Abstract
Initial evidence suggests some Operation Enduring/Iraqi Freedom (OEF/OIF) veterans suffer from significant physical symptoms. It is not known if other medical conditions may explain these symptoms or if they are causing functional limitations. We compared OEF/OIF veterans with CFS to Desert Shield/Storm veterans with CFS seen at a post-deployment VA clinic soon after their respective deployments. We found 17.6% of OEF/OIF veterans met criteria for CFS. Compared to Desert Shield/Storm veterans with CFS, the OEF/OIF veterans with CFS demonstrated worse mental health function and similar physical health function.
Keywords: Quality of Life, Function, Veterans, Chronic Fatigue Syndrome, Iraq, Military, Gulf War Illness, Physical symptoms, Mental Health, PTSD
The United States mobilized over two and a half million service members to Operation Enduring Freedom (OEF) and Operation Iraqi Freedom (OIF). There is initial evidence to suggest that some OEF/OIF Veterans are experiencing wide-spread physical symptoms (e.g., back pain, headaches, nausea) (Iverson, Pogoda, Gradus, & Street, 2013; L. T. McAndrew, RF; Osinubi, OY; Jasien, JV; Quigley, KS, 2012; Quigley et al., 2012), an idea also suggested by the Institue of Medicine (2013). The experience of increased physical symptoms after combat is consistent with reports after previous wars. Hyams, Wignall & Roswell (1996) found an increase in reporting of physical symptoms after every war since the US civil war. Jones et al., (2002) also found increases in physical symptoms after every war since the Boer War.
Increases in physical symptoms were particularly notable after Operation Desert Shield/Desert Storm. Returning veterans complained of debilitating fatigue, pain and cognitive dysfunction. These symptoms correspond closely to Chronic Fatigue Syndrome (CFS) in non-veterans (Fukuda et al., 1994). CFS, a poorly understood illness, can be defined by persistent chronic fatigue of at least 6 months duration and four additional symptoms. CFS is only diagnosed once all medical conditions that could be causing the presenting symptom complex have been excluded (Fukuda et al., 1994). The rate of CFS among civilians is less than 1% (Jason et al., 1999; Reyes et al., 2003) and as high as 2.6% in primary care (Bates et al., 1993; Buchwald et al., 1995; Wessely, Chalder, Hirsch, Wallace, & Wright, 1997). In comparison, the rates of CFS among Desert Shield/Desert Storm veterans is 2.1% - 5.6% (Kang, Natelson, Mahan, Lee, & Murphy, 2003; McCauley et al., 2002). Desert Shield/Desert Storm veterans with CFS like conditions have significant functional impairments (Blanchard et al., 2006). Further, the cause of this increase in physical symptoms remains contested and there are few effective treatments.
To date, no study has examined CFS specifically among OEF/OIF veterans, but a number of studies have found evidence that veterans self-report increased physical symptoms after OEF/OIF deployment. Hoge et al. (2007) found among non-treatment seeking OEF/OIF veterans that 6.5% of soldiers without post traumatic stress disorder reported severe levels of physical symptoms and 11.5% of soldiers with post traumatic stress disorder reported severe levels of physical symptoms. McAndrew (In Press) found that one year after deployment to OEF/OIF, in a sample of 319 soldiers, almost 60% self-reported significant levels of wide-spread symptoms (11% of which reported severe symptoms). Symptoms were defined using the Center for Disease Control (CDC) definition of Chronic Multi-Symptom Illness (CMI) (Fukuda et al., 1998). Chronic Multi-Symptom Illness is an umbrella term for significant multi-system physical symptoms which has fewer exclusion criteria than CFS. The largest study to examine rates of physical symptom reporting after OEF/OIF was the Millenium Cohort Study, an epidemiological study of 73,078 OEF/OIF military personnel (Smith et al., 2014). The Millenium Cohort Study compared OEF/OIF military personnel who deployed to OEF/OIF military personnel who did not deploy to Desert Shield/Desert Storm veterans who deployed. They found that compared to OEF/OIF military personnel who did not deploy, deployment to OEF/OIF resulted in a 1.7 increase in odds of having self-report significant wide-spread symptoms (this was defined using an approximation of the CDC definition for Chronic Multi-Symptom Illness). An estimated 26.5% of OEF/OIF military personnel who deployed met criteria for clinically significant wide-spread symptoms after deployment. OEF/OIF military personnel who deployed reported fewer physical symptoms as compared to Operation Desert Shield/Desert Storm veterans.
The majority of studies to examine the levels of physical symptoms after OEF/OIF deployment have shown high levels of physical symptoms after deployment. What is not known is if the physical symptoms experienced by OEF/OIF veterans meet criteria for CFS, as was seen after Desert Shield/Desert Storm. This would require a medical evaluation to rule out medical conditions that may explained the symptoms. Further, it is not well known if the physical symptoms experienced by OEF/OIF Veterans are causing significant functional impairment. Our goal was to answer these questions by comparing the functional impairment of OEF/OIF veterans with CFS and without CFS who presented to our specialty clinic to Desert Shield/Storm veterans who CFS who presented soon after their deployment.
Methods
The research design was a cross-sectional chart review comprised of self-report data, clinician evaluation, and laboratory results. This research was approved by the New Jersey Department of Veterans Affairs Institutional Review Board and Research and Development Committee and participants either signed a consent form or we received a waiver of consent prior to including participants’ data.
Participants
OEF/OIF veteran outpatient participants (N=675) were enrolled at the U.S. Department of Veterans Affairs New Jersey War Related Illness and Injury Study Center (NJ WRIISC) between 2001 and 2010. The NJ WRIISC provides comprehensive clinical assessments to address post-deployment health concerns with a focus on medically unexplained symptoms. Veterans could be referred from their provider or self-referred. OEF/OIF veterans were assessed on average 2 years after OEF/OIF deployment.
A comparison cohort of Operation Desert Shield/Desert Storm veteran participants (N=200) was enrolled at VA’s Center for Environmental Hazards Research which was in operation between 1994 and 2000. The primary mission of the Center for Environmental Hazards Research was to study health consequences of deployment during the Desert Shield/Desert Storm. The Desert Shield/Desert Storm veteran cohort was recruited through letters sent to individuals on the Department of Veterans Affairs Persian Gulf Registry, and via local flyers and advertisements. Desert Shield/Desert Storm veterans were assessed on average 6 years after their combat deployment.
Definition of CFS and physical symptoms
In both veteran cohorts, CFS was diagnosed using the 1994 case definition (Fukuda et al., 1994). CFS is defined by persistent chronic fatigue of new onset and at least six months duration in addition to four out of eight symptoms that include: short-term memory or concentration problems, sore throat, tender lymph nodes, muscle pain, multi-joint pain, headaches, unrefreshing sleep and fatigue after exercise. An individual is not diagnosed with CFS if clinical evaluation reveals medical or psychiatric conditions that can explain the fatiguing illness such as: sleep apnea, anemia, major depressive disorder with psychotic features, bipolar disorder, severe obesity or certain medications (see (Fukuda et al., 1998; Pollet et al., 1998) for full definition and exclusion criteria). Head injury resulting in unconsciousness of at least 30 minutes was also excluded.
In both veteran cohorts, CFS symptoms were ascertained through the same self-report questionnaire designed to assess the criteria required to meet the 1994 case definition of CFS. The questionnaire asks about the time of onset and severity of the eight symptoms listed above. This questionnaire has been used in previous studies to capture self-report of CFS and has been used clinically to screen for CFS (e.g. (Kang et al., 2003; Lange et al., 2013)). The self-report questionnaire also asked about diagnoses and medications that would exclude veterans from a diagnosis of CFS. Next, veterans in both cohorts received a comprehensive medical examination administered by a physician complete with laboratory testing. The medical examination was used to probe for medical, psychiatric and laboratory results that could explain the veterans’ symptoms and these veterans were excluded from additional analyses. Neither alcohol nor substance abuse was used to exclude cases in either sample.
Health Function
We used the self-report Medical Outcomes Study Short Form-36 (SF-36) to assess functional status. The SF-36 compares favorably with other functional measures (D. Jones et al., 2001; Kazis et al., 2002). The measure has eight subscales, and composite physical and mental health scores. Scores range from 0 to 100 with a mean of 50 and a standard deviation of 10. Higher scores denote better functioning. OEF/OIF veterans were assessed with the Veterans Rand-36 (VR-36), whereas the Desert Shield/Desert Storm veterans were assessed with the SF-36 version 1. The VR-36 differs from SF-36 as it uses a five-point response for seven of the items (used to score the role physical and role emotional subscales) as opposed to the dichotomous response choice used in the SF-36 version 1. Kazis and colleagues compared the VR-36 to the SF-36 version 1 in a survey of 2162 veterans and determined that the modified items have the same interpretation as the original items (Kazis et al., 2004). The VR-36 was developed from the MOS RAND SF-36. The SF-36 is a registered trademark of the Medical Outcomes Trust. The 1998 norms were used to score both versions to facilitate comparisons across cohorts. For ease of discussion the remainder of the paper refers to these measures simply as the SF-36.
PTSD
The 17 item PTSD Checklist (PCL) was used to measure PTSD symptom severity in the OEF/OIF cohort (Weathers, 1993). The PCL asks participants to rate on a five point scale from 1(not at all) to 5 (extremely) how much the symptom/statement has bothered them over the past month. We used a cut off of 50 which has been shown to have a sensitivity of .82 and a specificity of .84 compared to a structured clinical interview (Weathers et al. 1993).
The 35 item Mississippi Scale for Combat-Related PTSD (M-PTSD) was used as a measure of PTSD symptoms in the Desert Shield/Desert Storm cohort (Hyer, Davis, Boudewyns, & Woods, 1991). The M-PTSD asks respondents to rate how true each question is for them on a five point likert scale (e.g. before I entered the military I had more close friends than I have now). We used a cut off of 107 which has been found to have a diagnostic accuracy of 90%, sensitivity of 93% and specificity of 89% compared to a structured clinical interview. PCL and M-PTSD scores are correlated at .68 to .86 in veteran populations (Orsillo, 2001).
Statistical Analysis
Statistical analyses were conducted using PASW version 18.0. We examine prevalence of CFS, physical symptoms, PTSD and functional status in the cohorts and used t-tests to explore demographic differences between OEF/OIF veterans with CFS to OEF/OIF veterans without CFS and between OEF/OIF veterans with CFS to Desert Shield/Desert Storm veterans with CFS. Next, a series of logistic regression analyses were conducted to compare rates of physical symptoms between OEF/OIF veterans with and without CFS and the rates of physical symptoms between Desert Shield/Desert Storm veterans with CFS and OEF/OIF veterans with CFS. We reported the rates of physical symptoms for each group in table 2 and the results of the logistic regression analyses comparing Desert Shield/Desert Storm veterans with CFS to OEF/OIF veterans with CFS in table 2.
Table 2.
Prevalence of CFS symptoms in OEF/OIF veterans with and without CFS, and GW veterans with CFS.
| OEF/OIF No CFS (N=416)a |
OEF/OIF CFS (N=119) |
GW CFS (N=100) |
OR* | 95% CI* | Significance (or p-value)* | |
|---|---|---|---|---|---|---|
| Concentration | 69.2% | 97.5% | 100% | - | - | NS |
| Joint Pain | 61.6% | 95.0% | 95.0% | - | - | NS |
| Fatigue after exercise | 38.3% | 87.8% | 99.0% | 12.3 | 1.5 – 98.1 | .02 |
| Poor Sleep | 71.6% | 100.0% | 100.0% | - | - | NS |
| Fever | 25.4% | 52.5% | 65.0% | 2.0 | 1.0 – 3.6 | .04 |
| Swollen Glands | 14.3% | 40.2% | 71.0% | 5.6 | 2.7 – 11.3 | <.001 |
| Sore Throat | 33.5% | 61.2% | 78.0% | 3.0 | 1.5 – 6.2 | .002 |
| Headaches | 47.3% | 85.6% | 98.0% | 17.4 | 2.2 – 137.2 | .007 |
| Muscle Pain | 55.1% | 95.0% | 96.0% | - | - | NS |
| Weakness | 36.4% | 78.2% | 91.0% | 3.1 | 1.3 – 7.7 | .01 |
Reported statistical comparison was only between OEF/OIF and GW veterans with CFS, and was adjusted for age, sex, and PTSD.
OEF/OIF veterans with CFS reported greater prevalence of all symptoms as compared to OEF/OIF veterans with no CFS.
We applied one MANCOVA to compare physical and mental functional status of OEF/OIF veterans with CFS to OEF/OIF veterans without CFS. In the MANCOVA there can be multiple dependent variables. We included each of the SF-36 subscales and the two composite scales (10 total) as the dependent variables. We initially controlled for age, sex, education, PTSD race and ethnicity. Only PTSD and age contributed significantly to the model. Therefore we only controlled for PTSD and age in subsequent analyses. There was no overlap in assessment time since deployment between the Desert Shield/Desert Storm veterans and OEF/OIF veterans therefore assessment time since deployment was not used as a control variable in the analyses as it “defined” the two groups (all Desert Shield/Desert Storm veterans were approx 6 years post-deployment and all OEF/OIF veterans were approx 2 years post-deployment).
We applied one MANCOVA to compare physical and mental functional status of OEF/OIF veterans with CFS to Desert Shield/Desert Storm veterans with CFS. We included each of the SF-36 subscales and the two composite scales (10 total) as the dependent variables. We initially controlled for age, sex, education, PTSD race and ethnicity. Only PTSD and age contributed significantly to the model. Therefore we only controlled for PTSD and age in subsequent analyses. There was no overlap in assessment time since deployment between the Desert Shield/Desert Storm veterans and OEF/OIF veterans therefore assessment time since deployment was not used as a control variable in the analyses as it “defined” the two groups (all Desert Shield/Desert Storm veterans were approx 6 years post-deployment and all OEF/OIF veterans were approx 2 years post-deployment).
Results
Demographics
We first examined the frequency of CFS among OEF/OIF veterans in our sample. Four percent of OEF/OIF veterans did not have complete data and so could not be classified. Thirty-four percent of OEF/OIF veterans screened positive for CFS; of these,16.3% were excluded from further analysis as they were using a medication or had a medical or psychiatric illness that could explain their symptoms (Fukuda et al., 1994). Therefore, 17.6% of OEF/OIF veterans in our sample met criteria for CFS.
We compared demographic characteristics of OEF/OIF veterans with and without CFS using t-tests. The only difference found was OEF/OIF veterans with CFS were assessed later post-deployment. We next compared demographic characteristics of OEF/OIF veterans with CFS to our sample of Desert Shield/Desert Storm veterans with CFS again using t-tests. Compared to OEF/OIF veterans with CFS, our sample of Desert Shield/Desert Storm veterans were assessed earlier post-deployment, more likely to be female, and more likely to self-identify as white and less likely to identify as Latino. There were no significant differences in education or age (see Table 1).
Table 1.
Demographic characteristics
| OEF/OIF NO CFS (n=416) |
OEF/OIF CFS (n=119) |
GW CFS (n=100) |
|
|---|---|---|---|
| Age | 31.2 (9.2) | 32.4 (9.5) | 33.8 (8.2) |
| Years since deployment | 1.6 (1.7) | 2.1 (1.4)a | 6.0 (.94)b |
| Male | 87.3% | 82.4% | 70.0%b |
| Years of Education | 13.4 (1.7) | 13.4 (1.8) | 13.5 (1.7) |
| White | 33.3% | 36.1% | 66.0%b |
| Black | 20.9% | 17.6% | 20.0% |
| Latino | 31.0% | 31.9% | 7.0% b |
| Other | 8.9% | 9.2% | 6.0% |
GW= Desert Shield/Desert Storm, CFS=Chronic Fatigue Syndrome, OEF/OIF=Operation Enduring Freedom/Operation Iraqi Freedom
statistically significant difference between OEF/OIF NO CFS and OEF/OIF CFS
statistically significant difference between OEF/OIF CFS and GW CFS
PTSD
We examined the rates of PTSD among OEF/OIF veterans with CFS, OEF/OIF veterans without CFS and Desert Shield/Desert Storm veterans with CFS. Among OEF/OIF veterans without CFS, 23% had probable PTSD. Among OEF/OIF veterans with CFS, 65% had probable PTSD and among Desert Shield/Desert Storm veterans with CFS 43% had probable PTSD.
Symptoms
A series of logistic regression analyses was conducted to compare rates of physical symptoms between OEF/OIF veterans with and without CFS. By definition, OEF/OIF veterans who screened positive for CFS had a higher prevalence of all reported symptoms than those without CFS. We then compared rates of symptoms in OEF/OIF veterans with CFS to Desert Shield/Desert Storm veterans with CFS (see Table 2). Desert Shield/Desert Storm veterans with CFS were more likely to report fatigue after exercise, fever, swollen glands, sore throat, headaches and weakness. There were no significant differences in concentration, joint pain, poor sleep or muscle pain.
Physical and Mental Health Functioning
We completed one MANCOVA to determine differences in physical and mental health functioning among OEF/OIF veterans with and without CFS. As expected, OEF/OIF veterans with CFS reported worse functioning on all scales of the SF-36 as compared to OEF/OIF veterans without CFS (see Table 3). OEF/OIF veterans with CFS scored greater than one standard deviation below the mean on all scales of the SF-36, while OEF/OIF veterans without CFS scored within one standard deviation of the mean on all scales of the SF-36.
Table 3.
MANCOVA comparing functioning of OEF/OIF veterans with CFS to OEF/OIF veterans without CFS controlling for age and probable PTSD
| OEF/OIF No CFS (N=416) |
OEF/OIF CFS (N=119) |
F | P value | |
|---|---|---|---|---|
| SF-36 PCS | 48.7 | 39.4 | 61.3 | <.001 |
| SF-36 PF | 48.9 | 37.9 | 67.4 | <.001 |
| SF-36 RP | 47.9 | 35.0 | 68.1 | <.001 |
| SF-36 BP | 45.5 | 35.1 | 43.6 | <.001 |
| SF-36 GH | 46.0 | 34.0 | 72.3 | <.001 |
| SF-36 MCS | 42.7 | 26.7 | 47.1 | <.001 |
| SF-36 VT | 46.5 | 34.2 | 57.0 | <.001 |
| SF-36 SF | 41.6 | 26.5 | 60.8 | <.001 |
| SF-36 RE | 45.3 | 28.8 | 46.6 | <.001 |
| SF-36 MH | 43.4 | 28.7 | 61.3 | <.001 |
PCS=Physical Composite Score, MCS=Mental Composite Score, PF=Physical Function, RP=Role Physical, BP=Bodily Pain, GH=General Health, VT=Vitality, SF=Social Function, RE=Role Emotional, MH=Mental Health.
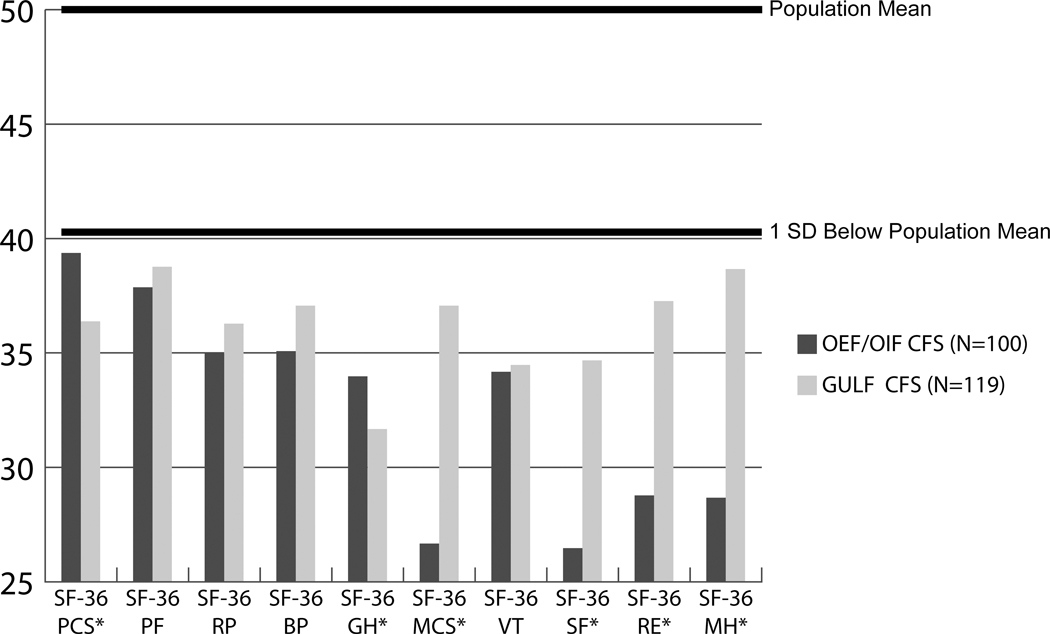
We performed a final MANCOVA to determine differences in physical and mental health functioning between OEF/OIF veterans with CFS and Desert Shield/Desert Storm veterans with CFS. On average, OEF/OIF veterans with CFS reported significantly poorer functioning on the mental composite scales, and on the social function, role emotional and mental health subscales. Desert Shield/Desert Storm veterans reported significantly poorer functioning on the physical composite scale and the general health function subscale. There were no differences in the physical function, role physical, body pain or vitality subscales (see Figure 1). Both Desert Shield/Desert Storm and OEF/OIF veterans scored greater than one standard deviation below the mean on all scales of the SF-36.
Figure 1.
Comparison of functioning between OEF/OIF veterans with CFS to Desert Shield/Desert Storm veterans with CFS. Adjusted SF-36 scores controlling for age and PTSD (higher scores indicate better functioning).
PCS=Physical Composite Score, MCS=Mental Composite Score, PF=Physical Function, RP=Role Physical, BP=Bodily Pain, GH=General Health, VT=Vitality, SF=Social Function, RE=Role Emotional, MH=Mental Health, CFS=Chronic Fatigue Syndrome, OEF/OIF=Operation Enduring Freedom, Operation Iraqi Freedom. *=significant difference between the groups
Discussion
As early as the US civil war, returning soldiers were described as having an irritable heart and reported to suffer from fatigue (Da Costa, 1871). In a review of US conflicts from the civil war to Desert Shield/Desert Storm, fatigue has been reported as a consistent problem in returning veterans (Hyams et al., 1996). Examination of physical symptoms among OEF/OIF veterans is still in its infancy and to our knowledge this is the first study to examine CFS. We found that CFS was high (17.6%) in our population of OEF/OIF veterans seeking treatment at a post-deployment clinic. Furthermore, OEF/OIF veterans with CFS had physical health functional impairments that are comparable to Desert Shield/Desert Storm veterans with CFS, but they had significantly worse mental health functioning.
The finding of high rates of CFS among OEF/OIF veterans is consistent with previous studies that show OEF/OIF veterans are self-reporting significant physical symptoms after deployment (C. Hoge et al., 2007; L. T. McAndrew, RF; Osinubi, OY; Jasien, JV; Quigley, KS, 2012; Quigley et al., 2012; Smith et al., 2014). The current study addressed limitations in previous studies by using a clinician administered medical examination. Many conditions can cause increases in physical symptoms. This study is the first to find that some OEF/OIF veterans are experiencing multi-symptom physical symptoms that are not better explained by other conditions. We found the prevelance of OEF/OIF veterans with CFS in a post-deployment clinic is 17%. Previous studies have used different definitions to capture these chronic physical symptoms (e.g., Chronic Multi-symptom Illness) and have not adequately excluded for potential comorbid medical conditions. Further research is needed to better understand the prevelance of wide-spread physical symptoms that are not caused by another medical condition outside of a treatment seeking context.
We also examined the functional impairment of veterans with CFS seen at our clinic. We found that the level of functional impairment is greater than one standard deviation below the mean. Thus the level of functional impairment is similar to or worse than the level of functional impairment found among individuals with other significant chronic illnesses such as cancer (Sprangers et al., 2000). Further, we found the level of functional impairment is similar to the level of Desert Shield/Desert Storm veterans with CFS. Desert Shield/Desert Storm veterans continue to have CFS and associated disability 25 years after the end of the war with few efficacious treatments. Our results are consistent with one other study to examine the functional impairment among OEF/OIF veterans with chronic physical symptoms. McAndrew et al., (In Press) examined the level of functional impairment among OEF/OIF veterans not seeking treatment and found those who screened positive for severe chronic multi-symptom illness also had functional impairment that was greater then one standard deviation below the mean. Together these studies suggest that some veterans returning from OEF/OIF are experiencing debilitating physical symptoms.
In contrast to the relatively few studies on CFS or multiple physical symptoms in OEF/OIF Veterans, there have been many published reports of the “signature illness” of OEF/OIF, post-traumatic stress disorder and mild traumatic brain injury (e.g. (Ramchand et al., 2010)). This may be due to physical symptoms being attributed to PTSD or mTBI by clinicians and/or Veterans. Although the higher rates of PTSD likely contribute to the poorer physical functioning for veterans from the current conflict, controlling for PTSD did not fully account for the impairment in physical functioning suggesting that PTSD is not the only variable contributing to this finding. Further, a growing literature suggests that the misattribution of symptoms to mTBI may be common (Uomoto & Williams, 2009) and cause diagnostic confusion (Hoge, Goldberg, & Castro, 2009).
The strength of this study was our unique ability to compare a noncomtemporaneous sample of OEF/OIF and Desert Shield/Desert Storm veterans both assessed soon after their deployment; however our study was not without limitations. These include a relatively small sample of Veterans seeking treatment at a VA tertiary care clinic. Like all clinical studies, the rate of CFS found in this study would not be the same rate as found in a nationally representative sample. Further there were differences between our two cohorts which may contribute to differences between our samples, including referrals, inclusion and exclusion criteria, different clinicians, years post-deployment and measurement of PTSD and health function. It is impressive that with all of the limitations we found striking similarities between the samples in regards to physical health function. Further, our data suggests a potentially understudied problem among OEF/OIF Veterans deserving of additional study. This study was not designed to examine the cause of CFS in either Desert Shield/Desert Storm veterans or OEF/OIF veterans. We did find a difference in the pattern of symptoms between the cohorts. Veterans from the Desert Shield/Desert Storm reported a greater prevalence of symptoms often seen in infectious or acute illness (sore throat, swollen glands and fatigue after exercise). OEF/OIF Veterans had worse mental health function.
In conclusion, our data suggests that OEF/OIF veterans seeking specialized post-deployment care are experiencing a high rate (17.6%) of chronic fatigue syndrome that are not accounted for by another medical or psychiatric condition. In addition, our study found both OEF/OIF veterans with CFS and Desert Shield/Desert Storm veterans with CFS have similar levels of physical functional impairment. It is clear that with over 2 million soldiers sent to the Afghanistan and Iraq theatres, these levels of functional impairment will require additional clinical and research resources to better understand both the sources of poor functioning and how to intervene to rehabilitate the functioning of these veterans.
Acknowledgments
Funding sources are US Department of Veterans Affairs, Veterans Health Administration, Office of Public Health and the Office of Research Development. LMM is funded by a Career Development Award from the Health Services Research Department (HSR&D) of the Veterans Affairs: CDA 13–017. The views expressed are those of the authors and do not reflect the official policy or position of the U.S. Government. The Department of Veterans Affairs had no input into the design of the research, the analyses, the interpretation of data, or decision to submit the paper.
Footnotes
Competing Interests: The authors have no competing interests to report.
Contributor Information
Lisa M. McAndrew, Department of Veterans Affairs, NJ War Related Illness and Injury Study Center University at Albany, Department of Educational and Counseling Psychology
Helena K. Chandler, Department of Veterans Affairs, NJ War Related Illness and Injury Study Center 385 Tremont Ave, East Orange, NJ 07081
Jorge M. Serrador, Department of Veterans Affairs, NJ War Related Illness and Injury Study Center 385 Tremont Ave, East Orange, NJ 07081 New Jersey Medical School-University of Medicine & Dentistry of NJ.
Karen S. Quigley, Interdisciplinary Affective Science Laboratory, Northeastern University, 235 Nightingale Hall, Boston, MA 02115 Department of Veterans Affairs, Bedford Memorial Hospital, 200 Springs Road, Bedford, MA.
Benjamin H. Natelson, Albert Einstein College of Medicine and Pain & Fatigue Study Center, Beth Israel Medical Center, NY, NY
Gudrun Lange, Department of Veterans Affairs, NJ War Related Illness and Injury Study Center 385 Tremont Ave, East Orange, NJ 07081 New Jersey Medical School-University of Medicine & Dentistry of NJ.
References
- Bates DW, Schmitt W, Buchwald D, Ware NC, Lee J, Thoyer E, . . . Komaroff AL (1993). Prevalence of fatigue and chronic fatigue syndrome in a primary care practice. Arch Intern Med, 153(24), 2759–2765. [PubMed] [Google Scholar]
- Blanchard MS, Eisen SA, Alpern R, Karlinsky J, Toomey R, Reda DJ, . . . Kang HK (2006). Chronic multisymptom illness complex in Gulf War I veterans 10 years later. Am J Epidemiol, 163(1), 66–75. doi: 10.1093/aje/kwj008 [DOI] [PubMed] [Google Scholar]
- Buchwald D, Umali P, Umali J, Kith P, Pearlman T, & Komaroff AL (1995). Chronic fatigue and the chronic fatigue syndrome: prevalence in a Pacific Northwest health care system. Ann Intern Med, 123(2), 81–88. [DOI] [PubMed] [Google Scholar]
- Da Costa J (1871). On irritable heart: A clinical study of a form of functional cardiac disorder and its consequences. Am J Med Sci, 61, 17–52. [Google Scholar]
- Fukuda K, Nisenbaum R, Stewart G, Thompson WW, Robin L, Washko RM, . . . Reeves WC (1998). Chronic multisymptom illness affecting Air Force veterans of the Gulf War. JAMA, 280(11), 981–988. [DOI] [PubMed] [Google Scholar]
- Fukuda K, Straus SE, Hickie I, Sharpe MC, Dobbins JG, & Komaroff A (1994). The chronic fatigue syndrome: a comprehensive approach to its definition and study. International Chronic Fatigue Syndrome Study Group. Ann Intern Med, 121(12), 953–959. [DOI] [PubMed] [Google Scholar]
- Hoge, Goldberg H, & Castro C (2009). Care of war veterans with mild traumatic brain injury--flawed perspectives. N Engl J Med, 360(16), 1588–1591. doi: 10.1056/NEJMp0810606 [DOI] [PubMed] [Google Scholar]
- Hoge C, Terhakopian A, Castro C, Messer S, & Engel C (2007). Association of posttraumatic stress disorder with somatic symptoms, health care visits, and absenteeism among Iraq war veterans. American Journal of Psychiatry, 164(1), 150–153. [DOI] [PubMed] [Google Scholar]
- Hyams KC, Wignall FS, & Roswell R (1996). War syndromes and their evaluation: from the US Civil War to the Persian Gulf War. Annals of Internal Medicine, 125(5), 398–405. [DOI] [PubMed] [Google Scholar]
- Hyer L, Davis H, Boudewyns P, & Woods MG (1991). A short form of the Mississippi Scale for Combat-Related PTSD. J Clin Psychol, 47(4), 510–518. [DOI] [PubMed] [Google Scholar]
- Iverson KM, Pogoda TK, Gradus JL, & Street AE (2013). Deployment-related traumatic brain injury among Operation Enduring Freedom/Operation Iraqi Freedom veterans: associations with mental and physical health by gender. J Womens Health, 22(3), 267–275. doi: 10.1089/jwh.2012.3755 [DOI] [PubMed] [Google Scholar]
- Jason LA, Richman JA, Rademaker AW, Jordan KM, Plioplys AV, Taylor RR, . . . Plioplys S (1999). A community-based study of chronic fatigue syndrome. Arch Intern Med, 159(18), 2129–2137. [DOI] [PubMed] [Google Scholar]
- Jones D, Kazis L, Lee A, Rogers W, Skinner K, Cassar L, . . . Hendricks A (2001). Health status assessments using the Veterans SF-12 and SF-36: methods for evaluating otucomes in the Veterans Health Administration. J Ambul Care Manage, 24(3), 68–86. [DOI] [PubMed] [Google Scholar]
- Jones E, Hodgins-Vermaas R, McCartney H, Everitt B, Beech C, Poynter D, . . . Wessely S (2002). Post-combat syndromes from the Boer war to the Gulf war: a cluster analysis of their nature and attribution. Bmj, 324(7333), 321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kang HK, Natelson BH, Mahan CM, Lee KY, & Murphy FM (2003). Post-traumatic stress disorder and chronic fatigue syndrome-like illness among Gulf War veterans: a population-based survey of 30,000 veterans. Am J Epidemiol, 157(2), 141–148. [DOI] [PubMed] [Google Scholar]
- Kazis LE, Liang MH, Lee A, Ren XS, Phillips CB, Hinson M, . . . Tompkins R (2002). The development, validation, and testing of a health outcomes burn questionnaire for infants and children 5 years of age and younger: American Burn Association/Shriners Hospitals for Children. J Burn Care Rehabil, 23(3), 196–207. [DOI] [PubMed] [Google Scholar]
- Kazis LE, Miller DR, Clark JA, Skinner KM, Lee A, Ren XS, . . . Ware JE Jr. (2004). Improving the response choices on the veterans SF-36 health survey role functioning scales: results from the Veterans Health Study. J Ambul Care Manage, 27(3), 263–280. [DOI] [PubMed] [Google Scholar]
- Lange G, McAndrew L, Ashford JW, Reinhard M, Peterson M, & Helmer DA (2013). War Related Illness and Injury Study Center (WRIISC): a multidisciplinary translational approach to the care of Veterans with chronic multisymptom illness. Mil Med, 178(7), 705–707. doi: 10.7205/MILMED-D-13-00053 [DOI] [PubMed] [Google Scholar]
- McAndrew LMH,DA; Phillips LA; Ray K; Quigley K (In Press). Operation Enduring Freedom Operation Iraqi Freedom report symptoms consistent with Chronic Multi-Symptom Illness one year after deployment Journal of Rehabilitation Research and Development. [DOI] [PubMed] [Google Scholar]
- McAndrew LT,RF; Osinubi OY; Jasien JV; Quigley KS (2012). Environmental exposure and health of Operation Enduring Freedom/Operation Iraqi Freedom veterans. J Occup Environ Med, 54(6), 665–669. doi: 10.1097/JOM.0b013e318255ba1b [DOI] [PubMed] [Google Scholar]
- McCauley LA, Joos SK, Barkhuizen A, Shuell T, Tyree WA, & Bourdette DN (2002). Chronic fatigue in a population-based study of Gulf War veterans. [Research Support, U.S. Gov’t, Non-P.H.S.]. Arch Environ Health, 57(4), 340–348. doi: 10.1080/00039890209601419 [DOI] [PubMed] [Google Scholar]
- Medicine I. o. (2013). Gulf War and Health: Treatment for Chronic Multisymptom Illness [PubMed] [Google Scholar]
- Orsillo S (2001). Measures for acute stress disorder and posttraumatic stress disorder. In Antony MOSM (Ed.), Practitioner’s guide to empirically based measures of anxiety (pp. 255–307). New York: Kluwer Academic/Plenum. [Google Scholar]
- Pollet C, Natelson BH, Lange G, Tiersky L, DeLuca J, Policastro T, . . . Kipen H (1998). Medical evaluation of Persian Gulf veterans with fatigue and/or chemical sensitivity. J Med, 29(3–4), 101–113. [PubMed] [Google Scholar]
- Quigley KS, McAndrew LM, Almeida L, D’Andrea EA, Engel CC, Hamtil H, & Ackerman AJ (2012). Prevalence of environmental and other military exposure concerns in Operation Enduring Freedom and Operation Iraqi Freedom veterans. J Occup Environ Med, 54(6), 659–664. doi: 10.1097/JOM.0b013e3182570506 [DOI] [PubMed] [Google Scholar]
- Ramchand R, Schell TL, Karney BR, Osilla KC, Burns RM, & Caldarone LB (2010). Disparate prevalence estimates of PTSD among service members who served in Iraq and Afghanistan: possible explanations. J Trauma Stress, 23(1), 59–68. doi: 10.1002/jts.20486 [DOI] [PubMed] [Google Scholar]
- Reyes M, Nisenbaum R, Hoaglin DC, Unger ER, Emmons C, Randall B, . . . Reeves WC (2003). Prevalence and incidence of chronic fatigue syndrome in Wichita, Kansas. Arch Intern Med, 163(13), 1530–1536. doi: 10.1001/archinte.163.13.1530 [DOI] [PubMed] [Google Scholar]
- Smith TC, Powell TM, Jacobson IG, Smith B, Hooper TI, Boyko EJ, & Gackstetter GD (2014). Chronic multisymptom illness: a comparison of Iraq and Afghanistan deployers with veterans of the 1991 Gulf War. Am J Epidemiol, 180(12), 1176–1187. doi: 10.1093/aje/kwu240 [DOI] [PubMed] [Google Scholar]
- Sprangers MA, de Regt EB, Andries F, van Agt HM, Bijl RV, de Boer JB, . . . de Haes HC (2000). Which chronic conditions are associated with better or poorer quality of life? J Clin Epidemiol, 53(9), 895–907. [DOI] [PubMed] [Google Scholar]
- Uomoto JM, & Williams RM (2009). Post-acute polytrauma rehabilitation and integrated care of returning veterans: toward a holistic approach. Rehabil Psychol, 54(3), 259–269. doi: 10.1037/a0016907 [DOI] [PubMed] [Google Scholar]
- Weathers FL,B (1993). The PTSD Checklist (PCL): Reliability, validity and diagnostic utility. Paper presented at the Annual Meeting of the International Society for Traumatic Stress Studies, San Antonio, TX. [Google Scholar]
- Wessely S, Chalder T, Hirsch S, Wallace P, & Wright D (1997). The prevalence and morbidity of chronic fatigue and chronic fatigue syndrome: a prospective primary care study. Am J Public Health, 87(9), 1449–1455. [DOI] [PMC free article] [PubMed] [Google Scholar]