Abstract
Objective
Parenting during pandemic restrictions places extreme demands on everyday family life, leading to increased stress levels for parents and distressed parent-child interactions. This RCT aimed to investigate whether cognitive reappraisal and self-compassion are helpful emotion regulation (ER) strategies to reduce individual and parental stress during the COVID-19 pandemic.
Method
An online intervention for parents was developed focusing on the application of ER strategies to pandemic requirements of families. A sample of 265 parents were randomly assigned to either cognitive reappraisal (CR; n = 88), self-compassion (SC; n = 90) or wait-list control (WLC; n = 87) group. Interventions included two video sessions (day 1 and day 3) and three email reminders to transfer the application of ER strategies to daily family life (days 2, 4, 5). Parents' perceived individual stress and parental stress were assessed at baseline (T0), at T1 prior to the booster session on day 3, and at T2 (7 days after baseline).
Results
Significant decreases from T0 to T2 emerged for both primary stress outcomes in both intervention groups. Individual stress significantly decreased in CR compared to WLC at T2, but not compared to SC. No time × group interactions for parental stress were found. However, mediation analyses suggested that parental stress was indirectly decreased via reductions in individual stress for CR compared to WLC at both time points.
Conclusions
COVID-19 will not be the last pandemic to affect family life. Cognitive reappraisal as a brief online intervention can ease acute stress and strengthen the mental health of parents in acute crises.
Keywords: Pandemic, Lockdown, Parenting, Emotion regulation, Stress reduction
Highlights
-
•
Online interventions for parents are feasible during pandemic restrictions.
-
•
A very brief two-session online intervention reduced acute individual stress of parents.
-
•
Cognitive reappraisal was more effective than self-compassion when compared to wait-list control.
-
•
Parental stress was indirectly decreased via reductions in individual stress.
1. Introduction
Parenting during the COVID-19 pandemic restrictions in the first half of 2020 was characterized by managing work-family life without regular childcare, leisure activities, or social peer contacts for children. Working parents suddenly had to act as teachers for their children during home schooling without prior experiences. #Stayathome was the global family condition for over 14 weeks after the WHO declared COVID-19 as a pandemic on 11th March 2020, and strict public protective measures were introduced in many countries (Ghebreyesus, 2020). Most families were affected by some form of lockdown and associated measures, from severe restrictions on meeting other people and travel, to quarantine measures in isolation. This drastic public health measure to reduce the reproduction rate of the coronavirus placed high demands on parents in everyday family life, with manifold psychological impacts. A global survey including data from 27 countries between 30th March and 6th April 2020 revealed that alongside being single and of younger age, being in quarantine with more than one child was especially associated with enhanced levels of stress (Kowal et al., 2020). Likewise, during this time period, an increase in depressive and anxiety symptoms was observed in adults living in Austria and Germany, indicating the strong impact of the COVID-19 pandemic on mental health in these countries (Bäuerle et al., 2020; Petzold et al., 2020; Pieh et al., 2020), comparable to similar findings from other countries (Xiong et al., 2020).
According to Lazarus' transactional model of stress and coping (Lazarus and Folkman, 1984), stress is perceived if individuals consider their current demands (stressors) as threatening, uncontrollable and stable (primary appraisal), while available coping strategies are considered as insufficient (secondary appraisal). Indeed, the pandemic restrictions were uncontrollable and threatened various basic needs (e.g., separation of loved ones, loss of self-determination, see review by Brooks et al., 2020). In particular, managing home schooling and childcare while working from home, disrupted routines, limited access to food and health care services, and financial worries were stated as primary parental stressors (Brown et al., 2020; Canady, 2020). Moreover, against the background of the uncertainty of the course of the virus, parents were unable to estimate how long the sudden changes would restrict their family life. Preliminary data collected between 2nd and 7th April in Italy, one of the countries with the highest number of COVID-19 cases outside of China in early 2020, confirmed that parents who considered dealing with pandemic restrictions as difficult perceived more subjective stress (Spinelli et al., 2020).
Given that it is quite realistic and appropriate to regard the pandemic situation as challenging for the parental role, the need for effective coping strategies became even more important. The current generation of parents with children of preschool or school age had to adapt to a global health crisis by adaptive parental behavior for the first time. If parents were able to adjust successfully, the effects of family quarantine might have been negligible or even positive. Indeed, some parents reported that more family time led to closer bonds, more warmth, a slowing down of daily life, and even reduced stress (Brown et al., 2020). On average, however, parents reported significantly higher subjective stress during the COVID-19 pandemic compared to adults without children (Canady, 2020). Moreover, negative affective states, poor sleep, and high anxiety and depression levels were experienced by most parents in the western United States (Brown et al., 2020).
With respect to parenting stress, preliminary data also revealed significant associations between the difficulties experienced during quarantine and psychological reactions that parents may show when engaging in their parenting role (Deater-Deckard, 1998; Spinelli et al., 2020). Abidin, 1976, Abidin, 1992 initially defined specific factors for the development of parental stress, which is conceptually distinct from parents' individual stress, including parental distress, child temperament/mental status and dysfunctional parent-child interactions as key components. In their empirical model, Ostberg and Hagekull (2000) emphasized the moderating influence of the relevance of stressors for the parental role, e.g. an inner working model of a ‘perfect’ parent even during the pandemic, who at the same time quickly feels unappreciated or abandoned by others. Accordingly, these parents might face greater challenges to their functioning as “good parents” and might have more difficulties to cope with pandemic restrictions. Hence, parental stress occurs when current demands exceed coping resources (Lazarus and Folkman, 1984), combined with an increasing loss of confidence in one's parental role (Ostberg and Hagekull, 2000) and additional stressors during the pandemic restrictions such as high workload, e.g. as essential healthcare workers, and childcare hassles.. Moreover, role reversals within the households, e.g. if one working parent, traditionally the mother, is predominantly responsible for home schooling and childcare, could have provoked additional strain on the parental dynamic.
Bidirectional relations between individual and parental stress can further mutually reinforce each other's effects (Holly et al., 2019). This might be reflected in initial findings suggesting that parents who experienced higher stress were at higher risk to abuse their children during COVID-19 lockdown in the western United States (Brown et al., 2020). Spinelli et al. (2020) showed that children's behavioral and emotional problems during quarantine were mediated by parents' individual and parental stress, with the latter having a stronger effect. Moreover, higher depression levels in parents during the pandemic, further intensified by a pre-existing history of mental illness (Brown et al., 2020; Wu et al., 2020), might additionally increase parent-child dyadic stress levels. It can be expected that highly stressed parents have more difficulties in responding sensitively to the needs and fears of their quarantined children. As a consequence, the children may feel misunderstood and behave more aggressively in parent-child interactions, which can ultimately increase the risk of developing emotional or behavioral problems in the long term (Spinelli et al., 2020). Early work conducted during April/May 2020 found that especially parents' perceived negative impact of COVID-19 and current subjective distress were associated with increases in externalizing and internalizing problems of their children (Whittle et al., 2020). Conversely, greater psychological distress, e.g. more worries, helplessness, and fear, in quarantined children (Saurabh and Ranjan, 2020), can aggravate parents' individual as well as parental stress. In sum, dysfunctional parent-child interactions might lead to increased stress levels of all family members in a subgroup of highly stressed parents during the lockdown. Given the toxic interplay between subjective and parental stress, there is consensus on the need for family-based interventions that promote positive parent-child interactions during the pandemic (Coyne et al., 2020; Fegert et al., 2020; Prime et al., 2020; Szabo et al., 2020).
One way to reduce parents' stress levels and thereby relieve family systems could be the enhancement of parents' adaptive coping strategies for the pandemic-specific challenges in everyday family life. Emotion regulation (ER) belongs to the coping strategies within a transdiagnostic approach aiming to foster positive affective states and regulate negative affective states (Gross, 2002, Gross, 2015). One of the most widely studied ER strategies, based on Gross' process model of emotion regulation (Gross, 2002, Gross, 2015), is cognitive reappraisal (CR), an antecedent-focused strategy that promotes cognitive change before emotional response tendencies become fully activated. Moreover, CR is a core component of cognitive behavioral therapy (CBT), which has proven efficacy in treating general stress and depression (Hofmann et al., 2012). Another currently much discussed ER strategy is self-compassion (SC), which might focus more on response modulation once emotional response tendencies have already been elicited (Gross, 2002, Gross, 2015). SC is often integrated in ‘third-wave’ CBT, and fosters a relationship of care and concern to oneself when faced with distress and negative affective states (Gilbert, 2009; Neff, 2003). According to Neff's original framework (2003), SC includes three positive components versus three negative components: mindfulness versus overidentification with distress, common humanity versus social isolation, and self-kindness versus harsh self-criticism. Recently, Neff et al. (2018) emphasized the balance of increased compassionate and reduced uncompassionate self-responding in times of suffering in order to SC as a holistic construct. Contrasting these two ER strategies, SC focuses on a mindfulness-based perception of negative affective states and coping with stress in a self-compassionate way, while CR aims at identifying and modifying dysfunctional thinking patterns by verifying the accuracy and functioning of thoughts that lead to emotional stress (Beck, 1979; Campbell-Sills and Barlow, 2007). However, recent studies challenge the distinction between CR and SC as distinct entities and point to relevant interrelations. Inwood and Ferrari (2018) demonstrated in their review that SC may attenuate stress and depressive symptoms by facilitating ER, for example through an improved tolerance of negative emotions (Diedrich et al., 2017). Bates et al. (2020) found in particular that the influence of compassionate self-responding to social anxiety symptoms in a student sample was mediated by CR. Accordingly, SC might encompass a more holistic emotional attitude toward disliked aspects of the self, including cognitive, affective and attentional components that might relate to all stages of Gross' emotion regulation cycle.
Recently, findings suggest that SC could be equally effective as or even superior to CR, especially for participants with major depressive disorder (Diedrich et al., 2014), but also for formerly and never depressed participants experiencing experimentally induced depressed mood (Ehret et al., 2018). Furthermore, the efficacy of reappraisal techniques in reducing depressed mood might be increased when utilizing SC as a preparatory strategy (Diedrich et al., 2016). Moreover, meta-analytic findings confirmed that SC-related therapies reduced depressive and anxiety symptoms in subclinical and clinical samples, with medium effect sizes (Wilson et al., 2019).
Considering that CR or SC are effective coping strategies which may enable a dynamic adjustment to the pandemic restrictions despite the continued uncontrollable and uncertain perspective of the pandemic (Coyne et al., 2020), both ER strategies might have a positive effect on secondary appraisal based on Lazarus' stress model (Lazarus and Folkman, 1984). Consistent with this expectation, Brown et al. (2020) showed that perceived control in dealing with pandemic restrictions buffered perceived stress and child abuse potential. Moreover, in a global pandemic that affects almost everybody in one way or another, the “common humanity” component of SC might be especially useful to mitigate negative emotional responses to solidarity-based restrictions for the benefit of risk groups. Similarly, Brooks et al. (2020) propose strengthening a sense of altruism in order to facilitate coping with quarantine situations. CR, in turn, focuses on verifying the accuracy of thoughts related to potential personal impacts induced by the pandemic restrictions. Thus, given previous research demonstrating the efficacy of both strategies in the treatment of depression and anxiety symptoms, we expect both to be effective in reducing individual stress of parents as well as their parental stress during the global pandemic, with a greater effect for SC.
Online interventions enable easily accessible, safe and cost-effective support compared to face-to-face interventions, which are less available during a pandemic with social distancing measures. Previous studies found that web-based self-guided interventions were helpful in managing perceived stress in non-clinical samples (Querstret et al., 2018) and adjustment problems (Moser et al., 2019) in the short term. Guided online self-help and face-to-face treatments achieved comparable effects in treating depression and anxiety disorders (d = −0.02, in favor of guided self-help; Cuijpers et al., 2009). Two recently evaluated online parenting interventions for parental depressive and stress symptoms using SC-related components demonstrated the feasibility of online interventions for highly stressed parents (Potharst et al., 2019; Riegler et al., 2020).
1.1. The current study
Given that online interventions may be a promising avenue for removing barriers to short-term support, we developed two very brief online interventions strengthening either CR or SC, adapted to the specific conditions of parents during the restrictions following the COVID-19 pandemic. In the present RCT, we investigated whether CR and SC mitigated parents' perceived individual and parental stress compared to a wait-list control (WLC) group over the course of eight days. We hypothesized that SC would lead to a stronger reduction of individual and parental stress at posttest II (T2, day 8 after baseline) compared to CR and WLC. We further expected CR to lead to a stronger reduction of individual and parental stress compared to WLC at T2.
2. Material and methods
2.1. Participants
Participants were recruited through announcements on social media channels addressing the impact of pandemic management on parenthood (e.g., #ParentsInCrisis and #PandemicParenting). The study was advertised as aiming to reduce stress in highly strained parents during the global pandemic. Inclusion criteria were (1) age 18 years or older, (2) taking care of at least one child aged 3 to 18 years who had attended a kindergarten or school prior to the pandemic outbreak, (3) having a device with an internet connection and speakers or headphones, and (4) German-language fluency. No exclusion criteria were defined.
2.2. Study procedure and randomization
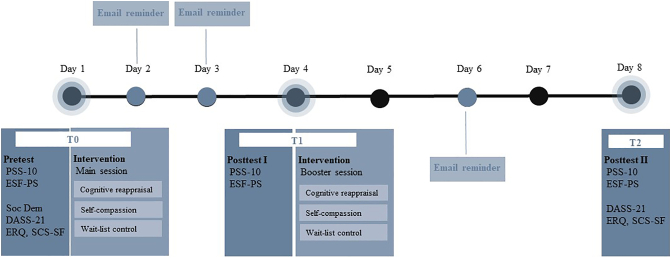
After providing informed consent, participants were randomly assigned to one of three conditions using a block-wise randomization procedure (block sizes of three or six): CR, SC or WLC (see Fig. 1 for study flow). The randomization allocation list was implemented in REDCap (Harris et al., 2019) by the first author and concealed to the second author who enrolled participants. The complete study was conducted within REDCap. Due to the nature and contents of the intervention, participants were not blinded. Participants received two online video interventions (main session on day 0 and booster session on day 3) in the treatment groups via smartphone, tablets or computers. The online videos (day 0: 20 mins, day 3: 10 mins) explained in depth how to practice either CR or SC as a parent affected by the pandemic restrictions. Furthermore, participants in the treatment groups received email reminders on days 1, 2, and 4, with helpful tips on how to implement either CR or SC in their daily family routine. Participants completed questionnaires at baseline prior to the main session (T0), at T1 prior to the booster session (3 days after baseline, posttest I), and at T2 (7 days after baseline, posttest II). Parents with more than one child were asked to answer with regard to an index child with whom they experienced the most stressful family situations during the pandemic restrictions. Data collection began on 27th April 2020 and closed on 15th June 2020 due to the stepwise reopening of schools and kindergartens for all children in Germany and Austria (see online supplement Fig. S1 for a timeline of restrictions affecting parents in Germany and Austria). The research project was approved by the Ethical Review Committee of the local medical association (Landesaerztekammer RLP, No. 2020-14980) and was preregistered at OSF (https://osf.io/bf4e6).
Fig. 1.
Study course of treatment and assessments.
2.3. Interventions
The two interventions were comparable regarding time flow and psychotherapeutic process (i.e., from depathologization and knowledge transfer to concrete therapeutic guidance). The early phase of the main session (first video) covered psychoeducation about possible psychological consequences of pandemic restrictions and benefits of ER strategies. The different components of CR or SC based on Beck's (1979) or Neff's (2003) framework were introduced using a typical stressful family situation caused by social distancing, in which a dysfunctional thought, e.g. “My child won't forgive me if I stop him/her from meeting up with friends”, and resulting negative affective states might arise. In the second phase, emotional activation was induced in both treatment groups by presenting pictures depicting potential restrictions on family life during the global pandemic (e.g. closed playgrounds). Next, eight possible automatic negative thoughts reported by patients of our affiliated outpatient clinic were presented, e.g. “I am not able to support my child sufficiently while home schooling” or “I don't know how I can manage to balance my work and childcare”. The participants were asked to select one personally relevant thought and adapt it to their own family situation during the pandemic. In the third phase, the participants were instructed to empathize with the physical and emotional experiences while imagining the specific family situation triggered by the selected negative thought. Next, they were guided to practice either CR or SC while addressing themselves in the first person.
The aim of the CR intervention was to identify and modify cognitive distortion via three different restructuring techniques by Beck (1979) adapted to the specific conditions of parents during pandemic restrictions. First, participants were asked to seek evidence and counterevidence for the selected thought during and before the pandemic. Next, they were instructed to check the short- and long-term functions of this thought to manage the current restrictions. Finally, they were guided to take a more realistic perspective by generating an alternative, more adaptive interpretation (e.g. “My child is allowed to be angry when I restrict him/her during the pandemic, but this does not change our relationship”).
The SC intervention was based on the self-compassion break by Neff and Germer (2018), practicing mindfulness, common humanity, and self-kindness adapted to the specific conditions of parents during pandemic restrictions. Therefore, common humanity was modified into a concept of common parenthood. First, participants were supported to practice mindfulness by naming their burdening emotions and acknowledging their suffering and distress during the pandemic-related family situation triggered by the selected thought. They were then guided to internalize this stressful family moment as a shared human experience of suffering during the pandemic, in order to establish a felt connection with other parents. Finally, participants were instructed to practice self-kindness by expressing a kind, warm and soothing self-talk while strengthening their self-esteem in the parental role during pandemic restrictions (e.g. “I wish to be kind to myself because this situation is difficult right now and compassion is the only thing that makes sense now. I am a good mother or father, even though I restrict my child during the pandemic”).
For the booster session (second video on day 3), participants in the intervention groups were guided to apply either the CR or the SC strategy to a freely chosen personal situation of mild to moderate stress intensity within their daily family life during the pandemic restrictions. Moreover, the three email reminders aimed to support the daily practice of the ER strategies during the course of the study, incorporating examples of the application of the different components of CR and SC to daily family life.
2.4. Measures
Intervention check. To investigate the comparability of CR and SC, intervention group participants were asked to rate their effort to apply the intervention (operationalized as one item asking “How hard did you try to apply the ER strategy?”), their success in applying the intervention (“How well did you manage to apply the ER strategy?”), and how demanding they found the intervention (“How demanding did you find the ER strategy to be?”) on a visual analogue scale (VAS) ranging from 0 (not at all) to 100 (very much). All three items were presented after each of the two video sessions.
Individual stress. Perceived individual stress was assessed with the German short form (PSS-10; Schneider et al., 2020) of the Perceived Stress Scale (PSS; Cohen et al., 1983), a widely used economic 10-item questionnaire asking about stress symptoms in the last month. All items began with “In the last month, how often have you… (e.g. found that you could not cope with all the things that you had to do?)” and were rated on a 5-point Likert scale from 1 (never) to 5 (very often). For each time point, an adapted introduction was used, which asked about perceived stress since the beginning of the pandemic restrictions or since the last measurement. Recent research on construct validity of the scale confirmed a two-factor model (perceived helplessness [PH], perceived self-efficacy [PSE]) alongside a unidimensional model by reversing the PSE items and summing up all items to a global score (Cohen et al., 1983; Reis et al., 2019; Schneider et al., 2020). For the global score, robust positive associations with depressive symptoms, anxiety, insomnia severity and fatigue, as well as negative associations with life satisfaction have been demonstrated (Klein et al., 2016; Reis et al., 2019). The internal consistency of the global score in the present study was good, with Cronbach's α = 0.89.
Parental stress. Perceived parental stress was measured using the parental stress subscale of the Parental Stress Questionnaire (PSQ; Domsch and Lohaus, 2010), a reliable 38-item instrument to assess four facets of stress in parenting. The subscale Parental Stress (PSQ-PS) measures parents' perceived parenting competence (e.g. “There are always days when I feel insecure about raising my child”), stress in interaction with the child (e.g. “I often have conflicts with my child”), and everyday problems caused by parenthood (e.g. “I have to help my child with everyday things (like dressing, brushing teeth, cleaning rooms) more than I would like”). All 17 items of the subscale are rated on a 4-point Likert scale ranging from 0 (does not apply) to 3 (applies completely). A version for preschool children and a version for school children exist. The latter version is only standardized for grades 1–6, but was also used for older school children in our study due to a lack of alternative instruments. Cronbach's α in the present study ranged from α = 0.90 (school version) to α = 0.93 (preschool version), indicating high internal consistencies. The test-retest reliabilities were similarly high in the original study, ranging from 0.89 (preschool version) to 0.91 (school version, grades 5–6) after a six-week interval (Domsch and Lohaus, 2010). Both primary outcome variables were assessed at T0 (baseline), T1 (day 3) and T2 (day 7).
Negative affective symptoms. As secondary outcomes, depressive, anxiety and stress-related symptoms at T0 were measured with the 21-item Depression Anxiety Stress Scales (DASS-21, Antony et al., 1998), the short form of the original DASS with 42 items (Lovibond and Lovibond, 1995). Each scale consists of seven items, asking about symptoms over the past week on a rating scale from 0 (did not apply to me at all) to 3 (applied to me very much, or most of the time). All three subscales were shown to be highly correlated with other depression and anxiety self-report scales, demonstrating convergent validity (Nilges and Essau, 2015). In the present study, the subscales showed good to high internal consistencies, with α = 0.84 (anxiety scale) to α = 0.90 (stress scale).
Moderator variables. To assess potential moderators of the application of the ER strategies in our study, we applied two questionnaires measuring trait CR and SC at baseline. Baseline trait CR was assessed with the CR subscale of the German version of the Emotion Regulation Questionnaire (ERQ, Abler and Kessler, 2009; Gross and John, 2003) using six items rated on a Likert scale from 1 (not true at all) to 7 (completely true). In community-based samples, CR scores were found to be significantly negatively correlated with alexithymia and psychological distress (Preece et al., 2020). The internal consistency in the current study was moderate (Cronbach's α = 0.85). Baseline trait SC was measured with the Self-Compassion Scale-Short Form (SCS-SF, Raes et al., 2011) of the SCS (Neff, 2003), comprising 12 items rated on a Likert scale from 1 (very rarely) to 5 (very often). For the German version, good internal consistency of Cronbach's α = 0.84 (in the current study α = 0.86) and a test-retest reliability of rtt = 0.83 were reported (Hupfeld and Ruffieux, 2011). Moreover, the global scores of the short and long form were highly correlated (r = 0.91; Hupfeld and Ruffieux, 2011). The ERQ and SCS-SF were applied at T0 and T2.
2.5. Data analysis
A conservative sample size calculation with G*Power 3.0 resulted in a total sample size of 93 participants to detect a between-within interaction (time × group) of an effect size of f = 0.15 with a power of 80% and an alpha level of 0.05. To compensate for dropouts, an oversampling of at least 30% was aimed for. Analyses were conducted and figures were produced using RStudio (RStudio Team, 2020). Participant characteristics for the total sample and by group were examined using F- or G-tests. Group differences between CR, SC, and WLC with respect to primary outcomes were analyzed by conducting linear mixed models (LMM) with fixed factors (within-subject factor time and between-subject factor group) and random intercept with the nlme package (Pinheiro et al., 2020). This can be regarded as a generalization of a repeated measures ANOVA which permits the inclusion of participants with missing values at T1 and T2 without imputations. Tukey's correction was used for post-hoc tests, and Cohen's d was reported in the case of significance. Primary analyses were intention-to-treat (ITT) analyses of all participants who were randomized and completed T0 measurements. Completer analyses were conducted for the purpose of comparison (per protocol, PP). All participants who completed the primary outcomes at all time points and watched both videos in their entirety were defined as completers. Video watching was checked by comparing time stamps before and after the video interventions (min. 18 min for the main session and 8 mins for the booster session). Robustness checks were conducted by post-hoc adjusting all models for age of the index child (continuous) and baseline ER traits (ERQ reappraisal, SCS-SF) and by comparing effect estimates and model fit indices. Secondary outcomes were analyzed similarly to primary outcomes on an exploratory basis. As exploratory analyses, cross-sectional mediation analyses were performed for completers with PROCESS for SPSS (Hayes, 2013) in order to analyze whether the relationship between group and parental stress was mediated by individual stress at both time points. Group was used as a multi-categorical predictor of PSS-10 (mediating variable), and group and PSS-10 as predictors of PSQ-PS. In line with Preacher and Hayes (2004), indirect effects were evaluated with 95% bias-corrected confidence intervals based on 10,000 bootstrap samples. If the confidence interval did not contain zero, the indirect effect was considered statistically significant. For the exploratory analyses, no correction for multiple testing was applied. Statistical significance was set at the 5% level for all analyses (two-tailed).
3. Results
3.1. Enrollment and participant characteristics
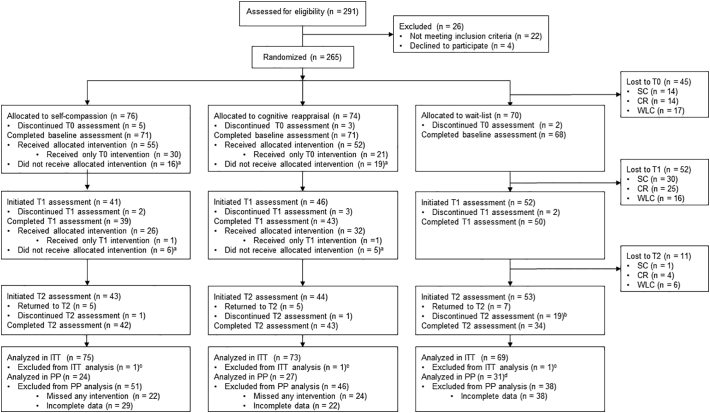
Of a total of 291 participants assessed for eligibility, 265 were enrolled and randomized to SC (n = 90), CR (n = 88) or WLC (n = 87). Fig. 2 depicts the participant flow through the study. Forty-eight participants were excluded from the ITT analyses because they were lost to T0 or did not complete the entire PSS-10. Table 1 summarizes the participant characteristics at baseline. The total ITT sample consisted of N = 217 (N = 211 for PSQ-PS) participants aged from 18 to 56 years (M = 40.63, SD = 6.21); 92.6% were female and 62.7% had a Master's university degree or higher. Participants in the CR (n = 73), SC (n = 75), and WLC (n = 69) groups did not differ significantly with respect to age, gender, education level, income, marital status, and parent-related variables (i.e., parental status, number of children). Participants had an average of two children, and most participants lived together with the other parent (82.5%). Since the restrictions began, most had been working regularly, either in an office (30.9%) or from home (44.2%, M = 24.01 h/week, SD = 11.00). The index children were predominantly of primary school age and male (56.2%). Regarding baseline distress measured with the DASS-21, participants reported mild stress (M = 9.47, SD = 4.98), mild depression (M = 5.18, SD = 4.30), and normal anxiety levels (M = 2.76, SD = 3.30, see Table 1).
Fig. 2.
CONSORT study flow diagram.
Note: aParticipants were counted as “did not receive allocated intervention” if the intervention video was not started or was terminated in less than 18 mins (8 mins for booster intervention). bDue to a technical error, wait-list control participants were unable to complete the T2 assessment in some cases. cOne participant per condition did not complete the main outcome questionnaire and was thus excluded from the ITT analysis. dDue to a technical error during T2 of the WLC, sample size for the PP analysis differs between individual and parental stress analyses.
Table 1.
Baseline demographic and clinical characteristics of the intention to treat (ITT) sample.
| Total |
Cognitive reappraisal |
Self-compassion |
Wait-list control |
Test statistics |
||
|---|---|---|---|---|---|---|
| (N = 217) | (CR, n = 73) | (SC, n = 75) | (WLC, n = 69) | G/F | p | |
| Age (yrs) | 40.63 (6.21) | 41.15 (5.81) | 41.09 (5.98) | 39.58 (6.80) | 1.46 (2, 214) | .235 |
| Sex (female) | 201 (92.63) | 65 (89.04) | 69 (92.00) | 67 (97.10) | 3.84 (2) | .147 |
| Highest educational level | ||||||
| Middle school or lower | 43 (19.82) | 11 (15.07) | 21 (28.00) | 11 (15.94) | 15.39 (12) | .221 |
| High school degree | 25 (11.52) | 8 (10.96) | 11 (14.67) | 6 (8.70) | ||
| College degree | 13 (5.99) | 7 (9.59) | 2 (2.67) | 4 (5.80) | ||
| University degree | 100 (46.08) | 33 (45.21) | 30 (40.00) | 37 (53.62) | ||
| Doctorate | 28(12.90) | 9 (12.33) | 10 (13.33) | 9 (13.04) | ||
| Other | 8 (3.69) | 5 (6.85) | 1 (1.33) | 2 (2.90) | ||
| Income per month | ||||||
| <1700€ | 21 (9.68) | 6 (8.22) | 6 (8.00) | 9 (13.04) | 4.75 (10) | .908 |
| 1700€–2600€ | 34 (15.67) | 11 (15.07) | 12 (16.00) | 11 (15.94) | ||
| 2600€–3600€ | 57 (26.27) | 20 (27.40) | 22 (29.33) | 15 (21.76) | ||
| >3600€ | 105 (48.39) | 36 (49.32) | 35 (46.67) | 34 (49.28) | ||
| Marital status | ||||||
| Married | 156 (71.89) | 56 (76.71) | 49 (65.33) | 51 (73.91) | 7.03 (8) | .534 |
| Separated/divorced | 16 (7.37) | 6 (8.22) | 5 (6.67) | 5 (7.25) | ||
| Single | 11 (5.07) | 2 (2.74) | 5 (6.67) | 4 (5.80) | ||
| In a partnership | 34 (15.67) | 9 (12.33) | 16 (21.33) | 9 (13.04) | ||
| Parental status | ||||||
| Single Parent | 17 (7.83) | 5 (6.85) | 5 (6.67) | 7 (10.14) | 6.94 (6) | .326 |
| Living together | 179 (82.49) | 62 (84.93) | 61 (81.33) | 56 (81.16) | ||
| Living separately | 19 (8.76) | 4 (5.48) | 9 (12.00) | 6 (8.70) | ||
| Other | 2 (0.92) | 2 (2.74) | 0 (0) | 0 (0) | ||
| Number of children | 2.09 (0.94) | 2.05 (1.01) | 2.05 (0.82) | 2 (0.97) | 0.93 (2, 214) | .396 |
| Index child | ||||||
| Age (yrs.) | 7.84 (3.78) | 7.40 (3.37) | 8.43 (3.88) | 7.65 (4.01) | 1.42 (2, 204) | .244 |
| Sex (male) | 122 (56.22) | 42 (57.53) | 42 (56.00) | 38 (55.07) | 0.66 (2, 204) | .717 |
| Essential workers | 80 (36.87) | 29 (39.73) | 25 (33.33) | 26 (37.68) | 1.22 (2, 204) | .543 |
| Working situation since restrictions began | ||||||
| Regularly attending office | 67 (30.88) | 24 (32.88) | 24 (32.00) | 19 (27.54) | 5.02 (6) | .542 |
| Short-time work | 12 (5.53) | 4 (5.48) | 5 (6.67) | 3 (4.35) | ||
| Work from home | 96 (44.24) | 30 (41.10) | 30 (40.00) | 36 (52.17) | ||
| Not working | 12 (5.53) | 3 (4.11) | 7 (9.33) | 2 (2.90) | ||
| Working from home (h/week) | 14.45 (12.76) | 15.02 (13.41) | 13.96 (13.65) | 14.43 (11.13) | 0.11 (2, 182) | .899 |
| DASS-21 | ||||||
| Stress | 9.47 (4.98) | 9.65 (4.73) | 9.36 (4.80) | 9.51 (5.49) | 0.11 (2, 210) | .892 |
| Depression | 5.18 (4.30) | 4.29 (3.70) | 4.51 (4.04) | 6.22 (4.70) | 3.12 (2, 210) | .046* |
| Anxiety | 2.76 (3.30) | 2.68 (3.16) | 2.68 (3.44) | 2.93 (3.34) | 0.13 (2, 210) | .883 |
| ERQ | ||||||
| Suppression | 3.10 (1.32) | 2.87 (1.24) | 3.04 (1.23) | 3.40 (1.43) | 2.96 (2, 207) | .054 |
| Reappraisal | 4.44 (1.12) | 4.37 (1.05) | 4.47 (0.96) | 4.50 (1.32) | 0.26 (2, 207) | .768 |
| SCS-SF | ||||||
| Global score | 3.11 (0.70) | 3.08 (0.74) | 3.13 (0.63) | 3.11 (0.74) | 0.11 (2, 208) | .892 |
Note. Data presented as means (SD) or numbers (%). DASS-21 = Depression Anxiety Stress Scales, ERQ = Emotion Regulation Questionnaire, SCS = Self-Compassion Scale-Short Form. As all participants were Caucasian, ethnicity was not separately reported. G-tests were conducted for categorical variables and ANOVAs for continuous variables. Group differences were analyzed with Tukey post hoc tests at *p ≤ .05, **p ≤ .01.
3.2. Attrition, treatment adherence, and intervention check
Overall, the attrition rate was moderate (36%, n = 80). Of those randomized to the treatment conditions, n = 43 (57%) of the SC group and n = 44 (59%) of the CR group followed up to T2 (see Fig. 2). Based on our conservative approach, n = 97 (n = 82 for PSQ-PS) completed all primary outcome measures and received the allocated intervention. Moreover, preliminary intervention checks showed that the two interventions were assessed as comparably motivating, successful, and challenging in terms of their application at T1, all t(104.09)s ≤ 1.27, ps ≤ .208. Interestingly, at the booster session (T2), the SC group reported the application of the intervention to be less demanding, t(57.82) = 2.50, p = .015, d = 0.66, and a higher successful application compared to the CR group, t(60.66) = −2.78, p = .007, d = 0.71 (see Supplement Table S1).
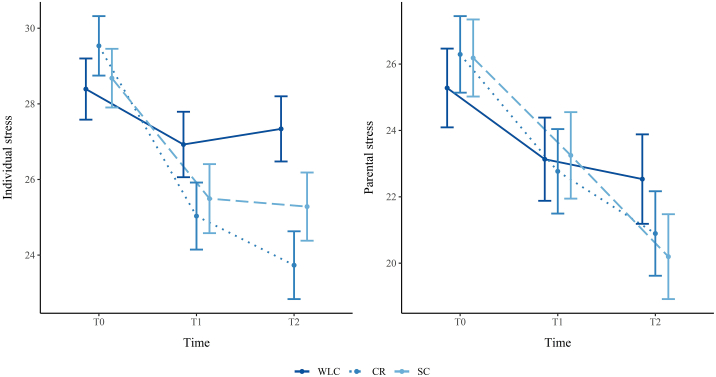
3.3. ITT analyses: changes in parents' individual and parental stress
Generalized linear mixed model (GLMM) analyses of individual stress revealed a significant main effect of time, but no main effect of group (see Table 2). Moreover, a significant interaction effect of time × group was found (see Fig. 3). Post-hoc paired t-tests showed a significant decrease in individual stress levels from T0 to T1 in the CR group, t(273) = 6.27, p < .001, d = 0.68, and in the SC group, t(273) = 4.22, p < .001, d = 0.48, but not in the WLC group. Moreover, significant changes emerged from T0 to T2 in both treatment groups, t(273) = 7.95, p < .001, d = 0.87 (CR), and t(273) = 4.59, p < .001, d = 0.51 (SC) respectively, but not from T1 to T2 (see Supplement Table S2). Group comparisons only revealed significantly lower individual stress at T2 in the CR group compared to the WLC group, t(214) = 2.90, p = .011, d = 0.54, but not in the SC group compared to the WLC group, t(214) = 1.65, p = .228, d = 0.31. The CR and the SC group did not differ significantly in their decrease of individual stress at T2, t(214) = −1.22, p = .443, d = 0.23.
Table 2.
Intention-to-treat (ITT) linear mixed model analysis of group, time and interaction effects on individual and parental stress.
| Fixed effects | Individual stress |
Parental stress |
||||
|---|---|---|---|---|---|---|
| F | df | p | F | df | p | |
| Intercept | 4162.08 | 1;273 | <.001** | 1413.48 | 1;246 | <.001** |
| Group | 0.16 | 2;214 | .865 | 0.01 | 2;208 | .992 |
| Time | 40.66 | 2;273 | <.001** | 43.83 | 2;246 | <.001** |
| Group × time | 6.03 | 4;273 | <.001** | 1.83 | 4;246 | .124 |
| Random effects | Variance | L.Ratio | p | Variance | L.Ratio | p |
| Intercept | 32.47 | 226.16 | <.001** | 77.86 | 260.92 | <.001** |
| Residual | 12.68 | 17.86 | ||||
| Model fit indices | Marginal | Conditional | Marginal | Conditional | ||
| Pseudo-R2 | .07 | .74 | .04 | .82 | ||
| AIC | 3074 | 3127 | ||||
| BIC | 3120 | 3172 | ||||
Note. N = 217 participants (parental stress: 211), 496 observations (parental stress: 463). AIC: Akaike Information Criterion. BIC: Bayesian Information Criterion. Marginal Pseudo-R2 indicates the proportion of variance explained by the fixed factors only, whereas conditional Pseudo-R2 indicates the proportion of variance explained by the overall model. *p < .05, **p < .01.
Fig. 3.
Estimated marginal means of perceived subjective stress and parental stress from T0 to T2 for cognitive reappraisal, self-compassion and wait-list control group.
Note: WLC: Wait-list control group. CR: Cognitive reappraisal group. SC: Self-compassion group. Error bars represent standard errors.
Regarding parental stress, only a significant main effect of time emerged (see Table 2). Post-hoc comparisons revealed significant differences between all time points, all t(246)s ≥ 5.64, all ps ≤ .003, 0.19 ≤ d ≤ 0.49, with the largest difference between baseline and booster session (posttest I, M = 2.87, SE = 0.51, p < .001). Although there was no significant interaction effect, exploratory group-separated post-hoc analysis revealed that the change between time points was mainly driven by T0 to T1 across all groups. Interestingly, only in the SC group emerged a significant difference between T1 and T2, which was similar in size to the change between baseline and booster, with t(246) = 3.18, p = .005, d = 0.31 (see Supplement Tables S3 and S4 for all post-hoc comparisons). Means for the primary stress outcomes are reported in Table 3. Moreover, Fig. 3 illustrates the group and time interactions for both stress outcomes. Including the age of the index child as a random factor did not significantly improve the model fit for either individual stress or parental stress, L-Ratio < 4.70, p > .097.
Table 3.
Observed means and standard deviations for each primary outcome by condition over time.
| Pre treatment (T0) |
Prior to booster session (T1) |
Post treatment (T2) |
||||
|---|---|---|---|---|---|---|
| M | SD | M | SD | M | SD | |
| PSS-10 | ||||||
| CR | 29.10 | 6.14 | 24.24 | 6.20 | 23.32 | 6.17 |
| SC | 29.11 | 6.79 | 25.32 | 5.26 | 24.79 | 5.54 |
| WCL | 28.49 | 7.43 | 27.29 | 7.43 | 27.91 | 8.28 |
| PSQ-PS (global) | ||||||
| CR | 26.16 | 9.46 | 20.79 | 7.73 | 19.47 | 9.17 |
| SC | 27.00 | 9.23 | 24.23 | 7.96 | 21.21 | 9.43 |
| WCL | 25.28 | 10.25 | 23.20 | 9.82 | 23.32 | 11.00 |
| PSQ-PS (preschool) | ||||||
| CR | 25.39 | 10.36 | 18.73 | 7.63 | 17.23 | 8.48 |
| SC | 24.65 | 9.49 | 20.31 | 7.57 | 17.5 | 9.00 |
| WCL | 24.06 | 9.26 | 21.46 | 10.58 | 24.06 | 9.26 |
| PSQ-PS (school) | ||||||
| CR | 27.03 | 8.42 | 22.95 | 7.41 | 21.81 | 9.47 |
| SC | 28.15 | 8.99 | 26.19 | 7.54 | 23.00 | 9.25 |
| WCL | 26.30 | 11.04 | 23.62 | 10.89 | 29.38 | 10.73 |
Note. PSS-10 = Perceived Stress Scale, global scale. PSQ-PS = Parental Stress subscale of the Parental Stress Questionnaire. CR = Cognitive reappraisal group, SC = Self-compassion group, WCL = Wait-list control group. Means (SD) of PSQ-PS are presented separately for preschool and school children and together (global).
The CR and SC groups showed comparable time effects on the DASS-21 subscales, with the largest reductions on the stress subscale from T0 to T2, t(136) = 4.15, p < .001, d = 0.49 (CR) and, t(136) = 3.64, p < .001, d = 0.43 (SC), respectively (see Supplement Table S5). Moreover, the results revealed an interaction effect of time × group for the anxiety subscale, F(2, 136) = 3.25, p = .042, and the stress subscale, F(2,136) = 3.86, p = .023 (see Supplement Fig. S2). Post-hoc comparisons yielded significant findings, with decreases in depression and stress from T0 to T2 in the CR and SC groups, whereas a reduction of anxiety levels was only observed for CR. Post-hoc group comparisons did not yield any significant findings for either the anxiety or the stress subscale at any time point (see Supplement Table S5).
3.4. PP analyses: changes in parents' individual and parental stress
When analyses were restricted to treatment completers, the same pattern of main findings emerged for individual and parental stress, indicating only a significant group × time interaction for individual stress (see Table 4). With respect to post-hoc comparisons, all effects observed in the ITT analyses remained statistically significant and increased in their effect sizes, with the exception of the T1 and T2 comparison in the SC group for parental stress (see Supplement Tables S6, S7 and S8).
Table 4.
Per-protocol (PP) linear mixed model analysis of group, time and interaction effects on individual and parental stress.
| Fixed effects | Individual stress |
Parental stress |
||||
|---|---|---|---|---|---|---|
| F | df | p | F | df | p | |
| Intercept | 1679.50 | 1;188 | <.001** | 721.73 | 1;158 | <.001** |
| Group | 2.19 | 2;94 | .118 | 0.77 | 2;79 | .468 |
| Time | 28.32 | 2;188 | <.001** | 24.52 | 2;158 | <.001** |
| Group × time | 4.44 | 4;188 | .002** | 1.05 | 4;158 | .386 |
| Random effects | Variance | Variance | ||||
| Intercept | 37.22 | 54.52 | ||||
| Residual | 12.31 | 18.87 | ||||
| Model fit indices | Marginal | Conditional | Marginal | Conditional | ||
| Pseudo-R2 | .07 | .74 | .04 | .82 | ||
| AIC | 1778 | 1600 | ||||
| BIC | 1818 | 1638 | ||||
Note. N = 97 participants (parental stress: 82), 291 observations (parental stress: 246). Sample sizes differ due to a technical error preventing some participants in the WLC group from submitting the parental stress questionnaire at T2. AIC: Akaike Information Criterion. BIC: Bayesian information criterion. Marginal Pseudo-R2 indicates the proportion of variance explained by the fixed factors only, whereas conditional Pseudo-R2 indicates the proportion of variance explained by the overall model. *p < .05, **p < .01.
3.5. Sensitivity analyses: influence of baseline stress and ER on efficacy of regulation strategies
At the request of the reviewers, we conducted exploratory analyses to test whether the differential efficacy of SC and CR might be moderated by initial stress levels. Following Diedrich et al. (2014), we used median splits to create groups of low (M = 23.65, SD = 4.08) and high (M = 34.66, SD = 4.03) individual stress levels (PSS-10) at baseline and low (M = 18.16, SD = 6.13) and high (M = 33.92, SD = 5.25) parental stress, respectively. Although model fit was improved with the inclusion of high vs. low baseline stress levels (L-Ratio > 207.99, p ≤ .001), the relevant three-way interaction (time × treatment group × stress level group) did not reach statistical significance for individual, F(4,267) = 1.17, p = .323, or parental stress, F(4,267) = 1.01, p = .405. However, when directly inspecting relevant post-hoc comparisons, parents experiencing higher individual stress at baseline displayed a significantly greater reduction of individual stress at T2 in the CR group compared to the WLC, t(211) = 3.73, p ˂ .001, d = 1.02, and in the SC group compared to the WLC, t(211) = 2.87, p = .012, d = 0.84. In contrast, parents with lower individual stress at baseline displayed a greater reduction of individual stress at T2 in the CR group compared to WLC, t(211) = 3.07, p = .007, d = 0.85, and in the CR group compared to the SC group, t(211) = −2.76, p = .017, d = 0.76. Similarly, significantly greater reductions of parental stress at T2 were found in parents with high baseline levels of parental stress in the CR group, t(205) = 2.71, p = .020, d = 0.72, and the SC group, t(205) = 2.41, p = .043, d = 0.64, compared to WLC. No difference emerged between CR and SC groups of parents with high levels of parental stress and between any group of parents with low levels of initial parental stress, t(205) ≤ 1.91, p ≥ .138. Additionally, we tested whether including baseline trait CR (ERQ) as a random slope significantly improves the model fit for individual stress, but no model improvement was found, L-Ratio = 5.32, p = .070. By contrast, including baseline trait SC (SCS-SF) as a random slope significantly improved the model fit, L-Ratio = 8.58, p = .013. However, effect sizes and statistical significance of the post-hoc comparisons were only marginally affected by including baseline SC (Δd = 0.03). Regarding parental stress, model fit was not improved by including baseline CR or baseline SC, L-Ratio ≤ 5.20, p ≥ .074.
3.6. Mediation analyses: treatment effects on parental stress mediated by individual stress
Given that our main analyses revealed no direct treatment effects on parental stress, we examined in an additional analysis whether the interventions decreased parental stress indirectly, mediated by reduced individual stress. A simple mediation analysis using two dummy-coded variables (CR vs. WLC, SC vs. WLC) revealed that group significantly predicted individual stress at T2 for CR compared to WLC, b = −6.063, t(79) = −3.229, p = .002, but not for SC compared to WLC, b = −3.364, t(79) = −1.744, p = .085 (see Supplement Fig. S3). Individual stress, in turn, significantly predicted parental stress at T2, b = 0.724, t(78) = 5.437, p < .001. There was no evidence that group directly influenced parental stress, b = −3.773, t(79) = −1.530, p = .130, and b = −2.616, t(79) = −0.970, p = .335, respectively. However, the relationship between group and parental stress was mediated by individual stress for CR compared to WLC, ab = −4.393, SE = 1.548, 95% CI[−7.695, −1.651], but not for SC compared to WLC, ab = −2.437, SE = 1.438, 95% CI[−5.434, 0.227]. This finding indicates that only the CR intervention decreased parental stress indirectly through reductions in individual stress. The same pattern of findings emerged for the relationships between individual stress and parental stress at T1 (see Supplement Table S9).
4. Discussion
Recent pandemic restrictions have aggravated parents' individual stress and dyadic stress with their children (Brown et al., 2020; Canady, 2020; Spinelli et al., 2020). The current study aimed to evaluate the stress-reducing effects of two minimal online ER interventions, namely CR and SC, for stressed parents during the COVID-19 pandemic. Our hypotheses were partially confirmed: Looking at time effects within groups separately, CR and SC interventions both led to medium to large reductions of individual and parental stress, mainly driven by changes due to the main session. However, only CR reduced parents' stress levels remarkably compared to the WLC without any treatment, with a medium effect size. Additionally, more severely stressed parents appeared to have also benefited from SC, whereas less stressed parents benefited more from CR than from SC interventions, at least for individual stress. Contrary to our expectations, parents did not report a higher stress reduction from SC compared to CR and no intervention, either for individual stress or for parental stress. Interestingly, mediation analyses revealed that reduced individual stress decreased the likelihood of engaging in dysfunctional parent-child interactions and ultimately mitigated parental stress. Due to statistical limitations, this mediating effect was only found for parents who received the CR intervention as allocated, and must be interpreted with caution.
The hypothesis that SC with common parenthood, as a potentially especially helpful component in a global pandemic, exceeds the efficacy of CR was not supported by our data. There are several possible explanations for this finding: First, SC might be less effective in reducing stress than in reducing depressed mood (Diedrich et al., 2014, Diedrich et al., 2016, and Ehret et al., 2018). Second, it is conceivable that the implementation of the SC intervention in the current study was not sufficiently powerful to transfer to daily family practice. Speaking against this argument, however, the SC group reported a more successful application after the booster session compared to the other treatment group. The self-compassion break that was instructed in our intervention is a relatively compact and rather complex intervention, that does not involve practicing the single components individually beforehand, even though we provided psychoeducational contents about SC in the first part of the intervention. Dreisoerner et al. (2021) demonstrated spill-over effects insofar as improvements in mindfulness (and also to a lesser degree in common humanity), but not in self-kindness, were accompanied by improvements in other components of SC. If, even for a predominantly student sample, a detailed writing exercise to practice self-kindness might not be effective without having practiced mindfulness before (see Dreisoerner et al., 2021), it is quite possible that the parents in our study might have been unable to apply SC as thoroughly as intended by the intervention.
Interestingly, in line with Diedrich et al. (2014), some evidence emerged that the efficacy of ER strategies might be moderated by the intensity of initial individual or parental stress. More intensive stress might be easier to change with the help of SC as compared to lower stress levels, as applying compassion to oneself is facilitated when one is experiencing more suffering. However, these exploratory analyses have to be considered with caution as our sample did not experience high levels of stress on a global level, and differences only emerged in post-hoc comparisons.
Although the CR group reported greater effort and less success in applying the strategy, they applied the intervention more effectively. It may have helped these parents that the cognitive restructuring of critical self-responding was directly tailored, whereas the parents in the SC group received more indirect support while strengthening compassionate self-responding. As Neff et al. (2018) recently recommended, increased compassionate and decreased uncompassionate self-responding should be instructed holistically in SC interventions. However, within the self-compassion break, it is challenging to guide the participants to be compassionate to themselves in particular when they are being self-critical, e.g. in the concrete moment of practice when they do not manage to validate their emotions. In sum, SC might be a complex and more holistic emotional attitude toward the self compared to CR (see also Inwood and Ferrari, 2018; Neff et al., 2018) that eventually cannot be taught well effectively in a very brief online-only format as implemented in the current study. Recent online RCTs that studied longer-lasting SC-related interventions including both mechanisms (e.g. Eriksson et al., 2018; Krieger et al., 2019) showed SC to be superior to WLCs and care as usual in terms of improving different distress symptoms. These promising findings indicate that stressed parents might also benefit from SC if offered on a more in-depth basis with intensive training. Moreover, Gilbert (2009) refers to the relevance of self-compassionate patient-therapist interactions and a high level of self-reflection to apply self-kindness in times of great distress and suffering. This is further supported by the fact that the main findings were not moderated by including a trait measure of SC in our statistical models. Next to intensive training, direct therapist support, for example via webcam, is worthy of consideration in the application of SC as recommended by Neff et al. (2018), possibly requiring some form of blended therapy approach.
In addition, although we used classical mood induction procedures, for which validity references exist (Westermann et al., 1996), the experimentally induced emotional activation by pictures and dysfunctional thoughts concerning impacts of pandemic restrictions for the parent role might not be adequate to elicit a sufficiently marked emotional response, especially in an online format. Based on Gross' model (2002), SC might be effective when emotions of helplessness, fear, and sadness are fully activated. This is also supported by the fact that the higher stressed parents in our sample might be better able to benefit from SC.
An explanation for the unexpected superior efficacy of CR may be that in a highly demanding phase of a pandemic, cognitive-based and antecedent-focused ER strategies that foster adaptive problem coping are easier to adopt than a more emotion-based ER such as SC. The latter can be overwhelming and thus perhaps inappropriate in an acute crisis, as we know from trauma research (Stanisławski, 2019). By contrast, CR is strongly associated with avoidance of elicited aversive emotions (Wolgast et al., 2011), which might predict difficulty in processing stressful events in the long term. Accordingly, college students with higher clinical distress and lower experiential avoidance reported the greatest post-traumatic personal growth after traumatic events (Kashdan and Kane, 2011). Therefore, it would be worthwhile to examine the additional benefit of a stepped-care approach: CR is presumably an effective ER strategy for all stressed parents during an acute stage of pandemic stress. SC might be a second intervention step within blended care especially for those parents with increased psychopathology, e.g. with high individual stress levels (as indicated by exploratory analyses) or clinically relevant depression scores.
Interestingly, we only found evidence of indirect effects of CR on parental stress, via reduced individual stress. This is in contrast to earlier findings showing that an online mindfulness training intervention led to a significant decrease in parental stress compared to a wait-list period (Potharst et al., 2019). It also raises the question of why parental stress decreased almost equally in all groups from baseline to booster session. One could argue that in an acute pandemic situation, after an initial state of distress or shock, parents might activate a “crisis mode” for their children and succeed in following their parental protective instincts (Schaller, 2018). As our sample was rather highly educated and financially well-off, it is plausible that we investigated a relatively privileged group of parents who adapted well to the unique COVID-19-related stressors and overcame an initial acute state of stress quite successfully. Moreover, existential worries during the pandemic may be less pronounced in both Austria and Germany compared to other countries due to a well-functioning health care system and strong governmental support. Receiving short-time working salaries between 80 and 90% of the last net income could have significantly reduced the financial family burden. The privileged nature of our sample may limit the generalizability of the findings. As previously indicated, further studies should add a pre-screening in order to include parents with highly elevated parental stress levels and a higher risk of child maltreatment. In addition, adaptations of our online intervention for other countries with different health care and economical systems should be carefully evaluated regarding their efficacy. Furthermore, it may be questioned whether an ER intervention can directly reduce parental stress at all. A calm and emotionally regulated attitude enables a better interaction in conflict situations with children (Bariola et al., 2011; Rutherford et al., 2015). However, skills that are inherently related to parenting, such as managing child misbehavior and encouraging desirable behavior, are also needed to deal with new challenging family situations during quarantine, which we did not implement in the respective interventions. To conclude, a more holistic training, combining the teaching of ER strategies with education skills adapted to the specific needs of parents during pandemic restrictions, could be a useful extension in further studies.
A number of limitations should be considered when interpreting the results of the present study. We did not measure either the frequency of application of the ER intervention in everyday life or personal feedback on the therapeutic process during study course. Further studies should focus in detail which types of personally relevant thoughts the participants chose to use in adapting CR and SC and how these ER strategies could be incorporated for the sake of engaging in the family routine. Moreover, as we did not objectively verify the extent of emotional activation (for instance by using a physiological measure), it is possible that emotions were not fully activated, which would be a basic requirement to maximize the stress-reducing effects of SC. In addition, it is questionable whether SC can be compared to CR as a stand-alone ER strategy in terms of its impact on distress, given its broader construct which might work through ER strategies, such as CR (Bates et al., 2020; Inwood and Ferrari, 2018). ER application frequency in daily life and emotional activation should be addressed more thoroughly in future research in order to examine how SC-related interventions could be optimized to mitigate parental stress. Moreover, a longer follow-up interval of at least several weeks would be required to assess the long-term efficacy of the interventions. With respect to our mediation analyses, we did not make full use of our longitudinal design due to a lack of prior hypothesis definition and insufficient power. Therefore, our cross-sectional finding regarding the indirect effect of individual stress on parental stress in the CR group should be replicated in longitudinal mediation analyses with an appropriate sample size to detect the postulated effects.
Nevertheless, several strengths of the study should be noted, including a WLC without treatment and high-quality online ER interventions adapted to the specific requirements of parents during pandemic restrictions. Moreover, to the best of our knowledge, this is the first clinical intervention study for stressed parents in the early acute state of the COVID-19 pandemic restrictions, the first participants were included at the end of April 2020. As such, the results illustrate primary stress reactions to the given stressors in pandemic-related everyday family life. Additionally, the early intervention of our RCT may have supported the parents in remaining to function in their parental role and prevent further increases in stress responses. Furthermore, these first brief ER interventions provide a well-evaluated starting point for the development of more comprehensive interventions as the pandemic progresses.
4.1. Conclusion
A simple, very brief online video training intervention that is easily accessible even under quarantine measures has the potential to reduce parents' stress during pandemics. To the best of our knowledge, this is the first study to evaluate the efficacy of online ER interventions in stressed parents during pandemic restrictions. Our findings provide initial evidence that CR constitutes an effective minimal online intervention to mitigate parents' individual stress directly and parental stress indirectly. Due to the preliminary nature of this study, our findings should be replicated and the long-term efficacy examined. To optimize SC as an online crisis intervention, a blended therapy approach with direct therapist support might be more promising than video-guided self-directed help. In sum, if a further wave of the COVID-19 pandemic, or other future pandemics, require restrictions or quarantine measures, it will be desirable to have effective, low-threshold ER training interventions at hand in order to prevent parents' stress and help families weather the crisis unscathed.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
Acknowledgments
We are thankful to all parents who participated in this study in highly stressful times.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.invent.2021.100388.
Appendix A. Supplementary data
Supplementary figures and tables S1-S9.
References
- Abidin R.R. University of Virginia; Charlottesville: 1976. A Model of Parenting Stress. [Google Scholar]
- Abidin R.R. The determinants of parenting behavior. J. Clin. Child Psychol. 1992;21(4):407–412. doi: 10.1207/s15374424jccp2104_12. [DOI] [Google Scholar]
- Abler B., Kessler H. Emotion Regulation Questionnaire – Eine deutschsprachige Fassung des ERQ von Gross und John. Diagnostica. 2009;55(3):144–152. doi: 10.1026/0012-1924.55.3.144. [DOI] [Google Scholar]
- Antony M.M., Bieling P.J., Cox B.J., Enns M.W., Swinson R.P. Psychometric properties of the 42-item and 21-item versions of the depression anxiety stress scales in clinical groups and a community sample. Psychol. Assess. 1998;10(2):176–181. doi: 10.1037/1040-3590.10.2.176. [DOI] [Google Scholar]
- Bariola E., Gullone E., Hughes E.K. Child and adolescent emotion regulation: the role of parental emotion regulation and expression. Clin. Child. Fam. Psychol. Rev. 2011;14(2):198–212. doi: 10.1007/s10567-011-0092-5. [DOI] [PubMed] [Google Scholar]
- Bates G.W., Elphinstone B., Whitehead R. Self-compassion and emotional regulation as predictors of social anxiety. Psychol. Psychother. 2020 doi: 10.1111/papt.12318. Advance online publication. [DOI] [PubMed] [Google Scholar]
- Bäuerle A., Teufel M., Musche V., Weismüller B., Kohler H., Hetkamp M., Dörrie N., Schweda A., Skoda E.-M. Increased generalized anxiety, depression and distress during the COVID-19 pandemic: a cross-sectional study in Germany. J. Public Health (Oxf.) 2020 doi: 10.1093/pubmed/fdaa106. Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck A.T. Guilford Publications; 1979. Cognitive Therapy of Depression. [Google Scholar]
- Brooks S.K., Webster R.K., Smith L.E., Woodland L., Wessely S., Greenberg N., Rubin G.J. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395(10227):912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown S.M., Doom J., Watamura S., Lechuga-Pena S., Koppels T. 2020. Stress and Parenting During the Global COVID-19 Pandemic. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell-Sills L., Barlow D.H. Incorporating emotion regulation into conceptualizations and treatments of anxiety and mood disorders. In: Gross J.J., editor. Handbook of Emotion Regulation. Guilford Press; 2007. pp. 542–559. [Google Scholar]
- Canady V.A. APA stress report amid COVID-19 points to parental challenges. Ment. Heal. Wkly. 2020;30(22):3–4. doi: 10.1002/mhw.32385. [DOI] [Google Scholar]
- Cohen S., Kamarck T., Mermelstein R. A global measure of perceived stress. J. Health Soc. Behav. 1983;24(4):385. doi: 10.2307/2136404. [DOI] [PubMed] [Google Scholar]
- Coyne L.W., Gould E.R., Grimaldi M., Wilson K.G., Baffuto G., Biglan A. First things first: parent psychological flexibility and self-compassion during COVID-19. Behav. Anal. Pract. 2020:1–7. doi: 10.1007/s40617-020-00435-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cuijpers P., Marks I.M., van Straten A., Cavanagh K., Gega L., Andersson G. Computer-aided psychotherapy for anxiety disorders: a meta-analytic review. Cogn. Behav. Ther. 2009;38(2):66–82. doi: 10.1080/16506070802694776. [DOI] [PubMed] [Google Scholar]
- Deater-Deckard K. Parenting stress and child adjustment: some old hypotheses and new questions. Clin. Psychol. Sci. Pract. 1998;5(3):314–332. doi: 10.1111/j.1468-2850.1998.tb00152.x. [DOI] [Google Scholar]
- Diedrich A., Grant M., Hofmann S.G., Hiller W., Berking M. Self-compassion as an emotion regulation strategy in major depressive disorder. Behav. Res. Ther. 2014;58:43–51. doi: 10.1016/j.brat.2014.05.006. [DOI] [PubMed] [Google Scholar]
- Diedrich A., Hofmann S.G., Cuijpers P., Berking M. Self-compassion enhances the efficacy of explicit cognitive reappraisal as an emotion regulation strategy in individuals with major depressive disorder. Behav. Res. Ther. 2016;82:1–10. doi: 10.1016/j.brat.2016.04.003. [DOI] [PubMed] [Google Scholar]
- Diedrich A., Burger J., Kirchner M., Berking M. Adaptive emotion regulation mediates the relationship between self-compassion and depression in individuals with unipolar depression. Psychol. Psychother. 2017;90(3):247–263. doi: 10.1111/papt.12107. [DOI] [PubMed] [Google Scholar]
- Domsch H., Lohaus A. Hogrefe; 2010. ESF - Elternstressfragebogen. [Google Scholar]
- Dreisoerner A., Junker N.M., van Dick R. The relationship among the components of self-compassion: a pilot study using a compassionate writing intervention to enhance self-kindness, common humanity, and mindfulness. J. Happiness Stud. 2021;22(1):21–47. doi: 10.1007/s10902-019-00217-4. [DOI] [Google Scholar]
- Ehret A.M., Joormann J., Berking M. Self-compassion is more effective than acceptance and reappraisal in decreasing depressed mood in currently and formerly depressed individuals. J. Affect. Disord. 2018;226:220–226. doi: 10.1016/j.jad.2017.10.006. [DOI] [PubMed] [Google Scholar]
- Eriksson T., Germundsjö L., Åström E., Rönnlund M. Mindful self-compassion training reduces stress and burnout symptoms among practicing psychologists: a randomized controlled trial of a brief web-based intervention. Front. Psychol. 2018;9:2340. doi: 10.3389/fpsyg.2018.02340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fegert J.M., Vitiello B., Plener P.L., Clemens V. Challenges and burden of the Coronavirus 2019 (COVID-19) pandemic for child and adolescent mental health: a narrative review to highlight clinical and research needs in the acute phase and the long return to normality. Child Adolesc. Psychiatry Ment. Health. 2020;14:20. doi: 10.1186/s13034-020-00329-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghebreyesus T.A. WHO director-general's opening remarks at the media briefing on COVID-19 – 11 March 2020. 2020. https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020
- Gilbert P. Introducing compassion-focused therapy. Adv. Psychiatr. Treat. 2009;15(3):199–208. doi: 10.1192/apt.bp.107.005264. [DOI] [Google Scholar]
- Gross J.J. Emotion regulation: affective, cognitive, and social consequences. Psychophysiology. 2002;39(3):281–291. doi: 10.1017/S0048577201393198. [DOI] [PubMed] [Google Scholar]
- Gross J.J. Emotion regulation: current status and future prospects. Psychol. Inq. 2015;26(1):1–26. doi: 10.1080/1047840X.2014.940781. [DOI] [Google Scholar]
- Gross J.J., John O.P. Individual differences in two emotion regulation processes: implications for affect, relationships, and well-being. J. Pers. Soc. Psychol. 2003;85(2):348–362. doi: 10.1037/0022-3514.85.2.348. [DOI] [PubMed] [Google Scholar]
- Harris P.A., Taylor R., Minor B.L., Elliott V., Fernandez M., O’Neal L., McLeod L., Delacqua G., Delacqua F., Kirby J., Duda S.N., REDCap Consortium The REDCap consortium: building an international community of software platform partners. J. Biomed. Inform. 2019;95:103208. doi: 10.1016/j.jbi.2019.103208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes A.F. Methodology in the Social Sciences. Guilford Press; 2013. Introduction to mediation, moderation, and conditional process analysis: a regression-based approach.http://lib.myilibrary.com/detail.asp?id=480011 [Google Scholar]
- Hofmann S.G., Asnaani A., Vonk I.J.J., Sawyer A.T., Fang A. The efficacy of cognitive behavioral therapy: a review of meta-analyses. Cogn. Ther. Res. 2012;36(5):427–440. doi: 10.1007/s10608-012-9476-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holly L.E., Fenley A.R., Kritikos T.K., Merson R.A., Abidin R.R., Langer D.A. Evidence-base update for parenting stress measures in clinical samples. J. Clin. Child Adolesc. Psychol. 2019;48(5):685–705. doi: 10.1080/15374416.2019.1639515. [DOI] [PubMed] [Google Scholar]
- Hupfeld J., Ruffieux N. Validierung einer deutschen Version der Self-Compassion Scale (SCS-D) Z. Klin. Psychol. Psychother. 2011;40(2):115–123. doi: 10.1026/1616-3443/a000088. [DOI] [Google Scholar]
- Inwood E., Ferrari M. Mechanisms of change in the relationship between self-compassion, emotion regulation, and mental health: a systematic review. Appl. Psychol. Health Well-Being. 2018;10(2):215–235. doi: 10.1111/aphw.12127. [DOI] [PubMed] [Google Scholar]
- Kashdan T.B., Kane J.Q. Posttraumatic distress and the presence of posttraumatic growth and meaning in life: experiential avoidance as a moderator. Personal. Individ. Differ. 2011;50(1):84–89. doi: 10.1016/j.paid.2010.08.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klein E.M., Brähler E., Dreier M., Reinecke L., Müller K.W., Schmutzer G., Wölfling K., Beutel M.E. The German version of the perceived stress scale - psychometric characteristics in a representative German community sample. BMC Psychiatry. 2016;16:159. doi: 10.1186/s12888-016-0875-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kowal M., Coll-Martín T., Ikizer G., Rasmussen J., Eichel K., Studzinska A., Koszałkowska K., Karwowski M., Najmussaqib A., Pankowski D., Lieberoth A., Ahmed O. Who is the most stressed during COVID-19 isolation? Data from 27 countries and areas. Appl. Psychol. Health Well-Being. 2020 doi: 10.1111/aphw.12234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krieger T., Reber F., von Glutz B., Urech A., Moser C.T., Schulz A., Berger T. An internet-based compassion-focused intervention for increased self-criticism: a randomized controlled trial. Behav. Ther. 2019;50(2):430–445. doi: 10.1016/j.beth.2018.08.003. [DOI] [PubMed] [Google Scholar]
- Lazarus R.S., Folkman S. Springer; 1984. Stress, Appraisal, and Coping. [Google Scholar]
- Lovibond S.H., Lovibond P.F. 2nd ed. 1995. Manual for the Depression Anxiety Stress Scales. (Psychology Foundation) [Google Scholar]
- Moser C., Bachem R., Berger T., Maercker A. Ziel: internet-based self-help for adjustment problems: results of a randomized controlled trial. J. Clin. Med. 2019;8(10) doi: 10.3390/jcm8101655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neff K., Germer C.K. The Guilford Press; 2018. The Mindful Self-compassion Workbook: A Proven Way to Accept Yourself, Build Inner Strength, and Thrive. [Google Scholar]
- Neff K.D. The development and validation of a scale to measure self-compassion. Self Identity. 2003;2(3):223–250. doi: 10.1080/15298860309027. [DOI] [Google Scholar]
- Neff K.D., Long P., Knox M.C., Davidson O., Kuchar A., Costigan A., Williamson Z., Rohleder N., Tóth-Király I., Breines J.G. The forest and the trees: examining the association of self-compassion and its positive and negative components with psychological functioning. Self Identity. 2018;17(6):627–645. doi: 10.1080/15298868.2018.1436587. [DOI] [Google Scholar]
- Nilges P., Essau C. Die Depressions-Angst-Stress-Skalen: Der DASS - ein Screeningverfahren nicht nur für Schmerzpatienten [Depression, Anxiety and Stress Scales: DASS - a screening procedure not only for pain patients] Schmerz (Berlin, Germany) 2015;29(6):649–657. doi: 10.1007/s00482-015-0019-z. [DOI] [PubMed] [Google Scholar]
- Ostberg M., Hagekull B. A structural modeling approach to the understanding of parenting stress. J. Clin. Child Psychol. 2000;29(4):615–625. doi: 10.1207/S15374424JCCP2904_13. [DOI] [PubMed] [Google Scholar]
- Petzold M.B., Bendau A., Plag J., Pyrkosch L., Mascarell Maricic L., Betzler F., Rogoll J., Große J., Ströhle A. Risk, resilience, psychological distress, and anxiety at the beginning of the COVID-19 pandemic in Germany. Brain Behav. 2020 doi: 10.1002/brb3.1745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pieh C., Budimir S., Probst T. The effect of age, gender, income, work, and physical activity on mental health during coronavirus disease (COVID-19) lockdown in Austria. J. Psychosom. Res. 2020;136:110186. doi: 10.1016/j.jpsychores.2020.110186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pinheiro J., Bates D., DebRoy S., Sarkar D., R Core Team Nlme: Linear and Nonlinear Mixed Effects Models [Computer Software] 2020. https://CRAN.R-project.org/package=nlme
- Potharst E.S., Boekhorst M.G.B.M., Cuijlits I., van Broekhoven K.E.M., Jacobs A., Spek V., Nyklíček I., Bögels S.M., Pop V.J.M. A randomized control trial evaluating an online mindful parenting training for mothers with elevated parental stress. Front. Psychol. 2019;10:1550. doi: 10.3389/fpsyg.2019.01550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preacher K.J., Hayes A.F. Spss and SAS procedures for estimating indirect effects in simple mediation models. Behav. Res. Methods Instrum. Comput. 2004;36(4):717–731. doi: 10.3758/bf03206553. [DOI] [PubMed] [Google Scholar]
- Preece D.A., Becerra R., Robinson K., Gross J.J. The Emotion Regulation Questionnaire: psychometric properties in general community samples. J. Pers. Assess. 2020;102(3):348–356. doi: 10.1080/00223891.2018.1564319. [DOI] [PubMed] [Google Scholar]
- Prime H., Wade M., Browne D.T. Risk and resilience in family well-being during the COVID-19 pandemic. Am. Psychol. 2020;75(5):631–643. doi: 10.1037/amp0000660. [DOI] [PubMed] [Google Scholar]
- Querstret D., Cropley M., Fife-Schaw C. The effects of an online mindfulness intervention on perceived stress, depression and anxiety in a non-clinical sample: a randomised waitlist control trial. Mindfulness. 2018;9(6):1825–1836. doi: 10.1007/s12671-018-0925-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raes F., Pommier E., Neff K.D., van Gucht D. Construction and factorial validation of a short form of the Self-Compassion Scale. Clin. Psychol. Psychother. 2011;18(3):250–255. doi: 10.1002/cpp.702. [DOI] [PubMed] [Google Scholar]
- Reis D., Lehr D., Heber E., Ebert D.D. The German version of the Perceived Stress Scale (PSS-10): evaluation of dimensionality, validity, and measurement invariance with exploratory and confirmatory bifactor modeling. Assessment. 2019;26(7):1246–1259. doi: 10.1177/1073191117715731. [DOI] [PubMed] [Google Scholar]
- Riegler J.L., Ray S.P., Moscato E.L., Narad M.E., Kincaid A., Wade S.L. Pilot trial of a telepsychotherapy parenting skills intervention for veteran families: implications for managing parenting stress during COVID-19. J. Psychother. Integr. 2020;30(2):290–303. doi: 10.1037/int0000220. [DOI] [Google Scholar]
- RStudio Team . RStudio, PBC; Boston, MA: 2020. RStudio: Integrated Development for R.http://www.rstudio.com/ [Google Scholar]
- Rutherford H.J.V., Wallace N.S., Laurent H.K., Mayes L.C. Emotion regulation in parenthood. Dev. Rev. 2015;36:1–14. doi: 10.1016/j.dr.2014.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saurabh K., Ranjan S. Compliance and Psychological Impact of Quarantine in Children and Adolescents due to Covid-19 Pandemic. Indian J Pediatr. 2020;87(7):532–536. doi: 10.1007/s12098-020-03347-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schaller M. The parental care motivational system and why it matters (for everyone) Curr. Dir. Psychol. Sci. 2018;27(5):295–301. doi: 10.1177/0963721418767873. [DOI] [Google Scholar]
- Schneider E.E., Schönfelder S., Domke-Wolf M., Wessa M. Measuring stress in clinical and nonclinical subjects using a German adaptation of the Perceived Stress Scale. Int. J. Clin. Health Psychol. 2020;20(2):173–181. doi: 10.1016/j.ijchp.2020.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spinelli M., Lionetti F., Pastore M., Fasolo M. Parents’ stress and children’s psychological problems in families facing the COVID-19 outbreak in Italy. Front. Psychol. 2020;11:1713. doi: 10.3389/fpsyg.2020.01713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stanisławski K. The Coping Circumplex Model: an integrative model of the structure of coping with stress. Front. Psychol. 2019;10:694. doi: 10.3389/fpsyg.2019.00694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szabo T.G., Richling S., Embry D.D., Biglan A., Wilson K.G. From helpless to hero: promoting values-based behavior and positive family interaction in the midst of COVID-19. Behav. Anal. Pract. 2020:1–9. doi: 10.1007/s40617-020-00431-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Westermann R., Spies K., Stahl G., Hesse F.W. Relative effectiveness and validity of mood induction procedures: a meta-analysis. Eur. J. Soc. Psychol. 1996;26(4):557–580. doi: 10.1002/(SICI)1099-0992(199607)26:4<557::AID-EJSP769>3.0.CO;2-4. [DOI] [Google Scholar]
- Whittle S., Bray K., Lin S., Schwartz O. 2020. Parenting and Child and Adolescent Mental Health During the COVID-19 Pandemic. [DOI] [Google Scholar]
- Wilson A.C., Mackintosh K., Power K., Chan S.W.Y. Effectiveness of self-compassion related therapies: a systematic review and meta-analysis. Mindfulness. 2019;10(6):979–995. doi: 10.1007/s12671-018-1037-6. [DOI] [Google Scholar]
- Wolgast M., Lundh L.-G., Viborg G. Cognitive reappraisal and acceptance: an experimental comparison of two emotion regulation strategies. Behav. Res. Ther. 2011;49(12):858–866. doi: 10.1016/j.brat.2011.09.011. [DOI] [PubMed] [Google Scholar]
- Wu M., Xu W., Yao Y., Zhang L., Guo L., Fan J., Chen J. Mental health status of students’ parents during COVID-19 pandemic and its influence factors. Gen. Psychiatry. 2020;33(4) doi: 10.1136/gpsych-2020-100250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiong J., Lipsitz O., Nasri F., Lui L.M.W., Gill H., Phan L., Chen-Li D., Iacobucci M., Ho R., Majeed A., McIntyre R.S. Impact of COVID-19 pandemic on mental health in the general population: a systematic review. J. Affect. Disord. 2020;277:55–64. doi: 10.1016/j.jad.2020.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary figures and tables S1-S9.