Abstract
Introduction:
Cutaneous warts caused by human papillomavirus are the most common dermatological diseases being contagious, recurrent, and recalcitrant. Most routinely used treatment modalities are destructive and can cause scarring. Immunotherapy is emerging as new modality of treatment, which enhances cell-mediated immunity against human papillomavirus for clearance of both treated and distant warts.
Aims:
The aim of this study was to compare efficacy between intralesional Vitamin D3, measles rubella (MR) vaccine, and purified protein derivative (PPD) injection in cutaneous warts.
Settings and Design:
This was a hospital-based interventional study.
Materials and Methods:
A total of 50 patients diagnosed with cutaneous warts were selected and divided into three groups with 15 patients in each. Treated with Vitamin D3 2 units of 6,00,000IU (15 mg/mL), 0.5 mL/dose 2 units of MR vaccine, and 10 TU of tuberculin PPD (0.1 mL) with 2 units of injections, respectively, with minimum three injections at 2-week intervals given. Follow-up of patients were done for 4 months.
Statistical Analysis Used:
A total of 45 patients were enrolled in the study and divided into three groups containing 15 patients each with the help of computer-generated random numbers.
Results:
Patients treated with Vitamin D3 showed complete clearance (12/15) with 3–4 sessions; side effect was pain at the site of injection. Injection with PPD was effective with complete clearance (10/15) but the number of session was higher. MR vaccine needs 6–8 sessions for complete clearance (3/15). Palmoplantar warts were more responding to treatment.
Conclusion:
Intralesional Vitamin D3, MR vaccine, and PPD are equally efficient in treating verrucae, although Vitamin D3 can be considered safe.
Keywords: Cutaneous warts, intralesional injection, PPD, R vaccine, vitamin D3
Key Message: Immunotherapy is one of the important modalities of treatment in cutaneous warts. The choice of intralesional injections depends on availability and efficacy.
INTRODUCTION
Cutaneous warts caused by human papillomavirus (HPV) are among the most common dermatological diseases. Warts are contagious, recurrent, and recalcitrant in nature. There are multiple treatment modalities, most of them being destructive resulting in scarring and/or dyspigmentation. Cell-mediated immunity (CMI) plays a major role in clearance of warts. Immunotherapy works on principal of enhancing the CMI, thereby clearing warts.[1,2] Various antigens have been used for this purpose. Immunotherapy is gaining popularity as an emerging new modality in treatment of warts. Very few studies have been published showing the efficacy of intralesional vitamin D3, purified protein derivative (PPD), and measles, mumps, and rubella (MMR) vaccine in the treatment of cutaneous warts with varied efficacy. The aim of this study was to compare the efficacy and safety in the treatment of different types of cutaneous warts.
MATERIALS AND METHODS
The study was conducted from February 2018 to February 2019 at the Department of Dermatology, Venereology and Leprosy, KVG Medical College, Sullia. The study was approved by the institutional Ethical Committee. This was a randomized single-blinded study. A total of 45 patients were enrolled in the study and were divided into three groups (groups A, B, and C) with help of computer-generated random numbers, each group containing 15 patients [Table 1].
Table 1.
Mode of treatment in three groups
| A | B | C |
|---|---|---|
| Vitamin D3 (0.2 mL, 15 mg/mL) + lignocaine (0.2 mL, 20 mg/mL) | MR vaccine (0.5 mL/dose) | 5 TU of tuberculin PPD 0.1 mL/dose |
| 15 | 15 | 15 |
MR, measles rubella vaccine; PPD, purified protein derivative
Patients in group A were injected with 2 units of vitamin D3 6,00,000 IU (15 mg/mL); patients in group B were injected with 2 units of measles rubella (MR) vaccine 0.5 mL/dose; and patients in group C were injected with 2 units of 5 TU of tuberculin PPD (0.1 mL/dose). In the case of multiple warts, two of the largest warts were selected for injection. Injections were given slowly into the base of each wart with a 27-gauge insulin syringe. For patients in group A, local anesthesia was injected before injecting vitamin D3 to prevent pain. Posttreatment, the patients were advised not to use any topical and oral medications.
Study design
Inclusion criteria
All patients, both males and females, clinically diagnosed to have warts (with no prior treatment with either topical or destructive modalities for at least 6 months) were selected for the study.
Exclusion criteria
Patients aged <10 years and >70 years
Warts with secondary infection
Pregnant and lactating females
Patients with keloidal tendency
Patients with evidence of immunosuppression including HIV
A prior history of hypersensitivity to intralesional injection
Past history of asthma, allergic skin disorders, meningitis, or convulsions
Anogenital warts
Cutaneous warts were diagnosed by history and clinical features. Baseline evaluation was made at the first visit, and the demographic data were recorded in a prestructured questionnaire designed for this study. Each patient’s clinical data including the site, number, size, and type of warts were noted on the first visit, along with clinical photographs.
The injections were repeated at 2 weekly intervals and in each visit the clinical response was documented by recording the number and size of warts. Most of the patients had complete clearance after three to four injections, whereas few required up to eight injections. The patients were followed up for 6 months after the last injection to evaluate treatment efficacy and for recurrence. Adverse reactions if any were noted every 2 weeks for the first 2 months and monthly thereafter.
The treatment response was graded as follows:
Complete clearance––resolution of all the warts both treated and distant warts. Moderate response––> 50% reduction in both size and number of lesions.
Mild response––< 50% reduction in both size and number of lesions.
No response–-no decrease in number or size or appearance of new warts.
RESULTS
A total of 45 patients were enrolled in our study. They were divided into three groups (groups A, B, and C) with 15 patients in each. Patients in group A were administered vitamin D3, group B MR vaccine, and group C PPD injection, respectively. Two patients in group B were lost for follow-up.
The clinical and demographic data are summarized in Table 2.
Table 2.
Summary of demographic and clinical data
| Total patients | 43 |
| Gender ratio (M:F) | 1:1.64 |
| Mean age in years (range) | 26 (10–57) |
| Mean number of warts (range) | 3.2 (1–12) |
| Type of wart (%) | |
| Verruca vulgaris | 8 (17.8) |
| Filiform wart | 2 (4.4) |
| Palmoplantar wart | 26 (57.8) |
| Plane wart | 9 (20) |
The duration of warts ranged from 1 week to 48 months with a mean of 1 year. The number of warts ranged from 1 to 12. The most common variant was palmoplantar warts (57.8%) followed by plane warts (20%), verrucae vulgaris (17.8%), and filliform warts (4.4%).
The mean numbers of intralesional injections for complete clearance (11) in group A were three injections; however, one patient showed complete clearance only after eight injections [Figures 1-3]. Recurrence was noted one patient at 6 months after the last injection [Table 3].
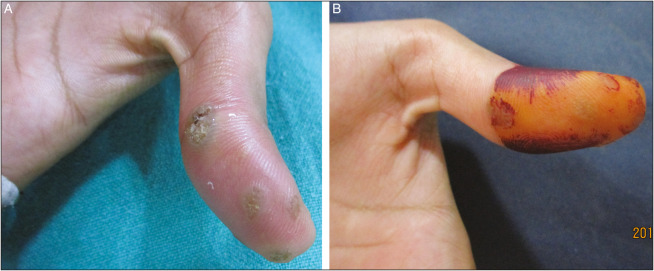
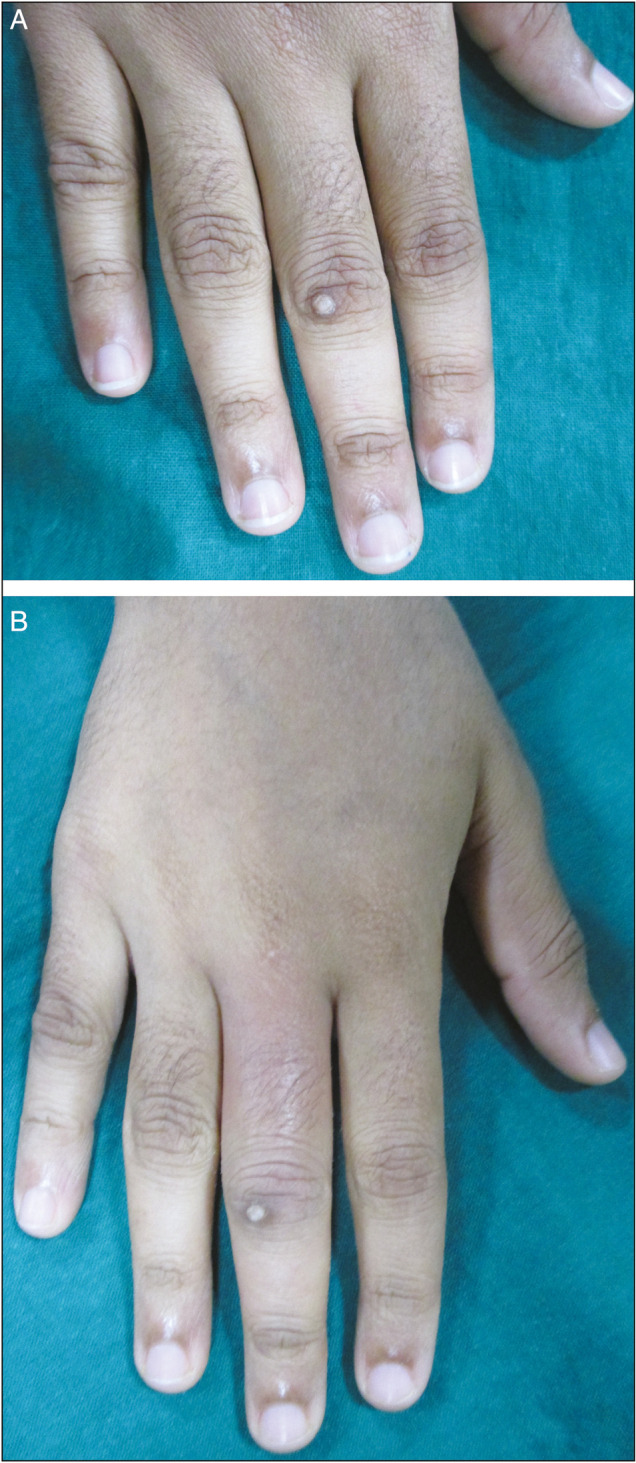
Figure 1.
Intralesional injection with vitamin D3 in the right sole of the feet at week 0 (A) and at week 3 (B) showing complete response leaving hyperpigmented scarring
Figure 3.

Intralesional injection of vitamin D3 on the solitary verruca at base of middle finger at week (0) and week (3) showing complete response
Table 3.
Treatment response in three groups
| Remarks | A | B | C |
|---|---|---|---|
| Complete response | 11 | 4 | 10 |
| Moderate response (>50%) | 3 | 3 | 1 |
| Mild response (<50%) | 1 | 4 | 3 |
| No response | 0 | 2 | 1 |
| Average number of injection required | 3 | 4 | 4 |
| Maximum number of injections | 8 | 5 | 7 |
| Recurrence | 1 | 0 | 1 |
| Adverse effects (number of patients) | 5 | 0 | 2 |
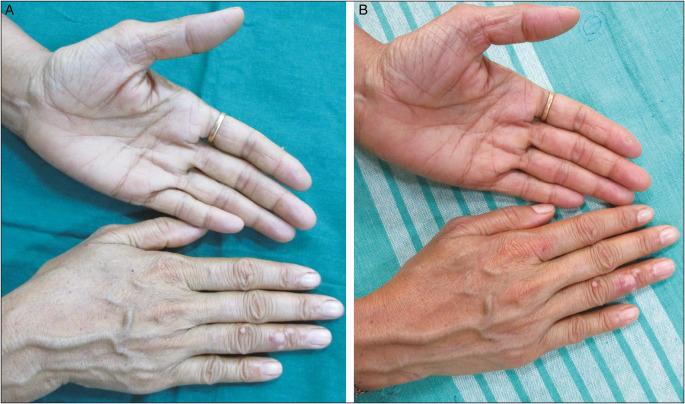
Figure 2.
Intralesional injection of vitamin D3 on the lateral aspect of foot at week 0 (A) and at week 3 (B) with complete response
In group B, 4 subjects showed complete clearance of warts with average requirement of four injections [Figures 4 and 5], whereas in group C complete clearance was observed in 10 subjects with average requirement of four injections. Recurrence was seen in one patient after 6 months of last injection [Table 3].
Figure 4.
Intralesional injection of MR vaccine in the dorsal aspect of the bilateral thumb at week 0 (A) and week 5 (B) with mild response few lesions have necrosed
Figure 5.

Intralesional injection of MR vaccine on the finger tips of palms at week 0 (A) and at week 5 (B) showing complete response
Adverse effects were most commonly seen in patients of group A followed by group C. Mild pain at the site of injection with persistent swelling was observed in five patients. The pain subsided within few hours and swelling resolved within 3–4 days.
In group C, two patients had mild swelling at the site of injection which resolved within 2 days. One among them developed fever on the third day which subsided with single dose of paracetamol 650 mg. The other patient developed erythema and itching surrounding the lesion after 1 week of injection [Figure 6] whereas in group C complete clearance was observed in 10 subjects with average requirement of 4 injections [Figures 7 and 8]. Interestingly the subsequent injections were uneventful in these two patients [Table 3].
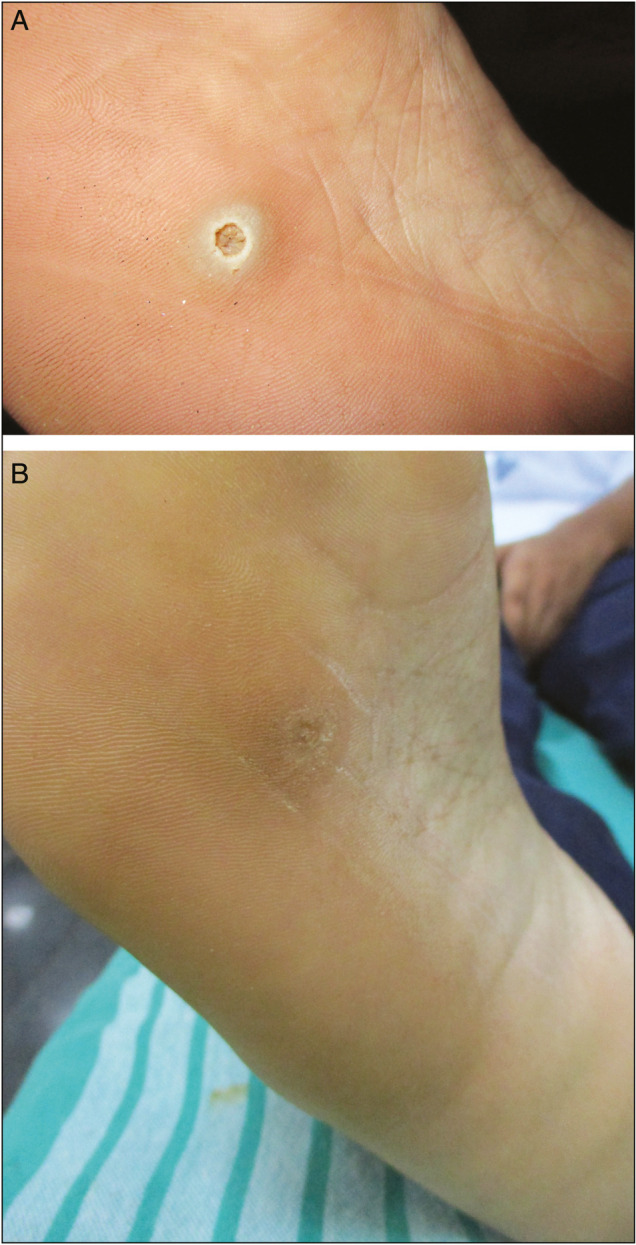
Figure 6.
Intralesional injection of PPD in the right thumb at week 0 (A) and at week 5 (B) with complete response
Figure 7.
Intralesional injection with purified protein derivative (PPD) in both ventral and dorsal aspect of palms at week 0 (A) and at week 4 (B) showing moderate response
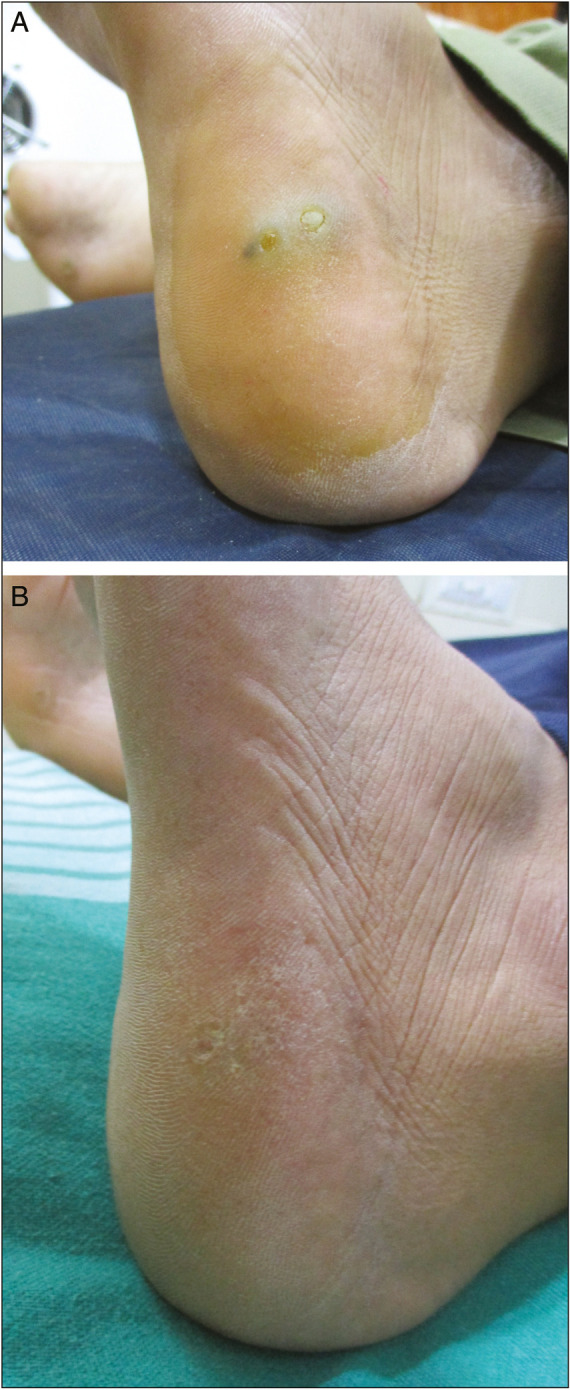
Figure 8.
Intralesional injection of PPD on the middle finger at week 0 (A) and at week 3 (B) showing moderate response, at week 4 complete shed off
DISCUSSION
Treatment of cutaneous warts is a therapeutic challenge at times. Various treatment modalities exist, each with its own pro and cons. Immune therapy has lately gained popularity due to its clearance rate, decreased recurrence, and insignificant adverse effects. It has been observed that a fully functional immune system is required to clear the HPV from epidermis. Various antigens such as BCG, PPD, MMR, Candida albicans, and Mycobacterium w vaccine have been used for immune therapy.[3]
Immunotherapy works by enhancing the CMI. It has been observed that the antigen injected (PPD and MR) stimulate the proliferation of peripheral mononuclear cells and T-helper cells against HPV infected cells. As the CMI gets more active, it also results in release of different immunoregulatory factors like interleukin (IL-21, IL-42), IFN-γ, TNF-α which further stimulate immune response against HPV.[4]
The mode of action of Vitamin D3 is still unclear. It is postulated that vitamin D acts by regulating epidermal cell proliferation and differentiation as well as to modulate cytokine production such as interleukin-6 (IL-6), IL-8, tumor necrosis factor (TNF-α), and TNF-γ via vitamin D receptor (VDR) pathway. In addition, vitamin D3 activates toll-like receptors (TLR) on macrophages that upregulate the expression of Vitamin D receptor (VDR) and Vitamin D 1α-hydroxylase genes, leading to induction of the antimicrobial peptide.[5]
PPD stimulates CMI nonspecifically through activation of Th1 cytokines, NK cells, and cytotoxic T cells. Meanwhile, PPD injection not only stimulates the local immunity but also activation of circulating T cells in the body leads to enhance clearance rate of injected as well as non injected, distant warts.[6,7,8] Although the product insert warns against use in pregnancy, no teratogenic effects of mantoux testing during pregnancy have been documented.
Meanwhile, it has been postulated that a functional host immune system, particularly CMI, is a necessary prerequisite for successful immunotherapy.
Table 4 shows various treatment response of cutaneous warts in different studies compared with the present study.
Table 4.
Response rate of various vaccines/antigen
| Study | Vaccine/antigen | Number of session given | Clearance rate (%) |
|---|---|---|---|
| Garg and Baveja[9,10] | Mycobacterium w vaccine | 10 | 93 |
| Saoji et al.[11] | PPD | 4 | 76 |
| Nofal et al.[12] | MMR vaccine | 5 | 63 |
| Majid and Imran[13] | C. albicans | 3 | 56 |
| Singh et al.[14] | Mycobacterium indicus pranii vaccine | 10 | 54 |
| Nimbalkar et al.[15] | PPD | 6 | 28 |
| Saini et al.[16] | MMR | More than 2 till resolution | 40 |
| Kavya et al.[17] | Vitamin D3 | 4 | 78.57 |
| This study | Vitamin D3 | 3 | 73.3 |
| PPD | 5 | 66.6 | |
| MR vaccine | 5 | 30.7 |
PPD = purified protein derivative, MMR = measles, mumps and rubella, C. albicans: Candida albicans
Side effects
Few patients treated with intralesional vitamin D3 showed necroses at injection site [Figure 9A] and one patient on intralesional PPD developed swelling over the dorsal aspect of the ring finger [Figure 9B].
Figure 9.
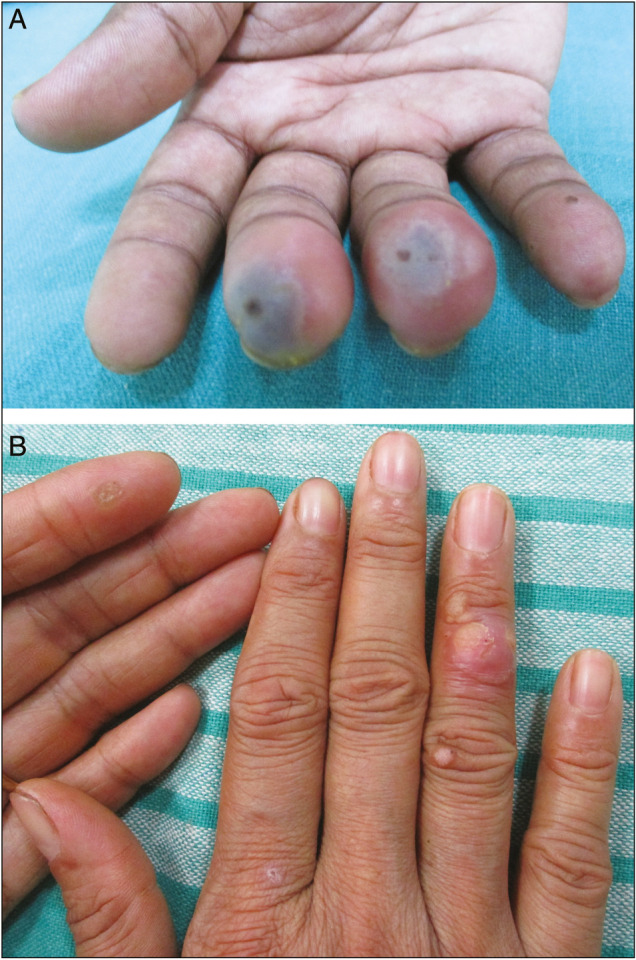
(A) On intralesional vitamin D3 injection at tip of the finger a patient developed necroses underlying injection site. (B) On intralesional PPD injection verruca over the dorsal aspect of the ring finger developed swelling
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Sterling JC, Handfield-Jones S, Hudson PM British Association of Dermatologists. Guidelines for the management of cutaneous warts. Br J Dermatol. 2001;144:4–11. doi: 10.1046/j.1365-2133.2001.04066.x. [DOI] [PubMed] [Google Scholar]
- 2.Gibbs S, Harvey I, Sterling J, Stark R. Local treatments for cutaneous warts: Systematic review. BMJ. 2002;325:461. [PMC free article] [PubMed] [Google Scholar]
- 3.Brodell RT, Johnson SM. Warts: diagnosis and management: an evidence based approach. New York, NY: Martin Dunitz; 2003. [Google Scholar]
- 4.Horn TD, Johnson SM, Helm RM, Roberson PK. Intralesional immunotherapy of warts with mumps, candida, and trichophyton skin test antigens: A single-blinded, randomized, and controlled trial. Arch Dermatol. 2005;141:589–94. doi: 10.1001/archderm.141.5.589. [DOI] [PubMed] [Google Scholar]
- 5.Liu PT, Stenger S, Li H, Wenzel L, Tan BH, Krutzik SR, et al. Toll-like receptor triggering of a vitamin D-mediated human antimicrobial response. Science. 2006;311:1770–3. doi: 10.1126/science.1123933. [DOI] [PubMed] [Google Scholar]
- 6.Eassa BI, Abou-Bakr AA, El-Khalawany MA. Intradermal injection of PPD as a novel approach of immunotherapy in anogenital warts in pregnant women. Dermatol Ther. 2011;24:137–43. doi: 10.1111/j.1529-8019.2010.01388.x. [DOI] [PubMed] [Google Scholar]
- 7.Wananukul S, Chatproedprai S, Kittiratsacha P. Intralesional immunotherapy using tuberculin PPD in the treatment of palmoplantar and periungual warts. Asian Biomed. 2009;3:739–43. [Google Scholar]
- 8.Elela IM, Elshahid AR, Mosbeh AS. Intradermal vs intralesional purified protein derivatives in treatment of warts. Golf J Dermatol Venereol. 2011;18:21–6. [Google Scholar]
- 9.Garg S, Baveja S. Intralesional immunotherapy for difficult to treat warts with mycobacterium w vaccine. J Cutan Aesthet Surg. 2014;7:203–8. doi: 10.4103/0974-2077.150740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gupta S, Malhotra AK, Verma KK, Sharma VK. Intralesional immunotherapy with killed mycobacterium w vaccine for the treatment of ano-genital warts: An open label pilot study. J Eur Acad Dermatol Venereol. 2008;22:1089–93. doi: 10.1111/j.1468-3083.2008.02719.x. [DOI] [PubMed] [Google Scholar]
- 11.Saoji V, Lade NR, Gadegone R, Bhat A. Immunotherapy using purified protein derivative in the treatment of warts: An open uncontrolled trial. Indian J Dermatol Venereol Leprol. 2016;82:42–6. doi: 10.4103/0378-6323.171650. [DOI] [PubMed] [Google Scholar]
- 12.Nofal A, Nofal E, Yosef A, Nofal H. Treatment of recalcitrant warts with intralesional measles, mumps, and rubella vaccine: A promising approach. Int J Dermatol. 2015;54:667–71. doi: 10.1111/ijd.12480. [DOI] [PubMed] [Google Scholar]
- 13.Majid I, Imran S. Immunotherapy with intralesional candida albicans antigen in resistant or recurrent warts: A study. Indian J Dermatol. 2013;58:360–5. doi: 10.4103/0019-5154.117301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Singh S, Chouhan K, Gupta S. Intralesional immunotherapy with killed mycobacterium indicus pranii vaccine for the treatment of extensive cutaneous warts. Indian J Dermatol Venereol Leprol. 2014;80:509–14. doi: 10.4103/0378-6323.144145. [DOI] [PubMed] [Google Scholar]
- 15.Nimbalkar A, Pande S, Sharma R, Borkar M. Tuberculin purified protein derivative immunotherapy in the treatment of viral warts. Indian J Drugs Dermatol. 2016;2:19–23. [Google Scholar]
- 16.Saini P, Mittal A, Gupta LK, Khare AK, Mehta S. Intralesional mumps, measles and rubella vaccine in the treatment of cutaneous warts. Indian J Dermatol Venereol Leprol. 2016;82:343–5. doi: 10.4103/0378-6323.175920. [DOI] [PubMed] [Google Scholar]
- 17.Kavya M, Shashikumar BM, Harish MR, Shweta BP. Safety and efficacy of intralesional vitamin D3 in cutaneous warts: An open uncontrolled trial. J Cutan Aesthet Surg. 2017;10:90–4. doi: 10.4103/JCAS.JCAS_82_16. [DOI] [PMC free article] [PubMed] [Google Scholar]