Abstract
This survey study assessed surgeons’ preference for total thyroidectomy vs lobectomy to treat patients with papillary thyroid cancer.
The incidence of papillary thyroid cancer has increased in the past 25 years without a clear increase in thyroid cancer deaths.1 Given these findings, there has been a shift toward recommending conservative surgical options, with current management guidelines favoring lobectomy, especially for patients with papillary thyroid microcarcinoma.2 Despite these recommendations, some studies have reported an increasing number of total thyroidectomies performed for small tumors, even with equivocal oncologic outcomes.3 The aim of this study is to identify surgeons’ attitudes regarding surgical management of microcarcinomas with the hypothesis that surgeons consider other factors, in addition to tumor size, when selecting a surgical procedure.
Methods
This survey study was approved by the institutional review boards of the University of Michigan, the University of Southern California, Los Angeles, and Emory University as well as the Committee for the Protection of Human Subjects, the Georgia Department of Public Health, and the California Cancer Registry. A waiver of written informed consent was obtained from all participants because a returned completed survey serves as implied consent to participate. Treating surgeons for patients with differentiated thyroid cancer were identified from the Surveillance, Epidemiology, and End Results (SEER) registries of Georgia and Los Angeles Counties. Between October 2018 and August 2019, surveys were mailed to 264 thyroid cancer surgeons. More detail on the survey methods, including the use of the modified Dillman method, has been published elsewhere.4 As a part of the survey, surgeons were presented with the following vignette: “A 40-year-old female patient presents to your office after an FNA [fine-needle aspiration] of a 0.9-cm right thyroid nodule was consistent with papillary thyroid cancer. No suspicious lymph nodes were seen on ultrasound evaluation.” Surgeons were asked which of 4 treatments they would offer the patient (Figure 1). They were then asked which factors would lead them to recommend total thyroidectomy over thyroid lobectomy for a 1-cm papillary thyroid tumor (Figure 2). Logistic regression was performed, and specialty, practice setting, years in practice, reading guidelines, and thyroid cancer case volume in the past year were included as covariates.
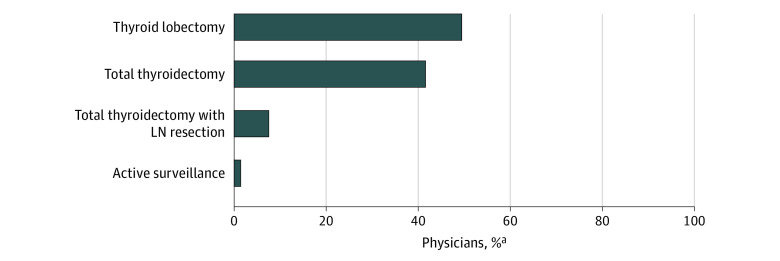
Figure 1. Surgeon-Reported Treatment of Papillary Thyroid Microcarcinoma.
Surgeon-reported use of thyroid lobectomy, total thyroidectomy, total thyroidectomy with lymph node (LN) dissection, and active surveillance for treatment of papillary thyroid microcarcinoma.
aPercentages are weighted to account for nonresponses.
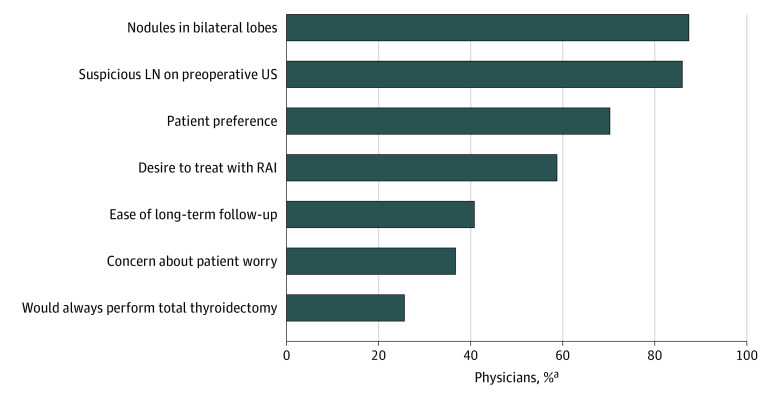
Figure 2. Reasons That Surgeons Recommend Total Thyroidectomy vs Lobectomy for a 1-cm Papillary Thyroid Tumor.
Surgeons reported the following reasons for their recommendation of total thyroidectomy: nodules in bilateral lobes (87.4%), suspicious lymph node (LN) on preoperative ultrasonography (US) (86.0%), patient preference (70.3%), desire to treat with radioactive iodine (RAI) (58.8%), ease of long-term follow-up (40.8%), concern about patient worry (36.7%), and would always perform total thyroidectomy (25.6%).
aPercentages are weighted to account for nonresponses.
Statistical analyses were performed using Stata, version 15.1 (StataCorp LLC) and R, version 4.0.2 (R Foundation for Statistical Computing). These analyses incorporated weighted percentages to account for nonresponses.
Results
The cohort is a subset of a larger cohort of 699 endocrinologists and surgeons who were surveyed; 448 responses were received yielding a response rate of 69.0%. Of 264 surgeons surveyed in this cohort, 134 (51.4%) were general surgeons and 130 (48.6%) otolaryngologists. A total of 150 (57.4%) were in private practice and 74 (27.4%) reported treating more than 20 patients with thyroid cancer in the past year. In response to the clinical vignette involving a 0.9-cm papillary thyroid tumor, many surgeons recommended either a total thyroidectomy (108 [41.6%]) or a total thyroidectomy with lymph node resection (20 [7.5%]), whereas 129 surgeons (49.4%) recommended a thyroid lobectomy (Figure 1). When surveyed about 7 reasons for recommending a total thyroidectomy vs thyroid lobectomy, the most frequently chosen reason was the presence of nodules in the other lobe (231 surgeons [87.4%]) followed by suspicious lymph nodes (227 [86.0%]) and patient preference (185 [70.3%]) (Figure 2). In the multivariable models, physicians in practice for more than 20 years (150 physicians [57.4%%]) were less likely than those in practice for less than 20 years (112 [42.6%]) to perform a total thyroidectomy based on ease of long-term follow-up (OR, 0.53; 95% CI, 0.31-0.91), patient preference (OR, 0.21; 95% CI, 0.11-0.43), or because of patient worry (OR, 0.52; 95% CI, 0.29-0.91). Interestingly, 68 surgeons (25.6%) would “always perform a total thyroidectomy.” In the multivariable analysis, physicians who treated more than 20 patients with thyroid cancer in the last year compared with surgeons who treated 0 to 10 patients were less likely to “always perform a total thyroidectomy” (OR, 0.36; 95% CI, 0.16-0.82). No other variables were statistically significant in the models.
Discussion
The rationale for a surgeon to recommend a total thyroidectomy rather than a lobectomy in the absence of adverse features, such as nodal disease, is varied and includes the presence of nodules in the contralateral lobe and patient preference. Despite previous work suggesting that observation of contralateral low-risk nodules is safe, most surgeons still report bilateral nodules as a reason to perform a total thyroidectomy.5 However, this study has limitations. Similar to most survey studies there is a risk of recall bias. Despite this limitation, thyroid surgery is not without its risks; thus, limiting the extent of surgery without sacrificing oncologic outcomes is paramount.6 Understanding the factors involved in surgeon recommendations is important, especially with evolving evidence and guidelines.
References
- 1.Davies L, Welch HG. Increasing incidence of thyroid cancer in the United States, 1973-2002. JAMA. 2006;295(18):2164-2167. doi: 10.1001/jama.295.18.2164 [DOI] [PubMed] [Google Scholar]
- 2.Haugen BR, Alexander EK, Bible KC, et al. 2015 American Thyroid Association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: the American Thyroid Association Guidelines Task Force on thyroid nodules and differentiated thyroid cancer. Thyroid. 2016;26(1):1-133. doi: 10.1089/thy.2015.0020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Welch HG, Doherty GM. Saving thyroids—overtreatment of small papillary cancers. N Engl J Med. 2018;379(4):310-312. doi: 10.1056/NEJMp1804426 [DOI] [PubMed] [Google Scholar]
- 4.Papaleontiou M, Zebrack B, Reyes-Gastelum D, et al. Physician management of thyroid cancer patients’ worry. J Cancer Surviv. 2020. doi: 10.1007/s11764-020-00937-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ritter A, Bachar G, Hirsch D, et al. Natural history of contralateral nodules after lobectomy in patients with papillary thyroid carcinoma. J Clin Endocrinol Metab. 2018;103(2):407-414. doi: 10.1210/jc.2017-01616 [DOI] [PubMed] [Google Scholar]
- 6.Papaleontiou M, Hughes DT, Guo C, Banerjee M, Haymart MR. Population-based assessment of complications following surgery for thyroid cancer. J Clin Endocrinol Metab. 2017;102(7):2543-2551. doi: 10.1210/jc.2017-00255 [DOI] [PMC free article] [PubMed] [Google Scholar]