Abstract
Objectives
Vaccines are recognized as the most effective strategy for long-term prevention of coronavirus disease 2019 (COVID-19) because they can reduce morbidity and mortality. The purpose of the present study was to evaluate willingness to pay (WTP) for a future COVID-19 vaccination among young adults in Southern Vietnam.
Methods
A cross-sectional, descriptive, and analytic study was undertaken with data collected from a community-based survey in southern Vietnam for 2 weeks in May 2020. The contingent valuation method was used to estimate WTP for COVID-19 vaccine. The average amount that respondents were willing to pay for the vaccine was US$ 85.9 2 ± 69.01.
Results
We also found the differences in WTP according to sex, living area, monthly income, and the level of self-rated risk of COVID-19.
Conclusion
Our findings possibly contribute to the implementation of a pricing policy when the COVID-19 vaccine is introduced in Vietnam.
Keywords: contingent valuation method, COVID-19, vaccination, Vietnam, willingness to pay
Introduction
At the end of 2019, a strange pneumonia caused by a novel serotype of coronavirus was first reported in Wuhan, China. This diseases spread rapidly across the world in just a few weeks. On March 11, 2020, the World Health Organization (WHO) declared the coronavirus outbreak as a pandemic.1 On May, 17 2020, there were 216 countries with >4.5 million confirmed cases, 300 000 confirmed deaths, and 2 million recovered cases.2 The infection can spread through direct or indirect transmission (aerosol in the air).3 The majority of secondary infected cases are contagion in families, hospital or healthcare facilities, and social meeting without safe protective methods. The risk factors comprise chronic comorbidities, obesity, and smoking.4, 5, 6, 7, 8
To mitigate the spread of COVID-19, residents must follow social distancing and self-protection guidelines because there is currently no effective antiviral therapy for COVID-19. The disease has influenced educational systems worldwide.9 The unemployed rate in the service-supply industry has increased, and the COVID-19 outbreak has effected low-income workers.10 , 11 In efforts to “flatten the curve,”12 governments have administered border closure, travel limitation, and quarantine,13 which affected the entire economy, causing concern about economic depression.14 Chains of services were forced to close, which caused agricultural products prices to decrease by 20%.11 COVID-19 poses significant effects on communities, business, and organizations around the world. For long-time prevention of COVID-19, the availability of an efficacious vaccine is in need.11 Vaccination has become the most effective method to protect people from infectious diseases.15 , 16 In early April 2020, there were 115 COVID-19 vaccine candidates, and 73 of 78 projects are at investigative or preclinical phases. Some of the candidates have recently stepped into the clinical stages.17
The contingent valuation (CV) method is defined as “a tool to calculate an amount or value on goods and services that are typically not exchanged in the marketplace,”18 and it estimates both use values and nonuse values of environmental goods.19 The common definition of WTP is the maximum price that a consumer will accept to purchase one unit of a product or service.20 Although users may not want to pay for the services, they are willing to pay this amount rather than go without such services. WTP corresponds to the maximum payment the consumer accepts to receive the benefits in the future.21 Vietnam, a lower middle-income country,22 will face difficulties in deciding whether to introduce a new vaccine into an expanded vaccination program or to circulate the vaccine in the private market for people with a tight budget. Therefore, the estimate for the price of COVID-19 vaccines is necessary for both economic benefits and community health. The present study applied contingent valuation method to determine willingness to pay for COVID-19 vaccine among young adults in the south of Vietnam.
Methods
Study Design
Our researchers designed a cross-sectional survey on communities in southern Vietnam during 2 weeks in May 2020. Southern Vietnam consist of southeast and southwest region with the total population was about 34.9 million people in 2018.23 Inclusion criteria were people who (1) were ≥18 years old, (2) lived at the study site for >6 months, (3) communicate well by Vietnamese, (4) did not have a history of COVID-19, and (5) were willing to participate and were able to provide written consent.
Sample Size
The formula24 chosen to determine sample size:
| (1) |
With N as the sample size being determined, p as the proportion having the characteristics being measured (0.5), Z as the value of normal distribution at 95% confidence level (1.96), d as tolerable standard error (0.05). Using this equation, the minimum sample size was 385. This study presumed at 10% nonresponse and incomplete feedback rate, so there are at least 423 participants taking part in this survey.
Measurements
A self-administered structured questionnaire was developed in Vietnamese. A pilot study of 40 participants was carried out to validate the questionnaire. The questionnaire was divided into 3 domains: sociodemographic characteristics (8 items), knowledge of COVID-19 vaccine and seeking for the information of COVID-19 vaccination (4 items), and willingness to pay for the vaccine (3 items).
Data Collection
Voluntary participants were recruited through convenience sampling. Face-to-face interviews were undertaken between a participant and 1 of 10 interviewers. All the interviewers were undergraduate students from University of Medicine Pham Ngoc Thach, Ho Chi Minh City who attended a short-term training (Table 1 ).
Table 1.
Characteristics among participants in southern Vietnam, 2020 (n = 495).
| Characteristic | Male (n = 183) |
Female (n = 312) |
Total (n = 495) |
P value∗ | |||
|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | ||
| Age, y | |||||||
| 18-24 | 56 | 30.60 | 132 | 42.31 | 221 | 44.65 | .009 |
| 25-40 | 114 | 62.30 | 153 | 49.04 | 229 | 46.26 | |
| ≥40 | 13 | 7.10 | 27 | 8.65 | 45 | 9.09 | |
| Province | |||||||
| HCM City | 79 | 43.17 | 167 | 53.53 | 246 | 49.70 | .026 |
| Other† | 104 | 56.83 | 145 | 46.47 | 249 | 50.30 | |
| Area | |||||||
| Urban | 148 | 80.87 | 253 | 81.09 | 401 | 81.01 | .953 |
| Rural | 35 | 19.13 | 59 | 18.91 | 94 | 18.99 | |
| Education level | |||||||
| High school or less | 10 | 5.46 | 10 | 3.21 | 20 | 4.04 | .352 |
| Bachelor’s degree | 139 | 75.96 | 251 | 80.45 | 390 | 78.79 | |
| Postgraduate degree of higher | 34 | 18.58 | 51 | 16.35 | 85 | 17.17 | |
| Marital status | |||||||
| Single/divorced/widowed | 102 | 55.74 | 213 | 68.27 | 315 | 63.64 | .005 |
| Living with spouse/partner | 81 | 44.26 | 99 | 31.73 | 180 | 36.36 | |
| Occupation | |||||||
| Farmer/worker | 14 | 7.65 | 12 | 3.85 | 26 | 5.25 | .002 |
| Civil servant/officer/engineer/business | 56 | 30.60 | 67 | 21.47 | 123 | 24.85 | |
| Healthcare staff (physician, pharmacist, etc) | 75 | 40.98 | 130 | 41.67 | 205 | 41.41 | |
| Undergraduate student | 38 | 20.77 | 91 | 29.17 | 129 | 26.06 | |
| Housewife/unemployed | - | - | 12 | 3.85 | 12 | 2.42 | |
| Income (US$)‡ | |||||||
| <200 | 51 | 27.87 | 94 | 30.13 | 145 | 29.29 | .436 |
| 200-325 | 30 | 16.39 | 65 | 20.83 | 95 | 19.19 | |
| 325-450 | 45 | 24.59 | 56 | 17.95 | 101 | 20.40 | |
| 450-650 | 22 | 12.02 | 40 | 12.82 | 62 | 12.53 | |
| 650-1300 | 20 | 10.93 | 38 | 12.18 | 58 | 11.72 | |
| ≥1300 | 15 | 8.20 | 19 | 6.09 | 34 | 6.87 | |
| Self-rated risk of COVID-19 | |||||||
| Low | 95 | 51.91 | 123 | 39.42 | 218 | 44.04 | .010 |
| Moderate | 56 | 30.60 | 136 | 43.59 | 192 | 38.79 | |
| High | 32 | 17.49 | 53 | 16.99 | 85 | 17.17 | |
Eliciting WTP
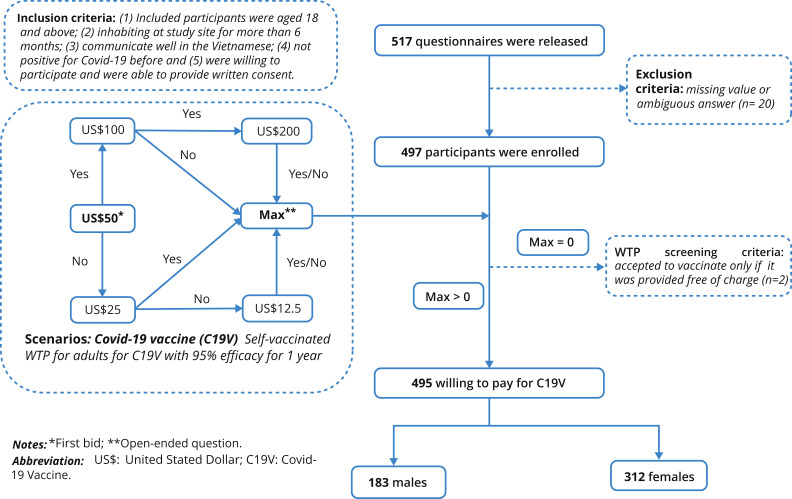
This study measured WTP by applied double-bounded dichotomous choice that gradually reduced the number of WTP responses for the hypothetical vaccine. The respondents were told about a hypothetical COVID-19 vaccine with typical attributes based on common features of a vaccine. The question was: “suppose that a vaccine COVID-19 was discovered that guaranteed 95% effective in a year. Suppose further that there are no adverse effects. Would you be willing to pay $50 for getting vaccinated?” If the respondent replied “yes” to this question, after that, similar questions with the price of $100, then $200 were asked. If the respondent answered “no” to the initial question ($50), they were asked the same question with a price at $25, then $12.5. After 2 questions, the participants’ maximum WTP was asked by an open-ended question. Because participants were not asked if they would get vaccinated for free, the lowest end for WTP was considered to be $0. We used double-bound dichotomous choice and bidding game approach to elicit WTP amount for COVID-19 (Fig. 1 ; Table 2 ).
Figure 1.
Characteristics among participants in Southern of Vietnam, 2020 (n = 495).
Table 2.
Information source regarding COVID-19 vaccine.
| Male |
Female |
Total |
P value∗ | ||||
|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | ||
| Heard about COVID-19 vaccine | |||||||
| No | 41 | 22.40 | 33 | 10.58 | 74 | 14.95 | <.001 |
| Yes | 142 | 77.60 | 279 | 89.42 | 436 | 85.05 | |
| Friends/relatives/colleagues | 66 | 36.07 | 122 | 39.10 | 188 | 37.98 | .502 |
| Health professionals (doctors, pharmacist, etc) | 56 | 30.60 | 116 | 37.18 | 172 | 34.75 | .138 |
| Books/newspapers | 49 | 26.78 | 87 | 27.88 | 136 | 27.47 | .790 |
| Social network/internet | 117 | 63.93 | 253 | 81.09 | 370 | 74.75 | <.001 |
| Seeking COVID-19 vaccine information | |||||||
| No | 39 | 21.31 | 65 | 20.83 | 104 | 21.01 | .900 |
| Yes | 144 | 78.69 | 254 | 81.41 | 406 | 82.02 | |
| Community health worker | 22 | 12.02 | 29 | 9.29 | 51 | 10.30 | .335 |
| Healthcare staff of hospital | 27 | 14.75 | 24 | 7.69 | 51 | 10.30 | .013 |
| Social network/internet/television | 132 | 72.13 | 223 | 71.47 | 355 | 71.72 | .876 |
| National guideline | 50 | 27.32 | 94 | 30.13 | 144 | 29.09 | .507 |
| Relatives/friends/colleagues | 48 | 26.23 | 73 | 23.40 | 121 | 24.44 | .479 |
COVID-19 indicates coronavirus disease 2019.
χ2 test, confidence level at 95%.
Statistical Analysis
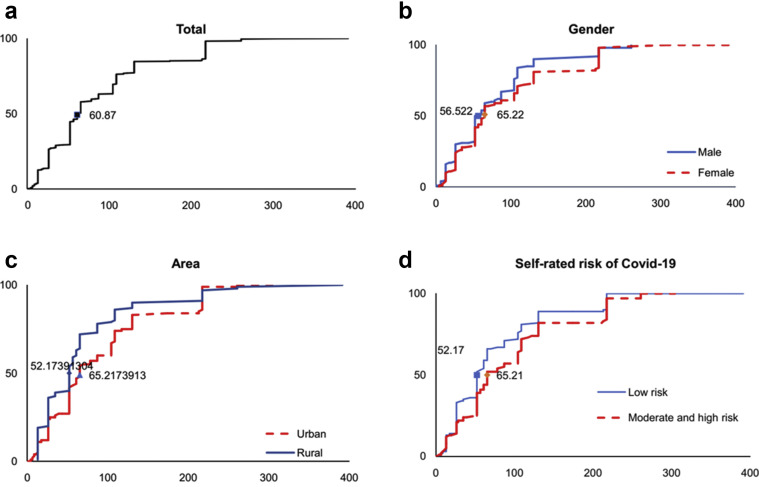
Microsoft Excel 2016 for Windows and SPSS version 20.0 were used for statistical analysis. Participants’ WTP was the maximum price expressed in the open-end question with an available scenario. WTP was summarized as the median and an interquartile range. Due to the non-normal distribution, the nonparametric tests were used to make a comparison in the median data between groups of participants with the Mann-Whitney U test for 2 variables and Kruskal-Wallis test for >2 variables. The statistically significance was set at P value less than .05. Figure 2 presents Cumulative percentage among gender, area and risk of COVID-19 group’ WTP for COVID-19 vaccination with medians reported.
Figure 2.
Cumulative percentages of WTP for COVID-19 vaccination among different groups of (a) Total (b) gender, (c) area and (d) risk of contracting.
Ethics Approval
The study protocol was reviewed and approved by the University of Medicine Pham Ngoc Thach, Ho Chi Minh City. Participants were asked to sign a written consent before enrolling. The anonymity and confidentiality of the participants were guaranteed.
Results
Of the total 495 respondents, 401 (81.01%) lived in urban areas. About 6.87% of the study population reported that their income was >1300 US$ monthly. Respondents were categorized into groups based on their risk of COVID-19, including 4.04% at a low level, 38.79% at a moderate level, and 17.17% at a high level. Nearly three-quarters of respondents (74.75%) accessed the information from social media and internet. The greatest percentage of participants seeking the information was via social network/internet/television with 71.72%.
Respondents tend to be willing to pay the number of US$ 85.92 ± 69.01 for COVID-19 vaccine. The significant differences were found in their willingness to pay regarding sex, living area, monthly income, and the level of self-rated risk of COVID-19 (P < .05). Specially, male participants (US$75.84) seem to be willing to pay for the vaccination less than their female counterpart (US$91.68). Urban residents might pay for the vaccine with US$89.53, compared with those living in rural areas with US$70.03. The higher income individuals earned per month, the greater amount of money they were willing to pay to prevent COVID-19. People who rated themselves as low risk seemed to pay less than those at the moderate and high risk of the disease.
Discussion
Awareness of COVID-19 Vaccine
The majority of the study sample reported they have known and sought for the information regarding COVID-19 vaccine. As COVID-19 is the ongoing worldwide pandemic, the demand for the vaccine to prevent the disease has risen significantly. According to a study in Thailand, 67.5% of respondent considered COVID-19 as a dangerous to seriously dangerous disease. In addition, a total of 57.9% reported feeling worried or most worried about the situation.26
The findings revealed that the most popular source of information about COVID-19 vaccine was social media and the internet (74.75%), whereas 34.75% of study subjects receive information from health professors. Meanwhile, only one-tenth of the study population has sought information relating to the vaccine from community health workers or healthcare staff at hospitals. Our results were consistent with the earlier studies in Vietnam regarding the vaccination of dengue fever,27 , 28 hepatitis B,29 and human papillomavirus.30 These research explored that different types of mass media consisting of social media, the internet, and television were main methods to provide information about COVID-19 vaccine to the Vietnamese general population. It can be explained by the rapid development of digital technology in Vietnam in the past few decades. Therefore, websites and television channels should be used for additional public campaigns that aim to draw citizens’ attention to the vaccination of COVID-19. On the other hand, communication with medical practitioners was another common source because people put the higher level of trust in them. This emphasized the vital role of medical staff in broadening knowledge of how to prevent the disease. The study in Thailand also confirmed more than half of the participants had heard COVID-19 from television (51.7%), 36.2% from the internet, and 6.7% from medical staff.26
Amount of WTP for COVID-19 Vaccine
We estimated the average WTP for a COVID-19 vaccine in our sample as US$ 85.92 ± 69.01, which was much higher than the fees for other vaccines in Vietnam. Respondents in the present study were WTP more because they experienced the outbreak of COVID-19. Obviously, the COVID-19 pandemic is a novel and dangerous disease.31 Other diseases were determined to have a lower mortality rate, such as typhoid fever (about 1%)32 or cholera (<1%).33 The starting point in this study was US$ 50, which was much higher than previously reported studies. The higher the first price is, the more people are willing to pay. Moreover, the high WTP was consistent with the high awareness and concern about COVID-19 vaccine in the study population (>80% have heard about COVID-19 vaccine and sought for the relevant information).
Nevertheless, the estimate of WTP for the vaccines to prevent COVID-19 in our sample was lower than in a study of dengue fever. Vo et al determined that the median WTP per adult and dengue vaccine were US$ 130.34 (type 1) and US$ 217.39 (type 2; for one person), or US$ 86.96 (type 1) and US$ 156.52 (type 2; for a parent). Additionally, parents were willing to pay US$ 108.70 (type 1) and US$ 195.65 (type 2) for their children’s’ vaccination.28 These variations may be due to discrepancies in the hypothetical scenarios, data collection, the starting point, and methods of statistical analysis.
WTP According To Sociodemographic Characteristics
The understanding of the importance of sociodemographic characteristics in the improvement of WTP for the COVID-19 vaccine and the strategies of vaccination programs in Vietnam. WTP for the COVID-19 vaccination in our research was affected by several factors. Participants, who were female, living in urban regions, earned higher wages, and at increased risk of COVID-19 were more likely to pay for the vaccine. Our findings were in line with the previous research. Vo et al emphasized those 5 factors having effects on WTP rates were income, marital status, living areas, locality, and education. As urban citizens earn a higher monthly income than those live in rural areas, they expressed a greater tendency to pay for dengue vaccine.28 Another study on WTP for dengue vaccine pointed out that individuals who were male and living in rural regions seem to be willing to pay less in comparison with the remaining groups.27 Therefore, the government should provide financial aid to enhance the vaccination campaign for poor people, especially for those living in remote areas (Table 3 ).
Table 3.
Willingness to pay (USD) for the COVID-19 vaccine from the perspective of the Vietnamese adults (2020, arithmetic mean [bootstrap 95% CI]).
| Variable | Mean | SD | Q1-25th | Q3-75th | 95% CI∗ | P value† |
|---|---|---|---|---|---|---|
| Sex | ||||||
| Male | 75.84 | 60.83 | 26.09 | 104.35 | 67.37-84.91 | .030 |
| Female | 91.68 | 22.27 | 28.26 | 130.43 | 80.07-97.01 | |
| Age, y | ||||||
| 18-24 | 85.96 | 65.57 | 34.24 | 108.70 | 77.93-94.69 | .102 |
| 25-40 | 82.30 | 30.23 | 26.09 | 108.70 | 72.77-90.47 | |
| ≥40 | 105.75 | 80.46 | 52.17 | 213.04 | 82.02-132.56 | |
| Province | ||||||
| HCM City | 79.86 | 31.02 | 26.09 | 108.70 | 72.50-88.21 | .264 |
| Other‡ | 91.71 | 35.81 | 26.09 | 130.43 | 82.51-101.15 | |
| Area | ||||||
| Urban | 89.53 | 18.33 | 32.61 | 130.43 | 83.53-96.85 | .004 |
| Rural | 70.03 | 68.22 | 26.09 | 86.96 | 56.43-85.01 | |
| Educational level | ||||||
| High school or less | 88.48 | 64.95 | 64.13 | 105.43 | 61.12-121.38 | .059 |
| Bachelor’s degree | 85.44 | 17.59 | 26.09 | 108.70 | 79.10-92.34 | |
| Postgraduate degree of higher | 86.98 | 69.61 | 28.26 | 130.43 | 73.05-102.22 | |
| Marital status | ||||||
| Single/divorced/widowed | 88.52 | 23.16 | 26.09 | 117.39 | 81.17-96.46 | .271 |
| Living with spouse/partner | 81.11 | 65.13 | 26.09 | 108.70 | 71.86-90.72 | |
| Occupation | ||||||
| Farmer/worker | 73.91 | 63.45 | 28.26 | 103.26 | 52.47-101.95 | .350 |
| Civil servant/officer/engineer/business | 79.76 | 63.17 | 26.09 | 108.70 | 69.49-91.51 | |
| Healthcare staff (physician, pharmacist, etc) | 90.00 | 61.77 | 28.26 | 130.43 | 80.46-100.40 | |
| Undergraduate student | 90.60 | 68.78 | 26.09 | 130.43 | 79.18-102.56 | |
| Housewife/unemployed | 51.09 | 30.19 | 26.09 | 65.22 | 34.39-68.76 | |
| Income (US$)§ | ||||||
| <200 | 79.88 | 62.78 | 26.09 | 108.70 | 70.40-90.43 | .045 |
| 200-325 | 77.37 | 67.41 | 26.09 | 104.35 | 65.60-91.28 | |
| 325-450 | 88.18 | 66.12 | 52.17 | 108.70 | 76.37-102.83 | |
| 450-650 | 78.86 | 67.54 | 26.09 | 108.70 | 61.74-97.01 | |
| 650-1300 | 97.53 | 75.10 | 52.17 | 130.43 | 78.59-117.06 | |
| ≥1300 | 120.52 | 88.13 | 52.17 | 217.39 | 91.73-147.63 | |
| Self-rated risk of COVID-19 | ||||||
| Low | 75.06 | 35.88 | 26.09 | 104.35 | 66.60-84.10 | .002 |
| Moderate | 100.19 | 73.30 | 52.17 | 130.43 | 90.76-111.31 | |
| High | 80.98 | 62.05 | 26.09 | 108.70 | 68.53-93.65 | |
| Total | 85.92 | 69.01 | 26.09 | 108.70 | 80.21-92.27 |
CI indicates confidence interval; COVID-19, coronavirus disease 2019; Q1, quartile 25% percentile; Q3, quartile 75% percentile; HCM City, Ho Chi Minh City; VND, Vietnam Dong.41
Arithmetic means and mean difference are calculated by bootstrapping method.
Mann-Whitney U test/Kruskal-Wallis test.
Other provinces in Southern of Vietnam.
Income per month; exchange rate: 1 USD = 23 000 VND (Dong et al.25).
In the present study, the self-rate risk of COVID-19 affected WTP for the vaccine. Respondents with high risk tend to pay more than those at low risk. Former research confirmed that if individuals perceived a high susceptibility to a disease, they would be more willing to pay for the vaccination. A study in Malaysia reported perception of susceptibility was related to WTP for hepatitis B vaccine.34 People who recognized themselves as susceptible to human papillomavirus in Korea were highly likely to accept the vaccination to prevent the disease.35 A cross-sectional study with the samples in 6 Europe countries indicated that the WTP for vaccines to prevent infection diseases rose with household income and risk aversion, while it decreased with age.36 Hence, it is critical to raise the public awareness of the COVID-19 pandemic as well as the need of the vaccine.
Vaccines as well as other healthcare services, which are nonmarket goods, are generally difficult to assess their cost side. Stated preference methods are used to explore the monetary value of this kind of goods and are likely to have a wide gap between the stated WTP and the WTP in real market. Protest zero bias is one of considerations that causes potential adversity on health economic stated-preference surveys. Based on a range of 10 debriefing statement, Frey et al found that one-fourth of protesters gave a zero WTP and only 0.4% of zero bids are genuine answers.37 Therefore, a WTP of zero may not represent a protest response. Nevertheless, how to treat protesters is a question because they are identified with various approaches38 , 39 and treated differently in WTP analysis.39, 40, 41 In this study, we excluded all respondents who gave zero bid answers because the WTP estimates may not be biased by only 2 eliminated values (0.4%). With potential protestors who gave a positive WTP (ie, higher than zero), we did not use any attempt to identify them and treated them as genuine statements. We supposed that COVID-19 vaccine is in a hot market. People who were prepared to pay to get vaccinated did have a positive outlook toward the vaccine, and it is not fair to suspect them to be protestors. If people have any hesitation on attributes of the vaccination (ie, afraid of injections, adverse effects, etc), they did not agree to get vaccinated. The acceptability toward the vaccine is another aspect that should be analyzed in a separated article.
Data collection were conducted based on convenience sampling. Passers-by on streets, markets, coffee shops, parks, hospitals, and around schools were invited to participate. However, an undesirable adversity happened during the sampling process; a large amount of people would not to talk due to worry about COVID-19 transmission. Healthcare professionals as well as undergraduates seems to be easier to persuade to take part in the interview. Moreover, we excluded individuals who had no income because they had no potential to pay for the vaccines. These 2 reasons explained the low proportion of white-collar workers (25%) and dependent people (ie, housewives and retired people [2.5%]), resulting in high percentage of healthcare staff and students.
Despite these biases, he study has some limitations. Firstly, our sample was small and selected in Ho Chi Minh City as well as its surrounding areas due to the limited budget and time constraints. Therefore, bias selection could be a potential problem, and this might raise the question of the validity of extrapolating the results to the entire country. Additionally, a cross-sectional design could decrease the generalizability of our findings and the possibility of exploring the causality between WTP and sociodemographic aspects. Additional research should cover the different regions and provinces across the country to attain nationally representative results.
Conclusion
The results will potentially contribute to the development of an evidence-based policy framework for the provision of the COVID-19 vaccine price. The pricing strategy should also be considered to reduce the cost of the vaccine as well as increase vaccination coverage.
Article and Author Information
Author Contributions: Concept and design: N. Vo, T. Nguyen, P. Nguyen, Tran, T. Vo
Acquisition of data: N. Vo, T. Nguyen, P. Nguyen, Tran, T. Vo
Analysis and interpretation of data: P. Nguyen, Tran, T. Vo
Drafting of the manuscript: T. Nguyen, P. Nguyen, Tran, T. Vo
Critical revision of the paper for important intellectual content: N. Vo, T. Nguyen, P. Nguyen, Tran, T. Vo
Statistical analysis: N. Vo, P. Nguyen, Tran, T. Vo
Supervision: T. Vo
Conflict of Interest Disclosures: The authors reported no conflicts of interest.
Funding/Support: The authors received no financial support for this research.
Acknowledgment
The authors are grateful to all respondents who participated in this study, and to the data collectors for their work on this study. We would like to thank the expert panel of the questionnaire used in this study.
References
- 1.Gorbalenya A.E. Severe acute respiratory syndrome-related coronavirus: the species and its viruses, a statement of the Coronavirus Study Group. BioRxiv. 2020 https://www.biorxiv.org/content/10.1101/2020.02.07.937862v1 [Google Scholar]
- 2.Worldometer Reported cases and deaths by country, territory, or conveyance. https://www.worldometers.info/coronavirus/
- 3.Moriyama M., Hugentobler W.J., Iwasaki A. Seasonality of respiratory viral infections. Annu Rev Virol. 2020;7(1):83–101. doi: 10.1146/annurev-virology-012420-022445. [DOI] [PubMed] [Google Scholar]
- 4.Yan L.-M., Wan L., et al. Viral dynamics in mild and severe cases of COVID-19. Lancet Infect Dis. 2020;20(6):656–657. doi: 10.1016/S1473-3099(20)30232-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Liu K., Fang Y.-Y., Deng Y., et al. Clinical characteristics of novel coronavirus cases in tertiary hospitals in Hubei Province. Chin Med J (Engl) 2020;133(9):1025–1031. doi: 10.1097/CM9.0000000000000744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sundararaj V. Optimal task assignment in mobile cloud computing by queue based ant-bee algorithm. Wirel Pers Commun. 2019;104:173–197. [Google Scholar]
- 7.Liang W., Guan W., Chen R., et al. Cancer patients in SARS-CoV-2 infection: a nationwide analysis in China. Lancet Oncol. 2020;21:335–337. doi: 10.1016/S1470-2045(20)30096-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Vinu S. An efficient threshold prediction scheme for wavelet based ECG signal noise reduction using variable step size firefly algorithm. Int J Intell Eng Syst. 2016;9:117–126. [Google Scholar]
- 9.UNESCO COVID-19 educational disruption and response. https://en.unesco.org/covid19/educationresponse
- 10.Thompson D. The coronavirus will be a catastrophe for the poor. https://www.theatlantic.com/ideas/archive/2020/03/coronavirus-will-supercharge-american-inequality/608419/
- 11.Centre TIA Types of vaccines. https://www.immune.org.nz/vaccines/vaccine-development/types-vaccines
- 12.Burkert A., Loeb A. Flattening the COVID-19 curves. https://blogs.scientificamerican.com/observations/flattening-the-COVID-19-curves/
- 13.Prices of agricultural commodities drop 20% post COVID-19 outbreak. https://realtime.rediff.com/news/india/Prices-of-agricultural-commodities-drop-20-post-COVID19-outbreak/955078599584b749?src=interim_alsoreadimage
- 14.Financial Times Coronavirus declared a pandemic as fears of economic crisis mount. https://www.ft.com/content/d72f1e54-6396-11ea-b3f3-fe4680ea68b5
- 15.Sundararaj V. Optimised denoising scheme via opposition-based self-adaptive learning PSO algorithm for wavelet-based ECG signal noise reduction. Int J Biomed Eng. Technol. 2019;31:325. [Google Scholar]
- 16.Hajj Hussein I., et al. Vaccines through centuries: major cornerstones of global health. Front Public Health. 2015;3:269. doi: 10.3389/fpubh.2015.00269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Le T.T., et al. The COVID-19 vaccine development landscape. Nat Rev Drug Discov. 2020;19:305–306. doi: 10.1038/d41573-020-00073-5. [DOI] [PubMed] [Google Scholar]
- 18.Ajzen I., Driver B. Contingent value measurement: on the nature and meaning of willingness to pay. Journal Consum Psychol. 1992;1(4):297–316. [Google Scholar]
- 19.Mitchell R.C., Carson R.T. McGraw-Hill; New York, NY: 1989. Using Surveys to Value Public Goods: The Contingent Valuation Method. [Google Scholar]
- 20.Varian H.R. 3rd ed. Norton; New York, NY: 1992. Microeconomic Analysis. [Google Scholar]
- 21.Le Gall-Ely M. Definition, measurement and determinants of the consumer's willingness to pay: a critical synthesis and avenues for further research. Recherche et Applications en Marketing (English Edition) 2009;24(2):91–112. [Google Scholar]
- 22.Kim J., Poensgen K. "Transition Finance Country Study Viet Nam: On the threshold of transition", OECD Development Co-operation Working Papers. No. 60 OECD Publishing; Paris: 2019. [DOI] [Google Scholar]
- 23.https://www.gso.gov.vn/en/population/
- 24.Lwanga S.K., Lemeshow S. World Health Organization; Geneva, Switzerland: 1991. Sample size determination in health studies: a practical manual. [Google Scholar]
- 25.https://www.sbv.gov.vn/TyGia/faces/TyGia.jspx?_afrLoop=20405391881987224&_afrWindowMode=0&_adf.ctrl-state=fgko1j03l_4
- 26.Srichan P., et al. Knowledge, attitude and preparedness to respond to the 2019 novel coronavirus (COVID-19) among the bordered population of northern Thailand in the early period of the outbreak: a cross-sectional study. WHO South-East Asia J Public Health. 2020;9(2):118–125. doi: 10.4103/2224-3151.294305. [DOI] [PubMed] [Google Scholar]
- 27.Nguyen L.H., Tran B.X., Do C.D., et al. Feasibility and willingness to pay for dengue vaccine in the threat of dengue fever outbreaks in Vietnam. Patient Prefer Adherence. 2018;12:1917–1926. doi: 10.2147/PPA.S178444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Vo T.Q., Tran Q.V., Vo Nx. Customers' preferences and willingness to pay for a future dengue vaccination: a study of the empirical evidence in Vietnam. Patient Prefer Adherence. 2018;12:2507–2515. doi: 10.2147/PPA.S188581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Nguyen A.T.L., LE X.T.T., Do T.T.T., et al. Knowledge, preference, and willingness to pay for hepatitis b vaccination services among woman of reproductive age in Vietnam. BioMed Research Int. 2019 doi: 10.1155/2019/9154918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tran B.X., Le X.T.T., Do T.T.T., et al. Knowledge, attitude, and practice on and willingness to pay for human papillomavirus vaccine: a cross-sectional study in Hanoi. Vietnam. Patient Prefer Adherence. 2018;12:945–954. doi: 10.2147/PPA.S165357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Worldometer Coronavirus pandemic. https://www.worldometers.info/coronavirus Available from:
- 32.World Health Organization. Background paper on vaccination against typhoid fever using new-generation vaccines. Presented at SAGE November 2007 meeting. Geneva, Switzerland; 2007.
- 33.Harris J.B., LaRocque R.C., Qadri F., Ryan E.T., Calderwood S.B. Cholera. Lancet. 2012;379(9835):2466–2476. doi: 10.1016/S0140-6736(12)60436-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Rajamoorthy Y., Radam A., Taib N.M., Rahim K.A., et al. Willingness to pay for hepatitis B vaccination in Selangor, Malaysia: a cross-sectional household survey. PLoS One. 2019;14(4) doi: 10.1371/journal.pone.0215125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Oh J.K., Lim M.K., Yun E.H., Lee E.-H., Shin H.-R. Awareness of and attitude towards human papillomavirus infection and vaccination for cervical cancer prevention among adult males and females in Korea: a nationwide interview survey. Vaccine. 2010;28(7):1854–1860. doi: 10.1016/j.vaccine.2009.11.079. [DOI] [PubMed] [Google Scholar]
- 36.Himmler S., van Exel J., Perry-Duxbury M., Brouwer W. Willingness to pay for an early warning system for infectious diseases. Eur J Health Econ. 2020;21(5):763–773. doi: 10.1007/s10198-020-01171-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Frey U.J., Pirscher F. Distinguishing protest responses in contingent valuation: a conceptualization of motivations and attitudes behind them. PLoS One. 2019;14(1) doi: 10.1371/journal.pone.0209872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Dziegielewska D.A., Mendelsohn R. Does “no” mean “no”? A protest methodology. Environmental and Resource Economics. 2007;38(1):71–87. [Google Scholar]
- 39.Bonnichsen, O. and J. Ladenburg. Reducing protest zero bias in stated preference surveys-Testing a protest reduction entreaty in a health economic choice experiment. iInternational Choice Modelling Conference. 2009. Citeseer.
- 40.Meyerhoff J., Liebe U. Protest beliefs in contingent valuation: explaining their motivation. Ecological Economics. 2006;57(4):583–594. [Google Scholar]
- 41.Strazzera E., Genius M, Scarpa R, Hutchinson G. The effect of protest votes on the estimates of WTP for use values of recreational sites. Environmental and Resource Economics. 2003;25(4):461–476. [Google Scholar]