Abstract
Hereditary disorders of connective tissue (HDCT) compromise a heterogeneous group of diseases caused by pathogenic variants in genes encoding different components of the extracellular matrix and characterized by pleiotropic manifestations, mainly affecting the cutaneous, cardiovascular, and musculoskeletal systems. We report the case of a 9-year-old boy with a discernible connective tissue disorder characterized by cutis laxa (CL) and multiple herniations and caused by biallelic loss-of-function variants in EFEMP1. Hence, we identified EFEMP1 as a novel disease-causing gene in the CL spectrum, differentiating it from other HDCT.
Keywords: FBLN3, EFEMP1, fibulin-3, cutis laxa, elastic fiber, extracellular matrix, inguinal hernia, diaphragmatic hernia
1. Introduction
Hereditary disorders of connective tissue (HDCT) are a heterogeneous group of diseases, mainly affecting the cutaneous, ocular, cardiovascular, pulmonary, and musculoskeletal systems. HDCT are caused by pathogenic variants in genes encoding structural and regulatory components of the extracellular matrix (ECM) [1].
Fibulins belong to a protein family implicated in both elastic fiber (EF) assembly and function. Loss-of-function variants in FBLN4 and FBLN5 both cause severe recessive cutis laxa (CL), characterized by loose redundant skin folds and variable systemic involvement, including prominent emphysema [2,3]. Fibulin-3, encoded by EFEMP1, is a secreted extracellular matrix glycoprotein, which is abundantly expressed in skin fibroblasts, retina, fascia, and vasculature [4]. It is believed to function as an important modulator of ECM biology via its interaction with various ECM molecules, including tropoelastin and (tissue inhibitors of) matrix metalloproteinases [5]. A recurrent gain-of-function variant (p.(Arg345Trp)) in EFEMP1 has previously been associated with Doyne honeycomb retinal dystrophy [6]. However, biallelic pathogenic variants in EFEMP1 were recently reported in two probands with a pronounced connective tissue phenotype, characterized by multiple herniations and joint hypermobility [7,8].
In this study, we present a 9-year-old Turkish boy with a novel, discernible connective tissue disorder characterized by cutis laxa and multiple herniations, associated with biallelic loss-of-function variants in EFEMP1.
2. Materials and Methods
2.1. Consent
The legal guardian of the patient in this manuscript gave written informed consent to publication of the case details. Specific informed consent was obtained for the publication of clinical pictures. This study was conducted in accordance with the 1984 Declaration of Helsinki and its subsequent revisions.
2.2. Molecular Analysis
Exome sequencing (ES) of the proband was performed on genomic DNA extracted from peripheral leukocytes. Target enrichment of the gDNA was obtained by the SureSelectXT Low Input Human All Exon V7 (Agilent Technologies, Santa Clara, CA, USA). Sequencing was performed on a NovaSeq 6000 platform (Illumina, San Diego, CA, USA) with a minimal expected coverage depth of 20×. All obtained variants were analyzed using the Seqplorer software, an in-house developed pipeline, which integrates population frequencies (GnomAD) [9] and in silico splice predictions (e.g., Mutationtaster, PolyPhen, SIFT (sorting tolerant from intolerant), CADD (Combined Annotation Dependent Depletion), Revel (Rare Exome Variant Ensemble Learner), Ada (Adaptive boosting), and RF (Random Forest scores) [10,11,12,13,14,15]. Variants with a minor allele frequency > 0.01 in the GnomAD database were filtered out and the remaining variants were selected according to their functional consequences, whereas only splice-site and stop-gain variants, insertions, deletions, and missense variants were retained. Candidate variants were classified according to the refined American College of Medical Genetics and Genomics (ACMG) guidelines [16,17] and confirmed by Sanger Sequencing on an ABI 3730 platform (Applied Biosystems, Waltham, MA, USA) in the proband and both parents. Obtained sequence profiles were compared with the EFEMP1 reference sequence (Refseq NM_001039348.3).
All variants were reported according to the nomenclature of the Human Genome Variation Society (HGVS, http://www.hgvs.org/VARONEM, accessed on 28 February 2021) [18].
3. Case Presentation
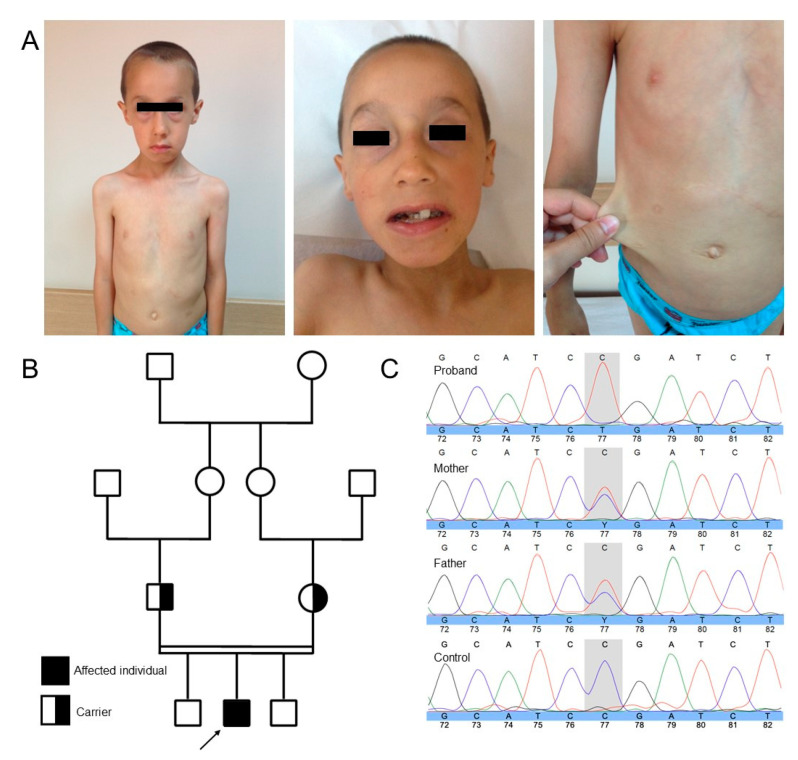
The proband is a boy with suspected HDCT. He was born at term after an uncomplicated pregnancy to consanguineous parents of Turkish origin. At birth, he presented with cutis laxa and a congenital diaphragmatic and right inguinal hernia, which were surgically corrected at the ages of 8 months and 1.5 years, respectively. During clinical examination upon referral aged 7, he showed failure to thrive (length: 112 cm (−0.67 SD); weight: 15.9 kg (−2.5 SD)), despite reportedly normal intake. His head circumference was normal (50 cm (−1.28 SD)). He presented with discernable craniofacial characteristics, including a long face, a high anterior hairline, telecanthus, blepharochalasis, sagging lower eyelids and cheeks, a long philtrum, full lips, downturned mouth corners, retrognathia, dental caries, malocclusion, and cutis laxa (Figure 1A). He further presented with muscle hypotonia and generalized joint hypermobility. His skin was markedly redundant, thin, translucent, and bruised easily. Scars healed normally. Routine laboratory tests including peripheral blood cell analysis, liver and kidney function tests, and coagulation were normal. Although his initial neuromotor development was normal, he showed mild intellectual disability (ID). Hearing, vision, the cardiovascular system, and the urinary tract were assessed as normal. Aged 9, he developed a left inguinal hernia. Exome sequencing identified a homozygous nonsense variant (c.1201C > T, p.(Arg401*)) in EFEMP1 (Figure 1C). This variant is absent in the Gnomad exomes and genomes databases, is classified as “pathogenic” by all used in silico prediction programs, and segregates with disease and carrier status in the reported family.
Figure 1.
(A) Clinical photographs taken at age 7. Note the long face, high anterior hairline, telecanthus, blepharochalasis, sagging lower eyelids and cheeks, long philtrum, full lips, downturned mouth corners, retrognathia, dental caries and malocclusion, and cutis laxa. (B) Pedigree of the reported consanguineous family of Turkish descent. The proband is indicated by the black arrow. (C) Sanger sequencing confirms the presence of a homozygous EFEMP1 nonsense variant (c.1201C > T, p.(Arg401*)) in the proband and identifies both parents as heterozygous carriers.
4. Discussion
We present a 9-year-old Turkish boy with a discernible connective tissue disorder consisting of cutis laxa and multiple herniations with homozygous loss-of-function mutations in EFEMP1 (OMIM#601548), which encodes fibulin-3. Several lines of evidence support the causality of the identified loss-of-function variant for the observed phenotype in the reported individual.
Firstly, fibulin-3 belongs to a family of 8 ECM glycoproteins associated with basement membranes and elastic fibers and is abundantly expressed in skin fibroblasts and fascia [4]. Fibulin-3 is structurally most related to fibulin-4 and -5, both critical molecules for EF assembly. Pathogenic variants in FBLN4 (EFEMP2) and FBLN5 cause autosomal recessive cutis laxa (ARCL) type 1b and 1a, which are associated with severe vasculopathy and developmental pulmonary emphysema, respectively. Of note, the latter condition is also associated with diverticula of the gastrointestinal and genitourinary system, as well as congenital diaphragmatic hernia. ARCL1c, a third disorder within the ARCL type 1 spectrum, shows considerable overlap with ARCL1a and is caused by pathogenic variants in LTBP4, which is an interaction partner of both FBLN4 and FBLN5 [2,3,19].
Secondly, Efemp1-knockout mice demonstrate herniations, loose skin, small body size or mass, atrophy of muscle and fat tissue, and dermal EF fragmentation. Interestingly, the resulting phenotype is highly dependent on the genetic background of the mice, as herniations are predominantly manifested in Efemp1−/− mice on the C57BL/6 background, but not the BALB/c background [20].
Thirdly, biallelic loss-of-function variants in EFEMP1 have previously been reported in 3 individuals of 2 distinctive families with multiple herniations and joint hypermobility, supporting loss-of-function as the molecular mechanism of a novel heritable connective tissue disease (Table 1). Our patient shows significant clinical overlap with the previously reported patients, with hernias of the integument and diaphragm and the presence of discernible facial features (with a long face and downslanted palpebral fissures) [7,8,21]. In contrast to the previously published individuals, our patient did not present with scoliosis, pectus deformity, or myopia. He further exhibited mild ID, which usually manifests in patients with ARCL type 2 and 3, but has not been associated with ARCL type 1 [19,22,23]. Exome analysis did not identify other pathogenic variants that could explain the ID, however this does not exclude genetic and non-genetic causes of ID. Our proband had a normal cardiovascular and pulmonary work-up, while multiple pulmonary bullae developed during puberty in one individual with biallelic truncating variants in EFEMP1 [8]. Although several mild cutaneous features were present in 3 patients, our proband was the only case exhibiting cutis laxa and easy bruising with infantile onset [7,8,21]. Of note, pulmonary emphysema was only reported in one patient [8]. Overall, this report adds evidence that biallelic loss-of-function variants in EFEMP1 are associated with a specific connective tissue disorders characterized by multiple hernias and skeletal and pulmonary manifestations. Although clinically variable, this disorder should be classified within the group of ARCL type 1 [7,8,19,21].
Table 1.
Summary of molecular and clinical characteristics of individuals with EFEMP1 pathogenic variants and comparison with ARCL type 1.
| EFEMP1-Related CL | ARCL1a | ARCL1b | ARCL1c | ||||
|---|---|---|---|---|---|---|---|
| This study | Bizzari et al. [7] | Driver et al. [8] | Beyens et al. [24] | ||||
| Mégarbané et al. [21] | |||||||
| Clinical characteristics | |||||||
| Craniofacial dysmorphism | + a | + a | + a | + a | + b | + c | + d |
| Dental crowding | − | + | + | − | − | − | − |
| Cutis laxa | + | − | − | − | + | + | + |
| Thin translucent skin | + | − | − | + | − | − | + |
| Diaphragmatic hernia | + | − | + | + | + | + | + |
| Inguinal hernia | + | + | + | + | + | + | + |
| Hypermobile joints | + | + | + | + | + | + | + |
| Muscle hypotonia | + | + | + | + | − | − | + |
| Scoliosis | − | − | + | + | − | + | − |
| Pectus deformities | − | + | + | + | − | + | + |
| Tall Stature | − | + | + | + | − | − | − |
| Aortopathy | − | − | − | − | + | + | + |
| Emphysema | − | − | − | + | + | − | + |
| Gastrointestinal abnormalities | − | + | + | − | − | − | + |
| Bladder diverticula | − | + | + | + | + | − | + |
| Molecular characteristics | EFEMP1 | EFEMP1 | EFEMP1 | EFEMP1 | FBLN5 | FBLN4 | LTBP4 |
| cDNA level | c.1201C > T | c.163T > C | c.163T > C | c.320_324delTG GCA c. 615T > A |
|||
| Protein level | p.(Arg401*) | p.(Cys55Arg) | p.(Cys55Arg) | p. (Met107fs) p.(Tyr205*) |
|||
| Zygosity | Homozygous | Homozygous | Homozygous | Heterozygous | |||
| Other | VCPKMT and MYO3 variants | ||||||
Note: ARCL, autosomal recesssive cutis laxa; +: characteristic present; −: not present; a: long face, telecanthus, downslanted palpebral fissures; b: high anterioir hairline, hypertelorism; c: high anterior hairline, large ears, broad nose, sagging cheecks; d: high anterior hairline, large ears, long philtrum; Grey background color indicates that the data refer to what is generally observed in ARCL1a, ARCL1b, or ARCL1c. Based on these data and the following papers: Bizzari et al. (2020) [7], Megarbane et al. (2012) [21], Driver et al. (2020) [8], and Beyens et al. (2020) [24].
In conclusion, biallelic loss-of-function variants in EFEMP1 cause a novel HDCT characterized by cutis laxa and recurrent herniations. As these patients additionally present with mild cutaneous and pulmonary manifestations, we propose this HDCT to be a classified as a subtype of ARCL type 1. This observation confirms that EFEMP1 has a pivotal role in abdominal wall integrity.
Acknowledgments
The authors thank the family for their kind availability in sharing the findings within the scientific community.
Author Contributions
Conceptualization, M.V. (Maxim Verlee), A.B., L.P., S.D.F., and B.C.; methodology, L.P., M.V. (Michiel Vanhooydonck), P.T., and S.S.; validation, S.S. and B.C.; formal analysis, M.V. (Maxim Verlee) and A.B.; investigation, M.V. (Maxim Verlee), A.B., A.G., and E.Y.G.; resources, A.G., E.Y.G., and B.C.; data curation, M.V. (Michiel Vanhooydonck), A.B., S.S., and B.C.; writing—original draft preparation, M.V. (Michiel Vanhooydonck) and A.B.; writing—review and editing, all authors; visualization, M.V. (Maxim Verlee), A.B., and L.P.; supervision, B.C.; project administration, B.C.; funding acquisition, B.C. All authors have read and agreed to the published version of the manuscript.
Funding
A.B. is supported by the Special Research Fund, Flanders of Ghent University (Belgium, grant 01N04516C to B.C.). This work is further supported by the Research Foundation Flanders (project G035620N to B.C.) and European Academy of Dermatovenereology (Switzerland, EADV project PPRC-2018-50 to B.C.). B.C. is a senior clinical investigator of the Research Foundation Flanders. The Ghent University Hospital is a member of the European Reference Network for Skin Disorders (ERN-Skin).
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Institutional Review Board (or Ethics Committee) of Ghent University Hospital (protocol code BC-07240 and date of approval 2 June 2020).
Informed Consent Statement
Written informed consent has been obtained from the patient (or legal guardian in case of minor) to publish this paper. Specific informed consent was obtained for the publication of clinical pictures. The ethic code number is B6702020000194.
Data Availability Statement
Data available in a publicly accessible repository. The data presented in this study are openly available in Clinvar, and the accession number is ‘SCV001548232.1’.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Murphy-Ryan M., Psychogios A., Lindor N.M. Hereditary disorders of connective tissue: A guide to the emerging differential diagnosis. Genet. Med. 2010;12:344–354. doi: 10.1097/GIM.0b013e3181e074f0. [DOI] [PubMed] [Google Scholar]
- 2.Elahi E., Kalhor R., Banihosseini S.S., Torabi N., Pour-Jafari H., Houshmand M., Amini S.S., Ramezani A., Loeys B. Homozygous missense mutation in fibulin-5 in an iranian autosomal recessive cutis laxa pedigree and associated haplotype. J. Investig. Dermatol. 2006;126:1506–1509. doi: 10.1038/sj.jid.5700247. [DOI] [PubMed] [Google Scholar]
- 3.Hucthagowder V., Sausgruber N., Kim K.H., Angle B., Marmorstein L.Y., Urban Z. Fibulin-4: A novel gene for an autosomal recessive cutis laxa syndrome. Am. J. Hum. Genet. 2006;78:1075–1080. doi: 10.1086/504304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yanagisawa H., Davis E.C. Unraveling the mechanism of elastic fiber assembly: The roles of short fibulins. Int. J. Biochem. Cell Biol. 2010;42:1084–1093. doi: 10.1016/j.biocel.2010.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Livingstone I., Uversky V.N., Furniss D., Wiberg A. The Pathophysiological Significance of Fibulin-3. Biomolecules. 2020;10:1294. doi: 10.3390/biom10091294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Stone E.M., Lotery A.J., Munier F.L., Héon E., Piguet B., Guymer R.H., VanDenburgh K., Cousin P., Nishimura D., Swiderski R.E., et al. A single EFEMP1 mutation associated with both Malattia Leventinese and Doyne honeycomb retinal dystrophy. Nat. Genet. 1999;22:199–202. doi: 10.1038/9722. [DOI] [PubMed] [Google Scholar]
- 7.Bizzari S., El-Bazzal L., Nair P., Younan A., Stora S., Mehawej C., El-Hayek S., Delague V., Mégarbané A. Recessive marfanoid syndrome with herniation associated with a homozygous mutation in Fibulin-3. Eur. J. Med. Genet. 2020;63:103869. doi: 10.1016/j.ejmg.2020.103869. [DOI] [PubMed] [Google Scholar]
- 8.Driver S.G.W., Jackson M.R., Richter K., Tomlinson P., Brockway B., Halliday B.J., Markie D.M., Robertson S.P., Wade E.M. Biallelic variants in EFEMP1 in a man with a pronounced connective tissue phenotype. Eur. J. Hum. Genet. 2019;28:445–452. doi: 10.1038/s41431-019-0546-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Karczewski K.J., Francioli L.C., Tiao G., Cummings B.B., Alfoeldi J., Wang Q.S., Collins R.L., Laricchia K.M., Ganna A., Birnbaum D.P., et al. The mutational constraint spectrum quantified from variation in 141,456 humans. Nature. 2020;581:434–443. doi: 10.1038/s41586-020-2308-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Adzhubei I., Jordan D.M., Sunyaev S.R. Predicting functional effect of human missense mutations using PolyPhen-2. Curr. Protoc. Hum. Genet. 2013;76:7.20.1–7.20.41. doi: 10.1002/0471142905.hg0720s76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Schwarz J.M., Rödelsperger C., Schuelke M., Seelow D. MutationTaster evaluates disease-causing potential of sequence alterations. Nat. Methods. 2010;7:575–576. doi: 10.1038/nmeth0810-575. [DOI] [PubMed] [Google Scholar]
- 12.Ng P.C., Henikoff S. SIFT: Predicting amino acid changes that affect protein function. Nucleic Acids Res. 2003;31:3812–3814. doi: 10.1093/nar/gkg509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rentzsch P., Witten D., Cooper G.M., Shendure J., Kircher M. CADD: Predicting the deleteriousness of variants throughout the human genome. Nucleic Acids Res. 2019;47:D886–D894. doi: 10.1093/nar/gky1016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ioannidis N.M., Rothstein J.H., Pejaver V., Middha S., McDonnell S.K., Baheti S., Musolf A., Li Q., Holzinger E., Karyadi D., et al. REVEL: An ensemble method for predicting the pathogenicity of rare missense variants. Am. J. Hum. Genet. 2016;99:877–885. doi: 10.1016/j.ajhg.2016.08.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Breiman L. Random forests. Mach. Learn. 2001;45:5–32. doi: 10.1023/A:1010933404324. [DOI] [Google Scholar]
- 16.Tavtigian S.V., Greenblatt M.S., Harrison S.M., Nussbaum R.L., Prabhu S.A., Boucher K.M., Biesecker L.G., on behalf of the ClinGen Sequence Variant Interpretation Working Group (ClinGen SVI) Modeling the ACMG/AMP variant classification guidelines as a Bayesian classification framework. Genet. Med. 2018;20:1054–1060. doi: 10.1038/gim.2017.210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nykamp K., Anderson M., Powers M., Garcia J., Herrera B., Ho Y.-Y., Kobayashi Y., Patil N., Thusberg J., Westbrook M., et al. Sherloc: A comprehensive refinement of the ACMG–AMP variant classification criteria. Genet. Med. 2017;19:1105–1117. doi: 10.1038/gim.2017.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.den Dunnen J.T., Dalgleish R., Maglott D.R., Hart R.K., Greenblatt M.S., McGowan-Jordan J., Roux A.-F., Smith T., Antonarakis S.E., Taschner P.E.M., et al. HGVS recommendations for the description of sequence variants: 2016 update. Hum. Mutat. 2016;37:564–569. doi: 10.1002/humu.22981. [DOI] [PubMed] [Google Scholar]
- 19.Callewaert B., Su C.-T., Van Damme T., Vlummens P., Malfait F., Vanakker O., Schulz B., Mac Neal M., Davis E.C., Lee J.G., et al. Comprehensive Clinical and Molecular Analysis of 12 Families with Type 1 Recessive Cutis Laxa. Hum. Mutat. 2013;34:111–121. doi: 10.1002/humu.22165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.McLaughlin P.J., Bakall B., Choi J., Liu Z., Sasaki T., Davis E.C., Marmorstein A.D., Marmorstein L.Y. Lack of fibulin-3 causes early aging and herniation, but not macular degeneration in mice. Hum. Mol. Genet. 2007;16:3059–3070. doi: 10.1093/hmg/ddm264. [DOI] [PubMed] [Google Scholar]
- 21.Megarbane A., Hanna N., Chouery E., Jalkh N., Mehawej C., Boileau C. Marfanoid habitus, inguinal hernia, advanced bone age, and distinctive facial features: A new collagenopathy? Am. J. Med. Genet. Part A. 2012;158:1185–1189. doi: 10.1002/ajmg.a.35279. [DOI] [PubMed] [Google Scholar]
- 22.Morava E., Lefeber D.J., Urban Z., De Meirleir L., Meinecke P., Kaesbach G.G., SykutCegielska J., Adamowicz M., Salafsky I., Ranells J.D., et al. Defining the phenotype in an autosomal recessive cutis laxa syndrome with a combined congenital defect of glycosylation. Eur. J. Hum. Genet. 2007;16:28–35. doi: 10.1038/sj.ejhg.5201947. [DOI] [PubMed] [Google Scholar]
- 23.Kivuva E.C., Parker M.J., Cohen M.C., Wagner B.E., Sobey G. De Barsy syndrome: A review of the phenotype. Clin. Dysmorphol. 2008;17:99–107. doi: 10.1097/MCD.0b013e3282f4a964. [DOI] [PubMed] [Google Scholar]
- 24.Beyens A., Boel A., Symoens S., Callewaert B. Cutis laxa: A comprehensive overview of clinical characteristics and pathophysiology. Clin. Genet. 2021;99:53–66. doi: 10.1111/cge.13865. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data available in a publicly accessible repository. The data presented in this study are openly available in Clinvar, and the accession number is ‘SCV001548232.1’.