Abstract
Background
Many mothers still give birth outside a health facility in Sub-Saharan Africa particularly in East African countries. Though there are studies on the prevalence and associated factors of health facility delivery, as to our search of literature there is limited evidence on the pooled prevalence and associated factors of health facility delivery in East Africa. This study aims to examine the pooled prevalence and associated factors of health facility delivery in East Africa based on evidence from Demographic and Health Surveys.
Methods
A secondary data analysis was conducted based on the most recent Demographic and Health Surveys (DHSs) conducted in the 12 East African countries. A total weighted sample of 141,483 reproductive-age women who gave birth within five years preceding the survey was included. All analyses presented in this paper were weighted for the sampling probabilities and non-response using sampling weight (V005), primary sampling unit (V023), and strata (V021). The analysis was done using STATA version 14 statistical software, and the pooled prevalence of health facility delivery with a 95% Confidence Interval (CI) was presented using a forest plot. For associated factors, the Generalized Linear Mixed Model (GLMM) was fitted to consider the hierarchical nature of the DHS data. The Intra-class Correlation Coefficient (ICC), Median Odds Ratio (MOR), and Likelihood Ratio (LR)-test were done to assess the presence of a significant clustering effect. Besides, deviance (-2LLR) was used for model comparison since the models were nested models. Variables with a p-value of less than 0.2 in the bivariable mixed-effect binary logistic regression analysis were considered for the multivariable analysis. In the multivariable mixed-effect analysis, the Adjusted Odds Ratio (AOR) with 95% Confidence Interval (CI) were reported to declare the strength and significance of the association between the independent variable and health facility delivery.
Results
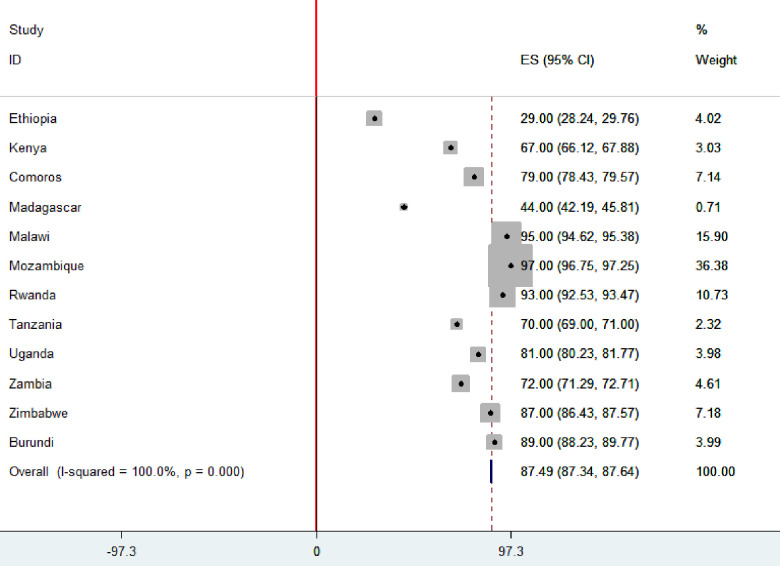
The proportion of health facility delivery in East Africa was 87.49% [95% CI: 87.34%, 87.64%], ranged from 29% in Ethiopia to 97% in Mozambique. In the Mixed-effect logistic regression model; country, urban residence [AOR = 2.08, 95% CI: 1.96, 2.17], primary women education [AOR = 1.61, 95% CI: 1.55, 1.67], secondary education and higher [AOR = 2.96, 95% CI: 2.79, 3.13], primary husband education [AOR = 1.19, 95% CI: 1.14, 1.24], secondary husband education [AOR = 1.38, 95% CI: 1.31, 1.45], being in union [AOR = 1.23, 95% CI: 1.18, 1.27], having occupation [AOR = 1.11, 95% CI: 1.07, 1.15], being rich [AOR = 1.36, 95% CI: 1.30, 1.41], and middle [AOR = 2.14, 95% CI: 2.04, 2.23], health care access problem [AOR = 0.76, 95% CI: 0.74, 0.79], having ANC visit [AOR = 1.54, 95% CI: 1.49, 1.59], parity [AOR = 0.56, 95% CI: 0.55, 0.61], multiple gestation [AOR = 1.83, 95% CI: 1.67, 2.01] and wanted pregnancy [AOR = 1.19, 95% CI: 1.13, 1.25] were significantly associated with health facility delivery.
Conclusion
This study showed that the proportion of health facility delivery in East African countries is low. Thus, improved access and utilization of antenatal care can be an effective strategy to increase health facility deliveries. Moreover, encouraging women through education is recommended to increase health facility delivery service utilization.
Background
Maternal and child mortality remains a major public health problem in low-and middle-income countries mainly in Sub-Saharan Africa (SSA) countries [1]. Globally, an estimated 358,000 maternal deaths occur annually, of which 99% occurred in low-and middle-income countries [2]. Even though the maternal mortality rate showed a substantial reduction in high-income countries [3], SSA continues to share the huge burden of global maternal mortality [4].
The World Health Organization (WHO) recommends health facility delivery as a key strategy to reduce maternal and infant mortality [5, 6]. According to the WHO, every pregnant woman should give birth at a health facility but only 48% of SSA births are delivered in a health facility [7, 8]. The lower proportion of health facility delivery is the reflection of poor affordability and accessibility of maternal health care services [9, 10].
Several studies found health facility delivery as a significant predictor responsible for the reduction of maternal and neonatal mortality [11, 12]. However, access to and use of maternal health care services in East African countries remains a major challenge [13, 14]. Previous revealed that maternal education [15], household wealth status [16], maternal occupation [17], husband education [18], distance to health facility [19], residence [20], parity [21], maternal age [20], marital status [22], Antenatal Care (ANC) visit during pregnancy [23, 24], type of gestation [24], and wanted pregnancy [25] were significantly associated factors with health facility delivery.
SSA is projected to have at least 80% of deliveries in health facilities particularly in East African countries, given international success in reducing maternal and neonatal mortality [26]. To improve health facility delivery in East African countries multisectoral collaboration is needed and international stakeholders might work on common factors responsible for the reduction of health facility delivery in different countries.
As far as our literature search is concerned, little is known about the pooled prevalence of health facility delivery and associated factors in East African countries. Therefore, this study aimed at investigating the pooled prevalence and associated factors of health facility delivery in East African Countries based on the most recent Demographic and Health Surveys (DHSs). The findings of this study may aid in the development of evidence-based public health policies to reduce maternal and newborn mortality. Furthermore, since this was a pooled analysis, the study power was increased, allowing for a thorough examination of effect modification within the data.
Methods
Data source and sampling procedures
The DHS data of 12 East African countries (Burundi, Ethiopia, Comoros, Uganda, Rwanda, Tanzania, Mozambique, Madagascar, Zimbabwe, Kenya, Zambia, and Malawi) [27] were used for this study. The DHS is a nationally representative survey that contains data on health and health-related indicators like mortality, morbidity, family planning service utilization, fertility, maternal and child health. The variables were extracted based on literature and appended together to determine the pooled prevalence and associated factors of health facility delivery in East Africa. The DHS employed a two-stage stratified sampling technique to select the study participants. In the first stage, Enumeration Areas (EAs) were randomly selected while in the second stage households were selected. Each country’s survey consists of different datasets including men, women, children, birth, and household datasets, and for this study, we used the women’s datasets (IR file). A total weighted sample of 141,483 reproductive-age women who gave birth in the last five years preceding the survey was included in this study (Table 1).
Table 1. The number of study participants in this study.
| Country | Number of reproductive age women who gave birth within 5 years preceding the survey | Study year | |
|---|---|---|---|
| Home delivery | Health facility delivery | ||
| Burundi | 1480 | 12131 | 2016/17 |
| Comoros | 604 | 2276 | 2012 |
| Ethiopia | 7809 | 3213 | 2016 |
| Kenya | 6436 | 13037 | 2014 |
| Madagascar | 7013 | 5394 | 2008/09 |
| Malawi | 791 | 16604 | 2015/16 |
| Mozambique | 285 | 11192 | 2011 |
| Rwanda | 537 | 7462 | 2014/15 |
| Tanzania | 3042 | 7010 | 2015/16 |
| Uganda | 2944 | 12326 | 2016 |
| Zambia | 3778 | 9564 | 2018 |
| Zimbabwe | 833 | 5585 | 2015 |
Study variables and measurements
The outcome variable for this study was the place of delivery. For mothers who had more than one child in the last five years preceding the survey, the most recent birth was selected. Place of delivery was categorized into home delivery (when the birth took place at home) or health facility delivery (when the birth took place at the hospital, health center, or health post). The response variable for the ith mother was represented by a random variable Yi with two possible values coded as 1 and 0. So, the response variable of the ith mother Yi was measured as a dichotomous variable with possible values Yi = 1, if ith mother gave birth at the health facility, and Yi = 0 if a mother gave birth at home delivery.
The independent variable retrieved from DHS were country, residence, maternal age, occupational status, women’s educational status, husband’s educational status, wealth status, distance to health care access, ANC visit during the index pregnancy, parity, marital status, preceding birth interval, number of gestation, and wanted pregnancy (Table 2). As the DHSs of the 12 East African countries were not conducted at the same time, we considered the year of the survey as an independent variable by considering 2008 as a reference. The Year of the survey was categorized as 2008 (Madagascar), 2011 (Mozambique), 2012 (Malawi), 2014 (Rwanda and Kenya), 2015 (Malawi, Tanzania, and Zimbabwe), 2016 (Burundi, Uganda, and Ethiopia), and 2018 (Zambia). However, the bi-variable analysis has a p-value of >0.2 and was not eligible for the multivariable analysis.
Table 2. The list of independent variables and their definitions and measurements.
| Variable name | Definition (measurement) |
|---|---|
| Country | Was coded as 0 “Burundi”, 1 “Comoros”, 2 “Ethiopia”, 3 “Kenya”, 4 “Madagascar”, 5 “Malawi”, 6 “Mozambique”, 7 “Rwanda”, 8 “Tanzania”, 9 “Uganda”, 10 “Zambia” and 11 “Zimbabwe” |
| Residence | Recoded as 0 for rural and 1 for urban |
| Age of respondent | Categorized as 0 for 15–24 years, 1 for 25–34 years and 2 for 35–49 years |
| Occupational status | Women occupation was No “if women were housewife and didn’t working”, and Yes “If a woman were working, she might be self-employed or government employed” |
| Maternal education status | Categorized as; didn’t have formal education, attained primary level of education, and “secondary education and above” |
| Husband education | Categorized as; didn’t have formal education, attained primary level of education, and “secondary education and above” |
| Wealth status | Categorized as; poor “if woman was in poorer and poorest household”, middle and rich “if woman was in richer and richest household” |
| Preceding birth interval | Was categorized as; less than 24 months and ≥ 24 months |
| ANC visit during pregnancy | Categorized as No “if woman didn’t have ANC visit during pregnancy” and Yes “If women had at least one ANC visit during pregnancy” |
| Distance to reach health facility | Categorized as;” A big problem” and “not a big problem” |
| Parity | Number of ever born children after 28 months of gestations categorized as; 1 birth, 2–4 birth, and ≥ 5 births |
| Number of gestations | Categorized as; single and multiple birth |
| Wanted pregnancy | Categorized as Yes “if wanted” and No “if mistimed or unwanted” |
| Marital status | Categorized as; not in union “if never married, divorced, widowed or separated” and in union “if married” |
Data management and analysis
We pooled the data from the 12 East African countries together after extracting the variables based on literature. Before any statistical analysis, the data were weighted using sampling weight (V005), primary sampling unit (V023), and strata (V021) to draw a valid conclusion. Data management and analysis were done using STATA version 14 statistical software. The pooled proportion of health facility delivery with the 95% Confidence Interval (CI) was reported using a forest plot. The hierarchical nature of DHS data could violate the independence of observations and equal variance assumption of the traditional logistic regression model. In such cases, advanced statistical models should be fitted to get a reliable estimate. Therefore, a mixed effect logistic regression model (fixed and random effect) was fitted using a cluster variable (V001) as a random variable. The presence of clustering effect was tested using the Intra-class Correlation Coefficient (ICC), Likelihood Ratio (LR) test, and Median Odds Ratio (MOR), and model comparison was made using deviance (-2LLR).
The ICC quantifies the degree of heterogeneity of health facility delivery between clusters (the proportion of the total observed individual variation in health facility delivery that is attributable to between cluster variations) [28].
MOR quantifies the variation or heterogeneity in health facility delivery between clusters and is defined as the median value of the odds ratio between the cluster at a high likelihood of health facility delivery and cluster at lower risk when randomly picking out two clusters (EAs) [29].
∂2 indicates that cluster variance.
Variables with a p-value <0.2 in the bi-variable analysis were considered in the multivariable mixed-effect logistic regression analysis. In the multivariable mixed-effect logistic regression model the Adjusted Odds Ratios (AOR) with a 95% Confidence Interval (CI) were reported to declare the statistical significance and strength of association between factors and health facility delivery.
Ethics consideration
Permission to get access to the data was obtained from the measure DHS program online request from http://www.dhsprogram.com.website and the data used were publicly available with no personal identifier.
Results
Socio-demographic and economic characteristics of the respondent
A total of 141,483 live births were included. Of these, 19,563 (13.8%) births were from Kenya, and 110,471 (78.1%) were in rural areas. Besides, 67,704 (47.9%) births were born to mothers aged 25–34 years. More than half (53.7%) of mothers and 41.9% of their husbands attained primary level of education (Table 3).
Table 3. Socio-demographic and economic characteristics of women who gave birth in the last five years in East African countries.
| Characteristics | Weighted frequency | Percentage (%) |
|---|---|---|
| Country | ||
| Burundi | 13,611 | 9.6 |
| Comoros | 2,880 | 2.0 |
| Ethiopia | 11,022 | 7.8 |
| Kenya | 19,563 | 13.8 |
| Madagascar | 12,407 | 8.8 |
| Malawi | 17,395 | 12.3 |
| Mozambique | 11,478 | 8.1 |
| Rwanda | 8,002 | 5.7 |
| Tanzania | 10,052 | 7.1 |
| Uganda | 15,270 | 10.8 |
| Zambia | 13,383 | 9.5 |
| Zimbabwe | 6,418 | 4.5 |
| Residence | ||
| Urban | 31,012 | 21.9 |
| Rural | 110,471 | 78.1 |
| Age in years | ||
| 15–24 | 42,167 | 29.8 |
| 25–34 | 67,704 | 47.9 |
| ≥ 35 | 31,612 | 22.3 |
| Women education status | ||
| No | 33,619 | 23.8 |
| Primary | 75,945 | 53.7 |
| Secondary and above | 31,907 | 22.5 |
| Husband education | ||
| No | 25,268 | 17.9 |
| Primary | 59,332 | 41.9 |
| Secondary and above | 56,882 | 40.2 |
| Women occupational status | ||
| No | 47,153 | 33.3 |
| Yes | 94,330 | 66.7 |
| Marital status | ||
| Not in union | 41,222 | 29.1 |
| In union | 100,261 | 70.9 |
| Wealth status | ||
| Poor | 64,368 | 45.5 |
| Middle | 27,586 | 19.5 |
| Rich | 49,529 | 35.0 |
Maternal obstetric and health services elated characteristics of the respondent
From a total of 141,483 births, 22,141 (15.7%) of the mothers were primipara, and 4,504 (3.2%) gave multiple births. About 93,360 (66.0%) of the mothers had ANC follow-up during pregnancy and 121,189 (85.7%) were wanted births. Regarding health care access, the majority (57.1%) of the mothers reported distance to reach a health facility as a big problem (Table 4).
Table 4. Maternal obstetric and health service-related characteristics of the respondent.
| Characteristics | Weighted frequency | Percentage (%) |
|---|---|---|
| Parity | ||
| 1 | 22,141 | 15.7 |
| 2–4 | 72,858 | 51.5 |
| ≥ 5 | 46,484 | 32.8 |
| Number of gestations | ||
| Single | 136,979 | 96.8 |
| Multiple | 4,504 | 3.2 |
| Preceding birth interval | ||
| < 24 months | 19,380 | 17.9 |
| ≥ 24 months | 88,934 | 82.1 |
| Health care access problem | ||
| No a big problem | 60,714 | 42.9 |
| A big problem | 80,769 | 57.1 |
| Wanted pregnancy | ||
| No | 20,294 | 14.3 |
| Yes | 121,189 | 85.7 |
| ANC visit during pregnancy | ||
| No | 48,123 | 34.0 |
| Yes | 93,360 | 66.0 |
ANC: Antenatal Care.
The pooled prevalence of institutional delivery in East African countries
The pooled proportion of health facility delivery in East African countries was 87.49% [95% CI: 87.34, 87.64], with the highest proportion in Mozambique (97%) and the lowest proportion in Ethiopia (29%) (Fig 1).
Fig 1. The proportion of health facility delivery in East African countries.
Factors associated with health facility delivery
Model comparison
The mixed-effect logistic regression model was the best-fitted model since it had a smaller deviance value (Table 5). Furthermore, the ICC value was 0.22 [95% CI: 0.21, 0.24] and MOR was 2. 52, it indicates if we randomly choose two women from different clusters, a woman from a cluster with higher health facility delivery were 2. 52 times more likely to deliver at a health facility than women from a cluster with a lower proportion of health facility. Besides, the likelihood ratio test was (LR test vs. Logistic model: X2 (01) = 6623.18, p<0.01) which informed that the mixed-effect logistic regression model is the better model over the basic model (Table 5).
Table 5. Model comparison and random effect results.
| Parameter | Standard logistic regression | Mixed-effect logistic regression analysis (GLMM) |
|---|---|---|
| LLR | -56792 | -55922 |
| Deviance | 113584 | 110844 |
| ICC | 0.22 [0.21, 0.24] | |
| LR-test | LR test vs. logistic model: chibar2(01) = 6623.18 Prob > = chibar2 <0.001 | |
| MOR | 2.52 [95% CI:2.41, 2.63] | |
| Cluster variance | 0.95 [95% CI: 0.86, 1.04] | |
*LLR; log-likelihood ratio, ICC; Intra-class Correlation Coefficient, MOR; Median Odds Ratio, LR-test; Likelihood Ratio test.
In the multivariable mixed-effect logistic regression model; country, residence, maternal and husband educational status, marital status, wealth status, maternal occupation, distance to the health facility, ANC visit during pregnancy, and wanted pregnancy was significantly associated with health facility delivery.
Mothers in Burundi, Kenya, Comoros, Malawi, Mozambique, Rwanda, Tanzania, Uganda, Zambia and Zimbabwe were 18.04 [AOR = 18.04, 95% CI: 16.65, 19.53], 1.97 [AOR = 1.97, 95% CI: 1.83, 2.12], 6.14 [AOR = 6.14, 95% CI: 5.48, 6.88], 36.99 [AOR = 36.99, 95% CI: 33.69, 40.62], 82.81 [AOR = 82.81, 95% CI: 72.66, 94.36], 22.89 [AOR = 22.89, 95% CI: 20.49, 25.58], 3.63 [AOR = 3.41, 95% CI: 3.18, 3.66], 6.67 [AOR = 6.67, 95% CI: 6.21, 7.16], 3.41 [AOR = 3.41, 95%: 3.18, 3.66] and 6.05 [AOR = 6.05, 95% CI: 5.46, 6.71] times higher odds of having health facility delivery compared to mothers in Ethiopia, respectively. Mothers who lived in urban area were 2.08 times [AOR = 2.08, 95% CI: 1.96, 2.17] higher odds of having health facility delivery than rural mothers.
Mothers who attained primary education, and secondary or above were 1.61 times [AOR = 1.61, 95% CI: 1.55, 1.67] and 2.96 times [AOR = 2.96, 95% CI: 2.79, 3.13] higher odds of having health facility delivery compared to mothers who did not have formal education, respectively. Mothers whose husband had a primary level of education, and secondary education or above were 1.19 times [AOR = 1.19, 95% CI: 1.14, 1.24] and 1.38 times [AOR = 1.38, 95% CI: 1.31, 1.45] higher odds of giving birth at a health facility than mother whose husband did not have formal education, respectively.
The odds of health facility delivery utilization by women who were in union were 1.23 times [AOR = 1.23, 95% CI: 1.18, 1.27] higher than women who were not in union, and mothers who had occupation were 1.11 times [AOR = 1.11, 95% CI: 1.07, 1.15] higher odds of having health facility than women who did not have an occupation. Women from a household with middle and rich wealth status were 1.36 [AOR = 1.36, 95% CI: 1.30, 1.41], and 2.14 [AOR = 2.14, 95% CI: 2.04, 2.23] times higher odds of health facility delivery than women from a poor household, respectively. The odds of health facility delivery among mothers who had a big health care access problem were decreased by 24% [AOR = 0.76, 95% CI: 0.74, 0.79] compared to women where health care access was not a big problem.
Mothers who had ANC follow-up during pregnancy had 1.54 [AOR = 1.54, 95% CI: 1.49, 1.59] times higher odds of health facility delivery than women who did not have ANC visit. The odds of health facility delivery among mothers who had two to four births, and five and above were decreased by 44% [AOR = 0.56, 95% CI: 0.55, 0.61] and 62% [AOR = 0.38, 95% CI: 0.35, 0.40] compared to women who were primipara, respectively. Mothers with multiple gestations were 1.83 [AOR = 1.83, 95% CI: 1.67, 2.01] times higher odds of delivering at a health facility compared to mothers with single gestation, and mothers whose pregnancy were wanted to have 1.19 [AOR = 1.19, 95% CI: 1.13, 1.25] times increased odds of health facility delivery (Table 6).
Table 6. Multivariable mixed-effect logistic regression analysis of determinants of health facility delivery in East African countries.
| Variable | Place of delivery | Crude Odds Ratio (COR) with 95% CI | Adjusted Odds Ratio (AOR) with 95% CI | |
|---|---|---|---|---|
| Home | Health facility | |||
| Country | ||||
| Burundi | 1480 | 12131 | 16.82 [15.67, 18.05] | 18.04 [16.65, 19.53] |
| Comoros | 604 | 2276 | 5.56 [5.01, 6.16] | 1.97 [1.83, 2.12] |
| Ethiopia | 7809 | 3213 | 1 | 1 |
| Kenya | 6437 | 13037 | 3.38 [3.19, 3.59] | 6.14 [5.48, 6.88] |
| Madagascar | 7013 | 5394 | 1.48 [1.40, 1.57] | 1.01 [0.94, 1.08] |
| Malawi | 791 | 16604 | 50.31 [46.08, 54.93] | 36.99 [33.69, 40.62] |
| Mozambique | 286 | 11192 | 77.15 [68.05, 87.47] | 82.81 [72.66, 94.36] |
| Rwanda | 537 | 7462 | 29.47 [26.63, 32.62] | 22.89 [20.49, 25.58] |
| Tanzania | 3042 | 7010 | 4.75 [4.47, 5.05] | 3.63 [3.37, 3.90] |
| Uganda | 2945 | 12326 | 7.78 [7.34, 8.25] | 6.67 [6.21, 7.16] |
| Zambia | 3778 | 9564 | 5.31 [5.01, 5.62] | 3.41 [3.18, 3.66] |
| Zimbabwe | 833 | 5585 | 14.25 [13.02, 15.60] | 6.05 [5.46, 6.71] |
| Residence | ||||
| Urban | 2997 | 22977 | 3.55 [3.41, 3.70] | 2.08 [1.96, 2.17] |
| Rural | 32557 | 77818 | 1 | 1 |
| Maternal education status | ||||
| No | 13920 | 19679 | 1 | 1 |
| Primary | 18482 | 57388 | 2.54 [2.47, 2.62] | 1.61 [1.55, 1.67] |
| Secondary and above | 3147 | 28722 | 7.16 [6.84, 7.48] | 2.96 [2.79, 3.13] |
| Husband education status | ||||
| No | 9797 | 15462 | 1 | 1 |
| Primary | 15623 | 43677 | 2.10 [2.04, 2.17] | 1.19 [1.14, 1.24] |
| Secondary and above | 10134 | 46657 | 3.25 [3.14, 3.37] | 1.38 [1.31, 1.45] |
| Respondent age in years | ||||
| 15–24 | 8908 | 33,219 | 1 | 1 |
| 25–34 | 17026 | 50611 | 0.78 [0.76, 0.81] | 1.05 [0.97, 1.10] |
| ≥35 | 9620 | 21965 | 0.60 [0.58, 0.62] | 1.05 [0.99, 1.11] |
| Marital status | ||||
| Not in union | 8256 | 32943 | 1 | 1 |
| In union | 27298 | 72852 | 0.63 [0.61, 0.65] | 1.23 [1.18, 1.27] |
| Maternal occupation status | ||||
| No | 12774 | 34277 | 1 | 1 |
| Yes | 22780 | 71518 | 1.26 [1.23, 1.30] | 1.11 [1.07, 1.15] |
| Wealth status | ||||
| Poor | 22262 | 42031 | 1 | 1 |
| Middle | 7075 | 20485 | 1.83 [1.77, 1.90] | 1.36 [1.30, 1.41] |
| Rich | 6217 | 43279 | 4.43 [4.28, 4.58] | 2.14 [2.04, 2.23] |
| Distance to health care access | ||||
| Not a big problem | 19282 | 66007 | 1 | 1 |
| Big problem | 16272 | 39788 | 0.71 [0.69, 0.73] | 0.76 [0.74, 0.79] |
| ANC visit during pregnancy | ||||
| No | 17064 | 30943 | 1 | 1 |
| Yes | 18490 | 74852 | 2.27 [2.22, 2.33] | 1.54 [1.49, 1.59] |
| Parity | ||||
| 1 | 2748 | 19390 | 1 | 1 |
| 2–4 | 16106 | 56683 | 0.50 [0.48, 0.52] | 0.56 [0.55, 0.61] |
| ≥ 5 | 16701 | 29721 | 0.25 [0.24, 0.27] | 0.38 [0.35, 0.40] |
| Number of gestations | ||||
| Single | 34689 | 102167 | 1 | 1 |
| Multiple | 865 | 3628 | 1.47 [1.36, 1.59] | 1.83 [1.67, 2.01] |
| Wanted pregnancy | ||||
| No | 6661 | 14031 | 1 | 1 |
| Yes | 29394 | 91763 | 1.36 [1.31, 1.41] | 1.19 [1.13, 1.25] |
Discussion
In East Africa, the proportion of health facility delivery was 87.49%. This was higher than a study reported in SSA [8]. The possible explanation could be due to the difference in the study period and the number of countries included in the study. It was significantly varied across counties, ranging from 29% in Ethiopia to 97% in Mozambique. This may be because of the lack of sufficient medical care and human resources in the Ethiopian health system to satisfy more than 100 million Ethiopians [30].
In the multivariable mixed effect binary logistic regression analysis; country, residence, maternal education status, husband education status, marital status, household wealth status, ANC visit during pregnancy, wanted pregnancy, health care access problem, parity, number of gestations, and occupational status were significantly associated with health facility delivery. In this study, the mother’s place of residence was significantly associated with health facility delivery. Urban mothers had higher odds of having health facility delivery than rural mothers. This is consistent with studies reported in SSA [31] and Africa [32]. This might be due to the residential disparity in availability and accessibilities of maternal health care services [33, 34]. Also, in urban areas maternal education [35], access to maternal health services [36], and access to information is relatively good than rural mothers [17, 34]. Furthermore, evidence suggests that the majority of women in rural areas preferred to give birth at home with traditional birth attendants for the sake of privacy and social acceptance than urban mothers [6].
Women who attained primary education or higher were more likely to give birth at a health facility than women with no formal education. It was in line with studies reported in Sub-Saharan Africa [31], China [37], and the WHO Global survey [38]. This may be because educated mothers would have a better understanding of the risks of childbirth, the provision of maternal health care, and the value of health facility delivery for newborns and their health [39]. In addition, maternal education plays a significant role in enhancing the mother’s health care decision-making autonomy [40]. Besides, husband education was a significant predictor of health facility delivery, women whose husbands completed primary education or higher were more likely to deliver in the health facility than women whose husbands did not have formal education. It was supported by previous studies reported in Pakistan [18], Nigeria [41], Nepal [42], and Sub-Saharan Africa [43]. This might be since educated husbands can empower women in making health care decisions and get involved in making birth preparedness and complication preparedness plan would also increase the center’s service use [44]. Besides, educated men would have better access to information about the importance of health facility delivery and complications of home delivery to the mother and their baby [45], and in fact, education leads to better health awareness, which may sensitize the mother to decide and utilize maternal health care services [46].
Being married had higher odds of health facility delivery than women who were not in a union. It was consistent study findings in Kenya [47] and Nigeria [41]. This might be due to married women had spousal support in making health care decisions towards maternal health service utilization as well as economic and social support [48]. Besides, when women pregnant without being in union are possibly less motivated to give birth at a health facility due to community stigmatization and marginalization [49].
Household wealth status and women’s occupation were found to be significant predictors of health facility delivery. Women who were from the household with middle and rich wealth stratus were more likely to give birth at a health facility than women who were from poor households. It was consistent with the study findings in Nepal [50] and SSA [31]. In some African countries such as Ethiopia, Tanzania, and Kenya, even though maternal health services are offered free of charge by law or pro-poor fee exemption [51], indirect costs such as transportation costs and other opportunity costs for mothers and newborns prohibit mothers from using health facility delivery from poor families [52].
In this study, parity was an important predictor of health facility delivery. Primiparous women had higher odds of health facility delivery than multi-parous women. This finding was supported by previous studies [20, 21, 41], it could be because primigravida women feel that they are more prone to complications during delivery and seek maternity care services [53]. Besides, Multiparous women often choose to give birth at home for the sake of privacy and feel they will not be complicated as they are familiar with childbirth [54]. Besides, multiparous women are the least likely to seek maternity care services due to greater confidence and cumulative experience of delivery [54]. Having an ANC visit during pregnancy increases the likelihood of health facility delivery than women who did not have ANC visits during pregnancy. It was consistent with previous studies [18, 55], this is attributed to the assumption that mothers who have ANC visit during pregnancy may increase women’s knowledge of birth preparedness and risks of pregnancy and childbirth, which may increase the possibility of getting delivery at health facilities [56, 57]. Furthermore, the use of ANC may signify the availability of a nearby health care service, which may also provide delivery care, and ANC providers should educate and advise women and their families on danger signs through a process to create individual birth plans that can prepare them for institutional delivery and make timely decisions in the event of an emergency to pursue health care [17]. Mothers whose pregnancy was wanted to have higher odds of health facility delivery than an unwanted pregnancy. When pregnancy is wanted, pregnant women may have ANC visits and regular medical check-ups, which could increase their knowledge of potential complications and safe delivery practices, ultimately encouraging them to pursue health facility delivery to get a healthy child [58].
The other most significant predictor of health facility delivery in this study was the type of gestation. Mothers who have multiple gestations had higher odds of health facility delivery than singletons. This was consistent with prior studies [24, 59], This may be because mothers with multiple gestations are at greater risk of complications related to pregnancy, such as obstructed labor, birth asphyxia, antepartum hemorrhage, preeclampsia, and postpartum hemorrhage [60], which may encourage women to give birth in a health facility. Besides, the health care access problem was associated with a lower likelihood of health facility delivery. This could be due to the reason that the health care access problem is the main factor for home delivery, it highlights that there is a need to make maternal health care services available and accessible to the community.
Though enhancing health facility delivery is identified as the best strategy to achieve the Sustainable Development Goal (SDG) 3 of ending preventable maternal mortality and reducing Maternal Mortality Ratio (MMR) to fewer than 70 maternal death per 100,000 live births by 2030, health facility delivery was low in East African countries. Therefore, the stakeholders, governmental and non-governmental organizations should promote health facility delivery through enhancing mothers’ ANC service utilization, and promoting women’s education. Besides, special emphasis should be given to rural residents and poor households to improve health facility delivery. Even though the World Health Organization’s recommendation for every pregnant woman to give birth at the health facility and by a skilled birth attendant, the rate remains low in East African countries. This may be because women need effective support to decrease home delivery practice. It is therefore important to improve women, family, and community awareness about institutional delivery, ANC follows up, and knowledge of danger signs of pregnancy.
Strength and limitations
The strength of this study was that it was based on a weighted large, nationally representative data set and could have adequate statistical power to detect the true association of factors with health facility delivery. Besides, the study is done using an advanced model to take into account the clustering effect (mixed-effect logistic regression) to get reliable standard error and estimate. However, the study finding is interpreted in light of limitations. First, as with other cross-sectional studies, the temporal relationship can’t be established. Second, the DHS didn’t incorporate information about health care availability and accessibility like distance to the health facility, and the quality of maternal health services provided which might influence the use of health facility delivery of reproductive-age women. Also, since data was collected from self-report from respondents there may be a possibility of social desirability bias.
Conclusions
This study found that health facility delivery in East Africa was far below to achieve a sustainable development goal. Country, urban residence, maternal education, husband education, multiple gestations, wanted pregnancy, ANC visit during pregnancy, middle and rich wealth status, having an occupation, and married marital status was positively associated with health facility delivery. Whereas, multiparty, and big health care access problem was negatively associated with health facility delivery. Thus, improved access and utilization of antenatal care can be an effective strategy to increase health facility deliveries. Moreover, encouraging women through education is recommended to increase health facility delivery service utilization.
Acknowledgments
We greatly acknowledge MEASURE DHS for granting access to the East African DHS data sets.
Abbreviations
- ANC
Antenatal Care
- AOR
Adjusted Odds Ratio
- CI
Confidence Interval
- DHS
Demographic Health Survey
- GLMM
Generalized Linear Mixed Models
- ICC
Intra-class Correlation Coefficient
- LLR
log-likelihood Ratio
- LR
Likelihood Ratio
- MOR
Median Odds Ratio
- SSA
Sub-Saharan Africa
- WHO
World Health Organization
Data Availability
The underlying data is available online from www.measuredhs.com.
Funding Statement
The author(s) received no specific funding for this work.
References
- 1.De Brouwere V, De Brouwere V, Tonglet R, Van Lerberghe W: Strategies for reducing maternal mortality in developing countries: what can we learn from the history of the industrialized West? Tropical medicine & international health 1998, 3(10):771–782. 10.1046/j.1365-3156.1998.00310.x [DOI] [PubMed] [Google Scholar]
- 2.Zureick-Brown S, Newby H, Chou D, Mizoguchi N, Say L, Suzuki E, et al. Understanding global trends in maternal mortality. International perspectives on sexual and reproductive health 2013, 39(1). 10.1363/3903213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.McClure EM, Goldenberg RL, Bann CM: Maternal mortality, stillbirth and measures of obstetric care in developing and developed countries. International Journal of Gynecology & Obstetrics 2007, 96(2):139–146. 10.1016/j.ijgo.2006.10.010 [DOI] [PubMed] [Google Scholar]
- 4.MAKU17 OE, OGWUMIKE FO, SANGOSANYA19 AO: Sub-Saharan Africa (SSA) and the millenium development goals (MDGs): Performance and strategic options. MILLENNIUM DEVELOPMENT GOALS (MDGS) AS INSTRUMENTS FOR DEVELOPMENT IN AFRICA 2014:305. [Google Scholar]
- 5.Claeson M, Bos ER, Mawji T, Pathmanathan I: Reducing child mortality in India in the new millennium. Bulletin of the World Health Organization 2000, 78:1192–1199. [PMC free article] [PubMed] [Google Scholar]
- 6.Titaley CR, Hunter CL, Dibley MJ, Heywood P: Why do some women still prefer traditional birth attendants and home delivery?: a qualitative study on delivery care services in West Java Province, Indonesia. BMC pregnancy and childbirth 2010, 10(1):43. 10.1186/1471-2393-10-43 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Magadi MA, Zulu EM, Brockerhoff M: The inequality of maternal health care in urban sub‐Saharan Africa in the 1990s. Population studies 2003, 57(3):347–366. 10.1080/0032472032000137853 [DOI] [PubMed] [Google Scholar]
- 8.Doctor HV, Nkhana-Salimu S, Abdulsalam-Anibilowo M: Health facility delivery in sub-Saharan Africa: successes, challenges, and implications for the 2030 development agenda. BMC public health 2018, 18(1):765. 10.1186/s12889-018-5695-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Organization WH: World health statistics 2010: World Health Organization; 2010. [Google Scholar]
- 10.UNICEF., Fund UNCs: The state of the world’s children 2009: maternal and newborn health, vol. 9: Unicef; 2008. [Google Scholar]
- 11.Paul BK, Rumsey DJ: Utilization of health facilities and trained birth attendants for childbirth in rural Bangladesh: an empirical study. Social science & medicine 2002, 54(12):1755–1765. 10.1016/s0277-9536(01)00148-4 [DOI] [PubMed] [Google Scholar]
- 12.Darmstadt GL, Lee AC, Cousens S, Sibley L, Bhutta ZA, Donnay F, et al. 60 million non‐facility births: Who can deliver in community settings to reduce intrapartum‐related deaths? International Journal of Gynecology & Obstetrics 2009, 107(Supplement):S89–S112. 10.1016/j.ijgo.2009.07.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Parkhurst JO, Penn-Kekana L, Blaauw D, Balabanova D, Danishevski K, Rahman SA, et al. Health systems factors influencing maternal health services: a four-country comparison. Health policy 2005, 73(2):127–138. 10.1016/j.healthpol.2004.11.001 [DOI] [PubMed] [Google Scholar]
- 14.Filippi V, Ronsmans C, Campbell OM, Graham WJ, Mills A, Borghi J, et al. Maternal health in poor countries: the broader context and a call for action. The Lancet 2006, 368(9546):1535–1541. 10.1016/S0140-6736(06)69384-7 [DOI] [PubMed] [Google Scholar]
- 15.Aggarwal R, Thind A: Effect of maternal education on choice of location for delivery among Indian women. 2011. [PubMed] [Google Scholar]
- 16.Phiri SNa, Kiserud T, Kvåle G, Byskov J, Evjen-Olsen B, Michelo C, et al. Factors associated with health facility childbirth in districts of Kenya, Tanzania and Zambia: a population based survey. BMC pregnancy and childbirth 2014, 14(1):219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gabrysch S, Campbell OM: Still too far to walk: literature review of the determinants of delivery service use. BMC pregnancy and childbirth 2009, 9(1):34. 10.1186/1471-2393-9-34 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Agha S, Carton TW: Determinants of institutional delivery in rural Jhang, Pakistan. International journal for equity in health 2011, 10(1):31. 10.1186/1475-9276-10-31 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lohela TJ, Campbell OM, Gabrysch S: Distance to care, facility delivery and early neonatal mortality in Malawi and Zambia. PloS one 2012, 7(12). 10.1371/journal.pone.0052110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ononokpono DN, Odimegwu CO: Determinants of maternal health care utilization in Nigeria: a multilevel approach. The Pan African Medical Journal 2014, 17(Suppl 1). 10.11694/pamj.supp.2014.17.1.3596 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gitonga E, Muiruri F: Determinants of health facility delivery among women in Tharaka Nithi county, Kenya. The Pan African Medical Journal 2016, 25(Suppl 2). 10.11604/pamj.supp.2016.25.2.10273 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Onah HE, Ikeako LC, Iloabachie GC: Factors associated with the use of maternity services in Enugu, southeastern Nigeria. Social science & medicine 2006, 63(7):1870–1878. 10.1016/j.socscimed.2006.04.019 [DOI] [PubMed] [Google Scholar]
- 23.Rockers PC, Wilson ML, Mbaruku G, Kruk ME: Source of antenatal care influences facility delivery in rural Tanzania: a population-based study. Maternal and Child Health Journal 2009, 13(6):879. 10.1007/s10995-008-0412-7 [DOI] [PubMed] [Google Scholar]
- 24.Samuelson JL, Buehler JW, Norris D, Sadek R: Maternal characteristics associated with place of delivery and neonatal mortality rates among very‐low‐birthweight infants, Georgia. Paediatric and perinatal epidemiology 2002, 16(4):305–313. 10.1046/j.1365-3016.2002.00450.x [DOI] [PubMed] [Google Scholar]
- 25.Fotso J-C, Ezeh A, Madise N, Ziraba A, Ogollah R: What does access to maternal care mean among the urban poor? Factors associated with use of appropriate maternal health services in the slum settlements of Nairobi, Kenya. Maternal and child health journal 2009, 13(1):130–137. 10.1007/s10995-008-0326-4 [DOI] [PubMed] [Google Scholar]
- 26.Moyer CA, Dako-Gyeke P, Adanu RM: Facility-based delivery and maternal and early neonatal mortality in sub-Saharan Africa: a regional review of the literature. African journal of reproductive health 2013, 17(3):30–43. [PubMed] [Google Scholar]
- 27.https://www.dhsprogram.com/Data. In.
- 28.Rodriguez G, Elo I: Intra-class correlation in random-effects models for binary data. The Stata Journal 2003, 3(1):32–46. [Google Scholar]
- 29.Merlo J, Chaix B, Ohlsson H, Beckman A, Johnell K, Hjerpe P, et al. A brief conceptual tutorial of multilevel analysis in social epidemiology: using measures of clustering in multilevel logistic regression to investigate contextual phenomena. Journal of Epidemiology & Community Health 2006, 60(4):290–297. 10.1136/jech.2004.029454 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Girma S, Kitaw Y, Ye-Ebiy Y, Seyoum A, Desta H, Teklehaimanot A: Human resource development for health in Ethiopia: challenges of achieving the millennium development goals. The Ethiopian Journal of Health Development (EJHD) 2007, 21(3). [Google Scholar]
- 31.Moyer CA, Mustafa A: Drivers and deterrents of facility delivery in sub-Saharan Africa: a systematic review. Reproductive health 2013, 10(1):40. 10.1186/1742-4755-10-40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Stephenson R, Baschieri A, Clements S, Hennink M, Madise N: Contextual influences on the use of health facilities for childbirth in Africa. American journal of public health 2006, 96(1):84–93. 10.2105/AJPH.2004.057422 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gage AJ, Guirlène Calixte M: Effects of the physical accessibility of maternal health services on their use in rural Haiti. Population studies 2006, 60(3):271–288. 10.1080/00324720600895934 [DOI] [PubMed] [Google Scholar]
- 34.Gage AJ: Barriers to the utilization of maternal health care in rural Mali. Social science & medicine 2007, 65(8):1666–1682. 10.1016/j.socscimed.2007.06.001 [DOI] [PubMed] [Google Scholar]
- 35.Raghupathy S: Education and the use of maternal health care in Thailand. Social science & medicine 1996, 43(4):459–471. 10.1016/0277-9536(95)00411-4 [DOI] [PubMed] [Google Scholar]
- 36.Haggerty JL, Roberge D, Lévesque J-F, Gauthier J, Loignon C: An exploration of rural–urban differences in healthcare-seeking trajectories: Implications for measures of accessibility. Health & place 2014, 28:92–98. 10.1016/j.healthplace.2014.03.005 [DOI] [PubMed] [Google Scholar]
- 37.Zhao J, Zhao Y, Du M, Binns CW, Lee AH: Maternal education and breastfeeding practices in China: a systematic review and meta-analysis. Midwifery 2017, 50:62–71. 10.1016/j.midw.2017.03.011 [DOI] [PubMed] [Google Scholar]
- 38.Karlsen S, Say L, Souza J-P, Hogue CJ, Calles DL, Gülmezoglu AM, et al. The relationship between maternal education and mortality among women giving birth in health care institutions: analysis of the cross sectional WHO Global Survey on Maternal and Perinatal Health. BMC public health 2011, 11(1):606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Mpembeni RN, Killewo JZ, Leshabari MT, Massawe SN, Jahn A, Mushi D, et al. Use pattern of maternal health services and determinants of skilled care during delivery in Southern Tanzania: implications for achievement of MDG-5 targets. BMC pregnancy and childbirth 2007, 7(1):29. 10.1186/1471-2393-7-29 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Acharya DR, Bell JS, Simkhada P, Van Teijlingen ER, Regmi PR: Women’s autonomy in household decision-making: a demographic study in Nepal. Reproductive health 2010, 7(1):15. 10.1186/1742-4755-7-15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Dahiru T, Oche OM: Determinants of antenatal care, institutional delivery and postnatal care services utilization in Nigeria. Pan African medical journal 2015, 21(1). 10.11604/pamj.2015.21.321.6527 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Thapa DK, Niehof A: Women’s autonomy and husbands’ involvement in maternal health care in Nepal. Social Science & Medicine 2013, 93:1–10. 10.1016/j.socscimed.2013.06.003 [DOI] [PubMed] [Google Scholar]
- 43.Hill J, Hoyt J, van Eijk AM, D’Mello-Guyett L, ter Kuile FO, Steketee R, et al. Factors affecting the delivery, access, and use of interventions to prevent malaria in pregnancy in sub-Saharan Africa: a systematic review and meta-analysis. PLoS medicine 2013, 10(7). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Iliyasu Z, Abubakar IS, Galadanci HS, Aliyu MH: Birth preparedness, complication readiness and fathers’ participation in maternity care in a northern Nigerian community. African journal of reproductive health 2010, 14(1). [PubMed] [Google Scholar]
- 45.Kakaire O, Kaye DK, Osinde MO: Male involvement in birth preparedness and complication readiness for emergency obstetric referrals in rural Uganda. Reproductive health 2011, 8(1):12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Mangeni JN, Nwangi A, Mbugua S, Mukthar V: Male involvement in maternal healthcare as a determinant of utilisation of skilled birth attendants in Kenya. East African medical journal 2012, 89(11):372–383. [PubMed] [Google Scholar]
- 47.Kitui J, Lewis S, Davey G: Factors influencing place of delivery for women in Kenya: an analysis of the Kenya demographic and health survey, 2008/2009. BMC pregnancy and childbirth 2013, 13(1):40. 10.1186/1471-2393-13-40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Furuta M, Salway S: Women’s position within the household as a determinant of maternal health care use in Nepal. International family planning perspectives 2006:17–27. 10.1363/3201706 [DOI] [PubMed] [Google Scholar]
- 49.Ono M, Matsuyama A, Karama M, Honda S: Association between social support and place of delivery: a cross-sectional study in Kericho, Western Kenya. BMC pregnancy and childbirth 2013, 13(1):214. 10.1186/1471-2393-13-214 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Karkee R, Lee AH, Khanal V: Need factors for utilisation of institutional delivery services in Nepal: an analysis from Nepal Demographic and Health Survey, 2011. BMJ open 2014, 4(3):e004372. 10.1136/bmjopen-2013-004372 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Bitrán R, Giedion U: Waivers and exemptions for health services in developing countries. Final draft. World Bank 2002, 89. [Google Scholar]
- 52.Ensor T, Cooper S: Overcoming barriers to health service access: influencing the demand side. Health policy and planning 2004, 19(2):69–79. 10.1093/heapol/czh009 [DOI] [PubMed] [Google Scholar]
- 53.Mishra US, Ramanathan M: Delivery-related complications and determinants of caesarean section rates in India. Health Policy and Planning 2002, 17(1):90–98. 10.1093/heapol/17.1.90 [DOI] [PubMed] [Google Scholar]
- 54.Fawsitt CG, Bourke J, Lutomski JE, Meaney S, McElroy B, Murphy R, et al. What women want: exploring pregnant women’s preferences for alternative models of maternity care. Health policy 2017, 121(1):66–74. 10.1016/j.healthpol.2016.10.010 [DOI] [PubMed] [Google Scholar]
- 55.Berhan Y, Berhan A: Antenatal care as a means of increasing birth in the health facility and reducing maternal mortality: a systematic review. Ethiopian journal of health sciences 2014, 24:93–104. 10.4314/ejhs.v24i0.9s [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Mbalinda SN, Nakimuli A, Kakaire O, Osinde MO, Kakande N, Kaye DK: Does knowledge of danger signs of pregnancy predict birth preparedness? A critique of the evidence from women admitted with pregnancy complications. Health Research Policy and Systems 2014, 12(1):60. 10.1186/1478-4505-12-60 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Moran AC, Sangli G, Dineen R, Rawlins B, Yaméogo M, Baya B: Birth-preparedness for maternal health: findings from Koupéla district, Burkina Faso. Journal of health, population, and nutrition 2006, 24(4):489. [PMC free article] [PubMed] [Google Scholar]
- 58.Fischer RC, Stanford JB, Jameson P, DeWitt MJ: Exploring the concepts of intended, planned, and wanted pregnancy. Journal of Family Practice 1999, 48:117–122. [PubMed] [Google Scholar]
- 59.Young BC, Wylie BJ: Effects of twin gestation on maternal morbidity. In: Seminars in perinatology: 2012: Elsevier; 2012: 162–168. [DOI] [PubMed] [Google Scholar]
- 60.Rao A, Sairam S, Shehata H: Obstetric complications of twin pregnancies. Best practice & research Clinical obstetrics & gynaecology 2004, 18(4):557–576. 10.1016/j.bpobgyn.2004.04.007 [DOI] [PubMed] [Google Scholar]