Abstract
Background
Providing oncology services during a pandemic can contribute to mental health challenges among healthcare workers. The present study aimed to evaluate the levels of depression, anxiety, and stress in healthcare and administrative staff in 5 oncology institutions in Bosnia and Herzegovina (BiH) in 2020 during the coronavirus disease 2019 (COVID-19) pandemic using the Depression, Anxiety and Stress Scale (DASS-21) questionnaire.
Material/Methods
A cross-sectional observational study enrolled 175 healthcare and administrative workers from 5 oncology institutions in BiH during December 2020. Data were collected using a questionnaire that captured general information about the participants and a DASS-21 questionnaire.
Results
Statistical analysis revealed a statistically significant difference in the levels of depression, anxiety, and stress (P=0.003, P=0.011, and P=0.022, respectively) among participants with comorbidities connected with increased risk of severe illness caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) compared with participants without comorbidities. There was also a statistically significant difference in the levels of stress among participants from different cities (P=0.031). Supplement intake and educational level were significantly related (P=0.012). High levels of stress and anxiety were accompanied by high levels of depression among participants (P<0.01).
Conclusions
The findings from the present study showed that the COVID-19 pandemic has had an effect on depression, anxiety, and stress levels in oncology staff in BiH. Monitoring these levels and providing interventions and support to oncology staff are increasingly important for their wellbeing and retention at a time of global crisis in healthcare.
Keywords: Anxiety; COVID-19; Depression; Medical Oncology; Medical Staff; Stress, Psychological
Background
After the outbreak of coronavirus disease 2019 (COVID-19) in December 2019, the virus quickly became a global pandemic. In addition to COVID-19’s serious consequences for an individual’s physical health, it is important to understand the virus’s consequences for mental health. As the world grapples with this major crisis, the relative risk of infection with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and the risk of mental health impairment associated with infection control need to be identified and weighed [1,2].
According to the World Health Organization (WHO), the most significant mental health impact of COVID-19 to date has been its influence in increasing rates of stress and anxiety among the general public. Certain subgroups, such as the elderly, individuals with specific health conditions, and health professionals, have been most affected by these problems [3].
In Bosnia and Herzegovina (BiH), the first cases of SARS-CoV-2 infection were recorded on March 5, 2020 in the Republika Srpska (RS) and on March 9, 2020 in the Federation of Bosnia and Herzegovina (FBiH) [4].
After a relatively stable trend in the number of COVID-19 cases throughout the second half of August and September 2020, the situation quickly and dramatically deteriorated, with an exponential rise in the number of cases in mid-October [5]. To prevent transmission of the disease among patients and hospital staff, work was reorganized during the COVID-19 pandemic, based on guidelines from leadership about the crisis [1].
During the COVID-19 pandemic, all oncology centers organized their work based on instructions about the crisis provided by headquarters. Mandatory protective and preventive measures for staff included use of personal protective equipment: surgical masks, gloves, and visors. Preventive measures for both patients and oncology staff included keeping physical distance in situations where possible, use of disinfectants, and mandatory temperature-taking before entering the hospital. Oncology staff organized teams to perform triage of patients before entry into hospitals. Wearing surgical masks and gloves was mandatory for all patients. Patients scheduled to be hospitalized for chemotherapy, immunotherapy,or radiotherapy must have tested negative for COVID-19 on reverse transcription polymerase chain reaction (RT-PCR) within the the past 48 hours. All patients who needed hospitalization on an emergency basis were admitted to isolation wards until the results of RT-PCR testing could be obtained. All oncology centers in BiH were informed about the European Society for Medical Oncology (ESMO) recommendations for management of patients with cancer during the COVID-19 pandemic and tried to adjust their work to those guidelines as much as possible [6].
In the current circumstances, most people are worried about contracting the virus and are also affected by a variety of different stressors associated with the pandemic. The resulting fear causes people to become anxious, which has a negative effect on mental health [1,7].
During pandemics, healthcare professionals have shown incredible dedication and care for their patients, even though the working conditions sometimes have been very difficult [8]. It is stressful to work in healthcare because the needs of patients and families must be addressed very quickly by medical professionals. Several studies have indicated that medical professionals routinely deal with stress, depression, and anxiety [9–12]. Other studies have reported that medical staff have experienced depression and anxiety because of the COVID-19 outbreak [8,13–18].
Oncology staff are at high risk of developing psychological and burnout disorders [19,20]. Because of the COVID-19 crisis, many oncologists also are now concerned about how to appropriately treat patients with cancer in the metastatic and adjuvant setting [21]. India’s experience showed that, despite the risk of infection with SARS-CoV-2, patients with cancer want continuous care for their disease. To achieve that goal required an extraordinary response from health workers, who had to balance the safety of themselves and their families against the risks of providing treatment to patients with cancer [22].
In terms of organization, the initial response in the oncology area was aimed at protecting patients from the risk of infection with SARS-CoV-2. Based on expert advice, a typical strategy involved limiting access to the hospital whenever possible, performing pre-hospitalization triage, eliminating unnecessary appointments and tests, delaying follow-up visits, prioritizing adjuvant and curative care over palliative treatment, and avoiding advanced lines of treatment. In this context, the risks of undermining the efficacy of cancer treatment and delaying diagnosis have to be weighed and should be the subject of future careful long-term research [23].
Providing oncology services during a pandemic, therefore, can contribute to mental health challenges among healthcare workers. The intensity of a pandemic’s short-term effects on healthcare workers differs in terms of stress, insomnia, anxiety, and depression. It can range from mild difficulty to suicide, depending on factors such as age, sex, and type of work [24].
The Depression, Anxiety and Stress Scale (DASS-21) questionnaire is a validated instrument that rates these 3 dimensions of mental health in adults (patients and non-patients) on a single, clear, and systematic scale [25–27].
The present study aimed to evaluate the levels of depression, anxiety, and stress in healthcare and administrative staff in 5 oncology institutions in BiH during the 2020 COVID-19 pandemic using the DASS-21 questionnaire.
Material and Methods
Ethics Statement
Ethics approval was obtained from the Hospital Ethics Committee. All procedures followed were in accordance with the Helsinki Declaration of 1975, as revised in 2000. Participation in the study was voluntary and anonymous. All participants gave their informed consent.
Study Participants
The present cross-sectional, observational study included oncology staff (physicians, nurses, medical radiation technologists, and administrators) at 5 institutions throughout BiH: the Oncology Clinic of University Clinical Hospital Mostar, the Clinic of Oncology of University Clinical Center Sarajevo, the Department of Oncology of Cantonal Hospital Zenica, the Department of Oncology of University Clinical Center Tuzla, and the Oncology Clinic at the University Clinical Center Banja Luka. Data were collected during December 2020. Considering the preventive measures that were in force at that time and the way the oncology centers worked, a total of 224 staff were available for testing, 175 of whom agreed to participate in the study. The response rate was 78.1%.
Participants provided general demographic information, including data about personal risk factors associated with heightened concern about COVID-19. Data were collected regarding age, education level, profession, department where participants worked, marital status, presence of comorbidities connected with increased risk of severe illness caused by SARS-CoV-2, body mass index (BMI), contact with patients infected with SARS-CoV-2, and use of dietary or drug supplementation with vitamins and essential nutrients that boost the immune system.
DASS-21 Questionnaire
Lovibond and Lovibond developed the DASS questionnaire to assess key symptoms of depression, anxiety, and stress and it also has been used to evaluate patient reaction to treatment. The questionnaire has been proven to have adequate psychometric properties and is equivalent to other accurate scales. The DASS-21 is the short form and findings from studies support its validity as an approved instrument for measuring adverse mental states and depression, anxiety, and stress in adults (patients and non-patients). The 21 items on the questionnaire comprise a set of 3 self-reported scales designed to assess DASS. The 7 elements on the scales are graded on a Likert scale from 0 to 3 (0: “Did not apply to me at all,” 1: “Applied to me to some degree or some of the time,” 2: “Applied to me to a considerable degree or a good part of the time,” and 3: “Applied to me very much or most of the time”). Depression, anxiety, and stress scores are measured by summarizing the scores of the related items. Because the DASS-21 is a shorter version of the 42-item original DASS, the score for each subscale must be multiplied by 2 to calculate the final score. According to the manual, the resulting ratings then are classified as: “normal, mild, moderate, severe, or extremely severe” [25–27].
Statistical Analysis
IBM SPSS Statistics software, version 23.0, was used for statistical analysis. Mann-Whitney U and Kruskal-Wallis H tests were used to evaluate distribution of levels of depression, anxiety, and stress scores among categorical variables. A chi-square test of independence was used to evaluate distribution of participants who did and did not take supplements, based on categorical variables. P values for the individual cells were calculated from the resulting Z scores for cross-tabulation. The relationship between levels of depression and levels of stress and anxiety was investigated using a Spearman correlation coefficient. P<0.05 was considered statistically significant.
Results
Demographic Data
The study sample included 175 members of the oncology staff from 5 institutions in BiH, the majority of whom were women (78.3%). Of the participants, 47.4%, 41.7%, and 10.9% were aged <35, 36 to 54, and >55 years, respectively. Most of the participants were married (64.6%) and had a post-secondary level of education (58.9%). Nearly half were nurses (48.6%), 29.1% were medical doctors, 10.3% were medical radiation technologists, and 11.4% of them were involved in administration. A total of 35 healthcare workers had conditions that were connected with increased risk of severe illness caused by SARS-CoV-2. Of the participants, 44% had contact with patients with COVID-19. Most of the participants (58.3%) had normal BMI. A total of 87 healthcare workers started using dietary supplements that boost the immune system during the pandemic. Baseline characteristics of the participants are shown in Table 1.
Table 1.
Summary of demographic, personal, and clinical characteristics of oncology staff in Bosnia and Herzegovina.
| Variables | Frequency (n) | Percent (%) |
|---|---|---|
| Gender | ||
| Male | 38 | 21.7 |
| Female | 137 | 78.3 |
| Profession | ||
| Medical doctor | 51 | 29.1 |
| Nurse | 85 | 48.6 |
| Medical radiation technologist | 18 | 10.3 |
| Administrative employee | 20 | 11.4 |
| Missing | 1 | 0.6 |
| Educational level | ||
| Primary education | 2 | 1.1 |
| Secondary education | 70 | 40.0 |
| Post-secondary education | 103 | 58.9 |
| Marital status | ||
| Married | 113 | 64.6 |
| Unmarried | 62 | 35.4 |
| Presence of comorbidities connected with increased risk of severe illness caused by SARS-CoV-2 | ||
| Yes | 35 | 20.0 |
| No | 140 | 80.0 |
| BMI | ||
| Underweight | 4 | 2.3 |
| Normal | 102 | 58.3 |
| Overweight | 61 | 34.9 |
| Obese | 8 | 4.6 |
| Age | ||
| <35 years | 83 | 47.4 |
| 36–54 years | 73 | 41.7 |
| >55 years | 19 | 10.9 |
| Contact with patients infected with SARS-CoV-2 | ||
| Yes | 77 | 44.0 |
| No | 98 | 56.0 |
| Use of immunity-boosting supplements | ||
| Yes | 87 | 49.7 |
| No | 88 | 50.3 |
| City | ||
| Mostar | 45 | 25.7 |
| Sarajevo | 33 | 18.9 |
| Zenica | 25 | 14.3 |
| Tuzla | 28 | 16.0 |
| Banja Luka | 44 | 25.1 |
BMI – body mass index, SARS-CoV-2 – severe acute respiratory syndrome coronavirus 2.
Staff Exposure to Patients with COVID-19
Of the participants, 44% had contact with patients with COVID-19. A Mann-Whitney U test showed no statistically significant difference in the scores for depression, anxiety, and stress between participants who did and did not have such COVID-19 exposure.
Prevalence of Depression, Anxiety, and Stress
Table 2 shows the overall prevalence of depression, anxiety, and stress among participants. In most participants, the levels were normal.
Table 2.
Overall prevalence of depression, anxiety, and stress among oncology staff in Bosnia and Herzegovina during the coronavirus disease 2019 pandemic.
| Variables | Frequency (n) | Percent (%) |
|---|---|---|
| Depression level | ||
| Normal | 131 | 74.9 |
| Mild | 22 | 12.6 |
| Moderate | 13 | 7.4 |
| Severe | 6 | 3.4 |
| Extremely severe | 3 | 1.7 |
| Anxiety level | ||
| Normal | 124 | 70.9 |
| Mild | 18 | 10.3 |
| Moderate | 20 | 11.4 |
| Severe | 5 | 2.9 |
| Extremely severe | 8 | 4.6 |
| Stress level | ||
| Normal | 125 | 71.4 |
| Mild | 23 | 13.1 |
| Moderate | 17 | 9.7 |
| Severe | 6 | 3.4 |
| Extremely severe | 4 | 2.3 |
Effects of Comorbidities
A statistically significant difference was found in the scores for depression in participants who had comorbidities (median=6, n=35) vs those who did not have comorbidities (median=3, n=140, U=1665.5, z=−2.98; P=0.003). A statistically significant difference also was found in the scores for anxiety in participants who had comorbidities (median=6, n=35) vs those who did not have comorbidities (median=2, n=140, U=1784.5, z=−2.53; P=0.011). A statistically significant difference was found in the levels of stress of participants who had comorbidities (median=12, n=35) and who did have not comorbidities (median=6, n=140, U=1838.0, z=−2.29; P=0.022) (Figure 1).
Figure 1.
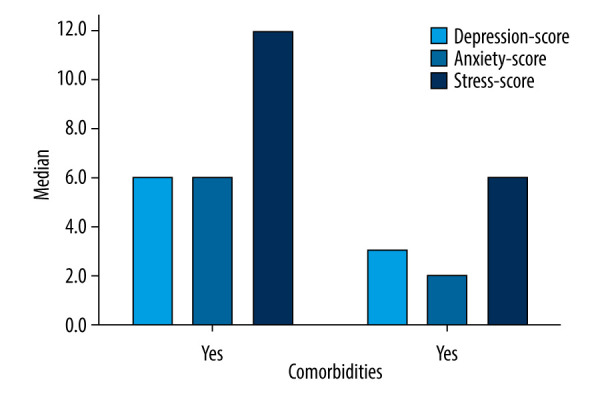
Scores for levels of depression, anxiety, and stress among oncology staff in Bosnia and Herzegovina with and without comorbidities connected with increased risk of severe illness caused by the severe acute respiratory syndrome coronavirus 2.
Differences in Depression, Anxiety, and Stress Among the Centers
No significant difference was found in the levels of depression and anxiety in participants from different cities but statistically significant differences were found in their levels of stress (Scores: Mostar, n=45; Sarajevo, n=33; Zenica, n=35; Tuzla, n=25; Banja Luka, n=44;) (χ2=4, n=175; P=0.031. The highest stress levels (median=12) were in the participants from Sarajevo and the lowest in those from Tuzla (median=6) (Figures 2, 3).
Figure 2.
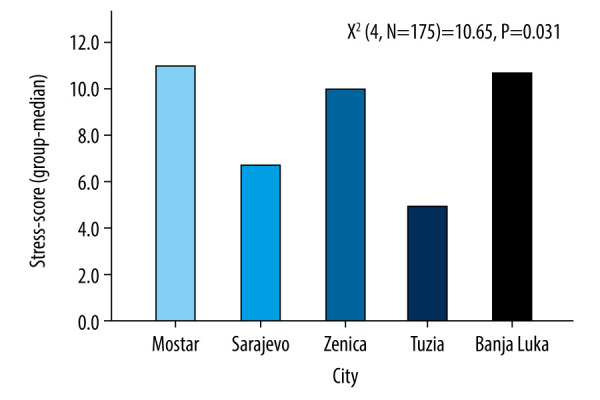
Scores for levels of stress among oncology staff from different cities in Bosnia and Herzegovina during the coronavirus disease 2019 pandemic.
Figure 3.
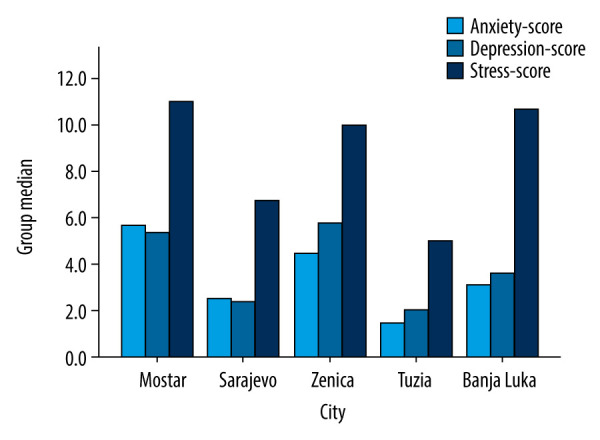
Scores for levels of depression, anxiety, and stress among oncology staff from different cities in Bosnia and Herzegovina during the coronavirus disease 2019 pandemic.
Interactions Between Depression, Anxiety, and Stress in Oncology Staff
The relationship between levels of depression and levels of stress and anxiety was investigated using the Spearman correlation coefficient. A statistically significant positive correlation was calculated between levels of depression and anxiety (r=0.448, n=175, P<0.01). There was also a statistically significant positive correlation between levels of depression and stress (r=0.536, n=175, P<0.01). High levels of stress and anxiety were accompanied by high levels of depression among participants (Table 3).
Table 3.
Relationship between levels of depression and levels of stress and anxiety among oncology staff in Bosnia and Herzegovina during the coronavirus disease 2019 pandemic.
| Spearman’s rho | Anxiety | Stress | |
|---|---|---|---|
| Depression | Correlation coefficient | 0.448 | 0.536 |
| Sig. (2-tailed) | P<0.01 | P<0.01 | |
| N | 175 | 175 | |
Other Results
A Mann-Whitney U test revealed no statistically significant difference in levels of depression, anxiety, and stress between men and women, married and unmarried participants, and participants taking and not taking supplements.
A Kruskal-Wallis test revealed a statistically significant difference in the levels of depression, anxiety, and stress in participants from different age groups and with different professions and educational levels.
A chi-square test of independence did not reveal a statistically significant relationship between supplement intake and sex, profession, or presence of comorbidities. It did reveal a statistically significant relationship between supplement intake and educational level (χ2=8.81; 4, n=175: P=0.012). Significantly fewer of the participants with education at the secondary school level took supplements (P=0.01), whereas they were taken by significantly more of the participants with a post-secondary education (P=0.02) (Table 4).
Table 4.
Relationship between use of supplements that boost immune system intake and educational level of oncology staff in Bosnia and Herzegovina during the coronavirus 2019 disease pandemic.
| Educational level | Total | |||||
|---|---|---|---|---|---|---|
| Primary | Secondary | Post-secondary | ||||
| Supplementation | Yes | Number | 2 | 26 | 59 | 87 |
| % using supplements | 2.3% | 29.9% | 67.8% | 100.0% | ||
| Adjusted residual (Z-score) | 1.4 | −2.7 | 2.4 | |||
| No | Number | 0 | 44 | 44 | 88 | |
| % using supplements | 0.0% | 50.0% | 50.0% | 100.0% | ||
| Adjusted residual (Z-score) | −1.4 | 2.7 | −2.4 | |||
| Total | 2 | 70 | 103 | 175 | ||
A Kruskal-Wallis test revealed a statistically significant difference in age among the participants from different cities (Mostar, n=45; Sarajevo, n=33; Zenica, n=35; Tuzla, n=25;
Banja Luka, n=44) (χ2=25.88; 4, n=175: P<0.01). The participants from Tuzla were the oldest (median age 42.5 years), whereas the participants from Banja Luka were the youngest (median age 30 years). The median age of participants from Mostar was 34 years.
Discussion
Results from the present study revealed a significant difference in the levels of depression, anxiety, and stress among participants with comorbidities connected with increased risk of severe illness caused by SARS-CoV-2 compared with participants without these comorbidities. There was also a statistically significant difference in the levels of stress in participants from different cities. There was a significant relationship between supplement intake and educational level. High levels of stress and anxiety were accompanied by high levels of depression.
Our study aimed to identify the prevalence of and factors associated with depression, anxiety, and stress among oncology staff at 5 institutions in a single country during the 2020 COVID-19 pandemic. There is a lack of evidence in this area in the literature. A 2014 cross-sectional study showed that anxiety and depression were common among physicians in China [12]. Another cross-sectional study performed the same year explored the prevalence of and factors associated with job stress and burnout in individuals in different medical professions. The results demonstrated that the level of work-related burnout was highest in nurses and lowest in medical technicians [11]. Studies have also investigated levels of depression, anxiety, and stress among emergency staff [9,10]. Several cross-sectional studies investigating mental health among healthcare professionals have been published during the COVID-19 pandemic [13–18]. Most of the respondents were healthcare professionals from different areas of medicine or frontline medical workers.
Information from the Centers for Disease Control and Prevention, based on the strongest and most consistent evidence, indicates that the risk of serious illness caused by SARS-CoV-2 increases with age and that age is the most significant factor associated with serious illness. People in their 50s, for instance, are at greater risk for serious illness than are individuals in their 40s. The greatest risk of serious COVID-19 disease is in those aged 85 years or older. Adults with certain comorbidities, regardless of age, have an increased risk of developing a serious disease caused by SARS-CoV-2. Serious illness with COVID-19 is characterized by hospitalization, Intensive Care Unit admission, intubation or mechanical ventilation, or death. The comorbidities known to increase risk of these complications are: “cancer; chronic kidney disease; chronic obstructive pulmonary disease; heart conditions, such as heart failure, coronary artery disease, or cardiomyopathies; immunocompromised state (weakened immune system) from solid organ transplant; obesity (BMI ≥30 kg/m2 but <40 kg/m2); severe obesity (BMI ≥40 kg/m2); pregnancy; sickle cell disease; smoking; and type 2 diabetes mellitus” [28].
Based on the above information, we assumed that participants in our study who were older and who had some of the comorbidities would have higher levels of depression, anxiety, and stress. As shown in the results, there was a statistically significant difference in levels of depression, anxiety, and stress between participants who had comorbidities and those who did not have comorbidities.
The findings from our research showed that there was a significant difference in the levels of stress in participants from different cities. Participants from Mostar had the highest levels of stress while participants from Sarajevo and Tuzla had the lowest levels of stress. The reasons could be related to different epidemiological situations in the cities, how work has been organized during the COVID-19 pandemic, or differences in the ages of the participants in each city. The results of a 2017 survey of healthcare workers showed that stressors related to organization of work, finance, and communication had the greatest influence on their mental health [29].
From the beginning of the pandemic in BiH to January 24, 2021, according to the Institute for Public Health FBiH, there were 10 978 confirmed cases of COVID-9 in Mostar, 19 815 in Sarajevo, 2200 in Zenica, and 5191 in Tuzla 5 191 [30]. According to the Government of the RS, Banja Luka had 10 961 confirmed COVID-19 cases during that same period [31]. The number of inhabitants in each city and the state number of recorded COVID-19 cases are factors important to emphasize. Results of the most recent 2013 population census in BiH showed that Mostar had a total population of 105 797, Sarajevo 275 524, Zenica 110 663, Tuzla 110 979, and Banja Luka 185 042 [32]. Therefore, the incidence rate for COVID-19 is highest in Mostar, which could be one reason why levels of stress were higher in respondents from there than in the other cities. Also, in December 2020, local elections were held in Mostar for the first time in 12 years, which could have contributed to increased stress levels. According to the Mental Health Foundation, political change can affect people in numerous ways and cause stress about their country’s future [33]. Although the results of the present study showed that the age distribution of participants varied by city, that should not have had an impact on the results regarding increased stress levels in participants in Mostar because their median age was 34 years.
Dietary or drug supplements containing vitamins and essential nutrients that boost the immune system are a low-cost and effective adjuvant strategy for the acute respiratory tract complications of COVID-19 [34]. During the pandemic, many people began taking dietary supplements to boost their immunity. As we can see from the results of the present study, most respondents who had a higher level of education took dietary supplements. A 2006 study of health care professionals who had enrolled in an online course about dietary supplements showed that their use was highest among women, older clinicians, and those with greater knowledge of and who counseled patients about dietary supplements [35].
The results of the present study showed that the extent of stress and anxiety was directly related to depression. A literature review shows that chronic stress and anxiety disorders are related to major depressive disorder. When chronic stress goes untreated, severe disabilities can occur, such as insomnia, immune system compromise, high blood pressure, anxiety, and muscle pain. Stress also plays a role in the development of major disorders, such as depression [36]. The results of the study that evaluated the degree of stress, anxiety, and depression among the Emergency Department personnel also showed that there was a significant relationship between rates of stress and anxiety in the participants and depression. Anxiety is known in psychology as an acute cause of persistent stress and it becomes a psychiatric illness if it causes the individual or others to suffer, prevents goals from being accomplished, and interferes with regular everyday activities. When stressful circumstances last too long or occur repeatedly, the result is anxiety. In this situation, the body becomes stressed and vulnerable to physical and mental diseases, such as anxiety [37]. Depression manifests in a range of psychological states, from listlessness to complete detachment from daily life, and is known to be one of the causes of persistent anxiety. Over time, without primary prevention, early diagnosis, and prompt intervention, anxiety can become a complex condition [9].
In a 2006 study, Xianyu and Lambert found that in Chinese head nurses, a heavy workload was a major cause of workplace stress [38]. In Eastern Europe, the rate of burnout among oncologists is high and younger oncologists are most vulnerable to it [39]. Providing oncology services during a pandemic further contributes to the challenges of mental health among health care workers. Preventive steps should be taken to deal with these issues, which adversely affect the delivery of adequate treatment and pose a danger to the health and wellbeing of oncologists.
The present study has several limitations. Because of the cross-sectional design, longitudinal follow-up is lacking. The primary limitation of this type of analysis is that because exposure and results are measured simultaneously, there is typically no proof of a temporal association between them. Also in the present study, not all of the oncology staff at the 5 institutions in BiH responded to the survery, which could have affected the results we obtained because they do not give a complete picture of the mental health of the entire oncology staff in BiH. We were also unable to differentiate between pre-existing depression, anxiety, and stress versus new cases. Because the study was cross-sectional, the impact of continuous changes on the psychological status of medical staff was not studied. The DASS-21 questionnaire resulted in a reliance on self-reported responses, which may not correlate with clinical diagnosis by a mental health professional. The strengths of the present study were that it was multicenter, not costly to perform, and did not require a lot of time. The DASS-21 questionnaire is a validated instrument, used worldwide, and easily applicable.
Conclusions
The aim of the present study was to assess depression, anxiety, and stress levels among oncology staff in various institutions in BiH during the COVID-19 pandemic. The findings showed that the pandemic had an impact on levels of depression, anxiety, and stress in oncology staff in BiH.
Our results revealed statistically significant differences in the levels of depression, anxiety, and stress in participants who had comorbidities connected with increased risk of severe illness from SARS-CoV-2 and participants who did not have the comorbidities. There was also a statistically significant relationship between supplement intake and educational level in participants. High levels of stress and anxiety were accompanied by high levels of depression among participants.
Monitoring levels of mental health and their associations and providing interventions and support to oncology staff are increasingly important for staff wellbeing and retention at a time of global crisis in healthcare.
Footnotes
Conflict of Interest
None.
Source of support: Departmental sources
References
- 1.Pajević I, Hasanović M, Avdibegović E, et al. Organization of mental healthcare in Bosnia and Herzegovina during coronavirus disease 2019 pandemic. Indian J Psychiatry. 2020;62(Suppl 3):S479–91. doi: 10.4103/psychiatry.IndianJPsychiatry_1044_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hermann A, Fitelson EM, Bergink V. Meeting maternal mental health needs during the COVID-19 pandemic. JAMA Psychiatry. 2021;78(2):123–24. doi: 10.1001/jamapsychiatry.2020.1947. [DOI] [PubMed] [Google Scholar]
- 3.World Health Organization (WHO) Europe. Mental health and COVID-19. 2020. https://www.euro.who.int/en/health-topics/health-emergencies/coronavirus-covid-19/publications-and-technical-guidance/noncommunicable-diseases/mental-health-and-covid-19.
- 4.Arapović J, Skočibušić S. The first two months of the COVID-19 pandemic in Bosnia and Herzegovina: Single-center experience. Bosn J Basic Med Sci. 2020;20:396–400. doi: 10.17305/bjbms.2020.4838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Organisation for Economic Co-operation and Development (OECD) The COVID-19 Crisis in Bosnia and Herzegovina. Nov 30, 2020. https://www.oecd.org/south-east-europe/COVID-19-Crisis-in-Bosnia-and-Herzegovina.pdf.
- 6.Curigliano G, Banerjee S, Cervantes A, et al. Managing cancer patients during the COVID-19 pandemic: An ESMO multidisciplinary expert consensus. Ann Oncol. 2020;31:1320–35. doi: 10.1016/j.annonc.2020.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kallivayalil RA. COVID-19 and Mental Health: Working together in India. WPA. 2020. https://www.wpanet.org/post/covid-19-and-mental-health-working-together-in-india.
- 8.Salopek-Žiha D, Hlavati M, Gvozdanović Z, et al. Differences in distress and coping with the COVID-19 stressor in nurses and physicians. Psychiatr Danub. 2020;32:287–93. doi: 10.24869/psyd.2020.287. [DOI] [PubMed] [Google Scholar]
- 9.Rahil GN. Evaluating the degree of stress, anxiety, and depression among the emergency personnel in Kerman University of Medical Sciences. Journal of Scientific Research and Essays. 2016;2:1–6. [Google Scholar]
- 10.Kozomara D, Babić D, Marijanović I, et al. Workplace stress in the university clinical settings: Comparison between the cardiac unit and emergency center medical staff. Psychiatr Danub. 2019;31:S796–804. [PubMed] [Google Scholar]
- 11.Chou LP, Li CY, Hu SC. Job stress and burnout in hospital employees: Comparisons of different medical professions in a regional hospital in Taiwan. BMJ Open. 2014;4:e004185. doi: 10.1136/bmjopen-2013-004185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gong Y, Han T, Chen W, et al. Prevalence of anxiety and depressive symptoms and related risk factors among physicians in China: A cross-sectional study. PLoS One. 2014;9:1–8. doi: 10.1371/journal.pone.0103242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Liu CY, Yang YZ, Zhang XM, et al. The prevalence and influencing factors in anxiety in medical workers fighting COVID-19 in China: A cross-sectional survey. Epidemiol Infect. 2020;148:e98. doi: 10.1017/S0950268820001107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fabi A, Pugliese P, Falbo PT, et al. The experience of oncology healthcare providers in the central Italy during the COVID-19 lockdown. Cancers (Basel) 2020;12:3031. doi: 10.3390/cancers12103031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Si MY, Su XY, Jiang Y, et al. Psychological impact of COVID-19 on medical care workers in China. Infect Dis Poverty. 2020;9:113. doi: 10.1186/s40249-020-00724-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.lbay RY, Kurtulmuş A, Arpacıoğlu S, et al. Depression, anxiety, stress levels of physicians and associated factors in Covid-19 pandemics. Psychiatry Res. 2020;290:113130. doi: 10.1016/j.psychres.2020.113130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wu Y, Wang J, Luo C, et al. A comparison of burnout frequency among oncology physicians and nurses working on the frontline and usual wards during the COVID-19 epidemic in Wuhan, China. J Pain Symptom Manage. 2020;60:e60–65. doi: 10.1016/j.jpainsymman.2020.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cai H, Tu B, Ma J, et al. Psychological impact and coping strategies of frontline medical staff in Hunan between January and March 2020 during the outbreak of Coronavirus Disease 2019 (COVID 19) in Hubei, China. Med Sci Monit. 2020;26:e924171. doi: 10.12659/MSM.924171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Guveli H, Anuk D, Oflaz S, et al. Oncology staff: Burnout, job satisfaction and coping with stress. Psychooncology. 2015;24:926–31. doi: 10.1002/pon.3743. [DOI] [PubMed] [Google Scholar]
- 20.Copur MS. Burnout in oncology. Oncology (Williston Park) 2019;33:687522. [PubMed] [Google Scholar]
- 21.Vrdoljak E, Sullivan R, Lawler M. Cancer and coronavirus disease 2019; How do we manage cancer optimally through a public health crisis? Eur J Cancer. 2020;132:98–99. doi: 10.1016/j.ejca.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ghosh J, Ganguly S, Mondal D, et al. Perspective of oncology patients during COVID-19 pandemic: A prospective observational study from India. JCO Glob Oncol. 2020;6:844–51. doi: 10.1200/GO.20.00172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cortiula F, Pettke A, Bartoletti M, et al. Managing COVID-19 in the oncology clinic and avoiding the distraction effect. Ann Oncol. 2020;31:553–55. doi: 10.1016/j.annonc.2020.03.286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Datta SS, Mukherjee A, Ghose S, et al. Addressing the mental health challenges of cancer care workers in lmics during the time of the COVID-19 pandemic. JCO Glob Oncol. 2020;6:1490–93. doi: 10.1200/GO.20.00470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lovibond SH, Lovibond PF. Manual for the depression anxiety and stress scales (DASS21) Second edition. Sydney, NSW: Psychology Foundation of Australia; 1995. pp. 1–3. [Google Scholar]
- 26.Ng F, Trauer T, Dodd S, et al. The validity of the 21-item version of the Depression Anxiety Stress Scales as a routine clinical outcome measure. Acta Neuropsychiatrica. 2007;19:304–10. doi: 10.1111/j.1601-5215.2007.00217.x. [DOI] [PubMed] [Google Scholar]
- 27.Antony MM, Bieling PJ, Cox BJ, et al. Psychometric properties of the 42-item and 21-item versions of the depression anxiety stress scales in clinical groups and a community sample. Psychological Assessment. 1998;10:176–81. [Google Scholar]
- 28.Centers for Disease Control and Prevention (CDC) People at increased risk and other people who need to take extra precautions. 2020. https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/index.html.
- 29.Trifunovic N, Jatic Z, Kulenovic AD. Identification of causes of the occupational stress for health providers at different levels of health care. Med Arch. 2017;71:169–72. doi: 10.5455/medarh.2017.71.169-172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Institute for public health of the Federation of Bosnia and Herzegovina (FBiH) COVID-19: Analytical and graphical presentation of FBiH data. 2021. https://covid-19.ba/
- 31.Goverment of Republica Srpska. COVID-19: Interactive map. 2021. https://koronavirususrpskoj.com/
- 32.Agency for Statistics of Bosnia and Herzegovina (BiH) Census 2013 in Bosnia and Herzegovina. 2013. https://www.popis.gov.ba/popis2013/mapa/?lang=bos.
- 33.Mental Health Foundation. Political change and mental health. Mar 21, 2019. https://www.mentalhealth.org.uk/blog/political-change-brexit-research.
- 34.Sahebnasagh A, Saghafi F, Avan R, et al. The prophylaxis and treatment potential of supplements for COVID-19. Eur J Pharmacol. 2020;15:173530. doi: 10.1016/j.ejphar.2020.173530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gardiner P, Woods C, Kemper KJ. Dietary supplement use among health care professionals enrolled in an online curriculum on herbs and dietary supplements. BMC Complement Altern Med. 2006;6:21. doi: 10.1186/1472-6882-6-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Baum A, Posluszny DM. Health psychology: Mapping biobehavioral contributions to health and illness. Ann Rev Psychol. 1999;50:137–63. doi: 10.1146/annurev.psych.50.1.137. [DOI] [PubMed] [Google Scholar]
- 37.Patti E, Acosta J, Chavda A, et al. Prevalence of anxiety and depression among emergency department staff. NY Med J. 2007;2:24–29. [Google Scholar]
- 38.Xianyu Y, Lambert VA. Investigation of the relationships among workplace stressors, ways of coping, and the mental health of Chinese head nurses. Nurs Health Sci. 2006;8(3):147–55. doi: 10.1111/j.1442-2018.2006.00281.x. [DOI] [PubMed] [Google Scholar]
- 39.Kust D, Murgic J, Vukovic P, et al. Oncologist burnout syndrome in Eastern Europe: Results of the multinational survey. JCO Oncol Pract. 2020;16:e366–76. doi: 10.1200/JOP.19.00470. [DOI] [PubMed] [Google Scholar]


