Abstract
Purpose
The aim of this study was to explore the status of quality of life between the ages 40–59 in relation to presbyopia and dry eye.
Methods
Near add power and preferred contact lens power were examined in 219 participants at three clinics. 2000 participants completed a web-based survey on presbyopic symptoms, symptomatic dry eye, sleep quality, and subjective happiness.
Results
Mean preferred corrected visual acuity was less than 20/20 in women (vs men, P<0.01) who were more often prescribed under-corrected contact lenses, whereas men preferred full correction. According to the annual progression rate of near add power in men (0.1468D/year), the estimated difference in presbyopia progression between men and women was 0.75 years in the right eye, and 1.69 years in the left eye, implying men might suffer presbyopia earlier than women due to higher myopic power of daily use contact lenses. The web-based survey revealed that men reported lower subjective happiness than women (P<0.001) and earlier onset of presbyopic symptoms by 1.1–1.7 years (P<0.05). Men received their first reading glasses 0.8 years earlier than women (P = 0.066). Multiple regression analysis demonstrated that awareness of presbyopic symptoms, visual burden, and dry eyes were significantly correlated with poor sleep quality and subjective happiness.
Conclusion
Presbyopia and dry eye were significantly associated with sleep quality and subjective happiness in middle-adulthood.
Introduction
Many middle-aged people may suffer presbyopia and dry eye. Presbyopia continuously progresses with aging and eventually requires most people to use near visual aids, in contrast to cataract and glaucoma, other common organic causes of loss of vision, that are treated by medical or surgical intervention [1–3]. Difficulty focusing is usually first experienced during the 30s to 40s depending on refraction and other visual factors in daily life and work. Most people initially adapt by increasing the distance from an object or removing myopic glasses. However, blurring, headache, eye pain, eye fatigue, neck pain, shoulder pain, and even productivity loss, often accompany difficulty focusing when it has become constant [4–8]. In the modern digital society, smartphone and computer displays with small letters are widely used across all generations, and the large impact of presbyopia on the economy and quality of life has emerged as a social problem in middle adulthood [9].
Dry eye disease (DED) is another prevalent geriatric eye disease, and may worsen with digital displays due to decreased blinking [10] and emitted blue light [11, 12]. DED is predominant in women, affecting quality of life (QOL), sleep, depression, and happiness [13–16]. QOL may worsen with presbyopia since difficulty focusing on near objects is a considerable burden in daily life. Recent survey results described a significant association between presbyopia and DED even after matching age/gender and comorbidity conditions [17] indicating these two disorders may concordantly worsen QOL. Middle-aged women more often work in professions in indoor settings that require near vision. Indeed, previous studies demonstrated women needed stronger near add power (the minimal additional power required to achieve sufficient near acuity under full distance refractive correction) than men [6–8]. Therefore, women may be more affected by presbyopia than men.
The deterioration of QOL due to ocular diseases could be measured with validated questionnaires. The Subjective Happiness Scale (SHS) [18, 19] has been used for DED, LASIK, and cataract surgery [20–22], and is closely associated with longevity [23]. The Pittsburg Sleep Quality Index (PSQI) is a sophisticated sleep quality scale [24, 25] assessing sleep disorders, which are strongly associated with life expectancy, cardiovascular disease, metabolic disorders, and hypertension [26–28]. However, to date, few studies described QOL in presbyopia [29].
The aim of this study was to explore the QOL in middle adulthood in relation to presbyopia and DED. Two complementary studies were carried out. The clinical study was conducted to determine the most recent preference of correction with contact lenses in middle adulthood in a visit to an vision care eye clinic. Near add power and preferred contact lens power for daily use were examined. The results of full ocular examinations by board-certified ophthalmologists and certified technicians would serve as a current clinical baseline data of presbyopia in middle adulthood. To further assess impact of presbyopia and DED on QOL, the web-based survey was performed to measure QOL-associated major indices including subjective happiness and sleep quality. Special attention was paid to sex differences in the onset and severity of presbyopia symptoms and burden.
Materials and methods
Clinical study
Study design and participants
This study was a clinic-based, retrospective, cross-sectional study involving healthy subjects attending the Jiyugaoka Ekimae Eye Clinic, Komoro Kosei General Hospital, and Tsukuba Central Hospital. The Institutional Review Board and Ethics Committee of the Tsukuba Central Hospital approved this study (approved on December 12, 2014, permission number 141201) and Jiyugaoka Ekimae Eye Clinic was approved as a collaborating institute of Tsukuba Central Hospital. Participants were recruited from April 2015 to March 2017 in these two institutions. The Institutional Review Board and Ethics Committee of Komoro Kosei General Hospital (approved on July 4, 2016, permission number 2802) approved this study and participants were recruited from July 2016 to March 2017. This study was carried out in accordance with the Declaration of Helsinki. The need for consent was waived by the Institutional Review Board. Consecutive patients were analyzed during the study period. Consecutive patients were analyzed during the study period.
This clinical study was a retrospective chart review since all examinations were routinely performed for contact lens prescription in participating clinics and hospitals. Every patient completed a health check sheet that included medical and family history before examination for contact lens prescription.
Inclusion and exclusion criteria
Participants aged 40 to 59 years visiting for contact lens prescription with bilateral phakic eyes and best-corrected visual acuity above 20/20 were included in the study. Individuals were excluded if they had glaucoma, vitreoretinal disease, any ocular surgery in the previous month, or acute ocular disease in the previous two weeks.
Ophthalmological examinations
Board-certified ophthalmologists examined all patients and excluded subjects with major age-related eye diseases, including cataract, glaucoma, and macular diseases. Ophthalmological evaluation of participants consisted of best-corrected visual acuity (Vision Chart, SSC-370R, Nidek Co., Ltd., Gamagori, Japan), autorefractometry (TonorefTM II, Nidek Co., Ltd., Aichi, Japan), slit-lamp biomicroscopy, funduscopy, and intraocular pressure measurements (TonorefTM II, Nidek Co., Ltd., Aichi, Japan). Binocular near add power was measured by a blinded examiner at a distance of 30 cm using a Bankoku near-acuity chart (Handaya Inc., Tokyo, Japan) or an automatic optometry system (AOS-700R; Nidek Co., Ltd., Gamagori, Japan) [30]. After determining the patient’s distance refractive correction, the minimal additional power required to achieve near acuity above 20/25 at 30 cm was measured in 0.25 D increments, and was recorded as near add power. Contact lens over-refraction was performed to determine participants preferred corrective power. Visual acuity for distance and near was measured using a decimal chart and converted to LogMAR for analysis. DED-related examinations consisted of tear break-up time, corneal staining test, and Schirmer test. They were carried out according to standard procedures [31–33]. The BUT was measured using wet fluorescein filter paper (Ayumi Pharmaceutical, Tokyo, Japan), applied at the lower lid margin. The fluorescein strip was wet with saline and the excess was flicked off. It was viewed with a suitable light source and yellow filter [34]. The BUT was defined as the time interval between the third blink and the appearance of the first dark spot in the cornea and was measured using a stopwatch. This was calculated with the mean of three measurements. A corneal staining score was determined to grade corneal epitheliopathy; graded at 0–2 for severity and area. Schirmer’s test was performed without topical anaesthesia. Strips of filter paper (Whatman No. 41; Showa Yakuhin Kako, Tokyo, Japan) were placed for 5 min at the outer third of the temporal lower conjunctival fornix, with the subject blinking spontaneously. The strips were then removed, and the length of the filter paper wetted by the spontaneous blinks was recorded (mm). Examination rooms were kept at 21–24 degrees centigrade and 40–60% humidity according to recommendation of Japanese Ministry of Health and Labor.
Web-based survey
Ethical approval and participant recruitment
The web-based survey was approved by the Institutional Review Board and Ethics Committee of the Keio University (Approved on July 29, 2016, permission number 2015–0280) and was carried out in accordance with the Declaration of Helsinki. In charge of the survey was Ipsos Incorporated (Tokyo, Japan), a company that is certified in the protection of personal information, and launched a survey website to recruit 2,000 people adjusted for age and gender. All subjects aged 40 to 59 years who used the web survey panel (Research Panel Incorporated, Tokyo, Japan) were asked to participate in this study. Entry requirement to the survey was age and sex with potential presbyopia at the age of 40–59. Among 1,000,000 panels from the general public in Japan, age-matched participants were randomly selected, and invitation mails were sent without introducing the aim of the study. The first 2,000 participants who satisfied requirements were enrolled. The study took place from April 7 to April 13, 2017. Participants received no money, but reward points which could be used on the panel website as compensation.
Consent was waived by the ethics committee for this opt-out study. Instead, the first screen of the app stated that this was a research app and all the data obtained would be used for the study. It was also clearly stated that the participation was totally voluntary and could be withdrawn anytime, and their anonymity was preserved. Only after they pushed the agree button at the bottom of the screen, they could proceed to the next screen of the app. The participants were also provided with the contact information about the study and the inquiry form from the app.
Questionnaires
Participants were asked to complete two questionnaires on major indices for quality of life; happiness was evaluated with the validated Japanese version of SHS [19] and sleep quality was measured with a validated Japanese version of PSQI [25]. The SHS is a four-item questionnaire of subjective global happiness; each item requires patients to rate the statements on a 7-point Likert scale. The possible scores range from 1 to 7, and higher values corresponded to higher subjective happiness. The PSQI is comprised of seven subscales that evaluate sleep quality, including subjective sleep quality, daytime dysfunction, sleep latency, sleep duration, habitual sleep efficacy, sleep disturbances, and use of sleep medications; the score was calculated according to separate algorithms and analyzed. Each component was scored on a scale of 0 to 3, with 3 indicating the worst score. The highest possible global score is 21, and the normal range on the PSQI is less than 6. Questions on presbyopia included awareness and impact of difficulties focusing, age of first awareness of difficulty focusing, and age of first vision aid for near. The answers could include reading glasses, progressive spectacle lenses, monovision contact lenses, and multifocal contact lenses in reference to their uncorrected vision. (Tables 1 and 2). The questions on awareness discerned between a sensation of difficulty focusing without concerns and the sensation of difficulty focusing that affected daily life, henceforth referred to as awareness and impact. The severity of visual burden was asked for near, middle-distance, and far vision (1: No burden without blurred vision, 2: No burden with blurred vision, 3 Burden with blurred vision). A short dry eye questionnaire [35] was used to detect symptomatic dry eye with three questions that are widely used in epidemiological studies. The content of the short questionnaire included three questions: (1) How often do your eyes feel dry (not wet enough)?, (2) How often do your eyes feel irritated?, and (3) Have you ever been diagnosed (by a clinician) as having dry eye syndrome?
Table 1. Survey results of quality of life indices and ocular symptoms.
| Men (N = 1006) | Women (N = 994) | P-value* | |
|---|---|---|---|
| Age | 49.0 ± 5.7 | 49.0 ± 5.7 | 0.891 |
| SHS | 4.16 ±1.0 | 4.38 ± 1.1 | < 0.001* |
| PSQI | 5.46 ± 2.92 | 5.32 ± 2.88 | 0.293 |
| Symptomatic DED (%) | 28.4 | 42.7 | < 0.001* |
| Awareness of difficulty focusing (%) | 71.6 | 69.8 | 0.376 |
| Impact of difficulty focusing (%) | 47.5 | 46.6 | 0.162 |
| Near correction (%) | 26.3 | 26.6 | 0.879 |
| Burden for near visionA | 1.59 ± 0.85 | 1.51 ± 0.79 | 0.027* |
| Burden for middle-distance visionA | 1.41 ± 0.72 | 1.40 ± 0.71 | 0.704 |
| Burden for far visionA | 1.47 ± 0.77 | 1.50 ± 0.71 | 0.445 |
*P<0.05, chi-squared test or t-test as appropriate.
A1 = No burden without blurred vision; 2 = No burden with blurred vision; 3 = Burden with blurred vision. Abbreviations; SHS, Subjective Happiness Scale, PSQI, Pittsburg Sleep Quality Index global score.
Table 2. Age of first awareness of difficulty focusing and first reading glasses.
| Symptom and mean age (y) | Men | Women | ⊿ | P-value* |
|---|---|---|---|---|
| Hard to see small letters up close | 43.9± 7.4 (6–59) | 45.6± 7.0 (7–59) | 1.7 | < 0.001* |
| Hard to focus on small object up close | 44.1± 7.7 (6–58) | 45.5±6.6 (10–57) | 1.4 | 0.010* |
| Hard to focus when changing focus from distance to near and near to distance | 43.8±7.1 (10–56) | 45.1 ±6.9 (14–57) | 1.3 | 0.040* |
| See better when I increase distance from the object | 45.6±4.9 (23–58) | 46.7±4.8 (14–58) | 1.1 | 0.021* |
| First reading glasses | 47.4±5.2 (30–58) | 48.2±4.4 (30–57) | 0.8 | 0.066 |
*P<0.05, t-test. min and max values in parenthesis.
Statistical analysis
The sample size was calculated with a 0.05 margin of error, 95% confidence interval. Effect size and standard deviation were derived from a previous clinical study. For example, an effect size of 0.16D was identified in a previous study of accommodation [36]. Thus, an appropriate sample size for [preferred corrective power of contact lens–full correction power for far OD] was 5, calculated with a 0.05 margin of error, 95% confidence interval, effect size of 0.16, and standard deviation 0.088. Regarding the web-based study, an effect size of 0.68 in SHS was identified in a previous study of SHS [22]. An appropriate sample size for SHS was 950, calculated with a 0.05 margin of error, 95% confidence interval, an effect size of 0.68, and standard deviation 1.1.
Where appropriate, data are given as mean ± standard deviation since the obtained data were normally distributed using the Kolmogorov-Smirnov test. The visual acuity was converted to the logMAR. The difference of optical parameters and responses between men and women were analyzed using unpaired t-test and chi-squared test as appropriate. Correlations were evaluated using a standardized partial regression coefficient. Regression analysis was performed to identify the factors affecting SHS and PSQI by simple correlation. Multiple regression analysis was then performed to determine the predictors of SHS and PSQI, and possible predictors (responses and presence) of DED. All analyses were performed using StatFlex (Atech, Osaka, Japan) with p < 0.05 considered significant.
Results
Clinical study
One hundred and six male and 113 female age-matched participants were enrolled in the clinical study. Refractive parameters were similar in both sexes (Table 3 and S1 Data). The clinical study showed that the distribution of refraction was high myopia (≤ -6.00D)(33.0%), mild myopia (> -6.00D)(61.3%), and hyperopia (5.7%) in men and high myopia (36.3%), mild myopia (61.9%), and hyperopia (1.8%) in women. During the examination for prescription of contact lenses for daily use, many women did not prefer best corrected power for their contact lens, and were prescribed with under-corrected power compared with men (men vs women, P = 0.003 in the right eye and P = 0.007 in the left eye). Scatter plots of near add power indicated a similar slope of the regression line in both sexes (Fig 1). There were 47 patients with zero diopter add power and all were myopic. Mean age was 43.3±2.9 (40–49) in men (n = 21) and 43.4±3.3 (40–54) in women (n = 26), respectively (P = 0.922, t-test). The spherical equivalent in the right eye was −4.81±2.10D (−1.75-−8.50D) in men and −4.46±2.15D (−0.12-−8.25D) in women, respectively (P = 0.580, t-test). All DED-related parameters were predominant in women.
Table 3. Refraction, near add power, and dry eye-related parameters in men and women.
| Men (N = 106) | Women (N = 113) | P-value* | |
|---|---|---|---|
| Age | 48.1 ±5.1 | 48.1±4.9 | 0.828 |
| Near add power (D) | 1.28±0.89 | 1.30±0.86 | 0.841 |
| Spherical equivalent OD (D) | −4.73 ±3.28 | −4.48±3.05 | 0.536 |
| Spherical equivalent OS (D) | −4.48±3.05 | −4.81 ±2.71 | 0.397 |
| Astigmatism OD (D) | 0.48±0.52 | 0.55±0.62 | 0.378 |
| Astigmatism OS (D) | 0.52±0.61 | 0.54 ±0.62 | 0.827 |
| Preferred corrective power of contact lens–full correction power for far OD (D) | 0.37 ±0.58 (+2.75 - −0.75) | 0.48 ± 0.50 (+2.50 - −0.5) | 0.192 |
| Preferred corrective power of contact lens–full correction power for far OS (D) | 0.26 ±0.51 (+1.25 - −0.75) | 0.51 ±0.57 (+3.00 - −1.00) | 0.002* |
| Preferred visual acuity with contact lens OD | −0.007±0.071 | −0.041 ±0.088 | 0.003* |
| Preferred visual acuity with contact lens OS | −0.008 ±0.077 | −0.038±0.082 | 0.007* |
| DED-related parameters | |||
| Tear break-up time (%, ≤5s) | 31.2 | 55.4 | < 0.001* |
| Corneal staining score | 0.136±0.42 | 0.292±0.54 | 0.019* |
| Schirmer test (%, ≤5mm) | 0 | 16.7 | <0.001* |
| Dry eye medication (%) | 28.9 | 75.3 | < 0.001* |
*P<0.05, chi-squared test or t-test as appropriate. DED, dry eye disease.
Fig 1. Scatter plots of near add power and age.
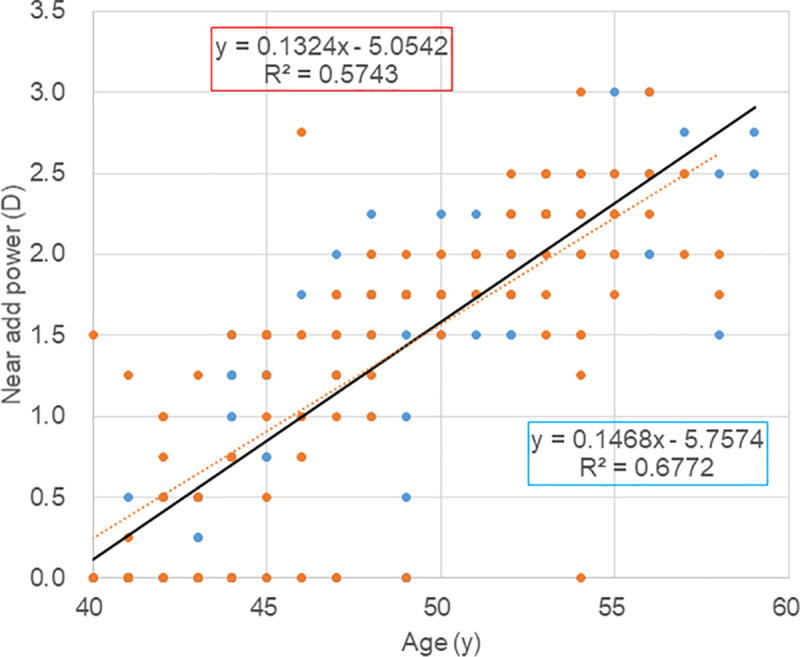
Annual progression of near add power was similar in men (black circle, solid regression line) and women (red triangle, dotted regression line). Symbol overlap may not accurately represent the number of participants. The number of zero near power cases was 21 men and 26 women with no difference. It is also indicated by similar regression lines of both groups.
Web-based study
The web-based survey revealed that the prevalence of awareness of difficulty focusing and the proportion of near correction was similar in both sexes (Table 1 and S2 Data). In contrast, burden with near vision was more serious in men (1.59±0.85) than women (1.51±0.79, P = 0.027). SHS was worse in men (4.16±1.00) than women (4.38±1.10; P< 0.001) and PSQI (5.46±2.92 for men and 5.32±2.88 for women) was similar (P = 0.293). Graphic presentation of the prevalence of symptoms and visual burden demonstrated that approximately 38% of participants already noticed difficulty focusing by the age of 40 years (Fig 2). The proportion of awareness of presbyopia was greater than that of impact across all ages surveyed. Despite an age-dependent increase of awareness of difficulty focusing, the proportion of near correction was very low until age 47, and then increased steeply. The severity of burden with near vision was apparently age-dependent, and burden with middle-distance vision were constant until slowing after age 48, whilst burden with far vision were constant across all ages surveyed.
Fig 2. Prevalence of symptoms and burden with vision, and the proportion of near correction.
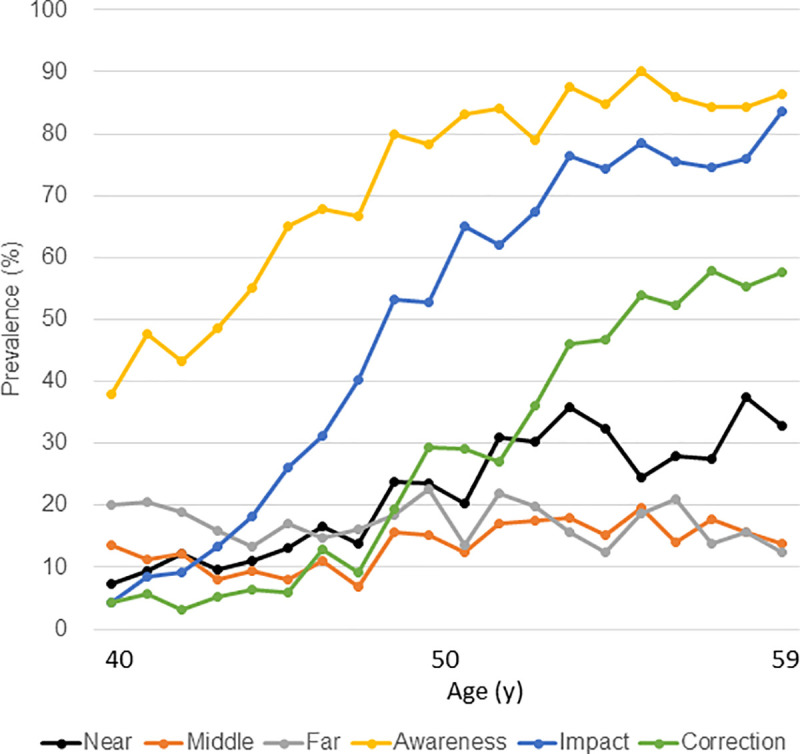
The proportion of awareness of presbyopia was greater than that of impact across all ages surveyed. Awareness of difficulty focusing was age-dependent. The proportion of near correction was very low until age of 47 and then increased steeply. The severity of burden with near vision was apparently age-dependent, and burden with middle-distance vision were constant until increasing after age of 48, whilst burden with far vision was constant across all ages surveyed. Symbols and abbreviations: Near (black), burden with near vision; Middle (red), burden with middle-distance vision; Far (grey), burden with far vision; Awareness (orange), awareness of difficulty focusing; Impact (blue), reported impact of difficulty focusing; Correction (green), near correction.
The prevalence of symptomatic DED was much greater in women than men (P<0.001). The onset of men’s near vision symptoms was earlier by 1.1–1.7 years (P<0.05; Table 2). The mean age of men’s first reading glasses was 0.8 years earlier than in women (P = 0.066, 47.4 years vs 48.2 years). Eleven men and 7 women had their first reading glasses before age 40. Eight (44.4%) of them were hyperopic, whereas 13.7% of all participants were hyperopic. The duration from earliest awareness of symptoms to first reading glasses was 2.6 years in men and 3.1 years in women.
Simple regression analysis of SHS and PSQI revealed male sex, visual burden, and no near correction was correlated with low SHS, whereas presbyopic symptoms and visual burden were correlated with poor PSQI (Tables 4 and 5). Although the results of DED and presbyopia were comparable, the presence of symptomatic DED was more strongly correlated with SHS and PSQI than presbyopic parameters. Multiple regression analysis with visual symptoms demonstrated male sex was the strongest factor for low SHS (P<0.001) and male sex was also the strongest factor in the multiple regression analysis with visual burden for low SHS (P<0.001). Regarding PSQI, multiple regression analysis with visual symptoms demonstrated awareness of difficulty focusing was only significantly correlated with poor PSQI (P<0.001) after adjustment for age and sex, and multiple regression analysis with visual burden demonstrated significant correlation with poor PSQI (P<0.001).
Table 4. Regression analysis for happiness and sleep.
| AHappiness | BSleep | |||
|---|---|---|---|---|
| Parameters for simple regression | beta | P* | beta | P* |
| Age (y) | 0.069 | 0.002 | 0.020 | 0.371 |
| CSex | -0.104 | <0.001 | 0.023 | 0.293 |
| Awareness of difficulty focusing | -0.025 | 0.272 | 0.140 | <0.001 |
| Impact of difficulty focusing | 0.008 | 0.694 | 0.056 | 0.012 |
| Near correction | 0.052 | 0.020 | 0.032 | 0.156 |
| Burden with near vision | -0.066 | 0.003 | 0.115 | <0.001 |
| Burden with middle distance vision | -0.046 | 0.038 | 0.063 | 0.005 |
| Burden with far vision | -0.079 | <0.001 | 0.101 | <0.001 |
| Dry eye | -0.087 | <0.001 | 0.163 | <0.001 |
| Happiness | - | - | -0.384 | <0.001 |
| Sleep | -0.384 | <0.001 | - | - |
| Multiple regression, Model 1: Symptoms with focusing | ||||
| Age | 0.082 | 0.002 | -0.028 | 0.285 |
| Sex | -0.102 | <0.001 | 0.020 | 0.355 |
| Awareness of difficulty focusing | -0.050 | 0.048 | 0.151 | <0.001 |
| Impact of difficulty focusing | -0.039 | 0.200 | 0.002 | 0.939 |
| Near correction | 0.053 | 0.052 | -0.006 | 0.809 |
| Multiple regression, Model 2: Burden with focusing | ||||
| Age | 0.079 | <0.001 | 0.002 | 0.925 |
| Sex | -0.100 | <0.001 | 0.017 | 0.422 |
| Burden with near vision | -0.068 | 0.010 | 0.110 | <0.001 |
| Burden with far vision | -0.073 | 0.006 | 0.095 | <0.001 |
*P<0.05, Standardized partial regression coefficient. A: Subjective happiness scale (0 (unhappy)-7 (happy)), B: Pittsburg Sleep Quality Index global score (higher score refers to poor sleep), C: Men = 1, Women = 0.
Table 5. Regression analysis for happiness and sleep stratified with sex.
| AHappiness | BSleep | |||||||
|---|---|---|---|---|---|---|---|---|
| Men | Women | Men | Women | |||||
| Parameters | beta | P* | beta | P* | beta | P* | beta | P* |
| Age (y) | −0.042 | 0.178 | −0.093 | 0.003* | 0.040 | 0.200 | 0.000 | 0.982 |
| Awareness of difficulty focusing | −0.071 | 0.032* | −0.035 | 0.295 | 0.166 | < 0.001* | 0.134 | < 0.001* |
| Impact of difficulty focusing | −0.037 | 0.310 | −0.038 | 0.318 | 0.074 | 0.044* | 0.052 | 0.172 |
| Near correction | 0.075 | 0.031* | −0.025 | 0.490 | 0.005 | 0.878 | 0.053 | 0.135 |
| Burden with near vision | −0.070 | 0.032* | −0.051 | 0.119 | 0.148 | < 0.001* | 0.109 | 0.001* |
| Burden with far vision | −0.085 | 0.007* | −0.065 | 0.039* | 0.154 | < 0.001* | 0.081 | 0.011* |
| Dry eye | −0.133 | < 0.001* | −0.074 | 0.019* | 0.163 | < 0.001* | 0.177 | < 0.001* |
| Happiness | – | – | – | – | −0.364 | < 0.001* | −0.404 | < 0.001* |
| Sleep | −0.364 | < 0.001* | −0.404 | < 0.001* | – | – | – | – |
| Multiple regression, Model 1: Symptom with focusing and DED | ||||||||
| Awareness of difficulty focusing | −0.058 | 0.103 | −0.020 | 0.588 | 0.144 | <0.001* | 0.123 | <0.001* |
| Impact of difficulty focusing | −0.058 | 0.160 | −0.018 | 0.672 | 0.030 | 0.446 | −0.031 | 0.482 |
| Near correction | 0.103 | 0.007 | −0.011 | 0.783 | −0.029 | 0.428 | 0.033 | 0.383 |
| DED | −0.122 | <0.001* | −0.071 | 0.024* | 0.146 | <0.001* | 0.169 | <0.001* |
| Model 2: Burden with vision | ||||||||
| Burden with near vision | −0.048 | 0.159 | −0.039 | 0.244 | 0.111 | 0.001* | 0.096 | 0.004* |
| Burden with far vision | −0.071 | 0.032* | −0.058 | 0.075 | 0.121 | <0.001* | 0.062 | 0.055 |
*P<0.05, Standardized partial regression coefficient.
A: Subjective happiness scale (0 (unhappy)-7 (happy))
B: Pittsburg Sleep Quality Index global score (higher score refers to poor sleep)
Discussion
The clinical results suggest men suffer presbyopia more severely than women, which it is contrary to our initial hypothesis that women may be more affected by presbyopia than men. This apparent discrepancy is explained as follows. The clinical results also demonstrated women actually adapted to presbyopia by using under-corrected contact lenses. They suffer less severely from presbyopia although presbyopia affects both genders equally because the amplitude of accommodation is the same in men and women of the same age. These clinical results may indicate women tolerated near vision symptoms longer than men by using under-corrected optical devices for daily use. Our speculation is supported by a previous study [8] reporting a weak association between accommodative amplitude and gender, and differences in the addition requirements for near vision were due to different preferred viewing distances or uncorrected hyperopia. Beginning in adolescence, girls spend more time on smartphones and suffer less eye fatigue than boys [37, 38]. Clinical data and survey results both suggested men suffered presbyopia earlier and more severely than women. Our speculation is based on burden for near vison (Table 1), happiness (Table 5), and sleep (Table 5), however, the detected differences were small and the clinical relevance may be limited. Further study is warranted to confirm our results.
The results of regression analysis for web-based survey data indicated presbyopic symptoms and burden with near vision were significantly associated with subjective happiness and sleep quality. The present results may be deemed contrary to our initial hypothesis that women may be more affected by presbyopia than men. This apparent discrepancy is explained as follows. The clinical results also demonstrated women actually adapted to presbyopia by using under-corrected contact lenses. They suffer less severely from presbyopia although presbyopia affects both genders because equally the amplitude of accommodation is the same in men and women of the same age.
One previous study assessed QOL associated with presbyopia using utility and described a small decrease in QOL (utility = 0.980). 10% of participants had a presbyopia-associated utility of 0.95 or less [29]. They used preference-based time trade-off utility analysis to evaluate individual values, whereas the outcome measure of the current study was to quantitively measure emotion (subjective happiness) and health index (sleep quality). There is a substantial difference between the two studies, possibly because participants may have been sensitive to the indices used in the current study. There are some cases in zero near add power in women independently of the subject’s age. The discrepancy between add power and age could be clarified in future research, including retrospective or prospective longitudinal studies. Pupillary diameter, corneal multifocality, and aberration may contribute to this apparently enhanced accommodation [39–42]. DED is a very common disease in middle adulthood, being associated with decreased QOL, subjective happiness, and sleep quality as reported in numerous studies. The present results demonstrated DED was associated with happiness and sleep more strongly than presbyopia. It may be advisable that middle aged persons may suffer worsened QOL, even without vision-threatening eye disease. The web-based survey results suggested presbyopia may reasonably worsen QOL of many people between the ages 40–59 and, additionally, other ocular disorders should be considered to evaluate QOL in this age group. Detailed interview and examination of other ocular diseases and systemic comorbidity would be contributory to disclose QOL of middle adulthood.
The web-based survey results indicate that age 48 was a critical point for presbyopia when the majority of people first wear reading glasses. Near add power may plateau around 45–48 years of age [5] and patients may likely then first visit an optician to check their vision and then see a physician. Vision care personnel are recommended to advise on potential risks of deteriorated QOL for middle-aged men, preferring full correction. In conclusion, presbyopia and dry eye disease were significantly associated with sleep quality and subjective happiness in middle-adulthood.
The strength of the present clinical study and web-based survey was age- and sex-matching in a sufficiently large sample size, and recruitment of middle-aged participants covering the age from the initiation to the plateau phase of presbyopia. Monofocal contact lens power was chosen to explore preferred daily vision because most patients use them to see comfortably without spectacles. Thus, preferred power of daily monofocal contact lenses may cover typical focusing tasks on participants, and is a relevant indicator for evaluating the burden of presbyopia.
The current study has several limitations. First, pupil size was not measured and it is a significant methodological limitation. Second, the clinical study participants were comprised of contact lens users, i.e., mostly myopes due to availability of patients. Myopic subjects may suffer presbyopia more severely than hyperopes since they can see near without correction for many years. Therefore, further studies should involve hyperopes and emmetropes. The type of lens was not registered, which presents a limitation since the type of lens can affect dryness symptoms. Third, this was a clinic-based study and may not represent the general population. A community-based study would be necessary to generalize the results. Fourth, the impact of presbyopia depends on lifestyle, hobbies, and work, therefore a more detailed survey would reveal the interaction between presbyopia and QOL in the middle-aged population. Fifth, the current study was comprised of two different studies. A single study with one cohort would further confirm the results, although the combination of two studies effectively conveyed reasonable results. Finally, the statistical results obtained with the current study were nominal and clinical relevance may not be significant. Further study should be warranted to further confirm our results.
Supporting information
(XLSX)
(XLSX)
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
The author(s) received no specific funding for this work.
References
- 1.Thakur RP, Banerjee A, Nikumb VB. Health Problems Among the Elderly: A Cross-Sectional Study Ann Med Health Sci Res. 2013. Jan-Mar; 3(1): 19–25. 10.4103/2141-9248.109466 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Holden BA, Fricker TR, Ho SM, Wong R, Schlenther G, Cronjé S, et al. Global vision impairment due to uncorrected presbyopia. Arch Ophthalmol 2008;126:1731–1739. 10.1001/archopht.126.12.1731 [DOI] [PubMed] [Google Scholar]
- 3.Kollbaum PS, Bradley A. Correction of Presbyopia: Old Problems With Old (And New) Solutions Clin Exp Optom. 2020. January;103(1):21–30. 10.1111/cxo.12987 [DOI] [PubMed] [Google Scholar]
- 4.Wolffsohn JS, Davies LN. Presbyopia: Effectiveness of correction strategies. Prog Retin Eye Res. 2019. January;68:124–143. 10.1016/j.preteyeres.2018.09.004 [DOI] [PubMed] [Google Scholar]
- 5.Duane A. Studies in monocular and binocular accommodation, with their clinical application. Trans Am Ophthalmol Soc 1922;20:132–157. [PMC free article] [PubMed] [Google Scholar]
- 6.Pointer JS. The presbyopic add. II. Age-related trend and a gender difference. Ophthalmic Physiol Opt. 1995;15(4):241–8. [PubMed] [Google Scholar]
- 7.Nirmalan PK, Krishnaiah S, Shamanna BR, Rao GN, Thomas R. A population-based assessment of presbyopia in the state of Andhra Pradesh, south India: the Andhra Pradesh Eye Disease Study. Invest Ophthalmol Vis Sci. 2006;47(6):2324–8. 10.1167/iovs.05-1192 [DOI] [PubMed] [Google Scholar]
- 8.Hickenbotham A, Roorda A, Steinmaus C, Glasser A. Meta-analysis of sex differences in presbyopia. Inv Ophthalmol Vis Sci 2012;53:3215–3220. 10.1167/iovs.12-9791 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Frick KD, Joy SM, Wilson DA, Naidoo KS, Holden BA. The global burden of potential productivity loss from uncorrected presbyopia. Ophthalmology 2015;122:1706–1710. 10.1016/j.ophtha.2015.04.014 [DOI] [PubMed] [Google Scholar]
- 10.Tsubota K, Nakamori K. Dry eyes and video display terminals. N Engl J Med. 1993. February 25;328(8):584. 10.1056/NEJM199302253280817 [DOI] [PubMed] [Google Scholar]
- 11.Niwano Y, Iwasawa A, Tsubota K, Ayaki M, Negishi K. Protective effects of blue light-blocking shades on phototoxicity in human ocular surface cells. BMJ Open Ophthalmol 2019;0:e000217. 10.1136/bmjophth-2018-000217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kaido M, Toda I, Oobayashi T, Kawashima M, Katada Y, Tsubota K. Reducing Short-Wavelength Blue Light in Dry Eye Patients With Unstable Tear Film Improves Performance on Tests of Visual Acuity. PLoS One 2016. April 5;11(4):e0152936. 10.1371/journal.pone.0152936 eCollection 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Uchino M, Schaumberg DA. Dry Eye Disease: Impact on Quality of Life and Vision. Curr Ophthalmol Reports 2013; 1 (2): 51–57. 10.1007/s40135-013-0009-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kawashima Dry sleep Kawashima M, Uchino M, Yokoi N, et al. The association of sleep quality with dry eye disease: the Osaka study. Clin Ophthalmol. 2016;10:1015–1021. 10.2147/OPTH.S99620 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ayaki M, Kawashima M, Negishi K, Kishimoto T, Mimura M, Tsubota K. Sleep and mood disorders in women with dry eye disease. Sci Rep. 2016;6:35276. 10.1038/srep35276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Han SB, Yang HK, Hyon JY, Wee WR. Association of dry eye disease with psychiatric or neurological disorders in elderly patients. Clin Interv Aging. 2017;12:785–792. 10.2147/CIA.S137580 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mai ELC, Lin C-C, Lian I, Liao R, Chen M, Chang C. Population-based study on the epidemiology of dry eye disease and its association with presbyopia and other risk factors Int Ophthalmol 2019; 39: 2731–2739. 10.1007/s10792-019-01117-5 [DOI] [PubMed] [Google Scholar]
- 18.Lyubomirsky S, Lepper HS. A measure of subjective happiness: preliminary reliability and construct validation. Soc Indic Res. 1999;46(2):137–155. [Google Scholar]
- 19.Matsunaga M, Isowa T, Yamakawa K, et al. Association between perceived happiness levels and peripheral circulating pro-inflammatory cytokine levels in middle-aged adults in Japan. Neuro Endocrinol Lett. 2011;32(4):458–463. [PubMed] [Google Scholar]
- 20.Matsuguma S, Negishi K, Kawashima M, Toda I, Ayaki M, Tsubota K. Patients’ satisfaction and subjective happiness after refractive surgery for myopia. Patient Prefer Adherence. 2018. September 25;12:1901–1906. 10.2147/PPA.S169902 eCollection 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yotsukura E, Ayaki M, Nezu N, Torii H, Arai H, Sakatani K, et al. Changes in Patient Subjective Happiness and Satisfaction with Cataract Surgery. Sci Rep. 2020. October 14;10(1):17273. 10.1038/s41598-020-72846-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kawashima M, Uchino M, Yokoi N, et al. Associations between subjective happiness and dry eye disease: a new perspective from the Osaka study. PLoS One. 2015;10(4):e0123299. 10.1371/journal.pone.0123299 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Frey BS. Happy people live longer. Science. 2011. February 4;331(6017):542–3. 10.1126/science.1201060 [DOI] [PubMed] [Google Scholar]
- 24.Buysse DJ, Reynolds CF III, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28: 193–213. 10.1016/0165-1781(89)90047-4 [DOI] [PubMed] [Google Scholar]
- 25.Doi Y, Minowa M, Utiyama M, Ohkawa M. Development of the Pittsburgh Sleep Quality Index Japanese version. Seishinka Chiryogaku 1998; 13: 755–763. In Japanese. [Google Scholar]
- 26.Nakajima H, Kaneita Y, Yokoyama E, et al. Association between sleep duration and hemoglobin A1c level. Sleep Med. 2008;9:745–752. 10.1016/j.sleep.2007.07.017 [DOI] [PubMed] [Google Scholar]
- 27.Gangwisch JE, Heymsfield SB, Boden-Albala B, et al. Short sleep duration as a risk factor for hypertension. Analyses of the First National Health and Nutrition Examination Survey. Hypertension. 2006;47:833–839. 10.1161/01.HYP.0000217362.34748.e0 [DOI] [PubMed] [Google Scholar]
- 28.Clerk A, Lange T, Hallqvist J, Jennum P, Rod NH. Sleep impairment and prognosis of acute myocardial infarction: a prospective cohort study. Sleep. 2014;37:851–858. 10.5665/sleep.3646 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Luo BP, Brown GC, Luo SC, Brown MM. The quality of life associated with presbyopia. Am J Ophthalmol. 2008. April;145(4):618–622. 10.1016/j.ajo.2007.12.011 [DOI] [PubMed] [Google Scholar]
- 30.Ayaki M, Tsuneyoshi Y, Yuki K, Tsubota K, Negishi K. Latanoprost may exacerbate progression of presbyopia. PLoS One. 2019. January 31;14(1):e0211631. 10.1371/journal.pone.0211631 eCollection 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Yokoi N, Georgiev GA, Kato H. Komuro A, Sonomura Y, Sotozono C, et al. Classification of fluorescein breakup patterns: A novel method of differential diagnosis for dry eye. Am. J. Ophthalmol. 2017; 180: 72–85. 10.1016/j.ajo.2017.05.022 [DOI] [PubMed] [Google Scholar]
- 32.Ayaki M, Negishi K, Kawashima M, Uchino M, Kaido M, Tsubota K. Age Is a Determining Factor of Dry Eye-Related Signs and Symptoms. Diagnostics (Basel). 2020. March 31;10(4):193. 10.3390/diagnostics10040193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Shimazaki J, Tsubota K, Kinoshita S, Ohashi Y. Definition and diagnosis of dry eye 2006. Atarashii Ganka 2007, 24, 181–184. Available online: http://www.atagan.jp/number/201703.htm (accessed on 1 January 2021). [Google Scholar]
- 34.Peterson RC, Wolffsohn JS, Fowler CW. Optimization of anterior eye fluorescein viewing. Am J Ophthalmol. 2006. October;142(4):572–5. 10.1016/j.ajo.2006.04.062 [DOI] [PubMed] [Google Scholar]
- 35.Gulati A, Sullivan R, Buring JE, Sullivan DA, Dana R, Schaumberg DA. Validation and Repeatability of a Short Questionnaire for Dry Eye Syndrome. Am. J. Ophthalmol. 2006; 142: 125–131. 10.1016/j.ajo.2006.02.038 [DOI] [PubMed] [Google Scholar]
- 36.Tsuneyoshi Y, Higuchi A, Negishi K, Tsubota K. Suppression of presbyopia progression with pirenoxine eye drops: experiments on rats and non-blinded, randomized clinical trial of efficacy. Sci Rep 2017;7: 6819. 10.1038/s41598-017-07208-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Japanese Ministry of Internal Affair and Communication. Year 2015 Annual Report of Information Technology and Communication in Japan. Available at: http://www.soumu.go.jp/johotsusintokei/whitepaper/ja/h27/html/nc372110.html; Accessed on Jul 7, 2020.
- 38.Ayaki M, Kawashima M, Uchino M, Tsubota K, Negishi K. Gender differences in adolescent dry eye disease: a health problem in girls. Int J Ophthalmol 2018; 11(2): 301–307. 10.18240/ijo.2018.02.20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Iida Y, Shimizu K, Ito M, Suzuki M. Influence of Age on Ocular Wavefront Aberration Changes With Accommodation. J Refract Surg. 2008;24:696–701. 10.3928/1081597X-20080901-09 [DOI] [PubMed] [Google Scholar]
- 40.Fukuyama M, Oshika T, Amano S, Yoshitomi F. Relationship between Apparent Accommodation and Corneal Multifocality in Pseudophakic Eyes. Ophthalmology 1999;106:1178–1181 10.1016/s0161-6420(99)90259-2 [DOI] [PubMed] [Google Scholar]
- 41.Oshika T, Mimura T, Tanaka S, Amano S, Fukuyama M, Yoshitomi F, et al. Apparent Accommodation and Corneal Wavefront Aberration in Pseudophakic Eyes. Invest Ophthalmol Vis Sci. 2002;43: 2882–2886. [PubMed] [Google Scholar]
- 42.Kubota M, Kubota S, Kobashi H, Ayaki M, Negishi K, Tsubota K. Difference in Pupillary Diameter as an Important Factor for Evaluating Amplitude of Accommodation: A Prospective Observational Study. J Clin Med J Clin Med. 2020. August 18;9(8):E2678. 10.3390/jcm9082678 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(XLSX)
(XLSX)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.


