Graphical abstract
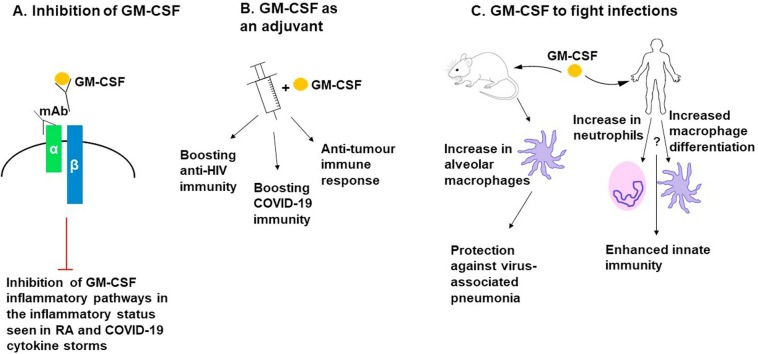
The various strategies of using GM-CSF in immunotherapy.
GM-CSF has been targeted in clinical trials in three different ways. (a) illustrates immunotherapies that inhibit GM-CSF binding its receptor in order to prevent the excessive inflammation in diseases by using Monoclonal antibodies (mAb) that either bind GM-CSF directly, or target the α subunit of the GM-CSFR preventing its binding to GM-CSF. (b) GM-CSF has been utilized as an adjuvant in vaccines to promote immunity against HIV, COVID-19 infections, as well as in cancer vaccines. (c) GM-CSF is used directly to enhance immunity against infections. In mice this was shown to increase the number of alveolar macrophages which resulted in protection against virus-associated pneumonia. In humans, many current trials postulate that it will promote an increase in neutrophils and macrophage differentiation to enhance innate immunity and prevent infections. The “?” in this figure indicate more data are needed to support these models of actions.
Keywords: Vaccine, IFN, Virus, Pro-inflammatory cytokines
Abstract
GM-CSF acts as a pro-inflammatory cytokine and a key growth factor produced by several immune cells such as macrophages and activated T cells. In this review, we discuss recent studies that point to the crucial role of GM-CSF in the immune response against infections. Upon induction, GM-CSF activates four main signalling networks including the JAK/STAT, PI3K, MAPK, and NFκB pathways. Many of these transduction pathways such as JAK/STAT signal via proteins commonly activated with other antiviral signalling cascades, such as those induced by IFNs.
GM-CSF also helps defend against respiratory infections by regulating alveolar macrophage differentiation and enhancing innate immunity in the lungs. Here, we also summarize the numerous clinical trials that have taken advantage of GM-CSF’s mechanistic attributes in immunotherapy. Moreover, we discuss how GM-CSF is used as an adjuvant in vaccines and how its activity is interfered with to reduce inflammation such as in the case of COVID-19. This review brings forth the current knowledge on the antiviral actions of GM-CSF, the associated signalling cascades, and its application in immunotherapy.
1. Introduction
1.1. The numerous roles of GM-CSF in the immune system
Granulocyte macrophage colony stimulating factor (GM-CSF) functions as a hematopoietic growth factor, as it stimulates proliferation and differentiation of bone marrow progenitor cells into granulocytes and macrophages [1]. Furthermore, GM-CSF enables survival and activation of mature myeloid cells [2]. Evidence from knock-out (KO) mouse studies indicate that although GM-CSF plays a role in steady state myelopoiesis, it is not essential for this process [3]. However, GM-CSF is needed to drive emergency myelopoiesis to efficiently clear infections by enhancing the numbers of newly recruited macrophages and granulocytes [4]. Further characterization of GM-CSF showed that it is crucial for the maturation of fetal monocytes into alveolar macrophages (AM) [5]. GM-CSF is also necessary for the steady-state maintenance of non-lymphoid tissue-resident CD103+ dendritic cells (DCs) across multiple tissues in mice. These cells are imperative for the initiation of CD8 + T cell actions in the lung [6,7]. The role that GM-CSF plays in host lung immunity and its homeostasis is discussed further in Section 3.1.
GM-CSF plays a key role in inflammation [2]; its basal circulating levels under homeostatic conditions are low, but significantly increase during inflammation [8]. Specifically, GM-CSF is produced by various immune cells including monocytes, macrophages, and activated T and B cells in response to infection [9]. During such events, pro-inflammatory cytokines including interleukin-6 (IL-6), tumor necrosis factor-α (TNF-α), and IL-23 induce GM-CSF production by activated CD4+ and CD8 + T cells. This is beneficial to the host when combating infections, but can be detrimental in chronic inflammatory conditions [10].
Several studies demonstrate how GM-CSF producing T cells are critical to the immune response against various bacterial and viral pathogens like Mycobacterium tuberculosis, Epstein–Barr virus (EBV), and human immunodeficiency viruses (HIV) [[11], [12], [13], [14], [15]]. This is largely due to the pro-inflammatory actions evoked after the recruitment and activation of myeloid cells by GM-CSF [16]. Particularly, GM-CSF drives the activation of macrophages to an M1-like pro-inflammatory phenotype in vitro [[17], [18], [19], [20]], producing chemokines such as C-C motif chemokine ligand-2 (CCL2), CCL24, CCL5, and CCL1 for leukocyte recruitment [21] and cytokines like TNF-α, IL-6, IL-12p70, IL-23, and IL-1β for pro-inflammatory actions upon stimulation [17,18]. These molecular signals also contribute to the role of GM-CSF in the differentiation and activation of T helper (Th) type 1 and Th17 cells, further promoting pro-inflammatory events and clearance of infections [22].
GM-CSF also has an important role in expanding myeloid-derived suppressor cells (MDSCs) at the resolution of inflammation for wound healing and tissue repair. Interestingly, tumors exploit this process as malignant cells secrete GM-CSF to reprogram tissue-resident macrophages into MDSCs that suppress CD8 + T cell responses [23]. Despite this function, numerous investigations are centered on the use of GM-CSF clinically as a therapeutic, which paradoxically includes cancer therapy. Talimogene laherparepvec, the GM-CSF encoding oncolytic virus has been approved for the local treatment of advanced melanoma. Moreover, recombinant GM-CSF has been approved for other clinical uses as well including treatment of neutropenia associated with stem cell transplantation. As an immunostimulatory agent, GM-CSF promotes the functions of antigen presenting cells for aiding the immune system in the aforementioned conditions. Currently, because GM-CSF is required for AM homeostasis and lung pathogen clearance, it is being investigated as a potential therapeutic for COVID-19 patients with respiratory failure [6].
Although GM-CSF possesses favorable roles during various disease states by inducing the activation, migration, survival, and renewal of effector macrophages and granulocytes, it has also been implicated in the exacerbation of such diseases. For example, GM-CSF drives the progression of diseases including rheumatoid arthritis (RA) and multiple sclerosis (MS) [8,17,24]. It seems to be associated with inflammatory pain in these diseases via the CCL17/GM-CSF pathway [25,26]. Nonetheless, there are various signalling pathways induced by GM-CSF which we discuss next, that enable survival, differentiation, and proliferative effects of the responding immune cells.
1.2. GM-CSF signalling pathways
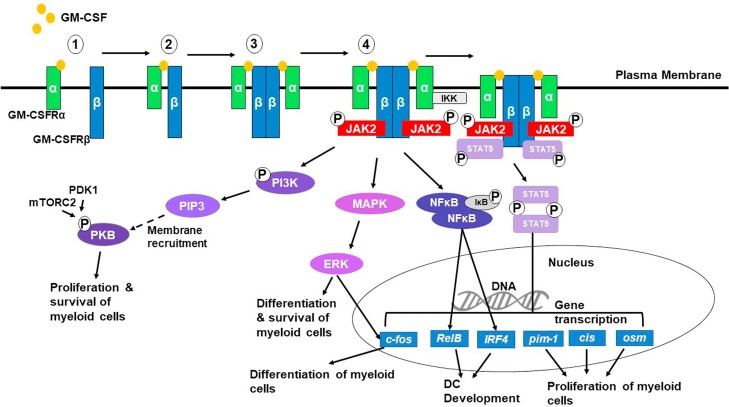
The first step in GM-CSF signalling is the binding of GM-CSF to its receptor (GM-CSFR). The GM-CSFR is a type I cytokine receptor composed of an α and β subunit, involved in binding and signalling [22]. While the α subunit is specific to GM-CSF, the β subunit is shared with IL-3 and IL-5 [22]. The GM-CSF receptor is expressed on myeloid cells but is also found on non-hematopoietic cells such as alveolar epithelial cells, fibroblasts, and vascular endothelial cells [27]. Although the exact mechanism behind GM-CSFR activation and signal transduction is not entirely delineated, it has been proposed that activation of the receptor occurs by GM-CSF binding to the α chain resulting in dimerization of the two subunits (Fig. 1 ) [27]. The discovery of the crystal structure uncovered that two α, β and GM-CSF complexes come together to form a heterohexameric complex (Fig. 1, step 3) [27]. The dodecamer conformation in the hexameric complexes can then trigger the initiation of four main signalling pathways including the janus kinase-signal transducer of activation of transcription (JAK-STAT), phosphoinositide 3-kinase (PI3K), mitogen-activated protein kinase (MAPK), and activated nuclear factor-κB (NFκB) pathways [28].
Fig. 1.
GM-CSF signaling pathways. To activate downstream signalling, multiple events occur as depicted (1-4) in this Fig. 1) GM-CSF binds to the α subunit of the GM-CSFR. 2) Dimerization of the two subunits upon GM-CSF binding. 3) Formation of the GM-CSFR hexameric complex followed by the lateral association of two hexameric complexes. 4) Several signalling pathways could result from GM-CSFR activation; JAK2 binds the β cytoplasmic tails and transphosphorylate each other, which activates the PI3K, MAPK, and JAK/STAT pathways, as well as the NFκB pathway. Activated NFκB dimers translocate into the nucleus and result in the transcription of genes for the differentiation and survival of myeloid cells such as RelB and IRF4. The JAK/STAT pathway induces the phosphorylation of STAT5, eventually causing STAT5 dimerization and translocation to the nucleus for transcriptional regulation of genes for the differentiation, proliferation, and survival of myeloid cells including c-fos, RelB, IRF4, pim-1, cis, and osm. The MAPK pathway also results in the differentiation and survival of myeloid cells via ERK kinase activation, through the transcription of genes such as c-fos. Finally, PI3K is phosphorylated by JAK2 resulting in signal transduction through a PIP3 intermediate, causing membrane recruitment of PKB followed by its phosphorylation by mTORC2 and PDK1, eventually leading to the proliferation and survival of myeloid cells.
To activate the JAK-STAT, PI3K, and MAPK pathways, JAK2 clusters to the β cytoplasmic tails of the complex, initiating kinase activation and transphosphorylation by the JAK2s (Fig. 1, step 4) [28]. In the JAK-STAT pathway, the phosphorylated JAK2s induce recruitment, phosphorylation, and dimerization of the transcription factor STAT5 [28]. The STAT5 dimers then translocate to the nucleus to induce transcription of genes involved in myeloid cell differentiation, proliferation, and survival [28]. These genes include c-fos to promote the differentiation of myeloid cells, RelB and IRF4 to stimulate DC development, and pim-1, cis, and osm to induce myeloid cell proliferation [28,29].
Activated JAK2 also phosphorylates and activates PI3K, which acts as a second messenger to regulate the activity of protein kinase B (PKB). PI3K recruits PKB to the plasma membrane for activation via phosphorylation by pyruvate dehydrogenase kinase 1 (PDK1) and mTOR complex 2 (mTORC2), needed for the proliferation and survival of myeloid cells [28]. Through a series of intermediates, the MAPK/ERK kinase (MEK) is also activated by JAK2, consequently triggering extracellular signal regulated kinase (ERK) and its kinase activity to regulate downstream transcription of genes such as c-fos to promote the differentiation and survival of myeloid cells [28,29]. Interestingly, Achuthan et al., reported a correlation between ERK activity and GM-CSF enhancement of human monocyte survival in vivo [25]. Furthermore, upon GM-CSF treatment, ERK1/2 activation has been found to induce multipotent mesenteric mesothelial cell differentiation into macrophages [30].
How GM-CSF initiates NFκB signalling has yet to be fully defined, but it is known to involve the IκB kinase (IKK) complex, which in turn phosphorylates IκB, the NFκB inhibitor, leading to IκB ubiquitination and degradation, consequently activating NFκB [31]. NFκB dimers then translocate to the nucleus where they regulate the transcription of genes such as RelB and IRF4 to promote DC development (Fig. 1) [28,29]. Although not yet fully elucidated, interferon regulatory factors (IRF) 4 and 5 have been also reported as important downstream targets of GM-CSF [22]. Reports have found that IRF4-dependent signalling appears to upregulate MHC class II expression in mouse macrophages and DCs due to GM-CSF treatment [32]. Moreover, in response to GM-CSF stimulation, IRF5 has been reported to promote macrophage polarization to the M1-like phenotype [33]. IRF5 has also been implicated in inducing the synthesis of type I interferons (IFNs) and TNF-α to promote an antiviral state in infections such as Newcastle disease virus (NDV), herpes simplex virus (HSV-1), and vesicular stomatitis virus (VSV) [34]. Thus, the GM-CSF signalling pathways contribute in part to key steps that help the immune system in fighting infections.
2. Cytokines and pathways associated with antiviral immunity
2.1. Antiviral activities of interferons
IFNs, commonly classified into three types (I, II, III), are a host-encoded, multi-gene family of inducible cytokines that possess various functions, namely, antiviral activity. The type I IFN response represents an early host defense through the establishment of an antiviral state, serving as the first line of immunity against viral infection. Specifically, upon stimulation of pattern-recognition receptors (PRRs) from viral antigens, a rapid production of IFN-β and subsequently, IFN-α is produced, which is dependent on phosphorylated IRF3 and activated NFκB [35]. The rapid type I IFN production then induces the phosphorylation of IRF7, needed to enhance the antiviral response [35].
The type I IFNs signal via the type I IFN receptor (IFNAR), which upon binding, activates the tyrosine kinases, JAK1 and TYK2 [36,37]. The tyrosine kinases then phosphorylate the transcription factors STAT1 and STAT2, which come together with IRF9 to form the trimeric IFN-stimulated gene factor 3 (ISGF3) complex. ISGF3 is responsible for the production of IFN-stimulated genes (ISG) with diverse functions including positive or negative regulation of antiviral IFN signalling and direct inhibition at various points of the viral replication cycle [38].
Similar to type I IFNs, type III IFNs (IFNλ1-4) are also regarded as antiviral [39,40]. The signalling cascade induced by type I and type III IFNs is similar [41]. However, the IFNλs are mainly produced by and target mucosal epithelial cells and some immune cells such as macrophages, peripheral blood lymphocytes, conventional DCs, and plasmacytoid DCs, where type I IFNs are expressed by and target all nucleated cells [39,40,42,43].
IFN-γ (type II IFN) signals via its tetrameric receptor, IFNGR [44]. Upon receptor activation, JAK1 and JAK2 auto-phosphorylate each other, then phosphorylate STAT1 leading to dimerization, nuclear translocation, and stimulation of target gene transcription [44]. IFN-γ functions as both an immunoregulatory and antiviral cytokine. For example, IFN-γ has a major role in polarizing macrophages into the M1 phenotype [45,46]. In the context of viral infections, IFN-γ released by activated T cells is crucial for establishing an antiviral state and long-term control of infection [47,48]. Specifically, Changotra et al. demonstrated the ability of IFN-γ to directly inhibit Murine Norovirus replication through reducing the levels of both structural and non-structural viral proteins resulting in a potent inhibition of overall virion production [49]. Additionally, the ability of IFN-γ to induce indoleamine 2,3-dioxygenase (IDO) and inducible nitric oxide synthase (iNOS) to deplete tryptophan and produce nitric oxide (NO), respectively shows powerful antiviral effects [50,51].
2.2. The antiviral activity of pro-inflammatory cytokines (IL-1β, TNF-α, IL-6)
Although IFNs are the main antiviral cytokines of the immune system, pro-inflammatory cytokines including IL-6, IL-1β, and TNF-α also display significant antiviral activity [[52], [53], [54], [55]]. It is interesting to note that these cytokines are among those that are highly upregulated by GM-CSF signalling during an infection [9,17,22]. IL-1β, TNF-α, and IL-6 are key mediators of the inflammatory response and are also involved in the physiological control of virus infections. Most, but not all, mechanistic explanations for IL-1β, TNF-α, and IL-6 antiviral activities have been credited to common pathways shared with IFNs. For instance, the potent ability of TNF-α to impede viral replication is largely due to its synergistic relationship with IFN-γ and IFN-β [56,57]. Though, there is evidence of TNF-α alone acting as a highly antiviral agent. Specifically, one report indicated that through an unknown mechanism, TNF-α can demonstrate stronger antiviral actions than both IFN-α and IFN-γ alone in an in vitro influenza virus (IV) infection [55]. Unfortunately, this unique finding was not further explored, but contributes to the evidence of the antiviral activities exhibited by TNF-α. Nevertheless, such actions are mediated by both subunits of the murine TNF-α receptor, TNFR1 and TNFR2 [54].
Recently, Luo et al. used a genetically engineered rabies virus encoding the IL-6 gene to evaluate the relevance of IL-6 during a viral infection [58]. This study revealed that IL-6 promoted an intensified innate immune response with up-regulated ISGs including ISG15, ISG20, 2'-5'-oligoadenylate synthetase (OAS) 1, OAS2, and MX2 [58]. Similarly, IL-1β is involved in the induction of IFN-α mediated antiviral genes such as OAS and protein kinase RNA-activated (PKR) [59]. In virally infected myeloid cells, such expression of ISGs has resulted through a process of IL-1β and IRF3 signalling crosstalk, further connecting pro-inflammatory cytokine antiviral actions to IFN signalling [60]. In line with this, IL-1β exerts antiviral functions via a gp130-JAK-STAT1-dependent pathway to control viral infections that inhibit or block IFN expression [53]. These findings reintroduce the notion that antiviral functions exhibited by these cytokines occur beyond a shared signalling with the IFNs.
Both IL-1β and IL-6 activate MAPK/ERK signalling pathways [61,62].This pathway has been implicated in the production of the antiviral protein, 1-8U through IL-1β signalling during a Hepatitis C Virus (HCV) infection [63]. Furthermore, an in vitro study investigating Hepatitis B Virus (HBV) infection found that exogenous IL-6 was able to directly suppress HBV replication via an IFN-independent mechanism [64]. Overall, there are innumerable molecular events mediating viral restriction by these cytokines, with the examples discussed herein highlighting IFN signalling crosstalk as well as IFN-independent mechanisms.
3. An indirect role of GM-CSF in antiviral immunity
3.1. GM-CSF in respiratory viral infections
AM and DCs play a crucial role in host lung defense through their ability to phagocytose and destroy pathogens, recruit and activate other inflammatory cells, and serve as important links between innate and adaptive immunity. Production of GM-CSF by alveolar epithelial cells (AEC) is critical for AM function and differentiation, pulmonary homeostasis, and driving pulmonary antiviral actions [65]. Moreover, mice lacking lung GM-CSF signalling (GM-/-) exhibit AM dysfunction and pulmonary alveolar proteinosis (PAP), in which surfactant accumulates within the alveoli [66]. When this occurs, AMs become defective in their antiviral activities including phagocytosis, superoxide production, cytokine release, and PRR expression [65]. Through the expression of the transcription factors, PU.1 and IRF5, GM-CSF regulates the diverse functions of AMs critical to both surfactant homeostasis and defense [33,65]. Thus, the presence of GM-CSF in the lung allows AMs and other immune cells to resist and clear various respiratory viral infections such as influenza and respiratory syncytial virus (RSV).
3.1.1. GM-CSF as a potent anti-influenza cytokine
The immune response to influenza relies on B cells, CD8 + T cells [67,68], and innate immunity driven by AMs [[69], [70], [71]]. During a pulmonary inflammatory event, GM-CSF is secreted by various cell types including macrophages, endothelial cells, fibroblasts, T cells and type II AECs [72]. Once GM-CSF is released, it enhances resistance of AMs and other cells to infection, augments viral clearance, reduces lung injury, and increases survival rates during IV infection [7,[73], [74], [75], [76]]. The use of GM-/- mice has demonstrated that without GM-CSF, mice display a reduced resistance to IV as a result of dysfunctional AMs being unable to effectively clear pathogens [74]. The mechanism for this impairment may be explained by findings that GM-CSF signalling, via PU.1, coordinates the ability of AMs to perform Fcɣ receptor-mediated phagocytosis of pathogens [65]. Additionally, AMs have also been shown to display GM-CSF-dependent production of reactive oxygen species (ROS), a phenomenon known to confer protection against IV pneumonia and secondary bacterial pneumonia, a condition commonly associated with morbidity and mortality post-IV infection [77].
The use of intranasally administered recombinant human GM-CSF (rHuGM-CSF) has demonstrated both in vitro and in vivo protection against IV infection [73]. Moreover, transgenic mice over-expressing GM-CSF (SPC-GM) demonstrate increased production of cytokines by activated target cells – mainly epithelial cells, monocytes, and macrophages, which aid in anti-IV responses [73,78]. In these mice, increased levels of monocyte chemoattractant protein-1 (MCP-1) and TNF-α in the lungs enabled a reduced viral burden [73,76]. In other studies, both MCP-1 and TNF-α helped in the protection against IV, but were associated with lung immunopathology if over produced [59,[79], [80], [81], [82]]. Interestingly, the induction of pulmonary TNF-α prior to IV infection actually reduces lung inflammation and damage [75]. SPC-GM mice administered GM-CSF intranasally demonstrate early elevated MCP-1 and TNF-α, accompanied with low histological evidence of lung injury [73,78]. Thus, in this model, GM-CSF initiates a potent early innate immune response to IV, controlling viral replication. Moreover, a recent study further elucidated a role of GM-CSF produced by IV-infected AECs in coordinating pulmonary DC antiviral functions by regulating the activation and proliferation of CD103+ migratory DCs [7]. In turn, GM-CSF will also help increase the recruitment of IFN-γ producing CD8+ and CD4 + T cells to the respiratory tract to efficiently clear IV [73]. Thus, GM-CSF enables enhanced viral clearance and antigen-specific recruitment of T cells.
3.1.2. GM-CSF in respiratory syncytial virus (RSV) infection
The rationale for employing GM-CSF in combatting RSV infection is based on the premise that it helps the maturation of AMs and induces the expression of various pro-inflammatory cytokines with associated antiviral activities. Researchers have introduced GM-CSF as a vaccine adjuvant expressed in recombinant RSV (rRSV) during immunization [[83], [84], [85]]. This vaccine preparation attenuated viral replication, stimulated pulmonary CD4 + T cells, and augmented the proliferation and activation of pulmonary antigen-presenting cells during a challenge with the infectious agent [83]. The enhanced CD4 + T cell stimulation results in an increased production of IFN-γ, which is a key cytokine responsible for reducing RSV infections [83,86].
RSV infections are involved in severe asthma exacerbation reactions in asthmatic patients [87]. GM-CSF has demonstrated success in improving the hyperinflammatory response in asthmatic lungs exposed to RSV infection [88]. Although the exact mechanism was not completely defined, the authors attributed the effects observed by GM-CSF to its role in AM maturation, which helped reduce viral titers in the lungs of adult mice. In asthmatic airways, AMs have been identified as immature and hyperinflammatory, especially in the context of a subsequent RSV infection [88,89]. Thus, the use of GM-CSF in mice for this particular situation is advantageous as it allows for the full maturation of AMs to control the inflammatory status and clear the viral infection.
3.1.3. GM-CSF in HIV infection
HIV is known to preferentially infect CD4 + T cells, using CD4 as its primary receptor, with either CCR5 or CXCR4 chemokine receptors as coreceptors to enter cells [90]. In addition to CD4 + T cells, HIV targets myeloid cells including blood monocytes, DCs, macrophages, and osteoclasts [91]. Cytokines such as GM-CSF in the environmental milieu play an imperative role in regulating cells of the myeloid lineage including their phenotype and response to pathogens. During an HIV infection, GM-CSF is among one of the cytokines that is affected, with its production being drastically reduced [92,93]. This has been one of the earliest rationales for investigating the role of GM-CSF in fighting against HIV. Since this finding, many anti-HIV roles have been revealed for GM-CSF. For example, GM-CSF is involved in the maturation of monocytes into macrophages. An in vitro study reported that GM-CSF suppresses the expression of CXCR4 and CCR5 mRNA through the differentiation of monocytes into macrophages [94]. Ultimately, this suggests that GM-CSF allows macrophages to become more resistant to infection by HIV. However, other studies have shown that exposure of fresh monocytes and monocyte-derived macrophages to GM-CSF actually results in an increase in CCR5, but not CXCR4 expression, which contrasts these findings by indicating that HIV entry is enhanced in macrophages [95,96]. Regardless of these controversial findings, Kedzierska et al. reported that the inhibitory effect of GM-CSF is unrelated to the level of maturation of monocyte-derived macrophages at the time of GM-CSF stimulation during HIV infection [95]. This same study concluded that macrophages exposed to GM-CSF and HIV infection displayed a three- to ten-fold decrease in HIV-1 mRNA compared to infected macrophages not exposed to GM-CSF [95]. These findings agree with others investigating HIV mRNA levels in infected macrophages exposed to GM-CSF [[97], [98], [99], [100]] and also suggests that HIV replication is inhibited by GM-CSF actions before or at viral transcription.
Mechanistically, this antiviral activity of GM-CSF against HIV results from signalling through the β-chain of the GM-CSFR, irrespective of signalling from the α-chain. Albeit, the reduction of HIV mRNA by GM-CSF is not a universal finding as other clinical trials conclude GM-CSF has no effect on viral mRNA levels [[101], [102], [103]]. However, within one of the aforementioned trials, GM-CSF treated patients maintained unchanged HIV mRNA levels for a longer period while levels increased in placebo patients, demonstrating GM-CSF as a useful anti-HIV agent [101]. The other trials that contrast the success of GM-CSF in reducing HIV mRNA may have reported so due to too low of a GM-CSF dosage [102]. Nonetheless, a finding that is universal throughout the literature is that GM-CSF increases CD4 + T cell counts [97,101,104,105], which would be beneficial to the patient during the infection. GM-CSF has also been demonstrated to augment the effectiveness of the antiretroviral agent, zidovudine (AZT), in HIV infected macrophages in vitro [106,107] by upregulating thymidine kinase [107,108] to increase intracellular phosphorylation of AZT into its active triphosphate form [109].
In the context of HIV-1 infection of macrophages, other cellular markers in addition to CD4 have been investigated for their role in enabling HIV-1 infection of cells. Remarkably, Siglec-1 has been identified as a facilitator for HIV-1 infection of DCs and macrophages through binding sialoglycans on the gp120 envelope of the virus [110,111]. Recently, Jobe et al. reported that GM-CSF-derived macrophages have reduced surface expression of Siglec-1, rendering them less permissive to HIV-1 infection [112]. Ultimately, this group showed that GM-CSF-derived macrophages allowed significantly less virus particles to enter the cells and subsequently undergo replication as opposed to M-CSF-derived macrophages [112].
3.1.4. Virus encoded inhibitors interfere with GM-CSF signalling
Viruses employ multiple strategies to interfere with the induction and functions of IFN-inducible proteins, such as ISGs. In the case of GM-CSF, its actions are antagonized by a number of viruses including HIV-1 and orf virus [[113], [114], [115]]. In particular, the orf virus encodes a protein called GM-CSF/IL-2-inhibition factor, which acts to inhibit ovine GM-CSF and IL-2 through functioning as a competitive decoy receptor [113,114]. However, further studies are required to determine the function of this inhibitor in murine or human orf virus infections.
Interestingly, HIV-1 antagonizes the activation of GM-CSF-induced STAT5A in human monocyte-derived macrophages [115]. Warby et al., reported that HIV-1 inhibits the activation of STAT5A, without impeding expression of the STAT5A mRNA, protein, or other known members of the associated signalling pathway [115]. Altogether, these data provide foundation for the involvement of GM-CSF in antiviral functions.
3.2. Potential mechanisms of how GM-CSF can support antiviral functions
The exact molecular mechanisms responsible for antiviral activities involving GM-CSF have yet to be fully elucidated. It is possible that GM-CSF exerts its actions through similar mechanisms as other pro-inflammatory cytokines like IL-1β, TNF-α, and IL-6 via signalling molecules common with type I and type III IFN pathways. [[56], [57], [58], [59], [60]].Evidence supporting this idea come from studies where human macrophages treated with GM-CSF have demonstrated greater receptor expression and sensitivity to type III IFN signalling, promoting the generation of a robust antiviral and immunostimulatory gene signature [43].
Furthermore, GM-CSF, type I and type III IFNs signal via JAK/STAT pathways, which are vital to the antiviral state [42]. The JAK family members JAK1, JAK2, and TYK2 activate the STAT transcription factors to induce antiviral ISG production [116]. Thus, it is possible that the involvement of JAK2 in GM-CSF signalling contributes to the antiviral activity of GM-CSF. JAK2 transphosphorylation activates pathways other than JAK/STAT including PI3K and MAPK pathways (Fig. 1), the latter was also shown to confer antiviral protection [117].
GM-CSF induces homodimerization and signalling through STAT5, facilitating the transcription of genes for myeloid cell differentiation and survival (Fig. 1) [28]. Interestingly, the antiviral type I IFNs have been reported to induce the phosphorylation and dimerization of various STAT proteins outside of the canonical STAT1 and STAT2, which includes STAT5 [36]. Do these associations imply crosstalk amongst the signalling pathways facilitated by type I IFNs and other cytokines, including GM-CSF? Further investigations into the molecular signalling between GM-CSF and the type I IFNs are required to answer such questions. Nonetheless, additional evidence for the potential involvement of STAT5 against viral infections arises from the inhibition of its activation during HIV-1 infection because inhibition of STAT5 activation by the virus enhances its ability to establish infection [115].
Additionally, the IRF family of factors, mainly IRF1, IRF3, IRF5, and IRF7 can function in conjunction with STAT transcription factors to establish the events that lead to the antiviral state [118]. For example, IRF5 is an important downstream target of GM-CSF signalling, as it is involved in the polarization of an M1 phenotype in macrophages [22,34]. M1 macrophages have been reported to demonstrate antiviral characteristics [110]. This is partly a result of upregulated iNOS and NO, which are vital for antimicrobial and antiviral defenses [45,50,119]. Furthermore, IRF5 has demonstrated numerous antiviral functions in vitro due to upregulation of IFN-α as well as early inflammatory cytokines [120]. Therefore, it is possible that IRF5 activation and an overall M1-like phenotype are likely implicated in the induction of an antiviral state engendered by GM-CSF signalling. Support of this postulation is provided by a recent study that performed an in-depth gene expression analysis on ex vivo isolated human monocytes differentiated in GM-CSF versus M-CSF [121]. The findings revealed that macrophages polarized by GM-CSF have significantly upregulated expression of genes involved in the IFN response. The genes detected include ISG15, interferon induced protein with tetratricopeptide repeats 1–3 (IFIT), MX1, and OAS2/3, which all function as key antiviral molecules [121].
4. GM-CSF in clinical trials and immunotherapy
Cytokines play a vital role in regulating the immune response. As such, several cytokines have been tested and used in immunotherapies to treat cancers, infections, inflammation, and autoimmune diseases. IL-2, IFN-α, and GM-CSF are cytokines that can potentiate immune reactions, promote anti-tumour activities, and help clear infections [122]. For example, IL-2 stimulates T-lymphocyte and natural killer (NK) cell proliferation, and can act synergistically with GM-CSF to enhance the immune response against foreign antigens [122]. Immunotherapies have also focused on inhibiting pro-inflammatory cytokines such as GM-CSF and TNF-α to reduce inflammation in cases of excessive pro-inflammatory cytokine release, which can occur in many autoimmune diseases and some viral infections [122]. In this section, we highlight how GM-CSF has been targeted in the recent years with regard to clinical immunotherapeutic interventions.
4.1. Interfering with GM-CSF functions to lessen inflammation
Several diseases can occur from excess inflammation, in which case the pro-inflammatory properties of GM-CSF can exacerbate the condition [123]. This is the case in several autoimmune diseases such as RA, MS, and psoriasis, as well as the state of hyper-inflammation seen in some viral infections such as COVID-19 [123]. Anti-GM-CSF immunotherapies have been tested in animals and human subjects to suppress GM-CSF pro-inflammatory pathways in conditions like these. There are several monoclonal antibodies (Abs) such as Namilumab that can neutralize GM-CSF to reduce the inflammation by binding directly to GM-CSF, impeding interaction with its receptor and blocking any downstream pro-inflammatory effects [124]. Mavrilimumab is another human monoclonal Ab that targets the GM-CSF receptor-α rather than GM-CSF itself [124]. Mavrilimumab competes with GM-CSF for binding to its receptor thereby preventing activation of GM-CSF-mediated inflammatory pathways [124].
RA is a chronic autoimmune disease associated with the production of autoantibodies causing systemic inflammation in the joints. Elevated levels of GM-CSF have been reported in the synovial fluid of RA patients and were implicated in the observed inflammation [9]. Mavrilimumab was employed in a clinical trial (NCT01706926) for the treatment of RA where subjects received 30−150 mg of Mavrilimumabevery other week for 24 weeks [125]. The results revealed a significant decrease in RA disease activity, measured by the erythrocyte sedimentary rate and C-reactive protein [126].
Currently, with the COVID-19 pandemic, studies have begun investigating the use of monoclonal Abs against GM-CSF to treat the hyper-inflammatory state experienced by some severe COVID-19 pneumonia patients [123]. GM-CSF plays an important role in normal lung health as it is synthesized at low levels in lung alveoli for macrophage development, maintenance, and host defenses [65]. Zhou et al., reported on elevated levels of GM-CSF in the blood of COVID-19 patients and those with severe pneumonia were found to have an even higher percentage of GM-CSF + CD4 + Th cells [127]. One study administered 6 mg/kg of Mavrilimumab intravenously along with standard care to patients with severe COVID-19 pneumonia, hypoxia, or systemic inflammation (NCT04318366) [128]. Preliminary data indicate improved respiratory function and quicker resolution of inflammation, resulting in reduced morbidity of the patients in the trial. Several other trials using different monoclonal Abs against GM-CSF are currently underway where the outcomes are still pending.
4.2. GM-CSF as an adjuvant component in vaccine preparations
As a vaccine adjuvant, GM-CSF increases the immunogenicity of the vaccine to mount an efficient immune response. GM-CSF has been tested in numerous animal and human trials as a vaccine adjuvant for anti-tumour immunotherapy in prostate, skin, breast, and lung cancers with variable outcomes. Many prostate cancer vaccines are peptide vaccines that elicit limited immune activation. Consequently, GM-CSF has been used as an adjuvant with these vaccines to increase the anti-tumour immune response, via increased tumour-specific antigen presentation to induce better cross priming of T cells [129].
In an active study that began in 2012, patients with prostate cancers were given intradermal injections of a prostate-specific antigen (PSA) together with IL-2 and GM-CSF as a vaccine combination over 14 weeks (NCT02058680) [130]. Interim results indicated that 8 out of 11 participants exhibited increased immune responses to PSA by week 19 with several patients exhibiting slower cancer progression [131]. However, in a different prostate cancer clinical trial (NCT01322490) using GM-CSF as an adjuvant to the PROSTVAC vaccine [132], there was no change in overall survival in the GM-CSF treated group compared to controls. This lack of effectiveness was likely due to induction of weak immune responses in this trial [133].
GM-CSF has also been given preoperatively as a neoadjuvant to induce an anti-tumour immune response for cancer treatment. In a pilot study (NCT00305669) using GM-CSF as a neoadjuvant before radical prostatectomy in people with prostate cancer, patients were given 250 mg/m2/day of GM-CSF subcutaneously over 28 days [134]. In this study, the neoadjuvant GM-CSF enhanced CD4+ and CD8 + T cell infiltration to the prostate, but the expected amelioration in antigen presenting cell (APC) recruitment did not occur. Although there was no long-term follow-up for patients in this study, the increased T cell infiltration to the tumour microenvironment is promising for tumour suppression [126].
The mixed results published in GM-CSF adjuvant cancer trials could be attributed to different dose regimens. Under certain conditions, GM-CSF can exhibit immunosuppression effects via increasing the numbers of myeloid-derived suppressor cells (MDSCs) and regulatory T cells (Tregs) [135], that actually aid tumour growth rather than halt it [135]. Serafini et al., performed a study on mice that revealed an upper threshold of 1500 ng /106 / day of GM-CSF being responsible for immunosuppression allowing for potent tumour growth [136]. Another study found that high doses (>100 μg/day) of GM-CSF resulted in negative outcomes in skin and colon cancer patients [135]. However, more recently Butterfield et al., used 250 μg/day in combination with a peptide vaccine for patients with melanoma and found that only a minority had increased levels of MDSCs [137]. Therefore, while there is evidence that GM-CSF can have opposing effects at different doses, no optimal dosing regimen has been fully determined to date.
GM-CSF has also been used as an adjuvant to combat viral infections such as HIV and COVID-19, based on its ability to enhance DC maturation, and their ability to present viral antigens [138]. Previous HIV trials employing GM-CSF as an adjuvant reported inconsistent results with various positive or negative outcomes including no effect compared to controls. A recent HIV trial (NCT01627678) [139], used Vacc-C5 (a peptide vaccine) with GM-CSF as an adjuvant to ameliorate the vaccine’s immunogenicity and help increase T cell levels [138] reported only marginal changes. A trial in progress is assessing a vaccine composed of DC loaded with antigens from COVID-19 alongside GM-CSF as an adjuvant in non-infected participants to evaluate if it enhances anti-COVID-19 immunity (NCT04386252) [140]. This trial has only just started, and the results are pending.
4.3. GM-CSF-dependent immunotherapies to combat infections
GM-CSF was employed in a novel clinical investigation (NCT02601365) in 2019 to treat respiratory virus-associated pneumonia [141]. This study (data yet to be published) was based on several human and mice trials that observed an increase in AMs and enhanced pulmonary innate immune reactions in response to GM-CSF treatment of the virus-associated pneumonia and pneumonia-associated acute respiratory distress syndrome (ARDS), respectively [74,142].
Few other trials have also used GM-CSF to prevent nosocomial infections. One trial is attempting to reduce hospital-acquired infections in ICU-patients by GM-CSF treatment (NCT02361528) [143]. In this study, GM-CSF is thought to promote the differentiation of granulocytes and macrophages and increase neutrophil levels to decrease the risk of nosocomial infection and reverse immunoparalysis caused by the down-regulation of innate and adaptive immune responses [144]. GM-CSF is also being tested in a trial (NCT03769844) to resolve immunoparalysis in pediatric sepsis-induced multiple organ dysfunction syndrome [145]. Here, GM-CSF is thought to increase TNF-α production and monocyte HLA-DR expression to improve clinical outcomes in children with immunoparalysis by mounting an inflammatory immune response [144]. Currently, ongoing trials (NCT04326920) [146] are also assessing GM-CSF as an immune stimulator to help clear the COVID-19 infection by using recombinant GM-CSF (Leukine) over 5 days, along with standard of care to treat patients with ARDS caused by COVID-19. Leukine is expected to boost the host’s innate immune response mounted towards the virus by expanding cell populations of AMs and lung DCs to help clear the infection [142]. It has been used previously to improve oxygenation in patients with pneumonia-associated ARDS [142], and thus it is anticipated to improve COVID-19-associated ARDS.
In summary, GM-CSF shows great potential as a novel immunotherapy to treat many diseases and infections. However, the lack of consistency seen in the results from several studies reveals that much more research must be done before it is ready for widespread use. Interfering with GM-CSF functions seems to be effective in treating many diseases, so long as GM-CSF is significantly involved in the disease-associated inflammation. Understanding the conditions under which GM-CSF inadvertently exerts an immunosuppressive effect rather than an immunostimulatory response is important for ensuring future success in clinical trials using GM-CSF as an adjuvant. This is especially important as the use of GM-CSF in antiviral immunotherapies is largely rationalized by the fact that GM-CSF enhances innate antiviral immunity at the cellular level by increasing cellular proliferation, maturation, and antigen presentation.
5. Conclusion
GM-CSF serves many roles in the immune system including survival, differentiation, and proliferation of immune cells, exerting its actions through four main signalling pathways (JAK/STAT, PI3K, MAPK, and NF-κB). In this review, we focused on the antiviral roles that GM-CSF serves in association with other antiviral cytokines. GM-CSF’s antiviral activities have been studied in respiratory viruses such as IV and RSV. Insight into the functions of GM-CSF has led to the initiation of numerous clinical trials, the results of which appear to be promising on many fronts. These range from anti-GM-CSF immunotherapies to treat hyper-inflammatory disease states to vaccine adjuvant therapies to promote anti-tumour responses, and more recently to help prevent infections. Overall, the information presented in this review summarizes the recently reported data on how GM-CSF helps clear viral infections. Clearly, GM-CSF’s mechanisms of action should be further investigated in diverse viral models to determine its efficacies in various settings of immunotherapies. Whether the best immunotherapeutic strategies relying on GM-CSF will employ the individual cytokine alone, or use it in combination with other antivirals drugs or vaccine adjuvants, remains to be revealed by future studies examining this exciting prospect.
Declaration of Competing Interest
The authors report no declarations of interest.
Acknowledgements
The authors are supported by grants and salary awards from the Natural Sciences and Engineering Research Council of Canada, and the Ministry of Ontario.
Biography

Sam Basta is a professor of Immunology at Queen’s University, Canada. He obtained his PhD while working at the Institute of Virology and Immunoprophylaxis from the University of Bern in Switzerland in 2000. His group studies how professional antigen presenting cells can orchestrate innate and adaptive immune responses during virus infection or tumour growth.
References
- 1.Burgess A.W., Metcalf D. The nature and action of granulocyte-macrophage colony stimulating factors. Blood. 1980;56(6):947–958. [PubMed] [Google Scholar]
- 2.Hamilton J.A., Stanley E.R., Burgess A.W., Shadduck R.K. Stimulation of macrophage plasminogen activator activity by colony-stimulating factors. J. Cell. Physiol. 1980;103(3):435–445. doi: 10.1002/jcp.1041030309. [DOI] [PubMed] [Google Scholar]
- 3.Metcalf D. Hematopoietic cytokines. Blood. 2008;111(2):485–491. doi: 10.1182/blood-2007-03-079681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hamilton J.A. GM-CSF in inflammation. J. Exp. Med. 2020;217(1) doi: 10.1084/jem.20190945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Guilliams M., De Kleer I., Henri S., Post S., Vanhoutte L., De Prijck S., Deswarte K., Malissen B., Hammad H., Lambrecht B.N. Alveolar macrophages develop from fetal monocytes that differentiate into long-lived cells in the first week of life via GM-CSF. J. Exp. Med. 2013;210(10):1977–1992. doi: 10.1084/jem.20131199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lang F.M., Lee K.M., Teijaro J.R., Becher B., Hamilton J.A. GM-CSF-based treatments in COVID-19: reconciling opposing therapeutic approaches. Nat. Rev. Immunol. 2020;20(8):507–514. doi: 10.1038/s41577-020-0357-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Unkel B., Hoegner K., Clausen B.E., Lewe-Schlosser P., Bodner J., Gattenloehner S., Janßen H., Seeger W., Lohmeyer J., Herold S. Alveolar epithelial cells orchestrate DC function in murine viral pneumonia. J. Clin. Invest. 2012;122(10):3652–3664. doi: 10.1172/JCI62139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Williamson D.J., Begley C.G., Vadas M.A., Metcalf D. The detection and initial characterization of colony-stimulating factors in synovial fluid. Clin. Exp. Immunol. 1988;72(1):67–73. [PMC free article] [PubMed] [Google Scholar]
- 9.Hamilton J.A. Colony-stimulating factors in inflammation and autoimmunity. Nat. Rev. Immunol. 2008;8(7):533–544. doi: 10.1038/nri2356. [DOI] [PubMed] [Google Scholar]
- 10.Becher B., Tugues S., Greter M. GM-CSF: From Growth Factor to Central Mediator of Tissue Inflammation. Immunity. 2016;45(5):963–973. doi: 10.1016/j.immuni.2016.10.026. [DOI] [PubMed] [Google Scholar]
- 11.Gonzalez-Juarrero M., Hattle J.M., Izzo A., Junqueira-Kipnis A.P., Shim T.S., Trapnell B.C., Cooper A.M., Orme I.M. Disruption of granulocyte macrophage-colony stimulating factor production in the lungs severely affects the ability of mice to control Mycobacterium tuberculosis infection. J. Leukoc. Biol. 2005;77(6):914–922. doi: 10.1189/jlb.1204723. [DOI] [PubMed] [Google Scholar]
- 12.Santodonato L., D’Agostino G., Nisini R., Mariotti S., Monque D.M., Spada M., Lattanzi L., Perrone M.P., Andreotti M., Belardelli F., Ferrantini M. Monocyte-derived dendritic cells generated after a short-term culture with IFN-alpha and granulocyte-macrophage colony-stimulating factor stimulate a potent Epstein-Barr virus-specific CD8+ T cell response. J. Immunol. 2003;170(10):5195–5202. doi: 10.4049/jimmunol.170.10.5195. [DOI] [PubMed] [Google Scholar]
- 13.Carbonneil C., Aouba A., Burgard M., Cardinaud S., Rouzioux C., Langlade-Demoyen P., Weiss L. Dendritic cells generated in the presence of granulocyte-macrophage colony-stimulating factor and IFN-alpha are potent inducers of HIV-specific CD8 T cells. Aids. 2003;17(12):1731–1740. doi: 10.1097/00002030-200308150-00002. [DOI] [PubMed] [Google Scholar]
- 14.Baiocchi R.A., Ward J.S., Carrodeguas L., Eisenbeis C.F., Peng R., Roychowdhury S., Vourganti S., Sekula T., O’Brien M., Moeschberger M., Caligiuri M.A. GM-CSF and IL-2 induce specific cellular immunity and provide protection against Epstein-Barr virus lymphoproliferative disorder. J. Clin. Invest. 2001;108(6):887–894. doi: 10.1172/JCI12932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Barouch D.H., Santra S., Tenner-Racz K., Racz P., Kuroda M.J., Schmitz J.E., Jackson S.S., Lifton M.A., Freed D.C., Perry H.C., Davies M.E., Shiver J.W., Letvin N.L. Potent CD4+ T cell responses elicited by a bicistronic HIV-1 DNA vaccine expressing gp120 and GM-CSF. J. Immunol. 2002;168(2):562–568. doi: 10.4049/jimmunol.168.2.562. [DOI] [PubMed] [Google Scholar]
- 16.Parajuli B., Sonobe Y., Kawanokuchi J., Doi Y., Noda M., Takeuchi H., Mizuno T., Suzumura A. GM-CSF increases LPS-induced production of proinflammatory mediators via upregulation of TLR4 and CD14 in murine microglia. J. Neuroinflammation. 2012;9(1):268. doi: 10.1186/1742-2094-9-268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cook A.D., Pobjoy J., Steidl S., Dürr M., Braine E.L., Turner A.L., Lacey D.C., Hamilton J.A. Granulocyte-macrophage colony-stimulating factor is a key mediator in experimental osteoarthritis pain and disease development. Arthritis Res. Ther. 2012;14(5):R199. doi: 10.1186/ar4037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fleetwood A.J., Lawrence T., Hamilton J.A., Cook A.D. Granulocyte-macrophage colony-stimulating factor (CSF) and macrophage CSF-dependent macrophage phenotypes display differences in cytokine profiles and transcription factor activities: implications for CSF blockade in inflammation. J. Immunol. 2007;178(8):5245–5252. doi: 10.4049/jimmunol.178.8.5245. [DOI] [PubMed] [Google Scholar]
- 19.Alothaimeen T., Seaver K., Mulder R., Gee K., Basta S. Granulocyte/Macrophage colony-stimulating factor-derived macrophages exhibit distinctive early immune response to lymphocytic choriomeningitis virus infection. Viral Immunol. 2020 doi: 10.1089/vim.2019.0178. [DOI] [PubMed] [Google Scholar]
- 20.Trus E., Basta S., Gee K. Who’s in charge here? Macrophage colony stimulating factor and granulocyte macrophage colony stimulating factor: competing factors in macrophage polarization. Cytokine. 2020;127 doi: 10.1016/j.cyto.2019.154939. [DOI] [PubMed] [Google Scholar]
- 21.Khajah M., Millen B., Cara D.C., Waterhouse C., McCafferty D.M. Granulocyte-macrophage colony-stimulating factor (GM-CSF): a chemoattractive agent for murine leukocytes in vivo. J. Leukoc. Biol. 2011;89(6):945–953. doi: 10.1189/jlb.0809546. [DOI] [PubMed] [Google Scholar]
- 22.Hamilton J.A. GM-CSF-Dependent inflammatory pathways. Front. Immunol. 2019;10(2055) doi: 10.3389/fimmu.2019.02055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dougan M., Dranoff G., Dougan S.K. GM-CSF, IL-3, and IL-5 Family of Cytokines: Regulators of Inflammation. Immunity. 2019;50(4):796–811. doi: 10.1016/j.immuni.2019.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Carrieri P.B., Provitera V., De Rosa T., Tartaglia G., Gorga F., Perrella O. Profile of cerebrospinal fluid and serum cytokines in patients with relapsing-remitting multiple sclerosis: a correlation with clinical activity. Immunopharmacol. Immunotoxicol. 1998;20(3):373–382. doi: 10.3109/08923979809034820. [DOI] [PubMed] [Google Scholar]
- 25.Achuthan A., Aslam A.S.M., Nguyen Q., Lam P.Y., Fleetwood A.J., Frye A.T., Louis C., Lee M.C., Smith J.E., Cook A.D., Olshansky M., Turner S.J., Hamilton J.A. Glucocorticoids promote apoptosis of proinflammatory monocytes by inhibiting ERK activity. Cell Death Dis. 2018;9(3):267. doi: 10.1038/s41419-018-0332-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rosas M., Gordon S., Taylor P.R. Characterisation of the expression and function of the GM-CSF receptor alpha-chain in mice. Eur. J. Immunol. 2007;37(9):2518–2528. doi: 10.1002/eji.200636892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hercus T.R., Thomas D., Guthridge M.A., Ekert P.G., King-Scott J., Parker M.W., Lopez A.F. The granulocyte-macrophage colony-stimulating factor receptor: linking its structure to cell signaling and its role in disease. Blood. 2009;114(7):1289–1298. doi: 10.1182/blood-2008-12-164004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.van de Laar L., Coffer P.J., Woltman A.M. Regulation of dendritic cell development by GM-CSF: molecular control and implications for immune homeostasis and therapy. Blood. 2012;119(15):3383–3393. doi: 10.1182/blood-2011-11-370130. [DOI] [PubMed] [Google Scholar]
- 29.de Groot R.P., Coffer P.J., Koenderman L. Regulation of proliferation, differentiation and survival by the IL-3/IL-5/GM-CSF receptor family. Cell. Signal. 1998;10(9):619–628. doi: 10.1016/s0898-6568(98)00023-0. [DOI] [PubMed] [Google Scholar]
- 30.Katz S., Zsiros V., Doczi N., Kiss A.L. Inflammation-induced epithelial-to-Mesenchymal transition and GM-CSF treatment stimulate mesenteric mesothelial cells to transdifferentiate into macrophages. Inflammation. 2018;41(5):1825–1834. doi: 10.1007/s10753-018-0825-4. [DOI] [PubMed] [Google Scholar]
- 31.Meads M.B., Li Z.W., Dalton W.S. A novel TNF receptor-associated factor 6 binding domain mediates NF-kappa B signaling by the common cytokine receptor beta subunit. J. Immunol. 2010;185(3):1606–1615. doi: 10.4049/jimmunol.0902026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lee M.C., Lacey D.C., Fleetwood A.J., Achuthan A., Hamilton J.A., Cook A.D. GM-CSF- and IRF4-Dependent signaling can regulate myeloid cell numbers and the macrophage phenotype during inflammation. J. Immunol. 2019;202(10):3033–3040. doi: 10.4049/jimmunol.1801549. [DOI] [PubMed] [Google Scholar]
- 33.Krausgruber T., Blazek K., Smallie T., Alzabin S., Lockstone H., Sahgal N., Hussell T., Feldmann M., Udalova I.A. IRF5 promotes inflammatory macrophage polarization and TH1-TH17 responses. Nat. Immunol. 2011;12(3):231–238. doi: 10.1038/ni.1990. [DOI] [PubMed] [Google Scholar]
- 34.Paun A., Reinert J.T., Jiang Z., Medin C., Balkhi M.Y., Fitzgerald K.A., Pitha P.M. Functional characterization of murine interferon regulatory factor 5 (IRF-5) and its role in the innate antiviral response. J. Biol. Chem. 2008;283(21):14295–14308. doi: 10.1074/jbc.M800501200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sun L., Wu J., Du F., Chen X., Chen Z.J. Cyclic GMP-AMP Synthase Is a Cytosolic DNA Sensor That Activates the Type I Interferon Pathway. Science. 2013;339(6121):786. doi: 10.1126/science.1232458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ivashkiv L.B., Donlin L.T. Regulation of type I interferon responses, Nature reviews. Immunology. 2014;14(1):36–49. doi: 10.1038/nri3581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Marchetti M., Monier M.-N., Fradagrada A., Mitchell K., Baychelier F., Eid P., Johannes L., Lamaze C. Stat-mediated signaling induced by type I and type II interferons (IFNs) is differentially controlled through lipid microdomain association and clathrin-dependent endocytosis of IFN receptors. Mol. Biol. Cell. 2006;17(7):2896–2909. doi: 10.1091/mbc.E06-01-0076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Malakhova O.A., Yan M., Malakhov M.P., Yuan Y., Ritchie K.J., Kim K.I., Peterson L.F., Shuai K., Zhang D.E. Protein ISGylation modulates the JAK-STAT signaling pathway. Genes Dev. 2003;17(4):455–460. doi: 10.1101/gad.1056303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kotenko S.V., Gallagher G., Baurin V.V., Lewis-Antes A., Shen M., Shah N.K., Langer J.A., Sheikh F., Dickensheets H., Donnelly R.P. IFN-lambdas mediate antiviral protection through a distinct class II cytokine receptor complex. Nat. Immunol. 2003;4(1):69–77. doi: 10.1038/ni875. [DOI] [PubMed] [Google Scholar]
- 40.Sheppard P., Kindsvogel W., Xu W., Henderson K., Schlutsmeyer S., Whitmore T.E., Kuestner R., Garrigues U., Birks C., Roraback J., Ostrander C., Dong D., Shin J., Presnell S., Fox B., Haldeman B., Cooper E., Taft D., Gilbert T., Grant F.J., Tackett M., Krivan W., McKnight G., Clegg C., Foster D., Klucher K.M. IL-28, IL-29 and their class II cytokine receptor IL-28R. Nat. Immunol. 2003;4(1):63–68. doi: 10.1038/ni873. [DOI] [PubMed] [Google Scholar]
- 41.Odendall C., Kagan J.C. The unique regulation and functions of type III interferons in antiviral immunity. Curr. Opin. Virol. 2015;12:47–52. doi: 10.1016/j.coviro.2015.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Stanifer M.L., Pervolaraki K., Boulant S. Differential regulation of type I and type III interferon signaling. Int. J. Mol. Sci. 2019;20(6):1445. doi: 10.3390/ijms20061445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Read S.A., Wijaya R., Ramezani-Moghadam M., Tay E., Schibeci S., Liddle C., Lam V.W.T., Yuen L., Douglas M.W., Booth D., George J., Ahlenstiel G. Macrophage coordination of the interferon lambda immune response. Front. Immunol. 2019;10(2674) doi: 10.3389/fimmu.2019.02674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Horvath C.M. The Jak-STAT pathway stimulated by interferon gamma. Sci. STKE. 2004;(260) doi: 10.1126/stke.2602004tr8. (2004) tr8. [DOI] [PubMed] [Google Scholar]
- 45.Banete A., Achita P., Harding K., Mulder R., Basta S. Immortalized murine macrophage cell line as a model for macrophage polarization into classically activated m(IFNgamma+LPS) or alternatively activated m(IL-4) macrophages. J. Clin. Cell. Immunol. 2015;6(- 2155-9899):1–7. [Google Scholar]
- 46.Tugal D., Liao X., Jain M.K. Transcriptional control of macrophage polarization. Arterioscler. Thromb. Vasc. Biol. 2013;33(6):1135–1144. doi: 10.1161/ATVBAHA.113.301453. [DOI] [PubMed] [Google Scholar]
- 47.Muller K.M., Ebensperger C., Tampe R. Nucleotide binding to the hydrophilic C-terminal domain of the transporter associated with antigen processing (TAP) J. Biol. Chem. 1994;269(19):14032–14037. [PubMed] [Google Scholar]
- 48.Huang S., Hendriks W., Althage A., Hemmi S., Bluethmann H., Kamijo R., Vilcek J., Zinkernagel R.M., Aguet M. Immune response in mice that lack the interferon-gamma receptor. Science. 1993;259(5102):1742–1745. doi: 10.1126/science.8456301. [DOI] [PubMed] [Google Scholar]
- 49.Changotra H., Jia Y., Moore T.N., Liu G., Kahan S.M., Sosnovtsev S.V., Karst S.M. Type I and type II interferons inhibit the translation of murine norovirus proteins. J. Virol. 2009;83(11):5683–5692. doi: 10.1128/JVI.00231-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Jarasch N., Martin U., Kamphausen E., Zell R., Wutzler P., Henke A. Interferon-gamma-induced activation of nitric oxide-mediated antiviral activity of macrophages caused by a recombinant coxsackievirus B3. Viral Immunol. 2005;18(2):355–364. doi: 10.1089/vim.2005.18.355. [DOI] [PubMed] [Google Scholar]
- 51.Brochériou I., Maouche S., Durand H., Braunersreuther V., Le Naour G., Gratchev A., Koskas F., Mach F., Kzhyshkowska J., Ninio E. Antagonistic regulation of macrophage phenotype by M-CSF and GM-CSF: implication in atherosclerosis. Atherosclerosis. 2011;214(2):316–324. doi: 10.1016/j.atherosclerosis.2010.11.023. [DOI] [PubMed] [Google Scholar]
- 52.Velazquez-Salinas L., Verdugo-Rodriguez A., Rodriguez L.L., Borca M.V. The role of interleukin 6 during viral infections. Front. Microbiol. 2019;10(1057) doi: 10.3389/fmicb.2019.01057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Orzalli M.H., Smith A., Jurado K.A., Iwasaki A., Garlick J.A., Kagan J.C. An antiviral branch of the IL-1 signaling pathway restricts immune-evasive virus replication. Mol. Cell. 2018;71(5):825–840. doi: 10.1016/j.molcel.2018.07.009. e6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ruby J., Bluethmann H., Peschon J.J. Antiviral activity of tumor necrosis factor (TNF) is mediated via p55 and p75 TNF receptors. J. Exp. Med. 1997;186(9):1591–1596. doi: 10.1084/jem.186.9.1591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Seo S.H., Webster R.G. Tumor necrosis factor alpha exerts powerful anti-influenza virus effects in lung epithelial cells. J. Virol. 2002;76(3):1071. doi: 10.1128/JVI.76.3.1071-1076.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Lucin P., Jonjić S., Messerle M., Polić B., Hengel H., Koszinowski U.H. Late phase inhibition of murine cytomegalovirus replication by synergistic action of interferon-gamma and tumour necrosis factor. J. Gen. Virol. 1994;75(Pt 1):101–110. doi: 10.1099/0022-1317-75-1-101. [DOI] [PubMed] [Google Scholar]
- 57.Mariani M.K., Dasmeh P., Fortin A., Caron E., Kalamujic M., Harrison A.N., Hotea D.I., Kasumba D.M., Cervantes-Ortiz S.L., Mukawera E., Serohijos A.W.R., Grandvaux N. The combination of IFN β and TNF induces an antiviral and immunoregulatory program via non-canonical pathways involving STAT2 and IRF9. Cells. 2019;8(8) doi: 10.3390/cells8080919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Luo J., Zhang B., Wu Y., Tian Q., Mo M., Long T., Mei M., Fan R., Lyu Z., Jiang H., Wu F., Lin Y., Guo X. Recombinant rabies virus expressing interleukin-6 enhances the immune response in mouse brain. Arch. Virol. 2018;163(7):1889–1895. doi: 10.1007/s00705-018-3808-8. [DOI] [PubMed] [Google Scholar]
- 59.Ichikawa T., Nakao K., Nakata K., Yamashita M., Hamasaki K., Shigeno M., Abiru S., Ishikawa H., Ishii N., Eguchi K. Involvement of IL-1beta and IL-10 in IFN-alpha-mediated antiviral gene induction in human hepatoma cells. Biochem. Biophys. Res. Commun. 2002;294(2):414–422. doi: 10.1016/S0006-291X(02)00502-8. [DOI] [PubMed] [Google Scholar]
- 60.Aarreberg L.D., Wilkins C., Ramos H.J., Green R., Davis M.A., Chow K., Gale M. Interleukin-1β signaling in dendritic cells induces antiviral interferon responses. mBio. 2018;9(2):e00342–18. doi: 10.1128/mBio.00342-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Tanaka T., Narazaki M., Kishimoto T. IL-6 in inflammation, immunity, and disease. Cold Spring Harb. Perspect. Biol. 2014;6(10) doi: 10.1101/cshperspect.a016295. a016295-a016295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.O’Neill L.A.J. The interleukin-1 receptor/Toll-like receptor superfamily: 10 years of progress. Immunol. Rev. 2008;226(1):10–18. doi: 10.1111/j.1600-065X.2008.00701.x. [DOI] [PubMed] [Google Scholar]
- 63.Zhu H., Liu C. Interleukin-1 inhibits hepatitis C virus subgenomic RNA replication by activation of extracellular regulated kinase pathway. J. Virol. 2003;77(9):5493. doi: 10.1128/JVI.77.9.5493-5498.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Kuo T.-M., Hu C.-p., Chen Y.-L., Hong M.-H., Jeng K.-S., Liang C.-C.T., Chen M.-L., Chang C. HBV replication is significantly reduced by IL-6. J. Biomed. Sci. 2009;16(1):41. doi: 10.1186/1423-0127-16-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Berclaz P.Y., Shibata Y., Whitsett J.A., Trapnell B.C. GM-CSF, via PU.1, regulates alveolar macrophage Fcgamma R-mediated phagocytosis and the IL-18/IFN-gamma -mediated molecular connection between innate and adaptive immunity in the lung. Blood. 2002;100(12):4193–4200. doi: 10.1182/blood-2002-04-1102. [DOI] [PubMed] [Google Scholar]
- 66.Dranoff G., Crawford A.D., Sadelain M., Ream B., Rashid A., Bronson R.T., Dickersin G.R., Bachurski C.J., Mark E.L., Whitsett J.A., et al. Involvement of granulocyte-macrophage colony-stimulating factor in pulmonary homeostasis. Science. 1994;264(5159):713. doi: 10.1126/science.8171324. [DOI] [PubMed] [Google Scholar]
- 67.Kuwano K., Braciale T.J., Ennis F.A. Cytotoxic T lymphocytes recognize a cross-reactive epitope on the transmembrane region of influenza H1 and H2 hemagglutinins. Viral Immunol. 1989;2(3):163–173. doi: 10.1089/vim.1989.2.163. [DOI] [PubMed] [Google Scholar]
- 68.Coro E.S., Chang W.L., Baumgarth N. Type I IFN receptor signals directly stimulate local B cells early following influenza virus infection. J. Immunol. 2006;176(7):4343–4351. doi: 10.4049/jimmunol.176.7.4343. [DOI] [PubMed] [Google Scholar]
- 69.Lau Y.F., Tang L.H., Ooi E.E., Subbarao K. Activation of the innate immune system provides broad-spectrum protection against influenza A viruses with pandemic potential in mice. Virology. 2010;406(1):80–87. doi: 10.1016/j.virol.2010.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Huber V.C., Lynch J.M., Bucher D.J., Le J., Metzger D.W. Fc receptor-mediated phagocytosis makes a significant contribution to clearance of influenza virus infections. J. Immunol. 2001;166(12):7381–7388. doi: 10.4049/jimmunol.166.12.7381. [DOI] [PubMed] [Google Scholar]
- 71.Kim H.M., Lee Y.W., Lee K.J., Kim H.S., Cho S.W., van Rooijen N., Guan Y., Seo S.H. Alveolar macrophages are indispensable for controlling influenza viruses in lungs of pigs. J. Virol. 2008;82(9):4265–4274. doi: 10.1128/JVI.02602-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Cakarova L., Marsh L.M., Wilhelm J., Mayer K., Grimminger F., Seeger W., Lohmeyer J., Herold S. Macrophage tumor necrosis factor-alpha induces epithelial expression of granulocyte-macrophage colony-stimulating factor: impact on alveolar epithelial repair. Am. J. Respir. Crit. Care Med. 2009;180(6):521–532. doi: 10.1164/rccm.200812-1837OC. [DOI] [PubMed] [Google Scholar]
- 73.Huang F.F., Barnes P.F., Feng Y., Donis R., Chroneos Z.C., Idell S., Allen T., Perez D.R., Whitsett J.A., Dunussi-Joannopoulos K., Shams H. GM-CSF in the lung protects against lethal influenza infection. Am. J. Respir. Crit. Care Med. 2011;184(2):259–268. doi: 10.1164/rccm.201012-2036OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Sever-Chroneos Z., Murthy A., Davis J., Florence J.M., Kurdowska A., Krupa A., Tichelaar J.W., White M.R., Hartshorn K.L., Kobzik L., Whitsett J.A., Chroneos Z.C. GM-CSF modulates pulmonary resistance to influenza A infection. Antiviral Res. 2011;92(2):319–328. doi: 10.1016/j.antiviral.2011.08.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Tuvim M.J., Evans S.E., Clement C.G., Dickey B.F., Gilbert B.E. Augmented lung inflammation protects against influenza A pneumonia. PLoS One. 2009;4(1):e4176. doi: 10.1371/journal.pone.0004176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Subramaniam R., Hillberry Z., Chen H., Feng Y., Fletcher K., Neuenschwander P., Shams H. Delivery of GM-CSF to protect against influenza pneumonia. PLoS One. 2015;10(4) doi: 10.1371/journal.pone.0124593. e0124593-e0124593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Subramaniam R., Barnes P.F., Fletcher K., Boggaram V., Hillberry Z., Neuenschwander P., Shams H. Protecting against post-influenza bacterial pneumonia by increasing phagocyte recruitment and ROS production. J. Infect. Dis. 2014;209(11):1827–1836. doi: 10.1093/infdis/jit830. [DOI] [PubMed] [Google Scholar]
- 78.Diallo M., Zheng Y., Chen X., He Y., Zhou H., Chen Z. Prospect of IL-2, IL-7, IL-15 and IL-21 for HIV immune-based therapy, Zhong nan da xue xue bao. Yi xue ban = J. Central South Univ. Med. Sci. 2011;36(11):1037–1045. doi: 10.3969/j.issn.1672-7347.2011.11.002. [DOI] [PubMed] [Google Scholar]
- 79.Dessing M.C., van der Sluijs K.F., Florquin S., van der Poll T. Monocyte chemoattractant protein 1 contributes to an adequate immune response in influenza pneumonia. Clin. Immunol. 2007;125(3):328–336. doi: 10.1016/j.clim.2007.08.001. [DOI] [PubMed] [Google Scholar]
- 80.Narasaraju T., Ng H.H., Phoon M.C., Chow V.T. MCP-1 antibody treatment enhances damage and impedes repair of the alveolar epithelium in influenza pneumonitis. Am. J. Respir. Cell Mol. Biol. 2010;42(6):732–743. doi: 10.1165/rcmb.2008-0423OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Marsolais D., Hahm B., Walsh K.B., Edelmann K.H., McGavern D., Hatta Y., Kawaoka Y., Rosen H., Oldstone M.B. A critical role for the sphingosine analog AAL-R in dampening the cytokine response during influenza virus infection. Proc. Natl. Acad. Sci. U. S. A. 2009;106(5):1560–1565. doi: 10.1073/pnas.0812689106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Hussell T., Pennycook A., Openshaw P.J. Inhibition of tumor necrosis factor reduces the severity of virus-specific lung immunopathology. Eur. J. Immunol. 2001;31(9):2566–2573. doi: 10.1002/1521-4141(200109)31:9<2566::aid-immu2566>3.0.co;2-l. [DOI] [PubMed] [Google Scholar]
- 83.Bukreyev A., Belyakov I.M., Berzofsky J.A., Murphy B.R., Collins P.L. Granulocyte-macrophage colony-stimulating factor expressed by recombinant respiratory syncytial virus attenuates viral replication and increases the level of pulmonary antigen-presenting cells. J. Virol. 2001;75(24):12128–12140. doi: 10.1128/JVI.75.24.12128-12140.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Ahlers J.D., Dunlop N., Alling D.W., Nara P.L., Berzofsky J.A. Cytokine-in-adjuvant steering of the immune response phenotype to HIV-1 vaccine constructs: granulocyte-macrophage colony-stimulating factor and TNF-alpha synergize with IL-12 to enhance induction of cytotoxic T lymphocytes. J. Immunol. 1997;158(8):3947–3958. [PubMed] [Google Scholar]
- 85.Disis M.L., Bernhard H., Shiota F.M., Hand S.L., Gralow J.R., Huseby E.S., Gillis S., Cheever M.A. Granulocyte-macrophage colony-stimulating factor: an effective adjuvant for protein and peptide-based vaccines. Blood. 1996;88(1):202–210. [PubMed] [Google Scholar]
- 86.Bukreyev A., Whitehead S.S., Bukreyeva N., Murphy B.R., Collins P.L. Interferon gamma expressed by a recombinant respiratory syncytial virus attenuates virus replication in mice without compromising immunogenicity. Proc. Natl. Acad. Sci. U. S. A. 1999;96(5):2367–2372. doi: 10.1073/pnas.96.5.2367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Simpson J.L., Moric I., Wark P.A.B., Johnston S.L., Gibson P.G. Use of induced sputum for the diagnosis of influenza and infections in asthma: a comparison of diagnostic techniques. Journal of Clinical Virology. 2003;26(3):339–346. doi: 10.1016/S1386-6532(02)00084-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Naessens T., Schepens B., Smet M., Pollard C., Van Hoecke L., De Beuckelaer A., Willart M., Lambrecht B., De Koker S., Saelens X., Grooten J. GM-CSF treatment prevents respiratory syncytial virus-induced pulmonary exacerbation responses in postallergic mice by stimulating alveolar macrophage maturation. J. Allergy Clin. Immunol. 2016;137(3) doi: 10.1016/j.jaci.2015.09.031. [DOI] [PubMed] [Google Scholar]
- 89.Grooten J., Schepens B., Smet M., Saelens X., Naessens T. The hyperinflammatory reactivity of post-asthma alveolar macrophages contributes to RSV-induced asthma exacerbations (HYP7P.269) J. Immunol. 2015;194(1 Supplement) 191.17. [Google Scholar]
- 90.Wilen C.B., Tilton J.C., Doms R.W. HIV: cell binding and entry. Cold Spring Harb. Perspect. Med. 2012;2(8) doi: 10.1101/cshperspect.a006866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Gohda J., Ma Y., Huang Y., Zhang Y., Gu L., Han Y., Li T., Gao B., Gao G.F., Inoue J.-i., Iwamoto A., Ishida T. HIV-1 replicates in human osteoclasts and enhances their differentiation in vitro. Retrovirology. 2015;12(1):12. doi: 10.1186/s12977-015-0139-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Esser R., Glienke W., von Briesen H., Rübsamen-Waigmann H., Andreesen R. Differential regulation of proinflammatory and hematopoietic cytokines in human macrophages after infection with human immunodeficiency virus. Blood. 1996;88(9):3474–3481. [PubMed] [Google Scholar]
- 93.Esser R., Glienke W., Andreesen R., Unger R.E., Kreutz M., Rübsamen-Waigmann H., von Briesen H. Individual cell analysis of the cytokine repertoire in human immunodeficiency virus-1-infected monocytes/macrophages by a combination of immunocytochemistry and in situ hybridization. Blood. 1998;91(12):4752–4760. [PubMed] [Google Scholar]
- 94.Di Marzio P., Tse J., Landau N.R. Chemokine receptor regulation and HIV type 1 tropism in monocyte-macrophages. AIDS Res. Hum. Retroviruses. 1998;14(2):129–138. doi: 10.1089/aid.1998.14.129. [DOI] [PubMed] [Google Scholar]
- 95.Kedzierska K., Maerz A., Warby T., Jaworowski A., Chan H., Mak J., Sonza S., Lopez A., Crowe S. Granulocyte-macrophage colony-stimulating factor inhibits HIV-1 replication in monocyte-derived macrophages. Aids. 2000;14(12):1739–1748. doi: 10.1097/00002030-200008180-00008. [DOI] [PubMed] [Google Scholar]
- 96.Tuttle D.L., Harrison J.K., Anders C., Sleasman J.W., Goodenow M.M. Expression of CCR5 increases during monocyte differentiation and directly mediates macrophage susceptibility to infection by human immunodeficiency virus type 1. J. Virol. 1998;72(6):4962–4969. doi: 10.1128/jvi.72.6.4962-4969.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Schooley R.T., Mladenovic J., Sevin A., Chiu S., Miles S.A., Pomerantz R.J., Campbell T.B., Bell D., Ambruso D., Wong R., Landay A., Coombs R.W., Fox L., Kamoun M., Jacovini J. Reduced mobilization of CD34+ stem cells in advanced human immunodeficiency virus type 1 disease. J. Infect. Dis. 2000;181(1):148–157. doi: 10.1086/315168. [DOI] [PubMed] [Google Scholar]
- 98.Brites C., Gilbert M.J., Pedral-Sampaio D., Bahia F., Pedroso C., Paula Alcantara A., das Gracas Sasaki M., Matos J., Renjifo B., Essex M., Whitmore J.B., Agosti J.M., Badaro R. A randomized, placebo-controlled trial of granulocyte-macrophage colony-stimulating factor and nucleoside analogue therapy in AIDS. J. Infect. Dis. 2000;182(5):1531–1535. doi: 10.1086/315901. [DOI] [PubMed] [Google Scholar]
- 99.Skowron G., Stein D., Drusano G., Melbourne K., Bilello J., Mikolich D., Rana K., Agosti J.M., Mongillo A., Whitmore J., Gilbert M.J. The safety and efficacy of granulocyte-macrophage colony-stimulating factor (Sargramostim) added to indinavir- or ritonavir-based antiretroviral therapy: a randomized double-blind, placebo-controlled trial. J. Infect. Dis. 1999;180(4):1064–1071. doi: 10.1086/314981. [DOI] [PubMed] [Google Scholar]
- 100.Matsuda S., Akagawa K., Honda M., Yokota Y., Takebe Y., Takemori T. Suppression of HIV replication in human monocyte-derived macrophages induced by granulocyte/macrophage colony-stimulating factor. AIDS Res. Hum. Retroviruses. 1995;11(9):1031–1038. doi: 10.1089/aid.1995.11.1031. [DOI] [PubMed] [Google Scholar]
- 101.Angel J.B., High K., Rhame F., Brand D., Whitmore J.B., Agosti J.M., Gilbert M.J., Deresinski S. Phase III study of granulocyte-macrophage colony-stimulating factor in advanced HIV disease: effect on infections, CD4 cell counts and HIV suppression. Leukine/HIV Study Group. Aids. 2000;14(4):387–395. doi: 10.1097/00002030-200003100-00012. [DOI] [PubMed] [Google Scholar]
- 102.Davison F.D., Kaczmarski R.S., Pozniak A., Mufti G.J., Sutherland S. Quantification of HIV by PCR in monocytes and lymphocytes in patients receiving antiviral treatment and low dose recombinant human granulocyte macrophage colony stimulating factor. J. Clin. Pathol. 1994;47(9):855–857. doi: 10.1136/jcp.47.9.855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Scadden D.T., Pickus O., Hammer S.M., Stretcher B., Bresnahan J., Gere J., McGrath J., Agosti J.M. Lack of in Vivo Effect of Granulocyte-Macrophage Colony-Stimulating Factor on Human Immunodeficiency Virus Type 1. AIDS Research and Human Retroviruses. 1996;12(12):1151–1159. doi: 10.1089/aid.1996.12.1151. [DOI] [PubMed] [Google Scholar]
- 104.Palumbo P.E., Raskino C., Fiscus S., Pahwa S., Fowler M.G., Spector S.A., Englund J.A., Baker C.J. Predictive value of quantitative plasma HIV RNA and CD4+ lymphocyte count in HIV-infected infants and children. JAMA. 1998;279(10):756–761. doi: 10.1001/jama.279.10.756. [DOI] [PubMed] [Google Scholar]
- 105.Jacobson J.M., Lederman M.M., Spritzler J., Valdez H., Tebas P., Skowron G., Wang R., Jackson J.B., Fox L., Landay A., Gilbert M.J., O'Neil D., Bancroft L., Al-Harthi L., Jacobson M.A., Merigan T.C., Jr., Glesby M.J. Granulocyte-macrophage colony-stimulating factor induces modest increases in plasma human immunodeficiency virus (HIV) type 1 RNA levels and CD4+ lymphocyte counts in patients with uncontrolled HIV infection. J. Infect. Dis. 2003;188(12):1804–1814. doi: 10.1086/379899. [DOI] [PubMed] [Google Scholar]
- 106.Hammer S.M., Gillis J.M., Pinkston P., Rose R.M. Effect of zidovudine and granulocyte-macrophage colony-stimulating factor on human immunodeficiency virus replication in alveolar macrophages. Blood. 1990;75(6):1215–1219. [PubMed] [Google Scholar]
- 107.Perno C.F., Cooney D.A., Gao W.Y., Hao Z., Johns D.G., Foli A., Hartman N.R., Caliò R., Broder S., Yarchoan R. Effects of bone marrow stimulatory cytokines on human immunodeficiency virus replication and the antiviral activity of dideoxynucleosides in cultures of monocyte/macrophages. Blood. 1992;80(4):995–1003. [PubMed] [Google Scholar]
- 108.Dhawan R.K., Kharbanda S., Nakamura M., Ohno T., Kufe D. Effects of granulocyte-macrophage colony-stimulating factor on 3’-azido-3’-deoxythymidine uptake, phosphorylation and nucleotide retention in human U-937 cells. Biochem. Pharmacol. 1990;40(12):2695–2700. doi: 10.1016/0006-2952(90)90589-d. [DOI] [PubMed] [Google Scholar]
- 109.Furman P.A., Fyfe J.A., St Clair M.H., Weinhold K., Rideout J.L., Freeman G.A., Lehrman S.N., Bolognesi D.P., Broder S., Mitsuya H., et al. Phosphorylation of 3’-azido-3’-deoxythymidine and selective interaction of the 5’-triphosphate with human immunodeficiency virus reverse transcriptase. Proc. Natl. Acad. Sci. U. S. A. 1986;83(21):8333–8337. doi: 10.1073/pnas.83.21.8333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Izquierdo-Useros N., Lorizate M., McLaren P.J., Telenti A., Kräusslich H.G., Martinez-Picado J. HIV-1 capture and transmission by dendritic cells: the role of viral glycolipids and the cellular receptor Siglec-1. PLoS Pathog. 2014;10(7) doi: 10.1371/journal.ppat.1004146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Zou Z., Chastain A., Moir S., Ford J., Trandem K., Martinelli E., Cicala C., Crocker P., Arthos J., Sun P.D. Siglecs facilitate HIV-1 infection of macrophages through adhesion with viral sialic acids. PLoS One. 2011;6(9) doi: 10.1371/journal.pone.0024559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Jobe O., Trinh H.V., Kim J., Alsalmi W., Tovanabutra S., Ehrenberg P.K., Peachman K.K., Gao G., Thomas R., Kim J.H., Michael N.L., Alving C.R., Rao V.B., Rao M. Effect of cytokines on Siglec-1 and HIV-1 entry in monocyte-derived macrophages: the importance of HIV-1 envelope V1V2 region. J. Leukoc. Biol. 2016;99(6):1089–1106. doi: 10.1189/jlb.2A0815-361R. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Deane D., McInnes C.J., Percival A., Wood A., Thomson J., Lear A., Gilray J., Fleming S., Mercer A., Haig D. Orf virus encodes a novel secreted protein inhibitor of granulocyte-macrophage colony-stimulating factor and interleukin-2. J. Virol. 2000;74(3):1313–1320. doi: 10.1128/jvi.74.3.1313-1320.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Felix J., Kandiah E., De Munck S., Bloch Y., van Zundert G.C., Pauwels K., Dansercoer A., Novanska K., Read R.J., Bonvin A.M., Vergauwen B., Verstraete K., Gutsche I., Savvides S.N. Structural basis of GM-CSF and IL-2 sequestration by the viral decoy receptor GIF. Nat. Commun. 2016;7:13228. doi: 10.1038/ncomms13228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Warby T.J., Crowe S.M., Jaworowski A. Human immunodeficiency virus type 1 infection inhibits granulocyte-macrophage colony-stimulating factor-induced activation of STAT5A in human monocyte-derived macrophages. J. Virol. 2003;77(23):12630. doi: 10.1128/JVI.77.23.12630-12638.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Leonard W.J., O’Shea J.J. Jaks and STATs: biological implications. Annu. Rev. Immunol. 1998;16:293–322. doi: 10.1146/annurev.immunol.16.1.293. [DOI] [PubMed] [Google Scholar]
- 117.Pervolaraki K., Stanifer M.L., Münchau S., Renn L.A., Albrecht D., Kurzhals S., Senís E., Grimm D., Schröder-Braunstein J., Rabin R.L., Boulant S. Type I and type III interferons display different dependency on mitogen-activated protein kinases to mount an antiviral state in the human gut. Front. Immunol. 2017;8:459. doi: 10.3389/fimmu.2017.00459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Chiang H.-S., Liu H.M. The molecular basis of viral inhibition of IRF- and STAT-Dependent immune responses. Front. Immunol. 2019;9(3086) doi: 10.3389/fimmu.2018.03086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Karupiah G., Xie Q.W., Buller R.M., Nathan C., Duarte C., MacMicking J.D. Inhibition of viral replication by interferon-gamma-induced nitric oxide synthase. Science. 1993;261(5127):1445. doi: 10.1126/science.7690156. [DOI] [PubMed] [Google Scholar]
- 120.Yanai H., Chen H.-M., Inuzuka T., Kondo S., Mak T.W., Takaoka A., Honda K., Taniguchi T. Role of IFN regulatory factor 5 transcription factor in antiviral immunity and tumor suppression. Proc. Natl. Acad. Sci. U. S. A. 2007;104(9):3402–3407. doi: 10.1073/pnas.0611559104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Rodriguez R.M., Suarez-Alvarez B., Lavín J.L., Ascensión A.M., Gonzalez M., Lozano J.J., Raneros A.B., Bulnes P.D., Vidal-Castiñeira J.R., Huidobro C., Martin-Martin C., Sanz A.B., Ruiz-Ortega M., Puig-Kröger A., Corbí A.L., Araúzo-Bravo M.J., Aransay A.M., Lopez-Larrea C. Signal integration and transcriptional regulation of the inflammatory response mediated by the GM-/M-CSF signaling Axis in human monocytes. Cell Rep. 2019;29(4):860–872. doi: 10.1016/j.celrep.2019.09.035. e5. [DOI] [PubMed] [Google Scholar]
- 122.Berraondo P., Sanmamed M.F., Ochoa M.C., Etxeberria I., Aznar M.A., Perez-Gracia J.L., Rodriguez-Ruiz M.E., Ponz-Sarvise M., Castanon E., Melero I. Cytokines in clinical cancer immunotherapy. Br. J. Cancer. 2019;120(1):6–15. doi: 10.1038/s41416-018-0328-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.De Luca G., Cavalli G., Campochiaro C., Della-Torre E., Angelillo P., Tomelleri A., Boffini N., Tentori S., Mette F., Farina N., Rovere-Querini P., Ruggeri A., D’Aliberti T., Scarpellini P., Landoni G., De Cobelli F., Paolini J.F., Zangrillo A., Tresoldi M., Trapnell B.C., Ciceri F., Dagna L. GM-CSF blockade with mavrilimumab in severe COVID-19 pneumonia and systemic hyperinflammation: a single-centre, prospective cohort study. Lancet Rheumatol. 2020;2(8):e465–e473. doi: 10.1016/S2665-9913(20)30170-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Crotti C., Raimondo M.G., Becciolini A., Biggioggero M., Favalli E.G. Spotlight on mavrilimumab for the treatment of rheumatoid arthritis: evidence to date. Drug Des. Dev. Ther. 2017;11:211–223. doi: 10.2147/DDDT.S104233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Albulescu M. 2012. A Study of Mavrilimumab in Subjects with Moderate-to-Severe Rheumatoid Arthritis.https://clinicaltrials.gov/ct2/show/NCT01706926 [Google Scholar]
- 126.Burmester G.R., McInnes I.B., Kremer J., Miranda P., Korkosz M., Vencovsky J., Rubbert-Roth A., Mysler E., Sleeman M.A., Godwood A., Sinibaldi D., Guo X., White W.I., Wang B., Wu C.-Y., Ryan P.C., Close D., Weinblatt M.E. A randomised phase IIb study of mavrilimumab, a novel GM–CSF receptor alpha monoclonal antibody, in the treatment of rheumatoid arthritis. Ann. Rheum. Dis. 2017;76(6):1020. doi: 10.1136/annrheumdis-2016-210624. [DOI] [PubMed] [Google Scholar]
- 127.Zhou Y.G., Fu B.Q., Zheng X.H., Wang D.S., Zhao C.C., Qi Y.J., Sun R., Tian Z.G., Xu X.L., Wei H.M. Pathogenic T-cells and inflammatory monocytes incite inflammatory storms in severe COVID-19 patients. Sci. Rev. 2020;7(6):998–1002. doi: 10.1093/nsr/nwaa041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Landoni G. 2020. COVID-19 Patients Characterization, Biobank, Treatment Response and Outcome Predictor (COVID-BioB)https://clinicaltrials.gov/ct2/show/NCT04318366 [Google Scholar]
- 129.Basta S., Alatery A. The cross-priming pathway: a portrait of an intricate immune system. Scand. J. Immunol. 2007;65(4):311–319. doi: 10.1111/j.1365-3083.2007.01909.x. [DOI] [PubMed] [Google Scholar]
- 130.Wang-Rodriguez J., Daniels A. 2012. Gregory, Phase 1A/1B Study of PSA/IL-2/GM-CSF Vaccine for Recurrent Prostate Cancer in Hormone Naive and Hormone Independent Patients (PSA)https://clinicaltrials.gov/ct2/show/NCT02058680 [Google Scholar]
- 131.Daniels G.A., McKinney M., Ongkeko W., Wang-Rodriguez J., Sakamoto K., Elliott R.L., Head J.F. A phase 1 clinical trial of a PSA/IL-2/GM-CSF containing prostate cancer vaccine in PSA defined biochemical recurrent prostate cancer patients. J. Clin. Oncol. 2016;34(15_suppl) e14584-e14584. [Google Scholar]
- 132.Gulley L., James, Kantoff P., Randomized A. 2011. Double-blind, Phase 3 Efficacy Trial of PROSTVAC-V/F +/- GM-CSF in Men With Asymptomatic or Minimally Symptomatic Metastatic Castrate-Resistant Prostate Cancer (Prospect)https://clinicaltrials.gov/ct2/show/NCT01322490 [Google Scholar]
- 133.Gulley J.L., Borre M., Vogelzang N.J., Ng S., Agarwal N., Parker C.C., Pook D.W., Rathenborg P., Flaig T.W., Carles J., Saad F., Shore N.D., Chen L., Heery C.R., Gerritsen W.R., Priou F., Langkilde N.C., Novikov A., Kantoff P.W. Phase III trial of PROSTVAC in asymptomatic or minimally symptomatic metastatic castration-resistant prostate Cancer. J. Clin. Oncol. 2019;37(13):1051–1061. doi: 10.1200/JCO.18.02031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Fong L. 2006. GM-CSF Before Surgery in Treating Patients With Localized Prostate Cancer.https://clinicaltrials.gov/ct2/show/NCT00305669 [Google Scholar]
- 135.Zhao W., Zhao G., Wang B. Revisiting GM-CSF as an adjuvant for therapeutic vaccines. Cell. Mol. Immunol. 2018;15(2):187–189. doi: 10.1038/cmi.2017.105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Serafini P., Carbley R., Noonan K.A., Tan G., Bronte V., Borrello I. High-dose granulocyte-macrophage colony-stimulating factor-producing vaccines impair the immune response through the recruitment of myeloid suppressor cells. Cancer Res. 2004;64(17):6337–6343. doi: 10.1158/0008-5472.CAN-04-0757. [DOI] [PubMed] [Google Scholar]
- 137.Butterfield L.H., Zhao F., Lee S., Tarhini A.A., Margolin K.A., White R.L., Atkins M.B., Cohen G.I., Whiteside T.L., Kirkwood J.M., Lawson D.H. Immune correlates of GM-CSF and melanoma peptide vaccination in a randomized trial for the adjuvant therapy of resected high-risk melanoma (E4697) Clin. Cancer Res. 2017;23(17):5034–5043. doi: 10.1158/1078-0432.CCR-16-3016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Brekke K., Sommerfelt M., Okvist M., Dyrhol-Riise A.M., Kvale D. The therapeutic HIV Env C5/gp41 vaccine candidate Vacc-C5 induces specific T cell regulation in a phase I/II clinical study. BMC Infect. Dis. 2017;17(1):228. doi: 10.1186/s12879-017-2316-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Wendel-Hansen V. 2012. Immunotherapy with Vacc-C5 with Adjuvant GM-CSF or Alhydrogel in HIV-1-infected Subjects on ART.https://clinicaltrials.gov/ct2/show/NCT01627678 [Google Scholar]
- 140.Dillman O. 2020. Robert, Phase Ib-II Trial of Dendritic Cell Vaccine to Prevent COVID-19 in Adults.https://clinicaltrials.gov/ct2/show/NCT04386252 [Google Scholar]
- 141.Halstead E.S. 2019. Inhaled GM-CSF for Respiratory Virus-Associated Severe Pneumonia (iGRASP)https://clinicaltrials.gov/ct2/show/NCT02601365 [Google Scholar]
- 142.Herold S., Hoegner K., Vadasz I., Gessler T., Wilhelm J., Mayer K., Morty R.E., Walmrath H.D., Seeger W., Lohmeyer J. Inhaled granulocyte/macrophage colony-stimulating factor as treatment of pneumonia-associated acute respiratory distress syndrome. Am. J. Respir. Crit. Care Med. 2014;189(5):609–611. doi: 10.1164/rccm.201311-2041LE. [DOI] [PubMed] [Google Scholar]
- 143.Lyon H.Cd. GRID; 2015. GM-CSF to Decrease ICU Acquired Infections.https://clinicaltrials.gov/ct2/show/NCT02361528 [Google Scholar]
- 144.Hall M.W., Geyer S.M., Guo C.Y., Panoskaltsis-Mortari A., Jouvet P., Ferdinands J., Shay D.K., Nateri J., Greathouse K., Sullivan R., Tran T., Keisling S., Randolph A.G., I. Pediatric Acute Lung, P.S.I. Sepsis Investigators Network Innate immune function and mortality in critically ill children with influenza: a multicenter study. Crit. Care Med. 2013;41(1):224–236. doi: 10.1097/CCM.0b013e318267633c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Hall M.W. GRACE; 2018. GM-CSF for Reversal of immunopAralysis in pediatriC sEpsis-induced MODS Study.https://clinicaltrials.gov/ct2/show/NCT03769844 [Google Scholar]