Abstract
Objective
Adults with congenital heart disease (ACHD) may be at a higher risk of a fatal outcome in case of COVID-19. Current risk stratification among these patients relies on personal experience and extrapolation from patients with acquired heart disease. We aimed to provide an expert view on risk stratification while awaiting results from observational studies.
Methods
This study was an initiative of the EPOCH (European Collaboration for Prospective Outcome Research in Congenital Heart disease). Among nine European countries (Austria, Belgium, Denmark, France, Germany, Italy, the Netherlands, Spain and Switzerland), 24 experts from 23 tertiary ACHD centres participated in the survey. ACHD experts were asked to identify ACHD-specific COVID-19 risk factors from a list of potential outcome predictors and to estimate the risk of adverse COVID-19 outcomes in seven commonly seen patient scenarios.
Results
82% of participants did not consider all ACHD patients at risk of COVID-19 related complications. There was a consensus on pulmonary arterial hypertension, Fontan physiology and cyanotic heart disease as risk factors for adverse outcomes. Among different ACHD scenarios, a patient with Eisenmenger syndrome was considered to be at the highest risk. There was a marked variability in risk estimation among the other potential outcome predictors and ACHD scenarios.
Conclusions
Pulmonary arterial hypertension, Fontan palliation and cyanotic heart disease were widely considered as risk factors for poor outcome in COVID-19. However, there was a marked disparity in risk estimation for other clinical scenarios. We are in urgent need of outcome studies in ACHD suffering from COVID-19.
Keywords: heart defects, congenital, COVID-19, global burden of disease
Key questions.
What is already known about this subject?
The novel SARS-CoV-2 responsible for COVID-19 is thought to interact with the cardiovascular system on multiple levels, leading to increased morbidity and mortality in patients with underlying cardiovascular diseases.
What does this study add?
Whether adults with congenital heart disease (ACHD) should be considered to be at increased risk of poor outcomes if suffering from COVID-19 is unclear.
In the absence of observational studies, our survey provides the first expert opinion in this respect.
How might this impact on clinical practice?
Our study provides a first impression on how risk stratification of ACHD in the current pandemic is handled in the absence of observational data.
The results presented in this manuscript may encourage ACHD professionals worldwide to collaborate in outcome studies reflecting the disease among these patients.
Introduction
COVID-19 has developed into a worldwide pandemic.1 As a response, strategies were developed to minimise transmission of the virus and reduce disease-related morbidity and mortality, including preferential protection of patients with underlying medical conditions.
Adults congenital heart disease (ACHD) patients may be such vulnerable persons. Due to their young age (the median age in European registries varies between 30 and 35 years),2 3 cardiovascular risk factors for adverse COVID-19 outcomes such as ischaemic heart disease, cerebrovascular disease, diabetes and hypertension are infrequently found among ACHD patients. However, many ACHD patients face a lifelong increased risk of arrhythmias, heart failure, paradoxical embolism and pulmonary vascular disease due to residual haemodynamic lesions or sequelae from previous interventions.4 5 Therefore, risk stratification among this rapidly growing cohort of rather young and otherwise healthy patients can be challenging.
Currently, risk estimation in ACHD is based on expert opinion.6–8 To further delineate COVID-19 risk perception among ACHD specialists, we conducted a survey among 23 tertiary European centres in different countries. The survey allows to identify areas of concordance and discordance regarding COVID-19 risk stratification in ACHD patients.
Methods
This survey was an initiative of the EPOCH (European Collaboration for Prospective Outcome Research in Congenital Heart disease; https://www.sacher-registry.com/epoch/). Board members of the European Society of Cardiology ACHD Working Group were invited to participate and identify additional tertiary ACHD centres in their countries. Twenty-three centres from Austria, Belgium, Denmark, France, Germany, Italy, the Netherlands, Spain and Switzerland participated in an online questionnaire using the platform SurveyMonkey. The questionnaire is provided as online supplemental material. All participating ACHD centres were tertiary care hospitals with intensive care units and the possibility to provide extracorporeal membrane oxygenation if necessary.
openhrt-2020-001455supp001.pdf (41.1KB, pdf)
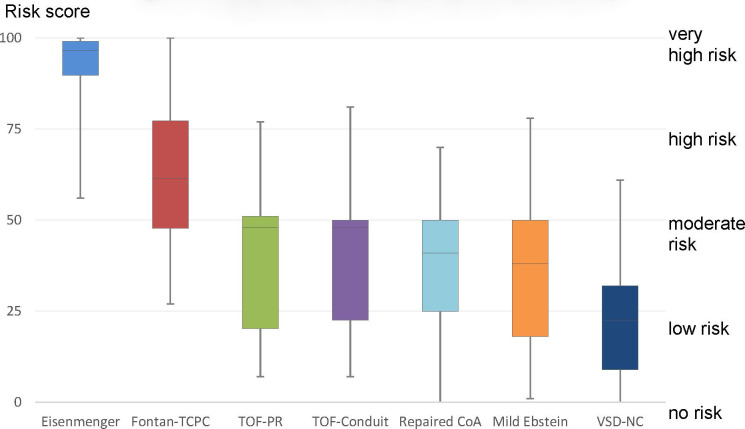
Participants were asked whether they considered all ACHD patients to be at risk of COVID-19-related complications or not and whether their standards for risk stratification were based on national or centre-specific agreement or on personal judgement. Participants then had to select general and ACHD-specific risk factors they considered as relevant for poor COVID-19-related outcome. Finally, participants estimated the risk of adverse COVID-19 outcomes in seven different common patient scenarios by scoring risks from 0 (no increased risk) to 100 (very high risk). Scores <25 were categorised as low risk, scores from 25 to 49 as low to moderate risk, scores from 50 to 74 as moderate to high risk, and scores ≥75 as high risk. Data from 24 questionnaires were collected from 5 to 20 April 2020. The results of the survey were analysed by descriptive statistics and are presented as mean±SD, median and IQR, or percentage, as appropriate. For the different ACHD scenarios, categorised risk scores (as described above) among ACHD specialists with clinical experience with ACHD COVID-19 cases and those without were compared by means of χ2 test. Overall, the null hypothesis was rejected for p values <0.05.
Patient and public involvement
There was no public or patient involvement in this survey.
Results
The mean number of patients under follow-up per year among the reporting centres was 1673±877. A median of 2 (1–4) full-time ACHD cardiologists were working per centre. At the time of the survey, 13 (57%) centres already had clinical experience with COVID-19 among their ACHD patients.
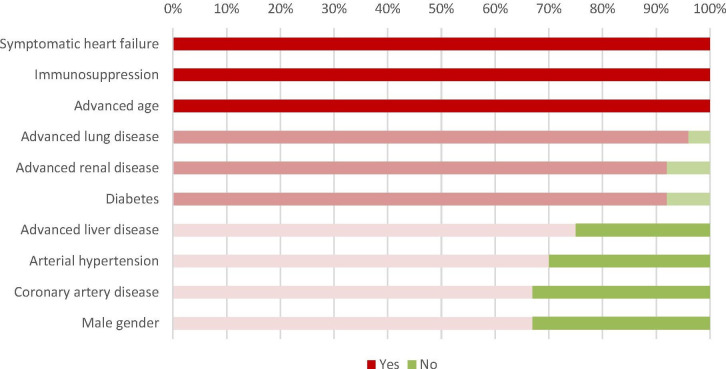
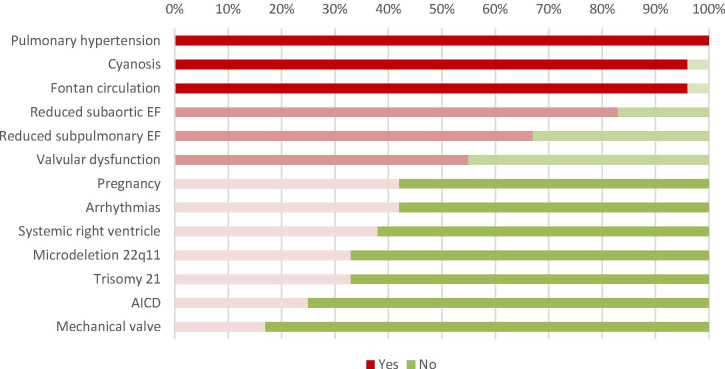
The majority (82%) of participants considered not all ACHD patients at risk of COVID-19-related complications. Overall, 75% of the participants based their decision on national/working group consensus, while 58% and 29% based their decision on personal judgement and centre-specific agreement, respectively. Among the general risk factors for adverse outcomes in COVID-19, all participants considered advanced age, symptomatic heart failure and immunosuppression as such (figure 1). Advanced lung and renal disease, as well as diabetes, were also considered as relevant for ACHD patients by the majority of the experts. There was less agreement with respect to male gender, coronary artery disease, arterial hypertension and advanced liver disease. Pulmonary arterial hypertension was unanimously considered as ACHD-specific risk factor, and 96% considered Fontan physiology and cyanotic heart disease as additional risk factors. The rating of all proposed general and ACHD-specific risk factors is depicted in figures 1 and 2. Among the different ACHD scenarios, a patient with Eisenmenger syndrome was considered to be at the highest risk, whereas a well-doing Fontan patient with an extracardiac conduit was scored at moderate to high risk. There was a marked variability in risk estimation for this scenario. One-third considered a well-doing Fontan patient to be at high risk for lesion (score >75), one-third at moderate to high risk (score 50–75) and one-third at low to moderate risk (score 25–49). All other scenarios were scored at low to moderate risk. The SD of the score among all scenarios ranged from 14 to 21 (figure 3).
Figure 1.
General risk factors (proportion of 'yes' votes)
Figure 2.
ACHD-specific risk factors (proportion of 'yes' votes). ACHD, adult with congenital heart disease; AICD, automatic implantable cardioverter defibrillator; EF, ejection fraction.
Figure 3.
Risk stratification (poor COVID-19 outcome) among seven possible ACHD scenarios. ACHD, adult with congenital heart disease; Fontan-TCPC, univentricular physiology with total cavopulmonary connection and good haemodynamics; repaired CoA, repaired aortic coarctation with mild residual hypertension; TOF-conduit, repaired tetralogy of Fallot with conduit implantation; TOF-PR, repaired tetralogy of Fallot with residual severe pulmonary regurgitation; VSD-NC, repaired ventricular septal defect and mild non-compaction cardiomyopathy.
Complexity of the heart defect and comorbidities were considered the most important risk factor for an adverse outcome in case of COVID-19 (for 33% and 29% of the responders, respectively).
For the different ACHD scenarios, comparison of categorised risk scores among ACHD specialists with clinical experience with ACHD COVID-19 cases and those without revealed no statistically significant difference in risk stratification.
Discussion
In the absence of observational studies, our survey provides the first systematically collected expert opinion on risk stratification of ACHD patients. Those with pulmonary arterial hypertension, Fontan palliation and cyanotic heart disease were considered at highest risk. There was however a marked disparity among ACHD specialists on risk estimation for the most common clinical scenarios.
ACHD patients currently compose a rather young population.2 3 Due to their age, a milder disease course in case of COVID-19 might be expected when compared with older general population. However, ACHD-specific disorders (eg, restrictive lung disease due to repeated thoracotomies, residual shunts and so on) or associated genetic disorders (ie, 22q11 microdeletion or trisomy of chromosome 21) have the potential to increase their risk for an adverse COVID-19 outcome.
In addition, the heterogeneity of cardiac defects and repair strategies performed in the past makes risk stratification among ACHD patients challenging even for ACHD experts, as illustrated by the disparity of estimated risk among the presented clinical scenarios. Reassuringly, most experts consider the majority of ACHD patients to be at low risk for poor outcomes in case of COVID-19. However, ACHD patients at advanced age and with symptomatic heart failure or immunosuppression, as well as those with pulmonary arterial hypertension, cyanosis and a Fontan circulation, are considered vulnerable in case of COVID-19.
The level of evidence of our research is considered to be lowest when using the classification of the Oxford (UK) Centre for Evidence-based Medicine: Levels of Evidence.9 However, until the much-needed outcome studies reflecting the disease course in ACHD patients are available, we may rely on the above-mentioned results not only to assess patient risk but also to reassure many of our patients.
Footnotes
Collaborators: EPOCH-ASO is funded by internal grants without support from the pharmaceutical industry. We thank the expert panel who (in addition to the coauthors of the manuscript) participated in this survey: Werner Budts (Belgium), Massimo Chessa (Italy), Julie De Backer (Belgium), Gerhard Diller (Germany), Rocío García Orta (Spain), María Elvira Garrido-Lestache Rodríguez-Monte (Spain), Elvira Ana González (Spain), Pablo Meras (Spain), Berta Miranda (Spain), Marielle Morissens (Belgium), Agnes Pasquet (Belgium), Joaquin Rueda Soriano (Spain), Annette Schophuus Jensen (Denmark), Lars Sondergaard (Denmark), Oktay Tutarel (Germany), Annemien van den Bosch (The Netherlands), Heleen van der Zwaan (The Netherlands). For more information about EPOCH (European Collaboration for Prospective Outcome Research in Congenital Heart disease), please visit: https://www.sacher-registry.com/epoch/.
Contributors: FJJR-R, DT, MG and MS contributed to drafting of the manuscript, conception of the research, critical revision of the manuscript for important intellectual content and supervision. ML, PG, LD-S, BB, HG and JB contributed to critical revision of the manuscript for important intellectual content and supervision.
Funding: EPOCH-ASO is funded by internal grants without support from the pharmaceutical industry.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Contributor Information
EPOCH:
Werner Budts, Massimo Chessa, Julie De Backer, Gerhard Diller, Rocío García Orta, María Elvira, Rodríguez-Monte Garrido-Lestache, Elvira Ana González, Pablo Meras, Berta Miranda, Marielle Morissens, Agnes Pasquet, Joaquin Rueda Soriano, Annette Schophuus Jensen, Oktay Tutare, Annemien van den Bosch, and Heleen van der Zwaan
Data availability statement
Data are available upon reasonable request.
Ethics statements
Patient consent for publication
Not required.
Ethics approval
Because no data on human subjects were reported, ethical/IRB approval for our survey was waived.
References
- 1. Control ECfDPa . COVID-19 situation update for the EU/EEA and the UK, as of 20, 2020. Available: https://www.ecdc.europa.eu/en/cases-2019-ncov-eueea [Accessed 20 Jun 2020].
- 2. Oliver Ruiz JM, Dos Subirá L, González García A, et al. Adult congenital heart disease in Spain: health care structure and activity, and clinical characteristics. Rev Esp Cardiol 2020;73:804–11. 10.1016/j.rec.2019.09.032 [DOI] [PubMed] [Google Scholar]
- 3. Tobler D, Schwerzmann M, Bouchardy J, et al. Swiss Adult Congenital HEart disease Registry (SACHER) - rationale, design and first results. Swiss Med Wkly 2017;147:w14519. 10.4414/smw.2017.14519 [DOI] [PubMed] [Google Scholar]
- 4. Greutmann M, Tobler D, Kovacs AH, et al. Increasing mortality burden among adults with complex congenital heart disease. Congenit Heart Dis 2015;10:117–27. 10.1111/chd.12201 [DOI] [PubMed] [Google Scholar]
- 5. Diller G-P, Kempny A, Alonso-Gonzalez R, et al. Survival prospects and circumstances of death in contemporary adult congenital heart disease patients under follow-up at a large tertiary centre. Circulation 2015;132:2118–25. 10.1161/CIRCULATIONAHA.115.017202 [DOI] [PubMed] [Google Scholar]
- 6. Radke RM, Frenzel T, Baumgartner H, et al. Adult congenital heart disease and the COVID-19 pandemic. Heart 2020;106:1302–9. 10.1136/heartjnl-2020-317258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Alsaied T, Aboulhosn JA, Cotts TB, et al. Coronavirus disease 2019 (COVID-19) pandemic implications in pediatric and adult congenital heart disease. J Am Heart Assoc 2020;9:e017224. 10.1161/JAHA.120.017224 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Diller G-P, Gatzoulis MA, Broberg CS, et al. Coronavirus disease 2019 in adults with congenital heart disease: a position paper from the ESC Working group of adult congenital heart disease, and the International Society for adult congenital heart disease. Eur Heart J 2020;323. 10.1093/eurheartj/ehaa960 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Oxford Centre for Evidence-Based Medicine: Levels of Evidence, March 2009. Available: https://www.cebm.ox.ac.uk/resources/levels-of-evidence/oxford-centre-for-evidence-based-medicine-levels-of-evidence-march-2009
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
openhrt-2020-001455supp001.pdf (41.1KB, pdf)
Data Availability Statement
Data are available upon reasonable request.