Abstract
Introduction
There is a paucity of data in scientific literature on the impact of Coronavirus Disease 2019 (COVID-19) pandemic on bariatric surgery. The aim of this study was to evaluate the impact of COVID-19 pandemic on Bariatric Surgery globally.
Methods
We conducted a global online survey of bariatric surgeons between 16/04/20 – 15/05/20. The survey was endorsed by five national bariatric surgery societies and circulated amongst their memberships. Authors also shared the link through their personal networks, email groups, and social media.
Results
703 respondents from 77 countries completed the survey. Respondents reported a drop in elective bariatric activity from a median (IQR) of 130 (60–250) procedures in 2019 to a median of 0 (0–2) between16/03/2020 and 15/04/2020 during the pandemic. The corresponding figures for emergency activity were 5 (2–10) and 0 (0–1) respectively. 441 (63%) respondents did not perform any bariatric procedures during this time period. Surgeons reported outcomes of 61 elective bariatric surgical procedures during the pandemic with 13 (21%) needing ventilation and 2 (3.3%) deaths. Of the 13 emergency bariatric procedures reported, 5 (38%) needed ventilation and 4 (31%) died. 90 (13%) surgeons reported having had to perform a bariatric surgical or endoscopic procedure without adequate Personal Protective Equipment.
Conclusions
COVID-19 pandemic led to a remarkable decline in global elective and emergency bariatric surgery activity at its beginning. Both elective and emergency procedures performed at this stage of the pandemic had considerable morbidity and mortality.
Keywords: Bariatric surgery, COVID-19, SARS CoV-2, Pandemic, Personal protective equipment, Survey, PPE
Introduction
The Coronavirus Disease 2019 (COVID-19) pandemic has had a significant impact on healthcare practices and delivery around the world. It is estimated that millions of elective and semi-urgent surgical procedures have either been cancelled or postponed [1] during the pandemic. Though there is little data on this, one suspects an anticipated higher risk associated with surgical procedures during the pandemic as well as a scarcity of precious hospital and critical care resources were some of the factors behind this.
The International Federation for the Surgery of Obesity and Metabolic Disorders (IFSO) issued guidelines on the 14th April 2020 and advised postponing all elective surgical and endoscopic bariatric and metabolic procedures during the pandemic [2]. But the pandemic was rife in many parts of the world in the month leading up to this date. There is a lack of data on the effect of the pandemic on global bariatric surgical activity prior to IFSO guidance, along with the morbidity and mortality of procedures that might have been carried out during this period.
As the pandemic situation improves in many parts of the world, healthcare systems are trying to understand what safeguards would be needed to deliver safe bariatric surgery. However, there is little data on what surgeons might feel are relevant safeguards. These factors can potentially make resuming bariatric surgery very difficult in many parts of the world. The problem might be further compounded by deep-rooted societal stigma against obesity [3], and low surgical priority accorded to bariatric surgery by many healthcare planners [4].
The aim of this study was to assess the effect of COVID-19 pandemic on global bariatric surgery practices at the beginning of the COVID-19 pandemic, and the views of the surgeons regarding future directions post- COVID-19 pandemic. We also used the opportunity to assess the availability of PPE for bariatric surgeons during the COVID-19 pandemic.
Material and methods
We created a multinational committee of bariatric surgery professionals from 8 countries (4 continents) to oversee this study to evaluate the effects of COVID-19 pandemic on Global Bariatric Surgery PRActiceS (The COBRAS Study). The study was endorsed by five national bariatric surgery societies (British Obesity and Metabolic Surgery Society, The Israeli Society for Metabolic and Bariatric Surgery, Norwegian Society for the Surgery of Obesity, Obesity Surgery Society of India, and Società Italiana di Chirurgia dell’Obesità e delle malattie metaboliche).
The study committee designed a 41-item questionnaire-based survey (https://www.getfeedback.com) following the principles of good practice in the conduct and reporting of survey research as recommended by the EQUATOR network guidelines [5]. The survey link was widely shared with bariatric surgeons using personal and professional networks, email groups of professionals, and social media (Facebook™, Researchgate™, Twitter™, Whatsapp™, and Linkedn™).
The survey went live on 16/04/2020 and was closed for analysis on 15/05/2020. Full details of the questionnaire have been provided in the Appendix. Only consultant bariatric surgeons who were in practice for at least 12 months at the time of the survey were included in the analysis.
Data have been presented as numbers (percentage) and median (IQR). Data were visualized by mapping onto a cylindrical equidistant projection of the world map using in house python software (python 3.7.7) based on Matplotlib (version 3.1.2) and Basemap (version 1.2.1). To locate each country on the map, the natural earth admin 0 countries file without boundary lakes was used, available at https://www.naturalearthdata.com/http//www.naturalearthdata.com/download/50m/cultural/ne_50m_admin_0_countries_lakes.zip. After rendering individual high-resolution maps within the Matplotlib/Python environment, graphs were finalized using EazyDraw, version 9.
Results
A total of 770 bariatric surgeons completed the survey. Of these, 67 respondents were excluded as they were either not a consultant bariatric surgeon or not in practice for at least 12 months at the time of taking the survey. A total of 703 responses were included for analysis.
Nationality and experience of the respondents
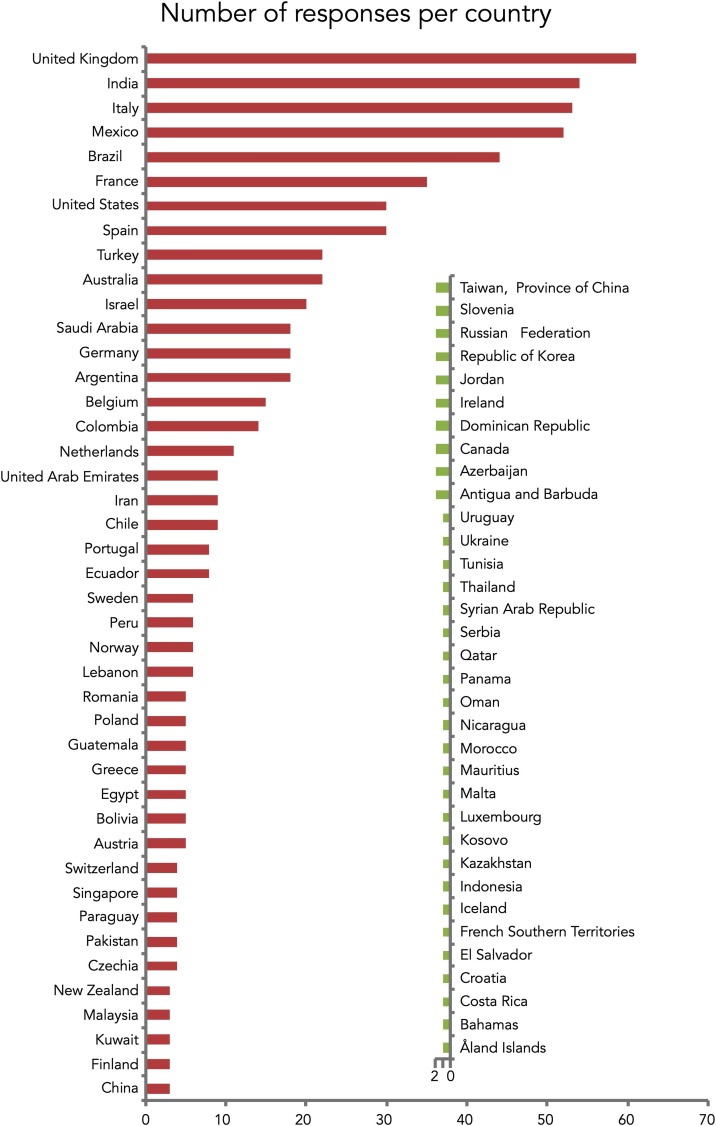
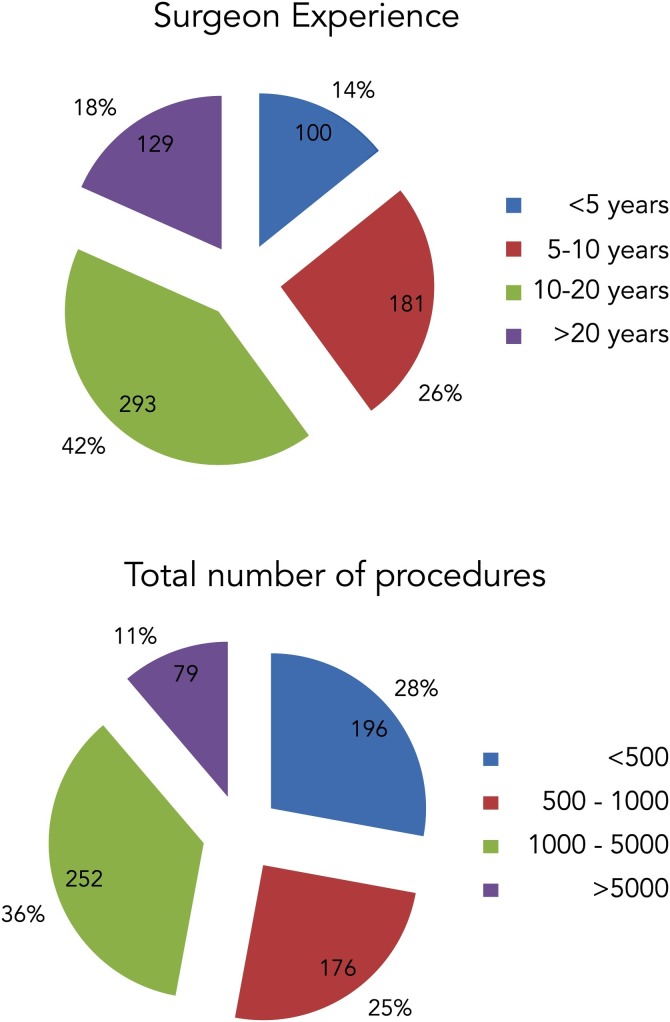
The 703 respondents included represented a total of 77 countries. The highest response was from the United Kingdom (61), closely followed by India (54), Italy (53), and Mexico (52). Fig. 1 provides a full list of countries and the number of respondents by country. Fig. 2 provides a summary of the respondents’ experience. More than half of the respondents were practising for more than 10 years and had performed more than 500 bariatric procedures
Fig. 1.
Number of respondents per country.
Fig. 2.
Surgical experience of respondents.
Impact of COVID-19 pandemic on elective and emergency bariatric activity
This is summarised in Table 1 . Respondents reported a median (IQR) elective bariatric yearly procedure volume during 2019 of 130 (60–250). The median volume of bariatric emergencies during 2019 was 5 cases (2–10). The median number of elective procedures performed during the time period from 16th March 2020 to 15th April 2020 was 0 (0–2). 441 (62.8%) of the respondents did not perform any bariatric procedures during this time period. The median volume of emergency cases during this pandemic period was 0 (0–1).
Table 1.
Surgeons responses to their practice in the COVID era.
| Numbers practicing | Decrease in practice | >50% decrease | 100% decrease | No change | Increase | Don’t Know | |
|---|---|---|---|---|---|---|---|
| Bariatric surgery | 703 (100%) | 661 (94%) | 626 (89%) | 436 (62%) | 4 (0.5%) | 20 (3%) | 0 (0%) |
| Bariatric endoscopic procedures | 363 (52%) | 317 (45%) | 290 (41%) | 207 (29%) | 13 (1.8%) | 8 (1%) | 25 (4%) |
| Swallowable balloon procedures | 97 (14%) | 90 (13%) | 81 (12%) | 63 (9%) | 6 (1%) | 0 (0%) | 0 (0%) |
COVID-19 infection after elective and emergency bariatric surgical or endoscopic procedure
A total of 33 (5%) surgeons reported at least one patient who developed COVID-19 after an elective bariatric procedure. The total number of such patients was 61. Of these 61 patients, 13 (21.3%) patients required mechanical ventilation, and 2 (3.27%) of these patients died as a result of COVID-19 infection.
12 (2%) surgeons reported at least one patient who developed COVID-19 after an emergency bariatric procedure. The total number of such patients was 13. Of these 5 (38%) patients required mechanical ventilation and 4 (31%) patients had a fatal outcome.
Restarting bariatric/endoscopic practice
308 (44%) respondents believed that if this pandemic was to continue for 6 months or longer, it will lead to surgeons deskilling. Web-based video sessions, dual consultant operating, triaging on the basis of co-morbidities (with lower acuity patients taking priority), and use of laparoscopic trainers were some of the qualitative suggestions by surgeons to mitigate this risk. However, 233 (33%) respondents did not think that deskilling would be an issue, and 160 (23%) weren’t sure.
When asked regarding safeguards prior to resuming bariatric surgery, 501 (72%) respondents stated that the patient should be aware of higher risks. With regards to viral carriage/immunity, 321 (46%) respondents stated that patients should be antigen-negative, 143 (20%) stated that patients should be antibody positive, and 54 (8%) respondents stated all theatre personnel should be antibody positive. A total of 263 (38%) respondents felt that there should be a dedicated site for elective bariatric operations where COVID - 19 patients are not treated. 141 (20%) respondents reported that they would not start bariatric elective work until the pandemic subsided completely.
With regards to endoscopic practice, 481 (69%) respondents believed that bariatric endoscopic procedures should only be performed with full PPE guidance. A total of 314 (45%) respondents felt that patients should be tested for viral carriage/immunity prior to endoscopy.
Impact of COVID 19 pandemic on obesity pandemic
472 (67%) respondents believed that the obesity prevalence would worsen as a result of the current COVID-19 pandemic. The respondents stated that the impact of obesity prevalence will be driven by increased food intake, worsening food quality, and reduction in physical activity.
Long term impact of COVID-19 pandemic on bariatric surgical and endoscopic procedures
When asked regarding the long-term impact of COVID-19 pandemic on the number of bariatric surgical procedures, 242 (34%) respondents felt that the numbers would increase, 248 (35%) stated that the numbers would decrease, and the remaining respondents either expected no change (121; 17%) or weren’t sure (91; 13%).
When asked regarding bariatric endoscopic procedures, 183 (26%) respondents expected the numbers to increase in the long-term, and 180 (26%) expected a decrease. A total of 136 (19%) respondents did not expect any change and a further 203 (29%) respondents were not sure.
Awareness of WHO guidelines/ Availability of PPE for surgery and endoscopy
Only 508 (72%) respondents were fully aware of the guidelines with regards to PPE usage. 157 (22%) respondents were aware but not fully clear and further 37 respondents (5%) were not aware at all.
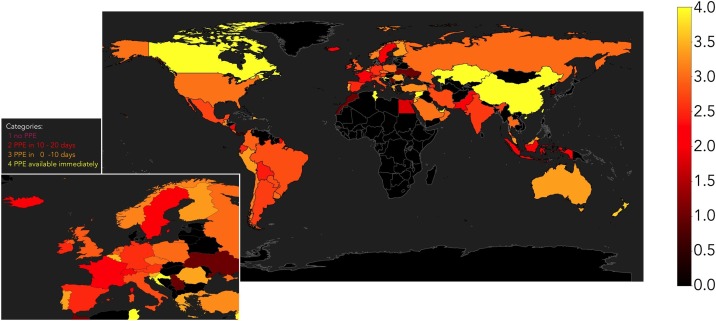
PPE equipment was available when needed to 243 (35%) respondents. There was a time lag to availability of up to 10 days for 206 (29%) respondents and 10–20 days for 134 (19%) respondents. A total of 119 (17%) respondents did not have all adequate PPE equipment available even at the time of answering the survey.
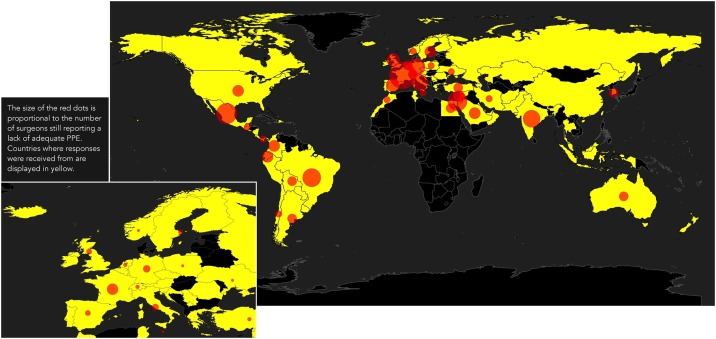
Remarkably, 90 (13%) respondents reported having had to perform a bariatric surgical or endoscopic procedure without adequate PPE equipment. Global variations in the availability of PPE are depicted in Fig. 3, Fig. 4 .
Fig. 3.
Global availability of PPE.
Fig. 4.
Centers/ surgeons still reporting a lack of adequate PPE.
Discussion
There is a lack of published data on COVID-19 and bariatric surgery [6]. This is the first global survey of bariatric surgeons assessing the impact of the COVID-19 pandemic on the provision of current bariatric surgical services and assessing future directions for the post-pandemic era. The survey found that the COVID-19 pandemic resulted in a significant reduction in the volume of surgical and endoscopic, elective and emergency bariatric procedures globally even before the publication of IFSO guidance [3], which advised surgeons to postpone all elective surgical and endoscopic bariatric/metabolic procedures during the pandemic.
The survey also showed a large variation in the bariatric surgeons’ views on when bariatric surgery could re-start, and tried to understand their thoughts on safeguards that would allow them to resume bariatric surgery safely during this pandemic. Significantly, a fifth of the surgeons were unwilling to start bariatric surgery again till the COVID-19 pandemic subsided completely. The survey suggests that delays in re-starting bariatric surgery might result in de-skilling of surgeons. The survey also showed that PPE was not available immediately at the start of the COVID-19 pandemic for the majority of the surgeons.
This study provides data on outcomes of elective and emergency bariatric procedures performed during the early part of the pandemic. Aminian et al. reported on outcomes of four patients who developed COVID-19 after bariatric surgery in Iran at the beginning of the pandemic [7]. Though two (50%) of these patients needed critical care, none needed ventilation and there was no mortality in this series. Our survey reports on a further 61 elective procedures and 13 emergency patients who underwent bariatric procedures and their subsequent outcomes from different parts of the world. The GENEVA collaborators have since published outcomes from their multi-centre international cohort study [8]. The authors of this study concluded that the 30-day morbidity and mortality following bariatric surgery during the COVID-19 pandemic with locally appropriate perioperative COVID-19 protocols was similar to pre-pandemic levels.
In this study, 21.3% patients undergoing elective bariatric surgery required mechanical ventilation, and 3.27% of these patients died as a result of COVID-19 infection. For the emergency cohort, 38% patients required mechanical ventilation and 31% patients had a fatal outcome. These outcomes are not too dissimilar to the study by the COVIDSurg collaborators [9] which reported an overall 30-day mortality of 23·8% (268 of 1128) and a 30-day mortality of 38·0% (219 of 577) in patients with pulmonary complications (75% patients in this study underwent emergency surgery).
It was interesting to note that the respondents reported performing a median of 0 procedures for the study period of one month (16th March 2020 to 15th April 2020) as opposed to a median yearly volume of 130 elective bariatric cases for 2019. This study period also predates the IFSO guidance [2] and the study by COVIDSurg collaborators which was the first to identify on a global scale that postoperative pulmonary complications occurred in half of patients with perioperative SARS-CoV-2 infection and were associated with high mortality [9]. This was probably due to heightened awareness amongst the bariatric community of poor outcomes associated with perioperative SARS-CoV-2 infection [10], especially in patients living with obesity and its co-morbidities [11]. Recommendations from esteemed surgical bodies may also have played a role [12].
This survey of 703 surgeons from 77 countries is one of the largest surveys of the bariatric surgeons in the world. This probably represents most countries in the world where bariatric surgery is performed given that there are only 66 national societies affiliated to IFSO [13]. Somewhat worryingly, this survey found that the COVID-19 pandemic not only resulted in a significant reduction in the volume of global elective surgical and endoscopic bariatric procedures but also a dramatic reduction in the number of bariatric emergencies performed worldwide. This reduction in emergency bariatric activity may have unforeseen adverse consequences. A possible explanation for the reduction could be reluctance amongst patients to seek healthcare for the fear of acquiring SARS-CoV-2. It is further possible that genuine bariatric emergencies were confused with gastrointestinal symptoms of COVID-19 [14].
The survey also found that the majority of the respondents expected a change in the volume of bariatric surgery in the post-COVID-19 era, but there was uncertainty amongst the bariatric surgeons regarding the direction of change, with similar proportions expecting an increase or a decrease. It was surprising to note that 26% of the respondents felt that numbers of endoscopic procedures would increase even though endoscopy is probably more aerosol-generating than surgery. A fifth of the surgeons indicated that were unwilling to start bariatric surgery again till the COVID-19 pandemic subsided completely. Of these an equal proportion of surgeons worked in the private sector only (52/141; 36.8%) or a combination of public and private sectors (60/141; 42.6%). Only a minority (28/141; 19.9%) worked exclusively in a publicly funded service. This might be a reflection of limited critical care resources in the private sector.
Most respondents in the survey felt that obesity prevalence will increase as a result of the COVID pandemic with social distancing restrictions affecting the ability to leave one’s residence, increased intake of calorie-dense food and reduction in physical activity as reasons for this postulated increase in obesity. The time it takes to restart bariatric procedures was important considering 44% of the surgeons felt there was a risk of deskilling, despite the majority of our survey respondents being experienced bariatric surgeons. Given that Type 2 diabetes, hypertension and obesity are predictors for severe COVID-19 infections [11] and that bariatric surgery is the most effective treatment resulting in sustained weight loss and large improvements in hypertension and Type 2 diabetes [15]; this global drop in the bariatric activity is particularly concerning and requires addressing.
An important finding of this survey was the global disparity in the availability of PPE. Countries such as Belgium (15 responses), United Arab Emirates (9 responses), China, and Canada had PPE available almost immediately. On the other hand, Serbia, Kosovo, Ukraine, Panama, Malta, Morocco, and Serbia were seen on the other side of the spectrum with a lack of adequate PPE at the time of completing the questionnaire. In addition, 90 surgeons reported performing surgery without PPE. This was compounded by a lack of understanding of the WHO guidelines for PPE usage with only 72% of the respondents being fully aware of the guidelines with regards to PPE usage.
There are some limitations to this study. Firstly, we have only captured data for one month during the pandemic. It is possible that outcomes in the subsequent months were better or worse. Secondly, owing to the snowball sampling methods used for the survey, it is difficult to provide an accurate response rate but 703 surgeons from 77 countries would probably constitute a representative sample for a relatively niche specialty such as bariatric surgery. Some of the larger countries where majority of the global bariatric surgery is performed are under-represented in this survey. Our findings cannot, therefore, be extrapolated to those regions. Additionally, responses to a survey may be affected by recall bias. To minimise that we used a relatively short period of 30-days immediately preceding the launch of the survey. Another limitation of this survey is that data on timing of SARS-CoV-2 infection with respect to surgery, modality for testing and possible source of infection (inpatient vs community transmission) were not captured.
This survey provides many useful pieces of information. It is the first study to attempt large-scale data collection on bariatric surgery at the beginning of the COVID-19 pandemic. It is also the second-largest survey ever of bariatric surgeons, the largest being a survey on practices concerning Sleeve Gastrectomy [16]. This is significant as we only included surgeons who were consultants or attending surgeons and had been practicing for at least a year. It is further remarkable because many surgeons many not have had easy access to their professional email accounts, or Internet during this period when many countries were in lockdown and some surgeons may have been self-isolating/quarantining.
This is the first comprehensive study documenting the effect of COVID-19 pandemic on global bariatric practices at the beginning of the pandemic [6]. We report on outcomes of 61 elective and 13 emergency bariatric procedures during the pandemic period with remarkably higher critical care need and mortality than would otherwise be expected for this group of patients. This study also attempts at finding out the safeguards bariatric surgeons believe might allow for a safe resumption of bariatric surgery during the pandemic.
In conclusion, there was a dramatic decline in bariatric surgical activity worldwide at the beginning of the COVID-19 pandemic. Although the decline in elective practice was expected, the drop in emergency bariatric volume is rather worrying. Both elective and emergency bariatric procedures performed at the beginning of the pandemic were associated with a high need for critical care and mortality.
Author contributions
Study conceptualisation and methodology design: RS & KM.
Data curation: RS.
Figures: CL & JS.
Manuscript preparation and review: All authors.
Conflict of interest disclosure
The authors declare that they have no conflict of interest.
Ethical statement
All of the authors have read and have abided by the statement of ethical standards for manuscripts submitted to the Obesity Research & Clinical Practice.
Sources of support
None.
Endorsements
British Obesity and Metabolic Surgery Society, The Israeli Society for Metabolic and Bariatric Surgery, Norwegian Society for the Surgery of Obesity, Obesity Surgery Society of India, and Società Italiana di Chirurgia dell’Obesità e delle malattie metaboliche
Appendix A
Survey sent to surgeons.
References
- 1.Collaborative, C Elective surgery cancellations due to the COVID-19 pandemic: global predictive modelling to inform surgical recovery plans. BJS (Br J Surg) 2020;107(11):1440–1449. doi: 10.1002/bjs.11746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Yang W. Recommendations for metabolic and bariatric surgery during the COVID-19 pandemic from IFSO. Obes Surg. 2020;30(6):2071–2073. doi: 10.1007/s11695-020-04578-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rubino F. Joint international consensus statement for ending stigma of obesity. Nat Med. 2020;26(4):485–497. doi: 10.1038/s41591-020-0803-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Stahel P.F. How to risk-stratify elective surgery during the COVID-19 pandemic? Patient Saf Surg. 2020;14:8. doi: 10.1186/s13037-020-00235-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kelley K. Good practice in the conduct and reporting of survey research. Int J Qual Health Care. 2003;15(3):261–266. doi: 10.1093/intqhc/mzg031. [DOI] [PubMed] [Google Scholar]
- 6.Chen Q., Allot A., Lu Z. Keep up with the latest coronavirus research. Nature. 2020;579(7798):193. doi: 10.1038/d41586-020-00694-1. [DOI] [PubMed] [Google Scholar]
- 7.Aminian A. Bariatric surgical practice during the initial phase of COVID-19 Outbreak. Obes Surg. 2020;30(9):3624–3627. doi: 10.1007/s11695-020-04617-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Singhal R. Global 30-day outcomes after bariatric surgery during the COVID-19 pandemic (GENEVA): an international cohort study. Lancet Diabetes Endocrinol. 2021;9(1):7–9. doi: 10.1016/S2213-8587(20)30375-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Collaborative, C Mortality and pulmonary complications in patients undergoing surgery with perioperative SARS-CoV-2 infection: an international cohort study. Lancet. 2020;396(10243):27–38. doi: 10.1016/S0140-6736(20)31182-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tao K.X. Recommendations for general surgery clinical practice in novel coronavirus pneumonia situation. Zhonghua Wai Ke Za Zhi. 2020;58(0):E001. doi: 10.3760/cma.j.issn.0529-5815.2020.0001. [DOI] [PubMed] [Google Scholar]
- 11.Zhou F. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Surgeons A.Co. 2020. COVID-19: guidance for triage of non-emergent surgical procedures.https://www.facs.org/covid-19/clinical-guidance/triage 17/03/2020 [cited 2020 17/04/2020]; Available from: [Google Scholar]
- 13.Societies I.M. 2018. IFSO.https://www.ifso.com/ifso-member-societies 2018 [cited 2020 23/05/2020]; Available from: [Google Scholar]
- 14.Betton L. COVID-19 digestive symptoms mimicking internal hernia presentation after Roux-en-Y-Gastric Bypass; comment on “Internal Hernia in the Times of COVID-19: to laparoscope or not to laparoscope?”. Obes Surg. 2020;30(9):3601–3602. doi: 10.1007/s11695-020-04664-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Schauer P.R. Bariatric surgery versus intensive medical therapy for diabetes - 5-Year outcomes. N Engl J Med. 2017;376(7):641–651. doi: 10.1056/NEJMoa1600869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Adil M.T. Perioperative practices concerning sleeve gastrectomy – a survey of 863 surgeons with a cumulative experience of 520,230 procedures. Obes Surg. 2020;30(2):483–492. doi: 10.1007/s11695-019-04195-7. [DOI] [PubMed] [Google Scholar]