Abstract
Purpose
Nurses who care for COVID-19 patients are more likely to be affected psychologically than nurses who do not, and reactions such as increased fear may lead to psychological problems among nurses. The aim of this study was to determine the COVID-19 fear level of surgical nurses by using the Fear of COVID-19 Scale.
Design
A descriptive and cross-sectional study.
Methods
Totally, 202 surgical nurses who take care of suspected or infected COVID-19 patients working in pandemic and surgical units of a university hospital were included in the study. For data collection, “Nurse Characteristics Form” and “Fear of COVID-19 Scale” were used. Study data was analyzed with the descriptive statistics, Mann-Whitney U test, Spearman Correlation test.
Findings
The mean total COVID-19 fear score of the nurses was 25.09 ± 7.29 (min: 7, max: 35) and nurses who received training related to COVID-19 had statistically lower fear than those who did not (U = 3773.500; P= .027). Losing a patient because of COVID-19, being older and experienced in nursing significantly affected the total fear score of nurses (respectively, U = 3899.000; P= .004; rs = 0.152; P = .031, rs = 0.205; P = .003).
Conclusions
Surgical nurses have a moderate level of COVID-19 fear and it is recommended to conduct appropriate on-line training programs to develop psychological support strategies.
Keywords: COVID-19, fear, pandemic, psychological impact, surgical nursing
Coronavirus disease 19 (COVID-19) is a viral infection caused by the SARS-CoV-2 virus and causing global health problems because of the pandemic.1 , 2 This disease was first reported in Wuhan, China's Hubei province, with the first cases of unknown pneumonia cases, and it was declared as a pandemic by WHO as of March 2020.3 , 4 As of April 03, 2021, the total number of reported and confirmed COVID-19 cases in the world was 129,902.402, including 2,831.815 deaths.5 In Turkey, the first COVID-19 positive cases were reported in March 2020, and as of April 03, 2021, Republic of Turkey Ministry of Health has reported a total of 3,445.052 confirmed cases including 32,078 deaths.6
Parallel to the rapid spread of the cases, several information about COVID-19 and news that highlight rising morbidity and mortality rates can cause fear and anxiety.7 , 8 Furthermore, stressor conditions such as the risk of virus transmission, the implementation of social isolation measures, quarantine procedures, financial losses, the risk of getting sick and death can also cause fear in individuals.9 , 10 Healthcare workers are the most affected group in this process and in addition to working in one-on-one contact with patients, they experience serious anxiety and fear due to the conditions such as increased workload, staying away from their families, changes in working conditions, being in isolation, and inability to access personal protective equipment.11 - 13 In a study conducted with nurses in Pakistan who take care of COVID-19 patients during the pandemic process, it was stated that 92.3% of the nurses experienced moderate and severe anxiety.12 Another study from China showed that 71.5% of the healthcare workers treating COVID-19 patients were distressed and 44.6% of them reported to have anxiety.14
Although COVID-19 is not a surgical condition, given the number of infected individuals in communities, it is inevitable that COVID-19 patients will also require surgical care. However, during the COVID-19 pandemic, health systems and hospitals should adapt their working procedures to this new situation to meet the increasing need for intensive care units and to make the control of infection effective. 13 , 15 Among the change practices, elective surgeries are cancelled, surgical procedures are restricted with conditions requiring emergency, many surgical units re-adapted their regular clinical activities to support the care of increasing COVID-19 cases and surgical nurses are re-assigned to strengthen the COVID-19 pandemic units or intensive care units.16 , 17 In addition to these changes encountered during the pandemic process, treatment and care processes continue in units such as emergency services, operating rooms and surgical intensive care units, and healthcare professionals also continue to care for patients suspected or infected with COVID-19 in these units.18 , 19 At the hospital where the present study was conducted, except cardiovascular surgery, all the nurses in surgical units started to take care of suspected or infected COVID-19 patients in pandemic and surgical units within the pandemic process.
It is likely that nurses who work primarily in the care of COVID-19 patients in these areas, which are among high-risk units, are more physically and psychologically affected by this process than nurses who do not. It has been reported that among the healthcare professionals affected by COVID-19 in Italy, 43.2% of them were nurses20 and in India, 27% of the COVID-related deaths among healthcare professional were from the surgical units including emergency care, general surgery and orthopedics.21 Similarly, studies from different countries searching the deaths from COVID-19 among healthcare professionals show that, most of them were working in the fields of emergency and surgical specialties.22, 23 - 24 In the literature, it is stated that psychological reactions such as anxiety and fear can have significant effects on individuals' behaviors such as excessive panic, inability to think clearly, and burnout, therefore it is important to evaluate the psychological responses of healthcare professionals to COVID-19.25 - 27
Considering that nurses provide one-on-one care to patients and patient safety is important in surgical units, it is important to evaluate the COVID-19 fear levels of nurses working in surgical units regarding. Although there are studies examining the anxiety levels of healthcare professionals in the literature, there are insufficient studies examining the COVID-19 fears of surgical nurses working pandemic units during the pandemic process. Therefore, this study aims to determine the COVID-19 fear level of surgical nurses who take care of suspected or infected COVID-19 patients in pandemic and surgical units. The data obtained from the study will contribute to the determination of the psychological effects of the pandemic process on surgical nurses.
Research Questions
The research questions of this study were:
-
1.
What is the COVID-19 fear level of surgical nurses?
-
2.
Do the descriptive characteristics of surgical nurses affect their COVID-19 fear level?
Methods
Study Design and Sample
This descriptive and cross-sectional study was carried out with the nurses in a research hospital of a city in Aegean region of Turkey during November, 2020. The study population comprised 216 nurses who worked as a surgical nurse before the pandemic and now continue to work in pandemic units including emergency service, surgical wards, intensive care units and operating room. The inclusion criteria were being voluntary to participate in this study, working in a surgical unit and being re-assigned to a pandemic unit, actively taking care of suspected or infected COVID-19 patients.
By inferring that the COVID-19 fear prevalence perceived by the nurses would be 50%, with a confidence level of 99.99% and the margin of error 5%, the study sample was calculated to be minimum 190.28 The final sample included 202 nurses. For data collection, the convenience sampling method was used, and all data were provided voluntarily.
Study Protocol and Data Collection
By using convenience sampling method, because of the difficulty to collect data via face-to-face during pandemic, nurses were invited to the study via a social media platform (WhatsApp) that is being used at the hospital and involves the cell phone numbers of all the hospital nurses. Before sharing the online survey link via social media platform, all nurses were informed about the purpose of the study, and surgical nurses who work in pandemic and surgical units (urology, orthopedic surgery, brain surgery, eye surgery, general surgery, emergency unit and operating room) were requested to participate this study voluntarily. Following, the online survey form created by using the Google Forms was sent as an online link and nurses were requested to fill out. In the online survey form, nurses were able to respond only once. Informed consent was obtained electronically from each nurse at the beginning page of the survey form. For data collection, “Nurse Characteristics Form” and “Fear of COVID-19 Scale (FCV-19S)” were used.
Nurse Characteristics Form
Nurse characteristics form was used to collect the descriptive characteristics of the nurses and was developed by the researchers in accordance with the relevant literature.12 , 13 , 29 This form consisted a total of twelve questions to determine the characteristics of nurses including age, gender, marital status, having a child, educational status, working schedule, duration of nursing experience, the status of receiving training related to COVID-19 and experience on COVID-19 (lost patient because of COVID-19, diagnosed with COVID-19, had or lost a relative diagnosed with COVID-19).
Fear of COVID-19 Scale (FCV-19S)
This scale was developed by Ahorsu et al26 to measure the fear of COVID-19 among individuals. The scale was translated and validated in Turkish by Satıcı et al30 The total Cronbach's alpha value was reported to be 0.82 for the original scale and to be 0.84 for the Turkish scale.26 , 29 In the literature, this scale was reported to be valid to identify the psychological impacts of COVID-19 on health professionals.31 , 32 In their study Khattak et al31 used this scale to evaluate the effect of COVID-19 fear on mental health of nurses and found the reliability value of this scale as 0.82. Labrague and de los Santos32 also used this scale in their study to examine the influence of fear of COVID-19 on nurses’ psychological distress and reported the Cronbach's alpha value of the scale as 0.87. In the present study, the total Cronbach's alpha value was found to be 0.92.
The scale includes 7 positive items; “I am most afraid of coronavirus” as the first item, “It makes me uncomfortable to think about coronavirus” as the second item, “My hands become clammy when I think about coronavirus” as the third item, “I am afraid of losing my life because of coronavirus” as the forth item, “When watching news and stories about coronavirus on social media, I become nervous or anxious” as the fifth item, “I cannot sleep because I'm worrying about getting coronavirus” as the sixth item and “My heart races when I think about getting coronavirus” as the seventh item. The items are scored using a 5-point Likert type scale including the answers; “5- strongly agree,” “4- agree," “3- neither agree nor disagree,” “2- disagree,” “1- strongly disagree.” The minimum score possible is 7 and the highest score possible is 35. The increase in total score indicates the greater fear of COVID-19.26 , 30
Ethical Considerations
In this study, all procedures were performed in accordance with the ethical standards, and by the Helsinki Declaration. To conduct this study, the necessary permission was obtained from the Turkey Republic Ministry of Health COVID-19 Scientific Research Evaluation Commission and the ethical (38824465-020) and institutional permissions (45786011-602.03.99) were obtained from the University Ethics Committee of the Faculty of Medicine and the hospital directory of this study. The permission to use the Turkish version of the FCV-19S was obtained via e-mail. Informed consent was obtained from nurses, and they were informed that the data will be kept confidential and will only be used for the study aim.
Data Analysis
The descriptive data of this study were evaluated using number, mean, standard deviation, and numbers with percentage. The data distribution was analyzed by ANOVA test and for the not normally distributed data, the Mann-Whitney U test and the Kruskal Wallis test were used to compare descriptive features of the nurses and the total scale score. To analyze the relationship between age and duration of nursing experience, and scale total scores, Spearman Correlation test was used. The IBM SPSS Statistics 22.0 (IBM, Armonk, NY, USA) software package was used for analyzing the data and P< .05 was considered as the statistical significance level.
Results
Of the nurses in this study, 71.3% were female; 53% were married; 51.5% had a child; 74.3% had undergraduate and higher education degree; 91.1% worked on the night shift; 64.9% received training (through in-service trainings, and participating in webinars) related to COVID-19 previously. The mean age of the nurses was 35.54 ± 8.38 years, and the mean duration of nursing experience was 147.41 ± 108.03 months. The mean total fear score of the nurses who received training related to COVID-19 was statistically lower than those who did not (U = 3773.500; P = .027) and of the nurses who lost a patient because of COVID-19 was statistically higher than those who did not (U = 3899.000; P = .004) (Table 1 ). Table 1 also presents the nurses’ experiences of COVID-19.
Table 1.
Fear Scores of Nurses According to Their Characteristics and COVID-19 Experiences (N = 202)
| Variables | n | % | Mean | SD | P Value Test |
|---|---|---|---|---|---|
| Gender Female Male |
144 58 |
71.3 28.7 |
25.64 23.74 |
7.01 7.83 |
U = 3614.000 P = .134 |
| Marital status Married Not married |
107 95 |
53.0 47.0 |
25.11 25.08 |
7.44 7.16 |
U = 5046.500 P = .931 |
| Having a child Yes No |
104 98 |
51.5 48.5 |
25.40 24.77 |
7.33 7.28 |
U = 4840.000 P = .537 |
| Educational status High school Undergraduate and higher |
52 150 |
25.7 74.3 |
25.17 25.07 |
7.74 7.15 |
U = 3767.500 P = .715 |
| Working schedule Night shift Day shift |
184 18 |
91.1 8.9 |
25.22 23.83 |
7.12 9.00 |
U = 1539.500 P = .622 |
| Received training related to COVID-19 | |||||
| Yes No |
131 71 |
64.9 35.1 |
24.25 26.66 |
7.37 6.93 |
U = 3773.500 P = .027* |
| Lost patient because of COVID-19 | |||||
| Yes No |
105 97 |
52.0 48.0 |
26.22 23.87 |
7.40 7.00 |
U = 3899.000 P = .004* |
| Diagnosed with COVID-19 Yes No |
32 170 |
15.8 84.2 |
23.68 25.36 |
8.37 7.07 |
U = 2557.500 P = .591 |
| Had a relative diagnosed with COVID-19 | |||||
| Yes No |
77 125 |
38.1 61.9 |
25.63 24.76 |
8.08 6.77 |
U = 4316.000 P = .217 |
| Lost relative because of COVID-19 | |||||
| Yes No |
10 192 |
5.0 95.0 |
21.60 25.28 |
9.25 7.16 |
U = 749.500 P = .242 |
U, Mann-Whitney U test; KW, Kruskal-Wallis test; SD, standard deviation.
Values shown in boldface: P < .05 was considered as the statistical significance level.
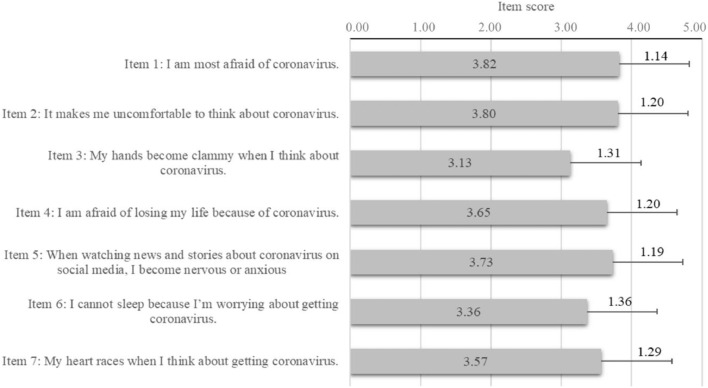
The mean total fear score of the nurses was found to be 25.09 ± 7.29 (min:7, max: 35). According to the item scores received from the scale, the mean score of “I am afraid of coronavirus” and “It makes me uncomfortable to think about coronavirus” were relatively higher than the other item scores (respectively, 3.82 ± 1.14; 3.80 ± 1.20) (Figure 1 ).
Figure 1.
Item scores received from the Fear of COVID-19 Scale (mean ± standard deviation).
A statistically significant correlation was found between the fear scores, and age and duration of nursing experience (respectively, rs = 0.152; P = .031, rs = 0.205; P = .003). There was no statistically significant difference between the nurses’ descriptive characteristics (gender, marital status, having a child, educational status, working schedule), COVID-19 experiences (diagnosed with COVID-19, had or lost a relative diagnosed with COVID-19) and the mean fear scale scores (P > .05; Table 2 ).
Table 2.
The Age and Duration of Nursing Experience of the Nurses With Total Scores of the Fear Scale With Correlation Coefficients and Significance Levels (N = 202)
| Total Scale Score Mean ± SD | Test P Value | |
|---|---|---|
| Age (min-max) |
35.54 ± 8.38 years (21-53) |
rs = 0.152 |
| P = .031* | ||
| Duration of nursing experience (min-max) | 147.41 ± 108.03 months (4-360) |
rs = 0.205 |
| P =.003* |
SD, standard deviation; rs, Spearman correlation.
Values shown in boldface: P < .05 was considered as the statistical significance level.
Discussion
With the sudden outbreak of the COVID-19 pandemic, the healthcare systems have been affected all around the world, and furthermore healthcare professionals have encountered important challenges, particularly surgical units. All the elective surgeries except for the urgent categories were cancelled, and nurses at the surgical units started to work at the pandemic units to care of suspected or infected COVID-19 patients. With this pandemic process, surgical nurses had to adapt with the new disease, the new healthcare system, the changed workplace environment, and take care of suspected or infected COVID-19 patients in pandemic and surgical units. There was a sudden interruption of their usual clinical perioperative care activities, and they had to adapt themselves with the re-assigned nursing roles and to work in unfamiliar COVID-19 pandemic unit conditions.33 Therefore, the aim of this study was to evaluate the psychological fear responses of surgical nurses to COVID-19. The study results showed that nurses had moderate fear of COVID-19, and the mean fear score was 25.09 ± 7.29, which was close to the midpoint 26.00. In the literature, studies conducted with healthcare professionals who work in intensive care units, and emergency services report that nurses experience excessive mental stress and fear of getting infected with COVID-19.34 , 35 In Turkey, Saracoglu et al36 conducted a study to investigate the risk of mental disorders among healthcare professionals and reported that intensive care unit nurses were at the highest risk for having anxiety, fear, and depression during COVID-19 pandemic. In their qualitative study Kackin et al37 examined the psychosocial problems of nurses who cared for patients diagnosed with COVID-19 and found that nurses were adversely affected by the pandemic process with feeling fear and showing depressive symptoms. Aksoy and Koçak38 stated that the most intense feeling due to COVID-19 among nurses who work in healthcare services was the feeling of fear. In Thailand, a study conducted by Apisarnthanarak et al,39 that evaluated the emotions of healthcare professionals for pandemic reported that 90% of them were fearful of COVID-19. Relevant literature also indicates that increased fear may cause increased anxiety and nurses who care for COVID-19 patients carry the risk of having mental problems even after the pandemic.30 , 40 , 41 After nearly seven months of pandemic process, nurses in the present study specify that they were still afraid of coronavirus and thinking about COVID-19 was making them uncomfortable. Based on the results, the fear of COVID-19 among nurses is not surprising but it is noticeable that the fear is still ongoing with a moderate level.
In this study, nurses who received training related to COVID-19 including the disease, its transmission, and prevention methods, using the personal protective equipment, care of suspected or infected patients had lower fear score than those who did not. With the first cases started around Turkey and in the city, the hospital directory and hospital education unit arranged in-service trainings according to the guidelines determined by the Science Board of Health Ministry of Turkey. The training topics included COVID-19 case definitions, classifications and treatments, considerations in approaching the patient, protective equipment, swabbing etc. On the other hand, nurses reported that they attended several seminars, online webinars, live steams of some universities, associations (including website of Republic of Turkey Ministry of Health, Turkish Nurses Association, Turkish Surgery and Operating Nurses Association, Koc University, Bartın University, Gumushane University etc.) in internet and on social media platforms such as YouTube and Instagram. The seminar and activity topics included the responsibilities of nurses during COVID-19 pandemic and up-to-date information about coronavirus. As COVID-19 is a novel infectious disease and is still not taken under control, applying trainings for healthcare professionals including the latest knowledge (such as using personal protective equipment, safety precautions, hygiene practices, infection control and intensive care of patients) are very important to protect and support them.42 , 43 In their study, Cui et al44 from China investigated the psychological impacts of COVID-19 in nurses and reported that attending infection prevention training improves nurses’ stress coping skills and effectively reduces their stress level. Similarly, a cross-sectional and descriptive study conducted with 261 frontline nurses working in five hospitals in the Philippines that examined the influence of COVID-19 fear on nurses reports that nurses who had not attended any training related to COVID-19 had a higher level of fear than those who attended. Alwani et al12 examined the knowledge and anxiety levels of nurses towards COVID-19 in Pakistan and found that training was important to increase nurses’ awareness and knowledge. The results showed that, informing nurses about subjects related to COVID-19 is effective in decreasing their level of fear.
In the present study, nurses who lost a patient because of COVID-19 showed higher level of fear than who did not. As because nurses witness their patients dying due to COVID-19, this may impact their emotional status with leading to fear.45 , 46 In a qualitative study that analyzes the experiences of nurses who care for COVID-19 patients, some nurses expressed that they had the fear of losing their family members and were distressed for the different dead body sealing method, thus, felt fear that the same could happen to themselves or to their family members.37 In their commentary, Nelson and Lee-Win reported that nurses who take care of COVID-19 patients feel a great sense of empathy for their patients.47 Nurses also see traumatic deaths, lost their young and/or old patients due to COVID-19 and feel fear to end up as one of these patients.48 The qualitative study conducted by Galehdar et al48 in China using nurses taking care of COVID-19 patients reported that the death of these patients was more painful than the other patients and their death, especially the young ones’, was traumatizing for them. The nurses expressed that it was very sad to see a patient suffering from taking a breath and they were feeling helpless and sad in front of a dying patient because of COVID-19. According to a review about the mental health issues of healthcare workers during the pandemic, nurses were stressed because of their patient's death.49 An article conducted during the pandemic reported that missed patient surveillance and burnout levels of medical-surgical nurses were higher than the nurses working in intensive care units.50 In accordance with these results, surgical nurses experience even greater levels of COVID-19 fear when facing patients die.
The present study found a positive relationship between the mean total fear scores of nurses and their age and duration of nursing experience. Similarly, a cross-sectional study by Li et al51 in Wuhan investigated the anxiety and related factors of frontline clinical nurses; the study found that age was associated with anxiety and that the nurses over 35 age had higher levels of anxiety than the younger nurses. Similarly, studies in the literature states that there is a relation between the fear level of COVID-19 of the civil population and their age; that older adult population has higher fear than youngers.52, 53, 54 In their cross-sectional and descriptive study, Taghaddom et al55 from Kuwait investigated the impact of the pandemic on nurses working in COVID-19 units and reported that although nurses’ psychological responses were better with their age and duration of nursing experiences, some of them were crying at work and experiencing fear. According to the results, it is understandable that older nurses are more fearful when caring for COVID-19 patients, given that COVID-19 infection mortality rises with patient age. Furthermore, the fact that more experienced nurses showed higher levels of fear can be attributed to their age, which is accompanied by more years of experience. Additionally, as nurses’ age and years of experience increase, their emotional response becomes worse, that could be a result of increased risk of being infected or dying due to COVID-19.
Strengths and Limitations
Although there are many studies that search the psychological effects of pandemic on nurses around the world, the important contribution of the study was that it was conducted with nurses specialized in surgical nursing. Based on the study results, it is thought that the results of this study will contribute to literature on the COVID-19 fear level of surgical nurses during the pandemic and to draw attention on this issue.
In this study, there are some limitations that should be considered. First, the data was limited with to the surgical nurses of one training and research hospital in Turkey. Thus, it limits the generalization of the results to all nurses. Second, the fear measurements are limited with the scale tool and the detailed reasons of the fear of COVID-19 are not evaluated in this study. Third, most of the nurses were working at the night shift and this limited generalizing the results to nurses who do not work the night shift. Therefore, the results about nurses’ COVID-19 fear are limited with the scale items and some descriptive characteristics of the nurses. Fourth, this study did not compare the fear levels of nurses before and after training related to COVID-19 as they started to receive the trainings with the first COVID-19 cases appeared. Fifth, this study did not discuss the positive effects of fear and anxiety of nurses (such as compliance with protective measures, hand washing etc.). In addition, we recommend for the future studies to examine factors that influence the pandemic fear of nurses with larger sample sizes, to search the effects of training programs on fear levels of nurses and search for the positive effects of COVID-19 fear on nurses.
Conclusion
The study showed that surgical nurses who take care of suspected or infected COVID-19 patients in pandemic and surgical units had a moderate level of COVID-19 fear. In addition, nurses who lost a patient because of COVID-19, are older and experienced in nursing had high levels of fear, and receiving training related to COVID-19 lowered their fear. Firstly, due to re-assignment of surgical nurses to COVID-19 pandemic units, we recommend conducting appropriate on-line training programs including the latest information related to COVID-19 to maintain the appropriate adaptation of the nurses. Secondly, to ensure psychological well-being of the surgical nurses, we recommended evaluating the psychological impact levels of nurses and developing psychological support strategies in decreasing their fear.
Acknowledgment
We thank to the nurses who participated in this study and saved their time.
Footnotes
Conflict of interest: None to report.
Funding: None to report.
References
- 1.Shereen MA, Khan S, Kazmi A, Bashir N, Siddique R. COVID-19 infection: origin, transmission, and characteristics of human coronaviruses. J Adv Res. 2020;24:91–98. doi: 10.1016/j.jare.2020.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rothan HA, Byrareddy SN. The epidemiology and pathogenesis of coronavirus disease (COVID-19) outbreak. J Autoimmun. 2020;109 doi: 10.1016/j.jaut.2020.102433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Timeline of WHO's response to COVID-19. Available at:https://www.who.int/emergencies/diseases/novel-coronavirus-2019/interactive-timeline#event-26. Accessed November 12, 2020.
- 4.WHO announces COVID-19 outbreak a pandemic. Available at:https://www.euro.who.int/en/health-topics/health-emergencies/coronavirus-covid-19/news/news/2020/3/who-announces-covid-19-outbreak-a-pandemic. Accessed November 12, 2020.
- 5.Coronavirus disease (COVID-19). Available at: https://www.who.int/emergencies/diseases/novel-coronavirus-2019. Accessed November 13, 2020.
- 6.Republic of Turkey Ministry. COVID-19 information page. Available at: https://covid19.saglik.gov.tr/?_Dil=2. Accessed April 3, 2021.
- 7.Shigemura J, Ursano RJ, Morganstein JC, Kurosawa M, Benedek DM. Public responses to the novel 2019 coronavirus (2019-nCoV) in Japan: mental health consequences and target populations. Psychiatry Clin Neurosci. 2020;74:281–282. doi: 10.1111/pcn.12988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bao Y, Sun Y, Meng S, Shi J, Lu L. 2019-nCoV epidemic: address mental health care to empower society. Lancet. 2020;395:e37–e38. doi: 10.1016/S0140-6736(20)30309-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Harper CA, Satchell LP, Fido D, Latzman RD. Functional fear predicts public health compliance in the COVID-19 pandemic. Int J Ment Health Addict. 2020:1–14. doi: 10.1007/s11469-020-00281-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Brooks SK, Webster RK, Smith LE, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395:912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shanafelt T, Ripp J, Trockel M. Understanding and addressing sources of anxiety among health care professionals during the COVID-19 pandemic. JAMA. 2020;323:2133–2134. doi: 10.1001/jama.2020.5893. [DOI] [PubMed] [Google Scholar]
- 12.Alwani SS, Majeed MM, Hirwani MZ, et al. Evaluation of knowledge, practices, attitude and anxiety of Pakistans nurses towards COVID-19 during the current outbreak in Pakistan. medRxiv. 2020:1–26. doi: 10.1101/2020.06.05.20123703. [DOI] [Google Scholar]
- 13.Saleem Z, Majeed MM, Rafique S, Siddiqui Z., Ghandhi D, Tariq H. COVID-19 pandemic fear and anxiety among healthcare professionals in Pakistan. Res Square. 2020:1–17. doi: 10.21203/rs.3.rs-37608/v2. [DOI] [Google Scholar]
- 14.Lai J, Ma S, Wang Y, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open. 2020;3 doi: 10.1001/jamanetworkopen.2020.3976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rymarowicz J, Stefura T, Major P, et al. General surgeons’ attitudes towards COVID-19: a national survey during the SARS-CoV-2 virus outbreak. Eur Surg. 2020:1–6. doi: 10.1007/s10353-020-00649-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Doussot A, Heyd B, Lakkis Z. We asked the experts: how do we maintain surgical quality standards for enhanced recovery programs after cancer surgery during the COVID-19 outbreak? World J Surg. 2020;44:2051–2052. doi: 10.1007/s00268-020-05546-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hwang ES, Balch CM, Balch GC, et al. Surgical oncologists and the COVID-19 pandemic: guiding cancer patients effectively through turbulence and change. Ann Surg Oncol. 2020;27:2600–2613. doi: 10.1245/s10434-020-08673-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Søreide K, Hallet J, Matthews JB, et al. Immediate and long-term impact of the COVID-19 pandemic on delivery of surgical services. Br J Surg. 2020;107:1250–1261. doi: 10.1002/bjs.11670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Stahel PF. How to risk-stratify elective surgery during the COVID-19 pandemic? Patient Saf Surg. 2020;14:8. doi: 10.1186/s13037-020-00235-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.COVID-19. Available at: http://www.salute.gov.it/imgs/C_17_notizie_4515_0_file.pdf. Accessed November 12, 2020.
- 21.Jayadevan R. A hundred lives lost: doctor deaths in India during the times of COVID-19. Preprints. 2020:1–10. doi: 10.20944/preprints202007.0346.v1. [DOI] [Google Scholar]
- 22.Ing EB, Xu QA, Salimi A, Torun N. Physician deaths from corona virus (COVID-19) disease. Occup Med (Lond) 2020;70:370–374. doi: 10.1093/occmed/kqaa088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Anand S, Staniec A, Montez-Rath M, Vlahos P. Using GIS mapping to track hot spots of kidney disease in California. N Engl J Med. 2020;382:2265–2267. doi: 10.1056/nejmc2001023. [DOI] [PubMed] [Google Scholar]
- 24.Kursumovic E, Lennane S, Cook TM. Deaths in healthcare workers due to COVID-19: the need for robust data and analysis. Anaesthesia. 2020;75:989–992. doi: 10.1111/anae.15116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Taylor S, Landry CA, Rachor GS, Paluszek MM, Asmundson GJG. Fear and avoidance of healthcare workers: an important, under-recognized form of stigmatization during the COVID-19 pandemic. J Anxiety Disord. 2020;75 doi: 10.1016/j.janxdis.2020.102289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ahorsu DK, Lin CY, Imani V, Saffari M, Griffiths MD, Pakpour AH. The fear of COVID-19 scale: development and initial validation. Int J Ment Health Addict. 2020:1–9. doi: 10.1007/s11469-020-00270-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wu Y, Wang J, Luo C, et al. A comparison of burnout frequency among oncology physicians and nurses working on the frontline and usual wards during the COVID-19 epidemic in Wuhan, China. J Pain Symptom Manage. 2020;60:e60–e65. doi: 10.1016/j.jpainsymman.2020.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sample size calculator. Available at: https://www.calculator.net/sample-size-calculator.html?type=1&cl=99.99&ci=5&pp=50&ps=216&x=78&y=14. Accessed September 1, 2020.
- 29.Mertens G, Gerritsen L, Duijndam S, Salemink E, Engelhard I. Fear of the coronavirus (COVID-19): predictors in an online study conducted in March 2020. J Anxiety Disord. 2020;74:10228. doi: 10.31234/OSF.IO/2P57J. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Satici B, Gocet-Tekin E, Deniz ME, Satici SA. Adaptation of the fear of COVID-19 scale: its association with psychological distress and life satisfaction in Turkey. Int J Ment Health Addict. 2020:1–9. doi: 10.1007/s11469-020-00294-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Khattak SR, Saeed I, Rehman SU, Fayaz M. Impact of fear of COVID-19 pandemic on the mental health of nurses in Pakistan. J Loss Trauma. In press (2020). https://doi.org/10.1080/15325024.2020.1814580
- 32.Labrague LJ, de los Santos J. Fear of COVID-19, psychological distress, work satisfaction and turnover intention among frontline nurses. J Nurs Manag. 2020 doi: 10.1111/jonm.13168. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lancaster EM, Sosa JA, Sammann A, et al. Rapid response of an academic surgical department to the COVID-19 pandemic: implications for patients, surgeons, and the community. J Am Coll Surg. 2020;230:1064–1073. doi: 10.1016/j.jamcollsurg.2020.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ho CS, Chee CY, Ho RC. Mental health strategies to combat the psychological impact of COVID-19 beyond paranoia and panic. Ann Acad Med Singap. 2020;49:155–160. [PubMed] [Google Scholar]
- 35.Khan KS, Mamun MA, Griffiths MD, Ullah I. The mental health impact of the COVID-19 pandemic across different cohorts. Int J Ment Health Addict. 2020:1–7. doi: 10.1007/s11469-020-00367-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Saracoglu KT, Simsek T, Karaman S, et al. The psychological impact of COVID-19 disease is more severe on intensive care unit healthcare providers: a cross-sectional study. Clin Psychopharmacol Neurosci. 2020;18:607–615. doi: 10.9758/cpn.2020.18.4.607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kackin O, Ciydem E, Aci OS, Kutlu FY. Experiences and psychosocial problems of nurses caring for patients diagnosed with COVID-19 in Turkey: a qualitative study. Int J Soc Psychiatry. 2020:1–10. doi: 10.1177/0020764020942788. [DOI] [PubMed] [Google Scholar]
- 38.Aksoy YE, Koçak V. Psychological effects of nurses and midwives due to COVID-19 outbreak: the case of Turkey. Arch Psychiatr Nurs. 2020;34:427–433. doi: 10.1016/j.apnu.2020.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Apisarnthanarak A, Apisarnthanarak P, Siripraparat C, Saengaram P, Leeprechanon N, Weber DJ. Impact of anxiety and fear for COVID-19 toward infection control practices among Thai healthcare workers. Infect Control Hosp Epidemiol. 2020;41:1–6. doi: 10.1017/ice.2020.280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mental health & COVID-19. Available at: https://www.who.int/teams/mental-health-and-substance-use/covid-19. Accessed November 18, 2020.
- 41.Xiang YT, Yang Y, Li W, et al. Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet Psychiatry. 2020;7:228–229. doi: 10.1016/S2215-0366(20)30046-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Aldohyan M, Al-Rawashdeh N, Sakr FM, Rahman S, Alfarhan AI, Salam M. The perceived effectiveness of MERS-CoV educational programs and knowledge transfer among primary healthcare workers: a cross-sectional survey. BMC Infect Dis. 2019;19:273. doi: 10.1186/s12879-019-3898-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Chen SC, Lai YH, Tsay SL. Nursing perspectives on the impacts of COVID-19. J Nurs Res. 2020;28:e85. doi: 10.1097/NRJ.0000000000000389. [DOI] [PubMed] [Google Scholar]
- 44.Cui S, Jiang Y, Shi Q, et al. Impact of COVID-19 on psychology of nurses working in the emergency and fever outpatient: a cross-sectional survey. Res Square. 2020:1–19. https://assets.researchsquare.com/files/rs-20777/v1/89643bc2-4734-445b-ba61-0165595e5ae8.pdf. Accessed November 13, 2020. [Google Scholar]
- 45.Alharbi J, Jackson D, Usher K. The potential for COVID-19 to contribute to compassion fatigue in critical care nurses. J Clin Nurs. 2020;29:2762–2764. doi: 10.1111/jocn.15314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Pappa S, Ntella V, Giannakas T, Giannakoulis VG, Papoutsi E, Katsaounou P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Brain Behav Immun. 2020;88:901–907. doi: 10.1016/j.bbi.2020.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Nelson SM, Lee-Winn AE. The mental turmoil of hospital nurses in the COVID-19 pandemic. Psychol Trauma. 2020;12:126–127. doi: 10.1037/tra0000810. [DOI] [PubMed] [Google Scholar]
- 48.Galehdar N, Kamran A, Toulabi T, Heydari H. Exploring nurses’ experiences of psychological distress during care of patients with COVID-19: a qualitative study. BMC Psychiatry. 2020;20:489. doi: 10.1186/s12888-020-02898-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Spoorthy MS, Pratapa SK, Mahant S. Mental health problems faced by healthcare workers due to the COVID-19 pandemic—a review. Asian J Psychiatr. 2020;51 doi: 10.1016/j.ajp.2020.102119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Lasater KB, Aiken LH, Sloane DM, et al. Chronic hospital nurse understaffing meets COVID-19: an observational study. BMJ Qual Saf. 2020 doi: 10.1136/bmjqs-2020-011512. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Li R, Chen Y, Lv J, et al. Anxiety and related factors in frontline clinical nurses fighting COVID-19 in Wuhan. Medicine (Baltimore) 2020;99:e21413. doi: 10.1097/MD.0000000000021413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Andrade EF, Pereira LJ, Oliveira APL, de, et al. Perceived fear of COVID-19 infection according to sex, age and occupational risk using the Brazilian version of the fear of COVID-19 scale. Death Stud. 2020:1–10. doi: 10.1080/07481187.2020.1809786. [DOI] [PubMed] [Google Scholar]
- 53.de Leo D, Trabucchi M. COVID-19 and the fears of Italian senior citizens. Int J Environ Res Public Health. 2020;17:3572. doi: 10.3390/ijerph17103572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Qiu J, Shen B, Zhao M, Wang Z, Xie B, Xu Y. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: implications and policy recommendations. Gen Psychiatr. 2020;33 doi: 10.1136/gpsych-2020-100213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Taghaddom SM, Alrashidi HM, Mohamed HD, Johnson MN. The impact of coronavirus on staff nurses’ feeling while giving direct care to COVID-19 patients in various COVID facilities. Open J Nurs. 2020;10:873–889. doi: 10.4236/ojn.2020.109060. [DOI] [Google Scholar]