The role of tumor necrosis factor α (TNF-α) inhibitors in the development of vitiligo is controversial. Several case reports have revealed a therapeutic benefit in patients affected by vitiligo receiving anti-TNF-α therapy for other diseases.1,2 The therapeutic effect of anti-TNF-α agents on vitiligo might result from opposing the inhibition of melanogenesis by TNF-α. Indeed, it has been demonstrated that TNF-α exerts a melanocytotoxic effect, reducing the level of tyrosinase in vitro.2,3 On the other hand, anti-TNF-α therapies have been associated with the development of a considerable number of autoimmune diseases, including vitiligo.4
Case report
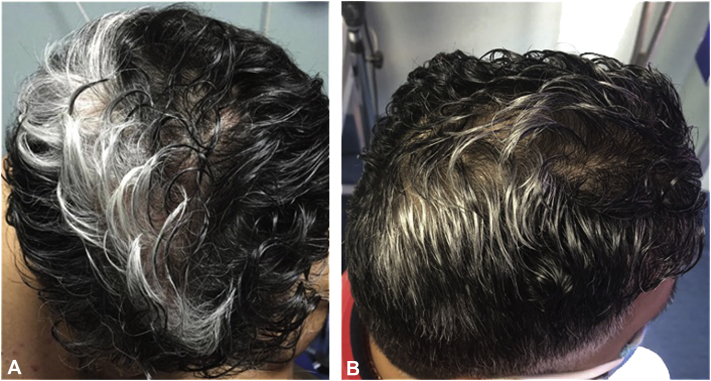
We report the case of a 40-year-old man with an 18-year history of psoriasis and psoriatic arthritis, a positive family history (through his father) of psoriasis and psoriatic arthritis, and an absence of comorbidities. Since 2008, he had been treated for periods of up to 4 years with cycles of cyclosporine A, which was withdrawn because of its transient and mild efficacy. In 2015, biologic therapy with an anti-TNF-α agent, adalimumab, was started. At baseline, the patient had a Psoriasis Area and Severity Index (PASI) score of 21, involvement of 30% of body surface area (BSA), and a Dermatology Life Quality Index (DLQI) of 7. After 12 weeks, PASI 1, BSA 3%, and DLQI 0 were recorded, and this excellent result was maintained for about 3 years. However, at follow-up visits in November 2018, a loss of efficacy of adalimumab therapy was recorded (loss of 50% of clinical improvement, with PASI 12, BSA 25%, and DLQI 6). Moreover, the patient reported whitening of his scalp and facial hair, including the beard, sideburns, and eyebrows, which were black before initiating adalimumab (Fig 1, A). Surprisingly, cutaneous manifestations of vitiligo were not recorded. Wood lamp examination of vitiligo-affected areas showed depigmented hair with bright white fluorescence, confirming the diagnosis. Laboratory tests performed to check for other autoimmune conditions revealed high levels of circulating thyroid autoantibodies (anti-thyroglobulin and anti-thyroid peroxidase) that were not present before the failure of adalimumab therapy. The biologic therapy was suspended, and topical therapy with corticosteroids and vitamin D was initiated. However, in January 2019, while the whitening persisted, the patient presented with total remission of autoimmune thyroiditis but with worsening of psoriasis and psoriatic arthritis (PASI 16.5, BSA 35%, and DLQI 12, with flare of joint pain). Treatment with ixekizumab, an anti-interleukin (IL) 17A agent, was started. The patient rapidly improved, with PASI 90 after 1 month and PASI 100 after 3 months. Good control of the psoriatic disease has been maintained to date after nearly 2 years of treatment. Repigmentation of the vitiligo-affected areas was observed after 3 months of treatment with ixekizumab, with further improvement at 9 and 18 months (Fig 1, B).
Fig 1.
Representative photographs of the psoriatic patient with vitiligo occurring during anti-tumor necrosis factor α treatment and improving after anti-interleukin-17A treatment. A, Vitiligo manifestations involving hair occurring in the psoriatic patient during therapy with adalimumab. B, Subtotal remission of vitiligo manifestations involving hair after 18 months of ixekizuamb treatment.
Discussion
Several theories have been proposed to explain the mechanism of the development of autoimmunity during treatment with anti-TNF-α agents. For example, autoantigens released during apoptosis, such as nucleosome, which are increased in patients receiving anti-TNF-α therapy, are considered responsible for the induction of autoantibodies.5 Moreover, cytotoxic T cells are thought to play an important role in the suppression of autoreactive B cells. In the presence of TNF blockade, this suppression is diminished, potentially allowing latent autoreactivity to be unmasked.5 In addition, there is evidence to suggest that an increased susceptibility to infection associated with anti-TNF drugs could result in expansion of polyclonal B cells and production of autoantibodies.5 Previous reports suggest that anti-TNF-α agents, including adalimumab, can induce the development of vitiligo; in 2 cases, vitiligo developed in a patient receiving adalimumab therapy for Crohn's disease.6,7 In another case, there was a rapid worsening of vitiligo (within 3 months) in a patient receiving adalimumab for ankylosing spondylitis.5 Recently, a case was reported of a 63-year-old man who developed vitiligo during treatment with adalimumab for plaque psoriasis, with subsequent gradual resolution of both skin conditions after switching to secukinumab.8 Curiously, in our patient, vitiligo affected only the scalp hair and facial hair, including the beard, sideburns, and eyebrows. Moreover, unlike the recent case, vitiligo manifestations resolved after ixekizumab therapy. In the present patient, ixekizumab resolved both the clinical manifestation of psoriasis after the failure of adalimumab and presumably the treatment-related vitiligo. In this regard, it is interesting to note that ixekizumab targets IL-17A, a mediator implicated in the pathogenesis of several inflammatory disorders, including psoriasis and vitiligo. Elevated levels of IL-17 have been found in the sera of patients with vitiligo, and the expression of IL-17A messenger RNA is also increased in vitiligo lesions.9 A synergistic effect of IL-17 and TNF-α on melanocytes has been described, inhibiting both pigmentation-related signaling and melanin production.
Repigmentation of hair is a rare event that has been reported after inflammatory processes. Rongioletti et al9 reported the case of a patient with psoriasis who experienced darkening and noticeable increase of scalp hair during therapy with secukinumab. The authors considered the patient's hair darkening as the result of a change in immune control over the hair cycle, removing the inhibitory influences of IL-17 after secukinumab administration.9 A variety of inflammatory mediators can promote or inhibit melanogenesis through different mechanisms, suggesting new targets for the development of novel therapies for the treatment of pigmented dermatoses, such as vitiligo. However, it is important to keep in mind that the regulatory network of inflammation is very complex, since many types of inflammatory cells and associated mediators are involved. The imbalance of inflammatory factors related to T-cell subsets plays an important role in the development of various skin diseases, as well as in paradoxical reactions during biologic therapy that targets a specific pathway, breaking delicate balances. The relationship between this imbalance or changes of T-cell subsets and melanogenesis, as well as the relationship between target therapies and vitiligo, has yet to be confirmed.
Conflicts of interest
None disclosed.
Footnotes
Funding sources: None.
IRB approval status: Not applicable.
References
- 1.Jung J.M., Lee Y.J., Won C.H. Development of vitiligo during treatment with adalimumab: a plausible or paradoxical response? Ann Dermatol. 2015;27(5):620–621. doi: 10.5021/ad.2015.27.5.620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Simón J.A., Burgos-Vargas R. Vitiligo improvement in a patient with ankylosing spondylitis treated with infliximab. Dermatology. 2008;216:234–235. doi: 10.1159/000112932. [DOI] [PubMed] [Google Scholar]
- 3.Martínez-Esparza M., Jiménez-Cervantes C., Solano F., Lozano J.A., García-Borrón J.C. Mechanisms of melanogenesis inhibition by tumor necrosis factor-alpha in B16/F10 mouse melanoma cells. Eur J Biochem. 1998;255(1):139–146. doi: 10.1046/j.1432-1327.1998.2550139.x. [DOI] [PubMed] [Google Scholar]
- 4.Exarchou S.A., Voulgari P.V., Markatseli T.E., Zioga A., Drosos A.A. Immune-mediated skin lesions in patients treated with anti-tumour necrosis factor alpha inhibitors. Scand J Rheumatol. 2009;38(5):328–331. doi: 10.1080/03009740902922612. [DOI] [PubMed] [Google Scholar]
- 5.Maruthappu T., Leandro M., Morris S.D. Deterioration of vitiligo and new onset of halo naevi observed in two patients receiving adalimumab. Dermatol Ther. 2013;26(4):370–372. doi: 10.1111/dth.12002. [DOI] [PubMed] [Google Scholar]
- 6.Posada C., Flórez A., Batalla A., Alcázar J.J., Carpio D. Vitiligo during treatment of Crohn's disease with adalimumab: adverse effect or co-occurrence? Case Rep Dermatol. 2011;3(1):28–31. doi: 10.1159/000324619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Palazzo G. Resolution of post-adalimumab vitiligo with secukinumab in a patient with psoriasis vulgaris. Oxf Med Case Reports. 2020;2020(1):omz134. doi: 10.1093/omcr/omz134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bassiouny D.A., Shaker O. Role of interleukin-17 in the pathogenesis of vitiligo. Clin Exp Dermatol. 2011;36(3):292–297. doi: 10.1111/j.1365-2230.2010.03972.x. [DOI] [PubMed] [Google Scholar]
- 9.Rongioletti F., Mugheddu C., Murgia S. Repigmentation and new growth of hairs after anti-interleukin-17 therapy with secukinumab for psoriasis. JAAD Case Rep. 2018;4(5):486–488. doi: 10.1016/j.jdcr.2018.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]