Abstract
The National Institute for Health and Care Excellence (NICE) describe “post COVID-19 syndrome” or “Long COVID” as a set of persistent physical, cognitive and/or psychological symptoms that continue for more than 12 weeks after illness and which are not explained by an alternative diagnosis. These symptoms are experienced not only by patients discharged from hospital but also those in the community who did not require inpatient care. To support the recovery of this group of people, a unique integrated rehabilitation pathway was developed following extensive service evaluations by Leeds Primary Care Services, Leeds Community Healthcare NHS Trust and Leeds Teaching Hospital NHS Trust. The pathway aligns itself to the NHS England “Five-point plan” to embed post-COVID-19 syndrome assessment clinics across England, supporting the comprehensive medical assessment and rehabilitation intervention for patients in the community. The pathway was first of its kind to be set up in the UK and comprises of a three-tier service model (level 1: specialist MDT service, level 2: community therapy teams and level 3: self-management). The MDT service brings together various disciplines with specialist skill sets to provide targeted individualized interventions using a specific core set of outcome measures including C19-YRS (Yorkshire Rehabilitation Scale). Community and primary care teams worldwide need such an integrated multidisciplinary comprehensive model of care to deal with the growing number of cases of post-COVID-19 syndrome effectively and in a timely manner.
Keywords: Post-COVID-19 condition, rehabilitation, community health, core set, C19-YRS
Background
At the time of writing, the COVID-19 pandemic has caused over 120 million infections and over 2 million deaths worldwide. The United Kingdom is one of the worst affected countries, with over 4 million confirmed cases and over 126 000 deaths.1 Up-to December 14, 2020, the city of Leeds in the North of England continued to experience high infection rates with 4795.4 cases per 100 000 compared to a 2875.8 national average.2 Whilst COVID-19 initially presents as an acute respiratory illness, the long-term emerging multi system impacts of the disease are now being appreciated by the medical community.3 This recognition has in large part been driven both by the advocacy of those experiencing post-COVID-19 syndrome and by the medical and scientific community.4
The National Institute for Health and Care Excellence (NICE) describe “post COVID-19 syndrome” or “Long COVID” as a set of persistent physical, cognitive and/or psychological symptoms that continue for more than 12 weeks after illness and which are not explained by an alternative diagnosis. Specific symptoms may include extreme tiredness, shortness of breath, chest pain, problems with memory, heart palpitations, dizziness, and joint pain.5 These symptoms are experienced not only by patients discharged from hospital but also those in the community who did not require inpatient care. The current estimate that 10% of people whose COVID-19 was managed at home are experiencing persistent symptoms beyond a month indicates a significant impact on the economy and health care as whole.6 In the UK, this has resulted in the allocation of funding to establish nationwide post-COVID assessment clinics.
Here we describe the configuration of a functioning comprehensive multidisciplinary rehabilitation pathway for those experiencing long term impacts after COVID-19 to help inform the development of these services in the UK and worldwide.
Implementation
The Community COVID-19 MDT pathway was established in September 2020, as part of the NHS England “Five-point plan” to embed post-COVID-19 syndrome assessment clinics across England.7 Initially a service evaluation was conducted by Leeds Primary Care Services, Leeds Community Healthcare NHS Trust, Leeds Teaching Hospital NHS Trust and The University of Leeds to capture the proportion of patients still suffering from persistent symptoms 7 weeks after hospital discharge.8 This led to ring-fenced funding for a COVID rehabilitation service and the establishment of a 3 tier model of post COVID management.
Three Tier Model of Management
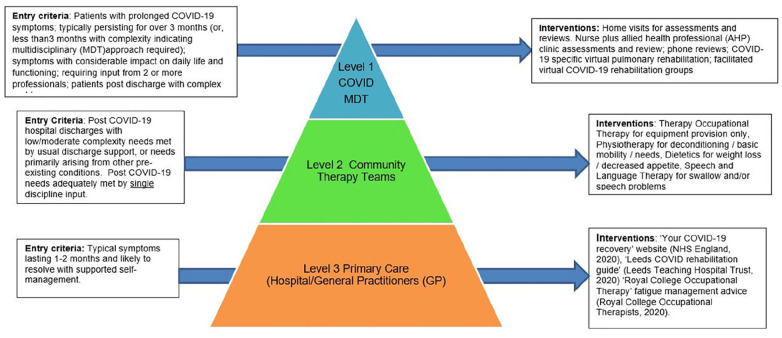
Patients with typical symptoms lasting between 1 and 2 months self-manage using the online resources outlined in Figure 1. Those who have Level 2 low/moderate complexity (such as single discipline needs) are supported by non-COVID specific care and therapy services, such as community occupational and physiotherapy. For patients who meet the Level 1 criteria of having prolonged symptoms over 3 months with a clear need for more than 1 specialist role are eligible for referral into the Community COVID-19 MDT.
Figure 1.
Tiered pathway of input needs.
The Level 1 Community COVID-19 MDT consists of 2 Allied Health Professional (AHP) Pathway Co-ordinators, 2 Physiotherapists, 2 Occupational Therapists, and 3 Consultants with specialisms in Rehabilitation Medicine, Respiratory Medicine and Cardiology; with specialist support from a Respiratory nurse, Respiratory Physiotherapists, 2 Dieticians, and 2 Neurological Occupational Therapists (see Table 1).
Table 1.
Composition of Level 1 COVID-19 MDT (Banding Levels as per NHS Agenda for Change).
| Rehabilitation therapists | Medical |
| Band 8a pathway co-ordinator (1.0 whole time equivalent, WTE) | Consultant in rehabilitation medicine (0.1 WTE) |
| Band 7 physiotherapist (2.0 WTE) | Consultant in respiratory medicine (0.1 WTE) |
| Band 7 occupational therapist (2.0 WTE) | Consultant cardiologist (0.1 WTE) |
| Specialist Allied Health Professionals | Research |
| Band 6 respiratory nurse (1.0 WTE) | Consultant in rehabilitation medicine (research) (0.1 WTE) |
| Band 6 respiratory physiotherapist (1.0 WTE) | Band 6 AHP researcher (1.0 WTE) |
| Band 7 dietitian (0.2 WTE) | Others |
| Band 6 dietitian (0.5 WTE) | Project manager (0.1 WTE) |
| Band 7 neuro occupational therapist (0.5 WTE) | Admin support (0.1 WTE) |
| Band 6 neuro occupational therapist (0.2WTE) | Post doctoral clinical psychologist trainee (0.5WTE) |
Adjunct Specialist Services
Where patients present with complex symptoms of cognitive communication or voice and upper airways disorders such as Inducible Laryngeal Obstruction, referrals are made to the Community Speech and Swallow service or the Acute Trust Specialist ENT Speech and Language therapy team.
There are also referral pathways from the Community COVID-19 MDT to established local mental health and psychology services for patients who are experiencing distressing thoughts and feelings that impact on their participation of valued activities and/or roles.
Pathway of Referral to Level 1 Community COVID-19 MDT
The vast majority (96%) of referrals come from General Practitioners (GP) surgeries, via the established “Single Point of Urgent Referral” triage system. GPs are made aware of the Community COVID-19 MDT service through usual communication avenues such as the internal bulletin briefings. Fewer referrals are directly from hospital services, with these being isolated to complex cases.
Referrals are also accepted from Level 2 “Neighbourhood” (community nursing and therapy) teams who may be supporting someone after a prolonged stay in hospital with concurrent long term conditions. Referrals are discussed with a community matron (an experienced, senior nurse) in the first instance who, alongside GP’s, ensure that differential diagnosis such as pulmonary embolisms (PE), heart failure, recurrent chest infections and undiagnosed respiratory conditions have been considered.
Pathway of Intervention
Once a referral is received, telephone contact is made with the patient to gather an email or address, enabling swift provision of the screening questionnaire. The questionnaire incorporates the C19-YRS questionnaire recommended by NHS Clinical Guidance for use as an outcome measure in post-COVID-19 syndrome assessment clinics.7 This scale, now available as a self-report version gathers symptom severity and functional disability in post-COVID-19 syndrome and acts a triage tool to the most appropriate clinician or treatment modality.9 As well as being patient-centered, this approach has also been found to significantly reduce clinician assessment time, enabling face to face therapy to be focused on gathering further information as required and providing therapeutic intervention.
The average timeframe from initial referral to receiving the completed screening questionnaire is 4 weeks. The patient is then contacted by a Pathway Coordinator via phone who discusses key symptoms further and advises on the appropriate next steps. The majority of patients are placed on a waiting list for therapy to commence (on average 7 weeks), and given self- management advice and materials to follow in the interim (see Figure 1; level 3 interventions). Where fatigue is a key persisting symptom, patients are offered a place on the virtual fatigue management course. Access to IT (information technology) is required but an IPad can be provided for free via a local “Digital Access” scheme should a patient not have access to a Smartphone or computer facilities.
In some cases, where there are medical concerns raised within the screening questionnaire such as unexplained chest pains, a patient may be discussed as a priority within the weekly specialist MDT clinic.
Specialist MDT Clinic
One of the unique interventions offered by the COVID-19 MDT service which differentiates it from the Level 2 and 3 services outlined in Figure 1 is the specialist MDT clinic. Patients with specific medical complexities, such as ongoing oxygen desaturation are discussed within a weekly virtual COVID-19 multidisciplinary team meeting (see Table 2). This forum is valuable in linking patients to appropriate pathways of investigation and treatment. It also helps to reduce the number of out-patient clinic attendances as the mixture of clinical specialists rationalize the need for investigations and correlate the clinical findings with the most appropriate and effective management approach.
Table 2.
Criteria for Escalation to the Specialist MDT Clinic.
| • Non resolving breathlessness that may require further investigations. |
| • Unexplained chest pain or palpitations requiring review of investigations and symptoms. |
| • Autonomic symptoms such as PoTS (Postural Orthostatic Tachycardia Syndrome). |
| • Pain that is not controlled with current medications or of unknown cause. |
| • Patients who are not making progress, or symptomatically deteriorating. |
| • Patients with atypical COVID-19 presentations that may need other investigations and/or onward referrals. |
| • Patients who have had an acute hospital admission for mental health reasons. |
| • Patients that continue to have frequent Accident and Emergency department (A&E) visits despite input from the COVID-19 rehabilitation services. |
Outcome Measures
Once the patient is on the active therapy caseload, initial baseline outcome measures are taken by the lead therapist within the first assessment. The outcome measures utilised in the level 1 MDT service is shown in Table 3. The core set of outcome measures are MRC, MIFS, EQ5D, 30 second sit-stand test and C19-YRS. As recommended by NHS England, outcome measures are taken at baseline, 8 weeks and 6 months.7
Table 3.
Core set of Outcome Measures.
| Symptom | Outcome measure |
|---|---|
| Fatigue | • COVID-19 Yorkshire Rehabilitation Scale (C19-YRS) |
| • Modified Impact Fatigue Scale (MIFS) | |
| • EuroQol-5D-5L (EQ5D-5L) | |
| Breathlessness | • C19-YRS |
| • Medical Research Council Breathlessness Scale) (MRC) | |
| • 30 second sit-stand test | |
| • The Borg Rating of Perceived Exertion (Borg RPE) | |
| Deconditioning | • C19-YRS |
| • 30 second sit-stand test | |
| • EQ5D-5L | |
| Cognition | • C19-YRS |
| • Addenbrooke’s Cognitive Examination (ACE-3) | |
| Anxiety and depression | • C19-YRS |
| • EQ5D-5L | |
| • Generalized Anxiety Disorder Assessment (GAD7) | |
| • Depression Severity (PHQ9) | |
| Pain | • C19-YRS |
Interventions
As a novel virus, there is no current established evidence base for Post COVID-19 syndrome; therefore interventions have relied on the assessment, clinical reasoning, experience and judgment of skilled clinicians. Post viral fatigue management approaches used are endorsed by The College of Occupational Therapists, focusing on energy management within activity and at rest.10 A traditional pulmonary rehabilitation approach is not taken by the team due to the predominance of fatigue in many cases, taking caution from the experience of those with chronic fatigue syndrome, in which incremental exercise programmes are advised against.11 Those patients who require consideration of ambulatory oxygen are assessed as per British Thoracic Society (BTS) guidelines.12 Interventions are led by the patient’s functional priorities and presenting symptoms, following the usual process of assessment, clinical reasoning and intervention planning. Each programme is guided by the individual’s goals, with specific interventions selected to reduce the impact of their symptoms (see Table 4). To improve strength and endurance, exercise programmes are prescribed but with caution, especially where a patient may be experiencing on-going fatigue problems. Patients are assessed on an individual basis, and the outcome recommendations range from a prescribed exercise programme and pacing of functional activity, to directing to NHS England’s “Your COVID recovery” webpage.13
Table 4.
Symptom and Interventions.
| Symptom | Example interventions considered: |
|---|---|
| Chest and pleuritic pain | • Education of self-management strategies (avoiding over exertion) |
| • Medical management occasionally required such as electrocardiogram (ECG) screening to rule out potentially life threatening diagnoses | |
| Repeated chest infections | • Secretion clearance strategies |
| • Swallowing screen for aspiration then medical management if required | |
| • Medical management to optimize underlying respiratory conditions may be required | |
| Muscular and joint pain | • Hot/cold therapy |
| • Exercise prescription for pain related deconditioning | |
| • Multi-disciplinary team discussion if potentially neuropathic pain | |
| Shortness of breath at rest | • Assessment of breathing pattern to rule out Breathing Pattern Disorder |
| • Use of Borg Rating of Perceived Exertion Scale (RPE) and oximetry | |
| • Breathing retraining (Diaphragmatic and nasal) | |
| • Assessment of N-terminal pro-brain natriuretic peptide (NT-proBNP) if indicated | |
| • Diffusing capacity for carbon monoxide (DCLO) and overnight pulse oximetry warranted in a minority of complicated cases | |
| Shortness of breath on exertion | • Breathing techniques whilst moving |
| • Purse lip breathing strategies if nasal breathing effortful | |
| • Positioning | |
| • Use of fan | |
| • Using Borg-RPE scale and oximetry with activity to guide and educate patient to safe level exercise | |
| • Assessment of NT-proBNP if indicated | |
| Desaturation on exertion | • Use of pulse oximetry to relate to breathlessness score on Borg-RPE scale, and recovery time |
| • Review how patient manages desaturation | |
| • Grade up activity gradually starting with non-de-saturation tasks | |
| • Education of self-management and breathing control for recovery/managing desaturation | |
| • Positioning | |
| • Assessment of NT-proBNP if indicated | |
| • Assessment of need for further respiratory investigation | |
| Palpitations and tachycardia | • Medical assessments such as ECG, ambulatory ECG, and thyroid function, biomarkers and exercise testing |
| • Advice around exercise | |
| • Medical management including salt loading and hydration volume, medications | |
| Dizziness | • Vestibular retraining if indicated |
| • Investigate whether related to postural drop or Postural Tachycardia Syndrome (PoTS) | |
| • Education/advice around postural drop and positional changes | |
| • Medication review | |
| Post viral fatigue or post-exertional malaise | • Diaries (fatigue/sleep/thinking) |
| • Education around pacing and prioritization | |
| • Identification of own unique occupational balance | |
| • Education on relaxation strategies and “quality” rest | |
| • Lifestyle management (diet, sleep and stress management) | |
| • Enrolment onto virtual fatigue course | |
| • Vocational support | |
| Anxiety and depression | • Enrolment onto virtual fatigue course |
| • Education on relaxation and mindfulness | |
| • Use of restorative activity | |
| • Referral to psychological services/Leeds Wellbeing service | |
| Poor memory and concentration | • Cognitive assessment if indicated |
| • Education around cognitive processes and post viral syndrome | |
| • Brain Training exercises (eg, Luminosity) | |
| • Diaries- fatigue/sleep/thinking | |
| • Vocational support | |
| • Memory aids | |
| • Education on relaxation and mindfulness | |
| • Use of restorative activity | |
| Voice Disorders Upper airways Disorders Reflux related laryngeal symptoms |
• Voice care advice and therapy |
| • Inducible laryngeal obstruction (ILO) management | |
| • Cough suppression techniques | |
| • Education and support of post viral laryngeal recovery | |
| • Specific relaxation techniquesand CBT strategies | |
| Word finding difficulties (anomia) | • Linguistic approach to improve semantics |
| • Cognitive approach to improve verbal short-term memory and speed of naming | |
| • Compensatory approach, for example, circumlocution | |
| • Interventions may be provided in person and/or via computer therapy to support dosage/independent practice |
Patients reporting mild symptoms of anxiety and depression and who are assessed appropriate for support in self-management have been guided to the “Leeds Mental Well-being” Service. This service provides an online resource tailored to “Coping with COVID-19” that covers a range of subjects from “introducing activity” to “improving sleep.”14
Virtual Fatigue Management Course
Post viral fatigue syndrome has been described as persistent post viral fatigue with additional symptoms such as activity induced fatigue, sleep disturbance, cognitive dysfunction and orthostatic intolerance.15 It is a particularly common and severe feature of post COVID-19 syndrome. A virtual platform for group therapy sessions has been established, consisting of an 8-week programme, based on principles of energy management, quality rest, optimal nutrition and physical maintenance. Sessions are conducted via MS Teams, lasting a maximum of 1 hour and split into 2 sections. The first section delivers pre-recorded education and advice, accompanied by PowerPoint slides (see Table 5). The latter part of the session is a dedicated space for peer support, moderated by the lead therapist and is informally structured around discussion topics of the week. Contribution is voluntary and confidential as per the agreed group contract established initially.
Table 5.
Virtual Fatigue Management Course Modules.
| Week | Module | Facilitator | Facilitated discussion questions |
|---|---|---|---|
| 1 | Overview and understanding fatigue | Occupational therapist and other MDT members | Are you able to recognize when you are becoming fatigued, and how? |
| Can you identify what may trigger your fatigue? | |||
| What would you like to get out of the programme in order to improve your quality of life and best manage your levels of fatigue? | |||
| 2 | Thinking about activity | Occupational therapist | What activities have people found manageable or more challenging? |
| Have people had experience of using an activity diary? How has this been incorporated into daily routines? How useful have these been? | |||
| 3 | Activity grading | Occupational therapist | How do you ensure you have a combination of activities? |
| Do you know when your stopping point is, or do you tend to only stop when your body tells you to do so? | |||
| 4 | Fatigue and exercise | Physiotherapist | What daily exercise are people managing now? |
| Has anyone tried to return to higher level exercise? How did this affect your fatigue levels and ability to do other activities? | |||
| 5 | Diet and nutrition | Dietician | Have you noticed a pattern between your fatigue and what you eat? |
| Have you altered your diet to try and improve your fatigue? | |||
| What did you try and did it help? | |||
| 6 | Sleep hygiene | Neuro occupational therapist | What do you find works well to improve your sleep to recover for the next day? |
| 7 | Cognition and communication | Neuro occupational therapist | What difficulties are you having with your memory, attention or communication? |
| Can you see any strategies that would be beneficial within your daily routines? | |||
| 8 | Mindfulness | Neuro occupational therapist | Can you see any strategies that would be beneficial within your daily routines? |
The Current Caseload Demographic
Young population-with average age of 48 (youngest is 27, oldest is 73)
Majority of patients are female (68%)
Majority have not had a hospital admission (74%)
Many were infected during the first phase of the pandemic (March and April 2020) and continue to have symptoms (82%)
Unable to work or have had to reduce hours (54%)*
*Many able to remain in work only due to current working from home arrangements
At the time of writing, the number of active patients supported by the service is 225.
Key areas of therapeutic intervention have been: fatigue management (70%), breathlessness (51%) and cognitive problems (12%). As expected for such a young age group, the key areas of functional impact are around return to work, parental roles and extended activities of daily living.
Discussion
In Leeds, a three-tiered system of rehabilitation has been developed to link the patient’s need with an appropriate service and intervention. At level 3, primary care services support patients in self-management. Within level 2, patients in the post-acute illness phase are supported by their local multidisciplinary non-specialist neighborhood teams, and at level 1, patients have complex post-COVID-19 syndrome and their rehabilitation is delivered by the specialist team described within this paper.
This model of care aligns to the most recent criteria set by NHS England and Improvement guidance for post-COVID-19 assessment and treatment clinics,7 integrating multidisciplinary intervention,16 access to diagnostic tests, accessible to all patients recovering from COVID-19 and having a local communication plan in place to raise awareness of both clinicians and the public. The key benefit of the 3 tiered model of care (see Figure 1) is that patients receive intervention from the appropriate service and clinician. Resources are directed where most appropriate; those with complex ongoing symptoms are seen by COVID specialist clinicians and have timely access to the medical MDT consultant discussions where necessary. The regular specialist MDT meetings have provided an effective forum for discussions around individual patient management, bringing specialists together to disentangle the complexities of post COVID-19 presentations, consider differential diagnoses and treatment strategies.
The tier system also delegates responsibilities at each level, giving health care professionals working in GP surgeries and hospitals clarity around which interventions to offer, and when referral is necessary into the post COVID-19 MDT.
The generalisability of the tiered model into other NHS primary care contexts and beyond relies on having protected, also known as “ring fenced” funding to replicate this model, and having access to community nurses, therapists and specialist clinicians with the right skill-set. Strong links are also necessary with GP surgeries to establish and maintain the referral pathway. Having a lead GP representative has assisted with communication and establishing consultant led training ensures that GPs complete the relevant investigations before referring into the post COVID-19 MDT.
A significant challenge that the team encountered has been achieving and establishing consistent and geographically equitable pathways of referral and access across the city. On-going communications work with GP links are supporting this issue. Service evaluation around patient satisfaction is underway using the Person Centered Coordinated Care Experience Questionnaire (P3C-EQ) however, feedback from individual patients to date (written and verbal) has been extremely positive, especially around the emotional and fatigue management support received. Likewise, outcome data and health informatics are also being gathered by the service to map patient trajectories and service impact. There have been few discharges since the service was established, indicating that this patient group are likely to remain under the care of the service for prolonged episodes, compared to usual community therapy services. As referral numbers increase further, this may pose capacity challenges to the service, however recent funding has been provided to increase capacity and reduce waiting times for patients.
This service continues to evolve in response to both the needs of patients and emerging knowledge of post-COVID-19 syndrome. It should also be acknowledged that this service is developing in a city that has experienced higher rates of infection compared to the national average, and therefore is likely to also see higher service referral numbers. The impact of this on capacity is an unknown at present, however it is likely that virtual platforms for group rehabilitation will be increasingly utilized as a means of providing input whilst patients are awaiting face to face therapy. Peer support is considered to be a vital therapeutic medium enabling reassurance and empowerment,17 and is clearly valued by people suffering from post COVID-19 Syndrome; apparent within the number of Facebook “Long COVID Support group” members which currently stands at 37 500.18
Future Work
At the time of writing, work is progressing in collaboration with Occupational Health services, with recognition that traditional models of “fit to work” do not meet the health needs of this new cohort of returning workers.
In partnership with the University of Leeds Psychometric Lab for Health Sciences, the C19-YRS is currently being developed and psychometrically tested for construct validity, responsiveness and stability using Rasch analysis.19 The outcome of this work will be to produce a reliable scale that can be used within an digital application platform. It is expected that this platform will enhance self-management, support prompt clinical intervention, and contribute to international understanding of COVID rehabilitation trajectory.
The authors anticipate that the direction of their future research will focus on the application of the C19-YRS and evaluation of specific interventions delivered by this service, most notably the virtual platform for education, advice, and self-management support.
Conclusion
The Community COVID-19 MDT in Leeds has rapidly established an integrated service pathway for an emerging patient group who have complex multidisciplinary needs. As the evidence base and our clinical knowledge expand, we expect the service to develop responsively to meet the needs of this patient cohort in terms of individualized interventions and comprehensive management of post-COVID-19 Syndrome.
The authors hope that this paper provides insight into the development of a dedicated COVID-19 Community MDT, and a template for establishing a pathway of care.
Acknowledgments
The authors would like to acknowledge the wider team of professionals working in the service, managerial staff and commissioning group who have been instrumental in setting up one of the first UK Long Covid services in Leeds. The authors also thank all the patients who have provided valuable insights during setting up of the service.
Footnotes
Author Contributions: JD and MS conceptualized the article and all authors participated in the writing and reviewing the manuscript.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Authors AP and MS posts are supported by research funding by the Leeds Clinical Commissioing Group (CCG). The development of C19-YRS scale is supported by the University of Leeds Medical Research Council (MRC) Confidence in Concept (CiC) grant.
ORCID iDs: Amy Parkin  https://orcid.org/0000-0001-8245-8477
https://orcid.org/0000-0001-8245-8477
Alex Simms  https://orcid.org/0000-0002-4715-8134
https://orcid.org/0000-0002-4715-8134
References
- 1. World Health Organisation, WHO Coronavirus Disease (COVID 19) Dashboard. WHO. November 2020. Accessed March 23, 2021. https://covid19.who.int/ [Google Scholar]
- 2. Leeds City Council Managing Coronavirus in Leeds. December 2020. Accessed December 21, 2020. https://www.leeds.gov.uk/coronavirus/managing-coronavirus-in-leeds
- 3. Roberts R, Levi M, Schilling R, Lim WS, Grocott MPW, McKee M. Covid-19: a complex multisystem clinical syndrome. BMJ. 2020;125:238-242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Alwan NA, Attree E, Blair JM, et al. From doctors as patients: a manifesto for tackling persisting symptoms of covid-19. BMJ. 2020;370:m3565. [DOI] [PubMed] [Google Scholar]
- 5. Post-COVID Syndrome (Long COVID). NHS England and NHS Improvement. January 2021. Accessed January 2021. https://www.england.nhs.uk/coronavirus/post-covid-syndrome-long-covid/ [Google Scholar]
- 6. Sudre CH, Murray B, Varsavsky T, et al. Attributes and predictors of long-covid: analysis of covid cases and their symptoms collected by the Covid Symptoms Study app. MedRxiv. October 2020. Accessed 12, January 2020. https://www.medrxiv.org/content/10.1101/2020.10.19.20214494v1
- 7. National Guidance for post-COVID syndrome assessment clinics. NHS England and NHS Improvement. November 2020. Accessed November 20, 2020. https://www.england.nhs.uk/coronavirus/publication/national-guidance-for-post-covid-syndrome-assessment-clinics/ [Google Scholar]
- 8. Halpin SJ, McIvor C, Whyatt G, et al. Post-discharge symptoms and rehabilitation needs in survivors of COVID-19 infection: a cross-sectional evaluation. J Med Virol. 2021;93:1013-1022. [DOI] [PubMed] [Google Scholar]
- 9. Self-report version of C19-YRS. University of Leeds. January 2021. Accessed February 7, 2021. https://licensing.leeds.ac.uk/product/c19-yrs-covid-19-yorkshire-rehabilitation-scale [Google Scholar]
- 10. How to manage post-viral fatigue after COVID-19: Practical advice for people who have recovered at home. Royal College of Occupational Therapists. May 2020. Accessed November 20, 2020. https://www.rcot.co.uk/how-manage-post-viral-fatigue-after-covid-19-0 [Google Scholar]
- 11. National Institute for Health and Social Care Excellence Guideline: Myalgic encephalomyelitis/chronic fatigue syndrome: diagnosis and management. Draft for consultation. NICE. November 2020. Accessed January 2021. ME/CFS (nice.org.uk) [Google Scholar]
- 12. British Thoracic Society: Guidelines for Home Oxygen Use in Adults. British Thoracic Society. June 2015. Accessed December 18, 2020. https://www.brit-thoracic.org.uk/quality-improvement/guidelines/home-oxygen/ [Google Scholar]
- 13. Your COVID Recovery; Guidance for the online interactive platform. NHS England and NHS Improvement. October 2020. Accessed 20 November, 2020. https://www.yourcovidrecovery.nhs.uk/ [Google Scholar]
- 14. Leeds Mental Health Wellbeing Service: Coping with COVID-19; online group classes. Leeds Community Healthcare NHS Trust. November 2020. Accessed November 20, 2020 https://www.leedscommunityhealthcare.nhs.uk/our-services-a-z/leeds-mental-wellbeing-service/online-group-classes/coping-with-covid-19/ [Google Scholar]
- 15. The ME Association, Post COVID-19 Fatigue, Post/Long COVID-19 Syndromes and Post COVID-19 ME/CFS. September 2020. Accessed January 12, 2021. MEA-Covid-19-MECFS-Post-Covid-Fatigue-Syndromes-and-Management-November-2020.pdf (meassociation.org.uk)
- 16. Sivan M, Rayner C, Delaney B. Fresh evidence of the scale and scope of long covid. BMJ. 2021;373:n853. [DOI] [PubMed] [Google Scholar]
- 17. National Voices: People shaping health and social care. National Voices. January 2020. Accessed January 18, 2021. https://www.nationalvoices.org.uk/sites/default/files/public/publications/peer_support_-_what_is_it_and_does_it_work.pdf [Google Scholar]
- 18. Long COVID support group. Facebook. January 2021. Accessed March 23, 2021. https://m.facebook.com/groups/longcovid/
- 19. Rasch G. Probabilistic Models for Some Intelligence and Attainment Tests. Danmarks Paedagogiske Institut; 1960/1980. [Google Scholar]