Abstract
Background
Costs can be a major barrier to medication adherence in low and middle-income countries and are an important target for policy-level interventions. The use of benzathine penicillin G (BPG) for secondary prevention of rheumatic heart disease (RHD) averts substantial morbidity and mortality, yet the total out-of-pocket costs for patients receiving this intervention are unknown.
Objective
To estimate the total out-of-pocket costs for obtaining BPG prophylaxis among RHD patients in India.
Methods
We prospectively collected self-reported drug-, transportation-, and provider-related costs for secondary prophylaxis among RHD patients presenting for follow-up to a tertiary care centre in New Delhi, India. Monthly costs were estimated by adjusting unit costs by frequency of drug administration.
Results
The cost data provided by 420 patients [mean age (±SD) 11.6 (±2.9) years] was analysed. Majority of the patients were male (65.2%), hailed from rural areas (87.1%), and belonged to lower socioeconomic strata (73.3%). The median monthly total out-of-pocket costs (IQR) for obtaining BPG injections was Indian rupee (INR) 62.5 (42.5–117.0). The median costs for procuring the drug (IQR) was INR 34.0(30.0–39.0). Whereas median costs (IQR) for health care provider and transportation was INR 16.0 [0–32.0]) and INR 11 [0–31.0] respectively. When expressed as mean (SD), the costs for transportation constituted 50% of the total costs, whereas the mean cost for drug procurement and drug administration constituted 30% and 22% of the total costs respectively.
Conclusion
RHD patients receiving BPG prophylaxis incur substantial out-of-pocket costs, with transportation costs constituting nearly half of the total expenditures. National investments in RHD control must be strategically directed at improving health care access and drug supply in order to lower the total costs of secondary prophylaxis and improve adherence rates.
Keywords: Rheumatic heart disease, secondary prophylaxis, adherence, aa, out of pocket expenditure, health economics
1. Introduction
Rheumatic heart disease (RHD) is the epitome of diseases of poverty and social injustice.1 Although its incidence receded dramatically in high-income countries over the second half of the twentieth century, RHD continues to affect 2–3% of school-age children in low- and middle-income countries (LMICs), and the global prevalence of 19.6 million is likely a gross underestimate because the majority of cases go undetected.2 The complications of RHD – heart failure, endocarditis, stroke, and maternal mortality – strike young adults at the most productive stages of their lives, and therefore generate staggering costs from lost productivity and premature mortality.3 Critically, much of this economic burden is preventable, as effective strategies for disease control have been available for nearly half a century.2,4 Secondary prophylaxis with 3-weekly Benzathine Penicillin G (BPG) injections among children with early RHD can greatly reduce the incidence of long-term complications.4 As a result, in the last decade various bodies including the World Heart Federation (WHF) and United Nations have issued policy statements in an attempt to reinvigorate global and national efforts towards control of RHD.5,6 Improvement in access to primary care and preventive services among populations at higher risk of RHD was one of the actions identified in the global resolution adopted unanimously by the member states of World Health Organization in the 71stWorld Health Assembly.7
Despite the fact that complications of RHD may be preventable by secondary prophylaxis, access to and adherence with prophylaxis remain suboptimal.8,9 Barriers to adherence include lack of access to high-quality BPG, fear of injection-site pain or anaphylaxis, and high out-of-pocket costs. High costs can be particularly problematic for adherence to secondary prophylaxis because RHD has predilection for the poorest and most socio-politically disadvantaged members of society. Importantly, even where the drug itself is free or relatively affordable, patients may still need to incur the costs related to the health care provider who administers the injection and for transportation costs to and from the health care facility. Examining the total out-of-pocket costs faced by patients can help identify health system- or policy-level interventions which may improve long-term adherence to secondary prophylaxis which is critical to any national program of RHD control.
Although the global burden appears to have declined, RHD continues to be a significant public health problem in India. India is home to 40% of the global RHD population – an estimated 13.17 million Indians are currently living with RHD.10 Following the economic boom of the past two decades and an increasing recognition of its ongoing epidemic of non-communicable diseases, India now has the resources and the political motivation to launch RHD prevention strategies on a national scale, but economic data to guide these investments are lacking. The objective of this study is to address this gap by estimating the total out-of-pocket costs of secondary prophylaxis of RHD among pediatric patients. We also analyzed the adherence of study population to the prophylactic regime and the factors affecting it.
2. Methods
We prospectively collected self-reported costs incurred during administration of secondary prophylaxis from families of RHD patients, aged less than 22 years, presenting for follow-up at the All India Institute of Medical Sciences (AIIMS). AIIMS is a 2483-bed referral center in New Delhi, India, where patients from all over the country present for tertiary care. The vast majority of these patients receive secondary prophylaxis at local health care facilities which are either government run centers or private clinics near their place of residence. They are periodically followed up at the referral clinic at AIIMS, with the frequency of their follow-up visits depending on the severity of underlying cardiac lesion. We established a pediatric RHD registry at AIIMS in June 2012, in which we enrolled all patients presenting to the pediatric cardiology clinic with confirmed RHD. Trained research assistants collected demographic and clinical data, including the compliance to medications from all patients at each visit. Socioeconomic status was classified based on the modified Kuppuswamy scale which takes into account, the education- and occupation-score of the head of household and the monthly family income.11 Starting in April 2013, the registry also included questions related to out-of-pocket expenditure incurred for receiving intramuscular BPG injection for secondary prophylaxis of RHD. Research assistants collected self-reported out-of-pocket costs associated with purchase of the drug, costs incurred in reaching the health care facility where the injection was administered, and any fees paid to the health care provider for administration of the drug. We recorded the cost incurred for each visit made by the patient and guardian, and converted them to monthly cost, based on the frequency of drug administration. For instance, if the patient received penicillin prophylaxis every 3 weeks, we estimated the monthly cost of penicillin prophylaxis = total cost of one dose ∗ 30/21. The patients who were receiving daily oral erythromycin for secondary prophylaxis (typically on account of a penicillin allergy) were excluded from the analysis. Outcome measures were drug costs, costs related to drug administration, and transportation costs. All costs were inflated to 2018 Indian rupees (INR) using Consumer Price Index.
In order to facilitate international comparisons, we also converted these costs to 2018 international dollars (I$), a hypothetical currency unit that allows the comparison of prices and currency values between countries. One international dollar purchases in a given country the same goods and services that a U.S. dollar would buy in the United States. Thus, it accounts for international exchange rates, and within-country commodity prices and purchasing power. For this study, we used World Bank data on purchasing power for India.12 In 2018, INR 18.10 was equal to one international dollar.
The adherence rates to penicillin prophylaxis was calculated on each visit by dividing the number of BPG injections taken between the current visit and the last visit by the number of injections supposed to be taken in that particular time period. A patient would be declared compliant, if their adherence rates was at least 80%. Written, informed consent was obtained from all patients (parents or legal guardians in the case of minors). The study protocol and consent procedure conform to the ethical guidelines of the 1975 Declaration of Helsinki and were approved a priori by the Institutional Ethics Committee of the All India Institute of Medical Sciences, New Delhi.
Categorical variables are expressed as frequencies (percentage), whereas parametric variables are expressed as median (inter-quartile range) and mean (±standard deviation). Comparisons between groups were made with chi-square test for categorical variables. All analyses were performed using the Stata Statistical Software: Release 14. College Station, TX: StataCorp LP.
3. Results
3.1. Demographics
Between 2013 and 2018, 420 patients and families provided their cost data (Table 1). The mean age (±SD) of patients was 11.6 (±2.9) years. Majority were boys (65.2%), lived outside New Delhi (92.4%), and hailed from rural areas (87.1%). Most of the patients belonged to either the lower or upper-lower socioeconomic class (73.3%).
Table 1.
Patient characteristics.
| Characteristics | N = 420 |
|---|---|
| Age, mean (SD), years | 11.6 (±2.9) |
| Boys, n (%) | 274 (65.2) |
| Area of residence, n (%) | |
| Rural | 366 (87.1) |
| Urban | 54 (12.9) |
| Socioeconomic status, n (%) | |
| Lower | 18 (4.3) |
| Lower/Upper lower | 290 (69.0) |
| Middle/Lower middle | 89(21.2) |
| Upper middle | 22 (5.2) |
| Upper | 1 (0.2) |
| Frequency of BPG injections, n (%) | |
| Three-weekly injections | 335 (79.8%) |
| Two-weekly injections | 85 (20.2) |
| Setting for obtaining prophylaxis, n (%) | |
| Private clinic | 348 (82.9) |
| Government clinic | 72 (17.2) |
BPG: Benzathine Penicillin G, n: number, SD: standard deviation.
3.2. Access to benzathine penicillin G injections
Majority of the patients obtained BPG injections from private clinics (82.9%). Patients and their caregivers reached the clinic either walking or by bicycle, or relied on public transportation. Patients traveled a median distance (IQR) of 2 (0–20) kilometers to obtain BPG injections, with 170 (40.4%) of them traveling farther than 2 km and 11 (2.6%) patients traveling farther than 100 km to get BPG injections.
3.3. Cost of penicillin prophylaxis
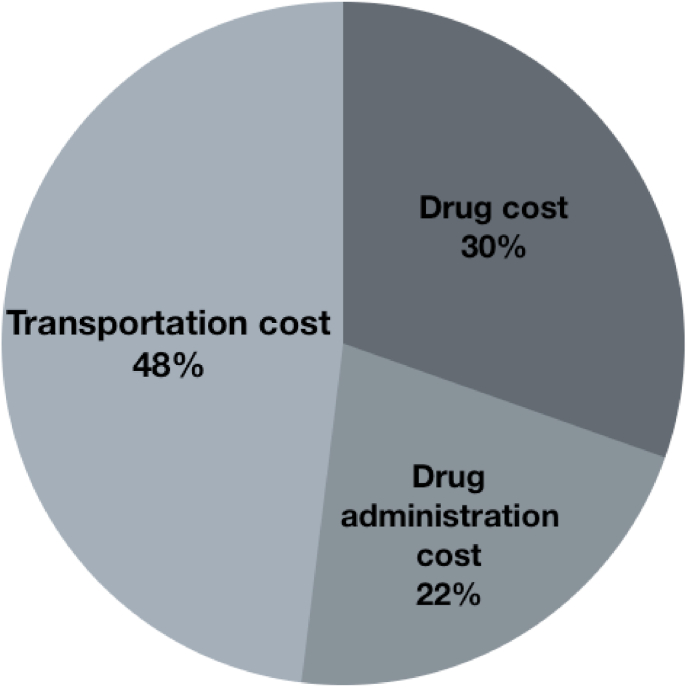
The total monthly out-of-pocket expenditure for getting Penicillin prophylaxis was [median (IQR)] INR 62.5 (42.5–117.0) or I$ 3.45 (2.35–6.46) (Table 2). The median cost (IQR) for procuring the drug was INR 34.0 [30.0–39.0]), median cost (IQR) for drug administration was INR 16.0 [0–32.0]) and median costs (IQR) for transportation was INR 11.0 [0–31.0]). When expressed in terms of mean (±SD), the cost for drug procurement constituted 30% of the total cost whereas, the mean cost for administering the drug and mean cost incurred in reaching the health care facility constituted 22% and 48% of the total mean costs respectively (Table 2 and Fig. 1). The cumulative costs incurred for reaching the health care facility and administering the drug exceeded the cost of the drug in 166 (39.5%) patients.
Table 2.
Monthly out-of-pocket costs for obtaining secondary prophylaxis with Benzathine Penicillin G injections for rheumatic heart disease.
| International Dollars [Median (IQR)] | Indian Rupees [Median (IQR)] | Indian Rupees (Mean ± SD) | |
|---|---|---|---|
| Total costs | 3.45 (2.35–6.46) | 62.5 (42.5–117.0) | 114.1 (±199.5) |
| Drug costs | 1.88 (1.66–2.15) | 34(30.0–39.0) | 34.7 (±14.9) |
| Drug administration costs | 0.88(0–1.77) | 16 (0–32.0) | 24.6 (±34.5) |
| Transportation costs | 0.61(0–1.71) | 11.0(0–31.0) | 54.8 (±199.1) |
IQR, inter-quartile range; SD, standard deviation.
Fig. 1.
Split up of out-of-pocket expenses incurred towards obtaining secondary prophylaxis with Benzathine Penicillin G injection.
Of the 412 patients who reported data regarding adherence to BPG injections, 380 (92.2%) were declared compliant, which meant that only 32 patients (7.8%) missed more than 20% of the BPG doses. Among 165 patients who missed at least one BPG dose, only few patients declared the reasons for doing so. Lack of knowledge regarding the importance of secondary prophylaxis was the commonest cause for missing doses in 26 patients (Table 3). Four patients were non-compliant to prophylaxis because of misinformation by the treating physician. The other causes for missing doses are mentioned in Table 3. There was no correlation between the patient compliance and the socioeconomic class of the patient or with any of the variables used to calculate socioeconomic class. There was no difference in compliance between families from rural or urban areas. Various components of the expenses and distance travelled did not show any difference with regards to the patient compliance.
Table 3.
Reasons for missing Benzathine penicillin G doses in patients who missed at least one dose.
| Reason | Number of patients |
|---|---|
| Lack of knowledge regarding the importance of secondary prophylaxis | 26 |
| Non-availability of drug | 9 |
| Fear of pain during injection | 4 |
| Misinformed by treating doctor | 4 |
| Unable to afford the involved out of pocket costs | 3 |
| Non-availability of physician | 1 |
4. Discussion
This is the first study to systematically evaluate total out-of-pocket costs for secondary prophylaxis of RHD among pediatric patients in India. Our findings suggest that transportation- and drug administration-related costs inflict a larger burden to the family than the drug cost itself, which constituted only 30% of those total costs. Commensurate with the long distances that patients had to travel in order to access clinical care, transportation costs constituted the largest component of total costs (48.04%). Despite the fact that the drug is supposed to be freely available in government clinics, many patients chose to obtain it from private health care providers, paying both for the drug as well as the fee related to its administration. This may partly be due to difficulties in accessibility of government run clinics (being too far or not open during convenient hours) and partly due to concerns regarding the quality of care in government run clinics. Our findings suggest that, policy interventions that focus only on drug costs without simultaneously addressing the barriers related to accessibility of health care systems are unlikely to sufficiently lower the total out-of pocket expenditures to boost adherence to secondary prophylaxis.
In keeping with the referral nature of AIIMS, the majority of our patients sought care from rural areas outside Delhi, particularly from neighboring states of Bihar, Madhya Pradesh, Rajasthan, and Uttar Pradesh. These are the India’s most densely populated regions, with relatively low human development indices related to poverty and weak health systems. Our finding that the majority of children with RHD were from the lower economic strata reinforces the adage that rheumatic disease in the 21st century is a disease of poverty. Out-of-pocket costs are a key barrier to adherence,13,14 and patients from lower economic strata may be particularly susceptible given competing economic priorities of the household. In a country with the monthly average household income of INR 8059 (I$ 445.25),15 any expenses towards healthcare would significantly impact the adherence to treatment, more so for a prophylactic therapy, the benefits of which would not be appreciated by the family. There was no significant difference in adherence rates between those belonging to lower and middle socioeconomic class, or between those residing in rural and urban areas. Nevertheless, it is concerning that, 3 families, belonging to lower socio-economic class, were unable to afford the prophylactic regime.
Among children and young adults with early manifestations of RHD, secondary prophylaxis with BPG can prevent expensive downstream complications such as severe valvular disease requiring valve replacement, and heart failure, stroke and endocarditis. Investing in secondary prophylaxis may therefore pay for itself even when economic evaluations only consider healthcare-related costs. However, these healthcare-related costs may be dwarfed by the costs to society from lost productivity related to morbidity or premature mortality, which is the natural course of advanced RHD. Our preliminary work suggests that these “indirect” costs may be five-fold greater than direct costs, and that women are disproportionately affected.16 All of these findings suggest that strategic investments in secondary prophylaxis may be a valuable investment for India and other low- and middle-income countries currently grappling with RHD.
Although our data are from a single, referral center in India, the insights gleaned from this this study are relevant to other low- and middle-income countries. Benzathine penicillin G is listed as an essential medicine by the World Health Organization, but the global supply of high-quality drug is inconsistent in many parts of the world.17,18 This is the result of poor regulation of the manufacturing and procurement processes, broken distribution systems, and, for some formulations, the need for a cold supply chain. Our data suggest that this has economic consequences for patients, who often have to purchase the drug at a private pharmacy (even when it is supposed to be available for free through the public health care system) and pay private medical practitioners to administer the intramuscular injection. The transportation costs, which constituted the major proportion of expenditure in our study, also underscore the need to optimize access to care by integrating high-quality RHD prevention programs within existing primary health care systems rather than building freestanding, siloed programs. Our data therefore support two of five targets for RHD control highlighted by the World Heart Federation position statement.5 This neglected disease has long sat in a blind spot of Indian policy makers, at least in part because of the absence of quantitative data regarding the economic losses resulting from the disease and its complications. Our findings suggest that policy interventions designed to boost adherence to secondary prophylaxis must invest in addressing access-related issues, including availability of high-quality penicillin at low total costs at primary health centers throughout the country. Also, measures should be taken to improve the awareness among the RHD community regarding the importance of strict adherence to prophylactic regimes.
Several limitations of our study merit attention. By collecting cost data from patients presenting to a referral clinic, we may have missed some patients who, on account of geographic or cost-related barriers, have chosen to forego medical care. This may have biased our results. We did not have information about wage losses resulting from the time a family member may have had to take off from work to accompany the child for clinical care, which may be a substantial component of the total economic burden of health care utilization. Although our registry contains patients from a large geographic area, costs in other parts of the country that are underrepresented in the dataset may systematically differ from our estimates. For instance, patients in the northeast and the Himalayan northwest face substantial geographic barriers to accessing high-quality primary care, and transportation costs in those settings may be far exceed our estimates. Self-reported costs of care may be subject to recall bias.
5. Conclusions
Patients receiving benzathine penicillin G for secondary prophylaxis of RHD in India incur substantial out-of-pocket costs, with transportation costs constituting nearly half of the total out-of-pocket expenditures. Because out-of-pocket costs can be a major barrier to long-term adherence, future national investments in RHD control must be strategically directed both at improving health care access and drug supply chains in order to lower the total costs of secondary prophylaxis.
Funding
None.
Declaration of competing interest
None.
Acknowledgements
None.
Contributor Information
Balaji Arvind, Email: drbarvind@gmail.com.
Anita Saxena, Email: anitasaxena@hotmail.com.
Dhruv S. Kazi, Email: dkazi@bidmc.harvard.edu.
Ann F. Bolger, Email: ann.bolger@ucsf.edu.
References
- 1.Carapetis J.R. Rheumatic heart disease in developing countries. N Engl J Med. 2007;357(5):439–441. doi: 10.1056/NEJMp078039. [DOI] [PubMed] [Google Scholar]
- 2.Kumar R.K., Tandon R. Rheumatic fever & rheumatic heart disease: the last 50 years. Indian J Med Res. 2013;137(4):643–658. [PMC free article] [PubMed] [Google Scholar]
- 3.Carapetis J.R., McDonald M., Wilson N.J. Acute rheumatic fever. Lancet. 2005;366(9480):155–168. doi: 10.1016/S0140-6736(05)66874-2. [DOI] [PubMed] [Google Scholar]
- 4.Stollerman G.H., Rusoff J.H., Hirschfeld I. Prophylaxis against group A streptococci in rheumatic fever: the use of single monthly injections of benzathine penicillin G. N Engl J Med. 1955;252(19):787–792. doi: 10.1056/NEJM195505122521901. [DOI] [PubMed] [Google Scholar]
- 5.Remenyi B., Carapetis J., Wyber R. Position statement of the World Heart Federation on the prevention and control of rheumatic heart disease. Nat Rev Cardiol. 2013;10(5):284–292. doi: 10.1038/nrcardio.2013.34. [DOI] [PubMed] [Google Scholar]
- 6.Sustainable Development Goals-17 goals to transform our world. United Nations. 2017. https://www.unorg/sustainabledevelopment/energy Online.
- 7.Executive Board 141 . World Health Organization; Geneva: 2017. Executive Board 141st Session, Geneva, 1 June 2017: Resolutions and Decisions, Annexes, Summary Records [Internet]https://apps.who.int/iris/handle/10665/272288 [Google Scholar]
- 8.Musoke C., Mondo C.K., Okello E. Benzathine penicillin adherence for secondary prophylaxis among patients affected with rheumatic heart disease attending Mulago Hospital : cardiovascular topics. Cardiovasc J Afr. 2013;24(4):124–129. doi: 10.5830/CVJA-2013-022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gasse B., Baroux N., Rouchon B. Determinants of poor adherence to secondary antibiotic prophylaxis for rheumatic fever recurrence on Lifou, New Caledonia: a retrospective cohort study. BMC Publ Health. 2013;13(1):131. doi: 10.1186/1471-2458-13-131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Watkins D.A., Johnson C.O., Colquhoun S.M. Regional, and national burden of rheumatic heart disease, 1990–2015. N Engl J Med. 2017;377(8):713–722. doi: 10.1056/NEJMoa1603693. [DOI] [PubMed] [Google Scholar]
- 11.Bairwa M., Rajput M., Sachdeva S. Modified kuppuswamy’s socioeconomic scale: social researcher should include updated income criteria, 2012. Indian J Community Med. 2013;38(3):185. doi: 10.4103/0970-0218.116358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.What is an “international dollar”? – world Bank data help desk [internet] https://datahelpdesk.worldbank.org/knowledgebase/articles/114944-what-is-an-international-dollar
- 13.Osterberg L., Blaschke T. Adherence to medication. N Engl J Med. 2005;353(5):487–497. doi: 10.1056/NEJMra050100. [DOI] [PubMed] [Google Scholar]
- 14.Choudhry N.K., Avorn J., Glynn R.J. Full coverage for preventive medications after myocardial infarction. N Engl J Med. 2013;365(22):2088–2097. doi: 10.1056/NEJMsa1107913. [DOI] [PubMed] [Google Scholar]
- 15.All India rural financial inclusion survey 2016-17 national bank for aggriculture and rural development. https://www.nabard.org/auth/writereaddata/tender/1608180417NABARD-Repo-16_Web_P.pdf (last accessed June 08, 2020)
- 16.Sandhu Alexander T., Kathikeyan G., Bolger Ann. Abstract 19839: clinical and economic burden of rheumatic heart disease in low-income Nations: estimating the cost-of-illness in India and Uganda. Circulation. 2014;130(suppl_2):A19839. A19839. [Google Scholar]
- 17.Kaplan E.L. Benzathine penicillin G: a documentably important antibiotic in need of a tune-up? Pediatr Infect Dis J. 2012;31(7):726–728. doi: 10.1097/INF.0b013e318259b75c. [DOI] [PubMed] [Google Scholar]
- 18.Taubert K., Marko S.B. Access to essential medicines: illuminating disparities in the global supply of benzathine penicillin G in the context of Rheumatic fever/Rheumatic Heart Disease prevention. J Am Coll Cardiol. 2013;61(10 Supplement):E2004. [Google Scholar]