Abstract
During the COVID-19 pandemic, social distancing measures often result in individual isolation, which can lead to adverse mental outcomes. We collected online questionnaires from 3,952 US adults to examine the impact of “shelter-in-place” guidelines on mental health, and to explore potential disparities and modifiable factors. Self-reported anxiety, depression, and PTSD symptoms were associated with more restrictive quarantine. Younger adults, women, those with lower income, more insecurity, more media exposure, reduced physical activity, or worsened family relationships were particularly affected. Targeted prevention on susceptible subpopulations, including young adults and lower SES groups, might help mitigate disparities in COVID-19-related mental health problems.
Keywords: COVID-19, Mental health, Social distancing
1. Introduction
The coronavirus disease 2019 (COVID-19) pandemic has caused unprecedented social distancing measures worldwide. Within the US, “shelter-in-place” guidelines or “stay-at-home” orders have been issued at some time in most states since March 2020 (Mervosh et al. 2020). Although highly effective in containing the spread of the virus, these measures may result in considerable mental health concerns (Brooks et al. 2020; Miller 2020), especially among vulnerable populations including those with low socioeconomic status (SES) and college students (McGinty et al. 2020; Wang et al. 2020; Wathelet et al. 2020). It is critical to understand the impact of “shelter-in-place” on mental health, and to identify vulnerable groups and coping strategies. We aimed to investigate the association of “shelter-in-place” with mental health symptoms, and to explore potential disparities and modifiable factors in COVID-19-related mental health symptoms among US adults.
2. Methods
We conducted a cross-sectional online survey based on the REDCap platform (Nashville, TN) between May 13 and August 25, 2020. The survey link was disseminated via social networks (e.g., Facebook, Twitter) and ResearchMatch (Harris et al. 2012). Adults residing in the US and aged ≥18 years were eligible for this study. Consent of participation was granted when the voluntary survey was answered. The study was approved by the Institutional Review Board of the University at Buffalo.
Quarantine status at the time of the survey was categorized as: (1) no restriction, (2) stayed at home most of the time but went to work/school sometimes, (3) stayed at home almost all the time, and (4) practiced isolation because of exposure history. Self-reported symptoms of anxiety, depression, and post-traumatic stress disorder (PTSD) were identified through the Generalized Anxiety Disorder Scale-7 items (GAD-7) (Spitzer et al. 2006), the Patient Health Questionnaire-9 items (PHQ-9) (Spitzer et al. 1999), and the primary care PTSD screen (PC-PTSD) (Prins et al. 2003), respectively. GAD-7 consists of seven items that detect the frequency of anxiety symptoms in the past two weeks. Each item includes options scored as 0 (not at all), 1 (several days), 2 (over half the days), and 3 (nearly every day), with a total possible score of 21 (Spitzer et al. 2006). PHQ-9 consists of nine items scoring the frequency (same as GAD-7) of depression symptoms over the past two weeks, with a summed score ranging from 0 to 27 (Spitzer et al. 1999). Scores of ≥10 on the GAD-7 and PHQ-9 scale were defined as moderate to severe anxiety and moderate to severe depression, respectively (Kroenke et al. 2001; Spitzer et al. 2006). PC-PTSD includes four items in dichotomous response format (yes/no) asking if respondents have experienced symptoms of PTSD in the past month (Prins et al. 2003). A sum score ≥3 on the PC-PTSD scale (i.e. respondents answered “yes” for 3 or more items) was defined as positive for PTSD symptoms (Prins et al. 2003). “Insecurity” was defined if participants reported concerns about money, health insurance, or food. We asked participants whether their physical activity and sleep duration had increased, decreased, or remained unchanged since the pandemic. We also asked about changes in relationships with parents, children, and spouse and assigned scores of 1, 0, or -1 if the relationship was better, unchanged (including not applicable), or worse. We added scores up and categorized relationship change into “No change”, “Better”, or “Worse” if the total score was equal to, above, or below 0. Media exposure was measured in hours/day spent on COVID-19-related information.
The associations of quarantine status and symptoms of mental illness were examined by logistic regression models, adjusting for a priori defined confounders, including age, gender, race, income, education, marital status, retirement status, and county-level incidence of COVID-19. Joint effects of quarantine status with social determinants, behavioral factors, relationship changes, or chronic disease status on anxiety, depression, and PTSD symptoms were analyzed by the GENMOD procedure, adjusting for abovementioned potential confounders. Statistical analyses were conducted using SAS 9.4 (Cary, NC).
3. Results
Of 3,952 participants (age mean [SD]: 52.2 [16.8], range:18-96) from 25 states in the US included in this study, 21.1% were male, 82.0% White, 7.5% students, 22.7% reported moderate to severe anxiety, 26.7% moderate to severe depression, and 21.8% PTSD symptoms. Those who were younger, female, smokers, with less than a college education, household income below $75,000, or insecurity were more likely to report symptoms of mental illness. Students reported a higher prevalence of mental health symptoms than the overall population (Supplemental Table).
Compared to no restriction, staying at home almost all the time was associated with 1.47 (95% CI: 1.15-1.87), 1.50 (95% CI: 1.19-1.90), and 1.57 (95% CI: 1.22-2.01) times higher odds of anxiety, depression, and PTSD. Isolation due to exposure was associated with 2.54 (95% CI: 1.70-3.79), 2.70 (95% CI: 1.84-3.95), and 2.60 (95% CI: 1.74-3.89) times higher odds of symptoms of anxiety, depression, and PTSD. However, the odds of mental health symptoms among individuals who went to work/school sometimes were not significantly different from those without restrictions (anxiety: OR=1.00, 95% CI: 0.87-1.35; depression: OR=0.98, 95% CI: 0.73-1.30; PTSD: OR=1.23, 95% CI: 0.91-1.67).
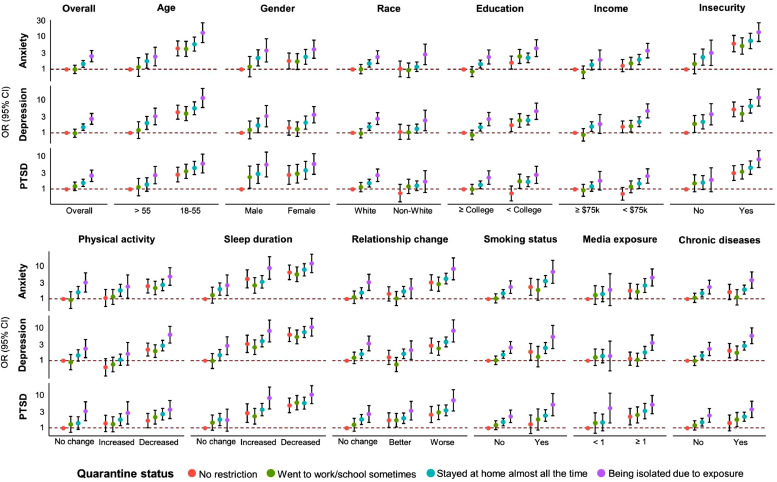
Associations of quarantine status with symptoms of anxiety, depression, and PTSD were stronger among people who were younger, female, smokers, with less than a college education, household income <$75,000, insecurity, ≥1-hour media exposure, decreased physical activity, decreased sleeping duration, or worsened family relationships (Fig. 1 ).
Fig. 1.
Joint effects of quarantine status and social determinants, behavioral factors, changes in relationships, or chronic disease status on reported symptoms of anxiety, depression, and PTSD.
Dots represent estimated ORs for symptoms of anxiety (GAD-7≥10), depression (PHQ-9≥10), and PTSD (screen score≥3), and error bars construct 95% CIs. Dashed lines indicate the null joint association (OR=1): participants with “no restriction” and the first level (furthest left) of each determinant/factor were the reference group, e.g., the reference group was participants with “no restriction” and aged >55 years for the joint effect of quarantine status and age. Insecurity was identified with reporting worries of money, health insurance, or food during the pandemic. Relationships changes were summarized from separated scores with parents, children, and spouse since the pandemic (1=improved, 0=unchanged [or not applicable], -1=worsened). Abbreviations: GAD-7, Generalized Anxiety Disorder Scale-7 items (GAD-7); PHQ-9, Patient Health Questionnaire-9 items; PTSD, Post-Traumatic Stress Disorder; OR, odds ratio; CI, confidence interval.
4. Discussion
The prevalence of anxiety and depression symptoms was much higher during than before the pandemic (anxiety: 8.1% and depression: 6.5%) (National Center for Health Statistics 2020). The high prevalence among students was worth noting, possibly resulting from multiple concerns about academic delays, financial support, and decreased social connections in this group (Zhai and Du 2020).
Consistent with previous studies, self-reported symptoms of adverse health outcomes were associated with more restrictive quarantine conditions (Benke et al. 2020; Tull et al. 2020). Younger adults, women, those with less income, and with insecurity regarding money, health insurance, or food were more vulnerable to “shelter-in-place”, which were also in line with other literature (Benke et al. 2020; Pierce et al. 2020). Although older people were at a higher risk of severe illness from COVID-19, younger adults seemed more susceptible to experiencing symptoms of mental illnesses during the pandemic, possibly because their social lives were disrupted suddenly due to quarantine measures (Benke et al. 2020), while older people might have retired and been more accustomed to staying home. We did not observe differences by race/ethnicity, possibly due to differences in the reporting of mental illnesses among African Americans (AA) (Bailey et al. 2019) or to the small number of AA participants in our study (6.4%). Moreover, together with evidence from other studies, our findings suggested that keeping physically active might help alleviate some of the negative mental health effects of quarantine. Physical activities may contribute to better mental health by increasing neurogenesis, reducing inflammation and oxidant stress, and improving self-esteem (Schuch et al. 2016; Schuch et al. 2018). In addition, being less exposed to COVID-19-related media information and improving family relationship may also be associated with lower reports of negative mental outcomes during the pandemic (Chen et al. 2020; Gao et al. 2020; Jacob et al. 2020; Pieh et al. 2020).
Some limitations of this study have to be acknowledged. First, our study was cross-sectional by design thus we were unable to determine temporality in the associations of mental health symptoms with quarantine conditions. Second, although the psychometric scales have been extensively validated, self-reported symptoms of mental illness could be subject to measurement error, particularly in the unusual circumstances of the pandemic. Third, our anonymous online survey was completed by a convenience sample of whoever was able to access it; we were not able to determine the response rate. People with access to social networks/internet were more likely to complete the survey. Also, people experiencing more mental illness symptoms might be more interested in participating in such a study. In both instances, selection bias might occur. Finally, our study population were predominantly White with high education levels which might limit our study findings to be generalized to other populations.
Our findings of associations of “shelter-in-place” with COVID-19-related mental health symptoms could possibly have implications for targeted prevention among susceptible populations. With the ongoing COVID-19 pandemic, “shelter-in-place” guidelines may continue and possibly exacerbate disparities in mental health. Promoting better, healthier behaviors, especially among the susceptible populations including students, young adults, and low-SES groups, might help address mental health problems during the pandemic with potential implications as well for social isolation and prevention when the pandemic has ended.
Author Contributions
Kexin Zhu: Investigation, Formal analysis, Visualization, Writing - original draft; Zhongzheng Niu: Investigation, Methodology, Writing - original draft; Jo L. Freudenheim: Conceptualization, Writing - review & editing; Zuo-Feng Zhang: Conceptualization, Writing - review & editing; Lijian Lei: Conceptualization; Gregory G. Homish: Conceptualization; Ying Cao: Conceptualization; Shauna C. Zorich: Writing - review & editing; Yihua Yue: Investigation; Rujie Liu: Investigation; Lina Mu: Conceptualization, Methodology, Supervision, Writing - review & editing.
Funding disclosure
This study was supported by the University at Buffalo Institutional Internal Funding.
Declaration of Competing Interest
None.
Acknowledgements
We acknowledge the anonymous participants in our online survey.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.psychres.2021.113959.
Appendix. Supplementary materials
References
- Bailey R.K., Mokonogho J., Kumar A. Racial and ethnic differences in depression: current perspectives. Neuropsychiatr Dis Treat. 2019;15:603–609. doi: 10.2147/NDT.S128584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benke C., Autenrieth L.K., Asselmann E., Pané-Farré C.A. Stay-at-home orders due to the COVID-19 pandemic are associated with elevated depression and anxiety in younger, but not older adults: results from a nationwide community sample of adults from Germany. Psychol Med. 2020:1–2. doi: 10.1017/S0033291720003438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brooks S.K., Webster R.K., Smith L.E., Woodland L., Wessely S., Greenberg N., et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. The Lancet. 2020;395:912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen B., Sun J., Feng Y. How Have COVID-19 Isolation Policies Affected Young People's Mental Health? - Evidence From Chinese College Students. Frontiers in psychology. 2020;11 doi: 10.3389/fpsyg.2020.01529. 1529-1529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gao J., Zheng P., Jia Y., Chen H., Mao Y., Chen S., et al. Mental health problems and social media exposure during COVID-19 outbreak. PLOS ONE. 2020;15 doi: 10.1371/journal.pone.0231924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris P.A., Scott K.W., Lebo L., Hassan N., Lighter C., Pulley J. ResearchMatch: a national registry to recruit volunteers for clinical research. Academic medicine: journal of the Association of. American Medical Colleges. 2012;87:66. doi: 10.1097/ACM.0b013e31823ab7d2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacob L., Tully M.A., Barnett Y., Lopez-Sanchez G.F., Butler L., Schuch F., et al. The relationship between physical activity and mental health in a sample of the UK public: A cross-sectional study during the implementation of COVID-19 social distancing measures. Mental Health and Physical Activity. 2020;19 doi: 10.1016/j.mhpa.2020.100345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K., Spitzer R.L., Williams J.B. The PHQ-9: validity of a brief depression severity measure. Journal of general internal medicine. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGinty E.E., Presskreischer R., Han H., Barry C.L. Psychological Distress and Loneliness Reported by US Adults in 2018 and April 2020. JAMA. 2020;324:93–94. doi: 10.1001/jama.2020.9740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mervosh, S.; Lu, D.; Swales, V. See which states and cities have told residents to stay at home. New York Times 2020:https://www.nytimes.com/interactive/2020/us/coronavirus-stay-at-home-order.html.
- Miller G. Social distancing prevents infections, but it can have unintended consequences. Science. 2020 https://www.sciencemag.org/news/2020/2003/we-are-social-species-how-will-social-distancing-affect-us [Google Scholar]
- National Center for Health Statistics Early Release of Selected Mental Health Estimates Based on Data from the January–June 2019. National Health Interview Survey. 2020 https://www.cdc.gov/nchs/data/nhis/earlyrelease/ERmentalhealth-508.pdf [Google Scholar]
- Pieh C., O´Rourke T., Budimir S., Probst T. Relationship quality and mental health during COVID-19 lockdown. PLOS ONE. 2020;15 doi: 10.1371/journal.pone.0238906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pierce M., Hope H., Ford T., Hatch S., Hotopf M., John A., et al. Mental health before and during the COVID-19 pandemic: a longitudinal probability sample survey of the UK population. The Lancet Psychiatry. 2020;7:883–892. doi: 10.1016/S2215-0366(20)30308-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prins A., Ouimette P., Kimerling R., Cameron R.P., Hugelshofer D.S., Shaw-Hegwer J., et al. The primary care PTSD screen (PC-PTSD): Development and operating characteristics. Primary Care Psychiatry. 2003;9:9–14. [Google Scholar]
- Schuch F.B., Deslandes A.C., Stubbs B., Gosmann N.P., Silva C.T., Fleck M.P. Neurobiological effects of exercise on major depressive disorder: A systematic review. Neuroscience and biobehavioral reviews. 2016;61:1–11. doi: 10.1016/j.neubiorev.2015.11.012. [DOI] [PubMed] [Google Scholar]
- Schuch F.B., Vancampfort D., Firth J., Rosenbaum S., Ward P.B., Silva E.S., et al. Physical Activity and Incident Depression: A Meta-Analysis of Prospective Cohort Studies. American Journal of Psychiatry. 2018;175:631–648. doi: 10.1176/appi.ajp.2018.17111194. [DOI] [PubMed] [Google Scholar]
- Spitzer R.L., Kroenke K., Williams J.B., Group P.H.Q.P.C.S. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Jama. 1999;282:1737–1744. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- Spitzer R.L., Kroenke K., Williams J.B., Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Archives of internal medicine. 2006;166:1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- Tull M.T., Edmonds K.A., Scamaldo K.M., Richmond J.R., Rose J.P., Gratz K.L. Psychological Outcomes Associated with Stay-at-Home Orders and the Perceived Impact of COVID-19 on Daily Life. Psychiatry Res. 2020;289 doi: 10.1016/j.psychres.2020.113098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C., Pan R., Wan X., Tan Y., Xu L., Ho C.S., et al. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. International journal of environmental research and public health. 2020;17:1729. doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wathelet M., Duhem S., Vaiva G., Baubet T., Habran E., Veerapa E., et al. Factors Associated With Mental Health Disorders Among University Students in France Confined During the COVID-19 Pandemic. JAMA Network Open. 2020;3 doi: 10.1001/jamanetworkopen.2020.25591. e2025591-e2025591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhai Y., Du X. Addressing collegiate mental health amid COVID-19 pandemic. Psychiatry Res. 2020;288 doi: 10.1016/j.psychres.2020.113003. 113003-113003. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.