Abstract
Cindy S Chu and co-authors review options for diagnosis, safe and radical cure, and relapse prevention of Plasmodium Vivax.
Summary points
The worldwide burden of Plasmodium vivax malaria has more than halved from an estimated 17.3 to 6.5 million cases between 2010 and 2019. This resulted from increased deployment of conventional malaria control measures (rapid diagnostic tests, effective antimalarial treatment, vector control) and significant global investment in malaria elimination. There is no generally available P. vivax vaccine, nor is there likely to be one in the near future.
The latest-generation RDTs used for P. vivax diagnosis have sensitivities comparable to microscopy. Ultrasensitive PCR methods which can detect parasite densities as low as 28/ml have revealed a much higher prevalence of asymptomatic P. vivax infection in malaria endemic regions than previously estimated.
Chloroquine remains an effective schizonticide for vivax malaria, except in Indonesia, Sabah and Papua New Guinea where there is high-level chloroquine resistance. Artemisinin combination therapies are effective alternative schizonticides that unify the treatment of all malarias. Relapses contribute significantly to the burden of P. vivax infections. Prevention of relapse requires “radical cure” with an 8-aminoquinoline (primaquine daily for 7 to 14 days, or single-dose tafenoquine). These drugs cause oxidant haemolysis in G6PD deficiency, so safe use requires G6PD testing. Overall, the risks of primaquine haemolysis have been overemphasised and the benefits of relapse prevention underappreciated.
Qualitative screening tests for G6PD deficiency (detecting <30% normal enzyme activity) are adequate for screening before giving primaquine for radical cure, but a quantitative point of care G6PD test to detect <70% normal enzyme activity is needed for tafenoquine.
Radical curative efficacy depends on the total 8-aminoquinoline dose given; higher primaquine doses (7 mg base/kg rather than 3.5 mg base/kg) are required in parts of Southeast Asia and Oceania. The currently recommended dose of tafenoquine (300 mg) is sub-optimal. In low transmission settings, elimination of vivax malaria is possible with current tools.
Introduction
Plasmodium vivax is more geographically dispersed than Plasmodium falciparum, with transmission occurring over a wider range of temperatures than for P. falciparum [1], and at latitudes as far as 64° North [2]. P. vivax is the predominant cause of human malaria in Asia and the Asia-Pacific regions where, with large populations and a declining incidence of P. falciparum infections, over 80% of the global P. vivax burden occurs [3]. P. vivax is also prevalent in the horn of Africa, Madagascar, and parts of Central and South America, but it has been eradicated from Europe, Russia, North America, and most of the Middle East [2,4].
Clinical management of P. vivax malaria relies on clinical suspicion, a reliable blood diagnostic, and access to efficacious effective schizonticidal (blood stage) and hypnozoiticidal (radical cure) drug regimens. Currently, P. vivax malaria is treated with chloroquine or artemisinin combination therapy (ACT) for the blood stage infection. While chloroquine has been standard treatment for vivax malaria for some 70 years, the emergence and global spread of chloroquine resistance in P. falciparum has meant that different treatments are now required for P. falciparum and the other human malarias. Use of ACTs (except artesunate-sulfadoxine-pyrimethamine) allows again a unified treatment for all malaria, and it provides a safety net in case of misdiagnosis or an unidentified mixed infection with P. falciparum. Despite declining susceptibility, chloroquine is still effective for P. vivax infection in most of the world, except for Indonesia, Sabah and Oceania where resistance is high grade [5,6]. Chloroquine is substantially less expensive than ACTs, although a unified treatment provides significant operational cost-savings.
Historically, P. vivax has been considered benign, although severe infections may sometimes occur [7–10]. Concomitant illness or chronic disease may contribute to the severity of P. vivax infection [11,12]. The management of severely ill patients with P. vivax malaria is similar to that of P. falciparum malaria [13]. P. vivax malaria in pregnancy is associated with miscarriage and low birth weight [14,15].
The great challenge for P. vivax malaria treatment is how to prevent relapses. These result from dormant liver stage parasites (hypnozoites) that activate weeks or months after the primary infection to cause a recurrent P. vivax infection (relapse). The intervals to and frequency of symptomatic relapses vary geographically and depend also on age and the intensity of transmission [16–18]. Frequent P. vivax infections are a major cause of morbidity in vivax malaria, particularly in young children in whom repeated relapse may cause severe anaemia, malnutrition, and growth delay [19, 20]. Thus, an important goal of treatment is to prevent relapse. This requires radical curative treatment with an 8-aminoquinoline in addition to treatment of the blood stage infection. The 8-aminoquinoline drugs cause haemolysis in patients with glucose-6-phosphate dehydrogenase deficiency (G6PDd), and this risk of dangerous iatrogenic haemolysis has limited their use substantially. In general, the harm caused by frequent relapse, particularly in young children, has been under appreciated, whereas the risks of haemolysis have been overemphasised, with a net result that primaquine radical cure has been underused.
Diagnosis of Plasmodium vivax malaria
Microscopy and rapid diagnostic tests
For over a century, the gold standard for diagnosing P. vivax malaria has been the microscopy observation of asexual parasites on a thick or thin blood film. Accurate microscopy requires trained laboratory staff supported with adequate laboratory supplies and well-maintained microscopes, which are not always available in resource-limited settings. The limit of detection for expert microscopy is about 50 parasites/uL which coincides approximately with the pyrogenic density [21]. The diagnostic sensitivity depends on the slide quality and the experience of the microscopist. Thus under field conditions, microscopy may miss some symptomatic cases because of the low parasite densities in P. vivax infections, but overall, it is suitably sensitive and specific for clinical diagnosis. Rapid diagnostic tests (RDTs) have been developed which detect antigens common to all malarias (e.g., aldolase) or those specific to P. vivax (e.g., PvLDH). First-generation RDTs had lower sensitivities for P. vivax parasitaemia [22] and could give false positive results [23] with high-density P. falciparum infections. The sensitivity and specificity of P. vivax RDTs have both been improved significantly. From 2008 to 2018, the proportion of P. vivax, P. falciparum, and pan-malaria RDTs meeting the current WHO performance threshold for procurement increased from approximately 20% to 90% [24]. During that decade, over 2.3 billion RDTs have been sold [25]. Access to reliable point-of-care diagnostic tools has allowed for early diagnosis and improved tremendously the ability to treat confirmed rather than suspected P. vivax infections.
Polymerase chain reaction (PCR) detection and genotyping
PCR allows low densities of malaria parasites to be detected reliably in blood samples. For low-volume blood samples such as filter paper blood spots, lower limits of reliable detection are typically in the range of 1 to 10 parasites/uL. In recent years, high-volume ultrasensitive PCR methods (uPCR) have been developed which amplify a larger amount of DNA, and these provide lower limits of detection around 28 parasites per mL (based on genus) with a second species-specific probe based on the 18S RNA gene [26]. These ultrasensitive methods allow detection of the majority of all infected people in endemic areas [27]. Most of these malaria-infected people are asymptomatic although, as parasite densities fluctuate over time, transmissible densities of gametocytes occur intermittently, and they are therefore a source of transmission [28]. PCR identification of infection is therefore an important component of epidemiological or clinical research assessment for submicroscopic recurrences, but it should not be used in disease diagnosis and management as it is too sensitive. That is, it will detect asymptomatic individuals who often have another reason for their febrile illness (reduced specificity).
Molecular genotyping is not needed for clinical management, although it is useful in clinical trials where, together with time-to-event information, it can help distinguish relapse from reinfection [29]. The interpretation of parasite genotyping is not as straightforward as it is for P. falciparum infections as relapses can be with genotypes similar or identical to the initial infection, or they can be with completely different genotypes resulting from heterologous hypnozoite activation [30, 31]. Nevertheless, combining genotype comparison with time-to-event information does allow probabilistic differentiation between relapses and reinfections.
Prevention
Insecticide-treated nets
Insecticide-treated nets (ITNs) are the mainstay of malaria control in most of the malaria-endemic world. Between 2017 and 2019, over 25,000,000 ITNs were distributed annually in malaria-endemic regions outside sub-Saharan Africa [4]. The effectiveness of ITNs depends on many factors which include distribution, coverage, adherence, maintenance, vector biting patterns, and levels of insecticide resistance [32]. Unsurprisingly ITNs are less effective if the anopheline vectors bite when people are not under or near their bed nets [33,34]. Most of the main vectors in SE Asia exhibit exophilic crepuscular biting patterns which decrease the effectiveness of ITNs in preventing malaria. In Papua New Guinea, anopheline vectors changed their behaviour to bite earlier after the introduction of bed nets [35]. Moreover, ITNs have no direct impact against relapse, which is often the main cause of vivax malaria (and once relapse proportions exceed 50%, relapses become the main cause of P. vivax infections). Despite these limitations, ITNs do provide partial benefit and are an adjunct method to prevent primary P. vivax infections and interrupt transmission [36]. Long-lasting nets (LLINs), in which the insecticide persists for the natural life of the net, are a substantial advance. There is rising concern about increasing pyrethroid resistance. Progress against pyrethroid resistance has been made in the forms of a new pyrrole insecticide, chlorfenapyr [37,38], and a chemical synergist which prevents insects from detoxifying pyrethroids, piperonyl butoxide (PBO) [39].
Insecticide use
The use of insecticides for malaria prevention focuses mainly on indoor residual spraying (IRS) and long-lasting ITNs, although there are a variety of other approaches. Organochlorides, organophosphates, carbamates, and pyrethroids are recommended by WHO for IRS. From 2000 to 2009, over 3,200 metric tonnes of insecticide were used against malaria vectors in P. vivax endemic regions [40]. Widespread insecticide use for agricultural treatments and large-scale malaria control programmes create intense selection pressure on vector populations to develop insecticide resistance [41,42]. Resistance to organochlorides and pyrethroids has been detected in the Americas, Asia, SE Asia, and the southern Pacific [42,43] where P. vivax is endemic, though even within a single country, resistance patterns may vary [44]. The full extent of insecticide resistance is not well characterised because routine monitoring in anopheline vector populations is not performed in all countries.
Vaccines
There is no generally available P. vivax vaccine, and none is on the near horizon. In contrast to P. falciparum, where hundreds of clinical trials and nearly 20 preclinical trials are registered, only 1 clinical trial and 2 preclinical trials are registered for P. vivax [45]. Potential vaccine strategies for P. vivax are irradiated sporozoites [46] and the blood stage antigens P. vivax Duffy binding protein (PvDBP), P. vivax merozoite surface proteins (PvMSP1, PvMSP3α, PvMSP9), P. vivax apical membrane antigen (PvAMA1), and the liver stage antigen P. vivax circumsporozoite protein (PvCSP) [47]. Transmission-blocking antigens are also potential targets. Phase I human trials have been conducted with PvCSP [48] and PvDBP [49] and asexual stage antigen Pv25 [50,51]. Currently, a single Phase I P. vivax vaccine trial (of a viral vectored PvDBP vaccine) is listed on the global WHO malaria clinical vaccine projects “Rainbow tables” (Trial NCT01816113) [45]. Vaccine development for P. vivax faces different challenges than with P. falciparum. P. vivax has greater genetic diversity [52] and cannot be maintained reliably in continuous cultures in vitro.
Chemoprophylaxis
Chemoprophylaxis is recommended to protect travellers from nonendemic areas entering a malaria-endemic area. Recommendations are largely focused on P. falciparum, the more dangerous malaria parasite, both to prevent severe disease, and also because nearly all the drugs which work against P. falciparum (either in pre-erythrocytic or “causal” prophylaxis, or in blood stage “suppressive” prophylaxis) are also effective against P. vivax. Intermittent presumptive treatment for infants and pregnant women (IPTi and IPTp) and seasonal malaria chemoprevention (SMC) are interventions which aim to prevent P. falciparum blood stage infections in populations that live in areas of moderate to high P. falciparum transmission. These are typically areas where P. vivax is either uncommon or absent. The only suppressive chemoprophylactic strategy specifically targeting P. vivax for endemic populations is a weekly chloroquine dose of 5 mg base/kg (300 mg base adult dose) given during pregnancy and lactation [53] as 8-aminoquinolines are contraindicated in this population (Table 1). This is seldom used, probably because of insufficient cost-effectiveness where incidence is low. But the cost-effectiveness balance does favour chloroquine prophylaxis to suppress relapse in pregnancy in women following an incident tropical (frequent relapse) P. vivax infection—and then it should be given. The role of IPTp with dihydroartemisinin-piperaquine in parts of Indonesia and Papua New Guinea, where transmission and resistance to chloroquine are both high, is under investigation with promising results in clinical trials [54].
Table 1. Chemoprophylactic regimens against Plasmodium vivax infection.
| Indication and treatment | Contraindicationsa | Dose | When to start | Treatment duration |
|---|---|---|---|---|
| Suppressive chemoprophylaxis in pregnancy | ||||
| Chloroquine | Severe renal or hepatic disease, can exacerbate psoriasisa | 300 mg base weekly | First antenatal visit or 3 weeks after treatment of vivax malaria | Continue until delivery |
| Suppressive chemoprophylaxis in travellers | ||||
| Any antimalarial regimen that is used for P. falciparum chemoprophylaxis (doxycycline or mefloquine) | Doxycycline: Myasthenia gravis, children <8 years, second or third trimester pregnancy Mefloquine: Epilepsy, history of or current psychiatric disease, severe hepatic disease |
Doxycycline 100 mg daily Mefloquine 250 mg base weekly |
1 day before travel 4 weeks before travel |
Continue for 4 weeks after return to nonendemic area |
| Causal prophylaxis in travellers | ||||
| Primaquine | G6PD deficiency, pregnancy, mothers breast feeding infants (<6 months)b or those who are G6PD deficient, and infants <6 months | 30 mg base daily with food | 1 day before travel | Continue until 7 days after return to nonendemic area |
| Tafenoquinec,d | G6PD deficiency (quantitative testing showing >70% normal activity required), pregnancy, mothers breast feeding infants who are G6PD deficient, history of psychotic disorder or current psychiatric symptoms | Loading dose of 200 mg base daily for 3 days, then 200 mg weekly with food (maximum 6 months) | 1 day before travel | |
| Atovaquone-proguanil | Pregnancy, severe renal disease (GFR <30 mL/min) | 250 mg/100 mg (1 tablet) daily with food | 1 day before travel | |
| Presumptive antirelapse therapy in travellers (PART)–necessary after suppressive chemoprophylaxis | ||||
| Primaquine | Same as for the causal prophylaxis indication | 0.25–0.50 mg base/kg/day with food | 7 days after return to the nonendemic area | 14 days |
| Tafenoquined (currently recommended only in combination with chloroquine treatment or chemoprophylaxis)c | Same as for the causal prophylaxis indication, except that history of psychiatric disorder or current psychiatric symptoms are not a contraindication | 300 mg base with food | 7 days after return to the nonendemic area | Single dose |
a Contraindications listed are in addition to allergy and apply only to the prophylaxis and not treatment indication.
b Minimal primaquine was excreted into mature breast milk in a study of breast feeding infants >28 days old [57].
c Tafenoquine product labelling has been changed so that only chloroquine may be used as the partner schizonticide [58,59]. Paediatric dosing recommendations are anticipated (TEACH trial) [60].
d The US Centers for Disease Control and Prevention (CDC) malaria guidance extends the use of tafenoquine for radical cure to PART [61].
GFR, glomerular filtration rate; G6PDd, glucose-6-phosphate dehydrogenase deficiency; PART, presumptive antirelapse therapy.
As countries eliminate malaria, the infections they encounter will increasingly be in travellers arriving from endemic areas. Suppressive chemoprophylaxis with drugs effective against P. falciparum has been the primary approach for malaria prevention (e.g., the same regimens apply to P. vivax), although they do not prevent the establishment of hypnozoites. The 8-aminoquinolines (primaquine and tafenoquine) have good activities against the pre-erythrocytic stages of all malarias, as well as blood stage activities against P. vivax, and so can be used for chemoprophylaxis. These drugs prevent later relapses as they kill hypnozoites (whereas IPTi or SMC with schizonticides only delay multiplication of the blood stage). Atovaquone-proguanil is also considered to provide highly effective causal prophylaxis against P. vivax but it does not prevent relapses. Recent observations in travellers showed a similar rate of P. vivax infections (40% to 50%) up to 1 year after returning to a nonendemic area following either atovaquone-proguanil, mefloquine, or doxycycline prophylaxis. This compares with a rate of only 1% to 2% in travellers who had received primaquine [55]. This suggests that while atovaquone is active against the developing hypnozoite, it is not active against the metabolically inert hypnozoite more than 3 days postinoculation [56]. The drugs, which act primarily on the liver stage (pre-erythrocytic) infection (i.e., causal prophylaxis), have the substantial advantage that they can be stopped within days of leaving the endemic area, whereas the blood stage suppressive drugs (mefloquine, tetracyclines, chloroquine) need to be continued for 1 month after leaving to capture late emerging blood stage infections. To ensure that relapses from P. vivax and Plasmodium ovale are prevented presumptive antirelapse therapy (PART) with a radical curative dose of 8-aminoquinolines (primaquine and tafenoquine) may be given following departure from an endemic area to persons receiving suppressive chemoprophylaxis (Table 1). The timing of the PART dose is important as it should be started while blood schizonticide concentrations remain above the mean inhibitory concentration. Thus, PART can be started within the final 2 weeks of doxycycline and mefloquine, and the final week of atovaquone-proguanil suppressive chemoprophylactic regimens.
Treatment of acute Plasmodium vivax malaria
Blood stage treatment
Since 1947, chloroquine has been the treatment of choice for blood stage infections with P. vivax. The standard treatment regimen is 25 mg of base equivalent/kg divided over 3 days and given either as 10 mg/kg initially followed either by 10 mg/kg at 24 hours and 5 mg/kg at 48 hours, or by 3 doses of 5 mg/kg 12 hourly [53]. Various other ways of giving this 25 mg/kg treatment dose have been recommended, and chloroquine may be administered safely over 36 hours provided that individual doses do not exceed 10 mg/kg. Although lower doses are effective, there is no reason to depart from this standard regimen in most regions. Absorption of chloroquine by mouth is reliable even when patients are prostrate [62], and there is seldom need for parenteral treatment. Indeed, parenteral formulations of chloroquine are no longer generally available, so those patients who do require initial parenteral treatment for severe P. vivax malaria should be given intravenous or intramuscular artesunate until they can take oral medication reliably [13]. ACTs are also highly effective (except for artesunate-sulfadoxine-pyrimethamine) and provide a slightly more rapid clinical and parasitological response than chloroquine [63–67]. The post-treatment suppression of early relapses depends on the elimination kinetics of the ACT partner drug—mefloquine, piperaquine, pyronaridine, and amodiaquine ACTs provide approximately similar durations of suppression compared with chloroquine, whereas artemether-lumefantrine provides a significantly shorter period of suppression [68]. Both chloroquine and ACTs are generally well tolerated antimalarial treatments. The weight-adjusted schizonticidal treatment regimens are similar in pregnant and lactating women [54]. Paediatric formulations are available for artemether-lumefantrine, artesunate-amodiaquine, dihydroartemisinin-piperaquine, and pyronaridine-artesunate, and the doses are similar to those recommended for falciparum malaria. Child-friendly formulations and smaller-dose tablets are needed for primaquine.
Primaquine and tafenoquine both have significant blood stage activities but as the therapeutic response is significantly slower than with chloroquine or ACTs, they should not be used as monotherapies for blood stage infections [69,70]. Nevertheless, the asexual stage activity of 8-aminoquinolines does contribute significantly to the treatment efficacy and prevents resistance to standard schizonticides by providing a combination treatment for the blood stage infection. P. vivax gametocytes are considered as sensitive as the asexual stages to antimalarial drugs [71] so, unlike P. falciparum, specific gametocytocidal treatment is not necessary.
High fevers can be managed with standard doses of paracetamol, and vomiting can be treated with antiemetics. If patients show signs of severe vivax malaria, then the management is exactly the same as for severe falciparum malaria [13]. Uncomplicated mixed infections with P. falciparum and P. vivax should be treated with an ACT and a radical curative regimen [53].
Antimalarial drug resistance
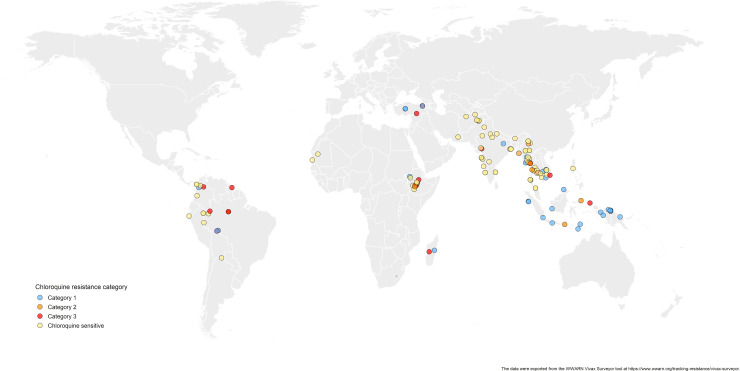
Chloroquine resistance in P. vivax has emerged more slowly than for P. falciparum. The mechanism of resistance and its molecular basis have proved elusive. Evidence of chloroquine resistance was detected first in a traveller returning from Papua New Guinea over 30 years ago [5,6]. Chloroquine resistance has been defined as a patent P. vivax infection in the presence of chloroquine + desethychloroquine levels >100 ng/mL in whole blood or >10 ng/mL in plasma [72]. Since then, chloroquine resistance has risen to high levels in Indonesia and Oceania (Fig 1) and so ACTs are used instead of chloroquine in this region. Dihydroartemisinin-piperaquine, artesunate-mefloquine, artemether-lumefantrine, and artesunate-pyronaridine are all very effective treatments of vivax malaria [62–65]. While amodiaquine is also more effective than chloroquine against resistant P. vivax, it is not as well tolerated as dihydroartemisinin-piperaquine, and resistance in P. falciparum is widespread in P. vivax-endemic regions. Amodiaquine-containing regimens are not therefore recommended for chloroquine-resistant P. vivax infections [73–74]. Despite evidence for slowly rising chloroquine resistance in P. vivax, chloroquine still remains effective throughout most malaria-endemic areas [65,75–79]. As the concomitant use of primaquine (for radical cure) provides significant independent asexual stage activity, it may mask low-level chloroquine resistance [80–82]. The lack of a molecular marker of chloroquine resistance and the limited availability of in vitro testing in vivax malaria [83] means that the epidemiology of chloroquine resistance is not well described. Antifol resistance occurs readily in P. vivax through mutations in Pvdhfr which are readily identified. Antifol resistance is geographically widespread [84,85]. P. vivax is also intrinsically relatively resistant to sulphonamides. This is why the artesunate-sulfadoxine-pyrimethamine ACT should not be used for P. vivax treatment.
Fig 1. Levels of chloroquine resistance against Plasmodium vivax from 1985–2019.
The data were exported from the WWARN Vivax Surveyor tool at https://www.wwarn.org/tracking-resistance/vivax-surveyor. Evidence for chloroquine resistance comes from P. vivax clinical trials published from 1985–2019. Some trials are from different years in the same area; this figure does not specify the change in chloroquine resistance pattern over time. CQS: Chloroquine sensitive, Category 1: very suggestive of resistance, Category 2: suggestive of resistance, Category 3: potential evidence of resistance.
Plasmodium vivax relapse
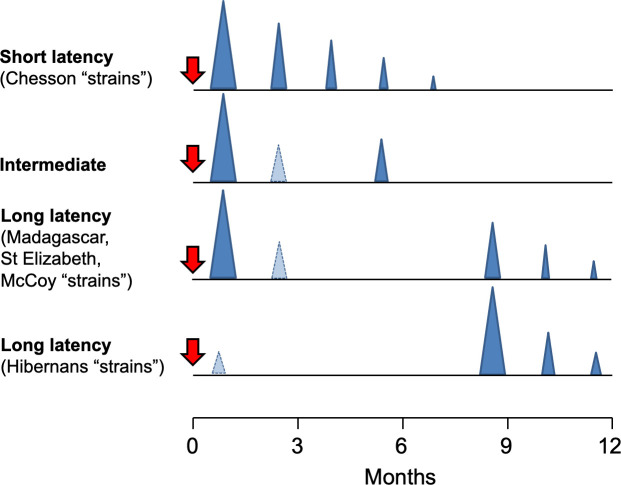
Relapses of P. vivax and P. ovale are the recurrent blood stage infections which originate from hypnozoites in the liver. Relapses occur with periodic regularity (Fig 2); short latency phenotypes prevalent in tropical climes relapse at approximately 3- to 4-week intervals. These intervals are prolonged by slowly eliminated antimalarial drugs. Longer latency phenotypes may relapse 8 to 9 months after a primary infection [86]. The proportion of infections which relapse varies between 20% and 100% depending on location and transmission intensity.
Fig 2. Plasmodium vivax relapse patterns.
The temporal patterns of P. vivax relapse in different “strains.” The red arrow indicates the infective mosquito bite which leads to the primary infection. The blue triangles represent patent P. vivax infections; the largest triangle is the primary infection. The proportions of successive relapses decline, and there is an increasing probability that the relapses are oligosymptomatic or asymptomatic. The translucent blue triangles are P. vivax infections which may sometimes occur. The short latency frequent relapse pattern (typified by the “Chesson strain”) is prevalent across tropical areas. The intermediate phenotype may occur in South Asia. The long latency phenotype (typified by the Madagascar, St Elizabeth, and McCoy strains) is found in Central America, North Africa, and central Asia, while the long latency “hibernans” phenotype, which was prevalent in Northern Europe and Russia, is still found in North Korea.
The multiplication of the blood stage infection of early relapses is suppressed by slowly eliminated antimalarials (e.g., chloroquine) prescribed for the previous clinical P. vivax episode. As a consequence, in tropical areas, relapses become patent 3–6 weeks after artemether-lumefantrine and 5–7 weeks after chloroquine, whereas they occur around 3 weeks after artesunate or quinine treatment [76].
Antirelapse (radical cure) treatment
Primaquine
For over 60 years, the mainstay of antirelapse treatment has been a 14-day primaquine regimen. Divergent policies and practices, concerns over haemolysis, and the unavailability of G6PD testing have contributed to low rates of primaquine uptake for radical cure in malaria-endemic countries [87].
The radical curative efficacy of primaquine depends on the total dose given. There have been relatively few randomised trials in which the radical curative efficacy of primaquine has been assessed with a necessary ≥4-month follow-up (1 year is preferable). In South America, 7-day regimens are used. The radical curative efficacy of the 7-day low-dose (total 3.5 mg base/kg) primaquine regimen was approximately 80% [88–92]. In SE Asia and Oceania, higher doses are needed for maximum efficacy [93]. The most commonly recommended higher dose is a total of 7 mg base/kg given over 14 days (adult dose 30 mg/day), although most countries still recommend the lower dose (3.5 mg base/kg total dose; adult dose 15 mg/day for 14 days or 30 mg/day for 7 days). Potentially poor adherence to the 14-day treatment reduces the effectiveness of radical cure. Recent studies show that shortening the course of the higher-dose treatment to 7 days (adult dose 60 mg/day) is efficacious and safe in G6PD normal patients, although significant haemolysis may occur in heterozygote females with intermediate G6PD activity who have tested normal with standard qualitative G6PD screening tests [94,95] (see below). G6PD quantitative tests may be needed for this short-course high-dose treatment. For patients who test as G6PD deficient, a weekly primaquine dose (0.75 mg base/kg/dose) given for 8 weeks has been recommended, although the safety of this dose has only been assessed in a few populations [53,96–98].
In early clinical trials, it was observed that chloroquine potentiated the radical curative efficacy of primaquine [99]. The mechanism underlying this relationship and its clinical significance remain unclear. Radical curative efficacy is similar when primaquine is paired with chloroquine or an ACT, and radical cure rates over 95% can be achieved after supervised dosing [29,94,95]. Primaquine requires metabolism to its bioactive metabolites by the liver isoenzyme CYP2D6 [100,101]. Primaquine failure may therefore occur in patients with CYP2D6 mutations associated with a poor or intermediate metaboliser phenotype. Overall, adherence likely plays a greater role in the failure of primaquine to prevent relapse. Resistance to primaquine has been reported, but there is no conclusive evidence of acquired resistance in liver stages.
Primaquine is contraindicated in pregnancy, is not recommended in infants <6 months, and has also been withheld from lactating women, although a recent study shows that the dose ingested by the breastfeeding infant is very small [57] and therefore very unlikely to exert any biological effect. This restriction may well be lifted. Primaquine is generally well tolerated. It may cause abdominal pain if larger doses (over 0.5 mg/kg) are taken on an empty stomach. This is lessened if given with food. The main adverse effect of the 8-aminoquinolines is dose-dependent oxidant haemolysis in G6PD deficiency. Primaquine-induced methaemoglobinaemia is usually mild, but it can be severe in NADH methaemoglobin reductase deficiency.
Haemolysis in G6PD deficiency
G6PD deficiency is the most common human enzymopathy. Gene frequencies average 8% to 10% across much of the tropical world [102]. The risk of haemolysis in G6PD deficiency is the main obstacle to the use of 8-aminoquinolines for radical cure. The enzyme deficiency is X-linked so males are either normal or deficient (hemizygotes), whereas women can be either normal, or fully (homozygotes) or partially deficient (heterozygotes). On average, at a population level, female heterozygotes have half their red cells which are normal and half which are G6PD deficient but, because of random X-inactivation (Lyonisation), these proportions vary substantially between individuals, thus causing wide variations in the degree of enzyme deficiency among female heterozygotes. Both primaquine and tafenoquine cause predictable dose-related haemolysis in G6PD-deficient individuals [103,104]. Haemolysis disproportionately affects older red blood cells because G6PD activity declines as red blood cells age [105]. There are approximately 200 different polymorphic G6PD deficiency genotypes [106]. The majority confer reduced enzyme activity, although the degree of deficiency varies substantially among the different genotypes. The extent of haemolysis depends on the dosage of drug and the genotype. In Africa, the less severe A-genotype is prevalent, whereas in Asia, the common genotypes confer greater enzyme deficiency. The most commonly used screen for G6PD deficiency is the qualitative G6PD fluorescent spot test (FST), which detects the naturally fluorescent NADPH. The FST detects <30% of normal G6PD activity reliably (deficient blood does not fluoresce) so it identifies the male hemizygotes, female homozygotes, and those heterozygotes with G6PD activity near the 30% threshold. The FST may not be feasible at lower-level healthcare settings as it requires electricity, trained laboratory staff, and quality control. New qualitative lateral flow G6PD RDTs are available. These can be performed where the FST cannot. These RDTs are an important support tool for diagnosing G6PD deficiency, and the safe prescription of primaquine as P. vivax radical cure is scaled up. Patients who have a test result indicating G6PD deficiency should not receive the standard primaquine regimen. Instead, in areas where the less severe G6PD variants (e.g., G6PD A-) are prevalent, they should receive a once weekly 0.75 mg base/kg dose for 8 weeks [53,96]. The safety of the weekly regimen has not been established in patients with G6PD variants that are severe (e.g., G6PD Mediterranean). However, a threshold for phenotypic severity has not been defined. Even with FST or RDT screening, there may still be significant haemolysis in G6PD heterozygote females who have slightly more than 30% of G6PD normal erythrocytes. Such females would be considered as G6PD normal and potentially given primaquine. Unfortunately, in many regions, G6PD testing is unavailable so the practitioner treating vivax malaria is faced with a dilemma—to give radical cure “at risk,” or to err on the side of safety and not give it. In this difficult choice, the substantial morbidity of recurrent P. vivax malaria, particularly in young children who may be ill every second month, has often been underappreciated [107]. Importantly, in gauging the risk, it is important to note that G6PD deficiency protects against P. vivax malaria, so at a population level, the risk of haemolysis in patients is lower than would be predicted from prevalence surveys in healthy individuals [108]. In a recent study in Afghanistan of Pashtun patients (in whom the main G6PD variant is the “severe” Mediterranean variant), the prevalence of G6PD deficiency in men (i.e., hemizygotes) presenting with vivax malaria was 4 times lower than in the healthy population [109]. The result of these various uncertainties has been a diverse array of National treatment recommendations and practices for radical cure. Many countries do recommend giving primaquine “at risk,” yet despite over 60 years of widespread use, the total number of documented fatalities from haemolysis is only fifteen [110,111]. The likely reason for this low number is that primaquine can be stopped as soon as there are symptoms or clinical evidence of substantial acute haemolysis (e.g., lassitude, exertional dyspnoea, haemoglobinuria, or abdominal discomfort) and, because primaquine and its oxidant metabolites are rapidly eliminated, the anaemia is limited. This probably explains why mass treatments with primaquine without G6PD testing, even in areas where G6PD Mediterranean was the main deficiency genotype, were not apparently associated with serious toxicity [110].
Tafenoquine
Tafenoquine is a slowly eliminated 8-aminoquinoline (terminal elimination half-life of approximately 12 days) which allows single-dose treatment. As with primaquine, tafenoquine is generally well tolerated and abdominal discomfort is lessened if given with food. During the long development of tafenoquine, concerns were raised about the potential for vortex keratopathy, electrocardiograph QT prolongation, and psychiatric reactions. The clinical evidence to date has largely resolved these issues [112–115] although, in the product labelling, tafenoquine for causal prophylaxis is considered contraindicated in persons with psychiatric symptoms. Being a single-dose treatment, tafenoquine addresses a major limitation of the 7- or 14-day primaquine regimen, the potential for poor adherence. However, this advantage is at the expense of a substantial risk of haemolytic toxicity in G6PD deficiency as, once tafenoquine is taken, it cannot be “stopped” if there is drug-induced haemolysis. A meta-analysis of the multicountry phase 3 studies showed that tafenoquine had a 6-month radical curative efficacy similar to low-dose primaquine (0.25 mg/kg/day for 14 days) in South America (67% versus 66%, respectively) and the horn of Africa (75% versus 80%, respectively), but the efficacy of the currently recommended 300 mg dose was significantly inferior in the SE Asian sites (74% versus 93%, respectively) [116,117]. These are disappointing radical curative efficacies and suggest that higher tafenoquine doses are probably needed in SE Asia and Oceania where P. vivax relapse rates are high, and also in South America where both radical cure regimens performed poorly [118]. Tafenoquine efficacy did not appear to be affected significantly by CYP2D6 polymorphisms in the Phase III trials [119], but more data are needed to confirm these early findings.
As described, tafenoquine’s advantage in being slowly eliminated (terminal half-life approximately 12 days), and thus effective in a single dose, is also its Achilles heel. If given to an individual who is G6PD deficient, the drug exposure and resulting haemolysis will persist until all the susceptible erythrocytes have been destroyed. Some female heterozygotes, who would be undetected by the standard screens, could still theoretically lose up to 70% of their red cells. This is why the higher G6PD activity threshold (>70% G6PD activity) has been chosen for tafenoquine eligibility. The gold standard method for G6PD quantitation is spectrophotometry requiring relatively expensive and sophisticated laboratory techniques, so it is not feasible in nearly all healthcare settings. Thus, for safe use of tafenoquine, new quantitative point-of-care G6PD tests have been developed. Studies to validate G6PD quantitative tests are completed [120,121] and under regulatory review. More extensive field testing is ongoing to assess the performance of these quantitative G6PD tests in field settings under “real world” conditions and the rates of incorrect test results or interpretations.
The current exclusions to tafenoquine apply to approximately 25% of the population in endemic areas, depending on the G6PD allelic frequency, and fertility and lactation rates [122]. Approving its use in lactating females would substantially improve potential population coverage. Tafenoquine has received regulatory approval in the United States of America, Australia, Brazil, and Thailand [116,117]. Results from the first trial assessing tafenoquine use in children (2 to 15 years) with P. vivax malaria show that dosing regimens in 4 weight bands were safe and efficacious and reached the target AUC0-∞ [60]. As a result, current restrictions on use in children will likely be lifted. Tafenoquine has usually been coadministered with chloroquine. In a recently completed clinical trial in Indonesian soldiers, dihydroartemisinin-piperaquine coadministered with tafenoquine (300 mg dose) was shown to be no different than dihydroartemisinin-piperaquine alone [58] in preventing recurrence of P. vivax malaria. These data prompted a product label change to Krintafel (the US regulatory approved form of tafenoquine for treatment) in early 2020 [59]. Now, only chloroquine is recommended to be the partner drug to tafenoquine for P. vivax malaria treatment. If followed this would prevent the use of tafenoquine in areas with chloroquine-resistant P. vivax parasites where national malaria programmes recommend ACTs for vivax malaria. Clearly, further clinical trials are needed to identify the correct dose of tafenoquine for radical cure [118] and resolve this partner drug uncertainty.
How can we identify hypnozoite carriers?
There is currently no test which identifies people with hypnozoites who may later relapse. Living or working in an area of P. vivax transmission is obviously a risk factor, and having had vivax malaria without radical treatment is clearly the major risk. Pregnant women cannot receive 8-aminoquinolines so are at significant risk if they have vivax malaria during pregnancy. If primaquine could be allowed during lactation (as breast milk excretion is minimal [57]), this should result in a recommendation to give radical cure after delivery. PCR, particularly high-volume uPCR, identifies the majority of asymptomatic P. vivax infections. Serology can also identify recent infection, although is not widely available.
Assessment of therapeutic responses
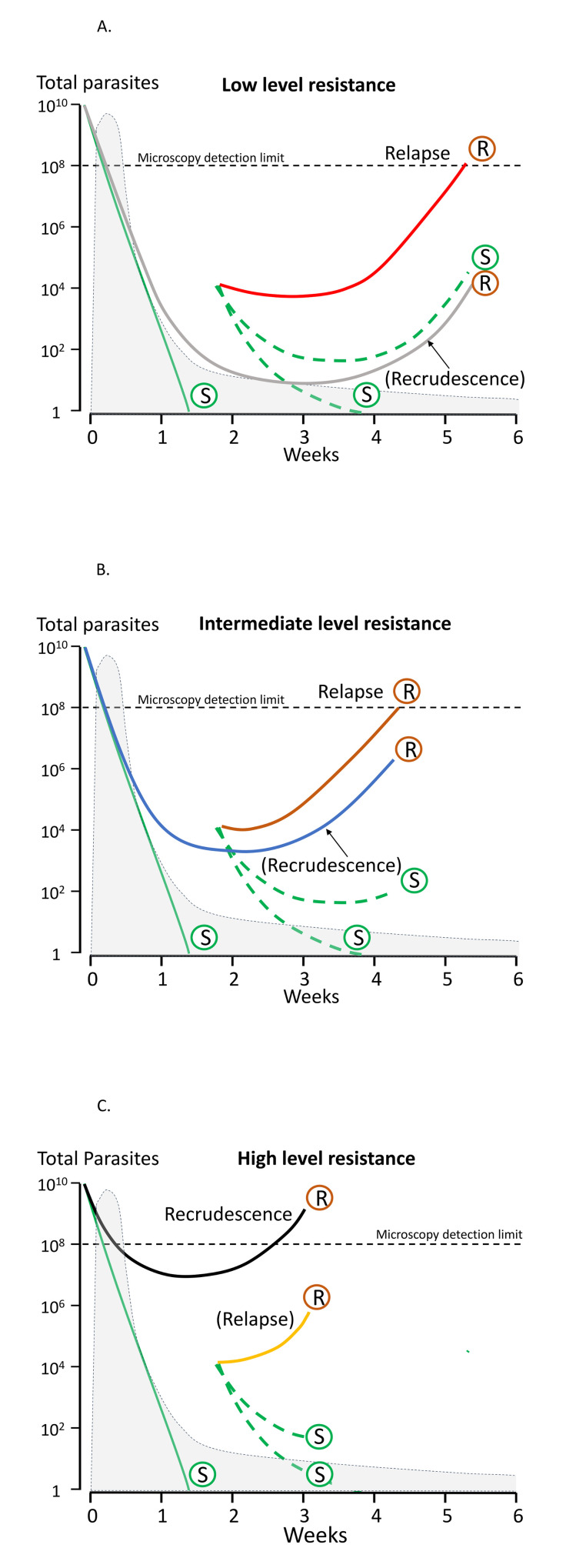
As in falciparum malaria, the treatment responses in P. vivax infections can be assessed by measurement of symptom resolution, fever clearance, and parasite clearance. The lower parasite densities in P. vivax mean that parasite rate clearance estimates are more difficult to assess, although sequestration is not a confounder in measuring parasite clearance rates because all parasite stages are in the circulation [123]. Quantitative polymerase chain reaction (qPCR) estimation of parasite clearance rates has been used successfully in human challenge experiments but is not widely available [124]. These parasite clearance estimates based on qPCR are not confounded by gametocytaemia (as they are in falciparum malaria) because P. vivax gametocyte clearance parallels asexual stage clearance after a blood schizonticide [71]. The major challenge in therapeutic assessment is distinguishing relapse, recrudescence, and reinfection, and therefore identifying early resistance. Both chloroquine and the ACT partner drugs are eliminated slowly so that suppressive blood concentrations persist for weeks after treatment [118]. Lumefantrine provides the shortest period of suppression and mefloquine the longest of the currently deployed ACTs. In tropical areas, the first sign of chloroquine resistance in vivo, well before slowing of parasite clearance, is the failure to suppress the first relapse [72,125]. This may not be evident unless patients are followed for 2 months in comparative studies (Fig 3A). As the level of resistance increases, the interval shortens and the first relapse becomes patent within 28 days (Fig 3B). Chloroquine should suppress relapse emergence within 28 days so recurrence within this period, whether from relapse or reinfection, still indicates resistance [125]. If a recurrent infection occurs within 28 days of starting chloroquine for the previous vivax infection, an ACT (such as dihydroartemisinin-piperaquine, artemether-lumefantrine, or artesunate-mefloquine) should be prescribed. Resistance can be confirmed by measuring the whole blood chloroquine level at the time of recurrent parasitaemia [93]. With higher levels of resistance (Fig 3C), recrudescence preempts the relapse. At this stage, parasite genotyping is informative as these early recurrences will all be of the same genotype as the initial infection [29].
Fig 3. Plasmodium vivax chloroquine treatment failure in scenarios of low, intermediate, and high levels of resistance in areas with frequent relapsing P. vivax [118].
The vertical axis shows the total number of parasites in the body in acute vivax malaria. The light grey shaded area is the blood chloroquine concentration profile. The limit of microscopy detection is approximately 50 parasites/uL. In each panel, chloroquine-sensitive parasites are shown by green lines and marked S. The relapses emerge from the liver approximately 2 weeks after starting treatment. There is uncertainty whether chloroquine eliminates or temporarily suppresses the first relapse (in most cases it suppresses but does not eliminate [118]) so dotted lines representing both scenarios are shown. Resistant parasites causing relapse and recrudescence are marked R. Upper panel (A): When there are low levels of resistance, the blood stage infection is cleared usually by the schizonticide, and the first relapse is suppressed until the drug levels fall below the mean inhibitory concentration (MIC) (e.g., in this illustrated example, chloroquine levels above the MIC are maintained until day 28, and relapse parasitaemia becomes patent 2 weeks later) [125]. Recrudescence is very unlikely (occurring only in those patients with low drug levels) and in patients with relapse, the recrudescence would not be detected because the relapse appears first. Middle panel (B): When resistance to chloroquine is at an intermediate level, the blood stage infection clears, but the first relapse becomes patent before 28 days. If a relapse occurs, it would still preempt any recrudescence. Lower panel (C): With high levels of resistance, the blood stage infection recrudesces before the relapse parasitaemia becomes patent.
Summary
Frequent recurrent P. vivax malaria causes substantial preventable morbidity. Better diagnosis, easier G6PD testing, and use of ACTs as an alternative to chloroquine are improving the clinical management of P. vivax malaria, but the challenge now is to make these more widely available. Primaquine radical cure is under used. Tafenoquine provides single-dose radical cure, but the optimum dose and method of using tafenoquine safely still need to be determined. The tools needed for P. vivax elimination are available. Malaria elimination activities conducted in remote settings [126–128] have been successful in reducing P. vivax incidence considerably, but continuing to sustained elimination will require substantial commitment and resources.
Acknowledgments
We would like to thank Jade D. Rae for her generous help with the mapping for Fig 1.
Abbreviations
- ACT
artemisinin combination therapy
- FST
fluorescent spot test
- G6PDd
glucose-6-phosphate dehydrogenase deficiency
- IPTi
intermittent presumptive treatment for infants
- IPTp
intermittent presumptive treatment for pregnant women
- IRS
indoor residual spraying
- ITN
insecticide-treated net
- LLIN
long-lasting net
- PART
presumptive antirelapse therapy
- PBO
piperonyl butoxide
- PCR
polymerase chain reaction
- PvAMA
P. vivax apical membrane antigen
- PvCSP
P. vivax circumsporozoite protein
- PvDBP
P. vivax Duffy binding protein
- PvMSP
P. vivax merozoite surface protein
- qPCR
quantitative polymerase chain reaction
- RDT
rapid diagnostic test
- SMC
seasonal malaria chemoprevention
- uPCR
ultrasensitive PCR
Funding Statement
The authors received no specific funding for this work.
References
- 1.Gething PW, van Boeckel TP, Smith DL, Guerra Ca, Patil AP, Snow RW, et al. Modelling the global constraints of temperature on transmission of Plasmodium falciparum and Plasmodium vivax. Parasit Vectors. 2011;4: 92. 10.1186/1756-3305-4-92 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mironova VA, Shartova N V., Beljaev AE, Varentsov MI, Korennoy FI, Grishchenko MY. Re-introduction of vivax malaria in a temperate area (Moscow region, Russia): A geographic investigation. Malar J. 2020;19:1–20. 10.1186/s12936-020-03187-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Howes RE, Battle KE, Mendis KN, Smith DL, Cibulskis RE, Baird JK, et al. Global Epidemiology of Plasmodium vivax. Am J Trop Med Hyg. 2016;95(Suppl 6):15–34. 10.4269/ajtmh.16-0141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Health Organization. World malaria Report 2020. Geneva; 2020. Available from: https://www.who.int/publications/i/item/9789240015791
- 5.Rieckmann KH, Davis DR, Hutton DC. Plasmodium vivax resistance to chloroquine? Lancet. 1989;2:1183–1184. 10.1016/s0140-6736(89)91792-3 [DOI] [PubMed] [Google Scholar]
- 6.Whitby M, Wood G, Veenendaal JR, Rieckmann KH. Chloroquine resistant Plasmodium vivax. Lancet. 1989;334:1395. 10.1016/s0140-6736(89)92002-3 [DOI] [PubMed] [Google Scholar]
- 7.Lacerda MVG, Mourão MPG, Alexandre MAA, Siqueira AM, Magalhães BML, Martinez-Espinosa FE, et al. Understanding the clinical spectrum of complicated Plasmodium vivax malaria: a systematic review on the contributions of the Brazilian literature. Malar J. 2012;11:12. 10.1186/1475-2875-11-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kochar DK, Das A, Kochar A, Middha S, Acharya J, Tanwar GS, et al. A prospective study on adult patients of severe malaria caused by Plasmodium falciparum, Plasmodium vivax and mixed infection from Bikaner, northwest India. J Vector Borne Dis. 2014;51:200–10. Available from: http://www.ncbi.nlm.nih.gov/pubmed/25253213 [PubMed] [Google Scholar]
- 9.Genton B, D’Acremont V, Rare L, Baea K, Reeder JC, Alpers MP, et al. Plasmodium vivax and Mixed Infections Are Associated with Severe Malaria in Children: A Prospective Cohort Study from Papua New Guinea. PLoS Med. 2008;5:e127. 10.1371/journal.pmed.0050127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lança EFC, Magalhães BML, Vitor-Silva S, Siqueira AM, Benzecry SG, Alexandre MAA, et al. Risk factors and characterization of Plasmodium vivax-associated admissions to pediatric intensive care units in the Brazilian Amazon. PLoS ONE. 2012;7:e35406. 10.1371/journal.pone.0035406 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Quispe AM, Pozo E, Guerrero E, Durand S, Baldeviano GC, Edgel KA, et al. Plasmodium vivax hospitalizations in a monoendemic malaria region: Severe vivax malaria? Am J Trop Med Hyg. 2014;91:11–17. 10.4269/ajtmh.12-0610 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kute VB, Trivedi HL, Vanikar A V, Shah PR, Gumber MR, Patel H V, et al. Plasmodium vivax malaria-associated acute kidney injury, India, 2010–2011. Emerg Infect Dis. 2012;18:842–5. 10.3201/eid1805.111442 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.World Health Organization. Severe Malaria. Trop Med Int Health. 2014;19:7–131. Available from: https://www.who.int/malaria/publications/atoz/severe-malaria-tmih-2014/en/ 10.1111/tmi.12313_2 [DOI] [PubMed] [Google Scholar]
- 14.Moore KA, Fowkes FJI, Wiladphaingern J, Wai NS, Paw MK, Pimanpanarak M, et al. Mediation of the effect of malaria in pregnancy on stillbirth and neonatal death in an area of low transmission: Observational data analysis. BMC Med. 2017;15: 1–11. 10.1186/s12916-017-0863-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Moore KA, Simpson JA, Wiladphaingern J, Min AM, Pimanpanarak M, Paw MK, et al. Influence of the number and timing of malaria episodes during pregnancy on prematurity and small-for-gestational-age in an area of low transmission. BMC Med. 2017;15: 1–12. 10.1186/s12916-017-0877-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Luxemburger C, Thwai KL, White NJ, Webster HK, Kyle DE, Maelankirri L, et al. The epidemiology of malaria in a Karen population on the western border of Thailand. Trans R Soc Trop Med Hyg. 1996;90:105–111. Available from: http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=8761562 10.1016/s0035-9203(96)90102-9 [DOI] [PubMed] [Google Scholar]
- 17.van den Eede P, Soto-Calle VE, Delgado C, Gamboa D, Grande T, Rodriguez H, et al. Plasmodium vivax sub-patent infections after radical treatment are common in Peruvian patients: results of a 1-year prospective cohort study. PLoS ONE. 2011;6:e16257. 10.1371/journal.pone.0016257 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Daher A, Silva JCAL, Stevens A, Marchesini P, Fontes CJ, Ter Kuile FO, et al. Evaluation of Plasmodium vivax malaria recurrence in Brazil. Malar J. 2019;18:1–10. 10.1186/s12936-019-2644-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Poespoprodjo JR, Fobia W, Kenangalem E, Lampah DA, Hasanuddin A, Warikar N, et al. Vivax malaria: a major cause of morbidity in early infancy. Clin Infect Dis. 2009;48:1704–1712. 10.1086/599041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Commons RJ, Simpson JA, Thriemer K, Chu CS, Douglas NM, Abreha T, et al. The haematological consequences of Plasmodium vivax malaria after chloroquine treatment with and without primaquine: a WorldWide Antimalarial Resistance Network systematic review and individual patient data meta-analysis. BMC Med. 2019;17:151. 10.1186/s12916-019-1386-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Boyd MF. Observations on naturally induced malaria. South Med J. 1934;27:155–159. [Google Scholar]
- 22.Ashley EA, Touabi M, Ahrer M, Hutagalung R, Htun K, Luchavez J, et al. Evaluation of three parasite lactate dehydrogenase-based rapid diagnostic tests for the diagnosis of falciparum and vivax malaria. Malar J. 2009/10/29. 2009;8:241. 1475-2875-8-241 [pii] 10.1186/1475-2875-8-241 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Maltha J, Gillet P, Cnops L, Van Den Ende J, Van Esbroeck M, Jacobs J. Malaria rapid diagnostic tests: Plasmodium falciparum infections with high parasite densities may generate false positive Plasmodium vivax pLDH lines. Malar J. 2010;9:1–7. 10.1186/1475-2875-9-198 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cunningham J, Jones S, Gatton ML, Barnwell JW, Cheng Q, Chiodini PL, et al. A review of the WHO malaria rapid diagnostic test product testing programme (2008–2018): Performance, procurement and policy. Malar J. 2019;18. 10.1186/s12936-019-3028-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.World Health Organization. World Malaria Report 2019. Geneva; 2019. Available from: https://www.who.int/publications-detail/world-malaria-report-2019
- 26.Imwong M, Hanchana S, Malleret B, Rénia L, Day NPJ, Dondorp AM, et al. High-throughput ultrasensitive molecular techniques for quantifying low-density malaria parasitemias. J Clin Microbiol. 2014;52: 3303–3309. 10.1128/JCM.01057-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Nguyen TN, von Seidlein L, Nguyen TV, Truong PN, Hung S Do, Pham HT, et al. The persistence and oscillations of submicroscopic Plasmodium falciparum and Plasmodium vivax infections over time in Vietnam: an open cohort study. Lancet Infect Dis. 2018;18:565–572. 10.1016/S1473-3099(18)30046-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.White NJ, Ashley EA, Recht J, Delves MJ, Ruecker A, Smithuis FM, et al. Assessment of therapeutic responses to gametocytocidal drugs in Plasmodium falciparum malaria. Malar J. 2014;13. 10.1186/1475-2875-13-483 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Taylor AR, Watson JA, Chu CS, Puaprasert K, Duanguppama J, Day NPJ, et al. Resolving the cause of recurrent Plasmodium vivax malaria probabilistically. Nat Commun. 2019;10:5595. 10.1038/s41467-019-13412-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Imwong M, Boel ME, Pagornrat W, Pimanpanarak M, McGready RM, Day NPJ, et al. The first Plasmodium vivax relapses of life are usually genetically homologous. J Infect Dis. 2012;205:680–3. 10.1093/infdis/jir806 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Imwong M, Snounou G, Pukrittayakamee S, Tanomsing N, Kim JR, Nandy A, et al. Relapses of Plasmodium vivax Infection Usually Result from Activation of Heterologous Hypnozoites. J Infect Dis. 2007;195: 927–933. 10.1086/512241 [DOI] [PubMed] [Google Scholar]
- 32.Stewart T, Marchand RP. Factors that affect the success and failure of insecticide treated net programs for malaria control in SE Asia and the Western Pacific. World Heal Organ. Geneva; 2003. Available from: http://www.who.int/malaria/publications/atoz/itn_r62.pdf [Google Scholar]
- 33.Smithuis FM, Kyaw MK, Phe UO, Van Der Broek I, Katterman N, Rogers C, et al. The effect of insecticide-treated bed nets on the incidence and prevalence of malaria in children in an area of unstable seasonal transmission in western Myanmar. Malar J. 2013;12. 10.1186/1475-2875-12-363 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kwansomboon N, Chaumeau V, Kittiphanakun P, Cerqueira D, Corbel V, Chareonviriyaphap T. Vector bionomics and malaria transmission along the Thailand-Myanmar border: a baseline entomologic survey. J Vector Biol. 2017;424: 84–93. [DOI] [PubMed] [Google Scholar]
- 35.Thomsen EK, Koimbu G, Pulford J, Jamea-Maiasa S, Ura Y, Keven JB, et al. Mosquito behavior change after distribution of bednets results in decreased protection against malaria exposure. J Infect Dis. 2017;215:790–797. 10.1093/infdis/jiw615 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.White MT, Walker P, Karl S, Hetzel MW, Freeman T, Waltmann A, et al. Mathematical modelling of the impact of expanding levels of malaria control interventions on Plasmodium vivax. Nat Commun. 2018;9:1–10. 10.1038/s41467-017-02088-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bayili K, N’do S, Namountougou M, Sanou R, Ouattara A, Dabiré RK, et al. Evaluation of efficacy of Interceptor® G2, a long-lasting insecticide net coated with a mixture of chlorfenapyr and alpha-cypermethrin, against pyrethroid resistant Anopheles gambiae s.l. in Burkina Faso. Malar J. 2017;16:1–9. 10.1186/s12936-017-1846-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ngufor C, Fagbohoun J, Critchley J, N’Guessan R, Todjinou D, Malone D, et al. Which intervention is better for malaria vector control: Insecticide mixture long-lasting insecticidal nets or standard pyrethroid nets combined with indoor residual spraying? Malar J. 2017;16:1–9. 10.1186/s12936-017-1987-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Protopopoff N, Mosha JF, Lukole E, Charlwood JD, Wright A, Mwalimu CD, et al. Effectiveness of a long-lasting piperonyl butoxide-treated insecticidal net and indoor residual spray interventions, separately and together, against malaria transmitted by pyrethroid-resistant mosquitoes: a cluster, randomised controlled, two-by-two fact. Lancet. 2018;391:1577–1588. 10.1016/S0140-6736(18)30427-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.van den Berg H, Zaim M, Yadav RS, Soares A, Ameneshewa B, Hii J, et al. Global Trends in the Use of Insecticides to Control Vector-Borne Diseases. Environ Health Perspect. 2012;120:577–582. Available from: 10.1289/ehp.1104340 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Mouchet J. Agriculture and Vector Resistance. Int J Trop Insect Sci. 1988;9:297–302. 10.1017/s1742758400006238 [DOI] [Google Scholar]
- 42.World Health Organization. Global report on insecticide resistance in malaria vectors: 2010–2016. Geneva;2018. Available from: https://www.who.int/malaria/publications/atoz/9789241514057/en/
- 43.Corbel V, N’Guessan R. Distribution, Mechanisms, Impact and Management of Insecticide Resistance in Malaria Vectors: A Pragmatic Review. IntechOpen. 2013. pp. 579–633. 10.5772/56117 [DOI] [Google Scholar]
- 44.van Bortel W, Trung HD, Thuan LK, Sochantha T, Socheat D, Sumrandee C, et al. The insecticide resistance status of malaria vectors in the Mekong region. Malar J. 2008;7:1–15. 10.1186/1475-2875-7-102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.World Health Organization. WHO malaria vaccine Rainbow tables. In: who.int; [Internet]. 2020. [cited 7 Aug 2020]. Available from: http://www.who.int/immunization/research/development/Rainbow_tables/en/ [Google Scholar]
- 46.Hoffman SL. The March Toward Malaria Vaccines. Am J Prev Med. 2015;49:S319–S333. 10.1016/j.amepre.2015.09.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Herrera S, Fernández OL, Vera O, Cárdenas W, Ramírez O, Palacios R, et al. Phase I safety and immunogenicity trial of Plasmodium vivax CS derived long synthetic peptides adjuvanted with montanide ISA 720 or montanide ISA 51. Am J Trop Med Hyg. 2011;84:12–20. 10.4269/ajtmh.2011.09-0516 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Bennett JW, Yadava A, Tosh D, Sattabongkot J, Komisar J, Ware LA, et al. Phase 1/2a trial of Plasmodium vivax malaria vaccine candidate VMP001/AS01B in malaria-naive adults: safety, immunogenicity, and efficacy. PLoS Negl Trop Dis. 2016;10:e0004423. 10.1371/journal.pntd.0004423 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Payne RO, Silk SE, Elias SC, Milne KH, Rawlinson TA, Llewellyn D, et al. Human vaccination against Plasmodium vivax Duffy-binding protein induces strain-transcending antibodies. JCI Insight. 2017;2:1–17. 10.1172/jci.insight.93683 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Malkin EM, Durbin AP, Diemert DJ, Sattabongkot J, Wu Y, Miura K, et al. Phase 1 vaccine trial of Pvs25H: A transmission blocking vaccine for Plasmodium vivax malaria. Vaccine. 2005;23:3131–3138. 10.1016/j.vaccine.2004.12.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Wu Y, Ellis RD, Shaffer D, Fontes E, Malkin EM, Mahanty S, et al. Phase 1 trial of malaria transmission blocking vaccine candidates Pfs25 and Pvs 25 formulated with montanide ISA 51. PLoS ONE. 2008;3. 10.1371/journal.pone.0002636 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Tham WH, Beeson JG, Rayner JC. Plasmodium vivax vaccine research–we’ve only just begun. Int J Parasitol. 2017;47:111–118. 10.1016/j.ijpara.2016.09.006 [DOI] [PubMed] [Google Scholar]
- 53.World Health Organization. Guidelines for the treatment of malaria, 3rd Edition. Geneva: World Health Organization; 2015. Available from: https://apps.who.int/iris/handle/10665/162441 [Google Scholar]
- 54.Ahmed R, Poespoprodjo JR, Syafruddin D, Khairallah C, Pace C, Lukito T, et al. Efficacy and safety of intermittent preventive treatment and intermittent screening and treatment versus single screening and treatment with dihydroartemisinin–piperaquine for the control of malaria in pregnancy in Indonesia: a cluster-randomised, open-la. Lancet Infect Dis. 2019;19:973–987. 10.1016/S1473-3099(19)30156-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Meltzer E, Rahav G, Schwartz E. Vivax malaria chemoprophylaxis: the role of atovaquone-proguanil compared to other options. Clin Infect Dis. 2018;66:1751–1755. 10.1093/cid/cix1077 [DOI] [PubMed] [Google Scholar]
- 56.Mikolajczak SA, Vaughan AM, Kangwanrangsan N, Roobsoong W, Fishbaugher M, Yimamnuaychok N, et al. Plasmodium vivax liver stage development and hypnozoite persistence in human liver-chimeric mice. Cell Host Microbe. 2015;17:526–535. 10.1016/j.chom.2015.02.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Gilder ME, Hanpithakphong W, Hoglund RM, Tarning J, Win HH, Hilda N, et al. Primaquine pharmacokinetics in lactating women and breastfed infant exposures. Clin Infect Dis. 2018;67:1000–7. 10.1093/cid/ciy235 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Baird JK, Sutanto I, Soebandrio A, Ekawati LL, Noviyanti R, Fernando D, et al. Evaluation of the efficacy and safety of tafenoquine co-administered with dihydroartemisinin-piperaquine for the radical cure (anti-relapse) of Plasmodium vivax malaria in Indonesia—INSPECTOR study. In ASTMH Annual Meeting. 2020. [Google Scholar]
- 59.Centers for Disease Control and Prevention. Change in Krintafel (tafenoquine) label [Internet]. 2020 [cited 30 Jul 2020]. Available from: https://www.cdc.gov/malaria/new_info/2020/tafenoquine_2020.html
- 60.Velez ID, Tran TH, Martin A, Sharma H, Rousell V, Hardaker L, et al. A randomized, open-label, non-comparative multicenter study to assess the pharmacokinetics, safety, and efficacy of tafenoquine in the treatment of pediatric subjects with Plasmodium vivax malaria (TEACH study). In ASTMH Annual Meeting. 2020. [Google Scholar]
- 61.Haston JC, Hwang J, Tan KR. Guidance for using tafenoquine for prevention and antirelapse therapy for malaria—United States, 2019 MMWR Morb Mortal Wkly Rep. 2019;68:1062–1068. 10.15585/mmwr.mm6846a4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.White NJ, Miller KD, Churchill FC, Berry C, Brown J, Williams SB, et al. Chloroquine Treatment of Severe Malaria in Children. N Engl J Med. 1988;319:1493–1500. 10.1056/NEJM198812083192301 [DOI] [PubMed] [Google Scholar]
- 63.Maguire J, Krisin, Marwoto H, Richie TL, Fryauff DJ, Baird JK. Mefloquine is highly efficacious against chloroquine-resistant Plasmodium vivax malaria and Plasmodium falciparum malaria in Papua, Indonesia. Clin Infect Dis. 2006;2197:1067–1072. Available from: http://cid.oxfordjournals.org/content/42/8/1067.short 10.1086/501357 [DOI] [PubMed] [Google Scholar]
- 64.Ratcliff A, Siswantoro H, Kenangalem E, Maristela R, Wuwung R, Laihad F, et al. Two fixed-dose artemisinin combinations for drug-resistant falciparum and vivax malaria in Papua, Indonesia: an open-label randomised comparison. Lancet. 2007;369:757–765. 10.1016/S0140-6736(07)60160-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Daher A, Pereira D, Lacerda MVG, Alexandre MAA, Nascimento CT, Alves De Lima E Silva JC, et al. Efficacy and safety of artemisinin-based combination therapy and chloroquine with concomitant primaquine to treat Plasmodium vivax malaria in Brazil: An open label randomized clinical trial RBR-79s56s RBR. Malar J. 2018;17:1–11. 10.1186/s12936-018-2192-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Grigg MJ, William T, Menon J, Barber BE, Wilkes CS, Rajahram GS, et al. Efficacy of artesunate-mefloquine for chloroquine-resistant Plasmodium vivax malaria in Malaysia: an open-label, randomized, controlled trial. Clin Infect Dis. 2016;62:1403–1411. 10.1093/cid/ciw121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Phyo AP, Lwin KM, Price RN, Ashley EA, Russell B, Sriprawat K, et al. Dihydroartemisinin-piperaquine versus chloroquine in the treatment of Plasmodium vivax malaria in Thailand: a randomized controlled trial. Clin Infect Dis. 2011;53:977–984. 10.1093/cid/cir631 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Smithuis F, Kyaw MK, Phe O, Win T, Aung PP, Oo APP, et al. Effectiveness of five artemisinin combination regimens with or without primaquine in uncomplicated falciparum malaria: an open-label randomised trial. Lancet Infect Dis. 2010;10:673–681. 10.1016/S1473-3099(10)70187-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Fukuda MM, Krudsood S, Mohamed K, Green JA, Warrasak S, Noedl H, et al. A randomized, double-blind, active-control trial to evaluate the efficacy and safety of a three day course of tafenoquine monotherapy for the treatment of Plasmodium vivax malaria. PLoS ONE. 2017;12:e0187376. 10.1371/journal.pone.0187376 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Pukrittayakamee S, Vanijanonta S, Chantra A, Clemens R, White NJ. Blood Stage Antimalarial Efficacy of Primaquine in Plasmodium vivax Malaria. J Infect Dis. 1994;169:932–935. 10.1093/infdis/169.4.932 [DOI] [PubMed] [Google Scholar]
- 71.Pukrittayakamee S, Imwong M, Singhasivanon P, Stepniewska K, Day NJ, White NJ. Effects of different antimalarial drugs on gametocyte carriage in P. vivax malaria. Am J Trop Med Hyg. 2008;79:378–84. Available from: http://www.ncbi.nlm.nih.gov/pubmed/18784229 [PubMed] [Google Scholar]
- 72.Baird JK, Leksana B, Masbar S, Fryauff DJ, Sutanihardja MA, Suradi, et al. Diagnosis of resistance to chloroquine by Plasmodium vivax: timing of recurrence and whole blood chloroquine levels. Am J Trop Med Hyg. 1997;56:621–626. 10.4269/ajtmh.1997.56.621 [DOI] [PubMed] [Google Scholar]
- 73.Hasugian AR, Purba HLE, Kenangalem E, Wuwung RM, Ebsworth EP, Maristela R, et al. Dihydroartemisinin-Piperaquine versus Artesunate-Amodiaquine: Superior Efficacy and Posttreatment Prophylaxis against Multidrug-Resistant Plasmodium falciparum and Plasmodium vivax Malaria. Clin Infect Dis. 2007;44:1067–1074. 10.1086/512677 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Pasaribu AP, Chokejindachai W, Sirivichayakul C, Tanomsing N, Chavez I, Tjitra E, et al. A randomized comparison of dihydroartemisinin-piperaquine and artesunate-amodiaquine combined with primaquine for radical treatment of vivax malaria in Sumatera, Indonesia. J Infect Dis. 2013;208: 1906–13. 10.1093/infdis/jit407 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Saravu K, Kumar R, Ashok H, Kundapura P, Kamath V, Kamath A, et al. Therapeutic assessment of chloroquine-primaquine combined regimen in adult cohort of Plasmodium vivax malaria from primary care centres in Southwestern India. PLoS ONE. 2016;11:e0157666. 10.1371/journal.pone.0157666 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Chu CS, Phyo AP, Lwin KM, Win HH, San T, Aung AA, et al. Comparison of the cumulative efficacy and safety of chloroquine, artesunate, and chloroquine-primaquine in Plasmodium vivax malaria. Clin Infect Dis. 2018;67:1543–1549. 10.1093/cid/ciy319 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Shumbej T, Jemal A, Worku A, Bekele F, Weldesenbet H. Therapeutic efficacy of chloroquine for treatment of Plasmodium vivax malaria cases in Guragae zone southern Central Ethiopia. BMC Infect Dis. 2019;19:4–9. 10.1186/s12879-019-4055-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Mesa-Echeverry E, Niebles-Bolívar M, Tobón-Castaño A. Chloroquine–primaquine therapeutic efficacy, safety, and plasma levels in patients with uncomplicated Plasmodium vivax malaria in a Colombian Pacific region. Am J Trop Med Hyg. 2019;100: 72–77. 10.4269/ajtmh.18-0655 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Rijal KR, Adhikari B, Ghimire P, Banjara MR, Das Thakur G, Hanboonkunupakarn B, et al. Efficacy of primaquine in preventing short- and long-latency Plasmodium vivax relapses in Nepal. J Infect Dis. 2019;220:448–456. 10.1093/infdis/jiz126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Costa MR, Martinez FE, Vieira JL. Chloroquine-resistant Plasmodium vivax, Brazilian Amazon. Emerg Infect Dis. 2007;13: 7–8. 10.3201/eid1307.061386 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Añez A, Moscoso M, Laguna Á, Garnica C, Melgar V, Cuba M, et al. Resistance of infection by Plasmodium vivax to chloroquine in Bolivia. Malar J. 2015;14:261. 10.1186/s12936-015-0774-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Xu S, Zeng W, Ngassa Mbenda HG, Liu H, Chen X, Xiang Z, et al. Efficacy of directly-observed chloroquine-primaquine treatment for uncomplicated acute Plasmodium vivax malaria in northeast Myanmar: A prospective open-label efficacy trial. Travel Med Infect Dis. 2020;36:101499. 10.1016/j.tmaid.2019.101499 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Russell B, Chalfein F, Prasetyorini B, Kenangalem E, Piera K, Suwanarusk R, et al. Determinants of in vitro drug susceptibility testing of Plasmodium vivax. Antimicrob Agents Chemother. 2008;52:1040–1045. 10.1128/AAC.01334-07 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Imwong M, Pukrittayakamee S, Looareesuwan S, Pasvol G, Poirriez J, White NJ, et al. Association of genetic mutations in Plasmodium vivax dhfr with resistance to sulfadoxine-pyrimethamine: geographical and clinical correlates. Antimicrob Agents Chemother. 2002;46:1161. 10.1128/AAC.45.11.3122-3127.2001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Hupalo DN, Luo Z, Melnikov A, Sutton PL, Rogov P, Escalante A, et al. Population genomics studies identify signatures of global dispersal and drug resistance in Plasmodium vivax. Nat Genet. 2016;48:953–958. 10.1038/ng.3588 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.White NJ. Determinants of relapse periodicity in Plasmodium vivax malaria. Malar J. 2011;10:297. 10.1186/1475-2875-10-297 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Recht J, Ashley EA, White NJ. Use of primaquine and glucose-6-phosphate dehydrogenase deficiency testing: divergent policies and practices in malaria endemic countries. PLoS Negl Trop Dis. 2018;12:e0006230. 10.1371/journal.pntd.0006230 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Duarte EC, Pang LW, Ribeiro LC, Fontes CJ. Association of subtherapeutic dosages of a standard drug regimen with failures in preventing relapses of vivax malaria. Am J Trop Med Hyg. 2001;65:471–476. 10.4269/ajtmh.2001.65.471 [DOI] [PubMed] [Google Scholar]
- 89.da Silva RSU, Pinto AY N, Calvosa VSP, De Souza JM. Esquemas terapêuticos encurtados para o tratamento de malária por Plasmodium vivax. Rev Soc Bras Med Trop. 2003;36:235–239. [PubMed] [Google Scholar]
- 90.Negreiros S, Farias S, Viana GMR, Okoth SA, Chenet SM, De Souza TMH, et al. Efficacy of chloroquine and primaquine for the treatment of uncomplicated Plasmodium vivax malaria in Cruzeiro do Sul, Brazil. Am J Trop Med Hyg. 2016;95:1061–1068. 10.4269/ajtmh.16-0075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Ladeia-Andrade S, Menezes MJ, de Sousa TN, Silvino ACR, de Carvalho JF, Salla LC, et al. Monitoring the efficacy of chloroquine-primaquine therapy for uncomplicated Plasmodium vivax malaria in the main transmission hot spot of Brazil. Antimicrob Agents Chemother. 2019;63:e01965–18. 10.1128/AAC.01965-18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Carmona-Fonseca J, Maestre A. Prevention of Plasmodium vivax malaria recurrence: Efficacy of the standard total dose of primaquine administered over 3 days. Acta Trop. 2009;112:188–192. 10.1016/j.actatropica.2009.07.024 [DOI] [PubMed] [Google Scholar]
- 93.Baird JK, Leksana B, Masbar S, Sutanihardja MA, Fryauff DJ, Subianto B. Whole Blood Chloroquine Concentrations with Plasmodium vivax Infection in Irian Jaya, Indonesia. Am J Trop Med Hyg. 1997;56:618–620. 10.4269/ajtmh.1997.56.618 [DOI] [PubMed] [Google Scholar]
- 94.Chu CS, Phyo AP, Turner C, Win HH, Poe NP, Yotyingaphiram W, et al. Chloroquine versus dihydroartemisinin-piperaquine with standard High-dose primaquine given either for 7 days or 14 days in Plasmodium vivax malaria. Clin Infect Dis. 2018;68:1311–1319. 10.1093/cid/ciy735 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Taylor WRJ, Thriemer K, von Seidlein L, Yuentrakul P, Assawariyathipat T, Assefa A, et al. Short-course primaquine for the radical cure of Plasmodium vivax malaria: a multicentre, randomised, placebo-controlled non-inferiority trial. Lancet. 2019;394:929–938. 10.1016/S0140-6736(19)31285-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Arnold J, Alving AS, Hockwald RS, Clayman CB, Dern RJ, Beutler E, et al. The effect of continuous and intermittent primaquine therapy on the relapse rate of Chesson strain vivax malaria. J Lab Clin Med. 1954;44:429–438. Available from: http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=13201852 [PubMed] [Google Scholar]
- 97.Leslie T, Mayan I, Mohammed N, Erasmus P, Kolaczinski J, Whitty CJM, et al. A randomised trial of an eight-week, once weekly primaquine regimen to prevent relapse of plasmodium vivax in Northwest Frontier Province, Pakistan. PLoS ONE. 2008;3:e2861. 10.1371/journal.pone.0002861 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Kheng S, Muth S, Taylor WRJ, Tops N, Kosal K, Sothea K, et al. Tolerability and safety of weekly primaquine against relapse of Plasmodium vivax in Cambodians with glucose-6-phosphate dehydrogenase deficiency. BMC Med. 2015;13:203. 10.1186/s12916-015-0441-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Alving AS, Arnold J, Hockwald RS, Clayman CB, Dern RJ, Beutler E, et al. Potentiation of the curative action of primaquine in vivax malaria by quinine and chloroquine. J Lab Clin Med. 1955;46:301–306. Available from: http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=13242948 [PubMed] [Google Scholar]
- 100.Bennett JW, Pybus BS, Yadava A, Tosh D, Sousa JC. Primaquine failure and cytochrome P-450 2D6 in Plasmodium vivax malaria. N Engl J Med. 2013;369:1380–1381. 10.1056/NEJMc1301936 [DOI] [PubMed] [Google Scholar]
- 101.Pybus BS, Marcsisin SR, Jin X, Deye G, Sousa JC, Li Q, et al. The metabolism of primaquine to its active metabolite is dependent on CYP 2D6. Malar J. 2013;12:212. 10.1186/1475-2875-12-212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Howes RE, Dewi M, Piel FB, Monteiro WM, Battle KE, Messina JP, et al. Spatial distribution of G6PD deficiency variants across malaria-endemic regions. Malar J. 2013;12:418. 10.1186/1475-2875-12-418 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Hockwald RS, Arnold J, Clayman CB, Alving AS. Toxicitiy of primaquine in negroes. JAMA. 1952;149:1568–1570. [DOI] [PubMed] [Google Scholar]
- 104.Rueangweerayut R, Bancone G, Harrell EJ, Beelen AP, Kongpatanakul S, Möhrle JJ, et al. Hemolytic potential of tafenoquine in female volunteers heterozygous for glucose-6-phosphate dehydrogenase (G6PD) deficiency (G6PD Mahidol variant) versus G6PD-normal volunteers. Am J Trop Med Hyg. 2017;97:702–711. 10.4269/ajtmh.16-0779 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Beutler E, Dern RJ, Alving AS. The hemolytic effect of primaquine IV. The relationship of cell age to hemolysis. J Lab Clin Med. 1954;44:439–442. Available from: http://www.translationalres.com/article/0022214354901638/fulltext [PubMed] [Google Scholar]
- 106.Minucci A, Moradkhani K, Hwang MJ, Zuppi C, Giardina B, Capoluongo E. Glucose-6-phosphate dehydrogenase (G6PD) mutations database: review of the “old” and update of the new mutations. Blood Cells Mol Dis. 2012;48:154–65. 10.1016/j.bcmd.2012.01.001 [DOI] [PubMed] [Google Scholar]
- 107.Thriemer K, Poespoprodjo J-R, Kenangalem E, Douglas NM, Sugiarto P, Anstey NM, et al. The risk of adverse clinical outcomes following treatment of Plasmodium vivax malaria with and without primaquine in Papua, Indonesia. PLoS Negl Trop Dis. 2020;79:1–17. 10.1371/journal.pntd.0008838 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Leslie T, Briceno M, Mayan I, Mohammed N, Klinkenberg E, Sibley CH, et al. The impact of phenotypic and genotypic G6PD deficiency on risk of Plasmodium vivax infection: a case-control study amongst Afghan refugees in Pakistan. PLoS Med. 2010;7:e1000283. 10.1371/journal.pmed.1000283 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Awab GR, Aaram F, Jamornthanyawat N, Suwannasin K, Pagornrat W, Watson JA, et al. Protective effect of Mediterranean-type glucose-6-phosphate dehydrogenase deficiency against Plasmodium vivax malaria. Elife. 2021; 10: e62448. 10.7554/eLife.62448 ; PMCID: PMC7884069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Recht J, Ashley EA, White NJ. Safety of 8-aminoquinoline antimalarial medicines. World Health Organization. Geneva: World Health Organization; 2014. Available from: https://www.who.int/malaria/publications/atoz/9789241506977/en/ [Google Scholar]
- 111.Monteiro WM, Moura-Neto JP, Recht J, Bassat Q, Lacerda MVG. Fatal primaquine-induced hemolysis in a patient with Plasmodium vivax malaria and G6PD A- variant in the Brazilian Amazon. Clin Infect Dis. 2016;62:1188. 10.1093/cid/ciw039 [DOI] [PubMed] [Google Scholar]
- 112.Green JA, Patel AK, Patel BR, Hussaini A, Harrell EJ, McDonald MJ, et al. Tafenoquine at therapeutic concentrations does not prolong Fridericia-corrected QT interval in healthy subjects. J Clin Pharmacol. 2014;54:995–1005. 10.1002/jcph.302 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Warrasak S, Euswas A, Fukuda MM, Ittiverakul M, Miller RS, Krudsood S, et al. Comparative ophthalmic assessment of patients receiving tafenoquine or chloroquine/primaquine in a randomized clinical trial for Plasmodium vivax malaria radical cure. Int Ophthalmol. 2018;39:1767–1782. 10.1007/s10792-018-1003-2 [DOI] [PubMed] [Google Scholar]
- 114.Ackert J, Mohamed K, Slakter JS, El-Harazi S, Berni A, Gevorkyan H, et al. Randomized placebo-controlled trial evaluating the ophthalmic safety of single-dose tafenoquine in healthy volunteers. Drug Saf. 2019;42:1103–1114. 10.1007/s40264-019-00839-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Duparc S, Chalon S, Miller S, Richardson N, Toovey S. Neurological and psychiatric safety of tafenoquine in Plasmodium vivax relapse prevention: a review. Malar J. 2020;19:1–18. 10.1186/s12936-020-03184-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Llanos-Cuentas A, Lacerda MVG, Hien TT, Vélez ID, Namaik-larp C, Chu CS, et al. Tafenoquine versus primaquine to prevent relapse of Plasmodium vivax malaria. N Engl J Med. 2019;380:229–241. 10.1056/NEJMoa1802537 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Lacerda MVG, Llanos-Cuentas A, Krudsood S, Lon C, Saunders DL, Mohammed R, et al. Single-dose tafenoquine to prevent relapse of Plasmodium vivax malaria. N Engl J Med. 2019;380:215–228. 10.1056/NEJMoa1710775 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.White NJ. Anti-malarial drug effects on parasite dynamics in vivax malaria. Malar J. 2021; 20: e161. 10.1186/s12936-021-03700-7 ; PMCID: PMC7981980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.St Jean PL, Xue Z, Carter N, Koh GCKW, Duparc S, Taylor M, et al. Tafenoquine treatment of Plasmodium vivax malaria: suggestive evidence that CYP2D6 reduced metabolism is not associated with relapse in the Phase 2b DETECTIVE trial. Malar J. 2016;15:97. 10.1186/s12936-016-1145-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Bancone G, Gornsawun G, Chu CS, Porn P, Pal S, Bansil P, et al. Validation of the quantitative point-of-care CareStart biosensor for assessment of G6PD activity in venous blood. PLoS ONE. 2018;13:e0196716. 10.1371/journal.pone.0196716 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Pal S, Bansil P, Bancone G, Hrutkay S, Kahn M, Gornsawun G, et al. Evaluation of a novel quantitative test for glucose-6-phosphate dehydrogenase deficiency: bringing quantitative testing for glucose-6-phosphate dehydrogenase deficiency closer to the patient. Am J Trop Med Hyg. 2018;100:213–221. 10.4269/ajtmh.18-0612 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Watson J, Taylor WRJ, Bancone G, Chu CS, Jittamala P, White NJ. Implications of current therapeutic restrictions for primaquine and tafenoquine in the radical cure of vivax malaria. PLoS Negl Trop Dis. 2018;12:e0006440. 10.1371/journal.pntd.0006440 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Fairley NH. Sidelights on malaria in man obtained by subinoculation experiments. Trans R Soc Trop Med Hyg. 1947;40:621–676. 10.1016/0035-9203(47)90025-4 [DOI] [PubMed] [Google Scholar]
- 124.McCarthy JS, Smith B, Reid M, Berman J, Marquart L, Dobbin C, et al. Blood schizonticidal activity and safety of tafenoquine when administered as chemoprophylaxis to healthy, nonimmune participants followed by blood stage Plasmodium falciparum challenge: a randomized, double-blind, placebo-controlled Phase 1b study. Clin Infect Dis. 2019;69:480–486. 10.1093/cid/ciy939 [DOI] [PubMed] [Google Scholar]
- 125.White NJ. The assessment of antimalarial drug efficacy. Trends Parasitol. 2002;18:458–464. 10.1016/s1471-4922(02)02373-5 [DOI] [PubMed] [Google Scholar]
- 126.von Seidlein L, Peto TJ, Landier J, Nguyen TN, Tripura R, Phommasone K, et al. The impact of targeted malaria elimination with mass drug administrations on falciparum malaria in southeast Asia: A cluster randomised trial. PLoS Med. 2019;16:1–26. 10.1371/journal.pmed.1002745 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Hsiang MS, Hwang J, Tao AR, Liu Y, Bennett A, Shanks GD, et al. Mass drug administration for the control and elimination of Plasmodium vivax malaria: an ecological study from Jiangsu province, China. Malar J. 2013;12:383. 10.1186/1475-2875-12-383 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Garfield RM, Vermund SH. Changes in malaria incidence after mass drug administration in Nicaragua. Lancet. 1983;322:500–503. 10.1016/s0140-6736(83)90523-8 [DOI] [PubMed] [Google Scholar]