Abstract
Objective
To develop best-practice recommendations using thermal indices to determine work-to-rest ratios and facilitate further implementation of environmental monitoring for heat safety in secondary school athletics in the United States.
Data Sources
A narrative review of the current literature on environmental monitoring for heat safety during athletics was conducted by content experts. A list of action-oriented recommendations was established from the narrative review and further refined using the Delphi method.
Conclusions
Assessment of wet bulb globe temperature at the site of activity and throughout the duration of the event is recommended to assist clinicians and administrators in making appropriate decisions regarding the duration and frequency of activity and rest periods. Activity-modification guidelines should be predetermined and approved by stakeholders and should outline specific actions to be followed, such as the work-to-rest ratio, frequency and timing of hydration breaks, and adjustment of total exercise duration, equipment, and clothing. Furthermore, integration of exertional heat illness injury data with environmental condition characteristics is critical for the development of evidence-based heat safety guidelines for secondary school athletics. Athletic trainers play an essential role in conducting prospective injury data collection, recording onsite wet bulb globe temperature levels, and implementing recommendations to protect the health and safety of athletes.
Keywords: wet bulb globe temperature, activity-modification guidelines, exertional heat illness, exertional heat stroke
Exertional heat stroke (EHS) continues to be one of the leading causes of death in sport and physical activity in the United States, including at the secondary school level.1 Authors of prior position statements2–5> have provided evidence-based recommendations on EHS prevention. In these position statements, environmental conditions were noted as a common risk factor for EHS in athletics, and the recommendation to monitor environmental conditions was made. However, few researchers have synthesized the scientific background and current literature that support this recommendation in order to facilitate its implementation.
On May 28, 2019, a multidisciplinary group of content experts gathered in Orlando, Florida, for a roundtable meeting to discuss preseason heat safety for the secondary school student-athlete. In total, 33 participants were purposefully selected and invited by the cochairs to provide a multidisciplinary representation of individuals (1) with expertise in the proper management and care of patients with exertional heat illness (EHI); (2) who were clinicians actively providing care to secondary school student-athletes; and (3) with expertise in the realms of biometeorology, thermal physiology, and epidemiology. Roundtable participants comprised clinically practicing secondary school athletic trainers (ATs; n = 7), sports medicine physicians (n = 5), emergency room physician (n = 1), scientists with expertise in the management and care of EHS (n = 12), and scientists with expertise in biometeorology (n = 2), thermal physiology (n = 5), and epidemiology (n = 1). Among the attendees, a working group was convened to draft the current document, which aims to develop best-practice recommendations on the use of thermal indices and environmental monitoring to determine work-to-rest ratios and facilitate further implementation of environmental monitoring during activity in the heat. The group members were selected from the roundtable attendees based on their scholarly work in the areas of environmental monitoring, thermal physiology, and EHS prevention. The working group comprised 12 roundtable participants: a sports medicine physician (n = 1) and scientists with expertise in the management and care of EHS (n = 6), biometeorology (n = 2), and thermal physiology (n = 3).
METHODS
To establish consensus, we used the Delphi method, which allows for the unbiased aggregation of expert opinion among stakeholders.6 To align with current best practices for using the Delphi method, we implemented a 2-phase approach consisting of exploration and evaluation phases. Each phase is described in the next sections.
Exploration Phase
During the exploration phase, an internal working group of content experts (n = 12) conducted a narrative review of the key topics pertaining to environmental monitoring for heat safety during athletics: (1) human heat balance, (2) methods of environmental monitoring for heat safety during activity, (3) activity-modification guidelines (AMGs), (4) practical applications and considerations, and (5) use of injury-surveillance data to determine activity-modification thresholds. Each topic was reviewed by content experts, and the narrative review served as the foundation for the action-oriented recommendations.
Evaluation Phase
On completion of the exploration phase, the internal working group prepared action-oriented recommendations for environmental monitoring to be implemented within the secondary school athletics setting. After a preliminary review by the internal working group, the recommendations were modified as necessary to ensure appropriateness and clarity. Members of the multidisciplinary group who attended the roundtable were then emailed a link to an anonymous online survey (Qualtrics) for scoring the recommendations.
Roundtable members scored each recommendation by drawing on their own expertise and background in the context of validity, feasibility, and clarity.6 The intent of assessing the recommendations based on these 3 constructs was to provide meeting attendees the opportunity to draw on their experiences, knowledge, background, and training in order to critically appraise the recommendations and supply objective assessments of the suitability of the recommendations for the target audience (ie, those involved in secondary school athletics). Validity was operationally defined as whether the recommendation was substantiated based on current data, theory, literature, or other scientific evidence. Feasibility was operationally defined as whether it was realistic to expect individuals or campuses to implement the recommendation, keeping in mind the widely varying resources and competing demands that individuals and institutions may face. Clarity was operationally defined as whether the recommendation was clear and easily understood. Scores used a 9-point scale; higher scores depicted a recommendation as being more valid, feasible, or clear. Roundtable members were also given the opportunity to provide written comments on each recommendation, which allowed them to draw on their expertise and experiences to add support to their scores. This approach, which is recommended for the Delphi process, provides content experts with a systematic way of solving complex problems and allows for each expert's contributions, objective assessment of the expert group's thoughts or opinions, and reappraisal and assessment of prior contributions while minimizing bias among contributing experts.6
After each recommendation was scored, we calculated the mean of each dimension (ie, validity, feasibility, clarity) using a previously published approach.7 The response rate for scoring of the online survey was 100% (N = 32/32). Any recommendation with a mean score of <3 on any dimension was discarded, and any recommendation with a mean score of ≥7 on a dimension was retained in the final version. Recommendations with a mean score of 4, 5, or 6 were revisited for revision.8 Written comments were reviewed by the internal working group and modifications were based on these comments. Once the final modifications were made, roundtable members anonymously scored the revised recommendations using the same criteria as in the first round. Scores of the modified recommendations were analyzed, and those items that were deemed valid, feasible, and clear were included in the final product. The response rate for the second round of scoring of the online survey was 81.3% (n = 26/32). For any recommendations that scored 4, 5, or 6 on any dimension after the second round of scoring, 4 roundtable members (Y.H., W.M.A., D.J.C., J.K.V.) discussed potential modifications to the recommendation until a consensus was reached.
A comprehensive set of recommendations was then produced. For further assessment of each recommendation retained in the final list, the strength of the recommendation was determined using the Strength of Recommendation Taxonomy (SORT), which is a well-established tool for grading evidence in the medical literature.9
NARRATIVE REVIEW
Human Heat Balance
Heat strain is the challenge of heat imposed on the body by external heat sources and metabolic heat created by the body. Thus, heat strain depends on the combined effects of (1) air temperature, (2) humidity, (3) wind flow, and (4) radiative loads, as well as the behavioral factors of metabolic activity (eg, exercise intensity, exercise duration) and clothing (Figure).10 The most effective way for humans to dissipate heat is via sweat evaporation.11 When vapor pressure is greater at the skin (Psk) than in the air (Pa), sweat evaporation is facilitated.12 When this cooling system is challenged by increasing values of Pa, however, evaporative cooling is inhibited.12 In these situations, heat storage and the resulting core temperature increase unless other means of cooling, such as conduction or convection, can be facilitated. To promote evaporative and convective heat loss, peripheral blood flow is maximized during exercise, shunting blood away from the internal organs.13 This redistribution of blood allows for perfusion of the sweat glands and evaporative heat loss. Heat is also lost via convection, which is maximized when the skin-to-air temperature difference is high. Convective heat loss is compromised when the temperature of the air rises above that of skin.11 Furthermore, both evaporative and convective heat dissipation are compromised when personal protective equipment and specific work uniforms (eg, American football uniform; nuclear, biological and chemical protective clothing; firefighting ensembles; military ensembles) must be worn during activity in hot weather.5 Protective equipment and uniforms typically create a microenvironment in which heat and moisture are trapped between the clothing and skin, limiting heat losses from the skin surface. When protective equipment is required, modifications of exercise and the amount of equipment worn may be needed to adjust exercise heat stress.10
Figure.
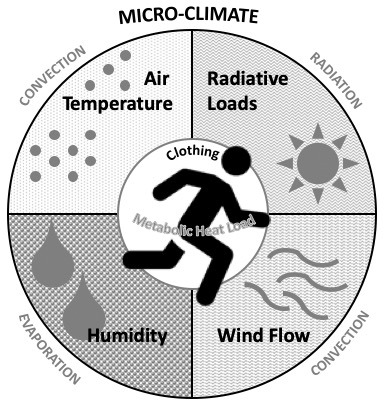
Heat strain at a given exercise intensity depends on heat exchange with the external environment (convection, radiation, evaporation), which is influenced by air temperature, radiative loads, wind flow, humidity, and insulation from clothing.
When heat balance remains in equilibrium during a bout of exercise or physical activity in a certain environment, the imposed heat strain is termed compensable, whereby the individual is able to complete a particular amount of work in a specific environment without the risk of EHI.10,11> If the environmental conditions or exercise intensity increase, the combination then results in uncompensable heat stress and an inevitable rise in core temperature, potentially to dangerous levels, unless accommodations are implemented.10,11> Therefore, the goal for clinicians caring for athletes under heat stress is to monitor environmental conditions and estimate workloads to maintain a compensable condition so that safety is maximized.
Methods of Environmental Monitoring for Heat Safety During Activity
Outdoor environmental factors, particularly wind speed and solar radiation, may vary greatly across space and time. Unfortunately, due to the limited availability of adequate weather instruments or sensors, most researchers of EHI and heat health rely on data from nearby weather stations, which may overestimate or underestimate the actual microclimate conditions that the athlete is experiencing.14–18> These misestimations are due to different surface types (eg, grass, turf, asphalt), sheltering, and anthropogenic heating, all of which can affect the overall temperature, wind speed, humidity, and radiant load at the site.19 Differences in apparent environmental conditions onsite may also arise due to the use of instruments that have low levels of precision or accuracy or are uncalibrated.
Although the 4 main environmental heat stress variables—air temperature, humidity, wind, and mean radiation loads (or mean radiant temperature)—can be monitored separately via simple and relatively inexpensive instruments, the integration of these variables into a simple heat stress metric to aid in decision making has historically received attention. The most prominent example for use in activity modification is the wet bulb globe temperature (WBGT).20 Heat stress metrics are used to assess and predict heat strain; an ideal heat stress assessment considers all aspects of heat generation and all body-environment heat exchange pathways.21 Heat stress metrics provide a single value along a continuous scale that indicates neutral to dangerous conditions. These metrics can generally be categorized from the simplest to the most complex: a direct metric is simple and does not assess physiological responses, whereas an empirical metric uses observed statistical relationships in physiological responses to environment and activity, and a rational metric applies human heat balance principles.20–25> In the United States, WBGT and heat index are the most widely used heat stress metrics. The WBGT is a direct index that was developed by the US Marine Corps under dangerously hot and humid conditions and incorporates influences from air temperature, humidity, wind, and radiation loads.26 It is derived from the following equation: WBGT = 0.7Tw + 0.2Tg + 0.1T, where Tw is the wet bulb temperature, Tg is the globe temperature, and T is the ambient temperature. In contrast, the heat index is a basic rational index that is simplified from its original version (apparent temperature) and derived from only air temperature and humidity.27 Although the heat index requires fewer variables to compute, it assumes a person is engaged in low-intensity activity in light-fitting clothing while in the shade and experiencing constant wind,28 making it inadequate for the majority of athletic events that occur in sunlit conditions.
Spatial or Temporal Scales and Instrument Considerations
When considering heat stress and heat strain predictions for a given location and sport activity, we must balance simplicity and accuracy, as well as provide real-time, informative, and actionable data to end users (eg, ATs and athletic directors). In general, standardized instrumentation and measurement procedures that meet these requirements for balance are lacking.29,30> Spatially, when addressing the use of a local weather station versus on-field or court measurements, research is required to determine which environmental conditions (depending on the design, surface, trees, and stadium19) may cause a misclassification of activity modification when nearby data, instead of on-field data, are used.31 Temporally, sensors are needed to provide user-defined moving averages (eg, integrated across 15-minute intervals) of steady and clinically meaningful exposure conditions as opposed to instantaneous fluctuations across thresholds, which can confuse decision making and may lead to unnecessary adjustments to activity.
What Level of Accuracy is Needed to Make Clinical Decisions?
Accurate meteorologic sensors for determining the WBGT are critical for heat safety decisions, given the important variations that can occur among commonly used sensors.32 Standardized sensors should display significant agreement with the International Organization for Standardization33 criteria for each WBGT component. Ensuring that the individual sensors are calibrated according to the manufacturer's specifications for effective decision making is also important. Further clinical testing, modeling, or both are needed to determine the relationship between sensor error for each variable and its relevance to human heat balance, which may also be influenced by the climate type (eg, dry or humid).34
Corrections Across Climate Types
In environmental physiology, low-wind, high-humidity conditions in warm environments are known to restrict evaporative cooling and lead to discomfort. Conversely, hot and dry conditions, which allow largely free evaporative cooling, may have deleterious effects when air temperature rises near or above skin temperature, no vapor is on the skin, or both. These factors are often worsened by athletic clothing.35 However, assumptions about the most widely used heat stress metric—the WBGT—are applied universally without considering humid versus dry climates. This may be inappropriate, given that environmental conditions yielding the same WBGT value from various combinations of air temperature, wind speed, relative humidity, and solar radiation may result in different physiological responses.20,36,37> The findings of both laboratory and field studies20,34,36,37> suggested that, for a given WBGT, heat stress may be greater in warm-humid than in hot-dry climate conditions. Thus, the WBGT may overestimate the heat stress risk in hot and dry environments but underestimate it when sweat evaporation is restricted20; however, further testing is needed. Corrections to the WBGT for both situations have been proposed by Gonzalez38 but have yet to be implemented. Such corrections have been proposed for consideration in recent consensus recommendations.39,40> In general, given the current literature and the fact that the WBGT is an environmental heat stress metric, which is a first approximation of heat stress, it is not a representation of human heat strain,39 and thus, we must adjust the WBGT measurement for proper use in hot and dry conditions. This process may involve adjusting the weighting of the coefficients in the WBGT equation or altering the threshold values in different climate types. Such adjustments will require that empirical assessments be performed in hot and dry climates.
Activity-Modification Guidelines
Activity Modifications and Cancellations
Various international and national medical and sports associations have established WBGT-based AMGs to help direct athletes, clinicians, and sporting event organizers to modify physical activity by changing exercise duration, exercise intensity, clothing ensembles, and frequency of rest and hydration breaks.4,5,41–47> These AMGs also set thresholds for activity cancellation, which range from 28°C to 34°C WBGT depending on the target population, geographic region, and type of activity (eg, practice, competition, endurance race). For example, the International Institute for Race Medicine41 set >28°C as the cancellation threshold for endurance race events, whereas Australian tennis officials43 set >34°C as the cancellation threshold for competitions. These differences are influenced by the mode and type of exercise: sustained, high-intensity exercise such as road race running warrants relatively lower thresholds, and geographic climate patterns are unique to their activity context. For example, a threshold lower than this value in Australian tennis may result in cancellation of most competitions. These cancellation thresholds are generally already taken into account for mass-participation events and games that attract many spectators.
In addition to cancellation thresholds, AMGs generally contain 3 or 4 levels of risk categories that guide coaches and clinicians when to modify the duration, intensity, equipment worn during activity, or all of these (Table 1).4,5,42> Traditionally, WBGT thresholds and activity modifications for risk categories have been established by consensus among experts in thermal physiology and military medicine.14,48> In recent years, authors15–17> have retrospectively examined the correlation between these risk categories and the incidence of exertional heat-related injuries and fatalities in the United States. Findings from these studies confirmed a heightened risk of EHS episodes and fatalities when the risk category indicated the need for event cancellation17 and an increased number of medical tent evaluations due to EHS when conditions were in higher risk categories.16 However, WBGT thresholds and the prevalence of EHS fatalities vary geographically.15 Researchers15,49,50> who assessed military and athlete populations advised that thresholds for AMGs be lower for those acclimatized to cooler conditions. Furthermore, Hosokawa et al16 found no association between WBGT risk categories and the prevalence of heat exhaustion compared with EHS during a summer road running race.
Table 1.
Examples of Incremental Activity Intensity, Duration, Equipment, and Work-to-Rest Ratio Modifications for Exercise in the Heata
| Level |
Intensity |
Duration |
Equipment |
Work-to-Rest Ratio (Total Rest, min/h) |
| 1 | No restriction | No restriction | No restriction | 5 : 1 (10) |
| 2 | Allow self-pacing | Maximum of 2-h activity | Remove protective equipment during breaks | 4 : 1–3 : 1 (12–15) |
| 3 | Relatively low-intensity exercise | Maximum of 2-h activity with increased rest breaks | No protective equipment during conditioning or practice | 2 : 1–1 : 1 (20–30) |
| 4 | Walk through, no conditioning | Maximum of 1-h activity | No protective equipment | Work < rest (continuous heat exposure should not exceed 30 min) |
| 5 | Cancel activity | Cancel activity | NA | Cancel activity |
Abbreviation: NA, not applicable.
Modified from Hosokawa et al.67
Implementation of AMGs
Although a generic description of risk categories (eg, exercise with discretion) may be simple and easy to understand, more quantifiable and actionable activity modifications (eg, provide ≥4 separate rest breaks of ≥4 minutes per hour) may facilitate AMG implementation. Detailed AMGs can also help eliminate variability and inappropriate application of these recommendations.4 For example, the Georgia High School Association developed an AMG that lists specific work-to-rest ratios by different WBGT risk categories and supplies instructions for equipment modifications for American football.14 The association based its risk categories and recommendations on epidemiologic data of EHIs in Georgia high school athletes and local weather patterns, which makes the AMG practical for its particular setting.51
Examples of implementation strategies for competition-specific activity modification in amateur and school-organized sports are scarce. At the professional level, if the WBGT exceeds 32°C, the Fédération de Football Association mandates 3-minute cooling breaks at the 30th and 75th minute of the game.52 These breaks are implemented by the referee on the pitch, which is a unique example of an AMG specific to competition.
Practical Application and Considerations
When drafting policies and procedures for performing environmental assessments in the field, a number of practical variables should be considered: the height and position of the WBGT monitor, placement of the monitor in similar environmental conditions as the activity, and reading the WBGT at predetermined time intervals.32 Onsite weather assessments are preferred over the use of a mobile phone application or distant weather station data, as these values do not always reflect local microclimate conditions. If a limited number of monitoring devices is available, institutional policy should document specific communication procedures for those supervising activity away from the assessment site. In addition, WBGT monitors should be turned on and exposed to the current environmental conditions at least 15 minutes before (or per the manufacturer's recommendations) the start of activity to allow the instrument to equilibrate to atmospheric conditions.51,53–55> Furthermore, it may be prudent for ATs, coaches, and athletic directors to establish a rule for sharing the instrument, the data, or both among various athletic facilities when certain locations are exposed to higher environmental heat. Preseason discussions can help minimize the need to conduct practices under high-risk conditions because locations with optimal playing conditions are limited. It may also allow for proactive adjustments to practice locations and times.
Location of Environmental Monitoring
The standard practice for heat stress monitoring is to conduct the assessment at the site of activity. For example, in 2 studies51,53> in which the authors investigated EHI rates among interscholastic and intercollegiate American football participants, WBGT measurements were taken adjacent to the practice field and at a height of 0.9 m (3 ft), thus capturing the most representative microclimate conditions experienced by the athletes. Cheuvront et al31 measured WBGT at 3 locations along the race course during the Boston Marathon. The measurement differences were not significant, and therefore, the practice of taking the environmental assessment at 1 location along the course was supported.31 Consequently, in settings where multiple adjacent sporting fields are hosting athletic events simultaneously, it may be feasible to reduce the number of monitoring sites. However, similar environmental conditions that result in the same heat risk category between fields or courts should first be confirmed and documented for hot and sunny days. Santee et al56 suggested that micrometeorologic assessments be taken at the approximate torso height of the participants (1.2 m) for accurate thermal assessment. Still, assessments should be taken at the height recommended by the manufacturer. It is important to note that measurements taken at a regional weather station, while convenient, do not necessarily represent local conditions for the 3 variables used to compute the WBGT (see earlier section, “Spatial or Temporal Scales and Instrument Considerations”)19,57>; if regional values are used, wind speed must be adjusted for human height in the WBGT algorithm, because it is often set at a height of 10 m.
Frequency of WBGT Measurements
During prolonged activity, environmental conditions may change, so policies should address the frequency of assessing WBGT onsite. Such changes in the environmental conditions, particularly wind speed and solar radiation, lead to fluctuating WBGT values, which can cause difficulty in determining activity modifications based on an institution's policy. Although few researchers have evaluated the effect of frequency on WBGT measures, the ideal frequency of WBGT measurements has been examined. In 2 studies51,53> of EHI rates among interscholastic and intercollegiate American football participants, WBGT measurements were taken at 15-minute intervals during practice, whereas another group54 took measurements at the beginning, middle, and end of the practice session. Differences in the timing of measurements in these studies were mostly influenced by logistical considerations; fixed interval measurements were only practical when devices with automated recording features were available. A realistic number of measurements taken manually (ie, designated personnel reading and recording WBGT measurements) was limited to the beginning, middle, and end of the practice session. Further, Kopec58 evaluated WBGT measurements based on different land surfaces. A significant time lag in WBGT values was noted, especially when the black globe measurements were affected by changes in cloud cover due to the time required for the globe temperature to reach a steady state. Additionally, changes in wind speed can lead to fluctuating WBGT values. The author suggested averaging WBGT values over a 30-minute period (ie, relying on a rolling average of the previous 30 minutes) before modifying activity intensity.58 This recommendation is particularly important when WBGT values are near the highest threshold of the index, warranting cancellation or significant modification of the activity. Based on the available evidence, we suggest that clinicians assess and record WBGT at intervals of ≤30 minutes to reflect atmospheric variations59 and include this guideline in practice policies. When assessing WBGT this frequently is impractical, we advise taking WBGT readings at ≤60 minutes, a standard already implemented by the Georgia High School Association.47 Measurement intervals >60 minutes are considered too long because sustained, high-intensity exercise lasting 30 to 60 minutes in warm weather can result in EHS.16 We believe that taking measurements every 30 minutes is not unduly burdensome with the use of technology such as a monitoring device that can automatically record and transfer readings to a smartphone or a tablet to minimize the physical effort. A simpler method, such as designating a staff member (eg, team manager or assistant coach) to take periodic readings of the environmental conditions and report back to the AT should also be considered so that activity-modification decisions can be made without interfering with other clinical responsibilities. When consecutive measures cross different AMG categories, clinicians should follow the recommendations of the higher risk category.
Special Considerations for Monitoring WBGT During Competition
Apart from road race events, few to no clinical data support the monitoring of WBGT values during competitions, unlike during practice sessions, or endorse creating policies for monitoring WBGT during competition.15,60> This lack of data may be due to numerous epidemiologic studies of EHI rates during practice sessions yet few that involved monitoring EHI rates during competitions.47,53,55,61> The rationalization was that participants in team sports were exposed to far longer periods of environmental stress and metabolic loads during practice sessions, when there were longer periods of activity between rest breaks than seen during competitions. However, in team sports with limited substitutions (eg, soccer), athletes who play the full match may have many fewer opportunities for rest breaks than during traditional practice sessions. Therefore, it is prudent to monitor WBGT during competitions, especially when they are held at peak times throughout the day or during atypically high WBGT conditions. This can help establish AMGs such as event-cancellation thresholds41,43> and inform policies regarding increased hydration breaks.44
Sport-governing organizations or institutions should take the lead in establishing AMGs for participating teams, yet ATs play a key role in ensuring that these guidelines are implemented on the field. To facilitate AMG implementation, ATs are advised to discuss activity-modification plans with coaches, referees, or both before athletic events or during the medical time out. Consequently, to make informed decisions about activity modifications, ATs should set up the WBGT device 30 minutes before the athletic event, thereby allowing ample time (≥15 minutes) for the device to equilibrate to the environment while leaving time for the staff discussion.
Use of Injury-Surveillance Data to Determine Activity-Modification Thresholds
The athletic training and sports medicine communities have recognized the importance of population-based investigations in developing injury-prevention strategies, including modifications during extreme heat.62,63> A variety of databases have been developed and refined to improve the surveillance of sport-related injuries and injury rates among athletes (eg, National Center for Catastrophic Injury Research, National Collegiate Athletic Association Injury Surveillance System, National High School Sports-Related Injury Surveillance System). These databases have aided researchers in identifying the leading causes of sudden death in sports and, in particular, the sports with heat exposure as a key risk factor.3,64> Limitations exist in the standardization and geolocation of EHIs across the country due to deidentification of case information. Nevertheless, such data are needed to elucidate the geographic and climatologic nature of EHIs for more appropriate regional recommendations.
Recognizing the hazard posed by heat exposure in secondary school and collegiate American football players, multiple authors18,51,53–55,65,66,68> have attempted to understand the relationship of environmental heat, EHI rates, and acclimatization among athletic populations of various ages and apply this knowledge to actionable injury prevention. Various data are required when developing policies for EHI (Table 2). Most commonly, onsite measurements of WBGT are collected throughout practices to better prevent heat stress.53–55> In addition, data relevant to the practice session, such as length and intensity, should be collected. Finally, the specific type of EHI (ie, exercise-associated muscle cramps, heat syncope, heat exhaustion, heat injury, or EHS) should be identified and documented by trained medical professionals. For cases of EHS, individual athlete characteristics, such as position, body mass index, preexisting illnesses or conditions, and use of medications or supplements should also be documented.4,17> As these data are accumulated, sports injury epidemiologists and clinicians should test the associations between environmental heat risk categories and incidence rates of heat-related injuries so that more refined, evidence-driven policies can be established. Additionally, the validity of AMG thresholds should be reviewed in consultation with biometeorology and meteorology specialists to examine the influence of geographic and regional climatologic characteristics.
Table 2.
Useful Variables to Record for Determinung the Association Between Meteorologic Conditions and Exertional Heat Illness (EHI) Incidence in Athleticsa
| Variables recorded daily |
| Sport type (continuous or noncontinuous) |
| Date and start time of exercise session |
| Weather conditions (eg, wet bulb globe temperature) |
| Number of participants per session |
| Exercise duration |
| Relative exercise intensity (low, moderate, high) |
| Clothing or equipment configuration |
| Variables recorded per EHI incident |
| EHI typeb (eg, exercise-associated muscle cramps, heat syncope, heat exhaustion, heat injury, exertional heat stroke) |
| Age, sex |
| Field position (eg, offense, defense, goalkeeper) |
| History of recent illness and EHI |
| Use of medications or supplements |
| Patient body mass and body composition |
| Heat-acclimatization status (ie, completed >10 d of organized practice in heat within last 3 mo) |
EHI incidence rate can be computed as the number of EHI incidents or total athlete-exposures. Incidence rates may be computed for each EHI type.
Modified from Casa et al.4
CONSENSUS PROCESS AND RESULTS
Our expert consensus on environmental monitoring for heat safety during activity is summarized in Table 3. After 2 rounds of the review process, all of the recommendations in Table 3 scored 7 or more (out of 9) for validity, feasibility, and clarity. One recommendation was removed due to a low feasibility score (6.69). The final recommendations encompassed 4 domains: (1) WBGT measurement methods (recommendations 1–4), (2) the contents of AMGs (recommendations 5–7), (3) organizational considerations for implementation (recommendations 8 and 9), and (4) data collection (recommendation 10).
Table 3.
Consensus on Current Expert Recommendations Regarding Environmental Monitoring for Heat Safety During Activity
| Recommendation |
Strength of Recommendation Taxonomy9 |
| 1. Heat stress monitoring should be conducted onsite at a location that representats all playing surfaces (ie, over similar surface and in an open location that is not influenced by surrounding buildings). | B |
| 2. The WBGT measurements should be taken at the activity location with an environmental monitor designed to measure WBGT at a height of 0.9–1.2 m (3–4 ft) from the playing surface. If limited monitoring sites or devices are available, institutional policy should document specific communication procedures for those supervising activity remote from WBGT assessment site(s). | C |
| 3. The WBGT measurement devices should remain exposed to the environment before activity per manufacturer's recommendations or ≥15 min. | B |
| 4. The WBGT measurements should be taken at intervals (frequency of recording) ≤30 min for the duration of the athletic activity. | C |
| 5. The AMGs should outline specific actions (eg, work-to-rest ratio, frequency and timing of hydration breaks, adjustment of total exercise duration, equipment adjustment) and be mandated for all athletic training and competitions. | C |
| 6. The AMG thresholds should be established based on geographic and regional climatologic characteristics. | B |
| 7. State athletic associations should develop and implement environmentally based AMGs that outline specific event modifications and cancellation policies. These guidelines should be developed by, or in coordination with, the state's sports medicine advisory committee or appropriate sports medicine professionals. | C |
| 8. Institutions should develop and implement policies and procedures detailing the procedures for WBGT monitoring and AMGs used for practices, conditioning sessions, and competitions. | C |
| 9. Before a competition, adequate time should be allotted for a medical time out, which includes a discussion of necessary accommodations due to the environmental heat (eg, additional hydration breaks, alteration of competition timing and length) with all decision makers onsite (eg, coaches, athletic director, referees). | C |
| 10. If an exertional heat illness occurs, the athlete's medical record should include details surrounding the injury, such as environmental conditions, time of year, duration and type of activity (eg, conditioning, scrimmage, skill practice), and physical characteristics (eg, fitness, acclimatization state, hydration state) to retrospectively identify risk factors responsible. | B |
Abbreviations: AMG, activity-modification guideline; WBGT, wet bulb globe temperature.
The expert consensus on environmental monitoring procedures is summarized in Table 4. All of the procedures listed in Table 4 achieved scores of 7 or more (out of 9) for validity, feasibility, and clarity after the second round of review.
Table 4.
Consensus on Current Expert Recommendations for Environmental Monitoring Procedures
| Recommendation |
Strength of Recommendation Taxonomy9 |
| 1. The environmental monitor used for determining WBGT should measure air temperature, wind speed, and black globe temperature and either measure or compute natural WBGT. | A |
| 2. For each athletic field, a location for onsite measurement that represents the field of play should be identified. If a limited number of measurement devices are available, a location that represents all playing fields for environmental monitoring through comparisons on hot and sunny days should be selected. | B |
| 3. The environmental monitor should be set up at a height of 0.9–1.2 m (3–4 ft) at least 30 min before practice or competition. This allows the device to equilibrate in the first 15 min and leaves an additional 15 min for a medical time out to discuss the accommodation plan based on WBGT. | C |
| 4. The athletic trainer, or other designated personnel (eg, athletic director) if the athletic trainer is not present, should discuss activity-modification plans with coaches and referees before practice or competition. | C |
| 5. The WBGT measurements should be taken at intervals of ≤30 min for the duration of the practice or competition and activity modified according to policy and procedures.a | C |
| 6. If the risk categories of consecutive measures frequently reflect different levels of activity modification, the activity modification for the higher risk category should be followed. | C |
Abbreviation: WBGT, wet bulb globe temperature.
When frequent WBGT assessment (ie, every 30 min) is impractical, we suggest taking measurements at least every 60 min.
Most of the guidelines in Tables 3 and 4 were classified as Strength of Recommendation Taxonomy category C, which is defined as a recommendation based on consensus, usual practice, opinion, disease-oriented evidence, or a case series for studies of diagnosis, treatment, prevention, or screening.9 This is mainly due to the lack of randomized controlled trial research and prospective cohort studies in the topic area. This lack of studies is an inherent limitation commonly observed in EHS research, as it is not ethically permissible to require participants to experience EHS. To strengthen the current recommendations in the future, more retrospective cohort studies and case series with high-quality data (Table 2) are warranted to synthesize observations from various settings.
CONCLUSIONS
Limited studies are available to establish evidence-based methods of environmental monitoring for heat safety in secondary school athletics. However, the findings of existing observational studies about EHI and research in thermoregulation and biometeorology elucidate key considerations for ensuring athlete safety during activities in the heat. Continued efforts to encourage ATs to conduct prospective injury data collection and record onsite WBGT measurements using a standardized method are needed to facilitate the development of evidence-based heat safety guidelines for secondary school athletics.
ACKNOWLEDGMENTS
We acknowledge the National Athletic Trainers' Association, Korey Stringer Institute, and American College of Sports Medicine for providing support for the roundtable meeting. We also thank the meeting attendees for their contributions at the roundtable meeting and to the Delphi voting process.
REFERENCES
- 1. .Kucera KL, Cantu RC. Catastrophic sports injury research: thirty-sixth annual report fall 1982–spring 2018. National Center for Catastrophic Sport Injury Research Web site. 20192019 https://nccsir.unc.edu/files/2019/10/2018-Catastrophic-Report-AS-36th-AY2017-2018-FINAL.pdf Accessed November 22.
- 2. .Binkley HM, Beckett J, Casa DJ, Kleiner DM, Plummer PE. National Athletic Trainers' Association position statement: exertional heat illnesses. J Athl Train. 2002;37(3):329–343. [PMC free article] [PubMed] [Google Scholar]
- 3. .Casa DJ, Guskiewicz KM, Anderson SA, et al. National Athletic Trainers' Association position statement: preventing sudden death in sports. J Athl Train. 2012;47(1):96–118. doi: 10.4085/1062-6050-47.1.96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. .Casa DJ, DeMartini JK, Bergeron MF, et al. National Athletic Trainers' Association position statement: exertional heat illnesses. J Athl Train. 2015;50(9):986–1000. doi: 10.4085/1062-6050-50.9.07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. .American College of Sports Medicine. LE Armstrong, Casa DJ, et al. American College of Sports Medicine position stand. Exertional heat illness during training and competition. Med Sci Sports Exerc. 2007;39(3):556–572. doi: 10.1249/MSS.0b013e31802fa199. [DOI] [PubMed] [Google Scholar]
- 6. .Adler M, Ziglio E. Gazing into the Oracle The Delphi Method and its Application to Social Policy and Public Health. London: Jessica Kingsley Publishers;; 1996. [Google Scholar]
- 7. .Kroshus E, Wagner J, Wyrick D, et al. Wake up call for collegiate athlete sleep: narrative review and consensus recommendations from the NCAA Interassociation Task Force on Sleep and Wellness. Br J Sports Med. 2019;53(12):731–736. doi: 10.1136/bjsports-2019-100590. [DOI] [PubMed] [Google Scholar]
- 8. .Zumsteg JM, Cooper JS, Noon MS. Systematic review checklist: a standardized technique for assessing and reporting reviews of life cycle assessment data. J Ind Ecol. 2012;16(suppl 1):S12–S21. doi: 10.1111/j.1530-9290.2012.00476.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. .Ebell MH, Siwek J, Weiss BD, et al. Strength of recommendation taxonomy (SORT): a patient-centered approach to grading evidence in the medical literature. Am Fam Physician. 2004;69(3):548–556. [PubMed] [Google Scholar]
- 10. .Grundstein A, Knox JA, Vanos J, Cooper ER, Casa DJ. American football and fatal exertional heat stroke: a case study of Korey Stringer. Int J Biometeorol. 2017;61(8):1471–1480. doi: 10.1007/s00484-017-1324-2. [DOI] [PubMed] [Google Scholar]
- 11. .Cramer MN, Jay O. Biophysical aspects of human thermoregulation during heat stress. Auton Neurosci. 2016;196:3–13. doi: 10.1016/j.autneu.2016.03.001. [DOI] [PubMed] [Google Scholar]
- 12. .Sawka MN, Castellani JW, Cheuvront SN, Young AJ. Physiologic systems and their responses to conditions of heat and cold. In: PA Farrell, Joyner MJ, Caiozzo VJ., editors. ACSM's Advanced Exercise Physiology 2nd ed. Philadelphia, PA: Wolters Kluwer | Lippincott Williams & Wilkins;; 2011. chap 23. [Google Scholar]
- 13. .Cheuvront SN, Kenefick RW, Montain SJ, Sawka MN. Mechanisms of aerobic performance impairment with heat stress and dehydration. J Appl Physiol (1985) 2010;109(6):1989–1995. doi: 10.1152/japplphysiol.00367.2010. [DOI] [PubMed] [Google Scholar]
- 14. .Kark JA, Burr PQ, Wenger CB, Gastaldo E, Gardner JW. Exertional heat illness in Marine Corps recruit training. Aviat Space Environ Med. 1996;67(4):354–360. [PubMed] [Google Scholar]
- 15. .Grundstein AJ, Hosokawa Y, Casa DJ. Fatal exertional heat stroke and American football players: the need for regional heat-safety guidelines. J Athl Train. 2018;53(1):43–50. doi: 10.4085/1062-6050-445-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. .Hosokawa Y, Adams WM, Belval LN, et al. Exertional heat illness incidence and on-site medical team preparedness in warm weather. Int J Biometeorol. 2018;62(7):1147–1153. doi: 10.1007/s00484-018-1517-3. [DOI] [PubMed] [Google Scholar]
- 17. .Grundstein AJ, Ramseyer C, Zhao F, et al. A retrospective analysis of American football hyperthermia deaths in the United States. Int J Biometeorol. 2012;56(1):11–20. doi: 10.1007/s00484-010-0391-4. [DOI] [PubMed] [Google Scholar]
- 18. .Yeargin SW, Cahoon E, Hosokawa Y, Mensch JM, Dompier TP, Kerr ZY. Environmental conditions and seasonal variables in American youth football leagues. Clin Pediatr (Phila) 2017;56(13):1209–1218. doi: 10.1177/0009922816684603. [DOI] [PubMed] [Google Scholar]
- 19. .Pryor JL, Pryor RR, Grundstein A, Casa DJ. The heat strain of various athletic surfaces: a comparison between observed and modeled wet-bulb globe temperatures. J Athl Train. 2017;52(11):1056–1064. doi: 10.4085/1062-6050-52.11.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. .Budd GM. Wet-bulb globe temperature (WBGT)—its history and its limitations. J Sci Med Sport. 2008;11(1):20–32. doi: 10.1016/j.jsams.2007.07.003. [DOI] [PubMed] [Google Scholar]
- 21. .Havenith G, Fiala D. Thermal indices and thermophysiological modeling for heat stress. Compr Physiol. 2015;6(1):255–302. doi: 10.1002/cphy.c140051. [DOI] [PubMed] [Google Scholar]
- 22. .Macpherson RK. The assessment of the thermal environment. A review. Br J Ind Med. 1962;19(3):151–164. doi: 10.1136/oem.19.3.151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. .Parsons K. Human Thermal Environments The Effects of Hot Moderate and Cold Environments on Human Health Comfort and Performance. Boca Raton, FL: CRC Press; 2014. 2019. 3rd ed. https://www.crcpress.com/Human-Thermal-Environments-The-Effects-of-Hot-Moderate-and-Cold-Environments/Parsons/p/book/9781466595996 Accessed June 5. [Google Scholar]
- 24. .de Freitas CR, Grigorieva EA. A comparison and appraisal of a comprehensive range of human thermal climate indices. Int J Biometeorol. 2017;61(3):487–512. doi: 10.1007/s00484-016-1228-6. [DOI] [PubMed] [Google Scholar]
- 25. .Epstein Y, Moran DS. Thermal comfort and the heat stress indices. Ind Health. 2006;44(3):388–398. doi: 10.2486/indhealth.44.388. [DOI] [PubMed] [Google Scholar]
- 26. .Yaglou CP, Minard D. Control of heat casualties at military training centers. AMA Arch Ind Health. 1957;16(4):302–316. [PubMed] [Google Scholar]
- 27. .Hosokawa Y, Grundstein AJ, Vanos JK, Cooper ER. Environmental condition and monitoring. Ch. 9. In: Sport and Physical Activity in the Heat Maximizing Performance and Safety. Cham Switzerland Springer; 2018:147–162. doi: 10.1007/978-3-319-70217-9_9. [DOI]
- 28. .Steadman RG. The assessment of sultriness. Part I: a temperature-humidity index based on human physiology and clothing science. J Appl Meteor. 1979;18(7):861–873. doi: 10.1175/1520-0450(1979)018<0861:TAOSPI>2.0.CO;2. [DOI] [Google Scholar]
- 29. .Oke TR. Instruments and observing methods report no. 81. Initial guidance to obtain representative meteorological observations at urban sites. World Meteorological Organization Web site. 2020 https://www.wmo.int/pages/prog/www/IMOP/publications/IOM-81/IOM-81-UrbanMetObs.pdf Published 2006. Accessed July 23.
- 30. .Johansson E, Thorsson S, Emmanuel R, Krüger E. Instruments and methods in outdoor thermal comfort studies—the need for standardization. Urban Clim. 2014;10(2):346–366. doi: 10.1016/j.uclim.2013.12.002. [DOI] [Google Scholar]
- 31. .Cheuvront SN, Caruso EM, Heavens KR, et al. Effect of WBGT index measurement location on heat stress category classification. Med Sci Sports Exerc. 2015;47(9):1958–1964. doi: 10.1249/MSS.0000000000000624. [DOI] [PubMed] [Google Scholar]
- 32. .Cooper E, Grundstein A, Rosen A, Miles J, Ko J, Curry P. An evaluation of portable wet bulb globe temperature monitor accuracy. J Athl Train. 2017;52(12):1161–1167. doi: 10.4085/1062-6050-52.12.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. .Technical Committee: ISO/TC 159/SC 5 Ergonomics of the physical environment. ISO 7243:2017 Ergonomics of the thermal environment—assessment of heat stress using WBGT (wet bulb globe temperature) index. 2019 http://www.iso.org/cms/render/live/en/sites/isoorg/contents/data/standard/06/71/67188.html Published online August 2017. Accessed September 25.
- 34. .Vanos JK, Grundstein AJ. Variations in athlete heat loss potential between hot-dry and warm-humid environments at equivalent WBGT thresholds. J Athl Train. In press doi: 10.4085/1062-6050-313-19. [DOI] [PMC free article] [PubMed]
- 35. .Armstrong LE, Johnson EC, Casa DJ, et al. The American football uniform: uncompensable heat stress and hyperthermic exhaustion. J Athl Train. 2010;45(2):117–127. doi: 10.4085/1062-6050-45.2.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. .Ramanathan NL, Belding HS. Physiological evaluation of the WBGT index for occupational heat stress. Am Ind Hyg Assoc J. 1973;34(9):375–383. doi: 10.1080/0002889738506866. [DOI] [PubMed] [Google Scholar]
- 37. .Budd GM. How do wildland firefighters cope? Physiological and behavioural temperature regulation in men suppressing Australian summer bushfires with hand tools. J Thermal Biol. 2001;26(4–5):381–386. doi: 10.1016/S0306-4565(01)00048-1. [DOI] [Google Scholar]
- 38. .Gonzalez RR. Biophysics of heat exchange and clothing: applications to sports physiology. Med Exerc Nutr Health. 1995;4:290–305. [Google Scholar]
- 39. .Racinais S, Alonso JM, Coutts AJ, et al. Consensus recommendations on training and competing in the heat. Br J Sports Med. 2015;49(18):1164–1173. doi: 10.1136/bjsports-2015-094915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. .Périard JD, Jay O, Alonso J-M, et al. Author's reply to Brocherie and Millet: ‘Is the wet-bulb globe temperature (WGBT) index relevant for exercise in the heat?'. Sports Med. 2015;45(11):1623–1624. doi: 10.1007/s40279-015-0392-x. [DOI] [PubMed] [Google Scholar]
- 41. .Mears S, Watson P. IIRM. Medical Care Manual. International Institute for Race Medicine Web site. 2016 http://www.racemedicine.org/en-us/Admin/Medical-Manual-Preview Accessed October 2.
- 42. .Recognize to Recover. Heat Guidelines. US Soccer Web site. 2019 https://static1.squarespace.com/static/57125d942eeb814000fb1ca5/t/5a1c4fdc8165f542d6d78d16/1511804893401/1609024+Heat+Guidelines.pdf Accessed May 5.
- 43. .Chalmers S, Jay O. Australian community sport extreme heat policies: limitations and opportunities for improvement. J Sci Med Sport. 2018;21(6):544–548. doi: 10.1016/j.jsams.2018.01.003. [DOI] [PubMed] [Google Scholar]
- 44. .Associated Press. Court orders FIFA to implement water breaks. USA Today Web site. 2019 https://www.usatoday.com/story/sports/soccer/2014/06/20/court-orders-fifa-to-implement-water-breaks/11106571/ Published June 20, 2014. Accessed May 5.
- 45. .Council on Sports Medicine and Fitness and Council on School Health, Bergerson MF, Devore C, Rice SG, American Academy of Pediatrics. Policy statement—climatic heat stress and exercising children and adolescents. Pediatrics. 2011;128(3):e741–e747. doi: 10.1542/peds.2011-1664. [DOI] [PubMed] [Google Scholar]
- 46. .NCAA heat acclimation policy. 2003–04 NCAA Division I Manual. Indianapolis, IN: National Collegiate Athletic Association; 2003. [Google Scholar]
- 47. .Georgia High School Association. Practice Policy for Heat and Humidity. Georgia High School Association Web site. 2020 https://www.ghsa.net/sites/default/files/documents/sports-medicine/HeatPolicy2018.pdf Accessed July 12.
- 48. .American College of Sports Medicine position stand on the prevention of thermal injuries during distance running. Med Sci Sports Exerc. 1987;19(5):529–533. [PubMed] [Google Scholar]
- 49. .Carter R, 3rd, Cheuvront SN, Williams JO, et al. Epidemiology of hospitalizations and deaths from heat illness in soldiers. Med Sci Sports Exerc. 2005;37(8):1338–1344. doi: 10.1249/01.mss.0000174895.19639.ed. [DOI] [PubMed] [Google Scholar]
- 50. .Poore S, Grundstein A, Cooper E, Shannon J. Regional differences in exertional heat illness rates among Georgia USA high school football players. Int J Biometeorol. 2020;64(4):643–650. doi: 10.1007/s00484-019-01853-4. [DOI] [PubMed] [Google Scholar]
- 51. .Cooper ER, Grundstein AJ, Miles JD, et al. Heat policy revision for Georgia high school football practices based on data-driven research. J Athl Train. 2020;55(7):673–681. doi: 10.4085/1062-6050-542-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. .Temperature measurement—FIFA Medical Platform. FIFA Medical Network Web site. 2019 https://www.fifamedicinediploma.com/topic/environment-temperature-measurement/ Accessed May 26.
- 53. .Cooper ER, Ferrara MS, Casa DJ, et al. Exertional heat illness in American football players: when is the risk greatest? J Athl Train. 2016;51(8):593–600. doi: 10.4085/1062-6050-51.8.08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. .Cooper ER, Ferrara MS, Broglio SP. Exertional heat illness and environmental conditions during a single football season in the southeast. J Athl Train. 2006;41(3):332–336. [PMC free article] [PubMed] [Google Scholar]
- 55. .Tripp BL, Eberman LE, Smith MS. Exertional heat illnesses and environmental conditions during high school football practices. Am J Sports Med. 2015;43(10):2490–2495. doi: 10.1177/0363546515593947. [DOI] [PubMed] [Google Scholar]
- 56. .Santee WR, Matthew WT, Blanchard LA. Effects of meteorological parameters on adequate evaluation of the thermal environment. J Thermal Biol. 1994;19(3):187–198. doi: 10.1016/0306-4565(94)90030-2. [DOI] [Google Scholar]
- 57. .Tripp B, Vincent HK, Bruner M, Smith MS. Comparison of wet bulb globe temperature measured on-site vs estimated and the impact on activity modification in high school football. Int J Biometeorol. 2020;64(4):593–600. doi: 10.1007/s00484-019-01847-2. [DOI] [PubMed] [Google Scholar]
- 58. .Kopec RJ. Response of the wet-bulb-globe-thermometer heat stress index to selected land use surfaces. Southeast Geogr. 1977;17(2):133–145. doi: 10.1353/sgo.1977.0009. [DOI] [Google Scholar]
- 59. .Grundstein A, Cooper E. Comparison of WBGTs over different surfaces within an athletic complex. Medicina (Kaunas) 2020;56(6):313. doi: 10.3390/medicina56060313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. .Grimmer K, King E, Larsen T, et al. Prevalence of hot weather conditions related to sports participation guidelines: a South Australian investigation. J Sci Med Sport. 2006;9(1):72–80. doi: 10.1016/j.jsams.2006.02.006. [DOI] [PubMed] [Google Scholar]
- 61. .Dick R, Ferrara MS, Agel J, et al. Descriptive epidemiology of collegiate men's football injuries: National Collegiate Athletic Association injury surveillance system, 1988–1989 through 2003–2004. J Athl Train. 2007;42(2):221–233. [PMC free article] [PubMed] [Google Scholar]
- 62. .Hoffman MA, Johnson ST, Norcross MF. The intersection of athletic training and public health. J Athl Train. 2019;54(2):121. doi: 10.4085/1062-6050-54-02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. .Dompier TP, Kucera KL, Drezner JA, Casa DJ, Register-Mihalik JK, Guskiewicz KM. Sudden death and catastrophic injury reporting: a call to action for athletic trainers. J Athl Train. 2019;54(2):122–123. doi: 10.4085/1062-6050-77-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. .Kerr ZY, Casa DJ, Marshall SW, Comstock RD. Epidemiology of exertional heat illness among U.S. high school athletes. Am J Prev Med. 2013;44(1):8–14. doi: 10.1016/j.amepre.2012.09.058. [DOI] [PubMed] [Google Scholar]
- 65. .Yeargin SW, Casa DJ, Armstrong LE, et al. Heat acclimatization and hydration status of American football players during initial summer workouts. J Strength Cond Res. 2006;20(3):463–470. doi: 10.1519/20596.1. [DOI] [PubMed] [Google Scholar]
- 66. .Yeargin SW, Casa DJ, Judelson DA, et al. Thermoregulatory responses and hydration practices in heat-acclimatized adolescents during preseason high school football. J Athl Train. 2010;45(2):136–146. doi: 10.4085/1062-6050-45.2.136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. .Hosokawa Y, Casa DJ, Trtanj JM, et al. Activity modification in heat: critical assessment of guidelines across athletic, occupational, and military settings in the USA. Int J Biometeorol. 2019;63(3):405–427. doi: 10.1007/s00484-019-01673-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. .Yeargin SW, Kerr ZY, Casa DJ, et al. Epidemiology of exertional heat illnesses in youth, high school, and college football. Med Sci Sports Exerc. 2016;48(8):1523–1529. doi: 10.1249/MSS.0000000000000934. [DOI] [PubMed] [Google Scholar]


