Abstract
Background: During a pandemic, women may be especially vulnerable to secondary health problems driven by its social and economic effects. We examined the relationship between changes in health-related socioeconomic risks (HRSRs) and mental health.
Materials and Methods: A cross-sectional survey of 3,200 women aged 18–90 years was conducted in April 2020 using a quota-based sample from a national panel (88% cooperation rate). Patterns of change in HRSRs (food insecurity, housing instability, interpersonal violence, and difficulties with utilities and transportation) were described. Weighted, multivariate logistic regression was used to model the odds of depression, anxiety, and traumatic stress symptoms among those with and without incident or worsening HRSRs.
Results: More than 40% of women had one or more prepandemic HRSRs. In the early pandemic phase, 49% of all women, including 29% with no prepandemic HRSRs, had experienced incident or worsening HRSRs. By April 2020, the rates of depression and anxiety were twice that of prepandemic benchmarks (29%); 17% of women had symptoms of traumatic stress. The odds of depression, anxiety, and posttraumatic stress symptoms were two to three times higher among women who reported at least one incident or worsening HRSR; this finding was similar for women with and without prepandemic HRSRs.
Conclusions: Increased health-related socioeconomic vulnerability among U.S. women early in the coronavirus disease 2019 (COVID-19) pandemic was prevalent and associated with alarmingly high rates of mental health problems. Pandemic-related mental health needs are likely to be much greater than currently available resources, especially for vulnerable women.
Keywords: COVID-19, disparities, mental health, health behaviors, social determinants of health
Introduction
Exposure to large-scale crises has been shown to cause both incident economic and interpersonal strain and to exacerbate poor socioeconomic conditions of already vulnerable women.1 During a pandemic, women may be especially vulnerable to secondary health problems driven by social and economic effects of the crisis.1,2
Secondary health effects of the coronavirus disease 2019 (COVID-19) pandemic may include physical and mental health conditions occurring among those affected, but not necessarily infected, by the novel coronavirus. Policymakers and advocates are calling for women's health research that assesses early phase socioeconomic changes resulting from the COVID-19 pandemic and the relationship of these changes to secondary health effects. To date, few large-scale studies present findings stratified by gender and, those that do, tend to focus on women of reproductive age.3
High rates of stress-related conditions, including anxiety, depression, distress and related health behaviors such as increased alcohol and tobacco use have been reported in several early COVID-19 studies.4–6 Higher vulnerability among women to secondary health effects of the COVID-19 pandemic may be driven, in part, by endemic factors such as a higher percentage of women in health, human, social services, and other essential worker roles7,8; gender-based disparities in wages; intimate partner and other interpersonal violence (IPV); limited control over reproduction; and a disproportionate share of responsibility for child rearing and other family caregiving responsibilities.9,10 A March 2020 poll, self-published by the Kaiser Family Foundation, found that more women than men were worried about the loss of income, their ability to afford COVID-19 testing or treatment if needed, and risk of exposure due to inability to afford staying home for work.11
In contrast to gender, pandemic-related socioeconomic vulnerabilities experienced by women are modifiable. Pandemic-related vulnerabilities, including food insecurity, housing and utility needs, transportation difficulties, and interpersonal safety, have been identified by the U.S. Centers for Medicare & Medicaid Services (CMS) and others as modifiable risk factors that should be assessed and addressed in the context of medical care.12–14 Studies preceding the COVID-19 pandemic find a higher prevalence of health-related socioeconomic risk factors (HRSRs), especially food insecurity and intimate partner violence, among women—especially women with children—than men.15–17 HRSRs have also been associated with preventable physical and mental illness12,18 and high health care costs due to higher emergency and inpatient utilization.13
We report results from the National U.S. Women's Health COVID-19 Study to describe changes in HRSRs in the early pandemic phase and to assess the relationship between these changes and secondary mental health effects of COVID-19. We hypothesized that both incident and worsening socioeconomic vulnerability would be associated with poorer mental health outcomes. This analysis informs near-term decisions about COVID-19 response and recovery, as well as long-term efforts to advance equitable interventions to optimize women's health during the pandemic and its aftermath.
Materials and Methods
A national sample of English-speaking women aged ≥18 years was recruited from a continuously refreshed research panel maintained by Opinions 4 Good (Op4G), a survey research firm. Op4G's panel is composed of a diverse group of 350,000 U.S. residents and has been used in prior academic studies of health.19,20 Panelists are recruited to studies via email and complete all surveys online. Op4G maintains data (e.g., sociodemographic characteristics, health conditions) for each participant to facilitate targeted recruitment of eligible individuals.
Participants for this study were recruited using a nested quota sampling strategy (Appendix Table AT1), stratified by race/ethnicity, age, and educational attainment. East/Southeast Asian women (Chinese, Filipino, Japanese, Korean, and/or Vietnamese) were oversampled. The distribution of age and education reflected the overall 2018 U.S. population of women aged ≥18.21
In contrast to online recruitment strategies that target unknown participants via links posted on websites, email blasts, or social media groups,22 recruitment via Op4G allowed us to quickly enroll a national sample of eligible individuals with known sociodemographic and health characteristics to assess early pandemic effects. Emails were sent to panel registrants with a personalized, one-time survey link from Op4G. Of 3,634 eligible panelists contacted, 3,200 completed a self-administered, web-based survey between April 10 and 24, 2020, yielding an 88% cooperation rate.23 Informed consent was documented digitally and participants received a small incentive for completing the survey. The University of Chicago Institutional Review Board approved the protocol.
Study design and measures
Validated survey measures were used whenever possible and novel measures were adapted from validated measures. The survey instrument underwent three rounds of testing by the research team, which included coinvestigators with extensive experience in survey research. Participants were permitted to skip any survey question, yet, item nonresponse was low. Of 152 survey questions, the mean percentage missing was 0.4% (range 0%–2.5%).
The survey queried the following: (1) sociodemographic characteristics, (2) prepandemic socioeconomic vulnerability, measured by assessing the HRSRs defined by the Centers for Medicare & Medicaid Services Accountable Health Communities (AHC) screening tool24 (food insecurity, housing stability, utilities difficulties, transportation difficulties, and IPV), (3) pandemic-related changes in HRSRs (adapted from the Accountable Health Communities screening tool), and (4) mental health conditions, including general anxiety (General Anxiety Disorder-7),25 depression (Patient Health Questionnaire-2),26 and traumatic stress symptoms (the two items from the Modified Posttraumatic Stress Disorder Checklist that were most commonly endorsed by U.S. adults surveyed after the 9/11 terrorist attacks: feeling very upset and disturbing thoughts).27
Race and ethnicity were determined using two questions: “What race do you consider yourself to be? Please select one or more” (white, black or African American, American Indian or Alaskan Native, Asian Indian, Chinese, Filipino, Japanese, Korean, Vietnamese, other Asian, Pacific Islander, or other) and “Do you consider yourself to be Hispanic, Latino/a/x or of Spanish origin?” (yes or no). Women who selected Chinese, Filipino, Japanese, Korean, and/or Vietnamese were categorized as East/Southeast Asian (an Asian subgroup that has experienced COVID-related targeting and violence).28 Those who selected other race, multiple races, Asian Indian, other Asians, American Indian or Alaskan Native, and Pacific Islander were categorized as “Other.”
For each of the HRSRs, prepandemic status was categorized as yes or no using the AHC screening tool instructions.24 Change in food insecurity was assessed using a single question about change in worry about “food running out before you got money to buy more” with a 5-point Likert scale (much more to much less) and recategorized as more, same, or less. Change in transportation was assessed using a single question about change in ease of getting transportation with a 5-point Likert scale (much easier to much harder) and recategorized as harder, same, or easier. Changes in housing and utility security were assessed by capturing current housing and utility security and comparing it to housing and utility security prepandemic.
Prepandemic IPV status was determined by summing the responses (5-point Likert scale, never = 1 point to frequently = 5 points) to each of four domains (physically hurt, insulted or talked down to, threatened with harm, screamed, or cursed at). Per the AHC instructions,24 individuals scoring fewer than 11 points were classified as negative for IPV and those scoring 11 or more points were classified as screening positive for IPV. It is important to note that using this conservative scoring system, adapted by CMS from the Hurt, Insult, Threaten, and Scream (HITS) intimate partner violence screening tool,24 an individual could screen negative for IPV even if she, for example, responded that another person frequently physically hurt (5 points) and sometimes threatened her (3 points).
Change in IPV was captured for each of the four domains of IPV using a 5-point Likert scale (much more to much less); a mean change score was calculated and categorized as more, same, or less. Individuals who screened negative for prepandemic IPV (score <11) but who indicated experiencing violence in one or more domains could have a mean change score indicating less violence in the early phase of the pandemic.
“Incident HRSRs” included any HRSR(s) that a person acquired in the early pandemic phase. The term “socioeconomically vulnerable” refers to all women indicating one or more HRSR.
Statistical analysis
Calibration via the raking-ratio method was used to generate pseudo design-based weights, so marginal distributions for age group, race, education, income category, and region matched those of 2018 population estimates. All analyses utilized the weights unless otherwise stated; variance estimates accounting for the raking procedure were obtained. All analyses were stratified by prepandemic HRSR status (0 HRSRs or 1+ HRSRs) due to differing patterns of change in HRSRs. Sociodemographic, economic and household characteristics, and health of the sample were described, as were patterns of incident and worsening HRSRs and improved HRSRs.
We described rates of depression, anxiety, and traumatic stress symptoms, comparing these rates to national prepandemic benchmarks and using bivariate logistic regression to model the odds of these outcomes by prepandemic HRSR status. Multivariate logistic regression was used to model the odds of depression, anxiety, and traumatic stress symptoms, (1) given any incident or worsening HRSRs (yes/no), (2) for each additional incident or worsening HRSRs (range 0–5), and (3) for each individual incident or worsening HRSRs (yes/no), controlling for all other incident or worsening HRSRs. Covariates included sociodemographic, economic, household, and health characteristics. Model results are presented as odds ratios with 95% confidence intervals (CIs). CIs are not adjusted for multiple testing. All analyses used Stata statistical software, version 16.1.
Results
Sample characteristics
Table 1 summarizes the characteristics of survey respondents compared to population benchmarks. Demographic characteristics of the weighted sample were similar to prepandemic population estimates, although fewer women in the present study were living alone.
Table 1.
Population Benchmarks and Weighted Sample Characteristics Stratified by Prepandemic Health-Related Socioeconomic Risk (HRSRs) (N = 3,176)a,b
| No prepandemic HRSRs (n = 1,601) |
≥1 prepandemic HRSR (n = 1,575) |
Total (weighted sample) |
Prepandemic population estimatec–h |
|
|---|---|---|---|---|
| % | % | % | % | |
| Sociodemographic characteristics | ||||
| Age | ||||
| 18–44 years | 35.1 | 56.8 | 44.6 | 44.6 |
| 45–64 years | 35.2 | 30.2 | 33.0 | 33.0 |
| 65 or more years | 29.8 | 13.0 | 22.4 | 22.4 |
| Race | ||||
| White | 79.2 | 65.9 | 73.4 | 71.9 |
| Black | 9.6 | 17.0 | 12.8 | 13.1 |
| East or Southeast Asian | 5.0 | 6.9 | 5.8 | 3.8 |
| Other | 6.2 | 10.2 | 8.0 | 11.0 |
| Hispanic | ||||
| Yes | 11.0 | 17.6 | 13.9 | 17.8 |
| No | 89.0 | 82.4 | 86.1 | 82.1 |
| Marital status | ||||
| Married or partnered | 66.8 | 55.8 | 62.0 | 53.6 |
| Single, divorced or widowed | 33.3 | 44.2 | 38.1 | 46.4 |
| Economic characteristics | ||||
| Income | ||||
| Less than $25,000 | 10.7 | 31.1 | 19.6 | 19.6 |
| $25,000–$49,999 | 18.0 | 25.6 | 21.3 | 21.3 |
| $50,000–$99,999 | 32.1 | 27.3 | 30.0 | 30.0 |
| $100,000 or more | 39.3 | 16.0 | 29.1 | 29.2 |
| Educational attainment | ||||
| High school or less | 30.6 | 45.7 | 37.2 | 37.2 |
| More than high school | 69.4 | 54.3 | 62.8 | 62.8 |
| Household characteristics | ||||
| Number in household | ||||
| Lives alone | 15.8 | 15.2 | 15.5 | 28.4 |
| Self +1 | 40.0 | 27.2 | 34.4 | 34.5 |
| Self +2 or more | 44.1 | 57.6 | 50.0 | 37.1 |
| Number of household children | ||||
| No children | 68.0 | 52.2 | 61.1 | 61.8 |
| 1 child | 13.5 | 22.6 | 17.4 | 15.0 |
| 2 or more children | 18.5 | 25.2 | 21.5 | 23.1 |
| Region | ||||
| Midwest | 22.4 | 18.4 | 20.7 | 20.8 |
| Northeast | 18.1 | 15.7 | 17.0 | 17.1 |
| South | 37.8 | 39.3 | 38.5 | 38.3 |
| West | 21.6 | 26.6 | 23.8 | 23.9 |
| Health characteristics | ||||
| Self-rated overall health | ||||
| Fair or poor | 13.9 | 26.3 | 19.3 | 19.5 |
| Good | 36.6 | 38.5 | 37.4 | 32.0 |
| Very good or excellent | 49.5 | 35.3 | 43.3 | 48.6 |
| Number of comorbidities | ||||
| 0 | 58.1 | 48.1 | 53.7 | — |
| 1 | 29.1 | 29.8 | 29.4 | — |
| 2 | 8.7 | 12.5 | 10.4 | — |
| 3 or more | 4.2 | 9.7 | 6.6 | — |
| Health-related socioeconomic risks | ||||
| Food | — | 85.0 | 37.2 | 41.8, 39.9 |
| Transportation | — | 36.1 | 15.8 | 20.3 |
| Utilities | — | 23.8 | 10.4 | 12.5 |
| Housing | — | 23.1 | 10.1 | 17.3 |
| IPV | — | 19.9 | 8.7 | 6.3 |
| Number of health-related socioeconomic risks | ||||
| 0 risks | 100.0 | 0.0 | 56.3 | 37.2 |
| 1 risk | 0.0 | 49.5 | 21.6 | 28.8 |
| 2 or more risks | 0.0 | 50.5 | 22.1 | 34.0 |
Women with no prepandemic HRSRs and women with ≥1 HRSRs were significantly different (p < 0.05) on all characteristics presented in this table.
Twenty four out of 3,200 women surveyed were missing data for the income variable used to generate calibration weights. Only those 3,176 for whom weights could be generated were included in this analysis. Ns for unweighted analyses may not total 3,176 due to missing data.
Calibration weights were utilized and were generated based on the following variables: age group, race, education, income, and prepandemic region.
Age, race, income, educational attainment, number in household. Benchmark data source: 2018 American Community Survey 1-year estimates retrieved from data.census.gov.21
Marital status, number of household children, region, self-rated overall health. Benchmark data source: 2018 Behavioral Risk Factor Surveillance System Data.29
Health-related socioeconomic risks: food, transportation, utilities. Benchmark data source: De Marchis et al.30
Health-related socioeconomic risks: food. Benchmark data source: Flood et al.31
Health-related socioeconomic risks: housing, number of health-related socioeconomic risks. Benchmark data source: Unpublished data provided by De Marchis May 13, 2020 and June 8, 2020.
Health-related socioeconomic risks: IPV. Benchmark data source: Chen et al.32
HRSRs, health-related socioeconomic risks; IPV, interpersonal violence.
More than 40% of participants, including 16% of women with a household income higher than $100K, indicated one or more HRSR in the 12 months prepandemic. Women with prepandemic socioeconomic vulnerability were more likely to be younger, single, nonwhite, Hispanic, have lower income but with more household members, and living in the western United States (p < 0.05). This group also reported poorer overall health (p < 0.05). Food insecurity was the most prevalent prepandemic HRSR (37% overall, 85% of those with any HRSR, 18% of people with a household income higher than $100K) and 22% of women indicated two or more prepandemic HRSRs. Nine percent of women screened positive for IPV in the 12 months before the pandemic.
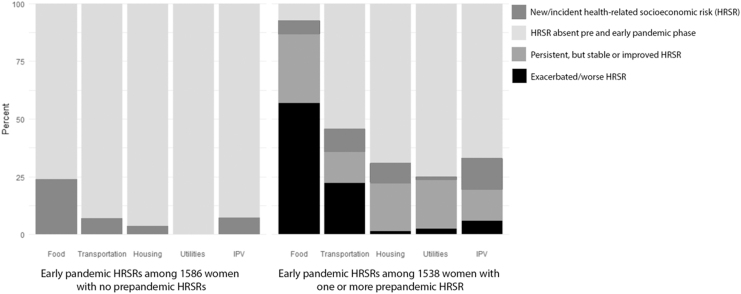
Overall, 49% of all women experienced incident or worsening HRSRs during the early phase of the pandemic, including 29% of women with no prepandemic HRSRs (Fig. 1). Forty percent of women reported incident or worsening food insecurity, 17% reported transportation difficulties, 13% reported IPV, 6% reported housing insecurity, and 2% reported utility difficulties.
FIG. 1.
Frequencies of incident, persistent, or worsening health-related socioeconomic risks (HRSRs) during the early phase of the pandemic stratified by prepandemic HRSR status (no or one or more HRSR) (N = 3,124). HRSRs, health-related socioeconomic risks.
Women with no prepandemic HRSRs
Among the 29% of these women who experienced incident HRSRs in the early pandemic phase, 78% became food insecure, 24% screened positive for IPV, 21% acquired difficulties with transportation, 11% developed housing instability, and fewer than 1% acquired difficulties with utilities (Fig. 1). Of women with no prepandemic HRSRs who experienced IPV in the early pandemic phase, nearly all reported an increase in being screamed or cursed at (99%) and experiencing insults or being talked down to (97%), 55% reported being threatened with harm, and 54% reported physical violence.
Women with one or more prepandemic HRSRs
In contrast to about a quarter of women with no prepandemic HRSRs, three quarters of the women with prepandemic HRSRs experienced incident or worsening risks in the early phase of the pandemic and 38% experienced two or more (Fig. 1). Again, food insecurity was the condition most likely to be exacerbated in this group: more than half of women (56%) with prepandemic HRSRs experienced worsening food insecurity in the early pandemic phase and 7% became newly food insecure.
Among women with any prepandemic HRSR, 13% had incident and 6% experienced increased IPV in the early pandemic phase. Of the subgroup that screened positive for prepandemic IPV, 32% experienced increased levels and 44% experienced persistent violence in the early pandemic phase. The patterns of incident or worsening verbal and physical violence were similar to those among women with no prepandemic HRSRs: 82% reported an increase in being screamed or cursed at, 89% reported an increase in insults or being talked down to, 61% reported an increase in being threatened with harm, and 56% reported an increase in physical violence.
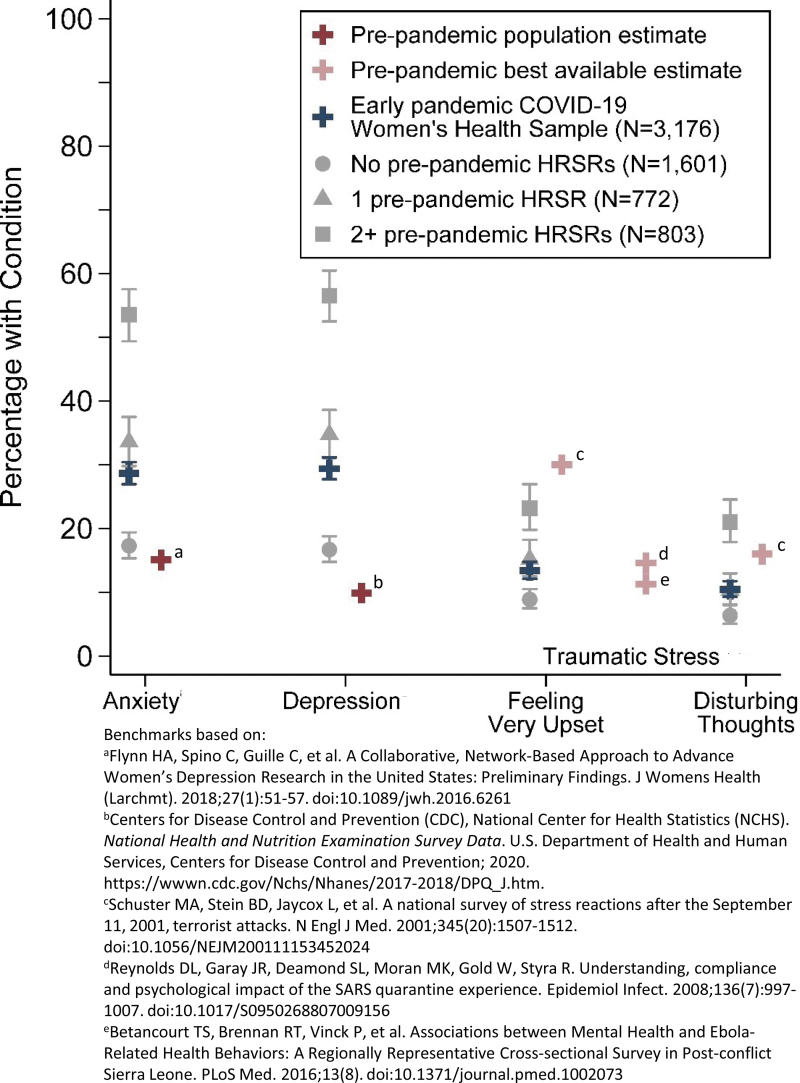
Mental health outcomes
Rates of depression (29%) and anxiety (29%) in the early phase of the pandemic were two to three times prepandemic population estimates33,34 (Fig. 2); 21% of women screened positive for clinical levels of both conditions. More than one in six women (17%) endorsed one or both traumatic stress symptoms. One in 10 women reported recurrent disturbing thoughts, compared to 16% of a national sample surveyed using the same measure soon after the September 11, 2001 attacks.27 Using other measures, studies of the severe acute respiratory syndrome (SARS) and Ebola epidemics found traumatic stress rates of 15% and 11%, respectively.35,36
FIG. 2.
Anxiety, depression, and posttraumatic health symptoms by prepandemic health-related socioeconomic risks compared to national or best available prepandemic benchmarks (N = 3,176).
The odds of depression, anxiety, and posttraumatic stress in the early phase of the pandemic were all significantly higher among women with prepandemic HRSRs (p < 0.01). For every additional prepandemic HRSR, the odds of early pandemic depression increased by a factor of 1.9 (95% CI: 1.8–2.1), the odds of anxiety increased by 1.9 (95% CI: 1.8–2.1), and the odds of traumatic stress symptoms increased by 1.5 (95% CI: 1.4–1.6).
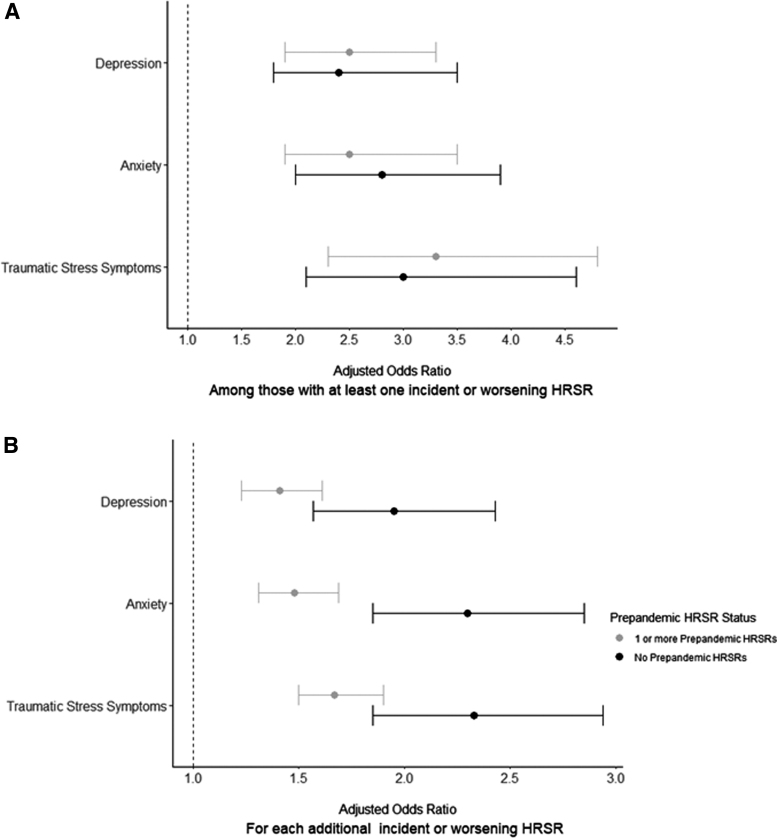
Figure 3 shows the adjusted odds of depression, anxiety, and traumatic stress symptoms among women with at least one incident or worsening HRSR versus none (panel A) and for each additional incident or worsening HRSR (panel B). The odds of depression, anxiety, and posttraumatic stress symptoms were two to three times higher among women who reported at least one incident or worsening HRSR; this finding was similar for women with and without prepandemic HRSRs.
FIG. 3.
Adjusted odds of depression, anxiety, and traumatic stress symptoms (A) among those with at least one incident or worsening health-related socioeconomic risk (HRSR) and (B) for each additional incident or worsening HRSR during the early phase of the pandemic (N = 3,124). Models adjusted for age, race/ethnicity, marital status, income, education, number of people in household, number of children in household, self-reported health and comorbidities.
Likewise, controlling for all other incident or worsening HRSRs, incident or worsening food insecurity—the most common incident condition—significantly increased the odds of depression, anxiety, and traumatic stress among women with and without prepandemic HRSRs (Table 2). Incident IPV significantly increased the odds of depression and traumatic stress, but not anxiety among women without prepandemic HRSRs. Among women with prepandemic HRSRs, incident or worsening IPV was not significantly associated with mental health problems.
Table 2.
Odds of Depression, Anxiety, and Traumatic Stress for Worsening Individual Health-Related Socioeconomic Risks
| No prepandemic health-related socioeconomic risks |
One or more prepandemic health-related socioeconomic risks |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Depression |
Anxiety |
Traumatic stress |
Depression |
Anxiety |
Traumatic stress |
|||||||
| aOR | 95% CI | aOR | 95% CI | aOR | 95% CI | aOR | 95% CI | aOR | 95% CI | aOR | 95% CI | |
| Health-related socioeconomic risks | ||||||||||||
| Food insecurity | 2.0 | 1.4–3.0 | 2.7 | 1.9–3.7 | 2.5 | 1.6–3.8 | 1.7 | 1.3–2.2 | 1.9 | 1.4–2.5 | 1.6 | 1.1–2.2 |
| Housing insecurity | 2.7 | 1.3–5.8 | 4.1 | 1.9–8.9 | 1.3 | 0.6–2.9 | 0.7 | 0.4–1.0 | 1.5 | 0.9–2.2 | 1.3 | 0.9–2.0 |
| Transportation difficulties | 1.4 | 0.8–2.6 | 1.8 | 1.0–3.1 | 2.5 | 1.4–4.3 | 2.0 | 1.5–2.7 | 2.0 | 1.5–2.6 | 1.9 | 1.4–2.6 |
| Utilities difficulties | — | — | — | — | — | — | 1.2 | 0.5–2.6 | 1.1 | 0.6–2.1 | 2.9 | 1.5–5.5 |
| IPV | 1.9 | 1.0–3.4 | 1.4 | 0.8–2.4 | 2.6 | 1.5–4.8 | 1.1 | 0.8–1.6 | 0.8 | 0.6–1.1 | 1.5 | 1.0–2.1 |
Models adjusted for age, race/ethnicity, marital status, income, education, number of people in household, number of children in household, self-reported health, and comorbidities.
aOR, adjusted odds ratio; CI, confidence interval.
Women with early pandemic improvement in HRSRs
Nearly a third (32%) of women with prepandemic HRSRs experienced an improvement in one or more HRSR during the early pandemic phase, most commonly restoration of utility service (13%) or improvement in one or more domains of IPV (also 13%). However, three quarters (76%) who experienced any improvement also experienced incident or worsening HRSRs in other domains. When compared to women who experienced only worsening HRSRs, those who reported only improvement had significantly lower odds of depression (adjusted odds ratio [aOR] 0.5, 95% CI: 0.3–0.8) and stress (aOR 0.5, 95% CI: 0.3–0.9). Anxiety followed a similar trend, but the finding was not significant (aOR 0.6, 95% CI: 0.4–1.1).
Discussion
High rates of anxiety, depression, and traumatic stress among U.S. women, seen in this study during the early phase of the COVID-19 pandemic, have also been observed among a diversity of populations globally.4,37 To our knowledge, however, this is the first study to link these secondary mental health effects among women to incident and worsening HRSRs, including IPV. Based on a national panel-based sample of U.S. women aged 18–90 surveyed in April 2020, we find a dose–response relationship between the number of prepandemic HRSRs and rates of depression, anxiety, and traumatic stress. More than a quarter of U.S. women with no prepandemic HRSRs, and more than three quarters of those with one or more, had new or worsening HRSRs in the early pandemic phase. Among these women, the adjusted odds of anxiety, depression, and traumatic stress were two- to threefold higher.
These findings corroborate concerns that women's pandemic-related mental health needs are likely to be much greater than can be addressed with currently available resources.38 Attention to modifiable HRSRs could yield downstream mental and physical health benefits for women, their dependents, and their communities.18,39
The 53% food insecurity rate observed among U.S. women in our April 2020 study is higher than rates reported by other early pandemic studies that are not disaggregated by gender: 21% in a U.S. population of 18–64 years in late March-early April40 and 15.4% in a general U.S. population in mid-May 2020.41 It is possible that food insecurity rates may have declined over time as pandemic-driven emergency food policies and distribution ramped up. One study of low income households (<250% of federal poverty level) reported early pandemic food insecurity rates disaggregated by gender. They found similarly high rates of low or marginal food insecurity overall (64%) but no significant gender differences.42
Higher food insecurity rates in our sample compared to other studies may also be attributable to measurement. While comparison studies used multi-item (6- and 18-item) United States Department of Agriculture (USDA) measures,43,44 we used the CMS-recommended two-item Hunger Vital Sign (HVS) screener. The HVS can overestimate food insecurity by classifying people as food insecure who would be classified using the longer measures as “marginally” food insecure.45
Not surprisingly, patterns of early pandemic phase socioeconomic changes were different for women with and without prepandemic HRSRs. Although women with no prepandemic HRSRs saw less change overall, nearly one in four screened positive for food insecurity by April 2020. Among women with prepandemic HRSRs, more than half of the 85% with preexisting food insecurity were faring even worse by April 2020 and an additional 7% of these women became food insecure. To our knowledge, similar data are not available for men, although an international meta-analysis of prepandemic food insecurity rates by gender found that female-led households were 75% more likely to be food insecure than male-led households.16
Incident and worsening food insecurity, modifiable conditions in a nation that wastes an estimated 133 billion pounds of food per month,46 were independently associated with a higher risk of secondary mental health conditions. This finding is consistent with prior studies.47–50 Extending Supplemental Nutrition Assistance Plan benefits to food insecure women during the pandemic is estimated to cost $129/person/month.51 In contrast, a 2011 study estimated that the annual direct health care costs for treating depression or traumatic stress exceeded $10,000 per person.52
Data from police and domestic violence support agency records indicate alarming upward trends in violence against women during the COVID-19 pandemic53–56 as has been seen in prior large-scale disasters.2,57–60 In our study, the baseline rate among women was similar to prepandemic estimates for IPV (9% compared to 7% in a national, 10 site clinical study using the same measure)30 (EH DeMarchis, UCSF, personal communication 5/13/20). These rates more than doubled in the early pandemic phase, similar to other studies.53,54
We find no comparable studies of early pandemic changes in IPV that stratify results by gender. One U.S. study led by University of Texas researchers surveyed a convenience sample of men and women in April 2020 using social media and email lists to query intimate partner violence, specifically.61 Among 1,759 people (mean age 42, standard deviation 13 years) with a current intimate partner (our analysis was not limited by partner status), the prevalence of IPV was 23% among men and 16% among women.
In our study, more than one in twenty women with no prepandemic HRSRs screened newly positive for IPV; more than half of these were experiencing physical violence. Rates of incident IPV among women with prepandemic HRSRs were double that of women with no prepandemic HRSRs and most women who screened positive for prepandemic IPV reported either worsening or no change in the early pandemic phase. Interestingly, the impact of incident or worsening IPV on mental health differed for women with and without prepandemic HRSRs. This finding may be partially explained, as reported by others,62 by very high rates of poor mental health among women with prepandemic IPV. In our study, two-thirds of women with prepandemic IPV had depression.
This study fills a gap in knowledge about positive change in HRSRs among women in the early pandemic phase. About a third of women with prepandemic HRSRs saw improvement in one or more domain. Consistent with local and state policies requiring or encouraging utility companies to maintain or restore service during shelter in place orders,63 almost no women reported loss of utilities and 30% of women with prepandemic utility difficulties reported restoration or cessation of threats to terminate service.
Nearly a quarter of women who screened positive for IPV prepandemic also reported some improvement. Because the IPV assessment included violence perpetrated by people outside the home, some women may have been protected by shelter in place, work from home, and social distancing policies. The April 2020 University of Texas study assessed change in severity of intimate partner violence among people who screened positive.61 Rates of diminished severity were similar among women and men (32% and 27%, respectively) and on a par with the rate of improvement in IPV found in our cohort. Improvement in HRSRs appeared to be somewhat protective against depression and traumatic stress; similar improvements in depressive symptoms and other mental health outcomes have been observed in intervention studies designed to address or mitigate HRSRs.18,64,65
Findings should be interpreted in light of limitations. Although the sample is, in many ways, representative of women in the United States national population—and rates of mental health problems in this sample are similar to those reported by other early pandemic studies—generalizability may be limited without a probability sample. To assess HRSRs, we elected to use the policy and practice-relevant measures advocated by the CMS.24 The two-item food insecurity screener may have contributed to higher estimates of food insecurity in our sample than estimates from studies using the more specific multi-item measures.45 The IPV measure was adapted by CMS from the HITS tool,66 which was designed specifically to assess intimate partner violence, a narrower construct. Estimates of IPV generated by the adapted HITS measure should be interpreted cautiously in comparison to estimates of intimate partner violence from other studies.
Our cross-sectional study design is also subject to recall bias; people suffering incident or worsening conditions in the early pandemic phase may recall their prepandemic status differently compared to people who experienced little change or improvement in conditions. Recall bias may have resulted in over- or underestimation of change in HRSRs. Change in HRSRs was assessed using novel measures developed for this study by adapting the existing AHC screening tool survey items. Due to the unique time sensitivity of this survey, these measures did not undergo formal psychometric testing. Finally, we are unable to make gender-based comparisons, as only women were surveyed and few contemporaneous surveys report data disaggregated by gender.
This study addresses calls for empirical evidence about women's health in the context of the COVID-19 pandemic and, specifically, the effects of pandemic-related socioeconomic changes on secondary health outcomes among women.10,67,68 The roles of women as mothers, informal caregivers, and essential health care and other workers point to the societal importance of women's mental health for the next phases of the COVID-19 pandemic and other crises of similar magnitude.
The effectiveness and trajectory of pandemic response and recovery efforts—including testing and treatment, self-isolation and quarantine, contact tracing and, hopefully, vaccination—will be profoundly determined by the health and safety of all women. Very high rates of food insecurity and IPV among U.S. women in the early phase of the COVID-19 pandemic should sound alarms across all health, human, social services, and public safety sectors.13,24 Efforts to study and implement HRSR assessment and mitigation strategies were well underway in the United States before the COVID-19 pandemic.12,39,69,70 Intervening to prevent and mitigate these conditions in the pandemic context is feasible and will help stem a rapidly evolving mental health crisis among U.S. women and those who depend on them.
Acknowledgments
We are grateful to Emilia De Marchis, Caroline Fichtenberg, and Laura Gottlieb at the UCSF Social Interventions Research and Evaluation Network (SIREN) for sharing results from referenced research for comparative analysis. We also acknowledge L. Philip Schumm, Victoria Winslow, and Charlie Fuller for their assistance with the development of this article. The survey for the 2020 U.S. National Women's Health COVID19 Study was developed at The University of Chicago by S.T.L., K.E.D., K.B., S.H., N.K.L., J.A.M., E.P., and L. Philip Schumm, MA, M.T., K.E.W., E.L.
Appendix
Appendix Table A1.
Quota Sample Distribution
| Race and age (years) |
Total | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| White |
African American/Black |
East/Southeast Asian |
Other |
||||||||||
| 18–44 | 45–64 | 65+ | 18–44 | 45–64 | 65+ | 18–44 | 45–64 | 65+ | 18–44 | 45–64 | 65+ | ||
| Education | |||||||||||||
| High school or less | 328 | 255 | 146 | 82 | 64 | 36 | 55 | 43 | 24 | 82 | 64 | 36 | 1,216 |
| More than high school | 536 | 417 | 238 | 134 | 104 | 60 | 89 | 69 | 40 | 134 | 104 | 60 | 1,984 |
| Total | 864 | 672 | 384 | 216 | 168 | 96 | 144 | 112 | 64 | 216 | 168 | 96 | 3,200 |
n, number of respondents in each cell.
Authors' Contributions
S.T.L. led conception and design of this study, acquisition of data, made substantial contributions to analysis and interpretation of data, led the writing of the article and provided material, administrative, and supervisory support. J.A.M. contributed substantially to the design of the work, led the data analysis, and interpretation and critically reviewed the article. K.B. contributed to conception and design of this study, as well as acquisition, analysis, and interpretation of data and editing of the article. K.E.D. contributed to conception and design of this study, acquisition, analysis, and interpretation of data, and drafting and editing of the article. S.H. contributed to the conception and design of this study, interpretation of data, and editing of the article. S.K. contributed to the literature review, writing, and editing of the article. N.K.L. contributed to the conception and design of this study, interpretation of data, and editing of the article. E.P. contributed to the conception and design of this study, as well as acquisition and interpretation of data, literature review, and editing of the article. M.T. contributed to study design, literature review, writing and editing of the article. M.V. contributed to the analysis of data and to the writing and editing of the article. K.E.W. contributed to the analysis and interpretation of data and to the writing and editing of the article. E.L. co-led conception and design of this study. He also contributed to the acquisition and interpretation of the data, writing, and editing of the article, and provided material support. All authors approved the final version of the submitted article.
Author Disclosure Statement
S.T.L. is founder and co-owner of NowPow, LLC. Neither the University of Chicago nor the University of Chicago Medicine is endorsing or promoting NowPow or its business, products, or services. S.T.L. and her spouse own equity in Glenbervie Health, LLC, and health care-related stocks and mutual funds managed by third parties. E.L. receives research funding from AbbVie and Arsenal Bio to perform translational ovarian cancer research that is completely unrelated to this study. All other authors report no disclosures.
Funding Statement
Research reported in this publication was supported by 5R01AG064949, 5R01MD012630, R21CA226726 (S.T.L., K.B., K.E.D., J.A.M., E.P., K.E.W.) and by 5R01HD097171-02 (S.H.). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. Material support for this survey was provided by the Joseph B. De Lee Endowment to the University of Chicago Department of Obstetrics and Gynecology.
References
- 1. Lee YS, Behn M, Rexrode KM. Women's health in times of emergency: We must take action. J Womens Health (Larchmt). September 1, 2020. [Epub ahead of print]; DOI: 10.1089/jwh.2020.8600 [DOI] [PubMed] [Google Scholar]
- 2. Wenham C, Smith J, Davies SE, et al. Women are most affected by pandemics—Lessons from past outbreaks. Nature 2020;583:194–198 [DOI] [PubMed] [Google Scholar]
- 3. Noursi S. COVID-19 and Women's Health. National Institutes of Health: Office of Research on Women's Health. Available at: https://orwh.od.nih.gov/about/director/messages/guest-blog-covid-19-and-womens-health Accessed October1, 2020
- 4. Ettman CK, Abdalla SM, Cohen GH, Sampson L, Vivier PM, Galea S. Prevalence of depression symptoms in US adults before and during the COVID-19 pandemic. JAMA Netw Open 2020;3:e2019686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Wang C, Pan R, Wan X, et al. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int J Environ Res Public Health 2020;17:1729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Stanton R, To QG, Khalesi S, et al. Depression, anxiety and stress during COVID-19: Associations with changes in physical activity, sleep, tobacco and alcohol use in Australian adults. Int J Environ Res Public Health 2020;17:4065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. McCormack G, Avery C, Spitzer AK-L, Chandra A. Economic vulnerability of households with essential workers. JAMA 2020;324:388–390 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Jones JA, Banks L, Plotkin I, Chanthavongsa S, Walker N. Profile of the public health workforce: Registered TRAIN learners in the United States. Am J Public Health 2015;105(Suppl 2):e30–e36 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Viveiros N, Bonomi AE. Novel coronavirus (COVID-19): Violence, reproductive rights and related health risks for women, opportunities for practice innovation. J Fam Violence. 2020:1–5. DOI: 10.1007/s10896-020-00169-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Gausman J, Langer A. Sex and gender disparities in the COVID-19 pandemic. J Womens Health (Larchmt) 2020;29:465–466 [DOI] [PubMed] [Google Scholar]
- 11. Frederiksen B, Gomez I, Salganicoff A, Ranji U. Coronavirus: A Look at Gender Differences in Awareness and Actions. Kaiser Family Foundation. Published March 20, 2020. Available at: https://www.kff.org/coronavirus-covid-19/issue-brief/coronavirus-a-look-at-gender-differences-in-awareness-and-actions/ Accessed September8, 2020
- 12. The National Academies of Science, Engineering and Medicine (NASEM). Integrating social care into the delivery of health care: Moving upstream to improve the nation's health. Washington, D.C.: The National Academies Press, 2019. DOI: 10.17226/25467 [DOI] [PubMed] [Google Scholar]
- 13. Alley DE, Asomugha CN, Conway PH, Sanghavi DM. Accountable health communities—Addressing social needs through Medicare and Medicaid. N Engl J Med 2016;374:8–11 [DOI] [PubMed] [Google Scholar]
- 14. Committee on Health Care for Underserved Women. ACOG Committee Opinion No. 729: Importance of social determinants of health and cultural awareness in the delivery of reproductive health care. Obstet Gynecol 2018;131:e43–e48 [DOI] [PubMed] [Google Scholar]
- 15. Coleman-Jensen A, Rabbitt MP, Gregory CA, Singh A. Household Food Security in the United States in 2019. U.S. Department of Agriculture, Economic Research Service. Available at: https://www.ers.usda.gov/webdocs/publications/84973/err-237.pdf Accessed September22, 2020
- 16. Jung NM, de Bairros FS, Pattussi MP, Pauli S, Neutzling MB. Gender differences in the prevalence of household food insecurity: A systematic review and meta-analysis. Public Health Nutr 2017;20:902–916 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Smith S, Zhang X, Basile K, et al. National Intimate Partner and Sexual Violence Survey: 2015 Data Brief. National Center for Injury Prevention and Control, Centers for Disease Control and Prevention, 2018. Available at: https://www.cdc.gov/violenceprevention/pdf/2015data-brief508.pdf Accessed December16, 2020
- 18. Poleshuck E, Wittink M, Crean HF, et al. A comparative effectiveness trial of two patient-centered interventions for women with unmet social needs: Personalized support for progress and enhanced screening and referral. J Womens Health (Larchmt) 2020;29:242–252 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Gruber-Baldini AL, Velozo C, Romero S, Shulman LM. Validation of the PROMIS® measures of self-efficacy for managing chronic conditions. Qual Life Res 2017;26:1915–1924 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Forrest CB, Bevans KB, Pratiwadi R, et al. Development of the PROMIS® pediatric global health (PGH-7) measure. Qual Life Res 2014;23:1221–1231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. U.S. Census Bureau. 2018 American Community Survey 1-year estimates. Published 2018. Available at: https://www2.census.gov/programs-surveys/acs/summary_file/2018/data/?# Accessed May15, 2020
- 22. Lane TS, Armin J, Gordon JS. Online recruitment methods for web-based and mobile health studies: A review of the literature. J Med Internet Res 2015;17:e183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. The American Association for Public Opinion Research. Standard Definitions: Final Dispositions of Case Codes and Outcome Rates for Surveys, 9th ed. AAPOR, 2016. Available at: https://www.aapor.org/AAPOR_Main/media/publications/Standard-Definitions20169theditionfinal.pdf Accessed May27, 2017
- 24. The Accountable Health Communities Health-Related Social Needs Screening Tool. Center for Medicare & Medicaid Services. Available at: https://innovation.cms.gov/Files/worksheets/ahcm-screeningtool.pdf Accessed December11, 2018
- 25. Spitzer RL, Kroenke K, Williams JBW, Löwe B. A brief measure for assessing generalized anxiety disorder: The GAD-7. Arch Intern Med 2006;166:1092–1097 [DOI] [PubMed] [Google Scholar]
- 26. Kroenke K, Spitzer RL, Williams JBW. The Patient Health Questionnaire-2: validity of a two-item depression screener. Med Care 2003;41:1284–1292 [DOI] [PubMed] [Google Scholar]
- 27. Schuster MA, Stein BD, Jaycox L, et al. A national survey of stress reactions after the September 11, 2001, terrorist attacks. N Engl J Med 2001;345:1507–1512 [DOI] [PubMed] [Google Scholar]
- 28. Jeung R, Nham K.. Incidents of Coronavirus-Related Discrimination. Asian Pacific Policy & Planning Council, Chinese for Affirmative Action, 2020. Available at: http://www.asianpacificpolicyandplanningcouncil.org/wp-content/uploads/STOP_AAPI_HATE_MONTHLY_REPORT_4_23_20.pdf. Accessed December4, 2020
- 29. Centers for Disease Control (CDC). Behavioral Risk Factor Surveillance System Survey Data. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, 2018. Available at: https://www.cdc.gov/brfss/annual_data/annual_2018.html. Accessed June11, 2020
- 30. De Marchis EH, Hessler D, Fichtenberg C, et al. Part I: A quantitative study of social risk screening acceptability in patients and caregivers. Am J Prev Med 2019;57(6 Suppl 1):S25–S37 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Flood S, King M, Rodgers R, Ruggles S, Warren JR. Integrated Public Use Microdata Series, Current Population Survey: Version 7.0 [Dataset]. Minneapolis, MN: IPUMS, 2020. Available at: 10.18128/D030.V7.0 Accessed June11, 2020 [DOI]
- 32. Chen P-H, Rovi S, Washington J, et al. Randomized comparison of 3 methods to screen for domestic violence in family practice. Ann Fam Med 2007;5:430–435 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Flynn HA, Spino C, Guille C, et al. A collaborative, network-based approach to advance women's depression research in the United States: Preliminary findings. J Womens Health (Larchmt) 2018;27:51–57 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Centers for Disease Control and Prevention (CDC), National Center for Health Statistics (NCHS). National Health and Nutrition Examination Survey Data. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, 2020. Available at: https://wwwn.cdc.gov/Nchs/Nhanes/2017–2018/DPQ_J.htm Accessed June11, 2020
- 35. Reynolds DL, Garay JR, Deamond SL, Moran MK, Gold W, Styra R. Understanding, compliance and psychological impact of the SARS quarantine experience. Epidemiol Infect 2008;136:997–1007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Betancourt TS, Brennan RT, Vinck P, et al. Associations between mental health and Ebola-related health behaviors: A regionally representative cross-sectional survey in post-conflict Sierra Leone. PLoS Med 2016;13:e1002073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Salari N, Hosseinian-Far A, Jalali R, et al. Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: A systematic review and meta-analysis. Global Health 2020;16:57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Galea S, Merchant RM, Lurie N. The mental health consequences of COVID-19 and physical distancing: The need for prevention and early intervention. JAMA Intern Med. 2020;180:817–818 [DOI] [PubMed] [Google Scholar]
- 39. Gottlieb LM, Wing H, Adler NE. A systematic review of interventions on patients' social and economic needs. Am J Prev Med 2017;53:719–729 [DOI] [PubMed] [Google Scholar]
- 40. Waxman E, Gupta P, Karpman M. More Than One in Six Adults Were Food Insecure Two Months into the COVID-19 Recession: Findings from the May 14–27 Coronavirus Tracking Survey. Urban Institute. Published July 2020. Available at: https://www.urban.org/sites/default/files/publication/102579/more-than-one-in-six-adults-were-food-insecure-two-months-into-the-covid-19-recession.pdf Accessed September28, 2020
- 41. Ahn S, Norwood FB. Measuring food insecurity during the COVID-19 pandemic of spring 2020. Appl Econ Perspect Policy 2020;43:162–168 [Google Scholar]
- 42. Wolfson JA, Leung CW. Food insecurity and COVID-19: Disparities in early effects for US adults. Nutrients 2020;12:1648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Carlson SJ, Andrews MS, Bickel GW. Measuring food insecurity and hunger in the United States: development of a national benchmark measure and prevalence estimates. J Nutr 1999;129(2S Suppl):510S–516S [DOI] [PubMed] [Google Scholar]
- 44. Blumberg SJ, Bialostosky K, Hamilton WL, Briefel RR. The effectiveness of a short form of the Household Food Security Scale. Am J Public Health 1999;89:1231–1234 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Gattu RK, Paik G, Wang Y, Ray P, Lichenstein R, Black MM. The hunger vital sign identifies household food insecurity among children in emergency departments and primary care. Children (Basel) 2019;6:107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Buzby JC, Wells HF, Hyman J. The Estimated Amount, Value, and Calories of Postharvest Food Losses at the Retail and Consumer Levels in the United States. U.S. Department of Agriculture, Economic Research Service, 2014. Available at: https://www.ers.usda.gov/webdocs/publications/43833/43680_eib121.pdf Accessed September28, 2020
- 47. Whitaker RC, Phillips SM, Orzol SM. Food insecurity and the risks of depression and anxiety in mothers and behavior problems in their preschool-aged children. Pediatrics 2006;118:e859–e868 [DOI] [PubMed] [Google Scholar]
- 48. Fitzpatrick KM, Harris C, Drawve G. Living in the midst of fear: Depressive symptomatology among US adults during the COVID-19 pandemic. Depress Anxiety 2020;37:957–964 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Ivers LC, Cullen KA. Food insecurity: Special considerations for women. Am J Clin Nutr 2011;94:1740S–1744S [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Gyasi RM, Obeng B, Yeboah JY. Impact of food insecurity with hunger on mental distress among community-dwelling older adults. PLoS One 2020;15:e0229840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. U.S. Department of Agriculture Food and Nutrition Service. Supplemental Nutrition Assistance Program Participation and Costs. U.S. Department of Agriculture Food and Nutrition Service. Published July 2020. Available at: https://fns-prod.azureedge.net/sites/default/files/resource-files/SNAPsummary-7.pdf Accessed September28, 2020
- 52. Ivanova JI, Birnbaum HG, Chen L, et al. Cost of post-traumatic stress disorder vs major depressive disorder among patients covered by medicaid or private insurance. Am J Manag Care 2011;17:e314–e323 [PubMed] [Google Scholar]
- 53. Boserup B, McKenney M, Elkbuli A. Alarming trends in US domestic violence during the COVID-19 pandemic. Am J Emerg Med. 2020;38:2753–2755 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Kofman YB, Garfin DR. Home is not always a haven: The domestic violence crisis amid the COVID-19 pandemic. Psychol Trauma 2020;12(S1):S199–S201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Mahase E. Covid-19: EU states report 60% rise in emergency calls about domestic violence. BMJ 2020;369:m1872. [DOI] [PubMed] [Google Scholar]
- 56. Roesch E, Amin A, Gupta J, García-Moreno C. Violence against women during covid-19 pandemic restrictions. BMJ 2020;369:m1712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Parkinson D. Investigating the increase in domestic violence post disaster: An Australian case study. J Interpers Violence 2019;34:2333–2362 [DOI] [PubMed] [Google Scholar]
- 58. Harville EW, Taylor CA, Tesfai H, Xu X, Buekens P. Experience of Hurricane Katrina and reported intimate partner violence. J Interpers Violence 2011;26:833–845 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Oxfam, Doctors of the World.. Dominican Republic Gender Analysis: A Study of the Impact of the Zika Virus on Women, Girls, Boys and Men. Oxfam International, 2017. Available at: https://oxfamilibrary.openrepository.com/bitstream/handle/10546/620261/rr-dominican-republic-gender-analysis-210417-en.pdf?sequence=1&isAllowed=y Accessed September30, 2020
- 60. Onyango MA, Resnick K, Davis A, Shah RR. Gender-based violence among adolescent girls and young women: A neglected consequence of the West African Ebola outbreak. In: Schwartz DA, Anoko JN, Abramowitz SA, eds. Pregnant in the time of Ebola: Women and their children in the 2013–2015 West African epidemic. Global Maternal and Child Health. Cham: Springer International Publishing, 2019:121–132. DOI: 10.1007/978-3-319-97637-2_8 [DOI] [Google Scholar]
- 61. Jetelina KK, Knell G, Molsberry RJ. Changes in intimate partner violence during the early stages of the COVID-19 pandemic in the USA. Inj Prev. 2021;27:93–97 [DOI] [PubMed] [Google Scholar]
- 62. Golding JM. Intimate partner violence as a risk factor for mental disorders: A meta-analysis. J Fam Violence 1999;14:99–132 [Google Scholar]
- 63. Ryan G. An Analysis of State and Voluntary Moratoria on Electric Utility Shutoffs. Center for Biological Diversity, 2020. Available at: https://www.biologicaldiversity.org/programs/energy-justice/pdfs/July-21-2020-Issue-Brief_State-Moratoria-on-Electric-ShutOffs.pdf Accessed October1, 2020
- 64. Coker AL, Smith PH, Whitaker DJ, Le B, Crawford TN, Flerx VC. Effect of an in-clinic IPV advocate intervention to increase help seeking, reduce violence, and improve well-being. Violence Against Women 2012;18:118–131 [DOI] [PubMed] [Google Scholar]
- 65. Kangovi S, Mitra N, Grande D, et al. Patient-centered community health worker intervention to improve posthospital outcomes: A randomized clinical trial. JAMA Intern Med 2014;174:535–543 [DOI] [PubMed] [Google Scholar]
- 66. Sherin KM, Sinacore JM, Li XQ, Zitter RE, Shakil A. HITS: A short domestic violence screening tool for use in a family practice setting. Fam Med 1998;30:508–512 [PubMed] [Google Scholar]
- 67. Wenham C, Smith J, Morgan R, Gender and COVID-19 Working Group. COVID-19: The gendered impacts of the outbreak. Lancet 2020;395:846–848 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. American College of Obstetricians and Gynecologists. ACOG to Congress: Prioritize Women's Health in Future COVID-19 Legislation. American College of Obstetricians and Gynecologists. Available at: https://www.acog.org/en/News/News Articles/2020/05/ACOG to Congress Prioritize Womens Health in Future COVID-19 Legislation Accessed July6, 2020
- 69. Lindau ST, Makelarski J, Abramsohn E, et al. CommunityRx: A population health improvement innovation that connects clinics to communities. Health Aff (Millwood) 2016;35:2020–2029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Lindau S, Makelarski J, Abramsohn E, et al. CommunityRx: A real-world controlled clinical trial of a scalable, low-intensity community resource referral intervention. Am J Public Health 2019;109:600–606 [DOI] [PMC free article] [PubMed] [Google Scholar]