Abstract
Background
The epidermal growth factor receptor (EGFR) family belongs to the transmembrane protein receptor of the tyrosine kinase I subfamily and has 4 members: EGFR/ERBB1, ERBB2, ERBB3, and ERBB4. The EGFR family is closely related to the occurrence and development of a variety of cancers.
Materials/methods
In this study, we used multiple online bioinformatics websites, including ONCOMINE, TCGA, CGGA, TIMER, cBioPortal, GeneMANIA and DAVID, to study the expression profiles, prognostic values and immune infiltration correlations of the EGFR family in glioma.
Results
We found that EGFR and ERBB2 mRNA expression levels were higher in glioblastoma (GBM, WHO IV) than in other grades (WHO grade II & III), while the ERBB3 and ERBB4 mRNA expression levels were the opposite. EGFR and ERBB2 were notably downregulated in IDH mutant gliomas, while ERBB3 and ERBB4 were upregulated, which was associated with a poor prognosis. In addition, correlation analysis between EGFR family expression levels and immune infiltrating levels in glioma showed that EGFR family expression and immune infiltrating levels were significantly correlated. The PPI network of the EGFR family in glioma and enrichment analysis showed that the EGFR family and its interactors mainly participated in the regulation of cell motility, involving integrin receptors and Rho family GTPases.
Conclusions
In summary, the results of this study indicate that the EGFR family members may become potential therapeutic targets and new prognostic markers for glioma.
Keywords: Glioma, EGFR family, Prognosis, Immune infiltration
Background
Brain and central nervous system (CNS) cancers (collectively referred to as CNS cancers) were responsible for substantial morbidity and mortality worldwide between 1990 and 2016 [1]. Glioma is a common brain tumor in humans and is one of the most malignant tumors among all cancers [2, 3]. Although various treatments for glioma, including surgery, radiotherapy, systemic therapy, tumor treatment fields, and supportive treatment, have recently made progress, the median survival period after diagnosis is still approximately 15 months, and long-term survival is unsatisfactory [4]. Because current treatments cannot significantly improve patient outcomes, the discovery of novel treatment strategies is critical. Therefore, the identification of new biomarkers is of great significance for improving the prognosis and developing individualized treatment.
The epidermal growth factor receptor (EGFR) family (also known as the HER family) belongs to the transmembrane protein receptor of the tyrosine kinase I subfamily, and it has 4 members: EGFR/ERBB1, ERBB2, ERBB3, and ERBB4, encoded by the proto-oncogenes ERBB1–4. The members of the EGFR family are similar in structure and consist of an extracellular ligand-binding domain, a hydrophobic transmembrane region and an intracellular segment containing a conserved tyrosine kinase domain [5, 6]. After the ligand binds to the extracellular domain, the protein conformation of the extracellular domain is changed. Phosphorylation of the tyrosine kinase in the intracellular domain initiates the signal transduction pathway, transmits the signal from outside the cell into the cytoplasm, and modulates the cell’s response to external stimuli, thereby regulating the growth, survival, transformation and apoptosis of normal cells [7, 8].
Overexpression and activation of the EGFR family can be seen in many human cancers and they are closely related to the clinicopathological characteristics and prognosis of many tumors, such as breast cancer [9], lung cancer [10], gastric cancer [11] and melanoma [12]. Previous studies have discovered EGFR family pathway dysregulation in gliomas and their relationship with the clinical characteristics and prognosis of human gliomas. However, the expression patterns and roles of the EGFR family proteins in gliomas are issues that urgently need attention.
In recent years, due to the continuous development and application of bioinformatics databases, an increasing number of tumor biomarkers have been discovered [13–16]. In addition, an increasing number of studies have shown that the EGFR family can be used as potential targets for the treatment of glioma [17, 18]. In this study, we downloaded EGFR family expression data from various online databases and analyzed the relationship between their transcription levels in gliomas and the clinical prognosis. Analysis of the tumor immune estimation resource (TIMER) database revealed a correlation between the EGFR family and tumor infiltrating immune cells in the tumor microenvironment. Our research shows that the EGFR family members may be potential therapeutic targets with promising prognostic value in glioma patients.
Materials and methods
Oncomine database analysis
We used the Oncomine database (https://www.oncomine.org/) [19] to extract the data of the expression levels of the EGFR family in various types of glioma tissues. Then, we analyzed the differential expression of the members of the EGFR family between cancer tissue and normal tissue through Student’s t-test. Critical value setting conditions: Fold change> 1.5, P-value< 0.01.
Acquisition of the data from the TCGA and CGGA dataset
The RNA sequencing data and clinical information in the TCGA-GBMLGG dataset were downloaded from UCSC Xena (https://xenabrowser.net/datapages/) [20]. In addition, the RNA sequencing data and clinical information in the CGGA dataset (mRNAseq_325) were also obtained from their official website (http://www.cgga.org.cn/index.jsp) [21]. For further analysis, a total of 668 samples from the TCGA dataset and 326 primary glioma samples from the CGGA dataset, which contained both gene expression and survival data, were extracted.
Tumor infiltrating immune cells analysis
The TIMER database (https://cistrome.shinyapps.io/timer/) is a database that can comprehensively and systematically analyze the interaction between tumors and immunity [22]. We downloaded the estimated data of tumor-infiltrating immune cells from the TIMER database and analyzed the correlation between the expression levels of the EGFR family members and the abundance of infiltrating immune cells in glioma.
cBioPortal analysis
cBioPortal (https://www.cbioportal.org/) provides a visual tool for research and analysis of cancer gene data and helps cancer tissue and cytology research gain molecular data understanding of their genetics, epigenetics, gene expression and proteomics. We can study the link between genetic changes and clinical practice by customizing the interface of the data. Through the cBioPortal online tool, we analyzed EGFR family alterations and their correlations with clinical factors. We used the glioma dataset for analysis of EGFR family expression with cBioPortal [23].
GeneMANIA analysis
The GeneMANIA database (http://www.genemania.org/) is a website dedicated to the study of protein-protein interaction (PPI) relationships [24]. It mainly provides data predictions including the following: protein predictions, protein interactions, coexpression, sharing of protein domains, subcellular colocalization, signaling pathways, genetic interactions, etc. and it can construct a PPI network. In this study, humans (Homo sapiens) were selected in the species selection interface to search for proteins interacting with members of the EGFR family.
DAVID analysis
DAVID (https://david.ncifcrf.gov/) is a public database that integrates biological data and analysis tools and can annotate genes and pathways [25]. GO is a bioinformatics tool that annotates genes and analyzes the biological processes in which they participate. KEGG is a database used to analyze the relevant signaling pathways in a large-scale molecular data set generated by high-throughput experimental technology. DAVID was used for GO enrichment analysis of the EGFR family in three aspects: molecular function (MF), cell composition (CC) and biological process (BP), as well as the enrichment analysis of KEGG pathways, to clarify the gene function and the cell signaling pathways of the members of the EGFR family.
Statistical analysis
Student’s t-test was used to analyze gene expression in the Oncomine, TCGA and CCGA databases as well as IDH wild-type and mutation data in the TCGA and CCGA databases. The survival curves were compared using the log-rank test. Spearman’s correlation analysis was used in the TIMER database. P < 0.05 was considered statistically significant.
Results
The mRNA expression levels of the EGFR family across different types of cancers
The Oncomine database was used to compare the mRNA expression levels of the EGFR family between tumor and normal tissues. This analysis revealed that EGFR family expression was significantly different in glioma tissues compared with normal tissues (Fig. 1b). According to the information from the datasets in Oncomine, in Sun’s datasets [26], the mRNA levels of EGFR were 9.390, 5.740, and 8.211 times higher in glioma tissues with different histological types than in normal tissues (Table 1). In the TCGA dataset, the expression of EGFR was 3.792- and 2.956-fold higher in glioma tissues with different histological types than in normal tissues (Table 1). In French’s dataset [27], the expression of EGFR was 9.847 times higher in anaplastic oligodendroglioma tissues than in normal tissues (Table 1). In Lee’s dataset [28], the expression of EGFR was 3.772 times higher in glioblastoma tissues than in normal tissues (Table 1). In Shai’s dataset [29], the expression of EGFR was 3.815 times higher in glioblastoma tissues than in normal tissues (Table 1). In Bredel’s dataset [30], the expression of EGFR was 5.840 times higher in glioblastoma tissues than in normal tissues (Table 1). In Murat’s dataset [31], the expression of EGFR was 10.667 times higher in glioblastoma tissues than in normal tissues (Table 1). In Watson’s dataset [32], the expression of ERBB2 was 5.166 times higher in meningioma tissues than in normal tissues (Table 1). In Bredel’s dataset [33], the expression of ERBB2 was 3.065 times higher in glioblastoma tissues than in normal tissues (Table 1). In Pomeroy’s dataset [34], the expression of ERBB3 was 8.973 times higher in classic medulloblastoma tissues than in normal tissues (Table 1). ERBB4 had no available research results that met the screening criteria.
Fig. 1.
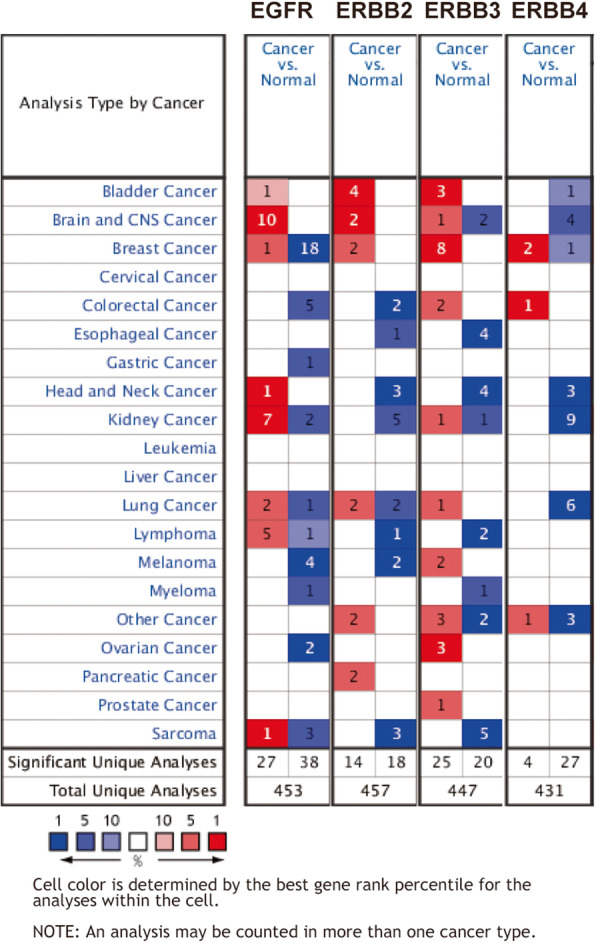
The expression of the EGFR family in different cancers
Table 1.
In different types of gliomas and normal brain tissues, differences in the transcriptional levels of the EGFR family
| EGFR family | Type of glioma vs. brain | Fold change | P | t-test | Reference |
|---|---|---|---|---|---|
| EGFR | Glioblastoma vs. Normal | 9.390 | 3.09E-27 | 14.885 | Sun [14] |
| Oligodendroglioma vs. Normal | 5.740 | 1.39E-15 | 10.540 | Sun [14] | |
| Anaplastic Astrocytoma vs. Normal | 8.211 | 9.39E-8 | 7.824 | Sun [14] | |
| Brain Glioblastoma vs. Normal | 3.792 | 5.10E-18 | 14.875 | TCGA | |
| Anaplastic Oligodendroglioma vs. Normal | 9.847 | 4.07E-9 | 9.400 | French [15] | |
| Glioblastoma vs. Normal | 3.772 | 9.78E-7 | 8.111 | Lee [16] | |
| Glioblastoma vs. Normal | 3.815 | 2.75E-5 | 4.729 | Shai [17] | |
| Glioblastoma vs. Normal | 5.840 | 9.51E-7 | 6.098 | Bredel [18] | |
| Brain Glioblastoma vs. Normal | 2.956 | 9.32E-101 | 26.116 | TCGA | |
| Glioblastoma vs. Normal | 10.667 | 1.16E-6 | 10.112 | Murat [19] | |
| ERBB2 | Meningioma vs. Normal | 5.166 | 8.89E-7 | 7.324 | Watson [20] |
| Glioblastoma vs. Normal | 3.065 | 1.70E-9 | 10.222 | Bredel [18] | |
| ERBB3 | Classic Medulloblastoma vs. Normal | 8.973 | 3.79E-8 | 6.404 | Pomeroy [21] |
| ERBB4 | NA | NA | NA | NA | NA |
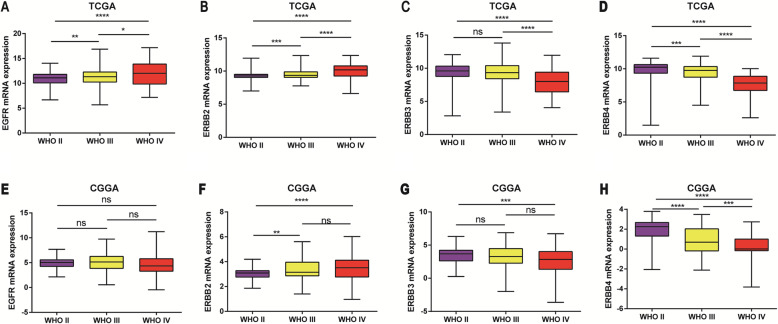
Subtype analysis of mRNA expression levels of the EGFR family in glioma
To analyze the transcription levels of the EGFR family in subtypes of glioma patients, the TCGA and CGGA databases were applied. According to the tumor grades, in the TCGA database, compared with WHO II & III, the EGFR transcription level was the highest in WHO IV (Fig. 2a). However, by analyzing the CGGA RNA-seq database, we found that this difference was not statistically significant (Fig. 2e). In the TCGA database, the transcription level of ERBB2 was the highest in WHO IV compared with WHO II & III (Fig. 2b). However, the transcription levels of ERBB3 and ERBB4 in WHO IV were significantly lower than those in II & III and this difference was statistically significant (Fig. 2c and d). Analysis of the CGGA RNA-seq data set also found that the transcription levels of ERBB2, ERBB3 and ERBB4 were similar (Fig. 2f, g and h). In summary, the mRNA levels of EGFR and ERBB2 were higher in advanced and poorly differentiated gliomas; however, the mRNA levels of ERBB3 and ERBB4 were lower in advanced and poorly differentiated gliomas.
Fig. 2.
The expression level of the EGFR family in different grades of glioma tissues. a, b, e and f The mRNA expression levels of EGFR and ERBB2 were significantly increased in GBM. c, d, g, and h The mRNA expression levels of ERBB3 and ERBB4 were significantly increased in glioma (WHO II). * represents p < 0.05, ** represents p < 0.01, *** represents p < 0.001, and **** represents p < 0.0001
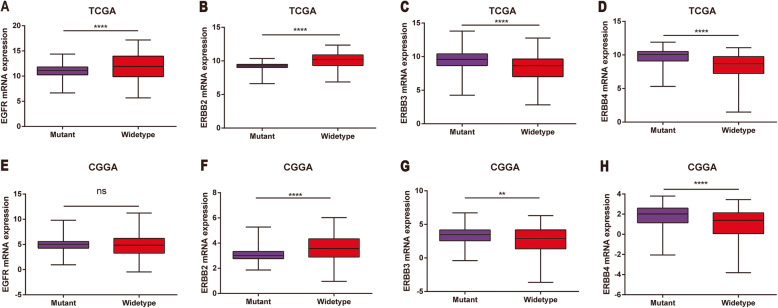
Mutations in isocitrate dehydrogenase (IDH) play an important role in the occurrence and development of glioma and serve as a potential prognostic marker for patients with glioma [35]. Therefore, we studied the expression level of EGFR in IDH mutant and wild type. In the TCGA data, the expression level of EGFR in IDH wild-type glioma was elevated (Fig. 3). However, in the CGGA RNA-seq data set, there was no significant difference in the expression level of EGFR in IDH wild-type glioma (Fig. 4a, e). In the TCGA data, the expression level of ERBB2 in IDH wild-type gliomas was notably increased (Fig. 1, 4b), and it was also increased in the CGGA RNA-seq datasets (Fig. 4f). Analysis of the TCGA data and the CGGA RNA-seq data found that ERBB3 and ERBB4 were notably increased in IDH mutant gliomas (Fig. 1, 4b, c and d), and the same result was found in the CGGA RNA-seq datasets (Fig. 4g and h). In conclusion, data analysis shows that the expression levels of the members of the EGFR family are notably different in different IDH states and they have the potential for use as biomarkers of IDH subtypes of glioma.
Fig. 3.
EGFR family expression was closely associated with IDH wild-type and mutation in glioma. a, b, e and f EGFR and ERBB2 were notably downregulated in IDH mutant glioma. c, d, g and h ERBB3 and ERBB4 were notably upregulated in IDH mutant glioma. * represents p < 0.05, ** represents p < 0.01, *** represents p < 0.001, and **** represents p < 0.0001
Fig. 4.
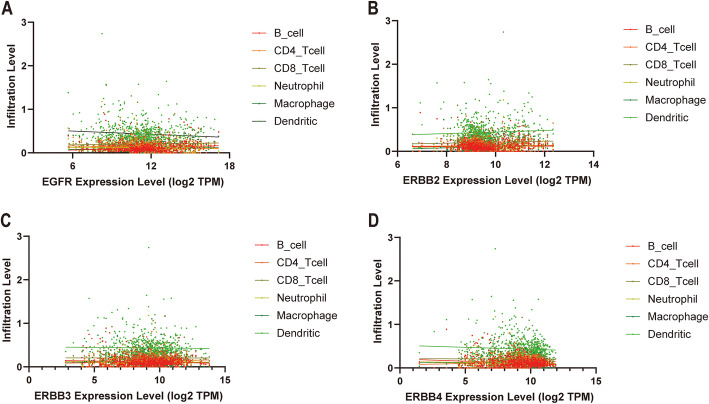
Correlation between the transcription level of the EGFR family and the immune infiltration level in glioma. a The transcription level of EGFR was positively correlated with the level of B cell infiltration in tumor tissues. b The transcription level of ERBB2 EGFR was positively correlated with the level of macrophage infiltration in tumor tissues. c and d The transcriptional expression levels of ERBB3 and ERBB4 were positively correlated with the level of CD4+ T cell infiltration in tumor tissues
Correlation between EGFR family expression and immune infiltrating levels in glioma
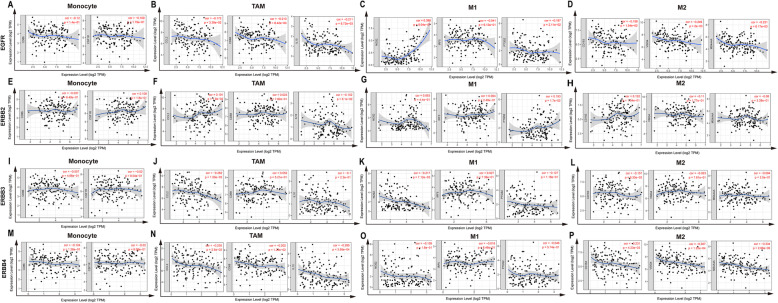
An increasing number of studies have shown that tumor-infiltrating lymphocytes can be used as related indicators to predict tumor metastasis and invasion [36, 37]. Therefore, by analyzing the TIMER database, we found a correlation between the expression levels of the members of the EGFR family and the level of immune infiltration in glioma tissues. As shown in Fig. 5 and Table 2, the expression level of EGFR mRNA was notably positively correlated with the level of B cell infiltration in glioma tissue (r = 0.1671, p < 0.0001). The expression level of EGFR mRNA was notably negatively correlated with the infiltration level of DCs (r = − 0.09997, p = 0.0088) and CD4+ T cells (r = − 0.1143, p = 0.0027) in glioma tissue. ERBB2 mRNA expression was notably positively correlated with the level of macrophage infiltration in gliomas (r = 0.1026, p = 0.0072). The mRNA expression of ERBB3 and ERBB4 in gliomas was notably positively correlated with the level of CD4+ T cell infiltration (ERBB3, r = 0.1200, p = 0.0016, ERBB4, r = 0.09663, p = 0.0114). The expression of ERBB3 and ERBB4 mRNA in gliomas was notably negatively correlated with the level of B cell infiltration (ERBB3, r = − 0.08882, p < 0.0201, ERBB4, r = − 0.1591, p < 0.001). However, the glioma control group showed that ERBB2 expression had no significant correlation with macrophage polarization in gliomas (Fig. 6a-o). These results strongly suggest that the members of the EGFR family play specific roles in regulating the immune infiltration of glioma.
Fig. 5.
EGFR family expression was correlated with macrophage polarization in glioma. Markers include CD86 and CSF1R of monocytes; CCL2, CD68, and IL10 of TAMs (tumor-associated macrophages); NOS2, IRF5, and PTGS2 of M1 macrophages; and CD163, VSIG4, and MS4A4A of M2 macrophages in glioma (n = 153). a-d Scatterplots of correlations between EGFR expression and gene markers of monocytes, TAMs, and M1 and M2 macrophages. e-h Scatterplots of correlations between ERBB2 expression and gene markers of monocytes, TAMs, and M1 and M2 macrophages. i-l Scatterplots of correlations between ERBB3 expression and gene markers of monocytes, TAMs, and M1 and M2 macrophages. m-p Scatterplots of correlations between ERBB4 expression and gene markers of monocytes, TAMs, and M1 and M2 macrophages
Table 2.
Correlation between EGFR family mRNA expression levels and immune cell infiltration level
| Description | EGFR | ERBB2 | ERBB3 | ERBB4 | ||||
|---|---|---|---|---|---|---|---|---|
| Cor | P | Cor | P | Cor | P | Cor | P | |
| B-cell | 0.1671 | < 0.0001 | 0.02272 | 0.5527 | −0.08882 | 0.0201 | − 0.1591 | < 0.0001 |
| CD4-Tcell | −0.1143 | 0.0027 | 0.03041 | 0.4268 | 0.1200 | 0.0016 | 0.09663 | 0.0114 |
| CD8-Tcell | 0.05893 | 0.1233 | 0.07340 | 0.0549 | −0.002242 | 0.9533 | −0.01364 | 0.7217 |
| Neutrophil | −0.04326 | 0.2582 | 0.06590 | 0.0848 | −0.02445 | 0.5229 | −0.06434 | 0.0925 |
| Macrophage | 0.07331 | 0.0551 | 0.1026 | 0.0072 | −0.01798 | 0.6386 | −0.05173 | 0.1763 |
| Dendritic cell | −0.09997 | 0.0088 | 0.06210 | 0.1044 | −0.01882 | 0.6229 | −0.06135 | 0.1087 |
Fig. 6.
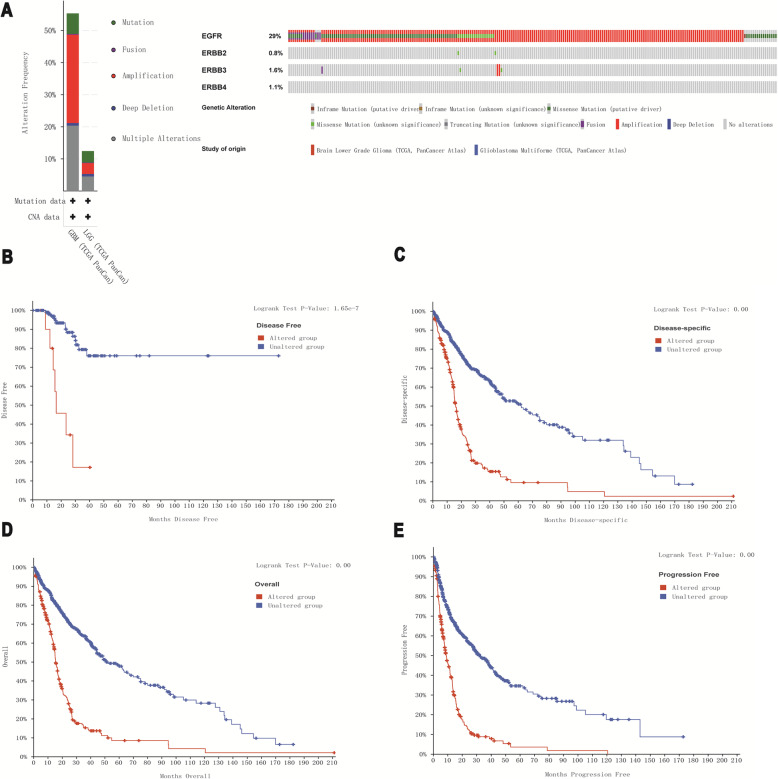
Relationship between EGFR family mutations and prognosis in gliomas. a The mutation rates of EGFR, ERBB2, ERBB3 and ERBB4 were 29, 0.8, 1.6 and 1.1%, respectively. b, c, d and e EGFR family mutations in glioma patients predicted poor OS, DFS, DS, and PFS
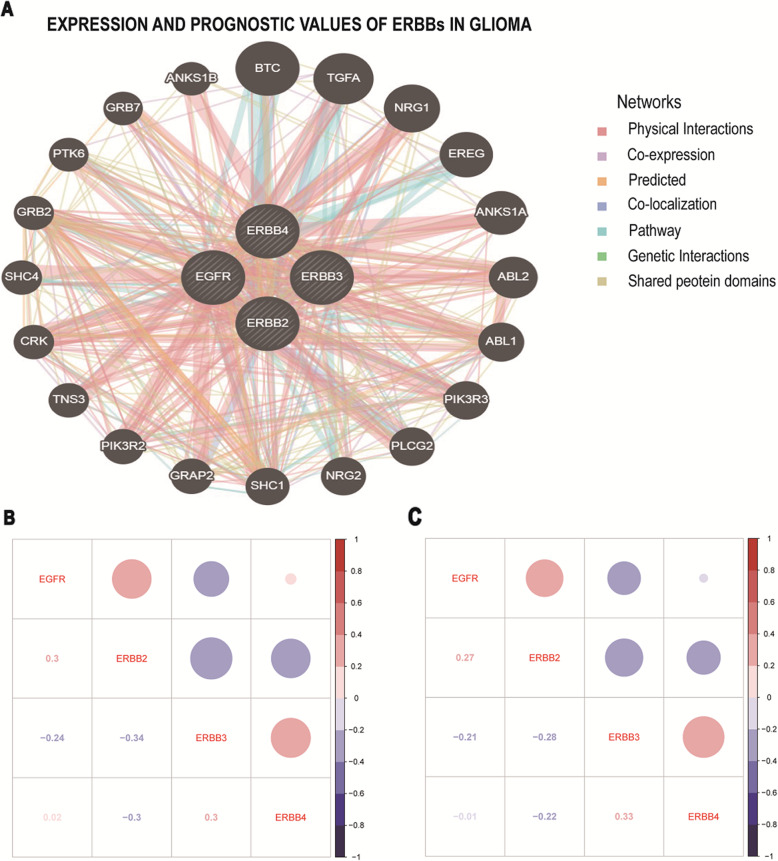
PPI network of the EGFR family in glioma and enrichment analysis
Next, we used Gene-MANIA to construct a PPI network for the EGFR family, and the results are shown in Fig. 7a. Then, GO and KEGG analyses based on DAVID were performed to identify the functional enrichment of the EGFR family and their associated genes (Table 3). Biological process (BP) enrichment terms showed that the EGFR family and their interacting proteins were significantly associated with the ERBB2 signaling pathway, regulation of cell motility, regulation of phosphatidylinositol 3-kinase signaling, phosphatidylinositol phosphorylation, phosphatidylinositol-mediated signaling, peptidyl-tyrosine phosphorylation, epidermal growth factor receptor signaling pathway, MAPK cascade, transmembrane receptor protein tyrosine kinase signaling pathway, positive regulation of GTPase activity, wound healing, and positive regulation of cell proliferation. MF enrichment showed that the EGFR family was significantly correlated with phosphatidylinositol-4,5-bisphosphate 3-kinase activity, Ras guanyl-nucleotide exchange factor activity, epidermal growth factor receptor binding, ephrin receptor binding, and receptor signaling protein tyrosine kinase activity. KEGG enrichment revealed that the EGFR family was related to the ERBB signaling pathway, glioma, non-small cell lung cancer pathways, neurotrophin signaling pathways, chronic myeloid leukemia pathways, random signaling pathways in microRNAs in cancer tissues, and cancer lycans signaling pathways. Overall, the potential mechanisms by which the EGFR family participates in the carcinogenesis of glioma were explored by PPI construction and enrichment analysis.
Fig. 7.
Predicted pathways and correlation of EGFR family gene expression in glioma. a A PPI network for the EGFR family was constructed in GeneMANIA. b, c Pearson’s test was used to study the correlations among the EGFR family members
Table 3.
GO and KEGG enrichment analysis of the EGFR family and their 20 interactors
| Category | Terms | Description | Count | FDR |
|---|---|---|---|---|
| BP | GO:0038128 | ERBB2 signaling pathway | 12 | 2.95E-21 |
| BP | GO:2000145 | regulation of cell motility | 10 | 2.63E-17 |
| BP | GO:0014066 | regulation of phosphatidylinositol 3-kinase signaling | 10 | 6.11E-13 |
| BP | GO:0046854 | phosphatidylinositol phosphorylation | 10 | 3.83E-12 |
| BP | GO:0048015 | phosphatidylinositol-mediated signaling | 10 | 1.18E-11 |
| BP | GO:0018108 | peptidyl-tyrosine phosphorylation | 10 | 3.45E-10 |
| BP | GO:0007173 | epidermal growth factor receptor signaling pathway | 8 | 1.01E-09 |
| BP | GO:0000165 | MAPK cascade | 10 | 4.45E-08 |
| BP | GO:0007169 | transmembrane receptor protein tyrosine kinase signaling pathway | 8 | 5.02E-08 |
| BP | GO:0043547 | positive regulation of GTPase activity | 11 | 1.83E-06 |
| BP | GO:0042060 | wound healing | 6 | 9.38E-05 |
| BP | GO:0008284 | positive regulation of cell proliferation | 9 | 1.55E-04 |
| MF | GO:0046934 | phosphatidylinositol-4,5-bisphosphate 3-kinase activity | 10 | 5.51E-14 |
| MF | GO:0004713 | protein tyrosine kinase activity | 11 | 7.11E-13 |
| MF | GO:0005088 | Ras guanyl-nucleotide exchange factor activity | 10 | 1.84E-11 |
| MF | GO:0005154 | epidermal growth factor receptor binding | 6 | 5.20E-07 |
| MF | GO:0046875 | ephrin receptor binding | 5 | 4.08E-05 |
| MF | GO:0004716 | receptor signaling protein tyrosine kinase activity | 4 | 2.80E-04 |
| KEGG | hsa04012 | ERBB signaling pathway | 18 | 2.00E-29 |
| KEGG | hsa05214 | Glioma | 8 | 1.53E-07 |
| KEGG | hsa05223 | Non-small cell lung cancer | 7 | 4.12E-06 |
| KEGG | hsa04722 | Neurotrophin signaling pathway | 8 | 1.21E-05 |
| KEGG | hsa05220 | Chronic myeloid leukemia | 7 | 1.93E-05 |
| KEGG | hsa04014 | Ras signaling pathway | 9 | 4.27E-05 |
| KEGG | hsa05206 | MicroRNAs in cancer | 9 | 2.66E-04 |
| KEGG | hsa05205 | Proteoglycans in cancer | 8 | 4.15E-04 |
| KEGG | hsa04510 | Focal adhesion | 8 | 5.07E-04 |
| KEGG | hsa05215 | Prostate cancer | 6 | 0.002482 |
| KEGG | hsa05200 | Pathways in cancer | 9 | 0.003013 |
| KEGG | hsa04915 | Estrogen signaling pathway | 6 | 0.004453 |
| KEGG | hsa05213 | Endometrial cancer | 5 | 0.00888 |
BP, Biological processes; MF, molecular functions; KEGG, Kyoto Encyclopedia of Genes and Genomes; GO, gene ontology; FDR, false discovery rates
The relationship between EGFR family alterations and prognosis in patients with glioma
To further understand the EGFR family, we used the cBioPortal online tool to study the alterations of the EGFR family and their correlation with prognosis. We found that among 885 patients with glioma, 272 patients had alterations in EGFR family genes (31%), and the most common genetic alteration was amplification (Fig. 1a). In addition, the cBioPortal database showed the correlations between EGFR family genetic alterations and overall survival (OS) (p < 0.001), disease-free survival (DFS) (p < 0.001), disease-specific survival (DSS) (p < 0.001), and progression-free survival (PFS) of patients with glioma (p < 0.001) (Fig. 1b, c, d, and e). We also used Pearson’s test to study the correlations among the expression levels of the EGFR family in the CGGA and TCGA datasets. We found some EGFR family members to be notably positively correlated: EGFR with ERBB2; ERBB3 with ERBB4. Some other EGFR family members were significantly negatively correlated: EGFR with ERBB3; ERBB2 with ERBB3 and ERBB4. The expression of EGFR had no association with ERBB4 (Fig. 7b and c).
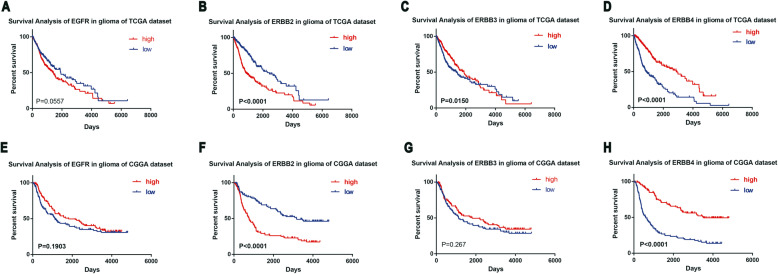
Prognostic values of the EGFR family in glioma
In addition, we used the TCGA and CGGA datasets to evaluate the prognostic impact of EGFR family expression on high-grade glioma. The results showed that high mRNA levels of ERBB2 and ERBB4 in glioma patients were associated with a poor prognosis (Fig. 8c, d, g and h), while the expression of EGFR and ERBB3 had no correlation with the prognosis of glioma patients (Fig. 8a, b, e and f). The results from the CGGA and TCGA data sets were similar. Next, through univariate and multivariate Cox analysis, we also found that age, tumor grade, IDH mutations and EGFR family member expression levels were prognostic factors of glioma patients (Table 4).
Fig. 8.
The prognostic value of the EGFR family in glioma. a, b, c and d Overall survival correlated with the expression of the EGFR family members in all grades of glioma in the TCGA dataset. e, f, g and h Overall survival correlated with the expression of EGFR family members in all grades of glioma in the CGGA dataset
Table 4.
Univariate and multivariate regression analysis was used to predict the overall survival rate of glioma patients
| Characteristic | TCGA (n = 668) | CGGA (n = 326) | ||||
|---|---|---|---|---|---|---|
| P | HR | 95%CI | P | HR | 95%CI | |
| Univariate | ||||||
| Age | < 0.0001 | 1.068 | 1.057–1.078 | < 0.0001 | 1.054 | 1.038–1.070 |
| Gender | 0.144 | 0.826 | 0.639–1.068 | 0.806 | 1.044 | 0.741–1.469 |
| Grade | < 0.0001 | 4.638 | 3.803–5.657 | < 0.0001 | 1.952 | 1.708–2.232 |
| IDH | < 0.0001 | 0.127 | 0.096–0.169 | < 0.0001 | 2.802 | 1.960–4.007 |
| EGFR | < 0.0001 | 1.187 | 1.103–1.278 | 0.808 | 1.013 | 0.914–1.123 |
| ERBB2 | < 0.0001 | 2.177 | 1.884–2.516 | < 0.0001 | 1.961 | 1.613–2.384 |
| ERBB3 | 0.001 | 0.879 | 0.818–0.946 | 0.005 | 0.866 | 0.783–0.958 |
| ERBB4 | < 0.0001 | 0.684 | 0.638–0.734 | < 0.0001 | 0.630 | 0.564–0.703 |
| Multivariate | ||||||
| Age | < 0.0001 | 1.033 | 1.021–1.044 | 0.001 | 1.029 | 1.012–1.046 |
| Gender | 0.596 | 0.931 | 0.715–1.212 | 0.482 | 0.882 | 0.620–1.253 |
| Grade | < 0.0001 | 2.218 | 1.727–2.848 | < 0.0001 | 1.752 | 1.485–2.066 |
| IDH | < 0.0001 | 0.341 | 0.235–0.495 | 0.429 | 1.192 | 0.771–1.841 |
| EGFR | 0.459 | 0.978 | 0.921–1.038 | 0.776 | 1.012 | 0.931–1.100 |
| Age | < 0.0001 | 1.032 | 1.020–1.044 | 0.002 | 1.027 | 1.010–1.044 |
| Gender | 0.537 | 0.920 | 0.706–1.199 | 0.531 | 0.894 | 0.629–2.067 |
| Grade | < 0.0001 | 2.185 | 1.700–2.809 | < 0.0001 | 1.751 | 1.483–2.067 |
| IDH | < 0.0001 | 0.375 | 0.253–0.554 | 0.876 | 1.036 | 0.662–1.622 |
| EGFR2 | 0.142 | 1.128 | 0.960–1.326 | < 0.0001 | 1.464 | 1.199–1.786 |
| Age | < 0.0001 | 1.034 | 1.022–1.045 | 0.001 | 1.029 | 1.012–1.045 |
| Gender | 0.646 | 0.940 | 0.722–1.224 | 0.491 | 0.884 | 0.621–1.257 |
| Grade | < 0.0001 | 2.288 | 1.780–2.942 | < 0.0001 | 1.745 | 1.479–2.059 |
| IDH | < 0.0001 | 0.335 | 0.231–0.484 | 0.437 | 1.188 | 0.768–1.835 |
| EGFR3 | 0.032 | 1.077 | 1.006–1.153 | 0.766 | 0.986 | 0.896–1.084 |
| Age | < 0.0001 | 1.033 | 1.021–1.045 | 0.001 | 1.027 | 1.011–1.043 |
| Gender | 0.623 | 0.936 | 0.719–1.218 | 0.678 | 0.927 | 0.650–1.323 |
| Grade | < 0.0001 | 2.282 | 1.755–2.967 | < 0.0001 | 1.575 | 1.322–1.876 |
| IDH | < 0.0001 | 0.333 | 0.227–0.488 | 0.329 | 1.248 | 0.800–1.946 |
| EGFR4 | 0.396 | 1.041 | 0.949–1.141 | < 0.0001 | 0.757 | 0.664–0.864 |
Discussion
Glioma is an invasive and highly diffuse brain tumor [38]. Current standard treatment for glioma patients includes maximum safe surgical resection, simultaneous radiotherapy and temozolomide, and then adjuvant temozolomide. Glioma is still an incurable disease; the average OS after standard treatment is 12–15 months, and relapse is inevitable [39]. Therefore, it is extremely important to explore new methods to improve the quality of life and survival times of glioma patients.
Research results in recent years have shown that the tumor microenvironment plays an important role in the occurrence and development of glioma. An in-depth understanding of the tumor microenvironment is beneficial to provide new immunotherapy for glioma patients to inhibit tumor development [40, 41]. In recent years, immune checkpoint inhibitors against members of the EGFR family have been widely tested against gliomas in clinical trials, opening up broad new prospects for the treatment of gliomas [42, 43]. In this study, we analyzed the expression of EGFR family members in gliomas and their relationships with prognosis and immune infiltration. Our results suggest that the EGFR family mRNA expression levels are related to the poor prognosis of glioma. In addition, EGFR family mRNA levels are correlated with the abundance of tumor-infiltrating immune cells. Overall, our study provides new insights into the important roles of the EGFR family members in the assessment of glioma prognosis and immune infiltration.
The abnormal expression of the EGFR family in a significant proportion of human cancers has been studied; however, the roles of the EGFR family members in gliomas is still uncertain [44, 45]. Here, to clarify the expression profile of the EGFR family members in all grades of gliomas, by analyzing glioma samples in the CGGA and TCGA datasets, we summarized the expression patterns and distribution of the EGFR family. We found that the expression of the EGFR family in glioma had significant changes at the mRNA levels. At the same time, the expression patterns of the EGFR family members in various subtypes of gliomas were significantly different, suggesting that the EGFR family is related to the malignant phenotype and tumor progression. In addition, the EGFR family member expression pattern is significantly different in IDH-mutated gliomas, suggesting that IDH may be a regulator of the EGFR family.
After binding and activation, EGFR can form a dimer structure with other members. They all preferentially bind to ERBB2 to form a stronger heterodimer. This initiates a series of cascade reactions through autophosphorylation, which participate in cell signal transmission. These signals reach the nucleus and they play important roles in normal cell proliferation, differentiation and migration [46]. EGFR gene amplification and overexpression can be seen in a variety of human malignancies, including non-small cell lung cancer [47], breast cancer [48], ovarian cancer [49], gastric cancer [50], etc. Abnormal EGFR gene activation is closely related to tumor cell proliferation, angiogenesis, tumor invasion and migration, and inhibition of apoptosis [51].
ERBB2 forms a heterodimer with other members of the family. This allows it to bind indirectly to the ligand, which activates the tyrosine kinase in its intracellular segment, triggering downstream signal transduction. The signal is transmitted to the nucleus through intercellular substances, activating cell proliferation-related genes, thereby promoting cell mitosis and modulating cell proliferation, differentiation, migration and tumor formation [52, 53]. ERBB2 is overexpressed to varying degrees in many malignancies, such as breast cancer [54], ovarian cancer [55], non-small cell lung cancer [56], and gastric cancer [57]. Besides, ERBB2 is upregulated in high grade gliomas and correlated with PD-L1 expression [58].
The ERBB3/ERBB2 dimer is the most active ERBB dimer, and it can activate the PI3K/AKT, Jak/Stat and other signaling pathways and regulate cell proliferation, differentiation, migration and other activities [59]. ERBB3 is closely related to the occurrence and development of various tumors. Abnormal activation and overexpression of the HER3 gene can be seen in malignant tumors such as breast cancer [60], gastric cancer [61], ovarian cancer [62], and prostate cancer [63].
After ligands bind to ERBB4 (neurodifferentiation factor heparin binding epidermal growth factor, etc.), it activates downstream PI3K/Akt and Ras/Raf/MAPK signaling pathways through autophosphorylation and mediates extracellular growth factor signaling through intracellular kinase cascade intracellular transmission, thereby regulating angiogenesis and cell growth, differentiation, proliferation and apoptosis [64].
In recent years, the importance of immune cell infiltration in tumors has gradually been recognized [65, 66]. Blocking immune checkpoints has become a promising cancer treatment [67]. However, the relationship between the EGFR family and immune infiltration in gliomas has not been studied. In this paper, the TIMER database was used to analyze the relationship between EGFR family expression levels and immune penetration in gliomas. The expression of EGFR has a notable correlation with the level of B cell infiltration. ERBB2 expression was notably correlated with the level of macrophage infiltration. The expression of ERBB3 and ERBB4 were positively correlated with the level of CD4+ T cell infiltration. These correlations may suggest a potential mechanism by which the EGFR family regulates glioma immune cells. These findings indicate that the EGFR family plays a crucial role in the regulation of glioma immune cells.
To explore the potential mechanism of EGFR family involvement in glioma carcinogenesis, we constructed a PPI network and performed GO and KEGG analyses of the EGFR family with DAVID. The results showed that EGFR family interacting genes are mainly involved in cell motility, which may affect integrin receptors and Rho family GTPases. Integrin receptors have been reported to interact with EGFR [68]. Moreover, Rho family GTPases play an important role in the interactions between the EGFR family members and other proteins. In summary, the interaction between integrin receptors/Rho family GTPases and the EGFR family may become a new antitumor therapy strategy that can regulate signaling pathways [69].
Conclusion
This study systematically analyzed the expression patterns of the EGFR family, their mutations, and their correlations with the prognosis of patients with glioma, advancing our understanding of the biological characteristics of glioma. These results revealed that the EGFR family might play an important role in the development of gliomas. The EGFR family members can also be used as molecular markers for glioblastoma, may be potential biomarkers for the diagnosis and prognosis of patients with glioma, and may be therapeutic targets for the treatment of glioma.
Acknowledgments
Not applicable.
Abbreviations
- EGFR
Epidermal growth factor receptor
- GBM
Glioblastoma
- CNS
Brain and central nervous system
- PPI
Protein-protein interaction
- MF
Molecular function
- CC
Cell composition
- BP
Biological process
- OS
Overall survival
- DFS
Disease-free survival
- DSS
Disease-specific survival
- PFS
Progression-free survival
Authors’ contributions
Junfei S and Jun S conceived the study and participated in the study design, performance, coordination and manuscript writing. BX, ZYH, HH, WJ, ZB and JJ performed the literature review and graphics production. Junfei S and Jun S revised the manuscript. All authors reviewed and approved the final manuscript.
Funding
This work was supported by the National Natural Science Foundation of China (No. 8150215).
Availability of data and materials
The datasets analyzed for this study were obtained from the Oncomine database (https://www.oncomine.org/), the UCSC Xena website (https://xenabrowser.net/datapages/) and the CGGA dataset (mRNAseq_325) (http://www.cgga.org.cn/index.jsp), the TIMER (https://cistrome.shinyapps.io/timer/) website, the cBioPortal (https://www.cbioportal.org/) and the GeneMANIA databases (http://www.genemania.org/), and DAVID (https://david.ncifcrf.gov/).
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no conflicts of interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Bin Xu, Zhengyuan Huo and Hui Huang contributed equally to this work.
Contributor Information
Bin Xu, Email: njykdxxb1227@163.com.
Zhengyuan Huo, Email: 984425942@qq.com.
Hui Huang, Email: hhnjmu97@163.com.
Wei Ji, Email: 549980821@qq.com.
Zheng Bian, Email: 876193723@qq.com.
Jiantong Jiao, Email: wxrmyyjjt@163.com.
Jun Sun, Email: wxrmsj@163.com.
Junfei Shao, Email: wxrmyysjf@163.com.
References
- 1.Anoop P, Patel JLF, Nichols E, Abd-Allah F, Abdela J, Abdelalim A, Abraha HN, Agius D, Alahdab F, Alam T, Allen CA, et al. Global, regional, and national burden of brain and other CNS cancer, 1990-2016: a systematic analysis for the global burden of disease study 2016. Lancet Neurol. 2019;18(4):376–393. doi: 10.1016/S1474-4422(18)30468-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Weller M, van den Bent M, Tonn JC, Stupp R, Preusser M, Cohen-Jonathan-Moyal E, Henriksson R, Le Rhun E, Balana C, Chinot O, et al. European Association for Neuro-Oncology (EANO) guideline on the diagnosis and treatment of adult astrocytic and oligodendroglial gliomas. Lancet Oncol. 2017;18(6):e315–e329. doi: 10.1016/S1470-2045(17)30194-8. [DOI] [PubMed] [Google Scholar]
- 3.Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394–424. doi: 10.3322/caac.21492. [DOI] [PubMed] [Google Scholar]
- 4.Wen PY, Weller M, Lee EQ, Alexander BA, Barnholtz-Sloan JS, Barthel FP, Batchelor TT, Bindra RS, Chang SM, Chiocca EA, et al. Glioblastoma in adults: a Society for Neuro-Oncology (SNO) and European Society of Neuro-Oncology (EANO) consensus review on current management and future directions. Neuro-Oncology. 2020;22(8):1073–1113. doi: 10.1093/neuonc/noaa106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kovacs E, Zorn JA, Huang Y, Barros T, Kuriyan J. A structural perspective on the regulation of the epidermal growth factor receptor. Annu Rev Biochem. 2015;84(1):739–764. doi: 10.1146/annurev-biochem-060614-034402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Arteaga CL, Engelman JA. ERBB receptors: from oncogene discovery to basic science to mechanism-based cancer therapeutics. Cancer Cell. 2014;25(3):282–303. doi: 10.1016/j.ccr.2014.02.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tebbutt N, Pedersen MW, Johns TG. Targeting the ERBB family in cancer: couples therapy. Nat Rev Cancer. 2013;13(9):663–673. doi: 10.1038/nrc3559. [DOI] [PubMed] [Google Scholar]
- 8.Begnami MD, Fukuda E, Fregnani JH, Nonogaki S, Montagnini AL, da Costa WL, Jr., Soares FA: Prognostic implications of altered human epidermal growth factor receptors (HERs) in gastric carcinomas: HER2 and HER3 are predictors of poor outcome. J Clin Oncol 2011, 29(22):3030–6. 10.1200/JCO.2010.33.6313. [DOI] [PubMed]
- 9.Steelman LS, Fitzgerald T, Lertpiriyapong K, Cocco L, Follo MY, Martelli AM, Neri LM, Marmiroli S, Libra M, Candido S, et al. Critical roles of EGFR family members in breast Cancer and breast Cancer stem cells: targets for therapy. Curr Pharm Des. 2016;22(16):2358–2388. doi: 10.2174/1381612822666160304151011. [DOI] [PubMed] [Google Scholar]
- 10.Lu S, Yu Y, Li Z, Yu R, Wu X, Bao H, Ding Y, Shao YW, Jian H. EGFR and ERBB2 Germline mutations in Chinese lung Cancer patients and their roles in genetic susceptibility to Cancer. J Thorac Oncol. 2019;14(4):732–736. doi: 10.1016/j.jtho.2018.12.006. [DOI] [PubMed] [Google Scholar]
- 11.Sampera A, Sanchez-Martin FJ, Arpi O, Visa L, Iglesias M, Menendez S, Gaye E, Dalmases A, Clave S, Gelabert-Baldrich M, et al. HER-family ligands promote acquired resistance to Trastuzumab in gastric Cancer. Mol Cancer Ther. 2019;18(11):2135–2145. doi: 10.1158/1535-7163.MCT-19-0455. [DOI] [PubMed] [Google Scholar]
- 12.Zhang K, Wong P, Salvaggio C, Salhi A, Osman I, Bedogni B. Synchronized targeting of notch and ERBB signaling suppresses melanoma tumor growth through inhibition of Notch1 and ERBB3. J Invest Dermatol. 2016;136(2):464–472. doi: 10.1016/j.jid.2015.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yu J, Hou M, Pei T. FAM83A is a prognosis signature and potential oncogene of lung adenocarcinoma. DNA Cell Biol. 2020;39(5):890–899. doi: 10.1089/dna.2019.4970. [DOI] [PubMed] [Google Scholar]
- 14.Lin W, Chen X, Chen T, Liu J, Ye Y, Chen L, Qiu X, Chia-Hsien Cheng J, Zhang L, Wu J, Qiu S. C1QTNF6 as a novel diagnostic and prognostic biomarker for clear cell renal cell carcinoma. DNA Cell Biol. 2020;39(6):1000–1011. doi: 10.1089/dna.2019.5299. [DOI] [PubMed] [Google Scholar]
- 15.Mei J, Hao L, Liu X, Sun G, Xu R, Wang H, Liu C. Comprehensive analysis of peroxiredoxins expression profiles and prognostic values in breast cancer. Biomarker research. 2019;7(1):16. doi: 10.1186/s40364-019-0168-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chen J, Cai Y, Xu R, Pan J, Zhou J, Mei J. Identification of four hub genes as promising biomarkers to evaluate the prognosis of ovarian cancer in silico. Cancer Cell Int. 2020;20(1):270. doi: 10.1186/s12935-020-01361-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.von Achenbach C, Weller M, Szabo E. Epidermal growth factor receptor and ligand family expression and activity in glioblastoma. J Neurochem. 2018;147(1):99–109. doi: 10.1111/jnc.14538. [DOI] [PubMed] [Google Scholar]
- 18.Clark PA, Iida M, Treisman DM, Kalluri H, Ezhilan S, Zorniak M, Wheeler DL, Kuo JS. Activation of multiple ERBB family receptors mediates glioblastoma cancer stem-like cell resistance to EGFR-targeted inhibition. Neoplasia. 2012;14(5):420–428. doi: 10.1596/neo.12432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rhodes DR, Kalyana-Sundaram S, Mahavisno V, Varambally R, Yu J, Briggs BB, Barrette TR, Anstet MJ, Kincead-Beal C, Kulkarni P, Varambally S, Ghosh D, Chinnaiyan AM. Oncomine 3.0: genes, pathways, and networks in a collection of 18,000 cancer gene expression profiles. Neoplasia. 2007;9(2):166–180. doi: 10.1593/neo.07112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tomczak K, Czerwinska P, Wiznerowicz M. The Cancer genome atlas (TCGA): an immeasurable source of knowledge. Contemp Oncol. 2015;19(1A):A68–A77. doi: 10.5114/wo.2014.47136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wang Z, Wang Z, Zhang C, Liu X, Li G, Liu S, Sun L, Liang J, Hu H, Liu Y, Zhang W, Jiang T. Genetic and clinical characterization of B7-H3 (CD276) expression and epigenetic regulation in diffuse brain glioma. Cancer Sci. 2018;109(9):2697–2705. doi: 10.1111/cas.13744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Li T, Fu J, Zeng Z, Cohen D, Li J, Chen Q, Li B, Liu XS. TIMER2.0 for analysis of tumor-infiltrating immune cells. Nucleic Acids Res. 2020;48(W1):W509–W514. doi: 10.1093/nar/gkaa407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gao J, Aksoy B, Dogrusoz U, Dresdner G, Gross B, Sumer S, Sun Y, Jacobsen A, Sinha R, Larsson E, et al. Integrative analysis of complex cancer genomics and clinical profiles using the cBioPortal. Sci Signal. 2013;6(269):pl1. doi: 10.1126/scisignal.2004088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Franz M, Rodriguez H, Lopes C, Zuberi K, Montojo J, Bader GD, Morris Q. GeneMANIA update 2018. Nucleic Acids Res. 2018;46(W1):W60–W64. doi: 10.1093/nar/gky311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Huang da W, Sherman BT, Lempicki RA: Systematic and integrative analysis of large gene lists using DAVID bioinformatics resources. Nat Protoc 2009;4(1):44–57. [DOI] [PubMed]
- 26.Sun L, Hui AM, Su Q, Vortmeyer A, Kotliarov Y, Pastorino S, Passaniti A, Menon J, Walling J, Bailey R, Rosenblum M, Mikkelsen T, Fine HA. Neuronal and glioma-derived stem cell factor induces angiogenesis within the brain. Cancer Cell. 2006;9(4):287–300. doi: 10.1016/j.ccr.2006.03.003. [DOI] [PubMed] [Google Scholar]
- 27.French PJ, Swagemakers SM, Nagel JH, Kouwenhoven MC, Brouwer E, van der Spek P, Luider TM, Kros JM, van den Bent MJ, Sillevis Smitt PA. Gene expression profiles associated with treatment response in oligodendrogliomas. Cancer Res. 2005;65(24):11335–11344. doi: 10.1158/0008-5472.CAN-05-1886. [DOI] [PubMed] [Google Scholar]
- 28.Lee J, Kotliarova S, Kotliarov Y, Li A, Su Q, Donin NM, Pastorino S, Purow BW, Christopher N, Zhang W, Park JK, Fine HA. Tumor stem cells derived from glioblastomas cultured in bFGF and EGF more closely mirror the phenotype and genotype of primary tumors than do serum-cultured cell lines. Cancer Cell. 2006;9(5):391–403. doi: 10.1016/j.ccr.2006.03.030. [DOI] [PubMed] [Google Scholar]
- 29.Shai R, Shi T, Kremen TJ, Horvath S, Liau LM, Cloughesy TF, Mischel PS, Nelson SF. Gene expression profiling identifies molecular subtypes of gliomas. Oncogene. 2003;22(31):4918–4923. doi: 10.1038/sj.onc.1206753. [DOI] [PubMed] [Google Scholar]
- 30.Bredel M, Bredel C, Juric D, Harsh GR, Vogel H, Recht LD, Sikic BI. Functional network analysis reveals extended gliomagenesis pathway maps and three novel MYC-interacting genes in human gliomas. Cancer Res. 2005;65(19):8679–8689. doi: 10.1158/0008-5472.CAN-05-1204. [DOI] [PubMed] [Google Scholar]
- 31.Murat A, Migliavacca E, Gorlia T, Lambiv WL, Shay T, Hamou MF, de Tribolet N, Regli L, Wick W, Kouwenhoven MC, et al. Stem cell-related "self-renewal" signature and high epidermal growth factor receptor expression associated with resistance to concomitant chemoradiotherapy in glioblastoma. J Clin Oncol. 2008;26(18):3015–3024. doi: 10.1200/JCO.2007.15.7164. [DOI] [PubMed] [Google Scholar]
- 32.Watson MA, Gutmann DH, Peterson K, Chicoine MR, Kleinschmidt-DeMasters BK, Brown HG, Perry A. Molecular characterization of human meningiomas by gene expression profiling using high-density oligonucleotide microarrays. Am J Pathol. 2002;161(2):665–672. doi: 10.1016/S0002-9440(10)64222-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Pomeroy SL, Tamayo P, Gaasenbeek M, Sturla LM, Angelo M, McLaughlin ME, Kim JY, Goumnerova LC, Black PM, Lau C, et al. Prediction of central nervous system embryonal tumour outcome based on gene expression. Nature. 2002;415(6870):436–442. doi: 10.1038/415436a. [DOI] [PubMed] [Google Scholar]
- 34.Picca A, Di Stefano AL, Sanson M. Current and future tools for determination and monitoring of isocitrate dehydrogenase status in gliomas. Curr Opin Neurol. 2018;31(6):727–732. doi: 10.1097/WCO.0000000000000617. [DOI] [PubMed] [Google Scholar]
- 35.Chen JR, Yao Y, Xu HZ, Qin ZY. Isocitrate dehydrogenase (IDH)1/2 mutations as prognostic markers in patients with Glioblastomas. Medicine (Baltimore) 2016;95(9):e2583. doi: 10.1097/MD.0000000000002583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Takada K, Kashiwagi S, Asano Y, Goto W, Kouhashi R, Yabumoto A, Morisaki T, Shibutani M, Takashima T, Fujita H, Hirakawa K, Ohira M. Prediction of lymph node metastasis by tumor-infiltrating lymphocytes in T1 breast cancer. BMC Cancer. 2020;20(1):598. doi: 10.1186/s12885-020-07101-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Caziuc A, Schlanger D, Amarinei G, Dindelegan GC. Can Tumor-Infiltrating Lymphocytes (TILs) Be a Predictive Factor for Lymph Nodes Status in Both Early Stage and Locally Advanced Breast Cancer? J Clin Med. 2019;8(4). [DOI] [PMC free article] [PubMed]
- 38.Greenall SA, Donoghue JF, Gottardo NG, Johns TG, Adams TE. Glioma-specific domain IV EGFR cysteine mutations promote ligand-induced covalent receptor dimerization and display enhanced sensitivity to dacomitinib in vivo. Oncogene. 2015;34(13):1658–1666. doi: 10.1038/onc.2014.106. [DOI] [PubMed] [Google Scholar]
- 39.Saleem H, Kulsoom Abdul U, Kucukosmanoglu A, Houweling M, Cornelissen FMG, Heiland DH, Hegi ME, Kouwenhoven MCM, Bailey D, Wurdinger T, et al. The TICking clock of EGFR therapy resistance in glioblastoma: target Independence or target compensation. Drug Resist Updat. 2019;43:29–37. doi: 10.1016/j.drup.2019.04.002. [DOI] [PubMed] [Google Scholar]
- 40.Boussiotis VA, Charest A. Immunotherapies for malignant glioma. Oncogene. 2018;37(9):1121–1141. doi: 10.1038/s41388-017-0024-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lieberman NAP, DeGolier K, Kovar HM, Davis A, Hoglund V, Stevens J, Winter C, Deutsch G, Furlan SN, Vitanza NA, Leary SES, Crane CA. Characterization of the immune microenvironment of diffuse intrinsic pontine glioma: implications for development of immunotherapy. Neuro-Oncology. 2019;21(1):83–94. doi: 10.1093/neuonc/noy145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Cheng W, Ren X, Zhang C, Cai J, Liu Y, Han S, Wu A. Bioinformatic profiling identifies an immune-related risk signature for glioblastoma. Neurology. 2016;86(24):2226–2234. doi: 10.1212/WNL.0000000000002770. [DOI] [PubMed] [Google Scholar]
- 43.Khasraw M, Reardon DA, Weller M, Sampson JH. PD-1 inhibitors: do they have a future in the treatment of glioblastoma? Clin Cancer Res. 2020. [DOI] [PMC free article] [PubMed]
- 44.Linder M, Glitzner E, Srivatsa S, Bakiri L, Matsuoka K, Shahrouzi P, et al. EGFR is required for FOS-dependent bone tumor development via RSK2/CREB signaling. EMBO Mol Med. 2018;10(11). [DOI] [PMC free article] [PubMed]
- 45.L S, Am H, Q S, A V, Y K, S P, A P, J M, J W, R B, et al. Neuronal and glioma-derived stem cell factor induces angiogenesis within the brain. Cancer Cell. 2006;9(4):287–300. doi: 10.1016/j.ccr.2006.03.003. [DOI] [PubMed] [Google Scholar]
- 46.Roskoski R., Jr Small molecule inhibitors targeting the EGFR/ErbB family of protein-tyrosine kinases in human cancers. Pharmacol Res. 2019;139:395–411. doi: 10.1016/j.phrs.2018.11.014. [DOI] [PubMed] [Google Scholar]
- 47.Hastings K, Yu HA, Wei W, Sanchez-Vega F, DeVeaux M, Choi J, Rizvi H, Lisberg A, Truini A, Lydon CA, Liu Z, Henick BS, Wurtz A, Cai G, Plodkowski AJ, Long NM, Halpenny DF, Killam J, Oliva I, Schultz N, Riely GJ, Arcila ME, Ladanyi M, Zelterman D, Herbst RS, Goldberg SB, Awad MM, Garon EB, Gettinger S, Hellmann MD, Politi K. EGFR mutation subtypes and response to immune checkpoint blockade treatment in non-small-cell lung cancer. Ann Oncol. 2019;30(8):1311–1320. doi: 10.1093/annonc/mdz141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Wang H, Yao F, Luo S, Ma K, Liu M, Bai L, Chen S, Song C, Wang T, Du Q, et al. A mutual activation loop between the Ca(2+)-activated chloride channel TMEM16A and EGFR/STAT3 signaling promotes breast cancer tumorigenesis. Cancer Lett. 2019;455:48–59. doi: 10.1016/j.canlet.2019.04.027. [DOI] [PubMed] [Google Scholar]
- 49.Luo XL, Deng CC, Su XD, Wang F, Chen Z, Wu XP, Liang SB, Liu JH, Fu LW. Loss of MED12 induces tumor dormancy in human epithelial ovarian Cancer via Downregulation of EGFR. Cancer Res. 2018;78(13):3532–3543. doi: 10.1158/0008-5472.CAN-18-0134. [DOI] [PubMed] [Google Scholar]
- 50.Fuse N, Kuboki Y, Kuwata T, Nishina T, Kadowaki S, Shinozaki E, Machida N, Yuki S, Ooki A, Kajiura S, Kimura T, Yamanaka T, Shitara K, Nagatsuma AK, Yoshino T, Ochiai A, Ohtsu A. Prognostic impact of HER2, EGFR, and c-MET status on overall survival of advanced gastric cancer patients. Gastric Cancer. 2016;19(1):183–191. doi: 10.1007/s10120-015-0471-6. [DOI] [PubMed] [Google Scholar]
- 51.Chen T, Zhou L, Li H, Tian Y, Li J, Dong L, Zhao Y, Wei D. Fatty acid synthase affects expression of ErbB receptors in epithelial to mesenchymal transition of breast cancer cells and invasive ductal carcinoma. Oncol Lett. 2017;14(5):5934–5946. doi: 10.3892/ol.2017.6954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Zoi I, Karamouzis MV, Adamopoulos C, Papavassiliou AG. RANKL signaling and ErbB receptors in breast carcinogenesis. Trends Mol Med. 2016;22(10):839–850. doi: 10.1016/j.molmed.2016.07.009. [DOI] [PubMed] [Google Scholar]
- 53.Pernas S, Barroso-Sousa R, Tolaney SM. Optimal treatment of early stage HER2-positive breast cancer. Cancer. 2018;124(23):4455–4466. doi: 10.1002/cncr.31657. [DOI] [PubMed] [Google Scholar]
- 54.Cortes J, Dieras V, Lorenzen S, Montemurro F, Riera-Knorrenschild J, Thuss-Patience P, Allegrini G, De Laurentiis M, Lohrisch C, Oravcova E, et al. Efficacy and safety of Trastuzumab Emtansine plus Capecitabine vs Trastuzumab Emtansine alone in patients with previously treated ERBB2 (HER2)-positive metastatic breast Cancer: a phase 1 and randomized phase 2 trial. JAMA Oncol. 2020;6(8):1203–1209. doi: 10.1001/jamaoncol.2020.1796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Yu TT, Wang CY, Tong R. ERBB2 gene expression silencing involved in ovarian cancer cell migration and invasion through mediating MAPK1/MAPK3 signaling pathway. Eur Rev Med Pharmacol Sci. 2020;24(10):5267–5280. doi: 10.26355/eurrev_202005_21309. [DOI] [PubMed] [Google Scholar]
- 56.Fan Y, Qiu J, Yu R, Cao R, Chen X, Ou Q, Wu X, Shao YW, Nagasaka M, Zhang J, Ou SHI. Clinical and molecular characteristics of Chinese non-small cell lung cancer patients with ERBB2 transmembrane domain mutations. Mol Oncol. 2020;14(8):1731–1739. doi: 10.1002/1878-0261.12733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Wang DS, Liu ZX, Lu YX, Bao H, Wu X, Zeng ZL, Liu Z, Zhao Q, He CY, Lu JH, Wang ZQ, Qiu MZ, Wang F, Wang FH, Li YH, Wang XN, Xie D, Jia WH, Shao YW, Xu RH. Liquid biopsies to track trastuzumab resistance in metastatic HER2-positive gastric cancer. Gut. 2019;68(7):1152–1161. doi: 10.1136/gutjnl-2018-316522. [DOI] [PubMed] [Google Scholar]
- 58.Mei J, Wang TJ, Xu R, Chen DZ, Zhang Y. Clinical and molecular immune characterization of ERBB2 in glioma. Int Immunopharmacol. 2021;94:107499. 10.1016/j.intimp.2021.107499. [DOI] [PubMed]
- 59.Shin DH, Jo JY, Han JY. Dual targeting of ERBB2/ERBB3 for the treatment of SLC3A2-NRG1-mediated lung Cancer. Mol Cancer Ther. 2018;17(9):2024–2033. doi: 10.1158/1535-7163.MCT-17-1178. [DOI] [PubMed] [Google Scholar]
- 60.Bittner AK, Keup C, Hoffmann O, Hauch S, Kimmig R, Kasimir-Bauer S. Molecular characterization of circulating tumour cells identifies predictive markers for outcome in primary, triple-negative breast cancer patients. J Cell Mol Med. 2020;24(15):8405–8416. doi: 10.1111/jcmm.15349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Li X, Zhao J, Zhang H, Cai J. Silencing of LncRNA metastasis-associated lung adenocarcinoma transcript 1 inhibits the proliferation and promotes the apoptosis of gastric Cancer cells through regulating microRNA-22-3p-mediated ErbB3. Onco Targets Ther. 2020;13:559–571. doi: 10.2147/OTT.S222375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Chen C, Gupta P, Parashar D, Nair GG, George J, Geethadevi A, Wang W, Tsaih SW, Bradley W, Ramchandran R, Rader JS, Chaluvally-Raghavan P, Pradeep S. ERBB3-induced furin promotes the progression and metastasis of ovarian cancer via the IGF1R/STAT3 signaling axis. Oncogene. 2020;39(14):2921–2933. doi: 10.1038/s41388-020-1194-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Brizzolara A, Benelli R, Vene R, Barboro P, Poggi A, Tosetti F, Ferrari N. The ErbB family and androgen receptor signaling are targets of Celecoxib in prostate cancer. Cancer Lett. 2017;400:9–17. doi: 10.1016/j.canlet.2017.04.025. [DOI] [PubMed] [Google Scholar]
- 64.Segers VFM, Dugaucquier L, Feyen E, Shakeri H, De Keulenaer GW. The role of ErbB4 in cancer. Cell Oncol. 2020;43(3):335–352. doi: 10.1007/s13402-020-00499-4. [DOI] [PubMed] [Google Scholar]
- 65.Nie H, Mei J, Zhang Q, An F, Zhan Q. Systematic characterization of the expression and prognostic values of Formin-like gene family in gastric Cancer. DNA Cell Biol. 2020;39(9):1664–1677. doi: 10.1089/dna.2020.5508. [DOI] [PubMed] [Google Scholar]
- 66.Giraldo NA, Becht E, Vano Y, Petitprez F, Lacroix L, Validire P, Sanchez-Salas R, Ingels A, Oudard S, Moatti A, Buttard B, Bourass S, Germain C, Cathelineau X, Fridman WH, Sautès-Fridman C. Tumor-infiltrating and peripheral blood T-cell Immunophenotypes predict early relapse in localized clear cell renal cell carcinoma. Clin Cancer Res. 2017;23(15):4416–4428. doi: 10.1158/1078-0432.CCR-16-2848. [DOI] [PubMed] [Google Scholar]
- 67.Zhao B, Wang Y, Wang Y, Chen W, Liu PH, Kong Z, et al. Systematic identification, development, and validation of prognostic biomarkers involving the tumor-immune microenvironment for glioblastoma. J Cell Physiol. 2020. [DOI] [PubMed]
- 68.Baig M, Zhang QW, Younis MR, Xia XH. A DNA Nanodevice simultaneously activating the EGFR and integrin for enhancing cytoskeletal activity and Cancer cell treatment. Nano Lett. 2019;19(10):7503–7513. doi: 10.1021/acs.nanolett.9b03325. [DOI] [PubMed] [Google Scholar]
- 69.Li KJ, Siao SC, Wu CH, Shen CY, Wu TH, Tsai CY, Hsieh SC, Yu CL. EGF receptor-dependent mechanism may be involved in the Tamm-Horsfall glycoprotein-enhanced PMN phagocytosis via activating rho family and MAPK signaling pathway. Molecules. 2014;19(1):1328–1343. doi: 10.3390/molecules19011328. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets analyzed for this study were obtained from the Oncomine database (https://www.oncomine.org/), the UCSC Xena website (https://xenabrowser.net/datapages/) and the CGGA dataset (mRNAseq_325) (http://www.cgga.org.cn/index.jsp), the TIMER (https://cistrome.shinyapps.io/timer/) website, the cBioPortal (https://www.cbioportal.org/) and the GeneMANIA databases (http://www.genemania.org/), and DAVID (https://david.ncifcrf.gov/).