Abstract
Purpose: Sexual minority (SM) individuals experience higher rates of anxiety and depression. Previous research on mental health disparities for SM cancer survivors has largely focused on adult survivors; however, studies are limited in the adolescent and young adult (AYA) population. This study's objective is to compare depression and anxiety symptoms between AYA, female cancer survivors who identify as an SM and those who identify as heterosexual.
Methods: A cross-sectional analysis of 1025 AYA survivors aged 18–40 years (2015–2017) was performed. Patients self-reported SM identification and depression and anxiety symptoms, as measured by the Patient Health Questionnaire (PHQ8) and Generalized Anxiety Disorder Scale (GAD7), respectively. Multivariable logistic regression tested associations between SM identification and depression and anxiety.
Results: Sixty-four participants (6%) identified as an SM. In adjusted analyses, SM participants had 1.88 higher odds of anxiety (odds ratio [OR] 1.88, confidence interval [95% CI] 1.05–3.35, p = 0.033) compared with heterosexual participants. SM participants did not have significantly higher odds of depression (OR 1.36, CI 0.75–2.47, p = 0.31). More social support was significantly associated with lower odds of depression (OR 0.91, CI 0.89–0.93, p < 0.001) and anxiety (OR 0.93, CI 0.91–0.94, p < 0.001).
Conclusions: AYA cancer survivors identifying as an SM had nearly twice the odds of anxiety, with social support that is protective for both anxiety and depression. While mental health screening is recommended throughout the cancer care continuum, these data support the need for reliable screening, clinician awareness of increased vulnerability in the AYA, SM survivor population, and clinician training on culturally competent care and generation of evidence-based interventions.
Keywords: mental health, depression, anxiety, sexual minority, LGBTQ, survivorship
Background
In the United States, there are nearly 400,000 adolescent and young adult (AYA), female cancer survivors, diagnosed between the ages of 15 and 39.1 This patient group represents a medically underserved population with unique challenges. AYA survivors report major concern over unmet psychological needs2; one study found that the majority of AYA survivors who needed mental health services did not receive them.3 AYA survivors frequently describe symptoms of post-traumatic stress, anxiety, depression, and fears of cancer recurrence.4
Sexual minority (SM) is a term used to describe individuals who identify as nonheterosexual (e.g., lesbian, gay, bisexual, or queer) or engage in same-sex sexual behavior.5 The 2013 National Health Interview Survey estimated that 2.5%–4% of adults identify as an SM in the United States.6 SM individuals represent an increasingly recognized medically underserved population.7 An estimated 420,000 to 1,000,000 SM cancer survivors live in the United States.8,9 Mixed results have been reported on risk for mental health outcomes among SM cancer survivors diagnosed in adulthood.10 SM cancer patients report less satisfaction with psychosocial care in the oncology setting.11 Mental health disorders are linked to worse health outcomes for cancer survivors, including higher mortality, faster disease progression, decreased treatment adherence, and increased costs throughout the health care system.10,12,13–15 To our knowledge, no studies have investigated psychological outcomes among AYA, SM cancer survivors specifically.
This study's objective is to compare self-reported depression and anxiety symptoms between AYA, female cancer survivors who identify as SM and those who identify as heterosexual. We hypothesized that AYA SM survivors have higher rates of depression and anxiety when compared with AYA heterosexual survivors. We investigated if social support modifies the association between SM identification and mood outcomes.
Methods
Participants
Cross-sectional analyses were performed using data from baseline questionnaires completed by participants in the Reproductive Window Study (WINDOW), a prospective cohort study on ovarian function in AYA, female cancer survivors. Eligibility criteria included a cancer diagnosis between ages 15 and 35, ages 18 and 40 at enrollment, completion of primary cancer treatment, and the presence of at least one ovary. Cancer types included the 10 most common cancers in AYA cancer survivors: breast, leukemia, lymphoma, gynecologic, intestines, gallbladder, pancreas, bone, soft tissue tumor of bone/fat, skin, and thyroid. Participants were enrolled between March 2015 and May 2017 and were recruited from the California and Texas Cancer Registries (38.1%), University of California, San Diego Health System (27.8%), cancer advocacy organizations (9.7%), physician referrals (5.5%), and other sources (18.8%). The State of California Committee for the Protection of Human Subjects and the institutional review boards at the University of California, San Diego, and the Texas Department of State Health Services approved this study.
Data collection
Potential participants were contacted through mailed recruitment letters, telephone calls, or emails that included directions to the secure, online study portal. Study questionnaires were completed through the study portal in English, which collected self-reported information on cancer and reproductive, medical, demographic, and lifestyle characteristics using questions derived from large cancer and reproductive cohort studies, with a total of 177 questions taking ∼30 minutes to complete.16,17 In the consent form, participants were advised that they did not have to answer questions that they did not feel comfortable to answer. Participants were compensated with a $10 gift card for questionnaire completion. Participants provided consent for HIPAA and medical record release. Cancer and treatment data were abstracted from primary medical records by two pediatric oncologists and one reproductive endocrinologist using the Childhood Cancer Survivor Study methods and case report forms, with high agreement on rereview.17,18
Identification as an SM was evaluated by the National Survey for Family Growth question: “Do you think of yourself as—heterosexual or straight; homosexual or lesbian; bisexual; or prefer not to answer?” Participants who responded heterosexual or straight were coded as heterosexual and those who responded homosexual or lesbian or bisexual were coded as SM. Patients who responded with prefer not to answer were excluded from the analysis as we were interested in the subgroup that self-identified as an SM.17
Health behavior information was collected using standardized questionnaires. Alcohol use was considered a three-level variable: current, former, or never. Additionally, any participants who reported consuming ≥4 alcoholic drinks within a 2-hour period during the last year were coded as having engaged in binge drinking. Cigarette use was considered a three-level variable: current, former, or never. Physical activity was assessed by asking participants how many days in the past week they were physically active for at least 30 minutes.19
Perceived stress was measured using the Perceived Stress Scale (10-item version), a standardized questionnaire of perceived stress in the past month. A higher score indicates a higher level of perceived stress.20
Social support was assessed using a questionnaire similar to the F-SozU K-9, a brief form of the Perceived Social Support Questionnaire, which is valid throughout cultures and in SM women.21,22 Participants were asked “How often is each of the following kinds of support available to you if you need it?”; examples include “Someone you can count on to listen to you when you need to talk” and “Someone to take you to the doctor if you need it.” Participants' responses were on a scale from 1 to 5, with 1 being “none of the time” and 5 being “all of the time,” and summed to generate a cumulative social support score (minimum of 9, low support; maximum of 45, high support).
Outcomes
Symptoms of depression and anxiety were assessed using the standardized and validated eight-item Patient Health Questionnaire (PHQ8)23 and the seven-item General Anxiety Disorder (GAD7)24 screening tools, respectively. The PHQ8 consists of eight of the nine Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-V), screening questions for depressive disorder. Patients were asked if they had experienced each symptom in the previous 2 weeks (with five possible responses: not at all, several days, more than half the days, nearly every day, and prefer not to answer). Responses of not at all were coded as 0 points, several days as 1 point, more than half the days as 2 points, and nearly every day as 3 points. Participants' responses to all questions were summed to generate a cumulative symptom score (PHQ8 maximum score 24, GAD7 maximum score 21). PHQ8 scores ≥10 were considered positive for depression, which is clinically relevant for major depression.25 GAD7 scores ≥10 were considered positive for anxiety, which has a high sensitivity and specificity for GAD.24
Statistical analyses
Data were examined for outliers. The distribution of continuous variables was evaluated for normality. Descriptive statistics are described with a mean and standard deviation for continuous variables and counts and percentages for categorical variables. Both outcome variables, PHQ8 and GAD7, were positively skewed, but kept in original scale due to the large sample size.25
Student's t-test or Pearson's chi-square test was used to compare characteristics by SM identification. We performed unadjusted logistic regression analyses to test for associations between SM identification and other covariates with depression and anxiety. Through a review of available literature, we selected a priori age at study enrollment, race, ethnicity, and social support as possible confounders for inclusion in multivariable regression as these factors can affect whether an individual feels comfortable identifying as an SM on a survey and may be associated with depression and anxiety. Other variables associated with both SM identification and mental health include, but are not limited to, marital status, job status, income, and education. However, in the causal pathway, these variables would not precede SM identification and thus were not considered confounders for inclusion in the logistic regression model. We tested whether social support was an effect modifier of the association between SM identification and depression or anxiety by introducing an interaction term to the adjusted logistic regression.
All tests were two-tailed; statistical significance was set at p-value <0.05. All analyses were performed using IBM SPSS Statistics for Mac iOS (version 25) for statistical software.
Results
Of the 1150 participants who consented, agreed, and were eligible to participate, 1071 (93%) completed the baseline questionnaire. Of the 1071 women enrolled in the WINDOW study, 13 were missing data on SM identification, 15 were missing data on GAD7 or PHQ8, and 18 were missing data on social support for a final study population of 1025 women.
Baseline characteristics by SM identification are provided in Table 1. Overall, 64 participants (6.2%) identified as an SM. Mean age at cancer diagnosis was 25, with leukemia, lymphoma, and breast cancer as the most common diagnoses. Few patients reported stage 4 disease. The majority of participants received surgery or chemotherapy as treatment for their cancer. While the level of education and reported income did not vary between groups, a significantly larger proportion of SM participants reported being unemployed (27%) compared with heterosexuals (14%) (p = 0.012). Alcohol use and physical activity did not vary between the groups. However, significantly higher proportions of SM participants reported current (11%) or former (28%) cigarette use compared with heterosexuals (current: 5%; former: 13%) (p = 0.001). Both groups reported similar levels of perceived stress (SM: mean score 17.4; heterosexual: 16.0; p = 0.14). In contrast, SM participants reported significantly less social support compared with heterosexual participants (SM: mean score 35.9; heterosexual: 38.1; p = 0.031).
Table 1.
Baseline Demographic Characteristics and Health Behaviors, Stratified by Identification as a Sexual Minority (N = 1025)
| Sexual Minority (N = 64) | Heterosexual (N = 961) | pa | |
|---|---|---|---|
| Age at enrollment, years, mean (SD) | 32.9 (5.3) | 33.3 (4.9) | 0.58 |
| Age at diagnosis, years, mean (SD) | 25.4 (6.1) | 25.8 (5.7) | 0.64 |
| Years since diagnosis, n (%) | |||
| <5 years | 13 (20.3) | 32 (34.1) | 0.023 |
| ≥5 years | 51 (79.7) | 633 (65.9) | |
| First cancer, n (%) | |||
| Breast | 15 (23.4) | 218 (22.7) | 0.88 |
| Leukemia or lymphoma | 25 (39.1) | 334 (34.8) | |
| Cervix, uterus, or ovary | 7 (10.9) | 108 (11.2) | |
| Intestines, gallbladder, pancreas, or stomach | 1 (1.6) | 25 (2.6) | |
| Bone, soft tissue tumor of muscle or fat | 6 (9.4) | 67 (7.0) | |
| Skin (including melanoma) | 2 (3.1) | 29 (3.0) | |
| Stage at cancer diagnosis, n (%)b | |||
| Stage 1 | 14 (21.9) | 180 (18.7) | 0.78 |
| Stage 2 | 21 (32.8) | 276 (28.7) | |
| Stage 3 | 10 (15.6) | 141 (14.7) | |
| Stage 4 | 4 (6.3) | 65 (6.8) | |
| Don't know or prefer not to answer | 6 (9.4) | 171 (17.8) | |
| Treatment received for first cancer, n (%) | |||
| Surgery to remove tumor | 39 (60.9) | 628 (65.3) | 0.47 |
| Radiation | 26 (40.6) | 450 (46.8) | 0.34 |
| Chemotherapy | 44 (68.8) | 645 (67.1) | 0.79 |
| Endocrine therapy | 12 (18.8) | 145 (15.1) | 0.43 |
| BM or stem cell transplant | 2 (3.2) | 42 (4.4) | 0.74 |
| Biologic therapy or immunotherapy | 2 (3.1) | 32 (3.3) | 0.93 |
| Race, n (%) | |||
| African American | 3 (4.7) | 26 (2.7) | 0.71 |
| Asian or Native American | 4 (6.3) | 70 (7.3) | |
| Mixed/other | 9 (14.1) | 168 (17.5) | |
| White | 48 (75.0) | 697 (72.5) | |
| Hispanic ethnicity, n (%) | 10 (15.6) | 243 (25.3) | 0.083 |
| Marital status, n (%) | |||
| Married or living with partner | 41 (64.1) | 669 (69.6) | 0.48 |
| Separated, divorced, or widowed | 2 (3.1) | 41 (4.3) | |
| Never been married | 21 (32.8) | 251 (26.1) | |
| Education, n (%) | |||
| Did not obtain a high school degree | 0 (0) | 10 (1) | 0.7 |
| Graduated from high school | 2 (3.1) | 35 (3.6) | |
| Graduated from college | 62 (96.9) | 916 (95.3) | |
| Job status, n (%) | |||
| Employed | 46 (71.9) | 823 (85.6) | 0.012 |
| Unemployed | 17 (26.6) | 132 (13.7) | |
| Prefer not to answer | 1 (1.6) | 6 (0.6) | |
| Income, n (%) | |||
| <$51,000 | 22 (34.4) | 248 (25.8) | 0.22 |
| >$51,000 | 37 (57.8) | 657 (68.4) | |
| Prefer not to answer | 5 (7.8) | 56 (5.8) | |
| Alcohol use, n (%) | |||
| Current | 58 (90.6) | 861 (89.6) | 0.94 |
| Former | 4 (6.3) | 62 (6.5) | |
| Never | 2 (3.1) | 38 (4.0) | |
| Binge drinking in last year, binary, n (%) | 28 (48.3) | 429 (49.8) | 0.82 |
| Cigarette use, n (%) | |||
| Current | 7 (10.9) | 51 (5.3) | 0.001 |
| Former | 18 (28.1) | 126 (13.1) | |
| Never | 39 (60.9) | 777 (80.9) | |
| I don't know | 0 (0) | 7 (0.7) | |
| Physical activity, days active, mean (SD) | 3.81 (1.95) | 4.09 (2.01) | 0.28 |
| Social support, mean (SD) | 35.9 (9.0) | 38.1 (7.9) | 0.031 |
| Perceived stress, mean (SD) | 17.4 (6.7) | 16.0 (7.2) | 0.14 |
| PHQ8, mean (SD) | 7.8 (5.8) | 6.0 (5.2) | 0.009 |
| GAD7, mean (SD) | 7.2 (5.7) | 5.7 (5.4) | 0.039 |
Independent unpaired t-test was used to test differences in continuous traits. For categorical variables, the Pearson χ2 test was used.
Percentages do not sum to 100% as information on the leukemia patient risk group is not presented.
BM, bone marrow; GAD7, Generalized Anxiety Disorder 7-item scale; PHQ8, Patient Health Questionnaire depression scale; PTSD, post-traumatic stress disorder.
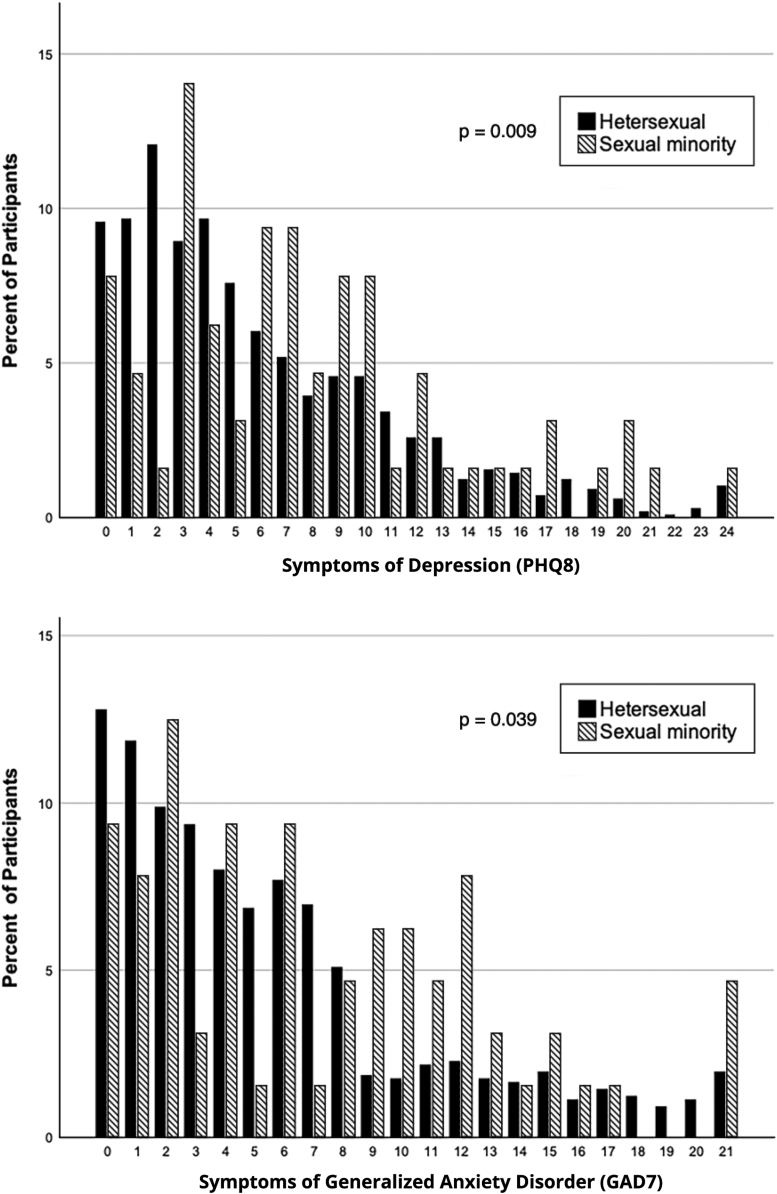
Thirty-one percent of SM participants met criteria for clinical depression compared with 23% of heterosexual participants (p = 0.12). The SM group had significantly higher mean PHQ8 scores compared with the heterosexual group (7.8 vs. 6.0, p = 0.009) (Fig. 1). In both unadjusted and adjusted analyses, SM participants did not have statistically significant higher odds of depression compared with heterosexual participants (Table 2). More social support was significantly associated with lower odds of depression in adjusted analyses (odds ratio [OR] 0.91, confidence interval [95% CI] 0.89–0.93, p < 0.001).
FIG. 1.
Distribution of the PHQ8 depression scale (PHQ8) (top) and the GAD7 (bottom) scores stratified by identification as a sexual minority in the Reproductive Window Study (WINDOW) (N = 1025). GAD7, Generalized Anxiety Disorder 7-item scale; PHQ8, 8-item Patient Health Questionnaire.
Table 2.
Effect of Identifying as a Sexual Minority on Depression and Anxiety (N = 1025)
| Depression |
Anxiety |
|||||||
|---|---|---|---|---|---|---|---|---|
| Unadjusted |
Adjusteda |
Unadjusted |
Adjusteda |
|||||
| Odds ratio (95% CI) | p | Odds ratio (95% CI) | p | Odds ratio (95% CI) | p | Odds ratio (95% CI) | p | |
| Sexual orientation | ||||||||
| Sexual minority | 1.55 (0.89–2.68) | 0.12 | 1.36 (0.75–2.47) | 0.31 | 2.15 (1.26–3.70) | 0.005 | 1.88 (1.05–3.35) | 0.033 |
| Heterosexual | Reference | Reference | Reference | Reference | ||||
| Age at enrollment | 0.97 (0.94–1.00) | 0.059 | 0.96 (0.94–1.00) | 0.024 | 0.98 (0.95–1.01) | 0.16 | 0.97 (0.94–1.01) | 0.10 |
| Race | ||||||||
| African American | 0.69 (0.26–1.85) | 0.46 | 0.44 (0.15–1.31) | 0.14 | 0.60 (0.21–1.75) | 0.35 | 0.41 (0.13–1.30) | 0.13 |
| Asian or Native American | 0.65 (0.34–1.22) | 0.18 | 0.58 (0.29–1.14) | 0.12 | 0.52 (0.25–1.06) | 0.073 | 0.48 (0.23–1.02) | 0.057 |
| Mixed/other | 1.28 (0.88–1.85) | 0.20 | 1.35 (0.84–2.17) | 0.22 | 1.09 (0.74–1.62) | 0.66 | 1.07 (0.66–1.75) | 0.78 |
| White | Reference | Reference | Reference | Reference | ||||
| Ethnicity | ||||||||
| Hispanic | 1.07 (0.77–1.49) | <0.001 | 0.84 (0.54–1.29) | 0.42 | 1.07 (0.76–1.52) | <0.001 | 0.97 (0.63–1.51) | 0.90 |
| Not Hispanic | Reference | Reference | Reference | Reference | ||||
| Social support | 0.91 (0.90–0.93) | <0.001 | 0.91 (0.89–0.93) | <0.001 | 0.93 (0.91–0.94) | <0.001 | 0.93 (0.91–0.94) | <0.001 |
Adjusted model controls for age at enrollment, race, ethnicity, and social support.
CI, confidence interval.
Thirty-four percent of SM participants met criteria for clinical anxiety compared with 20% of heterosexual participants (p = 0.004). The SM group had significantly higher mean GAD7 scores compared with the heterosexual group (7.2 vs. 5.7, p = 0.039) (Fig. 1). In adjusted analysis, SM participants had 1.88 higher odds of anxiety compared with heterosexual participants (Table 2). More social support was also significantly associated with lower odds of anxiety in adjusted analysis (OR 0.93, CI 0.91–0.94, p < 0.001).
An interaction term for SM identification and social support was introduced into the multivariable models and was not significantly associated with either depression (p = 0.43) or anxiety (p = 0.58).
In exploratory analyses, we stratified participants into adolescents (15–18 years) and young adults (19–39 years) at age of diagnosis; there were 12 adolescents and 51 young adults who identified as an SM. In AYA survivors diagnosed between ages 15 and 18, SM identification was not associated with anxiety (unadjusted OR 1.36, p = 0.66) or depression (unadjusted OR 1.08, p = 0.90). In comparison, in AYA survivors diagnosed between ages 19 and 39, SM identification was associated with anxiety (unadjusted OR 2.28, p = 0.007), but not depression (unadjusted OR 1.69, p = 0.09). In other exploratory analyses, the addition of socioeconomic status factors (job status, income, and education) as potential mediators to the adjusted models in Table 2 did not change the magnitude of association between SM identification and depression (adjusted OR 1.26, p = 0.46) or anxiety (adjusted OR 1.80, p = 0.048). The addition of cancer characteristics (years since cancer diagnosis, type of cancer, and type of treatment) to the adjusted models in Table 2 also did not substantively change the associations (adjusted ORdepression 1.47, p = 0.22; adjusted ORanxiety 2.11, p = 0.01).
Discussion
National cancer societies have issued recommendations to reduce health care disparities for SM patients across the cancer care continuum.26 The American Society of Clinical Oncology's recently published strategies include improvement of metrics and increased data collection to address the needs of these patients. Our study examined mental health outcomes and the effect of social support among the unique population of AYA, female, SM cancer survivors. In this cohort, 6% identified as an SM, slightly higher than 2013 estimates of 2.5%–4% in the general population.2 Our study found high prevalence of anxiety and depression; SM identification among AYA, female cancer survivors was associated with higher odds of anxiety, but not depression.
AYA SM survivors had nearly twice the odds of anxiety compared with heterosexual survivors, which was robust to adjustment for demographic characteristics and social support, as well as socioeconomic and cancer characteristics, in exploratory analyses. Prior data in AYA cancer survivors show major, unmet mental health needs,4 but a lack of research on whether needs varied by SM identification. One study observed more SM women reporting current use of antidepressant medication compared with heterosexual women (40.6% vs. 21.0%), but no difference in use of antianxiety medication (8.7% vs. 7.4%).28 While data in older cancer survivors are mixed,10 the present study suggests more mental health morbidity in the young SM population. AYA survivors are challenged by developmental and psychosocial stressors, such as new partnerships, education and employment, finances, and questions of fertility, which are distinct from older cancer survivors.4 SM identification may further augment these stressors, contributing to more mental health symptoms.
Our findings support the need to screen for anxiety symptoms in AYA survivors and in particular those who identify as SM. Clinical guidelines recommend regular surveillance for mental health needs throughout the cancer continuum,26 but implementation of routine screening is highly variable.27 Sexual and gender identification also remains underaddressed despite calls for health care providers to inquire about their patients' sexual orientation and gender identity.28,29 In separate recent surveys, only 26% of oncologists asked patients about their gender and sexual orientation,30 35% of SM patients indicated that their oncologists were aware of their gender and sexual orientation,11 and 58% of SM cancer patients had to bring up their sexual orientation to their physician as a way to correct a mistaken assumption that they were heterosexual.31 The heteronormative framework often used by health care providers causes isolation and feelings of invisibility among SM cancer patients.32 Strategies for enabling a patient to feel more supported by their provider included communicating with patients about their sexual orientation. The National LGBT Cancer Network advocates that addressing sexual orientation in clinical settings allows for optimal cancer care.31 In addition, SM cancer survivors report wanting and needing culturally sensitive mental health referrals.31
We observed no higher odds of depression despite our a priori hypothesis.33 This likely stemmed from limited power, but there are observations that surviving cancer may alternatively contribute to feelings of resilience, which may protect against poor mental health outcomes. Past studies show that AYA cancer survivors endorse a positive impact of cancer in multiple areas of their life, including planning/goals and health competence.34 In this cohort, we did not have measures of resilience to explore its relationship with depression and whether that differed from anxiety.
SM individuals in our cohort reported significantly lower levels of social support compared with heterosexual individuals. Social support was associated with lower odds of both depression and anxiety, but was not found to be an effect modifier, suggesting that social support is protective for these mental health outcomes in AYA, female cancer survivors regardless of SM identification. SM survivors may rely more on nonfamilial contacts for support as many SM individuals have experienced alienation from their families,35 in contrast to heterosexual survivors who are more likely to rely on family.36,37 However, LGBT-specific support groups are not often offered and challenging to find.31 One study suggested that health care providers should screen their SM cancer patients by asking “I know this can be stressful; who do you have who can support you?” to open a dialog about diverse sources of support.11 This study found that having a partner present during delivery of cancer diagnosis was associated with better current self-reported health, demonstrating the importance of including same-sex partners in the cancer care process. The National LGBT Cancer Network recommends development of psychosocial and educational social support groups specifically for SM survivors and caregivers.34 Additional research is needed to develop evidence-based interventions targeting improving social support.
Several limitations should be discussed. Participants were recruited from various health care settings for a study on ovarian function among cancer survivors, and had high rates of college education (>95%), introducing a sampling bias in which generalizability may be limited. Sexual orientation was measured through self-identification, and it is possible that participants did not feel comfortable reporting how they identify. We did not collect gender identity data of participants. In considering that some transgender individuals may have been classified as heterosexual, if they are more likely to have poor mental health outcomes than cisgender individuals, then we would have biased our results toward the null by not capturing gender. Because participants were not asked about the gender of the people they have intimate relationships with, participants with SM sexual behavior may not have identified as an SM. Both would result in misclassification of SM participants as heterosexual, biasing results toward the null. Mental health outcomes were derived from self-reported data regarding symptoms in the last 2 weeks, but were not verified by health care providers, which may have led to inaccurate reporting in both SM and heterosexual participants. Although the proportion of SM participants is reflective of the general population, our sample size of SM participants is low, which may limit power to find differences in depression. Finally, mental health outcomes of AYA male survivors who identify as SM as well as comparisons with AYA individuals without cancer were not captured.
In conclusion, we observed that AYA, female cancer survivors who identify as an SM have nearly two times higher odds of anxiety compared with heterosexual survivors. Social support played a role in mental health outcomes as it was protective of both depression and anxiety in AYA, female cancer survivors. While findings require replication in a larger population-based cohort, current results highlight clinical needs for fidelity in screening for both sexual orientation and mental health issues in cancer survivorship. Provider awareness of higher mental health needs in AYA SM survivors, culturally competent training in the care of this population, inclusion of same-sex partners in care delivery, and providing access to resources such as LGBT support groups are needed to improve the care of AYA survivors who identify as an SM.
Disclaimer
The content is solely the responsibility of the authors and does not necessarily represent the official views of its funders.
Author Disclosure Statement
A.C.D. is employed by and owns stock in bluebird bio, Inc., which had no oversight for funding for this project. The other authors have no conflicts of interest to disclose.
Funding Information
The study was partially supported by the National Institutes of Health, grants R01HD080952 and 1TL1TR001443 of CTSA funding. K.S. is a Dedman Family Scholar in Clinical Care.
References
- 1. American Cancer Society. Cancer treatment & survivorship facts & figures 2016–2017. Atlanta: American Cancer Society; 2017 [Google Scholar]
- 2. Millar B, Patterson P, Desille N. Emerging adulthood and cancer: how unmet needs vary with time-since-treatment. Palliat Support Care. 2010;8:151–8 [DOI] [PubMed] [Google Scholar]
- 3. Keegan TH, Lichtensztajn DY, Kato I, et al. Unmet adolescent and young adult cancer survivors information and service needs: a population-based cancer registry study. J Cancer Surviv. 2012;6:239–50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Barnett M, McDonnell G, DeRosa A, et al. Psychosocial outcomes and interventions among cancer survivors diagnosed during adolescence and young adulthood (AYA): a systematic review. J Cancer Surviv. 2016;10:814–31 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Mayer KH, Bradford JB, Makadon HJ, et al. Sexual and gender minority health: what we know and what needs to be done. Am J Public Health. 2008;98:989–95 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Ward BW, Dahlhamer JM, Galinsky AM, Joestl SS. Sexual orientation and health among U.S. adults: national health interview survey, 2013. Natl Health Stat Report. 2014:1–10 [PubMed] [Google Scholar]
- 7. Quinn GP, Sanchez JA, Sutton SK, et al. Cancer and lesbian, gay, bisexual, transgender/transsexual, and queer/questioning (LGBTQ) populations. CA Cancer J Clin. 2015;65:384–400 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Gates G. How many people are lesbian, gay, bisexual and transgender? The Williams Institute; 2011 [Google Scholar]
- 9. Foundation. L. Coming out with cancer: living after cancer treatment. Austin, TX; 2010
- 10. Gordon JR, Baik SH, Schwartz KTG, Wells KJ. Comparing the mental health of sexual minority and heterosexual cancer survivors: a systematic review. LGBT Health. 2019;6:271–88 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Kamen CS, Smith-Stoner M, Heckler CE, et al. Social support, self-rated health, and lesbian, gay, bisexual, and transgender identity disclosure to cancer care providers. Oncol Nurs Forum. 2015;42:44–51 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Satin JR, Linden W, Phillips MJ. Depression as a predictor of disease progression and mortality in cancer patients: a meta-analysis. Cancer. 2009;115:5349–61 [DOI] [PubMed] [Google Scholar]
- 13. Mausbach BT, Yeung P, Bos T, Irwin SA. Health care costs of depression in patients diagnosed with cancer. Psychooncology. 2018;27:1735–41 [DOI] [PubMed] [Google Scholar]
- 14. Pan X, Sambamoorthi U. Health care expenditures associated with depression in adults with cancer. J Community Support Oncol. 2015;13:240–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Cochran SD, Mays VM, Sullivan JG. Prevalence of mental disorders, psychological distress, and mental health services use among lesbian, gay, and bisexual adults in the United States. J Consult Clin Psychol. 2003;71:53–61 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Freeman EW, Sammel MD, Gracia CR, et al. Follicular phase hormone levels and menstrual bleeding status in the approach to menopause. Fertil Steril. 2005;83:383–92 [DOI] [PubMed] [Google Scholar]
- 17. Groves RM, Mosher WD, Lepkowski JM, Kirgis NG. Planning and development of the continuous National Survey of Family Growth. Vital Health Stat. 1 2009:1–64 [PubMed] [Google Scholar]
- 18. Leisenring WM, Mertens AC, Armstrong GT, et al. Pediatric cancer survivorship research: experience of the Childhood Cancer Survivor Study. J Clin Oncol. 2009;27:2319–27 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Din H. Examining the roles of pregnancy intention and perceived infertility risk on preconception health behaviors to optimize pregnancy among female survivors of adolescent and young adult cancers. San Diego: San Diego State University/University of California; 2020 [Google Scholar]
- 20. Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24:385–96 [PubMed] [Google Scholar]
- 21. Weiss BJ, Garvert DW, Cloitre M. PTSD and trauma-related difficulties in sexual minority women: the impact of perceived social support. J Trauma Stress. 2015;28:563–71 [DOI] [PubMed] [Google Scholar]
- 22. Lin M, Hirschfeld G, Margraf J. Brief form of the Perceived Social Support Questionnaire (F-SozU K-6): validation, norms, and cross-cultural measurement invariance in the USA, Germany, Russia, and China. Psychol Assess. 2019;31:609–21 [DOI] [PubMed] [Google Scholar]
- 23. Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Spitzer RL, Kroenke K, Williams JB, Lowe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166:1092–7 [DOI] [PubMed] [Google Scholar]
- 25. Lumley T, Diehr P, Emerson S, Chen L. The importance of the normality assumption in large public health data sets. Annu Rev Public Health. 2002;23:151–69 [DOI] [PubMed] [Google Scholar]
- 26. Coccia PF, Altman J, Bhatia S, et al. Adolescent and young adult oncology. Clinical practice guidelines in oncology. J Natl Compr Canc Netw. 2012;10:1112–50 [DOI] [PubMed] [Google Scholar]
- 27. Ekwueme DU, Lunsford NB, Khushalani JS, Rim SH. Public health efforts to address mental health conditions among cancer survivors. Am J Public Health. 2019;109:S179-80 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. American Cancer Society. Lesbian, gay, bisexual, transgender, queer (LGBTQ) people with cancer fact sheet. Atlanta, GA: American Cancer Society, Inc. 2020 [Google Scholar]
- 29. Ceres M, Quinn GP, Loscalzo M, Rice D. Cancer screening considerations and cancer screening uptake for lesbian, gay, bisexual, and transgender persons. Semin Oncol Nurs. 2018;34:37–51 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Shetty G, Sanchez JA, Lancaster JM, et al. Oncology healthcare providers' knowledge, attitudes, and practice behaviors regarding LGBT health. Patient Educ Couns. 2016;99:1676–84 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Margolies L, Scout NFN. LGBT Patient-centered outcomes: cancer survivors teach us how to improve care for all. New York: The National LGBT Cancer Network; April 2013. Accessed July22, 2020 from: www.cancer-network.org/patient_centered_outcomes
- 32. Cathcart-Rake EJ, Breitkopf CR, Kaur J, et al. Teaching health-care providers to query patients with cancer about sexual and gender minority (SGM) status and sexual health. Am J Hosp Palliat Care. 2019;36:533–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Harper MA, Espeland MA, Dugan E, et al. Racial disparity in pregnancy-related mortality following a live birth outcome. Ann Epidemiol. 2004;14:274–9 [DOI] [PubMed] [Google Scholar]
- 34. Bellizzi KM, Smith A, Schmidt S, et al. Positive and negative psychosocial impact of being diagnosed with cancer as an adolescent or young adult. Cancer. 2012;118:5155–62 [DOI] [PubMed] [Google Scholar]
- 35. Ryan C, Huebner D, Diaz RM, Sanchez J. Family rejection as a predictor of negative health outcomes in white and Latino lesbian, gay, and bisexual young adults. Pediatrics. 2009;123:346–52 [DOI] [PubMed] [Google Scholar]
- 36. Kamen C. Lesbian, gay, bisexual, and transgender (LGBT) survivorship. Semin Oncol Nurs. 2018;34:52–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Badger T, Segrin C, Dorros SM, et al. Depression and anxiety in women with breast cancer and their partners. Nurs Res. 2007;56:44–53 [DOI] [PubMed] [Google Scholar]