Abstract
Many parents who interact with the child welfare system present with substance use issues, which means their children are at risk for prenatal exposure to alcohol and other drugs. Because child welfare agencies play an important role in identifying and providing services to mitigate negative impacts of prenatal exposures, we conducted a search for literature addressing child welfare information sources, policies, and practices related to this population. The search yielded 16 research/evaluation and 16 policy/practice papers, with most addressing exposures to both alcohol and other drugs. The literature most commonly reports that children identified as exposed are referred to child protection agencies during the newborn period. This practice may lead to underidentification, especially of children with prenatal exposure to alcohol. Research suggests that this population is at risk for poorer child welfare outcomes and that there are specific service needs for these children. This review indicates that there is an overall lack of research literature regarding identification of prenatally exposed children involved in the child welfare system that could best inform child welfare policies and practices. Studies investigating how the child welfare system identifies and cares for children with prenatal exposures are needed.
Keywords: Child welfare, child maltreatment, prenatal alcohol exposure, prenatal substance exposure, FASD
Introduction
Alcohol and other drugs are known teratogens resulting in adverse birth outcomes as well as potential lifelong neurodevelopmental impairments (O’Rahilly & Müller, 2001; Preece & Riley, 2011). Newborns exposed to certain drugs in utero, such as opioids, cocaine, or stimulants, often experience visible signs of withdrawal from these substances at birth, known as neonatal abstinence syndrome (NAS). In addition, these infants are at increased risk of prematurity, seizures, and stroke (Gray, 2011). Babies born with prenatal exposure to alcohol are often not recognized at birth. They do not show signs of withdrawal, and most do not present with the dysmorphic facial features associated with fetal alcohol syndrome (Streissguth et al., 2004). Yet children prenatally exposed to alcohol carry risks of lifelong conditions with a range of effects on their physical and mental health or cognitive functioning (Turchi & Smith, 2018). A report from the National Academies of Science’s Institute of Medicine stated, “Of all the substances of abuse (including cocaine, heroin, and marijuana), alcohol produces by far the most serious neurobehavioral effects in the fetus.” (Stratton, Howe, & Battaglia, 1996, p. 35). This is important because several studies have indicated drug users are typically polysubstance users, with alcohol and tobacco being the most frequent co-used substances (Esser, Guy, Zhang, & Brewer, 2019; Radel, Baldwin, Crouse, Ghertner, & Waters, 2018). This pattern holds for pregnant women (Jarlenski et al., 2017).
Substance use is an ongoing challenge for child welfare systems. It is estimated that 50% to 80% of cases in the child welfare system involve parental substance use (Osterling & Austin, 2008). A Department of Health and Human Services 2018 report found between the years 2012 and 2016, counties that experienced a 10% increase in drug overdoses or drug-related hospitalizations also experienced nearly a 3% increase in the number of children entering foster care. The report also stated the substance use of the biological parent was associated with a greater likelihood of a child’s removal from the home (Radel et al., 2018).
Since substance use is often a long-term issue, inferring that at least some children served by the child welfare system were prenatally exposed to alcohol, opioids, or other drugs is reasonable. However, there are currently no national data sources that “count” how many are involved in the child welfare system. National datasets, such as the Adoption and Foster Care Analysis and Reporting System (AFCARS), house data that states are required to collect on all children in foster care. The consistency of information varies due to differences in how each state defines types of child abuse, categorizes family characteristics, and dedicates resources to ensure data quality. Even with these limitations, research using multistate and national datasets is useful in gaining a sense of the potential scope of the problem. Using data from the National Survey of Child and Adolescent Welfare (NSCAW), Wulczyn, Michelle, and Fisher (2011) found alcohol or drug use by caregivers was reported by case workers for 61% of referred infants. Analysis of the AFCARS data from 2012 to 2017 showed 44.2% of entries of children under 1 year old to foster care involved caregiver substance use (Meinhofer & Angleró-Díaz, 2019). The number of very young children brought into care due to parental use of substances suggests there is an increased likelihood of mothers using substances during pregnancy, which in turn indicates that children may be at an elevated risk for prenatal exposure.
Neurobehavioral impairments associated with prenatal exposures can make these children difficult to parent, especially for parents with already compromised skills due to addiction (Chasnoff, Telford, Wells, & King, 2015a). NAS symptoms of excessive crying, sleep problems, and an inability to be soothed can be frustrating to new parents. Research has shown preschool or school-aged children with prenatal exposures often have poor attention skills, impulse control, and behavior regulation (Coles et al., 1997). These behavioral impairments can interact with learning and memory, including forgetting previously learned material, difficulty understanding cause-and-effect, and an inability to learn from one’s own experiences (Bertrand & Dang, 2012; Henry, Sloane, & Black-Pond, 2007). However, the majority of children with prenatal alcohol exposure will score within normal range on standardized tests of neurodevelopment (e.g., IQ, language acquisition, motor skills), making the impairments “hidden” to parents, teachers, and case workers. This creates a situation in which behaviors and deficits can be misinterpreted as misbehavior, disobedience, or even a behavioral disorder.
There are interventions to reduce the harmful neurocognitive impacts of prenatal exposures on children, and help caregivers effectively parent children (Bertrand, 2009; Jirikowic, Gelo, & Astley, 2010; Petrenko, 2015). When entering the child welfare system, if children are recognized to be at risk for prenatal exposures, the agency’s assessment of a child’s needs and referrals to services can promote the child’s health, development, and long-term well-being. Given the potential lifelong impact of exposures on children, it is important to understand the available literature on how child welfare agencies manage cases in which the child could have been prenatally exposed to drugs and alcohol. Unfortunately, there is not a clear understanding of the information sources, policies, and practices child welfare agencies and case workers use to address appropriate prenatal substance exposure screening and referral. A structured search and review were conducted to describe the available peer-reviewed literature concerning children with prenatal exposure to alcohol and other drugs in the care of the U.S. child welfare system. The purpose of this review was to: (1) understand what the published literature reveals about information sources, policies, and practices used to identify and care for children served by the child welfare system who are prenatally exposed (to different substances and across the age span), and (2) examine the strengths and gaps of the literature in these areas and identify needs for future research to better understand child welfare practices and policies regarding this vulnerable population.
Methods
Search methods followed the structure outlined in the Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols Structure (PRISMA-P) (Shamseer et al., 2015). Care of a child in the U.S. child welfare system was defined to include a child reported for suspected child abuse and neglect, currently or with a history of receiving services from child welfare (e.g., in-home services, foster care, kinship care), and/or being adopted from the public child welfare system. Prenatal substance exposure included maternal use of illicit substances and alcohol.
The literature search was conducted in May 2018. To capture recent policies and practices in the context of the U.S. child welfare system, articles were limited to those published from 2006 to 2018 and excluded if not written in English. To capture information and perspectives from policymakers and practitioners, we sought both research and nonresearch articles. Because the child welfare system involves not only public child welfare agencies but also other important stakeholders such as family dependency courts and child and family service providers, the search was conducted in ERIC, Medline, PsychInfo, and SocIndex databases. It incorporated multiple terms used by a wide variety of disciplines. Search terms and expression structure are presented in Table A1 of the Appendix.
The search identified 50 articles. The full text of each paper was reviewed to determine if inclusion criteria were met: (1) addressed the U.S. child welfare system and/or a population of children currently or previously under legal guardianship of the system and (2) addressed children with prenatal substance exposure. Eighteen did not meet inclusion criteria, yielding a final sample of 32 articles (see Figure 1).
Figure 1.
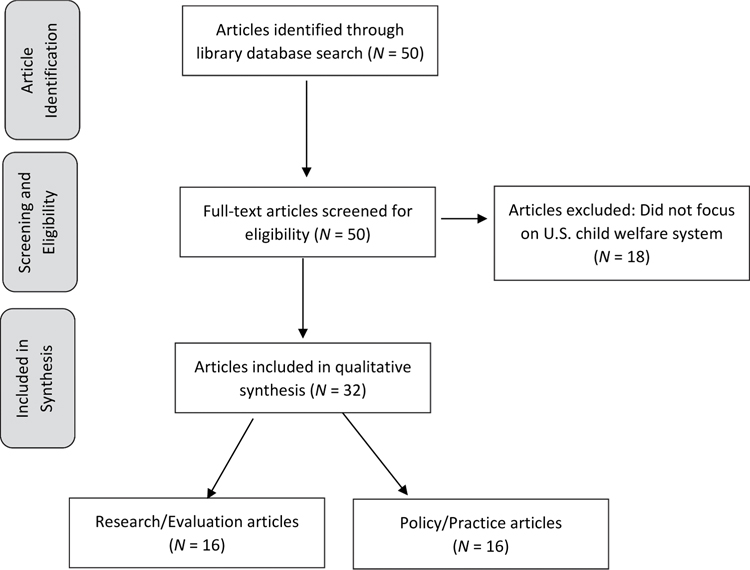
Identification and screening of articles.
The analysis consisted of abstracting information describing characteristics of children (substances exposed to, age) and information sources used by research studies to identify children with prenatal exposures. Analysis of child welfare policies and practices began by examining the broad focus of articles. Articles were categorized by primary tasks of child welfare agencies: (1) responses to reports of child abuse and neglect, (2) assessments of child needs and referrals, and (3) providing safe temporary and permanent homes for children. Not all articles addressed these primary tasks, which led to the emergence of two additional categories. These included articles that did not address typical child welfare practices, but rather described service improvement efforts such as model programs serving limited populations, and manuscripts that addressed broader systemic issues, such as recommendations related to national data collection efforts.
Results
Types of articles
Sixteen of the 32 articles described findings investigating populations of children with prenatal substance exposure and their interactions with the child welfare system. These comprised research studies (N = 12) and results of program evaluations (N = 4). The remaining 16 articles included structured reviews of policies, instruments, and evidence-based practices, as well as recommendations to improve policies, practices, and services for children with prenatal substance exposure and their families.
Scope of literature and information sources regarding children identified as prenatally exposed
Type of substance
Table 1 describes the distribution of articles by substances addressed and by age of child. Research/evaluation studies were more likely than policy/practice articles to address both drugs and alcohol exposure. Policy/practice materials were similarly proportionate in focusing on exposure to drugs only, alcohol only, and both drugs and alcohol. Research/evaluation articles referring to specific drugs most often included opioids and cocaine, while policy/practice articles were more likely to address drugs in general..
Table 1.
Types of prenatal substance exposures and ages of children addressed in a structured review of articles, U.S., 2006–2018.
| Types of articles | Research/Evaluation studiesa N=16(%) |
Policy/Practiceb N=16(%) |
Total number of articles N=32(%) |
|---|---|---|---|
| Types of substances | |||
| Drugs-only | 3 (19) | 4 (25) | 7 (22) |
| Alcohol-only | 1 (6) | 6 (38) | 7 (22) |
| Both drugs and alcohol | 12 (75) | 6 (38) | 18 (56) |
| Specific drugs addressedc | |||
| Cannabis | 4 (27) | 0 (0) | 4 (16) |
| Cocaine | 8 (53) | 1 (10) | 9 (36) |
| Methamphetamines | 4 (27) | 0 (0) | 4 (16) |
| Opioids | 9 (60) | 3 (30) | 12 (48) |
| Drugs not specified | 5 (33) | 6 (60) | 11 (44) |
| Ages of childrend | |||
| Newborns/< 1 yeare | 11 (69) | 5 (31) | 16 (50) |
| Infants and toddlers | – | 3 (19) | 3 (9) |
| 3–6 years | 1 (6) | – | 1 (3) |
| 4–18 years | 2 (13) | – | 2 (6) |
| >15 years | 1 (6) | – | 1 (3) |
| 0–18 | 1 (6) | 8 (50) | 9 (28) |
Original research (n = 12) and program evaluations (n = 4)
Structured reviews (e.g., policies, validated instruments), program model descriptions without evaluation results, or informational summaries for practitioners/policy makers
Specific drugs reported in 15 research and 10 policy/practice articles; articles could address more than one type of drug)
Age of population at beginning of study
Most often neonates, one study focused on infants less than 1 year of age
The 16 research/evaluation articles included three large-scale studies in one state (Prindle, Hammond, & Putnam-Hornstein, 2018; Putnam-Hornstein, Prindle, & Leventhal, 2016) and a single county (Roberts & Nuru-Jeter, 2012) that investigated factors, including type of substance associated with whether newborns were reported to child welfare. Sun, Freese, and Fitzgerald (2007) explored whether the type of exposure was associated with case substantiation and future maltreatment. Another study examined the relationship between prenatal drug and alcohol exposures, child maltreatment, and foster care transitions (Smith, Johnson, Pears, Fisher, & DeGarmo, 2007). Several studies addressed the impact of treatment services for maternal substance use on later interactions with child welfare (Huang & Ryan, 2011; McCann et al., 2010; Ryan, Choi, Hong, Hernandez, & Larrison, 2008; Twomey, Caldwell, Soave, Fontaine, & Lester, 2010). Other research compared service delivery to children exposed to drugs and alcohol in rural and urban locations (Chasnoff et al., 2015a) and mental health, behavioral and educational outcomes of adopted children (Crea, Guo, Barth, & Brooks, 2008; Harwood, Feng, & Yu, 2013). Reports to child welfare of prenatal exposure to opioids and alcohol were described over time (Lynch, Sherman, Snyder, & Mattson, 2018). Studies focused on drugs-only included exposure to cocaine (Doris, Meguid, Thomas, Blatt, & Eckenrode, 2006), opioids (França, Mustafa, & McManus, 2016), and drugs in general, excluding alcohol (Crea et al., 2008). Only one study focused on alcohol-only exposure (Chasnoff, Wells, & King, 2015b).
Of the 16 policy/practice articles, three focused on opioids only (Knopf, 2015; Mirick & Steenrod, 2016; Schiff & Patrick, 2017) and one addressed cocaine only (Katz, Ceballos, Scott, & Wurm, 2007). Six policy/practice articles addressed alcohol only: three described speech and language services tailored to the needs of children in child welfare (Hyter, 2007; Hyter & Way, 2007; Rogers-Adkinson & Stuart, 2007); two addressed dependency court models to increase access and coordination of services to children (Burd, Cohen, Rizwan, & Norris, 2011; Paley & Auerbach, 2010); and one reviewed the variability of policies across states related to alcohol use during pregnancy (Drabble, Thomas, O’Connor, & Roberts, 2014). Six policy/practice articles addressed both drugs and alcohol. These included treatment strategies for families impacted by prenatal exposure (Burry & Wright, 2006; Leve et al., 2012). Others described methods and limitations in identifying newborns (Anthony, Austin, & Cormier, 2010; Drescher Burke, 2007), the need for data systems (Young & Collins, 2015), and policies and practices to better understand the prevalence of prenatal substance exposure in child welfare (Young, Boles, & Otero, 2007).
Age of child
The age range of children addressed by articles is described in Table 1. Of the 16 research/evaluation articles, 11 examined newborn populations. These articles described the number of reports to child protection over time (França et al., 2016; Lynch et al., 2018), factors associated with whether reports were made (Prindle et al., 2018; Putnam-Hornstein et al., 2016; Roberts & Nuru-Jeter, 2012), whether these reports resulted in a substantiated case, subsequent maltreatment (Sun et al., 2007) as well as foster care placement (Doris et al., 2006). Program evaluations assessed whether enhanced treatment services for mothers, who were reported to child welfare, reduced the number of newborns prenatally exposed to substances (Ryan et al., 2008) and influenced child permanency outcomes (Huang & Ryan, 2011; McCann et al., 2010; Twomey et al., 2010). Research with children aged 3–6 years examined the effects of exposure on child maltreatment and placement transitions (Smith et al., 2007). Studies including older children investigated the relationship of exposure to child well-being, including educational and mental/behavioral health outcomes (Chasnoff et al., 2015a; Crea et al., 2008; Harwood et al., 2013) and changes in service recommendations for children after diagnosis of a fetal alcohol spectrum disorder (FASD) (Chasnoff et al., 2015b).
Policy/practice articles focused on newborns addressed the effects of policies around substance use during pregnancy (Drabble et al., 2014; Roberts & Nuru-Jeter, 2012; Schiff & Patrick, 2017) and training of child welfare staff to better understand medication-assisted treatment for pregnant women (Knopf, 2015). Recommendations were made to support more consistent identification of maternal substance use during pregnancy (Anthony et al., 2010) and to identify exposed newborns (Drescher Burke, 2007). For infants and toddlers, strategies to support visitation between birth parents and children (Burry & Wright, 2006) and court program models (Burd et al., 2011; Katz et al., 2007; Paley & Auerbach, 2010) were described. Policy/practice articles tended to address a wider age range (Hyter, 2007; Hyter & Way, 2007; Rogers-Adkinson & Stuart, 2007). Two articles focused on families providing care to children with prenatal substance exposure, including strategies to strengthen child-caregiver attachment (Mirick & Steenrod, 2016) and a review of evidence-based practices for potential use with families caring for foster children, including children with prenatal substance exposure (Leve et al., 2012). To increase the understanding of prevalence and response to children prenatally exposed, two articles recommended policies to integrate substance use service providers and child welfare data systems (Young et al., 2007; Young & Collins, 2015).
Information sources used by studies to identify children with prenatal exposures
Table 2 describes information sources used by studies to address children with prenatal exposures by age. Child welfare administrative data which recorded reports to child protective services were most commonly used to identify newborns with prenatal exposure to substances (Huang & Ryan, 2011; Lynch et al., 2018; McCann et al., 2010; Roberts & Nuru-Jeter, 2012; Ryan et al., 2008; Sun et al., 2007; Twomey et al., 2010). Hospital birth discharge records reporting medical diagnoses were used by several studies (França et al., 2016; Prindle et al., 2018; Putnam-Hornstein et al., 2016). One study used newborn toxicology screening results, supplemented with review of maternal obstetrical records (Doris et al., 2006). To identify children beyond the newborn period, studies used reviews of multiple records, including child welfare, court, and adoptive history case files (Chasnoff et al., 2015a, 2015b). Two studies used parental reports of prenatal substance exposure of their adopted children (Crea et al., 2008; Harwood et al., 2013). Hospital data may fail to identify newborns with prenatal exposures due to inconsistent medical practice, limitations of toxicology testing, and failure to test newborns without recognizable symptoms (Drescher Burke, 2007). To address this limitation, two studies used hospital administrative data that included both maternal substance use disorder diagnoses and prenatal substance exposure diagnoses to identify affected newborns (Prindle et al., 2018; Putnam-Hornstein et al., 2016).
Table 2.
Information sources used by studies to identify children with prenatal substance exposures by age, structured review of articles, U.S., 2006–2018.
| Ages of children | Information sources used to identify prenatal substance exposurea | Number of studies |
|---|---|---|
| Newborns/< 1 year(N = 11) | Child welfare data: Allegations of newborns with prenatal substance exposure reported to child protective services | 7 |
| Hospital administrative data: ICD-9 diagnostic codes reported at birth | 3 | |
| Positive newborn toxicology screen, review of medical charts | 1 | |
| 3–6 years (N = 1) | Review of child welfare case records | 1 |
| 4–18 years (N = 2) | Review of child’s birth: medical, child welfare, court, and/or adoption records | 2 |
| > 15 years (N = 1) | Adoptive parent report | 1 |
| 0–18 years (N = 1) | Adoptive parent report | 1 |
Information sources listed are those used to identify prenatally exposed children. Other data sources were used to investigate variables of interest, such as child welfare data to determine child outcomes.
Estimating the prevalence of prenatal substance exposures was not the purpose of this review. If it were, estimates of prevalence based on reported research would be unreliable given the small number of studies, data source limitations, and study samples that are not representative of the broader population of children served by child welfare agencies. However, to explore differences in the reported number of children prenatally exposed to alcohol, the review examined study data sources used to identify child populations. The subset of four articles focusing on children with exposure to alcohol was examined for methodology (Table 3). These studies varied in research questions, methods, and study samples. It is important to note that determining prevalence was not intended by these studies and should not be interpreted as estimates of the prevalence of prenatal alcohol exposure in the child welfare population. When information on substance use during pregnancy was obtained from the maternal medical record, each demonstrated the tendency toward markedly higher percentage of children identified as prenatally exposed to alcohol.
Table 3.
Manuscripts reporting data sources identifying prenatal exposure to alcohol, structured review of articles, U.S., 2006–2018.
| Sample size | Data sources used to identify child’s prenatal exposure to alcohol | Percentage identifieda | |
|---|---|---|---|
| Newborns reported to child protection for prenatal substance exposure (Sun et al., 2007) | 457 | Reports to child protection for prenatal exposure confirmed by positive toxicology | 0.4 |
| Children aged 3–6 transitioning to a new foster care placement (Smith et al., 2007) | 117 | Review of caseworker reports based on available information (e.g., report of family members, psychological evaluations, court reports) | 15 |
| Children currently or formerly in foster care referred to clinic for behavioral issues (Chasnoff et al., 2015b) | 547 | Review of child’s birth, medical, child welfare, and/or court records to determine prenatal alcohol exposure; pediatric, neurologic, and dysmorphology examination of child to diagnose FASD | 28.5 |
| Children aged newborn to 3 years in foster care whose mothers were suspected of using cocaine during pregnancy (Doris et al., 2006) | 146 | Review of maternal medical records documenting use of alcohol during pregnancy | 32 |
Refers to percentage of children identified with prenatal exposure to alcohol and other drugs for each article.
Research by Doris et al. (2006) is particularly illustrative of the added value of obtaining maternal medical records. To compare child welfare outcomes of infants born to mothers suspected of cocaine use, the study identified 100 newborns who tested positive for cocaine at birth with the intention of comparing them to a control group of 100 newborns who tested negative for cocaine. However, after reviewing maternal medical records, information on maternal self-reports and/or test results indicated almost one quarter of the newborns assigned to the cocaine-negative control group had likely been exposed to cocaine during pregnancy. This compelled researchers to remove 24 newborns from the study and reduced the control group from 100 to 76. The review of medical records also found many mothers reported use of alcohol in both groups, including 53 (70%) of infants in the cocaine-positive group and 21 (28%) of infants in the cocaine-negative group (Doris et al., 2006).
Child welfare policies and practices
Table 4 categorizes the broad focus of articles in relation to child welfare policies and practices. Eight articles addressed child welfare responses to children identified as newborns. This included six studies of child and family characteristics associated with reports to child protection and later child welfare interactions (Doris et al., 2006; Lynch et al., 2018; Prindle et al., 2018; Putnam-Hornstein et al., 2016; Roberts & Nuru-Jeter, 2012; Smith et al., 2007) and two articles on hospital and agency policies related to reporting newborns to child protection (Drescher Burke, 2007; Sun et al., 2007). The only study that reported outcomes in relation to child welfare practices was Sun et al. (2007), who studied whether focused training on substance use and effects of prenatal exposure was associated with different responses to reports of prenatally exposed newborns.
Table 4.
Child welfare system policies and practices addressed in manuscripts, structured review of articles, U.S., 2006–2018.
| Policy and practices | Article focus | Number of articles |
|---|---|---|
| Respond to reports of child abuse and neglect | Research on child and family factors associated with reports to child protection, investigations of maltreatment, and child placement in foster care | 6 |
| Hospital and agency policies and practices in response to reports of prenatally exposed newborns | 2 | |
| Assess child and family needs and refer to appropriate services | Studies of service needs and characteristics of children with co-occurring disorders | 2 |
| Recommendations of standardized screens to collect information on maternal use of substances during pregnancy | 1 | |
| Provide safe temporary care and permanent home for the child | Visitation practices with birth families who have children affected by prenatal substance exposure | 1 |
| Recommendations of evidence-based practices that could be used to support foster families caring for children | 1 | |
| Studies of factors associated with child’s post-adoption outcomes: health, educational, and mental health | 2 | |
| Efforts to improve service delivery | Descriptions of model court programs focused on identifying children and referring children and families to services | 2 |
| Descriptions of model programs intended to enhance substance use treatment to parents and services for children | 5 | |
| Recommendations to improve speech and language therapist’s practice by considering the child’s history of maltreatment and prenatal substance exposure | 3 | |
| System-wide policy and practices | Policy recommendations to effectively address prenatal substance exposure by reducing punitive responses and increasing resources | 3 |
| Policy recommendations to support data collection and reporting across child welfare and substance abuse treatment systems | 2 | |
| Child welfare staff knowledge and training needs to respond to families and children affected by prenatal exposure to substances | 2 |
Three articles addressed family assessment and service referrals. These included recommendations to assess maternal use of substances during pregnancy using validated instruments (Anthony et al., 2010), research on the relationship between an accurate FASDs diagnosis and child referrals to services (Chasnoff et al., 2015b) and a study of factors that may increase the likelihood of children needing services to address mental health needs (Chasnoff et al., 2015a). There were no studies or descriptions of assessment and referral processes used by child welfare agencies.
Providing safe temporary and permanent care of children was addressed in four articles. Visitation strategies that could be used by caseworkers to help birth parents recognize and respond to the needs of affected infants were described (Burry & Wright, 2006), and research-based interventions that could be used to help foster families parent affected children were suggested (Leve et al., 2012). Two studies examined factors related to long-term outcomes of adopted children (Crea et al., 2008; Harwood et al., 2013). There were no studies or descriptions of child welfare agency practices used to support foster families caring for affected children.
Ten articles focused on enhancing service delivery; seven were descriptions of efforts to improve service delivery beyond typical practices, including five programs designed to increase parent access to substance use services (Huang & Ryan, 2011; Katz et al., 2007; McCann et al., 2010; Ryan et al., 2008; Twomey et al., 2010). Two model dependency court programs were described that promoted screening practices and processes to recognize children who could be affected by prenatal exposure but were not identified at birth (Burd et al., 2011; Paley & Auerbach, 2010). Three articles promoted awareness and understanding of the combined effect of prenatal exposures and child maltreatment to speech and language service providers (Hyter, 2007; Hyter & Way, 2007; Rogers-Adkinson & Stuart, 2007). There was no information on the service referrals that might be typically received by children with exposures.
Articles addressing systemic issues included recommendations to improve state policies to reduce stigma and improve access to substance use treatment (Drabble et al., 2014; França et al., 2016; Schiff & Patrick, 2017), address isolated and inadequate data systems (Young et al., 2007; Young & Collins, 2015) and increase practitioner understanding of treatment of opioid use (Knopf, 2015) and the impact of opioid use on parenting (Mirick & Steenrod, 2016). No literature addressing child welfare staff training or understanding of prenatal exposures was found.
Discussion
This structured review provides insight into the scope and types of literature that explore identification of children with prenatal substance exposure and suggests areas of future study that could provide the basis for developing child welfare policies and/or practices regarding these children. Over a 22 year period, the review yielded only 32 peer-reviewed articles that directly addressed these issues. Articles were split evenly between research and nonresearch. Most research studies (75%) addressed both alcohol and drugs. Half focused on newborns and children under 1 year of age, and most concentrated on hospital reports of newborns with prenatal substance exposure. In relation to child welfare activities, there was an emphasis on responses by agencies to reports of newborns. Finally, the review found little research on child welfare policies and/or practices in identifying or caring for these children, including documenting and sharing information among service providers.
Identifying and responding to children with prenatal exposure to substances, including alcohol
The lack of hospital reports to child welfare agencies of newborns prenatally exposed to substances and the rise in use of opioids led to revisions of the Child Abuse Prevention and Treatment Act (CAPTA) and Comprehensive Addiction Recovery Act (CARA). This legislation promotes consistent hospital reports to child welfare and the development of plans to refer families to services. However, the literature on implementation of CAPTA/CARA is small and somewhat narrow in focus. The concentration on newborns in research articles reflects data sources that rely predominantly on hospital reports of prenatally exposed infants (under CAPTA/CARA) and hospital administrative data of birth and delivery records. However, most children with prenatal alcohol exposure will not be identified in this period (Gray, 2011). The limitations of hospital data may carry over to child welfare administrative data which relies on hospital reports to identify children with prenatal exposures.
Identifying children affected by alcohol exposure typically occurs after the newborn period and relies on sources other than toxicology tests, including maternal history of alcohol use during pregnancy (Chasnoff et al., 2015a, 2015b). With a primary focus on only the youngest children and a few/single referral sources, there are likely large numbers who were prenatally exposed to alcohol and in contact with child welfare, but not identified by case workers. This is observed by Chasnoff et al. (2015b), who reported that over 80% of children with FASDs in a child welfare sample were not diagnosed or not appropriately diagnosed. This underidentification results in 1) children and families who do not receive much needed services and 2) an increased risk of child maltreatment due to poor parental coping skills combined with difficult child behaviors stemming from the prenatal brain damage.
Yet, even when children are known to be prenatally exposed to alcohol, child welfare systems may not respond as vigorously as compared to their response to infants’ exposure to drugs. Putnam-Hornstein et al. (2016) found infants were reported to child protective services less often when diagnosed with alcohol exposure and most often with exposure to cocaine. Paley and Auerbach (2010) suggested lack of staff knowledge of the importance of FASDs interfered with early child identification and services. The inequity of response to alcohol exposure versus that to other substances needs to be addressed. Smith et al. (2007) reported prenatal alcohol exposure predicted later child maltreatment, and Chasnoff et al. (2015a) found evidence that children with FASDs in child welfare programs in rural areas are at higher risk for co-occurring mental health diagnoses. Early identification of prenatal alcohol exposure appropriately connects children with services that will promote development and mitigate the negative impact of FASDs on their functioning.
The inability to accurately assess prevalence is a significant gap in information. Estimates of the prevalence of prenatal exposures in the child welfare population in the United States are limited by inconsistent state data collection and the inability to integrate substance use treatment data systems and child welfare data systems (Young et al., 2007). International research and studies of children receiving diagnostic services suggest that there may be a large population of children in child welfare who are affected. A recent international meta-analysis on the pooled prevalence of FAS and FASD among children in out-of-home care was estimated to be 14% (Popova, Lange, Shield, Burd, & Rehm, 2019). A study of 547 children cared for by foster or adoptive parents referred to a clinic in Illinois for behavioral assessments found 28.5% met criteria for diagnosis of FASDs (Chasnoff et al., 2015b). These numbers hint at the potential scope of the issue, yet the absence of national prevalence data may conceal the magnitude of the problem, and hinder state and agency planning for resource needs.
Ongoing monitoring and public health surveillance through national databases such as AFCARS or National Child Abuse and Neglect Data System (NCANDS) provide a platform for research to begin identifying family risk factors, developing case profiles, and assessing effectiveness of programs. Currently AFCARS only documents whether parental (not specified to mother or father) alcohol/drug abuse and/or youth alcohol/drug abuse were reasons for removal. In 2018, NCANDS added two data elements based on the requirements of CAPTA/CARA: (1) whether the referred child was affected by substance use, withdrawal symptoms, or FASDs; and (2) whether the infant and the caregiver were referred to appropriate services. Future research will reveal the adequacy of these new NCANDS data elements. However, it is important to note that unless improvements are made by the child welfare system to identify older children, prevalence data may inaccurately estimate the number of children affected.
Importance of understanding child welfare practice and policies
Federal legislation outlines the primary responsibilities of the public child welfare system which are to protect children, provide children with permanent homes, and promote their well-being (Adoption and Safe Families Act, 1997). The scarce information on typical child welfare practices is notable, because there is evidence that prenatal exposures reduce the likelihood of ensuring positive outcomes for children.
Prenatal substance exposure may be associated with poorer outcomes for children who have experienced or are at risk of abuse. They may be at increased risk for maltreatment (Ammerman, 1991) and may be more likely to enter the child welfare system (Doris et al., 2006). Once children enter, they may be at higher risk for placement instability (Smith et al., 2007). The harm that placement instability causes to a child’s health and development has been confirmed through research (Harden, 2004), and the importance of the issue is reflected by efforts to improve stable placements in federal legislation, such as the Family First Prevention Services Act (FFPSA) of 2018. Behavioral issues are commonly present in children who were prenatally exposed (Jaudes & Mackey-Bilaver, 2008), which may be a factor underlying research suggesting a greater number of placement transitions for these children (Bada et al., 2008; Smith et al., 2007). Unstable temporary placements, in turn, can decrease a child’s functioning and communication abilities and increase externalizing behavioral issues (Bada et al., 2008). Once children are placed in permanent homes, they may continue to be at risk for poorer post-adoption adjustment (Crea et al., 2008; Goldman & Ryan, 2011; Harwood et al., 2013).
Identifying children who have been affected is a necessary step to ensure that service referrals will adequately address children’s needs. Systematic practices to identify children who may be affected are recommended (Burd et al., 2011; Paley & Auerbach, 2010). Because identifying children affected by alcohol exposure relies on sources other than toxicology tests at birth, routine collection of information on maternal substance use during pregnancy is necessary (Anthony et al., 2010). To provide service referrals for children caseworkers collect, document, and review information on the child from multiple sources, such as caregivers, schools, and a broad array of service providers. Education on the subtle effects of prenatal exposure, which may not emerge until later in development, could increase staff’s ability to notice indicators that suggest a child may be affected. Yet, the absence of information on typical child welfare agency policies and caseworker practices prevents understanding of if and how children are identified, particularly those who are not identified as newborns.
To mitigate the impact on children with prenatal exposure, studies recommend services that address both issues related to maltreatment and the child’s history of prenatal exposures (Chasnoff et al., 2015a, 2015b; Crea et al., 2008; Harwood et al., 2013) and recommend practices in relations to birth, foster and adoptive families that could promote stable and permanent homes for children (Burry &Wright, 2006; Leve et al., 2012; Mirick & Steenrod, 2016). Yet, information on child welfare policies and practices that facilitate referrals to services, and research on whether improved practices and support for caregivers enhance child outcomes, is missing.
Collaboration and communication between child welfare service providers are likely necessary to identify and care for children. Information needed to help determine a child’s history of prenatal exposure may be spread across systems (Smith et al., 2007). Professionals, such as substance use treatment providers, may obtain information on maternal history of drug and alcohol use during pregnancy. Schools and caregivers may report academic issues or child behaviors that suggest a child may be affected. Young et al. (2007) suggested that data access and sharing between child welfare and substance use treatment service systems would improve identifying and enhance service delivery to prenatally exposed children. Articles on the usefulness of documentation policies that facilitate easy access and sharing of information across professionals are lacking and would be a contribution to the literature.
Limitations
As with most literature searches and syntheses, this structured review has important limitations. The keywords used to conduct the search were limited to those most directly linked to the topic, which could have missed relevant articles. Inclusion and exclusion criteria reduced the pool of articles examined. A search on related topics, such as research on families with substance use disorders in child welfare, was also not included. Without these restrictions, the search would have likely resulted in a large number of false positive “hits,” yet these limitations may have also led to missed articles addressing one or more topics. Finally, this review was only of existing literature and did not directly obtain data from child welfare agencies and professionals regarding their knowledge, practice, policies, or needs regarding children with prenatal exposure to alcohol and/or other drugs.
To address this last limitation, as well as the general lack of existing literature, a research study to better understand current policies and practices in child welfare agencies related to the identification and care of children with prenatal substance exposure is currently underway. The study, conducted in five states, includes (1) review of state and agency policy and practice guideline documents, (2) interviews with state child welfare directors, and (3) survey and interviews with local child welfare staff (e.g., case workers, clinical staff, administrative staff, data managers). In addition, case records from two states will be reviewed for documentation of prenatal exposure to alcohol and other drugs, and focus groups will be conducted with foster and adoptive caregivers. This study will build upon information from this structured literature review to learn about current promising practices, challenges, and ideas about potential future practices. Educational, support, and resource needs of child welfare professionals will also be identified.
Conclusion
This structured review of the literature on children with prenatal exposure to alcohol and other drugs in the child welfare system offers important information for the field and researchers to consider in future work. A strength of the literature is that most research studies addressed prenatal alcohol exposure as well as other drug exposures. Acknowledging the additional harmful effect of alcohol is important for child welfare professionals to take into account because its effect may mimic other drugs, interact with other drugs, or even be more harmful than other drugs as noted by the IOM (Preece & Riley, 2011; Stratton et al., 1996). However, looking at substances addressed in articles may be somewhat misleading with respect to reported numbers of exposure type. Several articles used hospital data and reports at birth to identify children who were prenatally exposed to substances including alcohol; however lack of valid biomarkers most likely leads to few reports of prenatal exposure to alcohol (Drescher Burke, 2007).
Recent federal legislation (Foundations for Evidence-Based Policymaking Act of 2018) has reinforced the need for policies to be supported by research. The field needs to have clear, evidenced-based, guidance, and tools to address the needs of these children and their families. Such guidance should be based on peer-reviewed literature. The lack of information on key child welfare activities that agencies use to identify and care for children, and the absence of research on the relationship between practices and associated child outcomes, is concerning. The adverse impact of prenatal exposure to alcohol and other drugs for children and their families is well established, and children with these exposures often need the services of child welfare agencies. They may be at higher risk of abuse and more likely to be reported to child protection. Once they enter the child welfare system, children may experience more frequent placement transitions, which may exacerbate the effects of prenatal exposures. They continue to be at higher risk for poorer long-term outcomes after exiting the child welfare system. If prenatal exposure is a factor in a family, child welfare agencies cannot rely only on parent treatment and skill building. A history of exposure must be considered and integrated into a child’s care to ensure safety and promote well-being. Yet without vetted literature on practices that may support positive child outcomes, child welfare agencies are left with a “best guess” for policies and guidance – or at worst not addressing this important issue at all.
Funding
This work was supported by the Children’s Bureau, Administration for Children and Families, HHS, under contract HHSP233201500133I, Task Order No. HHSP23337007T, with additional funding provided under an interagency agreement with Centers for Disease Control and Prevention.
Appendix Methods
Literature Eligibility Criteria
The following eligibility criteria were developed to address the objectives of the review. Articles were eligible for consideration if they—
Addressed the U.S. child welfare system, and/or children served by a state/county/tribal child welfare agency
Addressed children at risk for or impacted by prenatal exposure to alcohol/substances, and/or with a diagnosis related to prenatal exposure to alcohol/substances
Were published between 2006 and 2018 (May) and in English
Peer-Reviewed Literature Search
The search for peer-reviewed literature was conducted in May 2018 using ERIC, Medline, PsychInfo, and SocIndex library databases. The search identified 32 published articles that met eligibility criteria.
Search strings were formulated to encompass keywords related to child welfare and prenatal alcohol or substance exposure. The Boolean search string used was— (child welfare OR child protection OR child protective services OR protective services or child abuse OR child abuse and neglect OR child neglect OR child maltreatment OR social work OR foster care OR maltreatment OR out-of-home-care OR kinship care OR kith and kin OR relative placement OR family reunification OR foster home care) AND (prenatal exposure OR prenatal alcohol exposure OR prenatal substance exposure OR substance-exposed infants OR prenatal exposure delayed effects OR fetal alcohol spectrum disorder OR neonatal abstinence syndrome)
Any literature captured in the search had at least one keyword matching a term related to child welfare and at least one term related to prenatal alcohol or substance exposure. Key terms are listed in Table A1.
Abstraction and Summarizing of Material
Information was abstracted and summarized using the following predefined coding schema:
Journal
Audience/system addressed
Type of article
Objective of article
Age of child population
Case process point
-
Child welfare services addressed
Type of substance addressed
Table A1.
Key terms: structured peer-reviewed library database search for articles, U.S., 2006–2018.
| Child welfare system/Children served by child welfare system | Prenatal exposure to alcohol and/or substances | ||
|---|---|---|---|
| Child protection | MeSH terms | Prenatal exposure | MeSH terms |
| Child protective services | Child welfare | Prenatal alcohol exposure | Prenatal exposure delayed effects |
| Protective services | Foster home care | Prenatal substance exposure | Fetal alcohol spectrum disorders |
| Child abuse | Substance exposed infants | Neonatal abstinence syndrome | |
| Child abuse/neglect | |||
| Child neglect | |||
| Child maltreatment | |||
| Foster care | |||
| Social work | |||
| Maltreatment | |||
| Out-of-home care | |||
| Kinship care | |||
| Kith and kin | |||
| Relative placement | |||
| Family reunification | |||
References
- Ammerman RT (1991). The role of the child in physical abuse: A reappraisal. Violence and Victims, 6, 87–101. 10.1891/0886-6708.6.2.87 [DOI] [PubMed] [Google Scholar]
- Anthony EK, Austin MJ, & Cormier DR (2010). Early detection of prenatal substance exposure and the role of child welfare. Children and Youth Services Review, 32(1), 6–12. 10.1016/j.childyouth.2009.06.006 [DOI] [Google Scholar]
- Bada HS, Langer J, Twomey J, Bursi C, Lagasse L, Bauer CR, Shankaran S, Lester BM, Higgins R, & Maza PL (2008). Importance of stability of early living arrangements on behavior outcomes of children with and without prenatal drug exposure. Journal of Developmental and Behavioral Pediatrics: JDBP, 29(3), 173–182. 10.1097/DBP.0b013e3181644a79 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bertrand J (2009). Interventions for children with fetal alcohol spectrum disorders (FASDs): Overview of findings for five innovative research projects. Research in Developmental Disabilities, 30(5), 986–1006. 10.1016/j.ridd.2009.02.003 [DOI] [PubMed] [Google Scholar]
- Bertrand J, & Dang EP (2012). Fetal alcohol spectrum disorders: Review of teratogenicity, diagnosis and treatment issues. In Holar D (Eds.) Handbook of children with special health care needs (pp. 231–258). New York, NY: Springer. [Google Scholar]
- Burd L, Cohen C, Rizwan S, & Norris J (2011). A court team model for young children in foster care: The role of prenatal alcohol exposure and fetal alcohol spectrum disorders. Journal of Psychiatry and Law, 39(1), 179–191. 10.1177/009318531103900107 [DOI] [Google Scholar]
- Burry CL, & Wright L (2006). Facilitating visitation for infants with prenatal substance exposure. Child Welfare, 85(6), 899–918. [PubMed] [Google Scholar]
- Chasnoff IJ, Telford E, Wells AM, & King L (2015a). Mental health disorders among children within child welfare who have prenatal substance exposure: Rural vs. urban populations. Child Welfare, 94(4), 53–70. [PubMed] [Google Scholar]
- Chasnoff IJ, Wells AM, & King L (2015b). Misdiagnosis and missed diagnoses in foster and adopted children with prenatal alcohol exposure. Pediatrics, 135(2), 264–270. 10.1542/peds.2014-2171 [DOI] [PubMed] [Google Scholar]
- Coles CD, Platzman KA, Raskind-Hood CL, Brown RT, Falek A, & Smith IE (1997). A comparison of children affected by prenatal alcohol exposure and attention deficit, hyperactivity disorder. Alcoholism, Clinical and Experimental Research, 21(1), 150–161. 10.1111/j.1530-0277.1997.tb03743.x [DOI] [PubMed] [Google Scholar]
- Crea TM, Guo S, Barth RP, & Brooks D (2008). Behavioral outcomes for substance-exposed adopted children: Fourteen years postadoption. American Journal of Orthopsychiatry, 78(1), 11–19. 10.1037/0002-9432.78.1.11 [DOI] [PubMed] [Google Scholar]
- Doris J, Meguid V, Thomas M, Blatt S, & Eckenrode J (2006). Prenatal cocaine exposure and child welfare outcomes. Child Maltreatment, 11(4), 326–337. 10.1177/1077559506293462 [DOI] [PubMed] [Google Scholar]
- Drabble L, Thomas S, O’Connor L, & Roberts SCM (2014). State responses to alcohol use and pregnancy: Findings from the alcohol policy information system (APIS). Journal of Social Work Practice in the Addictions, 14(2), 191–206. 10.1080/1533256X.2014.900409 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drescher Burke K (2007). Substance-exposed newborns: Hospital and child protection responses. Children and Youth Services Review, 29(12), 1503–1519. 10.1016/j.childyouth.2007.06.007 [DOI] [Google Scholar]
- Esser MB, Guy GP, Zhang K, & Brewer RD (2019). Binge drinking and prescription opioid misuse in the US, 2012–2014. American Journal of Preventative Medicine. 10.1016/j.amepre.s019.02.025 [DOI] [PMC free article] [PubMed]
- França UL, Mustafa S, & McManus ML (2016). The growing burden of neonatal opiate exposure on children and family services in Massachusetts. Child Maltreatment, 21(1), 80–84. 10.1177/1077559515615437 [DOI] [PubMed] [Google Scholar]
- Goldman GDL, & Ryan SD (2011). Direct and modifying influences of selected risk factors on children’s pre-adoption functioning and post-adoption adjustment. Children and Youth Services Review, 33(2), 291–300. 10.1016/j.childyouth.2010.09.012 [DOI] [Google Scholar]
- Gray R (2011). Epidemiology of drug and alcohol use during pregnancy. In Preece PM & Riley EP (Eds.), Alcohol, drugs and medication in pregnancy: The long-term outcome for the child (pp. 11–22). London, England: Mac Keith Press. [Google Scholar]
- Harden BJ (2004). Safety and stability for foster children: A developmental perspective. The Future of Children, 14(1), 31–47. 10.2307/1602753 [DOI] [PubMed] [Google Scholar]
- Harwood R, Feng X, & Yu S (2013). Preadoption adversities and postadoption mediators of mental health and school outcomes among international, foster, and private adoptees in the United States. Journal of Family Psychology: JFP: Journal of the Division of Family Psychology of the American Psychological Association (Division 43), 27(3), 409–420. 10.1037/a0032908 [DOI] [PubMed] [Google Scholar]
- Henry J, Sloane M, & Black-Pond C (2007). Neurobiology and neurodevelopmental impact of childhood traumatic stress and prenatal alcohol exposure differences in the behavioral and emotional impact of prenatal alcohol exposure and postnatal trauma. Language, Speech and Hearing Services in Schools, 38(April), 99–108. 10.1044/0161-1461(2007/010) [DOI] [PubMed] [Google Scholar]
- Huang H, & Ryan JP (2011). Trying to come home: Substance exposed infants, mothers, and family reunification. Children and Youth Services Review, 33(2), 322–329. 10.1016/j.childyouth.2010.09.015 [DOI] [Google Scholar]
- Hyter YD (2007). Prologue: Understanding children who have been affected by maltreatment and prenatal alcohol exposure. Language, Speech, and Hearing Services in Schools, 38 (2), 93–98. 10.1044/0161-1461(2007/009) [DOI] [PubMed] [Google Scholar]
- Hyter YD, & Way I (2007). Epilogue: Understanding children who have been affected by maltreatment and prenatal alcohol exposure: Future directions. Language, Speech, and Hearing Services in Schools, 38(2), 157–159. 10.1044/0161-1461(2007/016) [DOI] [PubMed] [Google Scholar]
- Jarlenski M, Barry CL, Gollust S, Graves AJ, Kennedy-Hendricks A, & Kozhimannil K (2017). Polysubstance use among US women of reproductive age who use opioids for nonmedical reasons. American Journal of Public Health, 107(8), 1308–1310. 10.2105/AJPH.2017.303825 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jaudes PK, & Mackey-Bilaver L (2008). Do chronic conditions increase young children’s risk of being maltreated? Child Abuse and Neglect, 32(7), 671–681. 10.1016/j.chiabu.2007.08.007 [DOI] [PubMed] [Google Scholar]
- Jirikowic T, Gelo J, & Astley S (2010). Children and youth with fetal alcohol spectrum disorders: Summary of intervention recommendations after clinical diagnosis. Intellectual and Developmental Disabilities, 48(5), 330–344. 10.1352/1934-9556-48.5.330 [DOI] [PubMed] [Google Scholar]
- Katz L, Ceballos SG, Scott K, & Wurm G (2007). The critical role of a pediatric nurse practitioner in an early intervention program for children with prenatal drug exposure. Journal for Specialists in Pediatric Nursing, 12(2), 123–127. 10.1111/j.1744-6155.2007.00102.x [DOI] [PubMed] [Google Scholar]
- Knopf A (2015). Addiction counselors train CPS workforce on MAT in conn. The Brown University Child and Adolescent Behavior Letter, 31(12), 4–4. [Google Scholar]
- Leve LD, Harold GT, Chamberlain P, Landsverk JA, Fisher PA, & Vostanis P (2012). Practitioner review: Children in foster care—vulnerabilities and evidence-based interventions that promote resilience processes. Journal of Child Psychology and Psychiatry, and Allied Disciplines, 53(12), 1197–1211. 10.1111/j.1469-7610.2012.02594.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lynch S, Sherman L, Snyder SM, & Mattson M (2018). Trends in infants reported to child welfare with neonatal abstinence syndrome (NAS). Children and Youth Services Review, 86, 135–141. 10.1016/j.childyouth.2018.01.035 [DOI] [Google Scholar]
- McCann KJ, Twomey JE, Caldwell D, Soave R, Fontaine LA, & Lester BM (2010). Services used by perinatal substance-users with child welfare involvement: A descriptive study. Harm Reduction Journal, 7(1), 19. 10.1186/1477-7517-7-19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meinhofer A, & Angleró-Díaz Y (2019). Trends in foster care entry among children removed from their homes because of parental drug use, 2000 to 2017. JAMA Pediatrics, 173(9), 881–883. 10.1001/jamapediatrics.2019.1738 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mirick RG, & Steenrod SA (2016). Opioid use disorder, attachment, and parenting: Key concerns for practitioners. Child and Adolescent Social Work Journal, 33(6), 547–557. 10.1007/s10560-016-0449-1 [DOI] [Google Scholar]
- O’Rahilly R, & Müller F (2001). Human embryology & teratology. New York, NY: John Wiley & Sons. [Google Scholar]
- Osterling KL, & Austin MJ (2008). Substance abuse interventions for parents involved in the child welfare system: Evidence and implications. Journal of Evidence-Based Social Work, 5(1–2), 157–189. 10.1300/J394v05n01_07 [DOI] [PubMed] [Google Scholar]
- Paley B, & Auerbach BE (2010). Children with fetal alcohol spectrum disorders in the dependency court system: Challenges and recommendations. The Journal of Psychiatry & Law, 38(4), 507–558. 10.1177/009318531003800407 [DOI] [Google Scholar]
- Petrenko CL (2015). Positive behavioral interventions and family support for fetal alcohol spectrum disorders. Current Developmental Disorders Reports, 2(3), 199–209. 10.1007/s40474-015-0052-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Popova S, Lange S, Shield K, Burd L, & Rehm J (2019). Prevalence of fetal alcohol spectrum disorder among special subpopulations: A systematic review and meta-analysis. Addiction, 114(7), 1150–1172. 10.1111/add.14598 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preece PM, & Riley EP (Eds.). (2011). Alcohol, drugs and medication in pregnancy: The long term outcome for the child. London, England: Mac Keith Press. [Google Scholar]
- Prindle JJ, Hammond I, & Putnam-Hornstein E (2018). Prenatal substance exposure diagnosed at birth and infant involvement with child protective services. Child Abuse & Neglect, 76, 75–83. 10.1016/j.chiabu.2017.10.002 [DOI] [PubMed] [Google Scholar]
- Putnam-Hornstein E, Prindle JJ, & Leventhal JM (2016). Prenatal substance exposure and reporting of child maltreatment by race and ethnicity. Pediatrics, 138(3), e20161273. 10.1542/peds.2016-1273 [DOI] [PubMed] [Google Scholar]
- Radel L, Baldwin M, Crouse G, Ghertner R, & Waters A (2018). Substance use, the opioid epidemic, and the child welfare system: Key findings from a mixed methods study. ASPE Research Brief. Washington, DC: Office of the Assistant Secretary for Planning and Evaluation, U.S. Department of Health and Human Services. [Google Scholar]
- Roberts SCM, & Nuru-Jeter A (2012). Universal screening for alcohol and drug use and racial disparities in child protective services reporting. The Journal of Behavioral Health Services & Research, 39(1), 3–16. 10.1007/s11414-011-9247-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogers-Adkinson DL, & Stuart SK (2007). Collaborative services: Children experiencing neglect and the side effects of prenatal alcohol exposure. Language, Speech, and Hearing Services in Schools, 38(2), 149–156. 10.1044/0161-1461(2007/015) [DOI] [PubMed] [Google Scholar]
- Ryan JP, Choi S, Hong JS, Hernandez P, & Larrison CR (2008). Recovery coaches and substance exposed births: An experiment in child welfare. Child Abuse & Neglect, 32(11), 1072–1079. 10.1016/j.chiabu.2007.12.011 [DOI] [PubMed] [Google Scholar]
- Schiff DM, & Patrick SW (2017). Treatment of opioid use disorder during pregnancy and cases of neonatal abstinence syndrome. JAMA Pediatrics, 171(7), 707–707. 10.1001/jamapediatrics.2017.0854 [DOI] [PubMed] [Google Scholar]
- Shamseer L, Moher D, Clarke M, Ghersi D, Liberati A, Petticrew M, Shekelle P, & Stewart LA (2015). Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: Elaboration and explanation. BMJ, 349, g7647. 10.1136/bmj.g7647 [DOI] [PubMed] [Google Scholar]
- Smith DK, Johnson AB, Pears KC, Fisher PA, & DeGarmo DS (2007). Child maltreatment and foster care: Unpacking the effects of prenatal and postnatal parental substance use. Child Maltreatment, 12(2), 150–160. 10.1177/1077559507300129 [DOI] [PubMed] [Google Scholar]
- Stratton K, Howe C, & Battaglia F (1996). Fetal alcohol syndrome: Diagnosis, epidemiology, prevention and treatment. Washington, DC: The National Academies Press. [Google Scholar]
- Streissguth AP, Bookstein FL, Barr HM, Sampson PD, O’Malley K, & Young JK (2004). Risk factors for adverse life outcomes in fetal alcohol syndrome and fetal alcohol effects. J Dev Behav Pediatr, 25(4), 228–238. 10.1097/00004703-200408000-00002 [DOI] [PubMed] [Google Scholar]
- Sun AP, Freese MP, & Fitzgerald M (2007). An exploratory study of drug-exposed infants: Case substantiation and subsequent child maltreatment. Child Welfare, 86(3), 33–50. [PubMed] [Google Scholar]
- Turchi RM, & Smith VC; AAP Committee on Substance Use and Prevention, AAP Council on Children with Disabilities. (2018). The role of integrated care in a medical home for patients with a fetal alcohol spectrum disorder. Pediatrics, 142(4), e20182333. 10.1542/peds.2018-2333 [DOI] [PubMed] [Google Scholar]
- Twomey JE, Caldwell D, Soave R, Fontaine LA, & Lester BM (2010). Vulnerable infants program of Rhode Island: Promoting permanency for substance-exposed infants. Child Welfare, 89(3), 121–142. [PubMed] [Google Scholar]
- Wulczyn F, Michelle E, & Fisher P (2011). Who are the infants in out-of-home care? An epidemiological and developmental snapshot. Chicago, IL: Chapin Hall Issue Brief: University of Chicago. [Google Scholar]
- Young NK, Boles SM, & Otero C (2007). Parental substance use disorders and child maltreatment: Overlap, gaps, and opportunities. Child Maltreatment, 12(2), 137–149. 10.1177/1077559507300322 [DOI] [PubMed] [Google Scholar]
- Young NK, & Collins J (2015). Special foreword: Substance use and child welfare. Child Welfare, 94(4), 11. [PubMed] [Google Scholar]


