Abstract
Background
Whether a modestly elevated homocysteine level is causally associated with an increased risk of cardiovascular disease remains unestablished. We conducted a Mendelian randomization study to assess the associations of circulating total homocysteine (tHcy) and B vitamin levels with cardiovascular diseases in the general population.
Methods
Independent single nucleotide polymorphisms associated with tHcy (n = 14), folate (n = 2), vitamin B6 (n = 1), and vitamin B12 (n = 14) at the genome-wide significance level were selected as instrumental variables. Summary-level data for 12 cardiovascular endpoints were obtained from genetic consortia, the UK Biobank study, and the FinnGen consortium.
Results
Higher genetically predicted circulating tHcy levels were associated with an increased risk of stroke. For each one standard deviation (SD) increase in genetically predicted tHcy levels, the odds ratio (OR) was 1.11 (95% confidence interval (CI), 1.03, 1.21; p = 0.008) for any stroke, 1.26 (95% CI, 1.05, 1.51; p = 0.013) for subarachnoid hemorrhage, and 1.11 (95% CI, 1.03, 1.21; p = 0.011) for ischemic stroke. Higher genetically predicted folate levels were associated with decreased risk of coronary artery disease (ORSD, 0.88; 95% CI, 0.78, 1.00, p = 0.049) and any stroke (ORSD, 0.86; 95% CI, 0.76, 0.97, p = 0.012). Genetically predicted increased vitamin B6 levels were associated with a reduced risk of ischemic stroke (ORSD, 0.88; 95% CI, 0.81, 0.97, p = 0.009). None of these associations persisted after multiple testing correction. There was no association between genetically predicted vitamin B12 and cardiovascular disease.
Conclusions
This study reveals suggestive evidence that B vitamin therapy and lowering of tHcy may reduce the risk of stroke, particularly subarachnoid hemorrhage and ischemic stroke.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12916-021-01977-8.
Keywords: Cardiovascular disease, Homocysteine, Mendelian randomization, B vitamins
Background
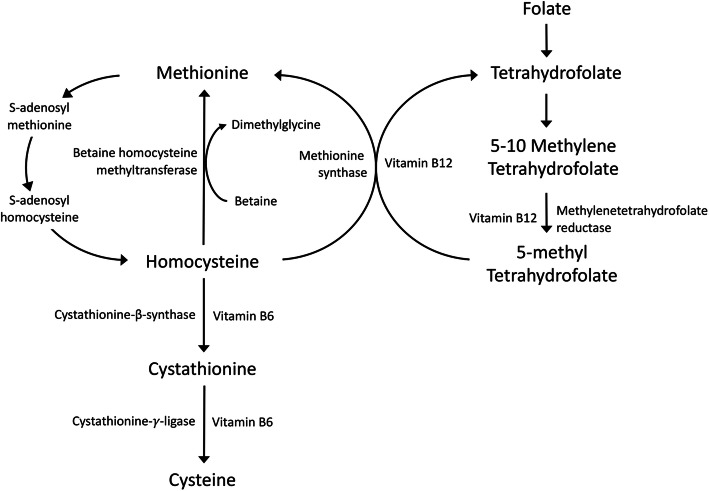
The B vitamins, including folate and vitamins B6 and B12, play vital roles in the metabolism of homocysteine (Fig. 1) [1]. Deficiency of either of these B vitamins can lead to an elevated circulating level of total homocysteine (tHcy), which has been implicated in the development of cardiovascular disease (CVD) [2–5]. The association has been supported by several possible underlying pathophysiologic mechanisms, such as impaired endothelial function, increased oxidative stress, induced vascular inflammation, stimulated vascular smooth muscle cell proliferation, and activated coagulation factors by homocysteinemia [1]. However, randomized controlled trials (RCTs) have generally not detected a protective effect of homocysteine-lowering therapy with B vitamins on total CVD [6–8] or coronary artery disease [4, 6]. Findings of corresponding RCTs on stroke are inconclusive [9–12]. Potential explanations for the inconsistent results may be related to small sample sizes, low adherence to the treatment, and different study populations and CVD outcomes.
Fig. 1.
Overview of folate, vitamin B6, and vitamin B12 in homocysteine metabolism. Homocysteine is reconverted to methionine by receiving a methyl group from 5-methyltetrahydrofolate, the active form of folate, or betaine in the remethylation pathway. Irreversible removal of homocysteine occurs through the transsulphuration pathway where homocysteine condenses with serine to form cystathionine
Using genetic variants as instrumental variables for an exposure (e.g., tHcy), the Mendelian randomization (MR) design can strengthen the causal inference by minimizing residual confounding and reverse causation. Previous MR studies showed that tHcy levels proxied by a single nucleotide polymorphism (SNP) in the MTHFR gene region were associated with stroke [13] and imaging burden of cerebral small vessel disease [14], but not with coronary artery disease [15, 16]. Studies utilizing more SNPs suggested a positive association of genetically predicted tHcy levels with risk of ischemic stroke, especially small vessel stroke [17], but no association with coronary artery disease [17–19] and atrial fibrillation [20]. Data are scarce for other cardiovascular diseases (CVDs).
Here, we conducted an MR study to assess the associations of genetically predicted tHcy levels with a wide range of CVDs. We also examined the associations of genetically predicted levels of folate and vitamins B6 and B12 with CVDs.
Methods
Outcome data sources
Summary-level data for 12 CVD endpoints were obtained from large genetic consortia [21–26], the UK Biobank study [27] and the FinnGen consortium [28]. Detailed descriptions on data sources are presented in Table 1.
Table 1.
Information on outcome data sources
| Data source | Cardiovascular disease | Population | Cases | Controls | Covariates adjusted in GWAS |
|---|---|---|---|---|---|
| Consortium (Nielsen et al.) | Atrial fibrillation | European | 60,620 | 970,216 | Birth year, sex, genotype batch, and one to four principal components |
| CARDIoGRAMplusC4D+UKBB | Coronary artery disease | Mixed | 122,733 | 424,528 | Not reported |
| HERMES consortium | Heart failure | European | 47,309 | 930,014 | Age and sex, and principal components in individual studies where applicable |
| MEGASTROKE consortium | Stroke | 40,585 | 406,111 | Age and sex | |
| Ischemic stroke | 34,217 | NA | |||
| ISGC | Intracerebral hemorrhage | European | 3223 | 3725 | Age, sex, and principal components |
| Consortium (Bakker et al.) | Subarachnoid hemorrhage | European | 7495 | 71,934 | Not reported |
| The UK Biobank study (UKBB) | Aortic aneurysm | European | 2261 | 365,300 | Age, sex, and ten genetic principal components |
| Aortic valve stenosis | 3528 | 364,033 | |||
| Stroke | 12,036 | 355,525 | |||
| Intracerebral hemorrhage | 1504 | 366,057 | |||
| Ischemic stroke | 6566 | 360,995 | |||
| Transient ischemic attack | 4813 | 362,748 | |||
| Venous thromboembolism | 16,412 | 351,149 | |||
| Peripheral vessel disease | 4593 | 362,968 | |||
| The FinnGen consortium | Aortic aneurysm | European | 1919 | 167,843 | Age, sex, the first ten genetic principal components, and genotyping batch |
| Atrial fibrillation | 17,325 | 97,214 | |||
| Coronary artery disease | 16,631 | 160,268 | |||
| Heart failure | 9576 | 159,286 | |||
| Stroke | 14,171 | 133,027 | |||
| Intracerebral hemorrhage | 1224 | 163,533 | |||
| Subarachnoid hemorrhage | 1019 | 163,508 | |||
| Ischemic stroke | 8046 | 164,286 | |||
| Transient ischemic attack | 6729 | 164,286 | |||
| Venous thromboembolism | 6913 | 169,986 | |||
| Peripheral vessel disease | 5323 | 167,843 |
CARDIoGRAMplusC4D Coronary ARtery DIsease Genome wide Replication and Meta-analysis plus The Coronary Artery Disease Genetics, GWAS genome-wide association study, HERMES Heart Failure Molecular Epidemiology for Therapeutic Targets, ISGC International Stroke Genetic Consortium, NA not available. The UK Biobank was included in Consortium (Nielsen et al.), HERMES consortium, ISGC, and Consortium (Bakker et al.)
Instrument selection
SNPs associated with tHcy and B vitamins were identified at the genome-wide significance threshold (p < 5 × 10−8) from meta-analyses of genome-wide association studies on tHcy (n = 44,147 individuals) [29], folate (n = 37,465 individuals) [30], vitamin B6 (n = 1864 individuals) [31], and vitamin B12 (n = 45,576 individuals) [30] in individuals of European ancestry. Linkage disequilibrium among SNPs for one exposure was estimated using PLINK clumping method based on 1000 Genomes European reference panel. Independent SNPs without linkage disequilibrium (r2 < 0.01 and clump window > 10 kb) were used as instrumental variables (Supplementary Table 1). The SNPs explained 6.0% of variance for tHcy [29], 1.0% of variance for folate [30], 1.3% of variance for vitamin B6 [31], and 6.0% of variance for vitamin B12 [30]. Proxy SNPs (r2 > 0.8) were used for specific tHcy- or B vitamin-associated SNPs that were unavailable in outcome datasets. Missing SNPs without suitable proxies were excluded from analyses.
Statistical analysis
We used the multiplicative random-effects inverse-variance-weighted model [32] as the main analysis. Estimates for one CVD endpoint from different sources were combined using the fixed-effects meta-analysis method. Three sensitivity analyses, including the weighted median [33], MR-Egger [34], and MR-PRESSO [35] approaches, were performed for tHcy and vitamin B12. The weighted median model generates consistent causal estimates assuming that more than a half of the weights derive from valid SNPs [33]. The MR-Egger regression can detect horizontal pleiotropy by p value for its intercept and provide estimate after correction for pleiotropic effects under the instrument strength independent of direct effect assumption although it consumes statistical power [34]. The MR-PRESSO method can detect outlying SNPs and provide causal estimates after removal of possible outliers under the assumption that the used SNPs are valid [35]. By searching phenotypes associated with used SNPs for tHcy in PhenoScanner V2 [36] (Supplementary Table 2), 4 SNPs (rs1047891, rs548987, rs2251468, and rs838133 [37]) associated with blood lipids and other traits were likely to exert pleiotropic effects. We performed additional sensitivity analysis with the exclusion of these 4 SNPs. The I2 statistic was calculated to assess the degree of heterogeneity [38] among estimates of SNPs in each analysis. Power was estimated using an online tool (Supplementary Table 3) [39]. The odds ratios (ORs) and corresponding 95% confidence intervals (CIs) of CVDs were scaled to one-standard deviation (SD) increase in genetically predicted circulating levels of tHcy and B vitamins. We used a conservative Bonferroni-based p value threshold of 0.001, accounting for 4 exposures and 12 outcomes. Associations with a p value between the Bonferroni-corrected significance level and the conventional significance level (i.e., < 0.05) were deemed as suggestive associations. All p values were two-sided and analyses were performed using the mrrobust package [40] in Stata/SE 15.0 and the TwoSampleMR package [41] in R Software 3.6.0.
Results
We observed suggestive associations of higher genetically predicted circulating tHcy levels with increased risk of any stroke, subarachnoid hemorrhage, and ischemic stroke (Fig. 2). For 1-SD increase in genetically predicted tHcy levels, the combined OR was 1.11 (95% CI, 1.03, 1.21; p = 0.008) for stroke, 1.26 (95% CI, 1.05, 1.51; p = 0.013) for subarachnoid hemorrhage, and 1.11 (95% CI, 1.03, 1.21; p = 0.011) for ischemic stroke. Results remained directionally consistent in the weighted median model (Supplementary Table 4). We noticed moderate heterogeneity in the analyses of stroke and ischemic stroke and possible pleiotropy in the MR-Egger analysis for ischemic stroke in FinnGen (Supplementary Table 4). Genetically predicted tHcy levels were not associated with any of other studied CVDs (Fig. 2). One to three outliers were identified in the MR-PRESSO analysis. The results remained overall consistent in the MR-PRESSO analysis after the removal of outliers (Supplementary Table 5). In the sensitivity analysis with exclusion of 4 pleiotropic SNPs, the associations remained (Supplementary Table 6). For 1-SD increase in genetically predicted tHcy levels, the combined OR was 1.14 (95% CI, 1.04, 1.24; p = 0.003) for stroke, 1.26 (95% CI, 1.03, 1.53; p = 0.024) for subarachnoid hemorrhage and 1.15 (95% CI, 1.04, 1.27; p = 0.002) for ischemic stroke.
Fig. 2.
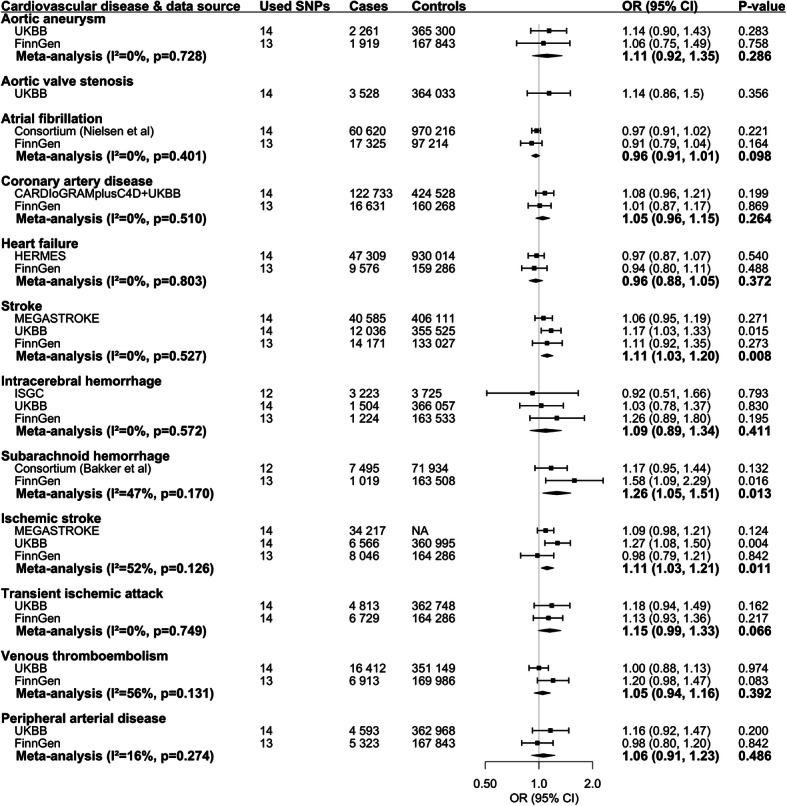
Associations of genetically predicted circulating homocysteine levels with risk of cardiovascular diseases. CARDIoGRAMplusC4D, Coronary ARtery DIsease Genome wide Replication and Meta-analysis plus The Coronary Artery Disease Genetics; CI, confidence interval; CVD, cardiovascular disease; HERMES; Heart Failure Molecular Epidemiology for Therapeutic Targets; ISGC, International Stroke Genetic Consortium; OR, odds ratio; UKBB, UK Biobank. The UK Biobank was included in Consortium (Nielsen et al.), HERMES consortium, ISGC, and Consortium (Bakker et al.)
The associations of genetically predicted circulating B vitamins with CVDs are shown in Supplementary Figure 1 to 3. There were suggestive associations of higher genetically predicted folate levels with decreased risk of coronary artery disease (ORSD, 0.88; 95% CI, 0.78, 1.00, p = 0.049) and any stroke (ORSD, 0.86; 95% CI, 0.76, 0.97, p = 0.012) (Supplementary Figure 1) as well as between higher genetically predicted vitamin B6 levels and lower risk of ischemic stroke (ORSD, 0.88; 95% CI, 0.81, 0.97, p = 0.009) and higher risk of peripheral artery disease (ORSD, 1.30; 95% CI, 1.09, 1.54, p = 0.004) (Supplementary Figure 2). Genetically predicted vitamin B12 levels were not associated with any CVD (Supplementary Figure 3 and Supplementary Table 5 and 7).
Discussion
This MR study investigated the potential causal role of circulating tHcy and B vitamins in a broad range of CVDs and revealed suggestive associations of higher genetically predicted tHcy levels with increased risk of any stroke, subarachnoid hemorrhage, and ischemic stroke. Furthermore, higher genetically predicted levels of folate and vitamin B6 were suggestively associated with a reduced risk of any stroke and ischemic stroke, respectively. Higher genetically predicted folate levels were additionally associated with a suggestive lower risk of coronary artery disease, whereas genetically predicted vitamin B6 levels showed a suggestive positive association with risk of peripheral artery disease. There was no evidence in support of any association between genetically predicted vitamin B12 levels and the 12 studied CVDs.
The detrimental role of tHcy in stroke, especially in ischemic stroke and small vessel disease, has been established in a large body of observational studies [3, 10], MR studies [13, 14, 17] and RCTs [42]. The present study confirmed such potential benefit of homocysteine-lowing therapy with B vitamins in the primary prevention of stroke. Nevertheless, this study did not support an association between genetically predicted vitamin B12 and stroke, which is in line with results of subgroup analyses for vitamin B12 supplementation and baseline blood vitamin B12 levels in relation to risk of stroke in a meta-analysis of 14 RCTs [10]. A possible explanation may be that vitamin B12 generates little impact on tHcy levels [17]. In a meta-analysis of 12 RCTs, daily folic acid (synthetic form of folate) supplementation reduced blood homocysteine levels by 25% and vitamin B12 supplementation produced an additional 7% reduction in blood homocysteine [43].
From a mechanistic perspective, homocysteinemia may increase the risk of ischemic stroke via several pathways. Excessive homocysteine can directly impair neuronal cells and blood-brain barrier function by promoting oxidative stress, protein homocysteinylation, and Ca2+ dysregulation. In addition, homocysteine can induce deoxyribonucleic acid hypomethylation and worsen apoptosis, neuronal death, and blood-brain barrier dysregulation [44]. Such actions can promote damage to brain parenchyma and susceptibility to damage from ischemic stroke [44]. Furthermore, the intact vascular endothelium is integral for preventing cardiovascular sequelae such as ischemic stroke, and high levels of homocysteine can also promote endothelial dysfunction in multiple ways. This includes increased oxidant stress, decreased bioavailability of nitric oxide, increased endothelial inflammation with expression of vascular adhesion molecules and leukocyte recruitment, increased platelet activation, and promotion of thrombosis [1, 45]. Together these consequences of the dysfunctional endothelium promote all stages of ischemic stroke from early atherosclerosis development through to thrombosis and this is likely to be an important mechanism contributing to the excess ischemic stroke risk which is established in patients with high levels of homocysteine.
Studies on homocysteine in relation to hemorrhagic stroke are scarce and conflicting. A meta-analysis of two prospective studies [46] and another cohort study [47] found that blood homocysteine was not associated with the risk of hemorrhagic stroke. A positive association between blood tHcy and hemorrhagic stroke was revealed in a meta-analysis of 7 studies including 667 patients with intracerebral hemorrhage [48]. However, this positive association was not replicated in a study that found no difference in the frequency of the T allele in the SNP located in the MTHFR gene between intracerebral hemorrhage cases and controls [49]. In another case-control study, genetic polymorphisms of homocysteine metabolism showed an association with risk of intracranial aneurysms [50]. The present study based on more tHcy-associated SNPs and hemorrhagic stroke cases suggested that an elevated level of tHcy appeared to be a risk factor for subarachnoid hemorrhage. Nevertheless, we did not observe any clear pattern of association between genetically proxied B vitamins and subarachnoid hemorrhage. Thus, more study is warranted to confirm our findings.
Circulating levels of tHcy have been associated with risk of coronary artery disease in observational studies [51]. However, this association was not replicated in the present and previous MR studies [15, 16, 18, 19]. This discrepancy may indicate that tHcy is likely to be a risk marker instead of a causal risk factor for coronary artery disease. Notably, we observed a weak protective effect of genetically predicted folate levels on coronary artery disease risk which corroborates observational findings [52, 53], although folic acid supplementation was not found to impact coronary artery disease risk in RCTs [42]. However, folic acid improved flow-mediated endothelial vasodilator function in multiple clinical intervention trials using this as a surrogate marker for cardiovascular disease risk [54]. A protective effect of folic acid on coronary artery disease is therefore likely to be mediated by improved endothelial function [55], and importantly, many of these studies were in hyperhomocysteinemic patients specifically [56, 57]. As folate supplementation is known to reduce homocysteine levels [43], this may be one such mechanism for our finding. Other mechanisms may include the antioxidant potential of folate or its interactions with eNOS which is atheroprotective [54]. Lastly, some diagnoses of coronary artery disease may represent angina or type 2 myocardial infarctions due to anemia, and it is plausible that higher folate levels may prevent such diagnoses, although this is unlikely to explain our findings on the population level. Our finding of reduced coronary artery disease risk with higher folate levels requires further investigation and is likely to be mediated by improved endothelial function.
The present study has several strengths and limitations. The major merit is the MR design, which reinforced the causal inference by diminishing residual confounding and other biases. In addition, we investigated the associations of genetically predicted tHcy and B vitamins with CVDs using several independent data sources, which guaranteed the robustness of our findings. In addition, we combined results based on non-overlapping data sources to increase the sample size, especially for infrequent endpoints. This study also employed more SNPs, which explained more phenotypic variance, to proxy circulating levels of tHcy and B vitamins. Thus, our findings should be more statistically powered even though certain weak associations might still have been overlooked. We confined the population in the present study to individuals of European ancestry to minimize population structure bias, with the exception for the analysis for coronary artery disease, which might be challenged by bias from ethnicity, based on consortium data where European individuals comprised over 80% of participants. Nevertheless, this population confinement limited the generalizability of our findings to other populations.
The instrumental variables for folate and vitamin B12 have been validated by using pernicious anemia and mean corpuscular volume as positive controls [58]. With regard to tHcy, several of its related SNPs are located in genes (e.g., MTHFR, MTR, and CBS) encoding enzymes in the metabolism of homocysteine. However, whether the SNP for vitamin B6 was valid remained uncertain given that no suitable positive control was tested, and the corresponding SNP was derived from a GWAS based on a small sample size [31], albeit with replication in another GWAS [59]. Thus, the observed associations for genetically predicted vitamin B6 need verification, especially the positive association for peripheral artery disease, which is conflicting with the observational finding [53]. Another limitation is the possibility of pleiotropy. However, our sensitivity analyses generated directionally consistent results albeit with wider CIs caused by inadequate power [33], and the MR-Egger regression (not for the analyses of folate and vitamin B6 due to few SNPs) indicated no pleiotropic effect in most analyses, which suggest that pleiotropy did not bias our results. In detail, some tHcy-associated SNPs influence the genetically predisposition to other cardiovascular risk factors, such as blood pressure and high-density lipoprotein cholesterol [17]. These factors exert pan-effects on a wide range of cardiovascular disease. Thus, a few of specific associations detected in the present study were less likely to be driven by these pleiotropic effects. In addition, high blood pressure and imbalanced lipids fraction might be consequence of endothelial dysfunction as well as altered lipoprotein metabolism caused by high levels of homocysteine [1]. Whether these traits belonged to horizontal pleiotropic factors or mediators named as horizontal pleiotropic factor in MR remained unknown. Canalization (e.g., genetic buffering or developmental compensation) might bias the MR results; however, the magnitude of this issue in MR analysis has not been well-understood yet [60]. In addition, we did multiple-testing adjustment based on the Bonferroni method, which might be too stringent to inflate risk of false-negative findings (type 2 errors).
Conclusions
This MR study provides limited evidence in support of a general benefit of lowering tHcy levels in the prevention of a broad range of CVDs in the general population. Nevertheless, our findings confirm and extend the evidence that B vitamin therapy lowering tHcy may play a role in the prevention of stroke, especially ischemic stroke and possibly subarachnoid hemorrhage.
Supplementary Information
Acknowledgements
The authors thank the Consortium (Nielsen et al.), CARDIoGRAMplusC4D (Coronary ARtery DIsease Genome wide Replication and Meta-analysis plus The Coronary Artery Disease Genetics), HERMES (Heart Failure Molecular Epidemiology for Therapeutic Targets) consortium, MEGASTROKE, ISGC (International Stroke Genetic Consortium), Consortium (Bakker et al.), the UK Biobank study, and the FinnGen consortium. The MEGASTROKE project received funding from sources specified at http://www.megastroke.org/acknowledgments.html. The author list of MEGASTROKE is listed in https://www.megastroke.org/authors.html. Analyses of UK Biobank data were performed under application 29202.
Authors’ contributions
Study conception and design: SY and SCL; data acquisition and analysis: SY, AMM, SB, and SCL; drafting the manuscript and figures: SY; reviewing the manuscript: SY, AMM, PC, SB, and S.C.L. The authors read and approved the final manuscript.
Funding
AMM is supported by EC-Innovative Medicines Initiative (BigData@Heart). SB is supported by Sir Henry Dale Fellowship jointly funded by the Wellcome Trust and the Royal Society (204623/Z/16/Z). SCL is supported by research grants from the Karolinska Institutet’s Research Foundation Grants (Grant number 2020-01842); the Swedish Research Council for Health, Working Life and Welfare (Forte; grant no. 2018-00123); the Swedish Research Council (Vetenskapsrådet; grant no. 2016-01042 and 2019-00977); and the Swedish Heart-Lung Foundation (Hjärt-Lungfonden; grant no. 20190247). Funders had no roles in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; or the decision to submit the manuscript for publication. Open Access funding provided by Karolinska Institute.
Availability of data and materials
All data analyzed in this study are available OSF data respiratory (https://osf.io/527zy/).
Declarations
Ethics approval and consent to participate
All studies included in cited genome-wide association studies had been approved by a relevant review board, and participants had provided written informed consent. The present MR analyses were approved by the Swedish Ethical Review Authority (2019-02793).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Kaul S, Zadeh AA, Shah PK. Homocysteine hypothesis for atherothrombotic cardiovascular disease: not validated. J Am Coll Cardiol. 2006;48(5):914–923. doi: 10.1016/j.jacc.2006.04.086. [DOI] [PubMed] [Google Scholar]
- 2.Klerk M, Verhoef P, Clarke R, Blom HJ, Kok FJ, Schouten EG. MTHFR 677C-->T polymorphism and risk of coronary heart disease: a meta-analysis. JAMA. 2002;288(16):2023–2031. doi: 10.1001/jama.288.16.2023. [DOI] [PubMed] [Google Scholar]
- 3.Homocysteine and risk of ischemic heart disease and stroke: a meta-analysis. JAMA. 2002, 288(16):2015–2022. [DOI] [PubMed]
- 4.Wald DS, Law M, Morris JK. Homocysteine and cardiovascular disease: evidence on causality from a meta-analysis. BMJ. 2002;325(7374):1202–1206. doi: 10.1136/bmj.325.7374.1202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Holmes MV, Newcombe P, Hubacek JA, Sofat R, Ricketts SL, Cooper J, Breteler MM, Bautista LE, Sharma P, Whittaker JC, et al. Effect modification by population dietary folate on the association between MTHFR genotype, homocysteine, and stroke risk: a meta-analysis of genetic studies and randomised trials. Lancet. 2011;378(9791):584–594. doi: 10.1016/S0140-6736(11)60872-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zhou C, Wu J, Fang S. Meta-analysis of B vitamin supplementation on plasma homocysteine, cardiovascular and all-cause mortality. Clin Nutr. 2013;32(2):314. doi: 10.1016/j.clnu.2013.01.001. [DOI] [PubMed] [Google Scholar]
- 7.Clarke R, Halsey J, Lewington S, Lonn E, Armitage J, Manson JE, Bønaa KH, Spence JD, Nygård O, Jamison R, Gaziano JM, Guarino P, Bennett D, Mir F, Peto R, Collins R, B-Vitamin Treatment Trialists’ Collaboration Effects of lowering homocysteine levels with B vitamins on cardiovascular disease, cancer, and cause-specific mortality: meta-analysis of 8 randomized trials involving 37 485 individuals. Arch Intern Med. 2010;170(18):1622–1631. doi: 10.1001/archinternmed.2010.348. [DOI] [PubMed] [Google Scholar]
- 8.Schnyder G, Roffi M, Flammer Y, Pin R, Hess OM. Effect of homocysteine-lowering therapy with folic acid, vitamin B12, and vitamin B6 on clinical outcome after percutaneous coronary intervention: the Swiss Heart study: a randomized controlled trial. JAMA. 2002;288(8):973–979. doi: 10.1001/jama.288.8.973. [DOI] [PubMed] [Google Scholar]
- 9.Zhang C, Wang ZY, Qin YY, Yu FF, Zhou YH. Association between B vitamins supplementation and risk of cardiovascular outcomes: a cumulative meta-analysis of randomized controlled trials. Plos One. 2014;9(9):e107060. doi: 10.1371/journal.pone.0107060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ji Y, Tan S, Xu Y, Chandra A, Shi C, Song B, Qin J, Gao Y. Vitamin B supplementation, homocysteine levels, and the risk of cerebrovascular disease: a meta-analysis. Neurology. 2013;81(15):1298–1307. doi: 10.1212/WNL.0b013e3182a823cc. [DOI] [PubMed] [Google Scholar]
- 11.Wald DS, Wald NJ, Morris JK, Law M. Folic acid, homocysteine, and cardiovascular disease: judging causality in the face of inconclusive trial evidence. BMJ. 2006;333(7578):1114–1117. doi: 10.1136/bmj.39000.486701.68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Spence JD, Yi Q, Hankey GJ. B vitamins in stroke prevention: time to reconsider. Lancet Neurol. 2017;16(9):750–760. doi: 10.1016/S1474-4422(17)30180-1. [DOI] [PubMed] [Google Scholar]
- 13.Casas JP, Bautista LE, Smeeth L, Sharma P, Hingorani AD. Homocysteine and stroke: evidence on a causal link from mendelian randomisation. Lancet. 2005;365(9455):224–232. doi: 10.1016/S0140-6736(05)70152-5. [DOI] [PubMed] [Google Scholar]
- 14.Cao Y, Su N, Zhang D, Zhou L, Yao M, Zhang S, Cui L, Zhu Y, Ni J. Correlation between total homocysteine and cerebral small vessel disease: a mendelian randomization study. Eur J Neurol. 2020. 10.1111/ene.14708. [DOI] [PubMed]
- 15.Lewis SJ, Ebrahim S, Davey Smith G. Meta-analysis of MTHFR 677C->T polymorphism and coronary heart disease: does totality of evidence support causal role for homocysteine and preventive potential of folate? Bmj. 2005;331(7524):1053. doi: 10.1136/bmj.38611.658947.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Clarke R, Bennett DA, Parish S, Verhoef P, Dötsch-Klerk M, Lathrop M, Xu P, Nordestgaard BG, Holm H, Hopewell JC, Saleheen D, Tanaka T, Anand SS, Chambers JC, Kleber ME, Ouwehand WH, Yamada Y, Elbers C, Peters B, Stewart AFR, Reilly MM, Thorand B, Yusuf S, Engert JC, Assimes TL, Kooner J, Danesh J, Watkins H, Samani NJ, Collins R, Peto R, for the MTHFR Studies Collaborative Group. Homocysteine and coronary heart disease: meta-analysis of MTHFR case-control studies, avoiding publication bias. Plos Med. 2012;9(2):e1001177. 10.1371/journal.pmed.1001177. [DOI] [PMC free article] [PubMed]
- 17.Larsson SC, Traylor M, Markus HS. Homocysteine and small vessel stroke: a mendelian randomization analysis. Ann Neurol. 2019;85(4):495–501. doi: 10.1002/ana.25440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zhao JV, Schooling CM. Homocysteine-reducing B vitamins and ischemic heart disease: a separate-sample Mendelian randomization analysis. Eur J Clin Nutr. 2017;71(2):267–273. doi: 10.1038/ejcn.2016.246. [DOI] [PubMed] [Google Scholar]
- 19.Miao L, Deng GX, Yin RX, Nie RJ, Yang S, Wang Y, Li H: No causal effects of plasma homocysteine levels on the risk of coronary heart disease or acute myocardial infarction: a Mendelian randomization study. Eur J Prev Cardiol 2019:2047487319894679. 10.1177/2047487319894679. [DOI] [PubMed]
- 20.Sun X, Lu Y, Wang Z, Wang Q, Zheng L. No causal association between plasma homocysteine levels and atrial fibrillation: a Mendelian randomization study. Nutr Metab Cardiovasc Dis. 2021;31(2):587–91. [DOI] [PubMed]
- 21.Nielsen JB, Thorolfsdottir RB, Fritsche LG, Zhou W, Skov MW, Graham SE, Herron TJ, McCarthy S, Schmidt EM, Sveinbjornsson G, Surakka I, Mathis MR, Yamazaki M, Crawford RD, Gabrielsen ME, Skogholt AH, Holmen OL, Lin M, Wolford BN, Dey R, Dalen H, Sulem P, Chung JH, Backman JD, Arnar DO, Thorsteinsdottir U, Baras A, O’Dushlaine C, Holst AG, Wen X, Hornsby W, Dewey FE, Boehnke M, Kheterpal S, Mukherjee B, Lee S, Kang HM, Holm H, Kitzman J, Shavit JA, Jalife J, Brummett CM, Teslovich TM, Carey DJ, Gudbjartsson DF, Stefansson K, Abecasis GR, Hveem K, Willer CJ. Biobank-driven genomic discovery yields new insight into atrial fibrillation biology. Nat Genet. 2018;50(9):1234–9. 10.1038/s41588-018-0171-3. [DOI] [PMC free article] [PubMed]
- 22.van der Harst P, Verweij N. Identification of 64 novel genetic loci provides an expanded view on the genetic architecture of coronary artery disease. Circ Res. 2018;122(3):433–443. doi: 10.1161/CIRCRESAHA.117.312086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Shah S, Henry A, Roselli C, Lin H, Sveinbjörnsson G, Fatemifar G, Hedman ÅK, Wilk JB, Morley MP, Chaffin MD, et al. Genome-wide association and Mendelian randomisation analysis provide insights into the pathogenesis of heart failure. Nat Commun. 2020;11(1):163. doi: 10.1038/s41467-019-13690-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Malik R, Chauhan G, Traylor M, Sargurupremraj M, Okada Y, Mishra A, Rutten-Jacobs L, Giese AK, van der Laan SW, Gretarsdottir S, et al. Multiancestry genome-wide association study of 520,000 subjects identifies 32 loci associated with stroke and stroke subtypes. Nat Genet. 2018;50(4):524–537. doi: 10.1038/s41588-018-0058-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Woo D, Falcone GJ, Devan WJ, Brown WM, Biffi A, Howard TD, Anderson CD, Brouwers HB, Valant V, Battey TW, Radmanesh F, Raffeld MR, Baedorf-Kassis S, Deka R, Woo JG, Martin LJ, Haverbusch M, Moomaw CJ, Sun G, Broderick JP, Flaherty ML, Martini SR, Kleindorfer DO, Kissela B, Comeau ME, Jagiella JM, Schmidt H, Freudenberger P, Pichler A, Enzinger C, Hansen BM, Norrving B, Jimenez-Conde J, Giralt-Steinhauer E, Elosua R, Cuadrado-Godia E, Soriano C, Roquer J, Kraft P, Ayres AM, Schwab K, McCauley J, Pera J, Urbanik A, Rost NS, Goldstein JN, Viswanathan A, Stögerer EM, Tirschwell DL, Selim M, Brown DL, Silliman SL, Worrall BB, Meschia JF, Kidwell CS, Montaner J, Fernandez-Cadenas I, Delgado P, Malik R, Dichgans M, Greenberg SM, Rothwell PM, Lindgren A, Slowik A, Schmidt R, Langefeld CD, Rosand J, International Stroke Genetics Consortium. Meta-analysis of genome-wide association studies identifies 1q22 as a susceptibility locus for intracerebral hemorrhage. Am J Hum Genet. 2014;94(4):511–21. 10.1016/j.ajhg.2014.02.012. [DOI] [PMC free article] [PubMed]
- 26.Bakker MK, van der Spek RAA, van Rheenen W, Morel S, Bourcier R, Hostettler IC, Alg VS, van Eijk KR, Koido M, Akiyama M, et al. Genome-wide association study of intracranial aneurysms identifies 17 risk loci and genetic overlap with clinical risk factors. Nat Genet. 2020;52(12):1303–1313. doi: 10.1038/s41588-020-00725-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sudlow C, Gallacher J, Allen N, Beral V, Burton P, Danesh J, Downey P, Elliott P, Green J, Landray M, Liu B, Matthews P, Ong G, Pell J, Silman A, Young A, Sprosen T, Peakman T, Collins R. UK biobank: an open access resource for identifying the causes of a wide range of complex diseases of middle and old age. Plos Med. 2015;12(3):e1001779. doi: 10.1371/journal.pmed.1001779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.FinnGen documentation of R4 release, 2020. https://finngen.gitbook.io/documentation/. Accessed 15 Dec 2020.
- 29.van Meurs JB, Pare G, Schwartz SM, Hazra A, Tanaka T, Vermeulen SH, Cotlarciuc I, Yuan X, Mälarstig A, Bandinelli S, et al. Common genetic loci influencing plasma homocysteine concentrations and their effect on risk of coronary artery disease. Am J Clin Nutr. 2013;98(3):668–676. doi: 10.3945/ajcn.112.044545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Grarup N, Sulem P, Sandholt CH, Thorleifsson G, Ahluwalia TS, Steinthorsdottir V, Bjarnason H, Gudbjartsson DF, Magnusson OT, Sparsø T, Albrechtsen A, Kong A, Masson G, Tian G, Cao H, Nie C, Kristiansen K, Husemoen LL, Thuesen B, Li Y, Nielsen R, Linneberg A, Olafsson I, Eyjolfsson GI, Jørgensen T, Wang J, Hansen T, Thorsteinsdottir U, Stefánsson K, Pedersen O. Genetic architecture of vitamin B12 and folate levels uncovered applying deeply sequenced large datasets. Plos Genet. 2013;9(6):e1003530. doi: 10.1371/journal.pgen.1003530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tanaka T, Scheet P, Giusti B, Bandinelli S, Piras MG, Usala G, Lai S, Mulas A, Corsi AM, Vestrini A, Sofi F, Gori AM, Abbate R, Guralnik J, Singleton A, Abecasis GR, Schlessinger D, Uda M, Ferrucci L. Genome-wide association study of vitamin B6, vitamin B12, folate, and homocysteine blood concentrations. Am J Hum Genet. 2009;84(4):477–482. doi: 10.1016/j.ajhg.2009.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Burgess S, Bowden J, Fall T, Ingelsson E, Thompson SG. Sensitivity analyses for robust causal inference from Mendelian randomization analyses with multiple genetic variants. Epidemiology. 2017;28(1):30–42. doi: 10.1097/EDE.0000000000000559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bowden J, Davey Smith G, Haycock PC, Burgess S. Consistent estimation in Mendelian randomization with some invalid instruments using a weighted median estimator. Genet Epidemiol. 2016;40(4):304–314. doi: 10.1002/gepi.21965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bowden J, Davey Smith G, Burgess S. Mendelian randomization with invalid instruments: effect estimation and bias detection through Egger regression. Int J Epidemiol. 2015;44(2):512–525. doi: 10.1093/ije/dyv080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Verbanck M, Chen CY, Neale B, Do R. Detection of widespread horizontal pleiotropy in causal relationships inferred from Mendelian randomization between complex traits and diseases. Nat Genet. 2018;50(5):693–698. doi: 10.1038/s41588-018-0099-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kamat MA, Blackshaw JA, Young R, Surendran P, Burgess S, Danesh J, Butterworth AS, Staley JR. PhenoScanner V2: an expanded tool for searching human genotype-phenotype associations. Bioinformatics. 2019;35(22):4851–4853. doi: 10.1093/bioinformatics/btz469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ripatti P, Rämö JT, Mars NJ, Fu Y, Lin J, Söderlund S, Benner C, Surakka I, Kiiskinen T, Havulinna AS, Palta P, Freimer NB, Widén E, Salomaa V, Tukiainen T, Pirinen M, Palotie A, Taskinen MR, Ripatti S, FinnGen Polygenic hyperlipidemias and coronary artery disease risk. Circ Genom Precis Med. 2020;13(2):e002725. doi: 10.1161/CIRCGEN.119.002725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21(11):1539–1558. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- 39.Brion MJ, Shakhbazov K, Visscher PM. Calculating statistical power in Mendelian randomization studies. Int J Epidemiol. 2013;42(5):1497–1501. doi: 10.1093/ije/dyt179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Spiller W, Davies NM, Palmer TM. Software application profile: mrrobust—a tool for performing two-sample summary Mendelian randomization analyses. Int J Epidemiol. 2018;48(3):684–690. doi: 10.1093/ije/dyy195. [DOI] [Google Scholar]
- 41.Hemani G, Zheng J, Elsworth B, Wade KH, Haberland V, Baird D, Laurin C, Burgess S, Bowden J, Langdon R, Tan VY, Yarmolinsky J, Shihab HA, Timpson NJ, Evans DM, Relton C, Martin RM, Davey Smith G, Gaunt TR, Haycock PC. The MR-base platform supports systematic causal inference across the human phenome. Elife. 2018;7. 10.7554/eLife.34408. [DOI] [PMC free article] [PubMed]
- 42.Li Y, Huang T, Zheng Y, Muka T, Troup J, Hu FB: Folic Acid Supplementation and the Risk of Cardiovascular Diseases: A Meta-Analysis of Randomized Controlled Trials. J Am Heart Assoc. 2016;5(8):e003768. [DOI] [PMC free article] [PubMed]
- 43.Collaboration HLT: Lowering blood homocysteine with folic acid based supplements: meta-analysis of randomised trials. Homocysteine Lowering Trialists’ Collaboration. BMJ 1998, 316(7135):894–898. [PMC free article] [PubMed]
- 44.Lehotský J, Tothová B, Kovalská M, Dobrota D, Beňová A, Kalenská D, Kaplán P. Role of homocysteine in the ischemic stroke and development of ischemic tolerance. Front Neurosci. 2016;10:538. doi: 10.3389/fnins.2016.00538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Pushpakumar S, Kundu S, Sen U. Endothelial dysfunction: the link between homocysteine and hydrogen sulfide. Curr Med Chem. 2014;21(32):3662–3672. doi: 10.2174/0929867321666140706142335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.He Y, Li Y, Chen Y, Feng L, Nie Z. Homocysteine level and risk of different stroke types: a meta-analysis of prospective observational studies. Nutr Metab Cardiovasc Dis. 2014;24(11):1158–1165. doi: 10.1016/j.numecd.2014.05.011. [DOI] [PubMed] [Google Scholar]
- 47.Cui R, Moriyama Y, Koike KA, Date C, Kikuchi S, Tamakoshi A, Iso H. Serum total homocysteine concentrations and risk of mortality from stroke and coronary heart disease in Japanese: the JACC study. Atherosclerosis. 2008;198(2):412–418. doi: 10.1016/j.atherosclerosis.2007.09.029. [DOI] [PubMed] [Google Scholar]
- 48.Zhou Z, Liang Y, Qu H, Zhao M, Guo F, Zhao C, Teng W. Plasma homocysteine concentrations and risk of intracerebral hemorrhage: a systematic review and meta-analysis. Sci Rep. 2018;8(1):2568. doi: 10.1038/s41598-018-21019-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Li Z, Sun L, Zhang H, Liao Y, Wang D, Zhao B, Zhu Z, Zhao J, Ma A, Han Y, Wang Y, Shi Y, Ye J, Hui R, Multicenter Case-Control Study in China Elevated plasma homocysteine was associated with hemorrhagic and ischemic stroke, but methylenetetrahydrofolate reductase gene C677T polymorphism was a risk factor for thrombotic stroke: a multicenter case-control study in China. Stroke. 2003;34(9):2085–2090. doi: 10.1161/01.STR.0000086753.00555.0D. [DOI] [PubMed] [Google Scholar]
- 50.Semmler A, Linnebank M, Krex D, Götz A, Moskau S, Ziegler A, Simon M. Polymorphisms of homocysteine metabolism are associated with intracranial aneurysms. Cerebrovasc Dis. 2008;26(4):425–429. doi: 10.1159/000155638. [DOI] [PubMed] [Google Scholar]
- 51.Humphrey LL, Fu R, Rogers K, Freeman M, Helfand M. Homocysteine level and coronary heart disease incidence: a systematic review and meta-analysis. Mayo Clin Proc. 2008;83(11):1203–1212. doi: 10.4065/83.11.1203. [DOI] [PubMed] [Google Scholar]
- 52.Wang ZM, Zhou B, Nie ZL, Gao W, Wang YS, Zhao H, Zhu J, Yan JJ, Yang ZJ, Wang LS. Folate and risk of coronary heart disease: a meta-analysis of prospective studies. Nutr Metab Cardiovasc Dis. 2012;22(10):890–899. doi: 10.1016/j.numecd.2011.04.011. [DOI] [PubMed] [Google Scholar]
- 53.Robinson K, Arheart K, Refsum H, Brattström L, Boers G, Ueland P, Rubba P, Palma-Reis R, Meleady R, Daly L, et al. Low circulating folate and vitamin B6 concentrations: risk factors for stroke, peripheral vascular disease, and coronary artery disease. European COMAC Group. Circulation. 1998;97(5):437–443. doi: 10.1161/01.CIR.97.5.437. [DOI] [PubMed] [Google Scholar]
- 54.Verhaar MC, Stroes E, Rabelink TJ. Folates and cardiovascular disease. Arterioscler Thromb Vasc Biol. 2002;22(1):6–13. doi: 10.1161/hq0102.102190. [DOI] [PubMed] [Google Scholar]
- 55.Liu Y, Tian T, Zhang H, Gao L, Zhou X. The effect of homocysteine-lowering therapy with folic acid on flow-mediated vasodilation in patients with coronary artery disease: a meta-analysis of randomized controlled trials. Atherosclerosis. 2014;235(1):31–35. doi: 10.1016/j.atherosclerosis.2014.03.032. [DOI] [PubMed] [Google Scholar]
- 56.Chambers JC, Ueland PM, Obeid OA, Wrigley J, Refsum H, Kooner JS. Improved vascular endothelial function after oral B vitamins: an effect mediated through reduced concentrations of free plasma homocysteine. Circulation. 2000;102(20):2479–2483. doi: 10.1161/01.CIR.102.20.2479. [DOI] [PubMed] [Google Scholar]
- 57.Title LM, Cummings PM, Giddens K, Genest JJ, Jr, Nassar BA. Effect of folic acid and antioxidant vitamins on endothelial dysfunction in patients with coronary artery disease. J Am Coll Cardiol. 2000;36(3):758–765. doi: 10.1016/S0735-1097(00)00809-3. [DOI] [PubMed] [Google Scholar]
- 58.Yuan S, Carter P, Vithayathil M, Kar S, Mason AM, Burgess S, Larsson SC. Genetically predicted circulating B vitamins in relation to digestive system cancers. 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Hazra A, Kraft P, Lazarus R, Chen C, Chanock SJ, Jacques P, Selhub J, Hunter DJ. Genome-wide significant predictors of metabolites in the one-carbon metabolism pathway. Hum Mol Genet. 2009;18(23):4677–4687. doi: 10.1093/hmg/ddp428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Lawlor DA, Harbord RM, Sterne JA, Timpson N, Davey Smith G. Mendelian randomization: using genes as instruments for making causal inferences in epidemiology. Stat Med. 2008;27(8):1133–1163. doi: 10.1002/sim.3034. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data analyzed in this study are available OSF data respiratory (https://osf.io/527zy/).