Abstract
Objective
To investigate whether exercise-based cardiac rehabilitation services continued during the COVID-19 pandemic and how technology has been used to deliver home-based cardiac rehabilitation.
Design
A mixed methods survey including questions about exercise-based cardiac rehabilitation service provision, programme diversity, patient complexity, technology use, barriers to using technology, and safety.
Setting
International survey of exercise-based cardiac rehabilitation programmes.
Participants
Healthcare professionals working in exercise-based cardiac rehabilitation programmes worldwide.
Main outcome measures
The proportion of programmes that continued providing exercise-based cardiac rehabilitation and which technologies had been used to deliver home-based cardiac rehabilitation.
Results
Three hundred and thirty eligible responses were received; 89.7% were from the UK. Approximately half (49.3%) of respondents reported that cardiac rehabilitation programmes were suspended due to COVID-19. Of programmes that continued, 25.8% used technology before the COVID-19 pandemic. Programmes typically started using technology within 19 days of COVID-19 becoming a pandemic. 48.8% did not provide cardiac rehabilitation to high-risk patients, telephone was most commonly used to deliver cardiac rehabilitation, and some centres used sophisticated technology such as teleconferencing.
Conclusions
The rapid adoption of technology into standard practice is promising and may improve access to, and participation in, exercise-based cardiac rehabilitation beyond COVID-19. However, the exclusion of certain patient groups and programme suspension could worsen clinical symptoms and well-being, and increase hospital admissions. Refinement of current practices, with a focus on improving inclusivity and addressing safety concerns around exercise support to high-risk patients, may be needed.
Keywords: rehabilitation medicine, telemedicine, COVID-19, adult cardiology
Strengths and limitations of this study.
This is the first international report on the effect that COVID-19 restrictions have had on exercise-based cardiac rehabilitation.
We report data from 330 cardiac rehabilitation healthcare professionals around the world, although the majority of data were from the UK.
Our mixed methods survey enabled us to investigate how technology has been used to deliver exercise-based cardiac rehabilitation as well the barriers to using technology.
Respondents were only able to complete the survey once, but we could have received more than one response from professionals working in a single cardiac rehabilitation programme.
Our data could be used to inform future research agendas, international healthcare policy and local healthcare decision making.
Introduction
Cardiac rehabilitation (CR) is a comprehensive programme of secondary prevention interventions for patients with heart disease, encompassing support for psychosocial health, medical risk management and cardiovascular risk factor modification, including exercise training.1 Exercise-based CR reduces cardiovascular deaths and recurrent myocardial infarction within 10 years and hospital admissions within 2 years, and improves health-related quality of life.2–5 Despite these benefits, only 49% (n=141 648) of eligible UK patients enrolled to a CR programme between 2012 and 2015.6 Increasing uptake to 65% could lead to 21 000 fewer hospital admissions and 8500 fewer deaths over 10 years.7 In response, NHS England set an ambitious target to increase CR uptake to 85% by 2029.8
COVID-19 is spread by a highly contagious virus. As of September 2020, it has infected 26 121 999 and has led to the death of 864 618 people worldwide.9 The rapid spread of COVID-19 infections resulted in governments imposing restrictions on face-to-face human contact.10 Numerous ‘non-essential’ healthcare services were suspended and patient attendance to continuing services has decreased due to fear of contracting COVID-19.11 12 The COVID-19 pandemic may therefore undermine efforts to increase uptake to exercise-based CR.
Before COVID-19, expanding the availability of home-based programmes was recommended to try and increase participation in exercise-based CR.13 Yet, in 2019, 8.8% of UK CR patients participated in home-based programmes.14 This is partly due to a lack of capacity within existing face-to-face services to offer home-based programmes.15 The recent suspension of face-to-face healthcare services, due to COVID-19, may have led to programmes rapidly adopting home-based, technology-facilitated services. Data from urgent and non-urgent care centres in the USA reported that teleconferencing consultations increased from 82 on 4 March 2020 to 1336 on 19 March 2020.16 If a similar rate of technology adoption occurred in CR, this could have helped to maintain patient participation. These methods could also be adopted in future standard practice to increase accessibility and subsequent uptake to CR programmes.
The aim of this mixed methods survey, conducted in collaboration with the British Association for Cardiovascular Prevention and Rehabilitation (BACPR), was to investigate whether exercise-based CR services continued during the COVID-19 pandemic. We also evaluated whether technology was used to deliver exercise-based CR, and the professional experiences of this technology, during the COVID-19 pandemic.
Materials and methods
Survey development
The methods and results are reported in conjunction with the Checklist for Reporting Results of Internet E-Surveys (online supplemental appendix 1).17 This voluntary, cross-sectional, international, open survey, targeted at a convenience sample of healthcare professionals in exercise-based CR, was developed by SN and AFO. The broad topic of questions relating to the COVID-19 pandemic included the following:
bmjopen-2020-046051supp001.pdf (2.1MB, pdf)
If and how CR services were provided.
The demographics and medical complexity of patients accessing CR services.
How technology was used to undertake patient assessments and deliver the exercise component of CR.
The barriers encountered when using technology to deliver the exercise component of CR.
The survey was reviewed by the members of the BACPR elected council prior to ethical approval and was amended accordingly. The BACPR council includes physicians, nurses, physiotherapists, exercise physiologists, exercise instructors, psychologists, dietitians and occupational therapists. The resulting 35-item questionnaire was uploaded to the Qualtrics XM online survey platform (Provo, Utah, USA). Qualtrics has ISO/IEC 27001 security certification. The automated database was password-protected and stored on secure Qualtrics and Sheffield Hallam University servers. The survey was presented across 21 pages, including background information and consent. There were 22 tick box items (19 mandatory), 7 mandatory numerical responses, 3 non-mandatory sliding bar responses, 2 non-mandatory free-text responses and 1 mandatory date entry response. Four questions also permitted free-text responses under the option ‘other’. Response validation was used on all questions, where appropriate. Survey progress was displayed on each page. Participants did not have a completeness check/review option at the end of the survey. Participants were only able to visit the website once from the same IP (internet protocol) address and had 7 days to complete the survey once started. The functionality of the survey was tested by SN, AFO, SD, SH and AC. The final version of the online survey can be found in Appendixonline supplemental appendix 2), was given institutional ethical approval by Sheffield Hallam University (ID: ER24303491), on the 29th May 2020. All participants provided informed consent., and all study procedures were carried out following the rules of the Declaration of Helsinki of 1975 (https://www.wma.net/what-we-do/medical-ethics/declaration-of-helsinki/), revised in 2013
bmjopen-2020-046051supp002.pdf (5.2MB, pdf)
Patient and public involvement
Patients and/or the public were not involved in the design, or conduct, or reporting or dissemination plans of this research.
Survey dissemination
On 2 June 2020, a recruitment email was sent to BACPR members; 746 healthcare professionals and academicsworking in CR. This was repeated on 25 June 2020. The survey was also promoted on social media platforms (online supplemental appendix 3). A link to the survey was not posted on any website. The survey closed at 12:00 on 31 July 2020. There were no incentives offered for participation.
bmjopen-2020-046051supp003.pdf (779.7KB, pdf)
Quantitative data analysis
Categorical data are reported as the number of responses, expressed as a percentage (%) of the respondents to each question. Continuous data are reported as median, with minimum and maximum values. Responses were reported for the full cohort and by the phase of CR that the respondents worked in. Phase I was defined as the inpatient stage, phase II as the early discharge phase, phase III as a clinically supervised outpatient programme and phase IV as long-term physical activity maintenance. The number of responses to each question varied and is detailed in tables 1 and 2 and online supplemental appendix 4. Tests of statistical significance were not conducted.
Table 1.
Provision of cardiac rehabilitation services during the COVID-19 pandemic, displayed as n (%)
| All | Phase I | Phase II | Phase III | Phase IV | |
| Service status | n=330 | n=14 | n=29 | n=164 | n=123 |
| Service able to see as many patients as usual | 44 (13.3) | 2 (14.3) | 6 (20.7) | 30 (18.3) | 6 (4.9) |
| Service able to see fewer patients than usual | 123 (37.3) | 6 (42.9) | 12 (41.4) | 77 (47.0) | 28 (22.8) |
| Service suspended (%) | 163 (49.4) | 7 (42.9) | 11 (37.9) | 57 (34.8) | 89 (72.4) |
| Patients accessing cardiac rehabilitation | n=161 | n=8 | n=17 | n=102 | n=34 |
| No patients are accessing the service | 18 (11.2) | 2 (25.0) | 3 (17.6) | 9 (8.8) | 4 (11.8) |
| Fewer patients are accessing the service | 111 (68.9) | 5 (62.5) | 13 (76.5) | 65 (63.7) | 28 (82.4) |
| Same number of patients are accessing the service | 32 (19.9) | 1 (12.5) | 1 (5.9) | 28 (27.5) | 2 (5.9) |
| Diversity of cardiac rehabilitation | n=151 | n=7 | n=16 | n=95 | n=33 |
| Patient population is less diverse than before COVID-19 | 22 (14.6) | 3 (42.9) | 1 (6.25) | 13 (13.7) | 5 (15.2) |
| Patient population is as diverse as it was before COVID-19 | 122 (80.8) | 4 (57.1) | 15 (93.8) | 78 (82.1) | 25 (75.8) |
| Patient population is more diverse than before COVID-19 | 7 (4.6) | 0 (0.0) | 0 (0.0) | 4 (4.2) | 3 (9.1) |
| Patient population is younger than before COVID-19 | 6 (4.1) | 0 (0.0) | 2 (13.3) | 2 (2.2) | 2 (6.3) |
| Patient population is similar to what it was before COVID-19 | 135 (92.5) | 5 (71.4) | 12 (80.0) | 89 (96.7) | 29 (90.6) |
| Patient population is older than before COVID-19 | 5 (3.4) | 2 (28.6) | 1 (6.7) | 1 (1.1) | 1 (3.1) |
| Estimated percentage of patients in the last 7 days that were >65 years | 70.0 (0.0–100.0) | 75.0 (60.0–85.0) | 67.0 (38.0–100.0) | 64.5 (0.0–100.0) | 80.0 (0.0–100.0) |
| Proportion of female participation is smaller | 11 (0.8) | 1 (16.7) | 0 (0.0) | 8 (9.4) | 2 (6.9) |
| Proportion of female participation is the same | 113 (83.7) | 4 (66.7) | 14 (93.3) | 69 (81.2) | 26 (89.7) |
| Proportion of female participation is larger | 11 (0.8) | 1 (16.7) | 1 (6.7) | 8 (9.4) | 1 (3.4) |
| Proportion of male participation is smaller | 6 (4.4) | 1 (16.7) | 1 (6.7) | 2 (2.4) | 2 (7.0) |
| Proportion of male participation is the same | 123 (91.1) | 4 (66.7) | 14 (93.3) | 79 (92.9) | 26 (89.7) |
| Proportion of male participation is larger | 6 (4.4) | 1 (16.7) | 0 (0.0) | 4 (4.7) | 1 (3.4) |
| Estimated percentage of patients in the last 7 days were female | 30.0 (0.0–80.0) | 40.0 (10.0–70.0) | 30.0 (1.0–57.0) | 30.0 (0.0–80.0) | 40.0 (1.0–73.0) |
Table 2.
Barriers to using technology in exercise-based cardiac rehabilitation, displayed as n (%)
| Barriers to using technology | All (n=107) | Phase I (n=6) | Phase II (n=9) | Phase III (n=68) | Phase IV (n=24) |
| Lack of patient confidence | 93 (86.9) | 2 (33.3) | 8 (88.9) | 60 (88.2) | 23 (95.8) |
| Patients do not have access to computers/tablets/smart phone | 86 (80.4) | 2 (33.3) | 4 (44.4) | 61 (89.7) | 19 (79.2) |
| Patients do not have an internet connection | 73 (68.2) | 2 (33.3) | 6 (66.7) | 48 (70.6) | 17 (70.8) |
| Patients lack interest in receiving services using technology | 65 (60.7) | 1 (16.7) | 5 (55.6) | 44 (64.7) | 15 (62.5) |
| Professionals are concerned about patient safety | 43 (40.2) | 0 (0.0) | 3 (33.3) | 34 (50.0) | 6 (25.0) |
| Patients are concerned about safety | 32 (29.9) | 2 (33.3) | 3 (33.3) | 21 (30.9) | 6 (25.0) |
| Internet security and patient confidentiality concerns | 27 (25.2) | 1 (16.7) | 4 (44.4) | 18 (25) | 4 (16.7) |
| Professionals not confident delivering service using technology | 24 (22.4) | 0 (0.0) | 2 (22.2) | 19 (27.9) | 3 (12.5) |
| Trusts/Health Boards do not support the delivery of health services using technology | 16 (15.0) | 1 (16.7) | 0 (0.0) | 14 (20.6) | 1 (4.2) |
| No barriers | 2 (1.9) | 1 (11.1) | 0 (0.0) | 1 (1.5) | 0 (0.0) |
bmjopen-2020-046051supp004.pdf (1.8MB, pdf)
Qualitative data analysis
Free-text answers were exported into NVivo V.11 software for thematic analysis. Answers were coded inductively. The resulting coding framework was then reviewed to identify patterns and themes in the data. Similar codes were grouped to form lower order themes, which were then grouped into higher order themes. Each theme was given a descriptive explanation with illustrative quotes.
Results
Responses
Four hundred and seven visits to the survey site were recorded. Seventy-seven (18.9%) did not progress past the study information and consent page (81.1% participation rate). Three hundred and thirty responses were analysed, 296 (89.7%) of which were from the UK. The remaining responses were from Japan (n=8, 2.4%), Australia (n=4, 1.2%), the USA (n=4, 1.2%), Ireland (n=4, 1.2%), Gibraltar (n=2, 0.6%), India (n=2, 0.6%), South Africa (n=2, 0.6%), Spain (n=2, 0.6%), the Bailiwick of Guernsey (n=1, 0.3%), Canada (n=1, 0.3%), the Isle of Man (n=1, 0.3%) and Kuwait (n=1, 0.3%).
Service provision during the COVID-19 pandemic
At the time of responding, 163 (49.3%) CR programmes had been suspended due to COVID-19 (table 1). The proportions of UK (n=147, 49.7%) and non-UK (n=16, 47.1%) services that had been suspended were similar. Phase IV programmes were most likely to have suspended all activities (n=89, 72.4%; table 1). The remaining questions in the survey were applicable to a maximum of 167 respondents. The number of responses to each question can be seen in table 1 and online supplemental appendix 4.
Following COVID-19 restrictions, 32 (19.9%) programmes reported that the same volume of patients were choosing to access their service (table 1). Most programmes reported that either fewer patients (n=111, 68.9%) or no patients (n=18, 11.2%) were choosing to access their service (table 1). Programmes believed that patients enrolling in CR were either as demographically as diverse (n=122, 80.8%) or more diverse than normal (n=7, 4.6%; table 1). UK CR programmes also estimated that 90.4% (0.0%–100.0%) of patients seen in the last 7 days were ‘White British’. Most CR programmes (92.5%) reported that the age of participants was similar to normal, with 70% (0.0%–100.0%) of patients enrolling in CR >65 years of age (table 1). Programmes also reported that the sex of patients participating in CR was proportionally similar to normal. Female participation in CR was estimated at 30% (0.0%–80%; table 1).
Technology adoption
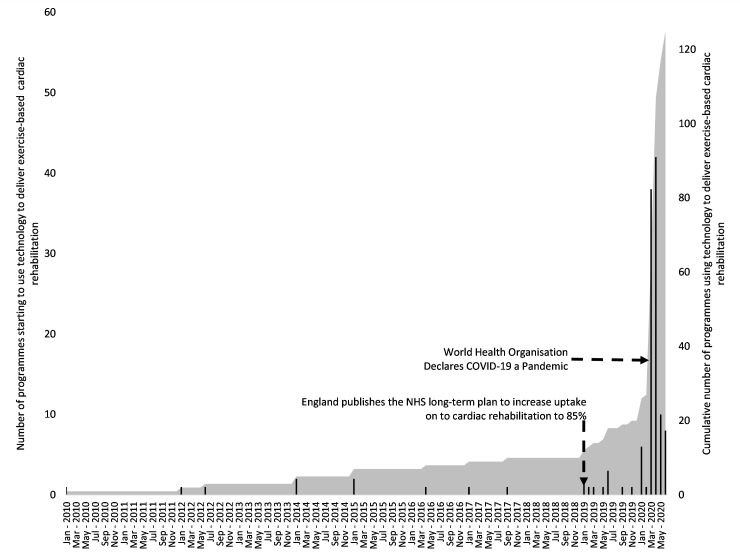
Figure 1 shows the increase in adoption of technology over time. The earliest date that a programme reported using technology was 10 January 2010. The latest was on 20 June 2020. Thirty-three (25.8%) used technology to deliver exercise-based CR before COVID-19 was declared a pandemic by the WHO.18 The median date of technology adoption was 30 March 2020. There were notable increases in technology adoption. The first coincided with the release of the UK’s NHS Long Term Plan.8 The second, more rapid increase, coincides with the COVID-19 pandemic.18
Figure 1.
Data showing the use of technology to deliver exercise-based cardiac rehabilitation between January 2010 and June 2020. Black bars indicate how many programmes started using their chosen technology on a given date. The grey area shows the cumulative number of cardiac rehabilitation programmes using technology.
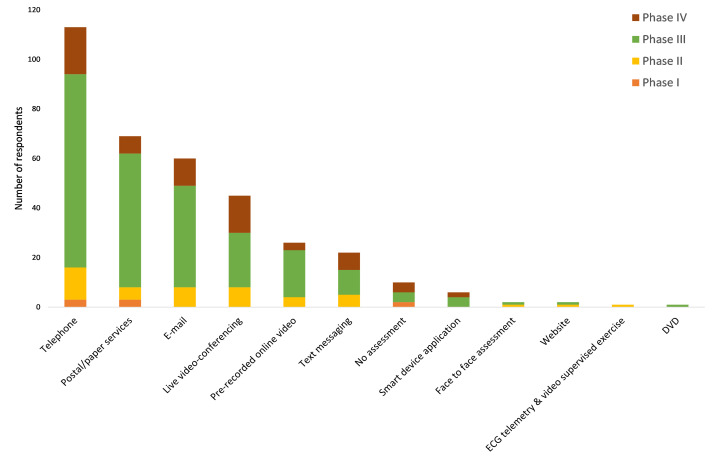
Technology use in patient assessment
The most commonly used technology to conduct patient assessment was telephone (n=113, 85.0%; figure 2). Thirty-two (24.1%) programmes reported that they were not assessing or estimating functional capacity. Practitioners mostly relied on patient self-reported fitness to estimate functional capacity (n=92, 69.2%). Some programmes estimated functional capacity by using a questionnaire (26.3%, n=35) or the patient’s own physical activity tracker (21.1%, n=28). One phase I (16.7%), two phase II (14.3%) and four phase IV (13.8%) CR programmes remotely supervised exercise testing (figure 2).
Figure 2.
Types of technology used to undertake baseline assessments.
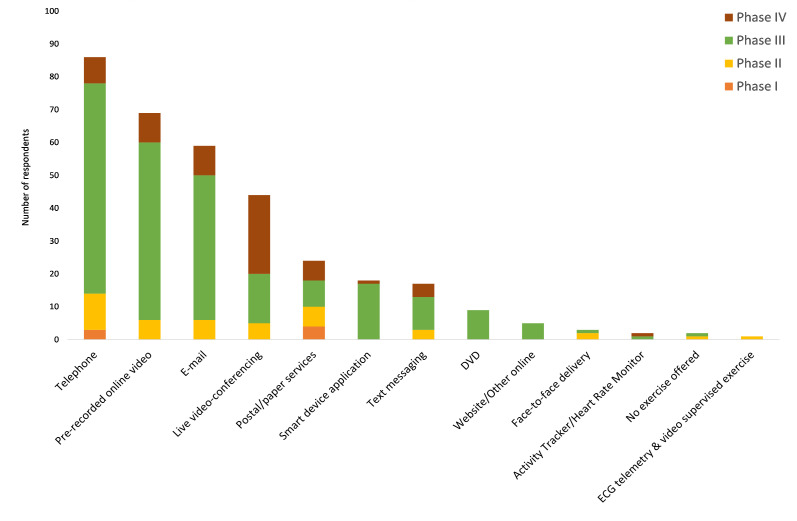
Technology use in physical activity and exercise prescription
Most services were able to provide physical activity advice (n=102, 82.9%). Seventy-two (58.5%) programmes also offered structured exercise training programmes. Telephone remained the most commonly used technology to facilitate the physical activity or exercise component of CR (n=86, 64.7%; figure 3). Prerecorded online videos (n=69, 51.9%) were also widely used, particularly among phase III programmes (n=54, 64.3%; figure 3). Most CR services were able to provide physical activity or structured exercise training to patients at low (n=117, 95.1%) and moderate (n=109, 88.6%) risk of exercise-induced cardiac events. Half (51.2%, n=63) were able to offer services to patients at high risk of exercise-induced cardiac events. Three (2.8%) programmes reported one adverse event resulting in minor injury while using technology to deliver the exercise component of CR (three events in total). There were no reports of life-changing injury or death.
Figure 3.
Types of technology used to deliver the exercise component of cardiac rehabilitation.
Barriers to using technology
The number of responses to each question about barriers to using technology is shown in table 2. Respondents were asked to state any barriers that they encountered when using technology. Only two (1.9%) programmes reported ‘no barriers’ (table 2). Most (n=93, 86.9%) encountered a ‘lack of patient confidence’ with technology (table 2). Qualitative analysis of the barriers to using technology fell into two categories: logistical and organisational barriers, and patient-related barriers. Logistical and organisational barriers were largely a result of healthcare organisations being unprepared and not familiar with using online healthcare delivery. Onerous governance processes and delayed access to the necessary information technology equipment were also described. Patient-related barriers were associated with communication (either language or understanding) and concerns that patients were either over-reporting their activity or not following the advice provided.
Practitioner experiences
Qualitative analysis of free-text answers to the final question allowing ‘Any other comments’ resulted in the identification of three higher order themes: (1) impact on patient experience, (2) challenges for the staff and (3) implications for future delivery.
Impact on patient experience
Survey respondents varied in their views about the impact on patient engagement and experience. Technology was acknowledged as a valuable means of connecting patients with CR staff, but a small number of respondents also highlighted that it was harder to establish rapport this way. One participant reported a decline in patients’ fitness outcomes, while another claimed that patients exercised harder at home without peers to distract them. More commonly, participants reported that, regardless of the perceived benefits of remote delivery, it was difficult to replicate the social benefits associated with group exercise delivery:
The lack of contact with other patients means the patients miss out on the social and emotional support from each other.
Challenges for professionals
Survey participants cited a range of challenges to adoption of technology, including the limitations of existing platforms, such as smart device applications for CR. These were described as lacking patient-centred or motivational content and being time-consuming to use. Participants reported further difficulties associated with COVID-19-related staff redeployment or illness, and reiterated barriers such as lack of access to technology and organisational delays caused by information technology and governance restrictions.
A large number of comments described concerns relating to practitioners’ inability to observe patients, limiting safe and accurate assessment of functional capacity. This had resulted in a more cautious approach, with respondents reporting that they prescribed only gentle or low-level exercise:
Our main concern has been the difficulty of not being able to complete functional capacity assessments, we have therefore recommended patients exercise at a lower level than we normally would.
Implications for future delivery
Many respondents were optimistic about continuing to incorporate technology in future CR delivery. Nevertheless, it was generally recognised that delivery should be flexible. Exercise programmes should be tailored to individual needs and risk levels and patients should be provided with a range of options for engaging with CR, including both face-to-face contact with CR staff and online/home-based exercise.
Several comments indicated opportunities for improvement in the technology available, with one participant suggesting that current formats were driven by National Audit of Cardiac Rehabilitation (NACR) data requirements as opposed to patient needs. Another respondent called for further research to inform more confident remote exercise prescription:
Still feel face to face assessment is superior for more frail patients …and for higher risk patients… Nevertheless, I am gaining more confidence in remote assessment, and would be reassured further by some research to demonstrate its safety and efficacy. I already know remote delivery has been shown to be safe and effective, but as far as I am aware this has been evidenced only when prescribed from face to face assessment.
Quantitatively, 94 (88.7%) programmes believed that technology should be available for patients in the future.
Discussion
To our knowledge, this is the first study to quantitatively document the effect that restrictions, imposed due to COVID-19, had on exercise-based CR programmes. We found that nearly half of all programmes had been suspended and that most centres reported a reduction in patient engagement with services during the COVID-19 pandemic. Practitioners reported that the age and sex of patients attending CR were similar to before the COVID-19 pandemic. Technology was rapidly adopted to deliver CR, with less sophisticated technology, such as the telephone, being most widely used. Higher risk patients were less likely to be offered remote CR using technology. Nearly all centres reported barriers to using technology to deliver CR. Finally, despite an openness to adopting technology by practitioners, there were concerns surrounding availability of and confidence in using technology. Qualitatively, patient assessment, less opportunity for socialisation and safety were highlighted.
Service provision
COVID-19 has resulted in many non-essential healthcare services being suspended. We have shown that this was true for half of exercise-based CR services. In 2019, 89 573 patients accessed exercise-based CR in the UK14; therefore, a high proportion of cardiac patients may have been negatively affected by this widespread service disruption. Given that exercise-based CR improves quality of life4 19 and reduces hospital admissions,3 suspension of services is likely to result in worsening clinical symptoms, well-being, and increased hospital admissions long term. This may place an increased burden on healthcare services in the coming months. Nevertheless, there was an increase in the use of technology in CR shortly after COVID-19 was declared a pandemic by the WHO.18 Comparing long-term patient outcomes from programmes that continued service provision with programmes that were unable to continue will help to determine the effectiveness of these changes.
Technology adoption and barriers
Recent editorials and reviews have suggested that COVID-19 could be a catalyst for large-scale changes in the way that CR is delivered.20 21 We found that most services started using technology to deliver exercise-based CR, at home, within 3 weeks of COVID-19 being declared a pandemic by the WHO18; only three services were providing face-to-face services. This suggests that the capacity of CR services to provide home-based rehabilitation programmes has rapidly increased. If maintained, subject to robust evidence, the potential for increased accessibility could positively influence participation in CR when face-to-face service has resumed.
Traditional modes of communication such as telephone were most commonly used. Surprisingly few services used teleconferencing, smart device applications and web-based systems. Healthcare professionals cited that patients often lacked confidence using equipment and/or that patients did not have the required equipment for technology use. The number and the sociodemographic profile of patients for whom this was a genuine barrier are unclear. Others have reported that age may be a factor, with people aged 22–44 years most likely to use teleconferencing facilities16 and people over 65 years being less likely to have a smart phone.22 This could warrant further investigation to address inequalities in the accessibility of technology-based provision of CR. Meanwhile, professionals’ concerns for patient safety (40.2%) and internet security (25.2%) were also likely to contribute to the low uptake of novel technology. Healthcare organisations being underprepared for the adoption of new technology may also play a role, although this was less frequently reported in quantitative analysis. ‘Top-down’ endorsement of technology by health Trusts, Health Boards or healthcare providers may give healthcare professionals confidence in using technology.
Participation
Participation in CR continued despite COVID-19 restrictions. However, programmes were able to offer services to fewer patients and updake was reduced. Furthermore, UK programmes reported that ~90% of participants were ‘White British’, which is proportionately higher than recently indicated (79%) in the 2019 NACR report.14 Future research should investigate the direct impact of COVID-19 on minority group participation in exercise-based CR and explore how to increase their participation when CR is delivered using technology. Encouragingly, programmes reported that similar proportions of men and women and people over the age of 65 years engaged with CR compared with pre-COVID-19 participation.
Data from our survey showed that 41.5% of programmes were unable to provide exercise-based CR to patients at high risk of exercise-induced cardiac events. CR should be available to all eligible patients, irrespective of risk.1 The development and refinement of future technology-based interventions should be inclusive of all risk levels. Qualitative comments highlighted concerns about using technology to remotely deliver exercise-based CR for frail patients. Safety concerns were also a common feature in our quantitative analysis (table 2). The wide use of ‘offline’ delivery modes such as telephone and prerecorded videos identified in our survey limits the capacity to evaluate physiological information during exercise and the scope for practitioners to tailor advice to the individual. It may be perceived as unsafe for patients at high risk of an exercise-induced cardiac event, but not for lower risk patients. Overcoming these concerns, through robust evidence, may be an important step in negating future health inequalities.
Limitations
The high UK response rate to our survey (n=296, 89.7%) makes it likely that our findings are representative of CR in the UK. However, the response rate from CR programmes outside of the UK was low. The generalisability of our findings outside of the UK may therefore be limited. Additionally, we aimed to recruit healthcare professionals rather than patients. Future research should investigate patient perceptions of using technology in CR so that a more complete understanding of barriers can be reported. We also asked study participants to report on whether they perceived that certain demographics of the patients engaging with their services had changed; therefore, we cannot exclude information bias. Finally, individual practitioners rather than centres were targeted to respond. Therefore, the risk of bias could have been increased by multiple practitioners from the same centre completing the survey.
Conclusions
Nearly half of all CR programmes have been suspended during COVID-19 restrictions. Technology was rapidly adopted by CR services, which may increase participation beyond COVID-19. However, higher risk patients may be disadvantaged by technology use, while people in the UK who are ‘White British’ may most likely benefit from it. Our findings indicate a role of technology in future CR delivery. There is a need for innovation in patient-centred, interactive technological resources that also foster confidence among practitioners. Future research needs to investigate the longer term adoption of technology in CR following COVID-19 and its effects on participation, patient experience, and safety.
Supplementary Material
Acknowledgments
The authors would like to thank the healthcare professionals who completed the survey and the BACPR committee for reviewing the design of the survey. The authors would also like to thank the individuals involved in promoting the survey within their networks.
Footnotes
Twitter: @A_ODoherty, @nichols87simon
Contributors: Conceptualisation was by SN. Study methodology was developed by SN, AFO, HH, SD, AC and SH. Investigations were conducted by SN, AFO, HH, SD, AC, SH, PHB and TB. Formal analysis was conducted by SN, AFO and HH. Investigation was coordinated by SN, AFO, HH, SD, AC, SH, PHB and TB. Data curation was led by SN and HH. The original draft manuscript was prepared by SN. Writing, review and editing were conducted by SN, AFO, HH, SD, AC, SH, PHB and TB. Visualisation, supervision and project administration were led by SN.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: SN has received funding from Research England, via the Advanced Wellbeing Research Centre Accelerator, to evaluate the effect of a technology platform for cardiac rehabilitation developed by Aseptika. SN, AFO, AC and HH have received funding from AstraZeneca to investigate factors influencing uptake to cardiac rehabilitation. SN, SD, TB and AC are members of the BACPR council. SD received funding from the Burdett Trust to investigate uptake to exercise referral schemes. SD participated in cardiovascular prevention advisory board for AstraZeneca. SH is Executive Director of the BACPR. PHB has received funding from the National Institutes of Health for cardiac rehabilitation-related research. PHB has also received consultation fees and honoraria from Merck, Boehringer Ingelheim, Corvia Medical and Boston Scientific.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data will be available on reasonable request 18 months after publication of the manuscript. Data can be requested by contacting the corresponding author or library-research-support@shu.ac.uk.
Ethics statements
Patient consent for publication
Not required.
Ethics approval
Sheffield Hallam University Ethics Board reviewed and approved this study (ID: ER24303491) on 29 May 2020. Electronic consent to participate in the survey was obtained from all participants. All study processes conform to the relevant regulations and standards. All study procedures were carried out following the rules of the Declaration of Helsinki of 1975 (https://www.wma.net/what-we-do/medical-ethics/declaration-of-helsinki/), revised in 2013.
References
- 1.Cowie A, Buckley J, Doherty P, et al. Standards and core components for cardiovascular disease prevention and rehabilitation. Heart 2019;105:510–5. 10.1136/heartjnl-2018-314206 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Abell B, Glasziou P, Hoffmann T. The contribution of individual exercise training components to clinical outcomes in randomised controlled trials of cardiac rehabilitation: a systematic review and meta-regression. Sports Med Open 2017;3:19. 10.1186/s40798-017-0086-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Powell R, McGregor G, Ennis S, et al. Is exercise-based cardiac rehabilitation effective? A systematic review and meta-analysis to re-examine the evidence. BMJ Open 2018;8:e019656. 10.1136/bmjopen-2017-019656 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dalal HM, Taylor RS, Jolly K, et al. The effects and costs of home-based rehabilitation for heart failure with reduced ejection fraction: the REACH-HF multicentre randomized controlled trial. Eur J Prev Cardiol 2019;26:262–72. 10.1177/2047487318806358 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Taylor RS, Long L, Mordi IR, et al. Exercise-based rehabilitation for heart failure: cochrane systematic review, meta-analysis, and trial sequential analysis. JACC Heart Fail 2019;7:691–705. 10.1016/j.jchf.2019.04.023 [DOI] [PubMed] [Google Scholar]
- 6.Sumner J, Grace SL, Doherty P. Predictors of cardiac rehabilitation utilization in England: results from the National audit. J Am Heart Assoc 2016;5 10.1161/JAHA.116.003903 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hinde S, Bojke L, Harrison A, et al. Improving cardiac rehabilitation uptake: potential health gains by socioeconomic status. Eur J Prev Cardiol 2019;26:1816–23. 10.1177/2047487319848533 [DOI] [PubMed] [Google Scholar]
- 8.NHS England . The NHS long term plan, 2019. Available: https://www.longtermplan.nhs.uk/wp-content/uploads/2019/01/nhs-long-term-plan.pdf
- 9.World Health Organisation . Weekly operational update on COVID-19, 2020. Available: https://www.who.int/docs/default-source/coronaviruse/situation-reports/wou-4-september-2020-approved.pdf?sfvrsn=91215c78_4 [Accessed 7 Sep 2020].
- 10.Le NK LA, Brooks JP, Khetpal S. Impact of government-imposed social distancing measures on COVID-19 morbidity andmortality around the world. Bull World Health Organ 2020. [Google Scholar]
- 11.Moroni F, et al. Collateral damage: medical care avoidance behavior among patients with myocardial infarction during the COVID-19 pandemic. JACC: Case Reports, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Garcia S, Albaghdadi MS, Meraj PM, et al. Reduction in ST-segment elevation cardiac catheterization laboratory activations in the United States during COVID-19 pandemic. J Am Coll Cardiol 2020;75:2871–2. 10.1016/j.jacc.2020.04.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Anderson L, Sharp GA, Norton RJ, et al. Home-based versus centre-based cardiac rehabilitation. Cochrane Database Syst Rev 2017;6:CD007130. 10.1002/14651858.CD007130.pub4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.British Heart Foundation . The National audit of cardiac rehabilitation: quality and outcomes report. 2019, 2019. [Google Scholar]
- 15.Turk-Adawi K, Supervia M, Lopez-Jimenez F, et al. Cardiac rehabilitation availability and density around the globe. EClinicalMedicine 2019;13:31–45. 10.1016/j.eclinm.2019.06.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mann DM, Chen J, Chunara R, et al. COVID-19 transforms health care through telemedicine: evidence from the field. J Am Med Inform Assoc 2020;27:1132–5. 10.1093/jamia/ocaa072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Eysenbach G. Improving the quality of web surveys: the checklist for reporting results of Internet E-Surveys (cherries). J Med Internet Res 2004;6:e34. 10.2196/jmir.6.3.e34 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.World Health Organisation Archived . WHO Timeline - COVID-19, 2020. [Google Scholar]
- 19.McGregor G, Powell R, Kimani P, et al. Does contemporary exercise-based cardiac rehabilitation improve quality of life for people with coronary artery disease? A systematic review and meta-analysis. BMJ Open 2020;10:e036089. 10.1136/bmjopen-2019-036089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Babu AS, Arena R, Ozemek C, et al. COVID-19: a time for alternate models in cardiac rehabilitation to take centre stage. Can J Cardiol 2020;36:792–4. 10.1016/j.cjca.2020.04.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nichols S, McGregor G, Breckon J, et al. Current insights into Exercise-based cardiac rehabilitation in patients with coronary heart disease and chronic heart failure. Int J Sports Med 2021;42:19–26. 10.1055/a-1198-5573 [DOI] [PubMed] [Google Scholar]
- 22.Strain T, Wijndaele K, Brage S. Physical activity surveillance through smartphone Apps and wearable Trackers: examining the UK potential for nationally representative sampling. JMIR Mhealth Uhealth 2019;7:e11898. 10.2196/11898 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2020-046051supp001.pdf (2.1MB, pdf)
bmjopen-2020-046051supp002.pdf (5.2MB, pdf)
bmjopen-2020-046051supp003.pdf (779.7KB, pdf)
bmjopen-2020-046051supp004.pdf (1.8MB, pdf)
Data Availability Statement
Data will be available on reasonable request 18 months after publication of the manuscript. Data can be requested by contacting the corresponding author or library-research-support@shu.ac.uk.