Abstract
Background
The 1998 Canadian clinical practice guidelines for the management of diabetes lowered the cutoff point for diagnosing diabetes mellitus from a fasting plasma glucose (FPG) level of 7.8 to 7.0 mmol/L. We studied the prevalence and clinical outcomes of undiagnosed and diagnosed diabetes within specific ranges of FPG among a cohort of subjects recruited in 1990.
Methods
In 1990 a representative sample of 2792 adult residents of Manitoba participated in the Manitoba Heart Health Survey, which included measurement of FPG and a question about each participant's past history of diabetes. Individuals who would now be classified as having undiagnosed diabetes under the new criteria were not considered as such in 1990. Through data linkage with the provincial health care utilization database, the use of health care by these individuals was tracked and compared with that of individuals whose diabetes had been diagnosed and with that of normoglycemic individuals over an 8-year period subsequent to the survey.
Results
The prevalence of undiagnosed diabetes in the adult population of Manitoba was 2.2%. Undiagnosed cases accounted for about one-third of all diabetes cases. Individuals with undiagnosed diabetes had an unfavourable lipid profile and higher blood pressure and obesity indices than normoglycemic individuals. Individuals who satisfied the new criteria for diabetes but remained undiagnosed had an additional 1.35 physician visits per year (95% confidence interval [95% CI] 0.93–1.96) and were more likely to be admitted to hospital at least once (odds ratio 1.23, 95% CI 0.40–3.79), compared with normoglycemic individuals.
Interpretation
Undiagnosed cases represent the unseen but clinically important burden of diabetes, with significant concurrent metabolic derangements and a long-term impact on health care use.
An individual with undiagnosed diabetes is someone whose diabetes has not been diagnosed by a physician but whose plasma glucose levels satisfy established criteria for diabetes. The most recent estimate of the burden of undiagnosed diabetes in the total population of the United States is 2.7% among adults aged 20 years and above, compared with 5.1% for diagnosed diabetes.1 It has also been shown in cross-sectional studies that undiagnosed diabetes is associated with a higher prevalence of hypertension, obesity, an unfavourable lipid profile and evidence of retinopathy and nephropathy when compared with values for normoglycemic individuals.2
Undiagnosed diabetes can only be detected in a survey or screening setting when individuals are tested for plasma glucose levels and are asked about a past history of physician-diagnosed diabetes. Under the 1985 World Health Organization (WHO) criteria, diabetes is defined by a fasting plasma glucose (FPG) level equal to or exceeding 7.8 mmol/L or a 2-hour post-challenge plasma glucose level equal to or exceeding 11.1 mmol/L, or both.3 In 1998 the Canadian clinical practice guidelines for the management of diabetes4 adopted the diagnostic criteria proposed by the American Diabetes Association (ADA) in 1997, which are based on the fasting value only, and lowered the cutoff point from 7.8 to 7.0 mmol/L. A new category of “impaired fasting glucose” (IFG) was created, encompassing individuals with FPG levels greater than or equal to 6.0 mmol/L but less than 7.0 mmol/L.5
A major difficulty in determining the clinical significance of undiagnosed diabetes prospectively is that once diabetes is detected, an individual is no longer “undiagnosed.” The change in diagnostic criteria proposed by the ADA and the Canadian practice guidelines, however, creates an opportunity to study the outcome of undiagnosed diabetes unaffected by clinical interventions.
In 1990 a representative sample of 2792 adult residents of Manitoba participated in a health and examination survey that included the measurement of FPG levels. This study identified subjects who would be classified as having undiagnosed diabetes under the new criteria, although their FPG level was not considered to be within the diabetic range in 1990. They constitute a unique cohort of individuals with undiagnosed diabetes to whom no special clinical interventions were directed.
This study used data linkage to determine the clinical significance of undiagnosed diabetes and also the predictive validity of the ADA criteria in a defined population of Canadians over a 10-year period.
Methods
This study involved linkage of 2 existing health data sets: the Manitoba Heart Health Survey (MHHS) and the Manitoba Health Services Insurance Plan (MHSIP).
The MHHS was a population-based cross-sectional survey that was conducted between October 1989 and February 1990 as part of a national effort to estimate the prevalence of cardiovascular risk factors and assess the level of knowledge about cardiovascular disease. Detailed descriptions of the design and methods of both the national study6 and the Manitoba survey7,8 have been published. The target population of the MHHS included all noninstitutionalized adult residents of the province aged 18–74 years. A stratified random sample was drawn from the registry of beneficiaries of the provincial health insurance plan. A total of 2792 individuals participated in the interviews, providing a response rate of 77%. Each participant was assigned a sampling weight, which was inversely proportional to the probability of selection.
In addition to a personal interview concerning past health history (including diabetes) and health behaviours (such as smoking, physical activity and alcohol use), participants underwent selected clinical measurements, including blood pressure and anthropometry, and laboratory tests to measure levels of FPG, glycosylated hemoglobin and lipids (total cholesterol, high-density lipoprotein [HDL], low-density lipoprotein and triglycerides). At the time of the survey, individuals with an FPG level that was greater than or equal to 7.8 mmol/L, considered as diabetes under the WHO criteria, were notified and advised to seek further evaluation and care by their own physicians. No specific instructions were given to individuals with an FPG level that was greater than or equal to 7.0 mmol/L but less than 7.8 mmol/L, individuals who would now also be considered as having diabetes.
The majority of physicians in Manitoba practise on a fee-for-service basis and receive payment from the provincial government by submitting a claim to the MHSIP for each patient's visit or each procedure performed. Salaried physicians also submit claims for monitoring purposes but do not receive payment. Such claims constitute the “medical file.” A separate “hospital file” exists for summaries of hospital discharges, including information on the patient, the attending physicians, the diagnoses and the procedures performed. Since there is no premium for health insurance in Manitoba, virtually all residents are registered with the MHSIP and receive their physician and hospital care free of charge. The MHSIP maintains and updates a population registry that contains dates of coverage. It is also possible to determine the date of death from the registry.
Data from the MHSIP claims database have been used in a substantial body of epidemiological and health services research.9 The accuracy, quality and research utility of this administrative database are well established.10,11 Although there are limitations, such as a lack of diagnostic precision, there are advantages including the comprehensive coverage of all health care contacts in a total population. MHSIP data have been used to study diagnosed diabetes specifically to estimate its prevalence and incidence and monitor its trend over time.12,13
MHHS data were linked with MHSIP data using a scrambled personal health insurance number (PHIN). Although personal identifying data on the survey forms were expunged from the MHHS data set, a retained sequence number permitted the linkage of the data back to the PHIN in the MHSIP population registry from which the MHHS survey sample was originally drawn. Data for 2674 (96%) of the 2792 subjects who participated in the interviews were successfully linked. Data from the MHSIP medical and hospital files for these individuals were extracted for 2 years prior to the MHHS survey date and for 8 years following the survey (from November 1, 1987, to November 30, 1997). Methodological papers on the linkage procedure have been published previously.14,15
Among the individuals included in the linked sample, 435 did not undergo any laboratory tests, and an additional 79 individuals had missing FPG values. Twenty-five individuals did not answer the question concerning their past history of diabetes. Two individuals were over 75 years old at the time of the survey, although they had not been at the time of selection. All these cases were deleted from the final data set, which comprised 2133 individuals, or 76% of the original sample of 2792 individuals. The proportion of interviewed subjects without measured FPG values is virtually identical (16%) among individuals who reported a past history of diabetes and those without past diabetes.
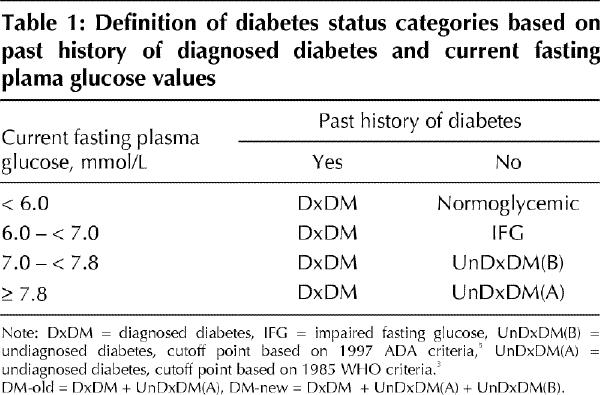
Two types of analyses were conducted: the first was cross-sectional, involving only the MHHS data set, and was designed to estimate the prevalence of diabetes and investigate the correlation of the various diabetes categories with selected metabolic indicators (plasma lipids, obesity and blood pressure), whereas the second was longitudinal, involving the linked MHHS–MHSIP data set, and was intended to compare health care use and other clinical outcomes for the various diabetes categories. Table 1 cross-tabulates past history of diabetes with current FPG levels to yield the various diabetes categories. The abbreviation DxDM refers to individuals with diagnosed diabetes. UnDxDM(A) refers to individuals with an FPG level that was greater than or equal to 7.8 mmol/L at the time of the survey. Although their diabetes was undiagnosed at the time, it ceased to remain so after the survey. The group referred to as UnDxDM(B) had an FPG level that was greater than or equal to 7.0 mmol/L but less than 7.8 mmol/L. Their condition remained undiagnosed after the survey. The abbreviation IFG refers to the group with impaired fasting glucose.
Table 1
In order to compare the data from Manitoba with those obtained for the US population according to the National Health and Nutrition Examination Survey of 1988–1994 (NHANES III), we computed age-standardized prevalence estimates using the 1980 US census population as standard.1
To measure health care utilization, we used 2 indicators: the mean number of consultations or physician visits per person-year of observation and the proportion of subjects with at least one stay in hospital during the period of observation. To determine whether the mean number of physician visits differed among the various categories of diabetes status, we performed multiple linear regression analyses, controlling for age and sex. Because the distribution of mean number of physician visits was highly skewed, we used logarithm-transformed values in the regression model, although we report the results as the number of physician visits. We used multiple logistic regression to compare the odds of being admitted to hospital at least once for the diabetes categories, controlling for age and sex.
To investigate whether the new criteria that lowered the cutoff point from 7.8 to 7.0 mmol/L affected clinical outcomes, we divided study subjects into 2 groups: diabetic and nondiabetic. Under the old criteria, the diabetic group (DM-old) comprised all cases of diagnosed diabetes (DxDM) and UnDxDM(A) cases; all other individuals were considered to be nondiabetic (non-DM). Under the new criteria, the diabetic group (DM-new) consisted of all DxDM, UnDxDM(A) and UnDxDM(B) individuals (Table 1). Cox proportional hazards analysis was used to compare the survival of nondiabetic and diabetic individuals (under the old and the new criteria) after adjusting for age and sex.
Results
The MHHS yielded 64 cases of undiagnosed diabetes, which corresponded to 15 580 individuals out of a total provincial adult population of 695 078, when weighting was taken into account (2.2%). Fig. 1 shows the age- and sex-specific prevalence of diagnosed diabetes (DxDM), undiagnosed diabetes (UnDxDM) and impaired fasting glucose (IFG) according to the 1997 ADA criteria. Among men aged 18–74 years, 2.2% (95% confidence interval [95% CI] 1.0%–3.3%) had undiagnosed diabetes, which was very similar to the prevalence of 2.3% among women (95% CI 1.0%–3.6%). Undiagnosed cases of diabetes accounted for 35% of all diabetes cases (DxDM and UnDxDM) among men, and 32% among women. Without the change in diagnostic criteria, 52% of the undiagnosed cases would not have been included in this category.
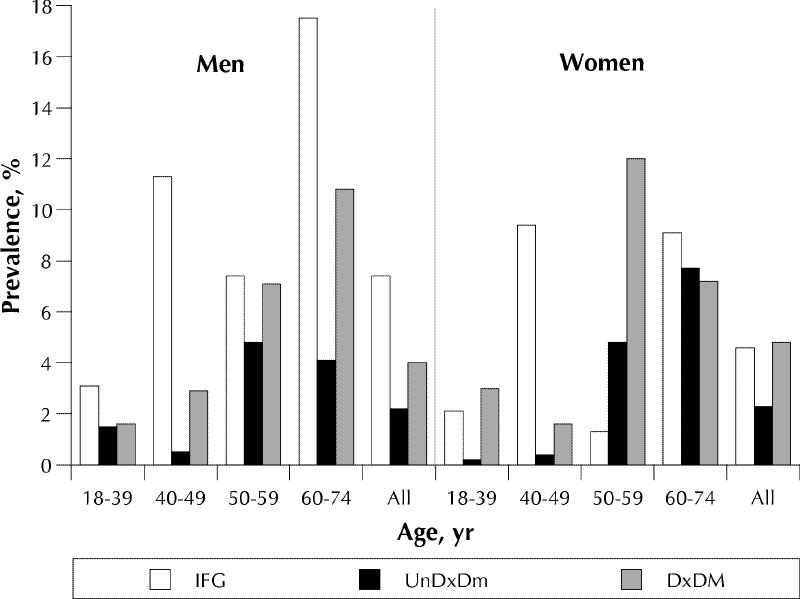
Fig. 1: Prevalence of diabetes and impaired fasting glucose in the adult population of Manitoba, according to the 1997 ADA criteria.5 IFG = impaired fasting glucose, UnDxDM = undiagnosed diabetes, DxDM = diagnosed diabetes.
When the 1980 US population was used as the standard, the Manitoba age-standardized prevalence of undiagnosed diabetes was 2.3% in men and 2.5% in women, compared with 3.1% in men and 2.5% in women in NHANES III.
Table 2 compares several key metabolic indicators for the different diabetes status categories. Normoglycemic individuals and those with IFG had lower mean FPG values than those with diagnosed diabetes. Individuals in the UnDxDM(A) group had higher values than those in the UnDxDM(B) group. Mean FPG values among the UnDxDM(A) group were higher than those among individuals with diagnosed diabetes (the DxDM group); the latter category included patients whose diabetes was being treated.
Table 2
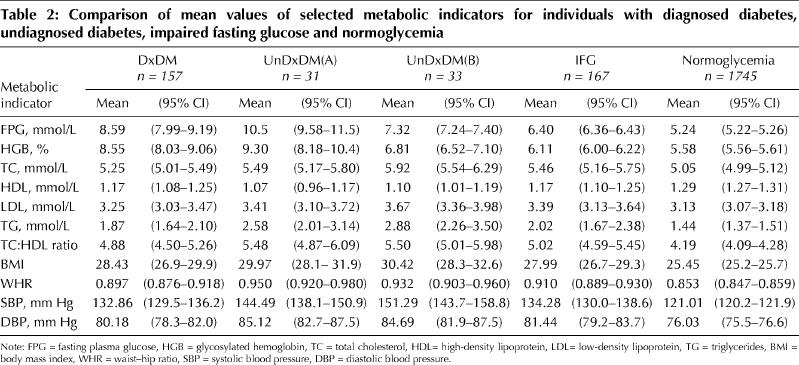
In general, individuals with undiagnosed diabetes had lower HDL cholesterol but higher triglycerides, total–HDL cholesterol ratio, glycosylated hemoglobin, body mass index, waist–hip ratio, and systolic and diastolic blood pressure than normoglycemic individuals. Compared with diagnosed cases, undiagnosed cases either did not differ significantly or had a worse metabolic profile (in terms of lipids, obesity, blood pressure). Comparing UnDxDM(A) and UnDxDM(B), there was no significant difference in any of the lipid, obesity or blood pressure measures.
The mean number of physician visits per year of observation was 4.83. A diagnosed case of diabetes accounted for an additional 1.49 visits (95% CI 1.17–1.91), compared with normoglycemic individuals, after controlling for age and sex. For undiagnosed diabetes cases, individuals in the UnDxDM(A) group had an additional 1.35 visits (95% CI 0.93–1.96); for the UnDxDM(B) group, the difference was 1.28 visits (95% CI 0.97–1.71).
We compared the odds of being admitted to hospital at least once for patients with undiagnosed diabetes and normoglycemic individuals. For the UnDxDM(A) group, the odds ratio (OR) was 1.23 (95% CI 0.40–3.79), whereas for the UnDxDM(B) group the OR was 2.07 (95% CI 0.62–6.87). As expected, people with diagnosed diabetes were at higher risk of being admitted to hospital than normoglycemic individuals (OR 1.90, 95% CI 1.08–3.36).
We found that diabetic individuals reported more physician visits than nondiabetic individuals. Using the new criteria, an individual with diabetes (DM-new) had an excess of 1.43 visits per year of observation (95% CI 1.16–1.76). With the old criteria, the excess was 1.42 visits (95% CI 1.18–1.71). Diabetic individuals were about twice as likely to have been admitted to hospital at least once. Comparing DM-new with non-DM individuals, the OR was 1.88 (95% CI 1.12–3.17); comparing DM-old with non-DM individuals, the OR was 1.76 (95% CI 1.09–2.83).
We also established the mortality rate of the entire cohort over the observation period. Fig. 2 compares the survival curves for DM-new, DM-old and non-DM individuals. Using Cox regression analysis, controlling for age and sex, we found that diabetic individuals were about twice as likely to die during the study period as nondiabetic individuals. Comparing DM-new with non-DM individuals, the hazard ratio was 1.93 (95% CI 1.38–2.70); comparing DM-old with non-DM, the hazard ratio was also 1.93 (95% CI 1.35–2.75). Because of the small number of events, we did not compare specific causes of death.
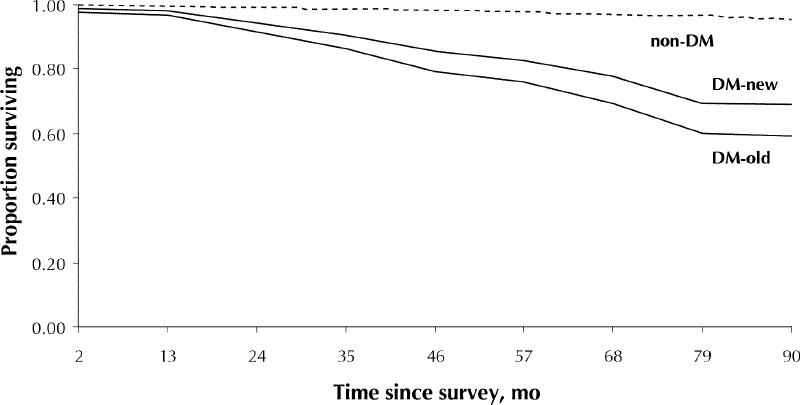
Fig. 2: Probability of survival among survey cohort members. Non-DM = nondiabetic individuals, DM-new = all individuals considered to have diabetes according to the new criteria,4 DM-old = all individuals considered to have diabetes according to the old criteria.3
Interpretation
Our data show that about 2% of the adult population (aged 18–74 years) of Manitoba have undiagnosed diabetes, based on the 1998 Canadian practice guidelines. Undiagnosed diabetes cases comprise about one-third of all diabetes cases. These data are comparable with those reported from the United States.1 Undiagnosed diabetes represents the unseen burden of a disease that is increasingly recognized as an important public health problem in the developed world.
Should we be concerned about this unseen burden and should any efforts be expended to identify undiagnosed cases of diabetes? We are able to establish the clinical significance of undiagnosed diabetes by showing the unfavourable lipid profile and higher blood pressure levels and obesity indices present in individuals with this condition at the time of its discovery. We were not able to detect a significant difference in clinical outcome between individuals who remained undiagnosed and normoglycemic individuals, using the indicators of mean number of physician visits per year and the odds of being admitted to hospital at least once during the study period.
The Canadian clinical practice guidelines recommend screening for all adults aged 45 years and over,4 although the health benefits of screening have not been established by a randomized controlled trial, and the justification for screening has been challenged.16 The decision to screen requires information on the burden of undiagnosed diabetes, its association with metabolic risk factors and potential long-term morbidity, as well as the costs and adverse effects of screening itself.17
There has been considerable discussion in the literature of the merits and pitfalls of the new ADA criteria.18,19 Our data indicate that the new criteria, by lowering the cutoff point of FPG, almost double the prevalence of undiagnosed diabetes. The new criteria, however, are as capable as the old of predicting increased morbidity and mortality among diabetic compared with nondiabetic individuals.
Because of the importance of glycosylation in the development of microvascular complications, it has been argued that individuals with an FPG level of 7.0–7.7 mmol/L without elevated levels of glycosylated hemoglobin should not be considered as having diabetes.20 Our data (Table 2) indicate that individuals with undiagnosed diabetes, even those with an FPG level of 7.0–7.7 mmol/L, have elevated glycosylated hemoglobin (6.81% [95% CI 6.52%–7.10%]) compared with normoglycemic individuals (5.58% [95% CI 5.56%–5.61%]) and thus are at risk for microvascular complications.
The use of data linkage to study the long-term clinical outcome of undiagnosed diabetes is less time-consuming and expensive than a true follow-up study requiring repeat examinations of survey cohort members. We were able to exploit the opportunity for a “natural experiment” created by the change in diagnostic criteria, allowing the pattern of health care use by individuals with undiagnosed diabetes to be monitored without their being subjected to increased clinical surveillance or interventions. It is anticipated that with a longer study period (and a larger number of person-years) of observation, we should be able to further explore clinical outcomes using more specific diagnostic categories beyond overall measures of health care use.
Footnotes
This article has been peer reviewed.
Acknowledgements: Dr. Young is a Medical Research Council of Canada Senior Scientist and Dr. Mustard is a Medical Research Council of Canada Scientist. This project was supported by a grant from the Canadian Diabetes Association in honour of Blanche Gunning.
Competing interests: None declared.
Reprint requests to: Dr. T. Kue Young, Department of Community Health Services, University of Manitoba, 750 Bannatyne Ave., Winnipeg MB R3E 0W3; fax 204 789-3905; tkyoung@cc.umanitoba.ca
References
- 1.Harris MI, Flegal KM, Cowie CC, Eberhardt MS, Goldstein DE, Little RR, et al. Prevalence of diabetes, impaired fasting glucose, and impaired glucose tolerance in U.S. adults. Diabetes Care 1998;21:518-24. [DOI] [PubMed]
- 2.Harris MI. Undiagnosed NIDDM: clinical and public health issues. Diabetes Care 1993;16:642-52. [DOI] [PubMed]
- 3.World Health Organization. Expert Committee on Diabetes Mellitus. Second report. Geneva: The Organization; 1985. [PubMed]
- 4.Meltzer S, Leiter L, Daneman D, Gerstein HC, Lau D, Ludwig S, et al. 1998 clinical practice guidelines for the management of diabetes in Canada. CMAJ 1998;159(8 Suppl):S1-29. Available: www.cma.ca/cmaj/vol-159/issue-8/diabetescpg/index.htm [PMC free article] [PubMed]
- 5.American Diabetes Association. Preport of the Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Diabetes Care 1997;20:1183-97. [DOI] [PubMed]
- 6.MacLean DR, Petrasovits A, Nargundkar M, Connelly PW, MacLeod E, Edwards A, et al. Canada heart health surveys: a profile of cardiovascular risk. Survey methods and data analysis. CMAJ 1992;146(11):1969-76. [PMC free article] [PubMed]
- 7.Gelskey DE, Young TK, Macdonald SM. Screening with total cholesterol: determining sensitivity and specificity of the National Cholesterol Education Program's guidelines from a population survey. J Clin Epidemiol 1994;47:547-53. [DOI] [PubMed]
- 8.Young TK, Gelskey DE. Is non-central obesity metabolically benign? Implications for prevention from a population survey of Canadians. JAMA 1995; 274:1939-41. [PubMed]
- 9.Roos NP, Shapiro E, editors. Health and health care: experience with a population-based health information system. Med Care 1995;33(12 Suppl):DS1-146. [PubMed]
- 10.Roos LL, Mustard CA, Nicol JP, McLerran DF, Malenka DJ, Young TK, et al. Registries and administrative data: organization and accuracy. Med Care 1993;31:201-12. [DOI] [PubMed]
- 11.Roos LL, Nicol JP. A research registry: uses, development, and accuracy. J Clin Epidemiol 1999;52:39-47. [DOI] [PubMed]
- 12.Young TK, Roos NP, Hammerstrand KM. Estimated burden of diabetes mellitus in Manitoba according to health insurance claims: a pilot study. CMAJ 1991;144(3):318-24. [PMC free article] [PubMed]
- 13.Blanchard JF, Ludwig S, Wajda A, Dean H, Anderson K, Kendall O, et al. Incidence and prevalence of diabetes in Manitoba, 1986–1991. Diabetes Care 1996;19:807-11. [DOI] [PubMed]
- 14.Robinson JR, Young TK, Roos LL, Gelskey DE. Estimating the burden of disease: comparing administrative data and self reports. Med Care 1997;35: 932-47. [DOI] [PubMed]
- 15.Muhajarine N, Mustard C, Roos LL, Young TK, Gelskey DE. Comparison of survey and physician claims data for detecting hypertension. J Clin Epidemiol 1997;50:711-8. [DOI] [PubMed]
- 16.Marshall KG. The folly of population screening for type 2 diabetes. CMAJ 1999;160(11):1592-3. Available: www.cma.ca/cmaj/vol-160/issue-11/1592.htm [PMC free article] [PubMed]
- 17.CDC Diabetes Cost-Effectiveness Study Group. The cost-effectiveness of screening for type 2 diabetes. JAMA 1998;280:1757-63. [PubMed]
- 18.McCance DR, Hanson RL, Pettitt DJ, Bennett PH, Haddren DR, Knowler WC. Diagnosing diabetes mellitus — do we need new criteria? Diabetologia 1997;40:247-55. [DOI] [PubMed]
- 19.Unwin N, Alberti KG, Bhopal R, Harland J, Watson W, White M. Comparison of the current WHO and new ADA criteria for the diagnosis of diabetes mellitus in three ethnic groups in the UK. Diabet Med 1998;15:554-7. [DOI] [PubMed]
- 20.Davidson MB, Shriger DL, Peters AL, Lorber L. Relationship between fasting plasma glucose and glycosylated hemoglobin: potential for false-positive diagnoses of type 2 diabetes using new diagnostic criteria. JAMA 1999; 281:1203-10. [DOI] [PubMed]


