were administered to all HCWs at the entry points to clinical areas, and isolation and testing were performed in case of symptoms or exposure. Meal and shift changing times of staff were staggered. A team of neurology faculty, infection control nurses, and nursing in-charges strictly monitored the protocols.
Over 2-and-a-1/2 months (25th March 2020–June 12th 2020), amongst 150 acute neurology admissions to our non-COVID ward, we could filter seven additional positive cases (apart from the two stroke cases mentioned above) using this strategy, in whom no febrile respiratory symptoms were reported on presentation; hence, COVID was not suspected initially. They were shifted to the COVID-designated center following the positive report. With time, resources have improved, and the overall hospital policy has evolved, integrating the experience gained from different case scenarios. It was seen that as the number of cases increased despite being negative on admission and having no febrile respiratory symptoms, patients were turning positive during tests performed for screening before procedures. At present, we are testing all patients before inpatient admission and within 48 h of any procedure. The holding area has been useful for isolating the positive patient awaiting transfer to the COVID-designated center. This way, even with increasing numbers of COVID cases (3,09,595 in India and 36,824 in Delhi as of 12th June 2020) we could continue providing care to non-COVID acute neurology cases.
Thus, a second triage using a more inclusive, dynamic (updated as per past learning) checklist to lower testing threshold, a mandatory holding in the system-specific in-patient area (with upgraded protection and infection control strategies similar to COVID- designated area) thus buying time for an in-depth history, evolution of new signs/symptoms and results of potential biomarkers, and incorporating the learning into pragmatic strategies has been quite helpful in our setting. This complemented the tele-neurology services we provided to 3930 patients over 2 months and can be potentially adapted to nontertiary neurology practice. We feel that sharing of similar strategies across health care systems can lead to incremental non-COVID health care delivery gains during these difficult times.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgements
We acknowledge Ms. Abhilasha Krishnamurthy (December Design Studio) for designing the figures.
REFERENCES
- 1.Agarwal A, Vishnu VY, Vibha D, Bhatia R, Gupta A, Das A, et al. Intracerebral hemorrhage and SARS-CoV-2: Association or causation. Ann Indian Acad Neurol. 2020;23:261–4. doi: 10.4103/aian.AIAN_362_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mao L, Jin H, Wang M, Hu Y, Chen S, He Q, et al. Neurologic manifestations of hospitalized patients with coronavirus disease 2019 in Wuhan, China. JAMA Neurol. 2020:e201127. doi: 10.1001/jamaneurol.2020.1127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yaghi S, Ishida K, Torres J, Grory BM, Raz E, Humbert K, et al. SARS2-CoV-2 and stroke in a New York healthcare system. Stroke. 2020;51:STROKEAHA120030335. doi: 10.1161/STROKEAHA.120.030335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ahmad I, Rathore FA. Neurological manifestations and complications of COVID-19: A literature review. J Clin Neurosci. 2020;77:8–12. doi: 10.1016/j.jocn.2020.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]