Abstract
OBJECTIVES:
To characterize current practices, barriers, and facilitators to assessing and addressing family caregivers’ needs and risks in primary care.
DESIGN:
Cross-sectional, national mail-based survey.
SETTING:
American Medical Association Masterfile database.
PARTICIPANTS:
U.S. primary care physicians (N = 106), including general internists (n = 44) and geriatricians (n = 62).
MEASUREMENTS:
Approaches to assessing and addressing family caregivers’ needs and risks; barriers and facilitators to conducting caregiver assessments.
RESULTS:
Few respondents reported conducting a formal caregiver assessment using a standardized instrument in the past year (10.5%). Informal, unstructured discussions about caregivers’ needs and risks were common and encompassed a range of issues, most frequently caregivers’ management of patients’ safety (41.0%), ability to provide assistance (40.0%), and need for support (40.0%). To address caregiver needs, most respondents endorsed referring patients to services (e.g., adult day care, home care) (69.8%), assessing the appropriateness of the patient’s living situation (67.9%), and referring caregivers to community agencies (63.2%). Lack of time was the most frequently cited barrier to assessing caregivers’ needs (81.1%). The most commonly endorsed facilitators were access to better referral options (67.0%) and easier referral mechanisms (65.1%). Practice patterns, barriers, and facilitators to caregiver assessment did not differ by physician type.
CONCLUSIONS:
Primary care physicians use informal, unstructured discussions rather than standardized instruments to assess caregivers’ needs and risks. There is heterogeneity in the topics discussed and types of referrals made. Findings indicate the lack of translation of caregiver assessment tools from research to practice
Keywords: caregiving, primary care, screening
INTRODUCTION
More than 90% of older adults who receive assistance in the community rely on help from a family member or other unpaid caregiver, either alone or in combination with paid care.1 Family caregivers not only provide the majority of disability-related assistance to older adults,2 they also assist with health management activities, such as arranging care, administering medications, and attending medical appointments.3–6 Across numerous studies, effective caregiver assistance has been linked with positive outcomes for older adults, including better adherence to treatment plans and improved physical functioning.7–9 However, caregivers receive inadequate preparation for the tasks they must assume.10 They report high levels of stress11 and are at risk for physical illness, depression and anxiety, and sleep disturbance.12–15
On the basis of such evidence, research and clinical practice guidelines recommend that primary care clinicians assess the needs of family caregivers and suggest appropriate referrals for support.11,16 The extent to which these guidelines are implemented in practice is unclear due to limited empirical data; however, emerging evidence suggests limited uptake. National surveys of family caregivers find that nearly half of respondents are never asked by health care providers whether they need help managing older adults’ care17 and less than 1 in 5 are asked what they need to take care of themselves.18 Quantitative data on primary care physicians’ approaches to identifying caregivers’ needs do not exist, but qualitative research and case reports suggest heterogeneity in existing practice patterns.19,20 A more complete understanding of physicians’ experiences with assessing and addressing caregivers’ needs is needed to inform the advancement of primary care delivery models that acknowledge the broader social context in which individuals manage their health21,22 and payment reforms that are poised to appropriately encourage explicit inclusion, assessment, and support of caregivers.23
To our knowledge, this is the first study to characterize current practices, barriers, and facilitators to family caregiver assessment in a national random sample of U.S. primary care physicians. The study was undertaken to examine both formal (use of standardized instruments) and informal approaches (unstructured discussions) to assess the needs and risks of caregivers of persons with and without dementia, acknowledging the unique challenges and disproportionate impact of caring for a person with cognitive impairment,24,25 as well as commonly used resources and referrals. The study also identifies structural barriers and attitudes that may impede uptake of caregiver assessment and potential facilitators for future integration.
The study sought to comparatively evaluate practice patterns of geriatricians and general internists, recognizing potential variability in training and experience with family caregivers. We hypothesize that geriatricians may be more attuned to the needs of family caregivers, especially those caring for persons with age-related diseases such as dementia, given specialty-specific education and increased prevalence of family accompaniment among older patients.26 Although internists’ long-term relationships with patients may afford personal investment in and knowledge of the family’s circumstances, time pressure may preclude routine discussion of caregiver issues.27–29
METHODS
Overview
We conducted a mail-based, cross-sectional survey of a national random sample of primary care physicians in the United States from March 2019 to November 2020. The survey was distributed via first class postal mail with an option to complete the survey online. A $25 gift card was included in the survey packet as an unconditional incentive. Follow-up phone calls were made to nonresponders 2 weeks after the initial mailing to remind them to complete and return the survey. These strategies that have been shown to improve response rates among health care providers participating in survey research.30 The study protocol was approved by the Weill Cornell Medicine Institutional Review Board as an exempt study.
Study Sample
The survey was mailed to a total of 500 primary care physicians (250 internal medicine physicians; 250 geriatricians) randomly selected from the American Medical Association (AMA) Masterfile. The AMA Masterfile includes nearly all physicians in the United States and is not limited to members of the AMA; all physicians are coded by primary medical specialty and board certification. The sampling frame for this study included physicians whose medical specialty designation was Internal Medicine with or without board certification in Geriatrics. Physicians were eligible to participate if they had been working in a primary care setting for at least 1 year beyond training. They were ineligible if they were not treating any older adults (age 65+) or were working abroad or for any of the armed forces.
Survey Instrument
Overview
The survey instrument (Supplementary Appendix S1) was designed to cover three domains, chosen on the basis of prior literature and important themes that emerged from in-depth interviews with primary care clinicians, patients, and caregivers:19 (1) physicians’ self-reported practices for identifying and addressing family caregivers’ needs, (2) perceived and anticipated barriers and facilitators to identifying and addressing caregivers’ needs, and (3) practice and demographic characteristics.
The instrument was iteratively revised and pilot-tested prior to administration to the target sample. A preliminary version was circulated to local primary care clinicians a weekly staff meetings and to researchers (gerontologists health services researchers, psychometricians) who were asked to provide feedback on the content and relative importance of individual items. Revisions were made to improve the overall organization and format, clarify ques tion wording, and reduce the total number of items to decrease time demands on participants. To verify the time commitment and appropriateness of individual items, an electronic version of the survey was distributed to profes sional organizations (e.g., American Geriatrics Society Gerontological Society of America) via online list-servs One hundred primary care providers responded; a timestamp was used to verify the average completion time.
Practices for Assessing and Addressing Caregiver Needs
To evaluate physicians’ formal assessment practices, participants were first asked whether their practice had a standardized procedure for assessing caregivers’ needs and whether they personally conducted a caregiver assessment using a standardized instrument in the past year. They were subsequently asked about the frequency of conducting formal assessments with caregivers of persons with and without dementia, with response choices ranging from “almost never (≤25% of visits)” to “almost always (≥75% of visits).”
To evaluate informal assessment practices, participants were first asked whether they had a conversation with caregivers of persons with versus without dementia about their needs and risks in the past year. They were subsequently asked about the frequency of these conversations, with response options ranging from “almost never (≤25% of visits)” to “almost always (≥75% of visits).”
Additional questions asked participants how often they discussed each of eight caregiver needs or risks, selected on the basis of consensus recommendations.31,32 These items included caregiver (1) burnout or stress, (2) ability to provide assistance, (3) willingness to provide assistance, (4) physical health, (5) mental health, (6) need for services or supports, (7) management of patient safety, and (8) role as health care proxy. Response options ranged from “almost never (≤25% of visits)” to “almost always (≥75% of visits).”
Based on previous reports,11,32,33 respondents were asked about the types of resources and referrals they provided to caregivers, including referral to medical services, community-based supports, academic-affiliated programs, and other resources (e.g., web-based materials).
Barriers and Facilitators
Respondents were provided with a list of common barriers to assessing caregivers’ needs derived from prior research11,19 and consensus reports,32,33 including organization- and practice-level challenges (e.g., HIPAA regulations, time constraints) as well as personal attitudes and beliefs (e.g., concerns about personal liability). Respondents were also asked to rate the helpfulness of several facilitators to addressing caregiver issues in the future (5-point scale), including referral-related facilitators (easier referral mechanisms), practice-related facilitators (colocation of case managers or mental health specialists), and training-related needs. Physicians were categorized according to those who rated each item as “very helpful” or “helpful” versus those who endorsed any other category.
Demographic and Practice Characteristics
Respondents provided information on their age, gender, race and ethnicity, number of years practicing, number of hours per week spent seeing outpatients, proportion of older adults (aged 65+) in their patient panels, proportion of older adults with and without dementia who are accompanied by a family caregiver to their primary care appointments, and proportion of their patient panel receiving Medicaid or Medicare. They also reported their practice type (private practice, academic affiliate, community health center, other), practice location (urban, suburban, rural), and state (categorized into U.S. Census Bureau defined regions). Provider specialty (geriatrics, internal medicine) was obtained from the AMA Masterfile.
Analytic Plan
Descriptive statistics were computed to summarize the demographic and practice characteristics of the full sample. Group differences in demographic and practice characteristics, current practices for assessing and addressing caregiver needs, and perceived barriers and facilitators were examined using chi-square and Fisher exact tests for categorical variables and t-tests for continuous variables. Two-tailed P-values less than .05 were considered statistically significant. The extent and nature of missing data was examined. As item nonresponse was low, we provide estimates for participants who responded. Statistical analyses were conducted using SPSS Version 23.0 and SAS Version 9.4.
RESULTS
Of the 500 physicians surveyed, 26 were ineligible because they had not worked in primary care for at least 1 year (n = 6), were not treating older adults (aged 65+) (n = 10), or were working abroad or for the armed forces (n = 10). Of the 474 eligible physicians, 106 completed the survey (22% overall response rate), of whom 44 were internists (19% response rate) and 62 were geriatricians (26% response rate). Demographic characteristics of respondents relative to the broader population of AMA primary care physicians were generally similar, although participants were slightly younger (Supplementary Table S1).
Internists and geriatricians did not vary significantly with respect to demographic characteristics. They were approximately 58 years of age, most were men (57.5%), and three quarters were White (75.0%) (Table 1). On average, respondents had been in practice for 26 years and spent 29 hours per week seeing outpatients. Geriatricians reported a larger proportion of older adults in their patient panels than internists (P < .001); they also reported a larger proportion of patients on Medicaid or Medicare (P < .001). On average, respondents estimated that 63.6% of older adults with dementia and 24.9% of older adults without dementia attended office visits with a family caregiver.
Table 1.
Description of Survey Respondents
| Physician Group |
||||
|---|---|---|---|---|
| All Physicians (N = 106) | Internists (n = 44) | Geriatricians (n = 62) | P value | |
| Physician characteristics | ||||
| Age, M ± SD | 57.7 ± 10.6 | 59.1 ± 10.3 | 56.3 ± 10.8 | .19 |
| Male, % | 57.5 | 63.6 | 54. | .32 |
| Race, % | .51 | |||
| White (non-Hispanic) | 75.0 | 75.0 | 75.0 | |
| African American | 3.8 | 2.3 | 5.0 | |
| Asian | 19.2 | 18.2 | 20.0 | |
| Other (including multi-racial) | 2.0 | 4.6 | 0.0 | |
| Hispanic/Latino ethnicity, % | 6.9 | 4.7 | 8.5 | .70 |
| Years practicing (not including training), M ± SD | 25.5 ± 11.7 | 27.3 ± 12.3 | 24.2 ± 11.2 | .18 |
| Hours per week spent seeing outpatients, M ± SD | 28.7 ± 13.3 | 30.9 ± 13.9 | 27.1 ± 12.7 | .16 |
| Self-reported proportion of older adults (≥65 years) in patient panel, M ± SD | 72.4 ± 24.3 | 47.0 ± 14.7 | 89.6 ± 10.1 | .00 |
| Self-reported proportion of older patients with dementia who attend visits with a caregiver, M ± SD | 63.6 ± 32.7 | 62.1 ± 34.6 | 65.5 ± 31.5 | .54 |
| Self-reported proportion of older patients without dementia who attend visits with a caregiver, M ± SD | 24.9 ± 21.3 | 20.5 ± 21.1 | 27.9 ± 21.1 | .63 |
| Self-reported proportion of patient panel receiving Medicaid or Medicare, M ± SD | 67.3 ± 26.1 | 48.7 ± 19.1 | 79.6 ± 22.7 | .00 |
| Practice characteristics | ||||
| Practice type, % | .34 | |||
| Private practice | 53.8 | 63.6 | 46.8 | |
| Academic-affiliate | 17.0 | 11.4 | 21.0 | |
| Community health center | 7.5 | 9.1 | 6.5 | |
| Other (hospital-based, multi-specialty, goverment health center) | 0.9 | 0.0 | 1.6 | |
| Practice location, % | .91 | |||
| Suburban | 44.3 | 45.5 | 43.5 | |
| Urban | 38.7 | 36.4 | 40.3 | |
| Rural | 17.0 | 18.2 | 16.1 | |
| Region (US Census Bureau defined), % | .12 | |||
| Northeast | 32.7 | 37.2 | 29.3 | |
| Midwest | 24.8 | 18.6 | 29.3 | |
| South | 20.8 | 14.0 | 25.9 | |
| West | 21.8 | 30.2 | 15.5 | |
Approximately half of all respondents worked in private practice (53.8%). The rest practiced at academic-affiliates (17.0%), community health centers (7.5%), or other settings (0.9%). Most physicians practiced in suburban (44.3%) or urban (38.7%) locations; a minority (17.0%) practiced in rural areas. There was a relatively even distribution across U.S. regions: 32.7% in the Northeast, 24.8% in the Midwest, 20.8% in the South, and 21.8% in the West.
Approaches to Assessing Caregivers’ Needs
A small minority of physicians reported that their practice had a standardized procedure for assessing caregivers’ needs (7.5%) and few had personally conducted a formal caregiver assessment in the last year (10.5%) (Table 2). With regard to frequency, a minority of respondents routinely (in at least 75% of visits) conducted formal assessments with dementia caregivers (10.9%) and non-dementia caregivers (8.0%). No significant differences were observed between physician groups with regard to formal assessment practices.
Table 2.
Formal and Informal Approaches to Assessing Caregiver Needs
| Physician Group |
||||
|---|---|---|---|---|
| All Physicians (N = 106) | Internists (n = 44) | Geriatricians (n = 62) | P value | |
| Formal approaches,a % | ||||
| Practice/clinic has a standardized procedure for caregiver assessment | 7.5 | 6.8 | 8.1 | .81 |
| Personally conducted a formal caregiver assessment using a standardized instrument in last year | 10.5 | 6.8 | 13.1 | .35 |
| Routinely conducted formal assessments with dementia caregiversb | 10.9 | 7.0 | 13.8 | .14 |
| Routinely conducted formal assessments with non-dementia caregiversb | 8.0 | 11.6 | 5.3 | .24 |
| Informal approaches,c % | ||||
| Had an informal conversation with a dementia caregiver about needs/risks in last year | 93.3 | 88.6 | 96.7 | .13 |
| Had an informal conversation with a non-dementia caregiver about needs/risks in last year | 80.8 | 69.8 | 88.5 | .02 |
| Routinely had informal conversations with dementia caregivers about their needs/risksd | 33.7 | 33.3 | 33.9 | .63 |
| Routinely had informal conversations with non-dementia caregivers about their needs/risksd | 15.5 | 23.3 | 11.1 | .42 |
Formal approaches refer to the use of a standardized instrument to evaluate caregiver needs and risks. Participants were first asked whether they had personally conducted a formal caregiver assessment within the past year and subsequently asked about the frequency of performing such an assessment.
Proportion of respondents who endorse performing formal caregiver assessment in ≥75% of visits.
Informal approaches refer to unstructured, informal conversations with caregivers about their needs and risks. Participants were first asked whether an informal conversation about caregivers’ needs/risks in the past year and subsequently about the frequency of these discussions.
Proportion of respondents who endorse having informal conversations in ≥75% of visits.
Most physicians assessed caregivers’ needs and risks informally (Table 2). Internists and geriatricians were equally likely to report having had informal discussions with dementia caregivers about his or her needs and risks in the past year (88.6% vs 96.7%; P = .13), but geriatricians were more likely to have had an informal conversation with a non-dementia caregiver (88.5% vs 69.8%; P < .05). With regard to frequency, approximately one third of respondents routinely (in at least 75% of visits) had informal conversations with dementia caregivers (33.7%); whereas 15.5% routinely (in at least 75% of visits) had such discussions with non-dementia caregivers.
Across all respondents, range of approximately 20% to 40% routinely discussed each of eight caregiver needs and risks (Table 3). The most commonly discussed topics were caregivers’ management of patients’ safety, ability to provide assistance, and need for services or supports, with approximately 40% of respondents routinely discussing each of these issues. The most infrequently discussed topics were caregivers’ physical (20.2%) and mental health (21.2%); approximately one third of respondents almost never discussed these issues.
Table 3.
Caregiver Needs and Risks Discussed Informally
| Physician Group |
||||
|---|---|---|---|---|
| Specific Issue Discussed, % | All Physicians (n = 106) | Internists (n = 44) | Geriatricians (n = 62) | P value |
| Burnout or stress | .98 | |||
| Almost never | 16.3 | 15.9 | 16.7 | |
| Sometimes | 53.8 | 54.5 | 53.5 | |
| Routinely | 29.8 | 29.5 | 30.0 | |
| Ability to provide assistance | .44 | |||
| Almost never | 14.3 | 15.9 | 13.1 | |
| Sometimes | 45.7 | 36.4 | 52.5 | |
| Routinely | 40.0 | 47.7 | 34.4 | |
| Willingness to provide assistance | .66 | |||
| Almost never | 23.1 | 25.0 | 21.7 | |
| Sometimes | 46.2 | 38.6 | 51.7 | |
| Routinely | 30.8 | 36.4 | 26.7 | |
| Caregiver physical health | .36 | |||
| Almost never | 34.6 | 29.5 | 38.3 | |
| Sometimes | 45.2 | 47.7 | 43.3 | |
| Routinely | 20.2 | 22.7 | 18.3 | |
| Caregiver mental health | .37 | |||
| Almost never | 35.6 | 34.1 | 36.7 | |
| Sometimes | 43.3 | 38.6 | 46.7 | |
| Routinely | 21.2 | 27.3 | 16.7 | |
| Caregiver need for services or supports | .48 | |||
| Almost never | 18.1 | 20.5 | 16.4 | |
| Sometimes | 41.9 | 43.2 | 41.0 | |
| Routinely | 40.0 | 36.4 | 42.6 | |
| Caregiver management of patients’ safety | .29 | |||
| Almost never | 14.3 | 20.5 | 9.8 | |
| Sometimes | 44.8 | 40.9 | 47.5 | |
| Routinely | 41.0 | 38.6 | 42.6 | |
| Caregiver role as health care proxy a | .93 | |||
| Almost never | 15.4 | 20.5 | 11.7 | |
| Sometimes | 48.1 | 38.6 | 55.0 | |
| Routinely | 36.5 | 40.9 | 33.3 | |
Note: “Almost never” defined as discussing issue in ≤25% of visits. “Sometimes” defined as discussing issue in 25% to 75% of visits. “Routinely” defined as discussing issue in ≥75% of visits.
Refers to health care agent for advance directives.
Use of Resources and Referrals
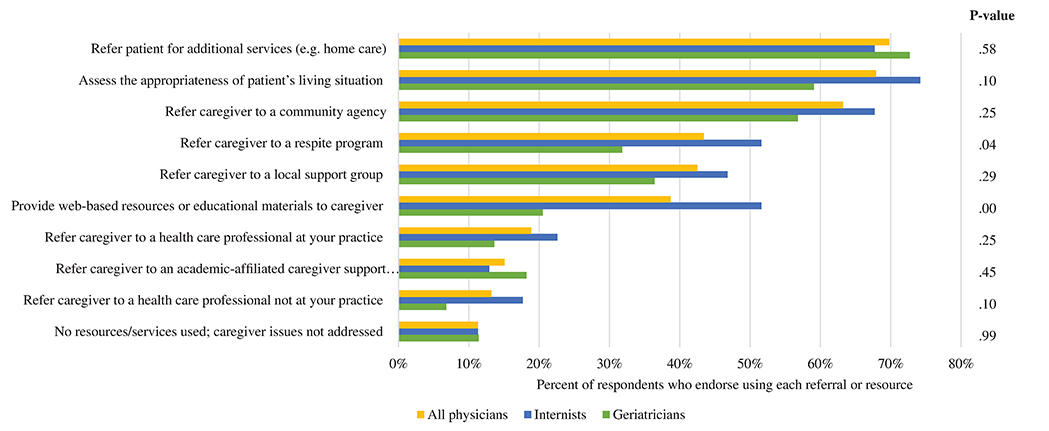
The majority of physicians endorsed referring the patient for additional services (69.8%), assessing the appropriateness of the patient’s living situation (67.9%), and referring the caregiver to a community agency (63.2%) (Figure 1). Compared with internists, geriatricians were significantly more likely to refer caregivers to respite programs (51.6% vs 31.8%; P < .05) or provide them with web-based resources or educational materials (51.6% vs 20.5%; P < .001). A large proportion of respondents reported referring caregivers to local support groups (42.5%), whereas much smaller proportions made referrals to other health care professionals (18.9% at the physician’s practice; 13.2% at a different practice) and to academic-affiliated support programs (15.1%). A small number of respondents reported using no resources or services (11.3%).
Figure 1.
Primary care clinicians’ use of resources and referrals in addressing caregiver needs and risks.
Barriers and Facilitators
Lack of time was the most frequently reported barrier to assessing caregivers’ needs, endorsed by 81.1% of respondents (Table 4). Inadequate reimbursement (39.6%) and inability to have private discussions with caregivers (33.0%) were concerns among one third of participants. Approximately one quarter of physicians endorsed referral-related barriers, including lack of access to (27.4%) and uncertainty about referral options (22.6%). Similar proportions reported uncertainty about assessing caregiver issues (24.5%), unwillingness of caregivers to discuss their needs (22.6%), and concerns about privacy/HIPAA regulations (20.8%). Few physicians reported discomfort raising sensitive topics with caregivers (8.5%) or concerns about personal liability (7.5%). Almost no respondents reported that assessing caregiver needs was the responsibility of other health care providers (2.8%) or was irrelevant to the clinical care of their patients (1.9%).
Table 4.
Barriers and Facilitators to Identifying and Addressing Caregiver Needs and Risks
| Physician Group |
||||
|---|---|---|---|---|
| All Physicians (N = 106) | Internists (n = 44) | Geriatricians (n = 62) | P value | |
| Barriers, % | ||||
| Lack of time | 81.1 | 81.8 | 80.6 | .88 |
| Inadequate reimbursement | 39.6 | 43.2 | 37.1 | .53 |
| Inability to have private discussion with the caregiver | 33.0 | 36.4 | 30.6 | .54 |
| Lack of access to referral options | 27.4 | 34.1 | 22.6 | .19 |
| Uncertainty about assessing caregiver issues | 24.5 | 25.0 | 24.2 | .92 |
| Uncertainty about referral option | 22.6 | 25.0 | 21.0 | .63 |
| Reluctance of caregivers to discuss needs | 22.6 | 25.0 | 21.0 | .63 |
| HIPAA regulations and privacy concerns | 20.8 | 25.0 | 17.7 | .36 |
| Discomfort bringing up sensitive topics with caregivers | 8.5 | 9.1 | 8.1 | .85 |
| None; do not discuss or assess caregiver issues | 7.5 | 4.5 | 9.7 | .32 |
| Concern about personal liability | 7.5 | 9.1 | 6.5 | .61 |
| Responsibility of other health care providers | 2.8 | 4.5 | 1.6 | .37 |
| Irrelevance to the clinical care of patients | 1.9 | 4.5 | 0.0 | .09 |
| Facilitators,a % | ||||
| Better availability of referral options | 71.0 | 66.7 | 74.1 | .41 |
| Easier referral mechanisms | 69.7 | 64.3 | 73.7 | .32 |
| Co-location of behavioral/mental health specialists | 67.0 | 69.0 | 65.5 | .71 |
| Co-location of care managers or social workers | 65.0 | 69.8 | 61.4 | .39 |
| Training in how to address caregiver issues | 64.4 | 57.1 | 69.5 | .20 |
| Co-location of caregiver’s primary care provider | 50.0 | 53.5 | 47.4 | .54 |
Note: Multiple responses allowed.
Proportion of respondents endorsing each facilitator as “helpful” or “very helpful.”
The most commonly endorsed facilitators were better referral options (71.0%) and easier referral mechanisms (69.7%). Practice-related facilitators, including co-location of behavioral or mental health specialists (67.0%) and co-location of care managers or social workers (65.0%) were endorsed by approximately two thirds of respondents, as was training in how to address caregiver issues (64.4%). Half of respondents indicated that co-location of the caregiver’s primary care physician would be helpful in addressing caregiver issues. Barriers and facilitators did not differ significantly by physician group.
DISCUSSION
In this national random sample, few primary care physicians reported using standardized caregiver assessment tools but most engaged in informal discussions about caregivers’ needs and risks. Only 7.5% of the physicians surveyed worked in practices that had a standardized procedure for assessing caregiver needs. Multiple barriers were found that inhibited assessment of caregivers’ needs, most prominently lack of time and inadequate reimbursement. Better referral options and easier referral mechanisms were the most commonly endorsed facilitators to assessing and addressing caregivers’ needs. Contrary to expectations, practice patterns, barriers, and facilitators to caregiver assessment were largely consistent between geriatricians and internists.
Results from this study reflect the growing awareness and interest in supporting family caregivers by the medical community. Whereas previous reports described family caregivers as an “invisible” workforce that is marginalized in medical encounters,34 recent surveys indicate that primary care clinicians believe that caregivers play an important role in patient care35 and feel that it is their responsibility to respond to caregiver concerns.36 Findings from the present study offer evidence for how such beliefs are put into practice. The vast majority of geriatricians and internists reported having at least one conversation with family caregivers about their needs and risks in the past year. Virtually no respondents reported that caregiver assessment was irrelevant to the clinical care of their patients.
Despite the advent of care delivery models that encourage family involvement in health care processes,37,38 there is a lack of consensus regarding the elements to be included in caregiver assessment and the frequency with which an assessment should be conducted. In this study, 40% of respondents regularly inquired about caregivers’ ability to provide assistance and need for services or supports, but nearly 20% almost never asked about these issues. Surveys of family caregivers indicate that large proportions are never asked by health care providers about their abilities and preferences,39 whether they need help managing older adults’ care,17 or what they need to take care of themselves.18 The vast majority report that they do not receive role-related training.10 Future research using real-time audio-recordings of the medical encounter may help to shed light on the disconnect between caregivers’ and clinicians’ perspectives on the topics discussed and training provided. As family caregivers’ circumstances and needs often fluctuate with patients’ cognitive and functional status,40 standardized protocols that involve reassessment at regular intervals merit consideration and careful planning to ensure optimal integration and sustainability.
Study findings underscore the lack of translation of caregiver assessment tools from research to practice. Numerous psychometrically validated assessment instruments have undergone rigorous development and testing in research contexts,32 but many of these instruments are lengthy and therefore not feasible for administration in primary care.41 Indeed, only 1 in 10 primary care physicians in this study reported using a standardized instrument to assess family caregivers’ needs. Lack of time was the most commonly endorsed barrier to caregiver assessment among both geriatricians and internists, a finding that is consistent with prior qualitative research and consensus reports.19,31
At present, no guidelines exist for how caregiver assessments should be incorporated into primary care delivery. Of course, future integration will require tailoring to individual practices given variability in organizational structure, resources, access to local caregiver resources, and potential for embedding caregiver data within health technology and information systems. Findings from this study and others10,19 strongly suggest the need for evidence-based guidelines that can be applied across structural and administrative mechanisms in primary care, especially given new quality measures that emphasize outcomes related to patient and caregiver experiences.42
The study points to several new directions for program design and evaluation that may lead to better integration of caregiver assessment into care planning and execution. First, the primary care environment makes advisable embedding short assessments within existing practice workflows.19,34 One approach that warrants consideration is the development of a brief screen, consisting of questions that ascertain basic information about caregivers’ risks and need for services, that is integrated into health information technology (electronic health record, patient portal). This approach may be particularly useful given increasing demands for telemedicine and remote access to health care.43
Second, physicians’ endorsement of referral-related facilitators, including easier referral mechanisms and better referral options underscores the need for assessment protocols that incorporate standardized procedures for connecting caregivers with services and supports that are tailored to their needs. Harnessing health information technology to record and track referrals will be critical to ensuring longitudinal support by facilitating linkages between clinical practice and community-based services.44 Third, to promote workforce capacity, the design of caregiver assessment protocols should be accompanied by brief and effective training for clinicians, as two-thirds of geriatricians and internists reported that training would help them to incorporate caregiver assessment into practice. Continuing Medical Education credits may help to encourage additional training in this area. Evidence-based guidelines will need to clearly articulate practice standards and requirements.
Fourth, reimbursement issues must be addressed. Potential opportunities include promoting reimbursement through the Centers for Medicare & Medicaid Cognitive Assessment and Care Planning code for persons with dementia, which includes caregiver assessment as a service element,23 or through annual Medicare visits, which include a health risk assessment for beneficiaries who are family caregivers. Consideration should also be given to the development of payment mechanisms that can be applied across health systems to encourage providers’ interactions with caregivers even when the patient is not present, including in-person consultations, telemedicine visits, and correspondence by email and phone.
Finally, there is likely a role for interdisciplinary teams to act on the assessment when serious problems are identified, as evidenced by the finding that the majority of respondents endorsed co-location of behavioral and mental health as a potential facilitator. Pragmatic trials that draw on implementation science frameworks will need to evaluate cost-effectiveness, patient perceived quality of care, and caregiver preparedness.
This study has several limitations. Although our response rate was achieved using best practices for engaging health care providers in survey research and is comparable to other physician surveys using the AMA Masterfile,45–47 generalizability of our study findings may be limited. Findings may also be subject to recall, social desirability, and nonresponse biases; for example, physicians with greater familiar or engagement with caregiver may have been more likely to participate. These biases may have resulted in conservative estimates regarding the use of assessment instruments and informal discussions as respondents are likely to be more aware of caregiver concerns. As such, caregiver assessment may actually be less frequent than was observed in this study. We also note that our study sample only included physicians and results may not extend to other primary care professionals. Finally, future research will need to examine clinicians’ use of resources and referrals by the patient’s dementia status as these questions did not distinguish caregivers of older persons with and without dementia.
CONCLUSIONS
Issues of family caregiving will become more prominent as the baby boom generation enters into their later years48 with growing numbers of older adults who rely on family caregivers at medical visits. As in other contexts, such as pediatrics49 and state Medicaid programs,50 meaningful and systematic assessment is a clear first step to identify needed services, incorporating family members into planning care, and ultimately improving patient outcomes.
Supplementary Material
Supplementary Appendix S1 Survey instrument.
Supplementary Table S1: Characteristics of Survey Respondents Compared to AMA Primary Care Physicians.
ACKNOWLEDGEMENTS
Financial Disclosure: This project was supported by grants K01AG061275 and UL1TR002384 from the National Institutes of Health.
Sponsor’s Role: The funding sources had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
We thank Julianna Maisano and Sylvia Lee for their assistance with survey distribution. We thank the National Coalition on Care Coordination (N3C) for endorsing the survey.
Footnotes
Conflict of Interest: The authors have no conflicts of interest to report.
SUPPORTING INFORMATION
Additional Supporting Information may be found in the online version of this article.
REFERENCES
- 1.Houser A, Gibson MJ, Redfoot D. Trends in Family Caregiving and Paid Home Care for Older People with Disabilities in the Community: Data from the National Long-Term Care Survey. Washington, DC: AARP Public Policy Institute; 2010. [Google Scholar]
- 2.IOM. Retooling for an Aging America: Building the Health Care Workforce. Washington, DC: The National Academies Press; 2008. [PubMed] [Google Scholar]
- 3.Riffin C, Van Ness PH, Iannone L, Fried T. Patient and caregiver perspectives on managing multiple health conditions. J Am Geriatr Soc. 2018;66 (10):1992–1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bookman A, Harrington M. Family caregivers: a shadow workforce in the geriatric health care system? J Health Polit Policy Law. 2007;32(6): 1005–1041. [DOI] [PubMed] [Google Scholar]
- 5.Riffin C, Van Ness PH, Wolff JL, Fried T. Family and other unpaid caregivers and older adults with and without dementia and disability. J Am Geriatr Soc. 2017;65(8):1821–1828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wolff JL, Spillman BC, Freedman VA, Kasper JD. A national profile of family and unpaid caregivers who assist older adults with health care activities. JAMA Intern Med. 2016;176(3):372–379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.DiMatteo MR. Social support and patient adherence to medical treatment: a meta-analysis. Health Psychol. 2004;23(2):207–218. [DOI] [PubMed] [Google Scholar]
- 8.Long KH, Moriarty JP, Mittelman MS, Foldes SS. Estimating the potential cost savings from the New York University caregiver intervention in Minnesota. Health Aff (Millwood) 2014;33(4):596–604. [DOI] [PubMed] [Google Scholar]
- 9.Van Houtven CH, Norton EC. Informal care and health care use of older adults. J Health Econ. 2004;23(6):1159–1180. [DOI] [PubMed] [Google Scholar]
- 10.Burgdorf J, Roth DL, Riffin C, Wolff JL. Factors associated with receipt of training among caregivers of older adults. JAMA Intern Med. 2019;179(6): 833–835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Schulz R, Eden J, Committee on Family Caregiving for Older Adults, National Academies of Science, Engineering, and Medicine. Families Caring for an Aging America. Washington, DC: National Academies Press; 2016. [PubMed] [Google Scholar]
- 12.Joling KJ, van Hout HP, Schellevis FG, et al. Incidence of depression and anxiety in the spouses of patients with dementia: a naturalistic cohort study of recorded morbidity with a 6-year follow-up. Am J Geriatr Psychiatry. 2010;18(2):146–153. [DOI] [PubMed] [Google Scholar]
- 13.Fonareva I, Oken BS. Physiological and functional consequences of caregiving for relatives with dementia. Int Psychogeriatr. 2014;26(5):725–747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pinquart M, Sörensen S. Differences between caregivers and noncaregivers in psychological health and physical health: a meta-analysis. Psychol Aging. 2003;18(2):250–267. [DOI] [PubMed] [Google Scholar]
- 15.Capistrant BD. Caregiving for older adults and the caregivers’ health: an epidemiologic review. Curr Epidemiol Rep. 2016;3:72–80. [Google Scholar]
- 16.Mitnick S, Leffler C, Hood VL, American College of Physicians Ethics P, Committee HR. Family caregivers, patients and physicians: ethical guidance to optimize relationships. J Gen Intern Med. 2010;25(3):255–260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wolff JL, Freedman VA, Mulcahy JF, Kasper JD. Family caregivers’ experiences with health care workers in the care of older adults with activity limitations. JAMA Netw Open 2020;3(1):e1919866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Caregiving in the US. Washington, DC: National Alliance for Caregiving and the AARP Public Policy Institute; 2015. [Google Scholar]
- 19.Riffin C, Wolff JL, Estill M, Prabhu S, Pillemer KA. Caregiver needs assessment in primary care: views of clinicians, staff, patients, and caregivers. J Am Geriatr Soc. 2020;68:1262–1270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Barnard D, Yaffe MJ. What is the physician’s responsibility to a patient’s family caregiver? Virtual Mentor. 2014;16(5):330–338. [DOI] [PubMed] [Google Scholar]
- 21.Stange KC, Nutting PA, Miller WL, et al. Defining and measuring the patient-centered medical home. J Gen Intern Med. 2010;25(6):601–612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Scholl S, Torda P, Peikes D, Han E, Genevro J. Engaging Patients and Families in the Medical Home. Agency for Healthcare Research and Quality: Rochville, MD; 2010. [Google Scholar]
- 23.Alzheimer’s Association. Cognitive Assessment and Care Planning Services: Alzheimer’s Association Expert Task Force Recommendations and Tools for Implementation. Chicago, IL: Alzheimer’s Association; 2018. [Google Scholar]
- 24.Kasper JD, Freedman VA, Spillman BC, Wolff JL. The disproportionate impact of dementia on family and unpaid caregiving to older adults. Health Aff (Millwood) 2015;34(10):1642–1649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Riffin C, Van Ness PH, Wolff JL, Fried T. Multifactorial examination of caregiver burden in a national sample of family and unpaid caregivers. J Am Geriatr Soc. 2019;67(2):277–283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wolff JL, Roter DL. Hidden in plain sight: medical visit companions as a resource for vulnerable older adults. Arch Intern Med. 2008;168(13): 1409–1415. [DOI] [PubMed] [Google Scholar]
- 27.Konrad TR, Link CL, Shackelton RJ, et al. It’s about time: physicians’ perceptions of time constraints in primary care medical practice in three National Healthcare Systems. Med Care. 2010;48(2):95–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kristjansson E, Hogg W, Dahrouge S, Tuna M, Mayo-Bruinsma L, Gebremichael G. Predictors of relational continuity in primary care: patient, provider and practice factors. BMC Fam Pract. 2013;14(1):72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wright M, Mainous AG III. Can continuity of care in primary care be sustained in the modern health system? Austr J Gen Pract. 2018;47(10):667–669. [DOI] [PubMed] [Google Scholar]
- 30.Dillman DA, Smyth JD, Christian LM. Internet, Mail, and Mixed- Mode Surveys: The Tailored Design Method. John Wiley & Sons Inc: New York, NY; 2009. [Google Scholar]
- 31.Caregiver assessment: Voices andviews from the field. Report from a National Consensus Development Conference. Volume II. San Francisco, CA: Family Caregiver Alliance; 2006. [Google Scholar]
- 32.Family Caregiver Alliance. Selected Caregiver Assessment Measures: A Resource Inventory for Practitioners. 2nd ed. San Francisco, CA: National Center on Caregiving; 2012. [Google Scholar]
- 33.Caregiver Assessment: Principles, Guidelines, and Strategies for Change. Volume I. San Francisco, CA: Family Caregiver Alliance; 2006. [Google Scholar]
- 34.Levine C. Putting the spotlight on invisible family caregivers. JAMA Intern Med. 2016;176(3):380–381. [DOI] [PubMed] [Google Scholar]
- 35.Primary Care providers’ Experiences with Family Caregivers. Washington, DC: AARP Public Policy Institute; 2019. [Google Scholar]
- 36.Yaffe MJ, Klvana J. Physician perspectives on the elderly patient-family caregiver-physician encounter. Isr Med Assoc J. 2002;4(10):785–789. [PubMed] [Google Scholar]
- 37.Advancing the Practice of Patient- and Family-Centered Care in Primary and Other Ambulatory Settings. Bethesda, MD: Institute for Patient- and Family-Centered Care; 2016. [Google Scholar]
- 38.Feinberg L. Moving toward Person- and Family-Centered Care. Washington, DC: AARP Public Policy Institute; 2012. [Google Scholar]
- 39.Van Houtven CH, Miller KE, O’Brien EC, et al. Development and initial validation of the caregiver perceptions about communication with clinical team members (CAPACITY) measure. Med Care Res Rev. 2019;76(6):784–806. [DOI] [PubMed] [Google Scholar]
- 40.Carpentier N, Bernard P, Grenier A, Guberman N. Using the life course perspective to study the entry into the illness trajectory: the perspective of caregivers of people with Alzheimer’s disease. Soc Sci Med. 2010;70(10): 1501–1508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Foundation TC. Family Caregiver Assessment in Health Care Settings: Summary of the Change Foundation’s Literature Review Adn Environmental Scan Project. The Change Foundation: Ontario, CA; 2016. [Google Scholar]
- 42.Forum NQ. NQF-Endorsed Measures of Person- and Family-Centered Care Phase 2. Washington, DC: Department of Health and Human Services; 2016. [Google Scholar]
- 43.Wosik J, Fudim M, Cameron B, et al. Telehealth transformation: COVID-19 and the rise of virtual care. J Am Med Inform Assoc. 2020;27(6):957–962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Reuben D, Levin J, Frank J, et al. Closing the dementia care gap: can referral to Alzheimer’s association chapters help? Alzheimers Dement. 2009;5(6): 498–502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bleich SN, Bennett WL, Gudzune KA, Cooper LA. National survey of US primary care physicians’ perspectives about causes of obesity and solutions to improve care. BMJ Open. 2012;2(6):e001871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ruiz R, Jeswani S, Andrews K, et al. Hoarseness and laryngopharyngeal reflux: a survey of primary care physician practice patterns. JAMA Otolaryngol Head Neck Surg. 2014;140(3):192–196. [DOI] [PubMed] [Google Scholar]
- 47.Garcia LC, Shanafelt TD, West CP, et al. Burnout, depression, career satisfaction, and work-life integration by physician race/ethnicity. JAMA Netw Open 2020;3(8):e2012762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Fingerman KL, Pillemer KA, Silverstein M, Suitor JJ. The baby boomers’ intergenerational relationships. Gerontologist. 2012;52(2):199–209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Olin SC, Kerker B, Stein RE, et al. Can postpartum depression be managed in pediatric primary care? J Womens Health (Larchmt). 2016;25(4):381–390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Lavelle B, Mancuso D, Huber A, Felver BEM. Expanding Eligibility for the Family Caregiver Support Program in SFY 2012: Updated Findings, 2014. Washington Department of Social and Health Services, Research and Data Analysis Division. http://leg.wa.gov/JointCommittees/ADJLEC/Documents/http://2014-05-19/Expanding_Eligibility_FCS_Report.pdf. Accessed August 4, 2020. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Appendix S1 Survey instrument.
Supplementary Table S1: Characteristics of Survey Respondents Compared to AMA Primary Care Physicians.