Abstract
Background: Music therapy (MT) and virtual reality (VR) have shown favorable patient-reported outcomes during serious illness.
Objectives: To evaluate implementation measures of feasibility, usability, and acceptability of a VR-based MT intervention.
Design: A pilot implementation study of a two-day VR–MT intervention using mixed methods. Patients created a personalized soundtrack with a music therapist, and then paired the soundtrack with a 360° VR environment.
Setting/Subjects: Hospitalized patients with palliative care needs.
Results: Of 23 patients (ages 20–74 years, 52% women), 17 completed the intervention, including 39% during an intensive care unit stay. Participants scored usability above average. For satisfaction, 53% chose the highest rating. Most participants spoke favorably of VR–MT, describing pleasant emotional and physical responses. Participants provided feedback on length, frequency of use, VR options, and timing of delivery.
Conclusion: This VR–MT intervention was feasible, usable, and acceptable for hospitalized palliative care patients. Further study will test VR–MT outcomes.
Keywords: music therapy, palliative care, virtual reality
Introduction
Palliative care is team-based multidimensional specialized care that provides patients with relief from symptoms and other suffering related to serious illness.1 There is growing research indicating that music therapy (MT) provides effective nonpharmacological psychosocial and symptom management.2 Similarly, recent studies have shown that virtual reality (VR)-based interventions improved outcomes during serious illness.3
MT for palliative care patients can include a broad range of techniques such as therapeutic singing, music-assisted relaxation, creative self-expression through music, and supportive verbal processing through music.4–6 MT addresses core components of palliative care, including improving physiological and emotional outcomes.7–12 VR represents technology that combines software and an all-in-one stand-alone headset to transport patients to an immersive 360° virtual environment. Specific to palliative care, a study of palliative care patients with terminal cancer demonstrated improvements in multiple symptoms after a 30-minute VR session.3 Another pilot study found that 83% of participants would recommend VR to someone living with a serious illness.13 Conceptually, therapeutic VR provides an immersive visual sensory experience that augments evidence-based MT approaches. In addition, development of a combined technology-based VR–MT intervention may enhance scalability.
To our knowledge, this is the first study that examines implementation measures for the combination of VR with an MT intervention comprising soundtrack creation, music listening, and therapeutic conversation by a board-certified music therapist.
Methods
Design
This study of hospitalized palliative care patients uses a mixed methods design to focus on implementation outcomes of feasibility, usability, and acceptability of a VR–MT intervention.14 We aimed to capture user experience to inform an iterative user-centered design process.15 This study was approved by the Colorado Institutional Review Board.
Setting and participants
The University of Colorado Hospital (UCH) palliative care inpatient team, which includes a board-certified music therapist, identified eligible participants during interprofessional rounds. Eligible patients included hospitalized adults age 18 years and older, with a palliative care consult, estimated length of stay of at least two days, and diagnosis of cancer, heart failure, or end-stage renal disease. Patients were excluded if deaf, legally blind, experiencing active delirium based on the Confusion Assessment Method,16 or unable to provide informed consent. Recruitment occurred September 2019 through February 2020 and participants were reimbursed $25 for research activities.
Intervention
Participants created a customized soundtrack with a music therapist for listening during a VR experience using a two-day protocol (Table 1). Participants used an Oculus Go VR (Facebook; Menlo Park, CA) headset. Video options included four nature-based videos from free online content (Atmosphaeres, Germany), downloaded onto the VR headset. Video content allowed participants to be immersed in a nonanimated nature environment including natural sounds. Soundtrack selections were streamed from Apple Music onto an iPad with headphones worn over the VR headset. After use, VR headsets were cleaned using a procedure recommended by UCH Infection Control, including use of antibacterial wipes and ultraviolet sanitation drawers.
Table 1.
Virtual Reality–Music Therapy Intervention Protocol
| Day 1: VR–MT consultation visit Goals of day 1: • Establish relationship with patient that creates comfortability in processing emotions within serious illness as an extension of palliative care • Obtain patient-preferred VR nature scene • Create personalized patient-preferred music soundtrack Materials needed: • VR environment options • Computer tablet/music application for soundtrack creation • Research-in-progress door sign |
Introduction • Establish link to palliative care team • Cultivate a therapeutic relationship to allow for discussions within serious illness—decide if optimal therapeutic relationship is one on one vs. inclusions of any family present • Give the patient a choice to select VR scene (visual) or soundtrack (auditory) selection first Soundtrack creation • Explore patient history and background of music engagement • Discuss patient relationships to music, including personal associations • Discuss desire of familiar vs. novel music • Have patient set personal goal for VR–MT experience (relaxation, resilience, escape, journey, etc.) • Create discussion space of processing patient rationale for music selections • Consider and discuss patient preferences for song order, including how individual songs may transition patient from one mood to another Selection of VR setting • Set patient goal for VR scene selection • Remind patient this is a stationary scene with natural movements—not games or actively moving within the setting • Create discussion space of processing patient rational for scene selection |
| Intermediary steps Materials needed: • Computer tablet/music application for soundtrack creation • Oculus go headset |
Soundtrack finalization and VR preparation • Finish downloading patient preferred songs • Finalize song selections if patient requested a genre/artist but wanted assistance in specific song selection • Finalize order of playlist • Queue VR headset to patient selected nature scene |
| Day 2: VR–MT immersive soundtrack and VR experience, including therapeutic debrief Goals of day 2: • Re-establish patient goals for VR–MT • Provide visual and auditory immersive experience for patient • Debrief patient experience, including emotional and physical responses Materials needed: • Oculus go headset • Playlist on music playing device • Headphones • Research-in-progress door sign • Debriefing tool • Patient education handout • Cleaning wipes |
Introduction • Re-establish rapport • Assess for any immediate needs or soundtrack/VR scene selection changes before intervention Description and intervention • Educate and remind patient of the intervention as tool for their established goal • Provide expectations of VR headset—adjustable straps, etc. • Allow time for patient to orient within VR space • Give patient permission to dance/sing/express themselves during intervention • Adjust sound levels of music and nature sounds as needed • Remind of protocol if any discomfort Therapeutic debrief • Create space for awareness and discussion of any physical and emotional responses—utilize debriefing tool for guidance (available upon request) • Discuss opportunity of using this experience as a tool for personal goals posthospitalization—share educational handout (available upon request) • Triage any further patient needs as appropriate • Provide closure and obtain permission to end the discussion Infection control and sanitation protocol • Follow all individual patient contact precautions • Wipe down all equipment with antibacterial wipes • Place all equipment in UV sanitation drawer |
MT, music therapy; UV, ultraviolet; VR, virtual reality.
Data collection
Feasibility
We tracked patient enrollment, including reasons for declining. We recorded the patients who completed the VR experience, reasons for discontinuation, and total time of VR–MT. We collected mortality data, including location of death.
Usability
Patients completed the System Usability Scale (SUS).17 The system usability instrument has 10 items related to perceived usability of technology-based tools using a 5-point Likert scale. Scores range from 0 to 100. Grades of ≥90 are considered superior usability ratings.18
Acceptability
Participants completed brief interviews and adapted satisfaction questions from the Mobile App Rating Scale19 (available upon request) immediately post-intervention. Brief interviews explored experiences of VR–MT and collected feedback for iterative design (Supplementary Data S1).
Data analysis
We used descriptive statistics to summarize quantitative data using SAS, version 9.4, and a qualitative descriptive approach to analyze interviews.20 Using an inductive and deductive approach, three researchers organized verbatim quotes related to acceptability, user experience, and user input on intervention refinement, and identified emergent themes.21 We reached data saturation, where information from newer interviews repeated what was expressed in prior interviews after 14 interviews.22 To increase transparency, we include verbatim quotes. Qualitative and quantitative data were given equal priority, collected concurrently, analyzed separately, and then integrated during interpretation.23
Results
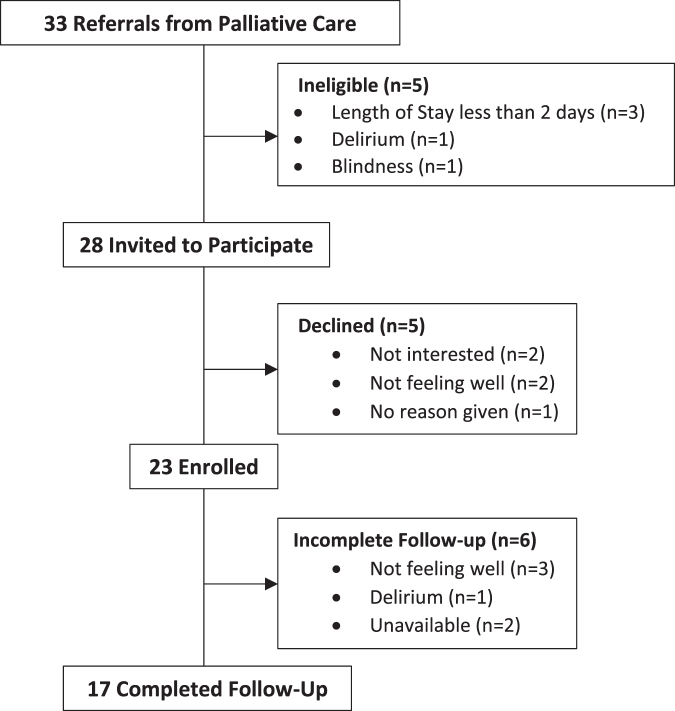
Over five months, 33 patients were offered VR–MT; 23 consented (Fig. 1). Five participants declined as “not interested” (2), “not feeling well” (2), or “no reason” (1). Seventeen patients completed VR–MT (74% completion). Ages ranged from 20 to 74 years with 52% women (Table 2). Ten participants died post-intervention: three died in the hospital, five died with hospice care, and details for two are unknown.
FIG. 1.
Study enrollment.
Table 2.
Participant Characteristics (N = 23)
| n (%) | |
|---|---|
| Age, years (SD) | 47.4 (17.1) |
| Female sex | 12 (52) |
| Ethnicity | |
| Hispanic | 3 (13) |
| Non-Hispanic | 20 (87) |
| Race | |
| White/Caucasian | 15 (66) |
| Black/African American | 4 (17) |
| Other | 4 (17) |
| Primary diagnosis | |
| Cancer | 14 (61) |
| Heart failure | 7 (30) |
| End-stage renal | 2 (9) |
| Patient location of completion | |
| Intensive care unit | 9 (39) |
| Floor | 14 (61) |
| Contact precaution during intervention | 6 (26) |
| Days in hospital at start of VR–MT, days (SD) | 14.7 (17.4) |
| Mortality | 10 (43) |
| Average number of days post-VR–MT, days (SD) | 27.9 (26.1) |
| Location of death | |
| Died in hospital without hospice | 3 (30) |
| Died under inpatient hospice care | 1 (10) |
| Died at home with hospice care | 3 (30) |
| Died at home without hospice | 1 (10) |
| Location of death unknown | 2 (20) |
SD, standard deviation.
Feasibility
VR–MT was feasible for patients in the intensive care unit (39%) and while receiving treatments such as extracorporeal membrane oxygenation, mechanical ventilation, heated high-flow oxygen, and dialysis. The average VR–MT time including questionnaires was 1.5 hours. Time with the music therapist averaged 28 minutes for soundtrack creation (day 1) and 35 minutes for VR–MT and debriefing (day 2). Playlists averaged four songs up to 20 minutes.
Usability
The average SUS composite score was 80.4 (standard deviation 13.8), which was associated with a grade of ∼90% (Supplementary Data S2). Regarding satisfaction, 53% chose the highest rating of 5 and 29% chose a rating of 4. Over half marked they would want to use VR–MT daily; 35% marked they would pay to use this type of intervention at home. Similarly, 65% would recommend this experience to everyone, 24% to many people.
Acceptability
Three themes related to acceptability emerged (Table 3). First, patients positively anticipated their participation in VR–MT. Participants commented that they began thinking about their music choices after hearing about the study. Second, participants appreciated the customized intervention design involved in VR–MT. They liked being able to choose anything they wanted musically. Third, physical acceptability of the VR headset and headphones varied. Most participants had never worn a VR headset. A few participants reported being unable to see the images clearly, some of whom had opted to not wear their glasses underneath. Although most feedback was favorable, two participants found the intervention to be acceptable but did not enjoy their experience. Both felt VR–MT was “too boring.”
Table 3.
Verbatim Quotes from Virtual Reality–Music Therapy Intervention Participants
| Implementation categories and themes | Verbatim quotes |
|---|---|
| Acceptability | |
| Positive anticipation about VR–MT | “It was really easy for me to pick out a playlist. I automatically started thinking about songs that I liked. So, it was really easy for me to think about if I wanted to space out, what I wanted to feel and listen to… The only hard part about it was just wondering what it was gonna be like.” (24-year-old woman) |
| Appreciation of ability to create a customized experience | “I was trying to think of music that is meaningful to me… a couple of the songs are a bit more sad and reflective. And some of the songs are really good. And I needed both. If I had all sad songs or all happy songs, it probably wouldn't have been as enjoyable to me.” (47-year-old woman) “I was able to give some pretty high-level, general information and (the music therapist) kind of drilled down into what I was looking for.” (55-year-old woman) |
| Variation in physical acceptability of the VR headset and headphones | “I was worried about maybe having a claustrophobic experience but I had none.” (59-year-old woman) “My overall reaction was claustrophobia.” (73-year-old man) “Putting on the virtual reality mask over my glasses was uncomfortable. It kind of smashed my frames into my face a little bit.” (55-year-old woman) |
| User experience | |
| Emotional response to VR–MT | “A sense of euphoria. A sense of peace. A sense of calming that was not there before.” (62-year-old man) “So heartwarming. It just opened my soul. I mean it felt like everything lifted straight up off my chest. I feel so relaxed and comfortable.” (54-year-old woman) |
| Respite from medical circumstances | “I can just put on headphones and kind of space out for awhile and be in my own little world that I get to pick out… To a place you want to be. Not somewhere you have to be or stuck. Which is a piece of control you can take back a little bit.” (24-year-old woman) “I could escape from the new diagnosis for 20 minutes. I gained that peace for 20 minutes.” (69-year-old woman) |
| Physical response to VR–MT | “All my pain reduced in there.” (56-year-old man) “When I had both the headset and the virtual reality mask on, my breathing changed and became slower and more calm and I relaxed.” (55-year-old woman) |
| User input on intervention refinement | |
| VR–MT length and frequency of use (dosing) | “A wonderful experience. If I had my way I would do that every day.” (54-year-old woman) “You could do several different lengths. You could do a 10 minute one…Some people would like an hour.” (47-year-old woman) |
| VR environments | “Definitely add more nature scenes. More options…different seasons would be cool…maybe more like national parks. Those are always beautiful.” (24-year-old woman) “Maybe changing the scene with each song and then, like, actually being interactive with what's going on… it seems kind of boring is what it was.” (25-year-old man) |
| Time of delivery | “More towards nighttime. When there's less going on.” (25-year-old man) “I don't know the optimal time…Early mornings, I love. But it seems like that's when I'm most emotional and upset is really the morning.” (69-year-old woman) |
User experience
Three themes emerged related to user experience (Table 3). First, all 14 participants described the intervention as comfortable and easy to engage in. They described ease in working with the music therapist to create their customized soundtrack. In terms of emotional response to VR–MT, participants reflected feeling surprised by their emotions, including one participant who was tearful while debriefing with the music therapist. Second, 10 participants described experiencing respite from their current situation of being hospitalized through the visual and auditory immersion in a virtual space outside the walls of their hospital room. Third, seven participants had physical responses to VR–MT. Participants described physical changes, including improved pain, decreased chest tightness, body relaxation, and positive changes in breathing. None of the participants reported negative physical responses.
User input on intervention refinement
Several comments related to user-centered intervention refinement (Table 3). Participants reported that the length and frequency of using VR–MT could change both between and within participants depending on their mood or availability based on hospital care, and thus, recommended options for length and frequency. Participants wanted more VR environment options. They suggested wanting specific places, seasonal options, specific movements within an environment, or different views within the environment. Participants desired for the scenes to be more interactive, such as the ability to walk around. When asked if there was an ideal time of day for the intervention, answers varied between participants, reflecting on factors such as times when there are less hospital interventions, times when they feel more or less symptoms, or times they feel more or less emotional.
Discussion
This study explored implementation outcomes of a two-day VR-based MT intervention with hospitalized palliative care patients. This is a unique application of VR by a music therapist to provide an immersive auditory and visual experience. VR–MT was feasible and acceptable for a wide range of patients. In general, participants positively described their VR–MT experience, although some noted physical challenges using the technology. Many participants described immediate changes, including experiencing respite. Most participants wanted to repeat the intervention and would recommend it to others.
Patient feedback was not only largely positive, but also identified the difference between having unlimited music selection options but limited VR video environment selections. By design, we used virtual environments with natural movements and excluded environments that enabled interaction by using a remote controller to decrease technology instructions. However, many participants suggested changes to VR environments to make them more interactive or able to align with their soundtracks. These findings highlight the importance of user input during iterative design.
There were several limitations. Participants were not randomized and the palliative care team may have influenced recruitment, thus influencing generalizability. For usability, the SUS was not particularly sensitive to the structured assistance of VR–MT, although our data are similar to another study that showed 67% of VR participants in the palliative care setting reported VR technology easy to use.13
Conclusion
A VR–MT intervention is feasible, usable, and acceptable for hospitalized palliative care patients, and resulted in important design consideration for implementation. Further investigation should measure patient-level outcomes on physical symptoms, emotional symptoms, or quality of life, as well as frequency and duration of VR–MT.
Supplementary Material
Acknowledgments
The authors thank the University of Colorado Hospital Palliative Care team for partnering in this study, and the National Mental Health Innovation Center, including Lauren Schviraga and Gwendolyn Gaumond, for technical assistance related to VR technology needs.
Authors' Contributions
All authors contributed to the design, acquisition, analysis, and/or interpretation of the data with substantial revisions to the final version for publication.
Funding Information
This study was supported in part by the National Institute on Aging of the National Institutes of Health (NIH) (award K76AG054782). Additional support through the Colorado Clinical and Translational Sciences Institute (CCTSI) from the Development and Informatics Service Center (NIH/NCRR CCTSI grant no. UL1 RR025780) for use of REDCap-based data management.
Author Disclosure Statement
No competing financial interests exist. The content of and views expressed in this article are solely the responsibility of the authors and do not necessarily represent the official views of the National Institutes of Health or the Department of Veterans Affairs.
Supplementary Material
References
- 1. Ferrell BR, Twaddle ML, Melnick A, Meier DE: National Consensus Project Clinical Practice Guidelines for Quality Palliative Care Guidelines, 4th Edition. J Palliat Med 2018;21:1684–1689 [DOI] [PubMed] [Google Scholar]
- 2. Gao Y, Wei Y, Yang W, et al. : The effectiveness of music therapy for terminally ill patients: A meta-analysis and systematic review. J Pain Symptom Manage 2019;57:319–329 [DOI] [PubMed] [Google Scholar]
- 3. Niki K, Okamoto Y, Maeda I, et al. : A novel palliative care approach using virtual reality for improving various symptoms of terminal cancer patients: A preliminary prospective, multicenter study. J Palliat Med 2019;22:702–707 [DOI] [PubMed] [Google Scholar]
- 4. Archie P, Bruera E, Cohen L: Music-based interventions in palliative cancer care: A review of quantitative studies and neurobiological literature. Support Care Cancer 2013;21:2609–2624 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Clements-Cortes A: Development and efficacy of music therapy techniques within palliative care. Complement Ther Clin Pract 2016;23:125–129 [DOI] [PubMed] [Google Scholar]
- 6. Wood C, Cutshall SM, Wiste RM, et al. : Implementing a palliative medicine music therapy program: A quality improvement project. Am J Hosp Palliat Care 2019;36:603–607 [DOI] [PubMed] [Google Scholar]
- 7. Gallagher LM, Lagman R, Mellar W, et al. : The clinical effects of music therapy in palliative medicine. Support Care Cancer 2006;14:859–866 [DOI] [PubMed] [Google Scholar]
- 8. Horne-Thompson A, Grocke D: The effect of music therapy on anxiety in patients who are terminally ill. J Palliat Med 2008;11:582–590 [DOI] [PubMed] [Google Scholar]
- 9. Krout RE: The effects of single-session music therapy interventions on the observed and self-reported levels of pain control, physical comfort, and relaxation of hospice patients. Am J Hosp Palliat Care 2001;18:383–390 [DOI] [PubMed] [Google Scholar]
- 10. Clements-Cortes A: The use of music in facilitating emotional expression in the terminally ill. Am J Hosp Palliat Care 2004;21:255–260 [DOI] [PubMed] [Google Scholar]
- 11. Hilliard RE: The effects of music therapy on the quality and length of life of people diagnosed with terminal cancer. J Music Ther 2003;40:113–137 [DOI] [PubMed] [Google Scholar]
- 12. Salmon D: Music and emotion in palliative care. J Palliat Care 1993;9:48–52 [PubMed] [Google Scholar]
- 13. Johnson T, Bauler L, Vos D, et al. : Virtual reality use for symptom management in palliative care: A pilot study to assess user perceptions. J Palliat Med 2020;23:1233–1238 [DOI] [PubMed] [Google Scholar]
- 14. Proctor E, Silmere H, Raghavan R, et al. : Outcomes for implementation research: Conceptual distinctions, measurement challenges, and research agenda. Adm Policy Ment Health 2011;38:65–76 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Yardley L, Morrison LG, Andreou P, et al. : Understanding reactions to an internet-delivered health-care intervention: Accommodating user preferences for information provision. BMC Med Inform Decis Mak 2010;10:52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Inouye SK, van Dyck CH, Alessi CA, et al. : Clarifying confusion: The confusion assessment method. A new method for detection of delirium. Ann Intern Med 1990;113:941–948 [DOI] [PubMed] [Google Scholar]
- 17. Sauro J: Measuring Usability with the System Usability Scale (SUS). https://measuringu.com/sus. 2011. (Last accessed January8, 2018)
- 18. Bangor A, Kortum PT, Miller JT: An empirical evaluation of the system usability scale. Int J Hum Comput Interact 2008;24:574–594 [Google Scholar]
- 19. Stoyanov SR, Hides L, Kavanagh DJ, et al. : Mobile app rating scale: A new tool for assessing the quality of health mobile apps. JMIR Mhealth Uhealth 2015;3:e27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Sandelowski M: Whatever happened to qualitative description? Res Nurs Health 2000;23:334–340 [DOI] [PubMed] [Google Scholar]
- 21. Vaismoradi M, Turunen H, Bondas T: Content analysis and thematic analysis: Implications for conducting a qualitative descriptive study. Nurs Health Sci 2013;15:398–405 [DOI] [PubMed] [Google Scholar]
- 22. Saunders B, Sim J, Kingstone T, et al. : Saturation in qualitative research: Exploring its conceptualization and operationalization. Qual Quant 2018;52:1893–1907 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Zhang W, Creswell J: The use of “mixing” procedure of mixed methods in health services research. Med Care 2013;51:e51–e57 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.