Abstract
Objective
The transition from pediatric to adult rheumatology care represents a particularly vulnerable time for patients with juvenile idiopathic arthritis (JIA) and childhood‐onset systemic lupus erythematosus (cSLE). Improving self‐management skills is important in optimizing health care transition. The study’s objectives were to 1) examine variability in transition readiness of adolescents and young adults within and between different ages, sexes, and disease types; 2) determine the association between age and transition readiness; and 3) identify specific challenges to transition readiness for adolescents.
Methods
Over 1 year, patients 14 to 20 years of age with JIA or cSLE were recruited from pediatric transition and young adult clinics at a single academic institution. Participants completed the 14‐item Transition‐Q at a single time point. Total scores range from 0 to 100; higher scores indicate greater health care self‐management skills as a proxy for transition readiness. Descriptive statistics summarized patient characteristics and Transition‐Q scores for the population. Regression analyses determined the association between age, sex, and disease type and Transition‐Q score.
Results
Among 70 participants, 61 had JIA and 9 cSLE (mean disease duration 4.6 years). The mean (SD) total Transition‐Q score was 59.8 (14.9). Age was significantly associated with Transition‐Q score (standardized β = 0.372l P = 0.002). The most commonly reported challenges were seeing the physician alone (without parents), making one’s own appointments, picking up prescriptions, and independent transportation for appointments.
Conclusion
Transition readiness appears to increase with patient age. There is significant variability in Transition‐Q scores between patients of the same age, suggesting that an individualized approach to improving self‐management skills is necessary.
Significance & Innovations.
Transition readiness in juvenile idiopathic arthritis and childhood‐onset systemic lupus erythematosus can be evaluated by using the Transition‐Q, a validated tool to measure health care self‐management skills that can be feasibly implemented into clinical practice.
Readiness for transition from pediatric to adult rheumatology care increased with patient age, with large variability in transition readiness scores, especially in those aged 16 and 17 years.
An individualized approach rather than an age‐based approach to improving self‐management skills is necessary to meet the needs of adolescents with chronic rheumatic conditions.
Introduction
Health care transition is defined as “the purposeful, planned movement of adolescents and young adults with chronic physical and medical conditions from child‐centered to adult‐oriented health care systems” (1). This transition is a complex process that occurs over time, not simply an administrative transfer that occurs after referral to an adult physician. For children with any chronic health condition such as cerebral palsy, diabetes or pediatric‐onset rheumatic disease, the transition from pediatric to adult care is inevitable. Considering that pediatric‐onset rheumatic disease can be more severe than adult‐onset disease (2,3), it is critical that optimal care continues across the transition period into early adulthood. For patients with juvenile idiopathic arthritis (JIA) and childhood‐onset systemic lupus erythematosus (cSLE), the transition period has been associated with increased risk of poor symptom and disease control, morbidity, and mortality (4, 5, 6, 7, 8, 9). Adults with JIA may struggle with activities of daily living compared with the general population (10), and adults with cSLE have two to three times the mortality rate of those with adult‐onset systemic lupus erythematosus, with rates peaking in young adulthood (4). This is a critical time to ensure that patients are engaged in their care, have adequate access to health care, and understand the increasing expectation for them to manage their own care.
Effective transition planning can increase a patient’s ability to manage their disease, thus improving short‐ and long‐term disease outcomes (10). Unfortunately, in rheumatic disease, approximately 50% of transfers to adult care are not successful because of loss to follow‐up or poor adherence to treatment (3). This leaves patients at high risk for unfavorable outcomes, most of which are preventable (5,7). In an effort to address these challenges, transition programs have been created with the goal of minimizing the number of patients lost to follow‐up in adult care and trying to improve the independence and skills of youth in managing their own care. A variety of transition programs have been described in the literature, including those that provide a shared care model between adult and pediatric rheumatology, those that provide a multidisciplinary team approach, and those that include a social worker or nurse coordinator.
Factors key to optimizing transition in patients with chronic health conditions include starting transition programs in early adolescence, co‐managing/coordinating care between pediatric and adult teams, sharing medical records, and providing education on self‐management and advocacy (11,12). Previous literature indicates that more than 50% of adolescents aged 12‐18 years with a variety of chronic health conditions lack basic skills to manage their own health (13). A patient’s ability to self‐manage is reflective of their readiness to transition and is important in determining transition success (9).
There are a variety of assessment tools that measure transition readiness in pediatric patients (2,14,15). Ideally, such a tool would be validated, easily and relatively quickly self‐administered, simple for adolescents to answer, widely available, and able to measure change over time. One such tool, known as the Transition‐Q, is a validated 14‐item questionnaire that can be administered in paper or by using the MyTransition application available free for download. Although this questionnaire has been used in chronic disease, it has never before been used in a rheumatology setting. Thus, the Transition‐Q is a novel tool capable of measuring transition readiness and fulfills these criteria.
The objectives of this study were to 1) examine variability in transition readiness using the Transition‐Q in adolescents and young adults within and between different ages, sexes, and disease types; 2) determine the association between age and transition readiness using the Transition‐Q; and 3) identify specific challenges to transition readiness for adolescents.
Patients and Methods
All individuals 14 to 20 years of age with JIA or cSLE who were seen in the McMaster Rheumatology Transition Clinic (14‐18 years old) or Young Adult Clinic (18‐20 years old) between January 2019 and March 2020 were invited to participate. The Rheumatology Transition Clinic is a multidisciplinary clinic where patients are seen by both an adult rheumatologist and a pediatric rheumatologist at the same time, as well as a nurse, physiotherapist, and child‐life specialist. The Young Adult Clinic is staffed by the same adult rheumatologist who saw the patient in the transition clinic. Both clinics are housed in the same health center associated with McMaster University, an academic tertiary care facility. Patients in the Young Adult Clinic had previously been patients in the transition clinic prior to turning 18. Individuals were excluded if they were 1) unable to read or understand English or 2) entirely dependent on caregivers for daily functioning, self‐care, and/or communication. Ethics approval was obtained from the Hamilton Integrated Research Ethics Board (2019‐5479‐GRA).
Pediatric and adult rheumatologists identified all eligible consecutive participants and directed them to the research assistant who explained the study objectives, procedures, and obtained informed written consent. Demographic data, disease duration, and comorbid nonrheumatic conditions were collected from patients’ charts. An active joint count and a physician global assessment, a reliable, validated outcome used to describe disease activity in these patients (11), were also collected on each patient.
In this cross‐sectional study, participants were given a paper version of the Transition‐Q to complete as they waited for the physicians to see them in the clinic. The Transition‐Q was designed to support youth with chronic disease who are moving from pediatric to adult care. As a proxy for transition readiness, it is a validated questionnaire that measures health care self‐management skills in adolescents with chronic health conditions (16,17). In increasing order from easy to difficult, the Transition‐Q poses 14 questions to which adolescents/young adults respond “never,” “sometimes,” or “always.” Responses are transformed to a score out of 100, with higher scores indicating greater self‐management skills (16,18).
Descriptive statistics were used to characterize our study population and to determine the variability of Transition‐Q scores within and between age groups. Potential differences in scores between sexes and disease types were analyzed by using linear regression analyses controlling for age and disease duration. We also determined the frequency of responses to each individual question on the Transition‐Q to identify potential areas of challenge or need.
Results
Seventy of 71 individuals who were approached to participate provided informed written consent. Characteristics of the participants are summarized in Table 1. The majority was female (69%) and had JIA (87%). The age distribution was as follows: 14 years, n = 8; 15 years, n = 6; 16 years, n = 20; 17 years, n = 24; 18 years, n = 10; 19 years, n = 1; 20 years, n = 1. The mean total Transition‐Q score for the entire study population was 59.8 (SD 15.0). Transition‐Q scores as they relate to age are shown in Figure 1. Age had a significant positive association with the total Transition‐Q score (standardized β = 0.364; P = 0.002).
Table 1.
Descriptive characteristics (N = 70)
| Mean (SD) or n (%) | Range | |
|---|---|---|
| Age, years | 16.4 (1.3) | 14‐20 |
| Female sex | 48 (69%) | – |
| Diagnosis | ||
| JIA | 61 (87.1%) | – |
| cSLE | 9 (12.9%) | – |
| Age at diagnosis, years | 11.7 (4.7) | 1‐18 |
| Disease duration, years | 4.7 (4.6) | 0‐16 |
| Transition‐Q score | 59.8 (15.0) | 31‐100 |
| PGA (n = 62) | 0.3 (0.8) | 0‐5 |
| Active joint count | 0.13 (0.41) | 0‐2 |
| Comorbid conditions a | 9 (12.9%) | – |
Percentage is rounded to the nearest 0.1. SD is rounded to the nearest 0.1.
Abbreviations: cSLE, childhood‐onset systemic lupus erythematosus; JIA, juvenile idiopathic arthritis; PGA, physician global assessment.
Examples of comorbid conditions include thyroid disease, type 1 diabetes, and asthma.
Figure 1.
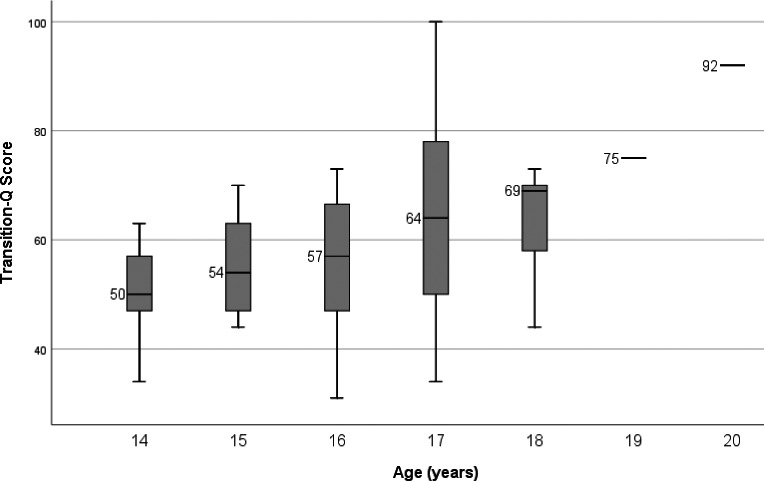
Median total Transition‐Q scores by age.
Female participants had a mean (SD) total Transition‐Q score of 62.3 (14.5), whereas male participants had a mean (SD) total Transition‐Q score of 54.4 (14.8). After controlling for age and disease duration, there was no significant difference in Transition‐Q scores between female and male participants. The mean (SD) total Transition‐Q score was 58.7 (15.1) among those with JIA and 67.9 (11.0) among those with cSLE. Given the small number of adolescents with cSLE (n = 9), we did not perform a statistical analysis of differences. We also did not take disease activity into consideration in our analyses because there was so little variability in our population.
Frequencies of responses to each question on the Transition‐Q are summarized in Table 2. The majority of participants (78.6%) always answered the doctor’s or nurse’s questions. However, most participants (82.9%) responded “never” to “I travel on my own to a doctor’s appointment.” Approximately half (47.1%) of the participants responded “never” to “I contact a doctor when I need to.” More than half (58.6%) of participants responded “never” to “I drop off or pick up prescriptions on my own” and “I book my own doctors’ appointments.”
Table 2.
Individual Transition‐Q responses
|
Never % |
Sometimes % | Always % | |
|---|---|---|---|
| Q.1 Answer questions | 0 | 21.4 | 78.6 |
| Q.2 Make my own health decisions | 4.3 | 25.7 | 68.6 |
| Q.3 In charge of medications | 7.1 | 32.9 | 60.0 |
| Q.4 Talk about health concerns | 5.7 | 40.0 | 54.3 |
| Q.5 Look for an answer about my health | 2.9 | 37.1 | 60.0 |
| Q.6 Talk about my health conditions | 4.3 | 35.7 | 60.0 |
| Q.7 Ask questions | 10.0 | 37.1 | 52.9 |
| Q.8 Speak to the doctor instead of my parent(s) | 2.9 | 47.1 | 50.0 |
| Q.9 Summarize my medical history | 11.4 | 25.7 | 62.9 |
| Q.10 Contact a doctor | 47.1 | 21.4 | 31.4 |
| Q.11 On my own during appointment | 60.0 | 30.0 | 10.0 |
| Q.12 Get own prescriptions | 58.6 | 18.6 | 22.9 |
| Q.13 Travel to appointment on my own | 82.9 | 14.3 | 2.9 |
| Q.14 Book my own appointments | 58.6 | 28.6 | 12.9 |
Correction added on 10 April 2021, after first online publication: Table 2 was updated with alternate wording as a result of copyright concerns.
Discussion
Adolescents with JIA and cSLE will inevitably need to be transitioned to adult care given the chronicity of these conditions. Supporting these adolescents in preparation for and through the transition period is of paramount importance and should begin with understanding their baseline level of health care self‐management skills so that efforts can be made to improve from there. This is the first study to examine transition readiness using the Transition‐Q in an adolescent and young adult rheumatology population.
Our results revealed that mean total Transition‐Q scores increased with age, suggesting that older adolescents have higher levels of self‐management skills than younger adolescents. Participants who are older have generally had longer exposure to our transition clinics because they would have started attending these clinics at the age of 14 years (if diagnosed prior to age 14) or soon after the time of diagnosis (if diagnosis occurred after age 14). In attending the transition clinics, patients were likely involved in conversations related to transition readiness and preparing for adult care, which may have contributed to the increased Transition‐Q scores relative to age. This could be secondary to increased self‐efficacy, societal expectations, and responsibility that increase with age. Adolescence is a time of significant physical development and neurodevelopment, which is often not recognized by health care providers. The limbic system, responsible for reward processing and pleasure seeking, matures before the prefrontal cortex, which is responsible for higher executive functioning. It is thought that planning, emotional regulation, judgement, and self‐awareness are skills that continue developing until age 25. Thus, given that advanced self‐management skills, such as transportation to appointments and picking up prescriptions, require a more mature level of planning and independence, this likely explains why these skills have yet to be developed in younger teens.
Although 78.6% of participants answered that they always answer a doctor’s or nurse’s questions, only 52% responded “always” to “I speak to the doctor instead of my parents speaking for me.” Perhaps this indicates that adolescents are responding to questions when directly asked by the health care provider, yet they do not feel as comfortable or as confident in initiating conversation and so leave this to their parents. In recognizing this, health care professionals may be able to foster active participation in the encounter by interacting primarily with the adolescent to encourage engagement, independence, and responsibility.
A study examining transition readiness using the Transition‐Q in similarly aged adolescents with chronic heart disease found a mean total Transition‐Q score of 63.0 (range 31‐92) (14), which is similar to our findings of 59.7 (range 31‐100). In both studies, patients answered “never” most frequently to “I travel on my own to a doctor’s appointment,” “I drop off or pick up my prescriptions when I need medicine,” and “I see the doctor or nurse on my own during an appointment.” Interestingly, 58.6% of patients in our study never booked their own doctor’s appointments, compared with 12% in the study by Ekim et al, which included younger patients (14). Although this could be secondary to differences in booking methods at the respective sites, this is an area that warrants further query. Responses to the Transition‐Q could be used to identify potential disease or site‐specific barriers to self‐management skills and areas for improvement and subsequent goal setting.
Previous literature has shown that another self‐management score, the Transition Readiness Assessment Questionnaire (TRAQ), was not associated with age in patients with chronic rheumatic, endocrine, and gastrointestinal conditions (15). In our study, the total Transition‐Q score increased with age. Our study examined patients 14 to 20 years of age, compared with 16 to 23 years of age in the Jensen et al study (15). The discrepancy in results may be due to differences in questions between the Transition‐Q and TRAQ. The TRAQ measures a broader skill set within two domains, including skills for chronic condition self‐management and skills for self‐advocacy and health care use. In contrast, the Transition‐Q focuses solely on self‐management skills. The differences could also be attributable to transition readiness having more variability in younger age groups. Although the study by Jensen et al comprised 56% rheumatic patients, the difference in results could also be reflective of differences seen in other chronic disease groups. A study examining transition readiness using the TRAQ in young adults aged 17 to 21 years with JIA, cSLE, and mixed connective tissue disease found older age to be significantly associated with higher transition readiness scores (19).
We found that there was no difference in total Transition‐Q scores in male compared with female participants. Previous literature examining transition readiness and sex found results similar to that in our study. Jensen et al found that transition readiness, as measured by the TRAQ, was not associated with sex. Other studies have found an association between higher TRAQ scores and female participants (19). They attribute this to increased self‐reported autonomy among female participants, which allows for better engagement in their health care (19). Although our results did not show statistically significant sex differences in Transition‐Q scores after we accounted for age, our smaller sample of male participants (n = 31%) may be a contributing factor to this lack of difference.
We recognize that other factors, in addition to age and sex, may impact transition readiness. A recent review investigating the potential association between transition readiness and both nonmodifiable (eg, demographic/ecological and disease factors) and modifiable (eg, psychosocial and self‐management/transition education factors) factors in 33 studies of youth with various chronic diseases (20) reported age (older) and sex (female) to be consistently associated with greater readiness. In the two studies that focused solely on rheumatology patients, only one other factor, greater health literacy, was correlated with higher transition readiness. Other factors identified in 76 pediatric rheumatology patients as being associated with increased self‐perceived autonomy (not specifically transition readiness) include a younger parent, having a family member with a similar disease, longer disease duration, having a comorbid nonrheumatic diagnosis, and having had a summer job (3). The question of whether disease activity is associated with or predictive of transition readiness in rheumatology patients has yielded inconsistent results (5,8,21,22) and must be examined in larger studies with variable disease activity in the population.
Limitations to the study include the relatively small sample size of 70 patients and the few numbers of patients at each end of the age spectrum (14 years old and 19‐20 years old). Given that the study was completed in a single tertiary care center, results may not be generalizable to all patients with JIA or cSLE. Indeed participants aged 18 years or older had previously been patients in the transition clinic and, thus, had been exposed to the multidisciplinary team and discussions about health care self‐management skills. Additionally, we did not collect data on the race, socioeconomic status, or reading level of the child, limiting our ability to investigate the association between these factors and transition readiness. Future research considerations would include investigation of changes in Transition‐Q scores over time in response to specific interventions (eg, targeted goal setting) and the collection of additional sociodemographic factors that may be associated with or may predict these changes. Clinically it would be beneficial to identify participants with low scores early in their transition journey to provide additional supports through the transition to adult care. Further studies may also examine the difference between transition readiness as reported by the patient and parent‐perceived transition readiness in the adolescent.
This study examined transition readiness using the Transition‐Q measure of health care self‐management skills. Readiness for transition from pediatric to adult rheumatology care increased with patient age. However, the large variability in transition readiness scores, especially in those aged 16 and 17, suggests that an individualized approach rather than an age‐based approach to improving self‐management skills is necessary to meet the needs of patients. Next steps include examining the trajectory of Transition‐Q scores over time within individuals and determining how transition management skills change as adolescents travel through the transition process.
Author contributions
All authors were involved in drafting the article or revising it critically for important intellectual content, and all authors approved the final version to be published. Dr. Batthish had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study conception and design
McColl, Semalulu, Beattie, Alam, Thomas, Herrington, Gorter, Cellucci, Garner, Heale, Matsos, Batthish.
Acquisition of data
McColl, Semalulu, Beattie, Alam, Thomas, Herrington, Gorter, Cellucci, Garner, Heale, Matsos, Batthish.
Analysis and interpretation of data
McColl, Semalulu, Beattie, Alam, Thomas, Herrington, Gorter, Cellucci, Garner, Heale, Matsos, Batthish.
Acknowledgments
We would like to acknowledge Debbie Poppa (pediatric rheumatology nurse), Jennifer Zuccolo (pediatric rheumatology physiotherapist), and Heather McKean (child‐life specialist) for their outstanding contributions to our multidisciplinary transition clinic at McMaster Children’s Hospital.
Funded by a grant from the Arthritis Society (AC‐19‐0517). Dr. Batthish’s work was supported by a New Investigator Fund from Hamilton Health Sciences.
Dr. Gorter is the director of the CanChild Centre for Childhood Disability Research at McMaster University, a nonprofit organization. CanChild developed, licences, and distributes the Transition‐Q measure that is discussed in the article. Dr. Gorter holds the Scotiabank Chair in Child Health Research at McMaster University. No other disclosures relevant to this article were reported.
References
- 1. Blum RW, Garell D, Hodgman CH, Jorissen TW, Okinow NA, Orr DP, et al. Transition from child‐centered to adult health‐care systems for adolescents with chronic conditions: a position paper of the Society for Adolescent Medicine. J Adolesc Health 1993;14:570–6. [DOI] [PubMed] [Google Scholar]
- 2. White PH, Ardoin S. Transitioning wisely: improving the connection from pediatric to adult health care. Arthritis Rheumatol 2016;68:789–94. [DOI] [PubMed] [Google Scholar]
- 3. Bingham CA, Scalzi L, Groh B, Boehmer S, Banks S. An assessment of variables affecting transition readiness in pediatric rheumatology patients. Pediatr Rheumatol Online J 2015;13:42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Felsenstein S, Reiff AO, Ramanathan A. Transition of care and health‐related outcomes in pediatric‐onset systemic lupus erythematosus. Arthritis Care Res (Hoboken) 2015;67:1521–8. [DOI] [PubMed] [Google Scholar]
- 5. Hazel E, Zhang X, Duffy CM, Campillo S. High rates of unsuccessful transfer to adult care among young adults with juvenile idiopathic arthritis. Pediatr Rheumatol Online J 2010;8:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Oen K. Long‐term outcomes and predictors of outcomes for patients with juvenile idiopathic arthritis. Best Pract Res Clin Rheumatol 2002;16:347–60. [PubMed] [Google Scholar]
- 7. Oen K, Malleson PN, Cabral DA, Rosenberg AM, Petty RE, Cheang M. Disease course and outcome of juvenile rheumatoid arthritis in a multicenter cohort. J Rheumatol 2002;29:1989–99. [PubMed] [Google Scholar]
- 8. Hersh AO, Pang S, Curran ML, Milojevic DS, von Scheven E. The challenges of transferring chronic illness patients to adult care: reflections from pediatric and adult rheumatology at a US academic center. Pediatr Rheumatol Online J 2009;7:13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Huang JS, Gottschalk M, Pian M, Dillon L, Barajas D, Bartholomew LK. Transition to adult care: systematic assessment of adolescents with chronic illnesses and their medical teams. J Pediatr 2011;159:994–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Conti F, Pontikaki I, D'Andrea M, Ravelli A, de Benedetti F. Patients with juvenile idiopathic arthritis become adults: the role of transitional care. Clin Exp Rheumatol 2018;36:1086–94. [PubMed] [Google Scholar]
- 11. McDonagh JE, Farre A. Are we there yet? An update on transitional care in rheumatology. Arthritis Res Ther 2018;20:5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Clemente D, Leon L, Foster H, Minden K, Carmona L. Systematic review and critical appraisal of transitional care programmes in rheumatology. Semin Arthritis Rheum 2016;46:372–9. [DOI] [PubMed] [Google Scholar]
- 13. Gorter JW, Amaria K, Cassidy C, DiRezze B, Grant C, Grewal K, et al. Teens Reaching Adulthood: Needs and Support for Improved Transitional Care in Ontario (TRANSITION). Presented at the 8th Annual Health Care Transition Research Consortium; 2016 October 26; Houston, TX.
- 14. Ekim A, Kolay M, Ferda Ocacki A. Readiness for transition from pediatric to adult care for adolescents with chronic heart disease. J Spec Pediatr Nurs 2018;23:1–6. [DOI] [PubMed] [Google Scholar]
- 15. Jensen PT, Paul GV, LaCount S, Peng J, Spencer CH, Higgins GC, et al. Assessment of transition readiness in adolescents and young adults with chronic health conditions. Pediatr Rheumatol Online J 2017;15:70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Klassen AF, Grant C, Barr R, Brill H, Kraus de Camargo O, Ronen GM, et al. Development and validation of a generic scale for use in transition programmes to measure self‐management skills in adolescents with chronic health conditions: the TRANSITION‐Q. Child Care Health Dev 2015;41:547–58. [DOI] [PubMed] [Google Scholar]
- 17. Klassen AF, Rosenberg‐Yunger ZR, D'Agostino NM, Cano SJ, Barr R, Syed I, et al. The development of scales to measure childhood cancer survivors' readiness for transition to long‐term follow‐up care as adults. Health Expect 2015;18:1941–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Andrich D. Sufficiency and conditional estimation of person parameters in the polytomous Rasch model. Psychometrika 2010;75:292–308. [Google Scholar]
- 19. Lazaroff SM, Meara A, Tompkins MK, Peters E, Ardoin SP. How do health literacy, numeric competencies, and patient activation relate to transition readiness in adolescents and young adults with rheumatic disease? Arthritis Care Res 2019;71:1264–1269. [DOI] [PubMed] [Google Scholar]
- 20. Varty M, Popejoy LL. A systematic review of transition readiness in youth with chronic disease. West J Nurs Res 2020;42:554–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Son MB, Sergeyenko Y, Guan H, Costenbader KH. Disease activity and transition outcomes in a childhood‐onset systemic lupus erythematosus cohort. Lupus 2016;25:1431–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Van Pelt PA, Dolhain RJ, Kruize AA, Ammerlaan JJ, Hazes JW, Bijlsma JW, et al. Disease activity and dropout in young persons with juvenile idiopathic arthritis in transition of care: a longitudinal observational study. Clin Exp Rheumatol 2018;36:163–8. [PubMed] [Google Scholar]


