Abstract
Acral melanoma (AM) is a rare and aggressive subtype of melanoma affecting the palms, soles, and nail apparatus with similar incidence among different ethnicities. AM is unrelated to ultraviolet radiation and has a low mutation burden but frequent chromosomal rearrangements and gene amplifications. Next generation sequencing of 33 genes and somatic copy number variation (CNV) analysis with genome-wide single nucleotide polymorphism arrays were performed in order to molecularly characterize 48 primary AMs of Italian patients in association with clinicopathological and prognostic features. BRAF was the most commonly mutated gene, followed by NRAS and TP53, whereas TERT promoter, KIT, and ARID1A were less frequently mutated. Gains and losses were recurrently found in the 1q, 6p, 7, 8q, 20 and 22 chromosomes involving PREX2, RAC1, KMT2C, BRAF, CCND1, TERT, and AKT3 genes, and in the 6q, 9, 10, 11q and 16q chromosomes including CDKN2A, PTEN, and ADAMTS18 genes, respectively. This study confirmed the variety of gene mutations and the high load of CNV in primary AM. Some genomic alterations were associated with histologic prognostic features. BRAF mutations, found with a higher rate than previously reported, correlated with a low Breslow thickness, low mitotic count, low CNV of the AMs, and with early-stage of disease.
Keywords: acral melanoma, BRAF, NRAS, PREX2, ARID1A, KIT, TP53, TERT promoter, copy number variations
1. Introduction
Acral melanoma (AM) is a rare subtype of malignant melanoma that originates from the glabrous skin of the palms, soles, and nail apparatus (subungual) [1]. The more commonly affected sites are the great toe and the thumb [2]. Although its annual incidence is similar among the different racial groups worldwide, settling at about 1 case per 100,000 people, in proportion AM is relatively rare in the European-derived population but common in Asian, African, and Hispanic people [2,3]. Moreover, for this reason, most studies focused on these last ethnicities. AM prognosis is quite poor, with a five-year overall survival (OS) ranging from 59% to 70%, mainly as a consequence of delayed diagnosis due to the unusual localization and of the effect of the different histotypes and molecular backgrounds [4,5,6,7,8]. Patients with AM are typically diagnosed at an advanced stage of disease with thick and ulcerated primary tumor and a high likelihood of metastases [4,5,6,7,8]. The treatment is the same as for the other cutaneous melanomas: wide surgical removal of the primary tumor and, if feasible, of regional nodal metastases for local disease and immunotherapy or targeted therapy (more rarely chemotherapy) for metastatic disease [9]
From the pathological point of view, AM is classified as acral lentiginous melanoma (ALM), which is the most common and aggressive form, superficial spreading melanoma (SSM), nodular melanoma (NM), and nevoid melanoma [9,10,11,12,13,14]. These differ not only in morphology but also in etiology, pathogenesis, and underlying molecular alterations [10]. Compared to other non-acral cutaneous melanomas showing a high number of mutations induced by ultraviolet (UV) radiation, this appears to be a less important etiologic factor for AM since this type of tumor has a low mutation burden and several chromosomal rearrangements and gene amplifications [15,16,17,18,19,20,21,22,23]. The reported frequencies of gene mutations vary in the different studies and this is probably due to the low number of analyzed cases, the predominant use of metastatic material, and the inclusion of different histotypes of melanoma in the casuistries. BRAF mutations have been reported to occur at a significantly lower rate in AM than in other non-acral skin melanomas (about 10–20% of cases versus 50% of cases, respectively) [15,16,17,18,23]. Mutated NRAS and KIT have been detected in about 15% of cases, with a respective range of 7–47% and 6–21% among the studies [16,17,22,23,24,25,26,27,28]. TP53 mutations have been reported as a rare and late event in AM [16,19,29]. Instead, mutations in NF1 and amplification of KIT, CCND1, PAK1, GAB2, CDK4, RICTOR, and TERT, have been more commonly found in AM than in other skin melanomas [16,19,20,28].
This study aimed to characterize the molecular landscape of primary AM in an Italian cohort of patients and to assess the possible associations of molecular alterations with the clinicopathological features and the prognosis of patients.
2. Results
2.1. Patients’ Characteristics
Of the original series of 74 FFPE AM samples, 26 (19%) did not yield amplifiable DNA for molecular analysis. The remaining 48 patients (81%) with analyzable samples had a mean age of 71.2 ± 13.2 years (range 47–88 years) and a male to female ratio of 1:1. The clinicopathological features of patients are summarized in Table 1. Most AMs were located in the foot (79%), followed by nail (15%) and hand (6%). The most common histotype was acral lentiginous melanoma (83%), followed by nodular melanoma (13%), superficial spreading melanoma (2%), and nevoid melanoma (2%). The vast majority of AMs were locally advanced (T3 and T4 stages; 80%). Ulceration was a common feature, being present in 58% of cases. Regression and lymphovascular and perineural invasion were present in 8%, 32%, and 23% of AMs, respectively.
Table 1.
Clinical and pathological characteristics of the 48 molecularly analyzed patients.
| Clinical and Pathological Variables | |
|---|---|
| Age at diagnosis (yrs) | |
| Mean (SD) | 71.2 (13.2) |
| Range | 47–88 |
| Breslow thickness (mm) | |
| Mean (SD) | 5.1 (3.7) |
| Range | 0.7–19.2 |
| Mitoses (number/mm2) | |
| Mean (SD) | 8.3 (8.4) |
| Range | 0–45 |
| Gender (n, %) | |
| Male | 24 (50%) |
| Female | 24 (50%) |
| Tumor site (n, %) | |
| Hand | 3 (6%) |
| Foot | 38 (79%) |
| Nail | 7 (15%) |
| Histotype (n, %) | |
| ALM | 40 (83%) |
| NM | 6 (13%) |
| SSM | 1 (2%) |
| Nevoid melanoma | 1 (2%) |
| pT classification (n, %) | |
| T1 | 1 (2%) |
| T2 | 6 (13%) |
| T3 | 16 (33%) |
| T4 | 23 (47%) |
| NE | 2 (5%) |
| Ulceration (n, %) | |
| Absent | 18 (37%) |
| Present | 28 (58%) |
| NE | 2 (5%) |
| Regression (n, %) | |
| Absent | 42 (87%) |
| Present | 4 (8%) |
| NE | 2 (5%) |
| Lymphovascular Invasion (n, %) | |
| Absent | 30 (62%) |
| Present | 15 (32%) |
| NE | 3 (6%) |
| Perineural invasion (n, %) | |
| Absent | 34 (71%) |
| Present | 11 (23%) |
| NE | 3 (6%) |
SD = standard deviation; ALM = acral lentiginous melanoma; NM = nodular melanoma; SSM = superficial spreading melanoma; NE = not evaluable.
2.2. Molecular Classification
Forty AM cases were stratified into the four TCGA classification groups based on the genotyping analysis by a 33-gene next generation sequencing (NGS) custom panel (30 samples) and hotspot Sanger sequencing (10 samples). Eight cases failed sequencing analysis. A frequency of mutually exclusive mutations of 35% for BRAF, 28% for NRAS, and 5% for NF1 genes was found; the remaining 32% of AMs were classified as triple wild-type (TWT). BRAF mutations were a p.V600E substitution in all cases but one (93%) with p.V600D substitution. BRAF mutations were found in all the four histotypes, with a frequency of 32% in acral lentiginous melanoma. NRAS mutations were missense in the p.Q61 codon for 8 cases (3 p.Q61R, 2 p.Q61K, 2 p.Q61H, and 1 p.Q61L) or the p.G12 codon for 3 cases (2 p.G12D and 1 p.G12C cases). These last mutations were found in two acral lentiginous melanomas and in a nodular melanoma. Overall, NRAS mutations were present in 29% of acral lentiginous melanomas. The two observed NF1 mutations were a p.G453D missense and p.K1345* nonsense unreported mutations, detected in a nodular melanoma and in an acral lentiginous melanoma, respectively.
We extended the mutational analysis of thirty cases to the main genes involved in melanoma pathogenesis using a custom-designed NGS panel (the genes included in the panel are reported in Supplementary Table S1). Overall, variants in at least one of 33 tested genes were identified in 26 of the 30 analyzed samples (87%) (mutations are reported in Supplementary Table S2). The TP53 gene was mutated in 9 cases (30%; all acral lentiginous melanomas except for a nodular melanoma), frequently in association with BRAF mutations (5 out of 9 samples). KIT mutations were detected exclusively in three acral lentiginous melanomas (10%); in one case it was found in association with a NF1 mutation and in another with a NRAS mutation. TERT promoter mutations were found in 4 cases (13%): two acral lentiginous melanomas also harbored a BRAF mutation, another a NRAS mutation, while a nodular melanoma harbored a NF1 mutation. Among the genes that mutated in more than one AM and mutually exclusive with the TCGA genes, we found 3 ARID1A mutations in TWT samples: p.Trp1670* and p.Glu1291Asp mutations reported as pathogenic variants in the Catalogue of Somatic Mutations in Cancer (COSMIC https://cancer.sanger.ac.uk/cosmic, accessed on 10 March 2021) and p.Thr1514Met unreported variant. In addition, we found 3 GRIN2A, 2 PTEN and 2 SF3B1 mutated cases. A single mutated AM was detected for KMT2C, MITF, BAP1, NOTCH2, NOTCH1, DCC, DDX3X, ADAMTS18, PIK3CA, RB1, KRAS, PREX2, ERBB4, KDR, and MAP2K2 genes (Supplementary Table S2).
2.3. Molecular Classification and Clinicopathological Features
Associations between the TCGA molecular classification and the clinicopathological characteristics of patients are shown in Table 2. Statistical analyses compared BRAF vs. NRAS vs. TWT groups (the NF1 group was excluded due to the small sample size). The TWT status was strongly associated with AM originating from the nail (p = 0.01), accounting for 4 out of 5 cases (80%). BRAF-mutated AM was related to a lower Breslow thickness (p = 0.02), a lower mitotic count (p < 0.01), and pT1-T2 stages (p = 0.03).
Table 2.
Clinical and pathological characteristics of the 40 patients with mutational data according to the TCGA classification.
| Clinical and Pathological Variables | BRAF | NF1 | NRAS | TWT | p-Value a |
|---|---|---|---|---|---|
| N patients | 14 | 2 | 11 | 13 | - |
| Age, yrs: median (IQR) | 70 (57–85) | 50; 86 | 74 (65–76) | 70 (61–79) | 0.99 |
| Breslow thickness, mm: median (IQR) | 2.4 (1.7–4.0) | 6.9; 8.6 | 3.7 (3.3–5.3) | 4.6 (3.7–7.0) | 0.02 |
| Mitoses, number/mm2: median (IQR) | 2 (1–5) | 10; 15 | 4 (4–5) | 7 (5–20) | 0.007 |
| Tumor site: n (%) | 0.01 | ||||
| Hand/foot | 14 (40%) | 1 (3%) | 11 (31%) | 9 (26%) | |
| Nail | 0 (0) | 1 (20%) | 0 (0) | 4 (80%) | |
| Histotype: n (%) | 0.60 b | ||||
| ALM | 11 (32%) | 1 (3%) | 10 (29%) | 12 (36%) | |
| Nevoid melanoma | 1 (100%) | 0 (0) | 0 (0) | 0 (0) | |
| NM | 1 (25%) | 1 (25%) | 1 (25%) | 1 (25%) | |
| SSM | 1 (100%) | 0 (0) | 0 (0) | 0 (0) | |
| pT classification: n (%) c | 0.03 | ||||
| T1-T2 | 5 (83%) | 0 (0) | 0 (0) | 1 (17%) | |
| T3-T4 | 8 (25%) | 2 (7%) | 11 (34%) | 11 (34%) | |
| Ulceration: n (%) c | 0.26 | ||||
| Absent | 7 (44%) | 0 (0) | 6 (37%) | 3 (19%) | |
| Present | 6 (27%) | 2 (9%) | 5 (23%) | 9 (41%) | |
| Regression: n (%) c | 0.55 | ||||
| Absent | 11 (31%) | 2 (5%) | 11 (32%) | 11 (32%) | |
| Present | 2 (67%) | 0 (0) | 0 (0) | 1 (33%) | |
| Lymphovascular Invasion: n (%) c | 0.90 | ||||
| Absent | 8 (31%) | 2 (8%) | 7 (27%) | 9 (34%) | |
| Present | 4 (36%) | 0 (0) | 4 (36%) | 3 (28%) | |
| Perineural invasion: n (%) c | 0.37 | ||||
| Absent | 11 (39%) | 1 (6%) | 8 (26%) | 8 (29%) | |
| Present | 1 (11%) | 1 (11%) | 3 (33%) | 4 (45%) |
ap-value calculated comparing BRAF mutated vs. NRAS mutated vs. triple wild-type (TWT) cases; the 2 NF1 mutated cases were excluded; b p-value calculated comparing ALM vs. Nevoid/NM/SSM cases; c cases without evaluable data were excluded (Table 1, NE cases); IQR: interquartile range; ALM = acral lentiginous melanoma; NM = nodular melanoma; SSM = superficial spreading melanoma.
2.4. Genomic Copy Number Alterations
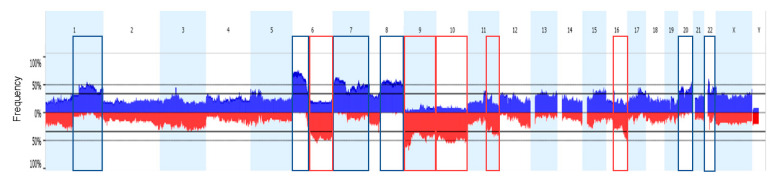
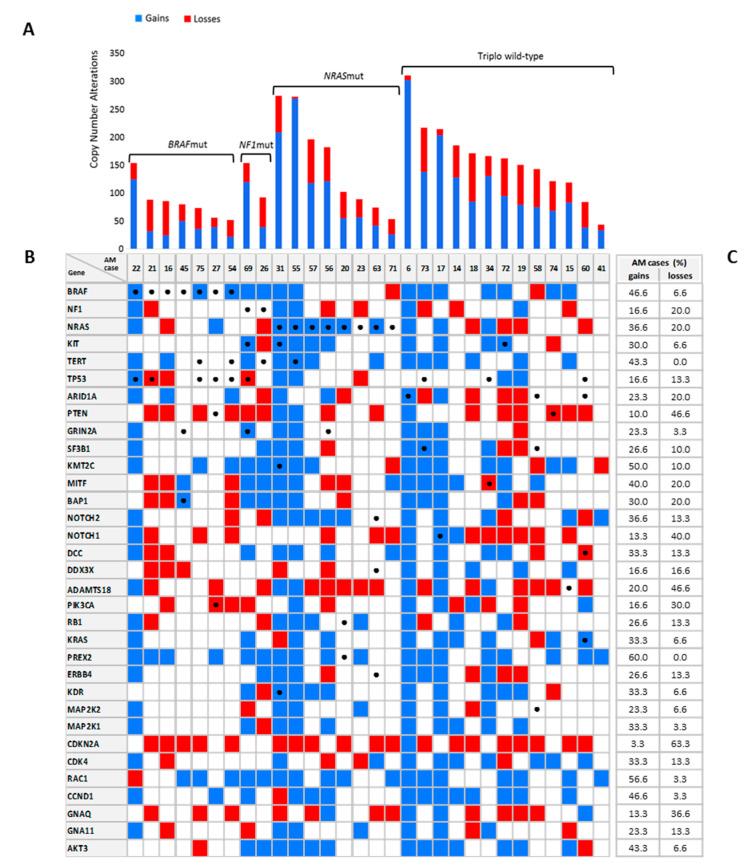
Somatic copy number variations (CNV) data were obtained using genome-wide single nucleotide polymorphism (SNP) arrays in 42 out of 48 analyzed AM samples. For all probes covering each locus, the average copy number was defined as a gain or loss if >2.0 or <2.0, respectively. In addition, a broader estimate concerning the percentage of genome changes was assessed, also considering the focal regions of loss of heterozygosis (LOH) and copy number (CN) neutral LOH. Overall, AMs showed a high percentage of genome change (median 34%, 2–91%) with a median of 121 CNVs (range 7–311). A high intertumoral heterogeneity with tetraploid samples and samples with only focal gains or losses were observed. Worth noting is that the AM (AM_43) with the lowest CNVs (n = 7) was the thin nevoid melanoma without ulceration and mitoses morphologically resembling a common nevus. On the other hand, the three cases presenting more than 80% of genome changes with more than 270 CNVs referred to locally advanced acral lentiginous melanomas with almost 65% of tetraploid tumor cells (data not shown) and with ulceration and number of mitoses/mm2 ≥ 4. In total, 66% of all identified CNVs were gains or amplifications mainly affecting both arms of the 7, 20, and 22 chromosomes and arm of the 1q, 6p, and 8q chromosomes (Figure 1). Among the sequenced genes, gains in PREX2 (60% of cases), RAC1 (57%), KMT2C (50%), BRAF (47%), CCND1 (47%), TERT (47%), and AKT3 (43%) genes were frequently observed. On the other hand, 34% of the CNVs were losses in the genomic region frequently spanning the 6q, 9, 10, 11q, and 16q chromosomes and more frequently involved in the CDKN2A (63% of cases), PTEN (47%) and ADAMTS18 (47%) genes (Figure 2B,C).
Figure 1.
Whole-genome copy number profile. Aggregate frequency plot of copy number variations (CNVs) for 42 acral melanomas (AMs). Blue and red indicates gains and losses, respectively. The y-axis indicates the percentage of the samples in the cohort having an aberration at a specific point along the genome. Regions more frequently involved in gain and losses events are highlighted in blue and red boxes respectively.
Figure 2.
Copy number changes and mutations in melanoma driver genes in 30 AMs. (A) Copy number gains (blue) and losses (red) for each AM sample according to TCGA classification (BRAF/NRAS/NF1 mutated and triple wild-type (TWT)). (B) Mutation and CNV analysis in 33 selected melanoma genes. For each AM sample, gene gains in blu and gene losses in red are reported. Genetic mutations are indicated by black dots. (C) Frequency of AM cases with gains and losses in the genes analyzed by next generation sequencing (NGS).
2.5. Genomic Copy Number, Molecular, and Clinicopathological Features
Combining all CNVs into TCGA molecular subgroups (Figure 2A), BRAF-mutated cases (median 78, range 61–89) showed a significant lower count of aberrations compared to NRAS (median 103, range 90–197) and TWT cases (median 163; range 122–186; p = 0.03; Table 3). Moreover, this different distribution corresponded to a significant difference in the number of gains (p = 0.04) rather than losses (p = 0.28). Total CNVs was higher in thicker AM (p = 0.04), as well as in AM with ulceration (p = 0.03). In these latter cases, the gains were statistically more than in AM without ulceration (p = 0.02). Poor histologic prognostic factors, such as high Breslow thickness, high mitotic count, and presence of ulceration were associated with the percentage of changed genome (p = 0.003, 0.004, and 0.0002, respectively). Although not statistically significant due to the small sample size, the number of CNVs and the percentage of changed genome in pT3-4 cases (median CNVs 144; changed genome 42%) were almost twice those of pT1-2 cases (median CNVs 73; changed genome 22%).
Table 3.
Clinicopathological characteristics and molecular data of the 42 patients with CNV analysis.
| Clinical and Pathological Variables | Total CN Alterations | Gains | Losses | Percentage of Changed Genome | ||||
|---|---|---|---|---|---|---|---|---|
| Summary Measures | p-Value | Summary Measures | p-Value | Summary Measures | p-Value | Summary Measures | p-Value | |
|
Age (yrs) (n = 42), Spearman correlation coefficient |
0.21 | 0.19 | 0.28 | 0.07 | 0.15 | 0.33 | 0.06 | 0.70 |
|
Breslow thickness (mm) (n = 40), Spearman correlation coefficient |
0.31 | 0.04 | 0.23 | 0.16 | 0.29 | 0.07 | 0.45 | 0.003 |
|
Mitoses (number/mm2) (n = 41), Spearman correlation coefficient |
0.24 | 0.13 | 0.17 | 0.30 | 0.29 | 0.07 | 0.44 | 0.004 |
| TCGA classification, | ||||||||
| BRAF (n = 12), median (IQR) | 78 (61–89) | 0.03 a | 39 (27–56) | 0.04 a | 30 (20–51) | 0.28 a | 29 (19–36) | 0.23 a |
| NF1 (n = 2), median (IQR) | 93; 155 | 40; 121 | 34; 53 | 55; 57 | ||||
| NRAS (n = 11), median (IQR) | 103 (90–197) | 58 (43–122) | 47 (32–62) | 30 (23–67) | ||||
| TWT (n = 13), median (IQR) | 163 (122–186) | 86 (76–131) | 53 (36–68) | 35 (33–68) | ||||
| Tumor site | 0.99 | 0.93 | 0.89 | 0.64 | ||||
| Hand/foot (n = 36), median (IQR) | 113 (81–175) | 69 (39–123) | 47 (30–63) | 33 (24–68) | ||||
| Nail (n = 6), median (IQR) | 133 (100–158) | 73 (47–91) | 53 (22–64) | 46 (33–66) | ||||
| Histotype | 0.09 | 0.07 | 0.34 | 0.67 | ||||
| ALM (n = 35), median (IQR) | 151 (88–178) | 84 (42–124) | 53 (30–67) | 34 (25–68) | ||||
| Nevoid/NM (n = 7), median (IQR) | 85 (68–99) | 40 (33–49) | 46 (26–57) | 42 (21–54) | ||||
| Ulceration | 0.03 | 0.02 | 0.36 | 0.0002 | ||||
| Absent (n = 15), median (IQR) | 89 (65–145) | 40 (30–78) | 53 (22–61) | 25 (20–32) | ||||
| Present (n = 25), median (IQR) | 155 (99–199) | 86 (51–138) | 53 (30–67) | 53 (33–70) | ||||
| Lymphovascular Invasion | 0.31 | 0.77 | 0.59 | 0.38 | ||||
| Absent (n = 26), median (IQR) | 113 (74–171) | 64 (40–122) | 42 (28–66) | 34 (24–57) | ||||
| Present (n = 13), median (IQR) | 155 (98–197) | 86 (36–119) | 61 (36–62) | 37 (30–69) | ||||
| Perineural invasion | 0.46 | 0.58 | 0.42 | 0.47 | ||||
| Absent (n = 28), median (IQR) | 114 (75–165) | 64 (38–124) | 42 (25–66) | 39 (25–69) | ||||
| Present (n = 11, median (IQR) | 168 (96–185) | 86 (49–121) | 61 (45–62) | 31 (26–54) | ||||
ap-value calculated comparing BRAF mutated vs. NRAS mutated vs. TWT cases; ALM = acral lentiginous melanoma; NM = nodular melanoma.
2.6. Survival
The median follow-up of the 42 patients with molecular data was 41 months (IQR 17–68) and, during the study period, 20 patients had tumor recurrence (48%). The five-year DFS was 43% (95% CI 28–65%), while the five-year OS was 50% (95% CI 36–71%). The association between survival and clinically relevant factors is reported in Supplementary Table S3. High Breslow thickness and ulceration were associated with impaired DFS (HR 1.20, 95% CI 1.05 to 1.36, p = 0.008 and HR 6.83, 95% CI 1.13 to 29.90, p = 0.01, respectively). Older age (HR 1.05, 95% CI 1.02 to 1.09; p = 0.005) and high Breslow values (HR 1.26, 95% CI 1.13 to 1.40; p < 0.0001) were associated with impaired OS.
3. Discussion and Conclusions
AM is a rare subtype of malignant melanoma occurring in the non-hair-bearing skin of the palms, soles, and nail apparatus [1]. Despite a similar incidence among different ethnicities, AM is the commonest melanoma in Asian, African, and Hispanic people, given the low incidence of other cutaneous melanomas [1,2,3,14]. Most studies on AM were mainly conducted on these populations and European-derived people were often marginally included [15,16,17,18,19,20,21,22,23]. The present study attempted to add information for this last group by analyzing an Italian cohort of patients. Moreover, it focused on primary tumors, whereas most of the available molecular data on AM were derived from metastatic tissues which, therefore, may have accumulated more molecular alterations. However, this choice, along with that of using FFPE archival material, led to technical difficulties. Indeed, on the one hand, neoplastic material was frequently scarce because lesions were small. On the other, nucleic acids were often damaged by treatments with acid solutions used for bone decalcification and/or with sodium hydroxide solutions for nail softening present in the surgical samples and degraded by formalin fixation and long-lasting storage times. This affected the yield of extraction and amplifiability of the DNA in about 20% of initial samples. However, the remaining casuistry showed clinical features similar to those reported in the literature, such as presentation in old age, no gender predilection, main occurrence on the foot and 15% of subungual cases, and predominance of the acral lentiginous melanoma histotype, supporting its validity [1,10].
Overall, the current results confirmed the low mutational burden and the high percentage of genomic changes of AM, as previously reported [15,16,17,18,19,20,21,22,23]. Worth noting is that all the molecular alterations were detected in primary tumors, highlighting that they are probably early events in the development and progress of AM. Moreover, a gradient was observed in the accumulation of genomic structural alterations with a higher number of CNVs and percentage of changed genome in locally advanced AM.
According to the literature, the rate of BRAF-mutated AMs (35%) was lower than those reported for the other non-acral cutaneous melanomas [1,15,17,18]. However, it was higher than those usually found in this melanoma subtype, which rarely exceeds 20% of cases [15,16,24,25,27]. An explanation could be the fact that the present series only included Italian patients. Indeed, Yeh and colleagues highlighted that BRAF mutations were more common in European-derived patients, as also supported by the finding of 30% of AMs with BRAF mutations in a German cohort [16,23]. Of course, this result is of great importance from the therapeutic point of view since many cases are eligible for targeted therapy. And the fact that in more than 90% of cases the mutation is a p.V600E substitution is noteworthy from the diagnostic point of view, since it can also be detected by immunohistochemistry. BRAF-mutated AMs were related to more favorable histologic prognostic factors (thinner lesions with lower mitotic count) and harbored fewer copy number aberrations, similarly to melanomas occurring in non-chronically sun-damaged skin, in line with other studies [15,16]. In particular, BRAF-mutated cases were correlated with a lower frequency of gains in the CCND1 locus compared to TWT AMs (29% and 61%, respectively), as reported by Curtin and colleagues [18]. No BRAF mutations were detected in subungual melanomas, confirming its rarity in this site [26,27]. The importance of this pathway in AM was also highlighted by the high percentage of cases with gains in the BRAF locus (47%).
The reported frequency of NRAS mutations in AM ranges from about 10% to 30% of cases, with markedly lower rates in melanomas of the nail apparatus [16,22,23,24,25,26,27]. In the present study, NRAS mutations were detected in 28% of AMs, none in subungual cases, and almost all in the acral lentiginous melanoma histotype. Although the most frequent NRAS mutation was in codon 61, as referred for the other non-acral cutaneous melanomas, about one-third of cases were mutated in codon 12. This is higher than usually reported in skin melanomas in a non-acral site, which is around 10%, but similar findings were already reported in AM [15,16,23,24,30]. Worth noting is that codon 12 of NRAS is not routinely investigated in skin melanoma because it rarely mutates. However, the present results suggest that this codon should be included in the mutational analysis of AM.
Only 5% of AMs were found to be NF1-mutated in this series, lower than the previously reported percentages [15,16,22,23] and NF1 losses were observed in other 6 AMs. AMs with NF1 impairment have been related with worse histologic prognostic factors, an association that can neither be confirmed nor excluded by the present results due to the paucity of cases in this group [15]. It is noteworthy that NF1-defective BRAF, NRAS, and KIT wild-type melanoma cell lines have been shown to respond to MEK inhibitors in preclinical studies [31]. Moreover, KIT mutations were rare (10% of cases), a result significantly lower than reported in older studies where it seemed to be the prevalent molecular alteration in AM but in line with the more recent ones [16,17,22,23,28].
Among TWT samples, ARID1A mutations were found in three cases suggesting an important role in AM oncogenesis. ARID1A is a core member of the switch/sucrose non-fermentable (SWI/SNF) chromatin-remodeling complex, a machinery that provides the access of proteins to DNA, and its mutations have been frequently reported in many different types of cancers [32,33]. The pathogenicity of ARID1A mutations in melanoma was already reported in previous studies and aberrations in this pathway seem to occur in about 20% of AMs [19,34,35]. Shain and colleagues theorized that in the oncogenetic cascade of malignant melanoma an initiating mutation in BRAF or NRAS activates the mitogen-activated protein kinase (MAPK) signaling pathway and subsequent additional mutations hit other genes involved in tumor progression, such as the tumor suppressor gene ARID1A [36]. However, the MAPK pathway was not impaired by gene mutations among these three AMs and gains involving BRAF and NRAS loci were found in only a case, thus mutated-ARID1A might act also as driver. Indeed, ARID1A negatively regulates TERT expression and activity and its mutations might provide a survival advantage through telomere maintenance [33]. Moreover, ARID1A mutations and reduced copy number are reported to be negatively associated with patient survival and/or checkpoint therapy responses in multiple types of cancer [37]. In agreement with pan-cancer data sets from The Cancer Genome Atlas in the Skin Cutaneous Melanoma category (from https://www.cbioportal.org/, accessed on 10 March 2021, TCGA), we found that 23% and 20% of samples were characterized by ARID1A copy number gains and losses respectively. Future studies in a large cohort of treated patients may clarify if the ARID1A gene status can affect patient outcome in AM.
TERT promoter C>T transitions are found in about 70% of melanomas occurring on sun-exposed skin, suggesting a possible causative role of UV radiation [1,15,16,17,19,22,23,38,39,40,41]. AMs, instead, rarely harbor these mutations, thus excluding the UV-correlated pathogenesis [1,15,16,17,19,22,23,38,39,40,41]. Indeed, the peculiar body site and the thick stratum corneum overlying the tumor could act as protection from solar damage. Accordingly, TERT promoter mutations were detected only in 4 cases (13%). However, gains of the TERT locus were found in 47% of cases, highlighting the importance of this gene in the development and progression of melanoma.
TP53 mutation is considered a pivotal event in tumor progression, since it impairs the function of the gene protein product preventing the activation of apoptosis or the arrest of the cell cycle in response to DNA damage. However, its occurrence was less frequent in melanoma than in other cancers and it was rarely reported in AM [16,19,29]. Interestingly, in the present series, nine cases (accounting for 30% of analyzed samples) harbored TP53 mutations and most were acral lentiginous melanomas. In the Catalogue of Somatic Mutations in Cancer, the TP53 mutation rate is about 9% in AM, reaching 25% in the acral lentiginous melanoma subtype and similar results were found in other studies [42,43,44,45]. Besides the fact that only primary tumors were analyzed in this study, these data suggest that TP53 mutations may be an early event in AM, allowing the accumulation of the high number of structural rearrangements and copy number changes usually found in this type of melanoma. Indeed, a high percentage of genome change was detected in the present AMs, especially in those cases with poor histologic prognostic features (thick lesion, presence of ulceration, and high mitotic count).
PREX2 and CDKN2A were among the genes mainly affected by structural alterations in this series of AMs. Gains in the PREX2 locus were detected in 60% of samples. PREX2 acts as a negative regulator of the PTEN tumor suppressor protein, thus promoting tumorigenesis by the activation of the PI3K signaling pathway [46,47]. Multiple mechanisms are implicated in PREX2 dysregulation in melanoma. Indeed, PREX2 gene amplification and rearrangements have been found [21]. Moreover, PREX2 mutations were detected in about 15% of melanomas and immortalized human melanocytes expressing mutant PREX2 have been reported to form tumors in mice [21]. Beside mutations, PREX2 is altered via overexpression in various cancer types, including melanoma [48]. Indeed, overexpression of wild-type PREX2 can promote tumor growth through the impairing of the PI3K pathway [47]. Altogether, these evidences suggest PREX2 as a key player in melanoma. CDKN2A is a well-known melanoma tumor-suppressor gene frequently deleted in all melanoma subtypes, particularly in mucosal and AM [18]. Indeed, CDKN2A losses were found in 63% of cases.
In summary, the present findings showed that several pathways (MAPK, PI3K, TP53, cell cycle, and SWI/SNF) may be impaired by genetic aberrations dominated by genomic structural variants. Survival analysis confirmed the prognostic value of classic histologic variables and ruled out any prognostic implication of molecular alterations which have, instead, predictive value of response to targeted therapy.
This study’s main strengths lie in the collection and analysis of primitive tumors only of homogeneous European-derived patients and in the use of solid and reliable molecular techniques. The main weaknesses of this investigation, instead, concern the retrospective setting, the limited number of cases analyzed, and the long-time span in which AMs were diagnosed. However, these features are shared with most studies on this topic and are mainly due to the rarity of this subtype of melanoma.
In conclusion, this study further supports most recent data regarding the frequencies and the variety of mutated genes and the high load of copy number variations in AM, highlighting their presence already at an early stage, mainly in tumors with poor histologic prognostic features. Moreover, it showed that the rate of BRAF mutations may be higher than previously reported in AMs of European-derived people and correlated with favorable prognostic factors such as low thickness, low mitotic count and an early-stages of patients with AM.
4. Materials and Methods
4.1. Samples
Archival formalin-fixed and paraffin-embedded (FFPE) primary tumor samples of 74 patients diagnosed with AM during the period 2000–2019 at the Padua University Hospital, at the Veneto Institute of Oncology, or at the University Hospital of Turin were collected for this retrospective study. All cases were reviewed, the diagnoses confirmed in all instances by a pathologist according to the fourth edition of the World Health Organization classification of skin tumors, and the staging was updated to the 8th edition of the Union for International Cancer Control (UICC) TNM Classification of Malignant Tumors [9,49]. This study was approved by the institutional ethical review board of the Veneto Institute of Oncology IOV-I.R.C.C.S.
4.2. DNA Extraction
Tumor cell enrichment was performed to ensure a tumor cell content of >80%. Five consecutive 10 μm-thick sections were cut from each FFPE sample; tumor cells were then manually microdissected and collected in a sterile tube for DNA extraction. DNA was automatically isolated using the MagNA Pure Compact Nucleic Acid Isolation Kit I (Roche, Mannheim, Germany) on the MagNA Pure Compact instrument (Roche). DNA concentration was fluorometrically measured using a Qubit dsDNA HS assay (ThermoFisher Scientific, Waltham, MA, USA) on a Qubit Fluorometer 3.0 (ThermoFisher Scientific, Waltham, MA, USA).
4.3. Sequencing Analysis
The DNA quality of ten AM cases only allowed BRAF codon 600 and NRAS codon 61 analysis by Sanger sequencing or by high sensitivity commercial real-time PCR-based assays, namely EasyPGX ready BRAF and EasyPGX ready NRAS (Diatech Pharmacogenetics, Ancona, Italy), in accordance with the manufacturer’s protocol. Sanger sequencing was performed by amplifying exon 15 of BRAF and exon 3 of NRAS. The amplified products were purified with Illustra GFX 96 PCR Purification Kit (GE Healthcare, Buckinghamshire, UK) and sequenced using the BigDye Terminator v1.1 Cycle Sequencing Kit (ThermoFisher Scientific). After purification with a BigDye XTerminator Purification Kit (ThermoFisher Scientific), sequences were analyzed on the 96-capillary automatic sequencer AB3730xl Genetic Analyzer (ThermoFisher Scientific).
The DNA of thirty AM cases was suitable for NGS sequencing. In accordance with the manufacturer’s protocol, 100 ng of dsDNA was used to construct the library using a TruSeq Custom Amplicon Low Input Kit (Illumina, San Diego, CA, USA) in combination with a 33 gene custom-designed panel (Illumina, San Diego, CA, USA; Supplementary Table S1). The included genes were selected based on literature-based evidences [35,45,50,51]. Briefly, samples were subjected to dual-strand amplicon-based PCR library preparation and the quality of the libraries was then estimated using a High Sensitivity DNA Analysis Kit (Agilent Technologies, Santa Clara, CA, USA) on a Bionalyzer 2100 system (Agilent Technologies, Santa Clara, CA, USA). Subsequent sequencing of pooled libraries was performed in the MiSeq sequencing platform (Illumina, San Diego, CA, USA) using V3 reagents.
Data analysis, including alignment to the hg19 human reference genome, variant calling and annotation was done using a customized somatic pipeline on SOPHiA DDM-v4 software (Sophia Genetics, Saint-Sulpice, Switzerland). The selection of variants was based on a minimum coverage of 400X, minimum frequency of mutated allele of 15% and previous classification as pathogenic, likely pathogenic or variant of unknown significance on common databases of somatic variants (COSMIC database and cBioPortal). In order to exclude common SNPs, we only considered variants (splicing variants, promoter variants and exonic missense and nonsense variants) with a reported frequency of ≤0.05. Intronic and synonymous variants were not included in the analysis. The detected variants were then validated by Sanger Sequencing, as described above.
4.4. Copy Number Variation (CNV) Analysis
From forty-two AM cases, 80 ng of dsDNA was analysed for genome-wide copy number variations (CNV) using the OncoScan CNV Assay (ThermoFisher Scientific, Waltham, MA, USA) on an Affymetrix SNP-array platform (ThermoFisher Scientific, Waltham, MA, USA), in accordance with the manufacturer’s protocol. This assay is based on molecular inversion probe technology specifically designed to handle limited amounts of highly degraded FFPE-extracted DNA.
Raw probe signal intensities (CEL files) obtained in this manner were processed using OncoScan Console software (ThermoFisher Scientific, Waltham, MA, USA). Normal FFPE controls from the OncoScan assay Kit were used to calculate log2 ratio and B-allele frequencies (BAF). Copy-number aberrations, percentage of genome changed, and sample ploidy were identified by OncoScan Nexus Copy Number 3 (Biodiscovery, Hawthorne, CA, USA) using the TuScan segmentation algorithm. Log2 ratios for each marker were calculated relative to the reference signal profile. For two copies of alleles, the log graph should be centered around 0 on the Y axis: genomic regions were classified as having gains or losses if the Log2 ratios exceeded or fell below this threshold.
The genomic region of LOH or CN neutral LOH were included in the “percentage of genome changed” overviewing the percentage of sample genome aberrations.
4.5. Statistical Analysis
Continuous data (age at diagnosis, Breslow thickness and number of mitoses) were summarized as mean and standard deviation (SD), or median and interquartile range (IQR). The association between variables was assessed using the Mann-Whitney test, Kruskal-Wallis test, Spearman correlation coefficient, Chi Square test, and Fisher’s exact test, as appropriate. Survival estimates were calculated using the Kaplan-Meier method. The association between clinically relevant variables and progression-free and overall survival (PFS and OS, respectively) was evaluated using Cox regression models, with effect sizes expressed as the hazard ratio (HR) with a 95 per cent confidence interval (95% CI). All tests were two-sided and a p-value less than 0.05 was considered statistically significant. Statistical analysis was performed using R 4.0 (R Foundation for Statistical Computing, Vienna, Austria) [52].
Acknowledgments
The authors thank Tiziana Zanin, Claudio Sorgato and Monica Quaggio for their technical assistance to the project and the association Piccoli Punti ONLUS for its long-lasting support.
Supplementary Materials
The following are available online at https://www.mdpi.com/article/10.3390/ijms22083826/s1.
Author Contributions
Conceptualization, A.P.D.T., C.M. and R.C.; methodology, L.E., C.Z., C.S. and S.P.; software, F.C.; formal analysis, L.E. and F.C.; investigation, L.E. and C.S.; resources, P.D.F., R.S. (Rebecca Senetta), A.L.T., F.G., L.D., A.F., R.S. (Roberto Salmaso), S.R., F.B. and S.M.; data curation, L.E.; writing—original draft preparation, R.C.; writing—review and editing, L.E., C.M. and F.C.; supervision, C.M. and R.C.; funding acquisition, C.M. All authors have read and agreed to the published version of the manuscript.
Funding
This study was supported by Institutional funding of the Veneto Institute of Oncology IOV-IRCCS (5x1000) grant BIGID219MENI.
Institutional Review Board Statement
This study was approved by the institutional ethical review board of the Veneto Institute of Oncology IOV-I.R.C.C.S. (Approval No. CESC-IOV 2017/62, 2017/09/11). The ethical regulations of institutes conducting research on human tissue were followed.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Data will be available upon request.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Bastian B.C. The Molecular Pathology of Melanoma: An Integrated Taxonomy of Melanocytic Neoplasia. Annu. Rev. Pathol. Mech. Dis. 2014;9:239–271. doi: 10.1146/annurev-pathol-012513-104658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Durbec F., Martin L., Derancourt C., Grange F. Melanoma of the hand and foot: Epidemiological, prognostic and genetic features. A systematic review. Br. J. Dermatol. 2011;166:727–739. doi: 10.1111/j.1365-2133.2011.10772.x. [DOI] [PubMed] [Google Scholar]
- 3.Whiteman D.C., Pavan W.J., Bastian B.C. The melanomas: A synthesis of epidemiological, clinical, histopathological, genetic, and biological aspects, supporting distinct subtypes, causal pathways, and cells of origin. Pigment. Cell Melanoma Res. 2011;24:879–897. doi: 10.1111/j.1755-148X.2011.00880.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kuchelmeister C., Schaumburg-Lever G., Garbe C. Acral cutaneous melanoma in caucasians: Clinical features, histopathology and prognosis in 112 patients. Br. J. Dermatol. 2000;143:275–280. doi: 10.1046/j.1365-2133.2000.03651.x. [DOI] [PubMed] [Google Scholar]
- 5.Bello D.M., Chou J.F., Panageas K.S., Brady M.S., Coit D.G., Carvajal R.D., Ariyan C.E. Prognosis of Acral Melanoma: A Series of 281 Patients. Ann. Surg. Oncol. 2013;20:3618–3625. doi: 10.1245/s10434-013-3089-0. [DOI] [PubMed] [Google Scholar]
- 6.Sheen Y.-S., Liao Y.-H., Lin M.-H., Chen J.-S., Liau J.-Y., Tseng Y.-J., Lee C.-H., Chang Y.-L., Chu C.-Y. A clinicopathological analysis of 153 acral melanomas and the relevance of mechanical stress. Sci. Rep. 2017;7:5564. doi: 10.1038/s41598-017-05809-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fortin P.T., A Freiberg A., Rees R., Sondak V.K., Johnson T.M. Malignant melanoma of the foot and ankle. J. Bone Jt. Surg. Am. Vol. 1995;77:1396–1403. doi: 10.2106/00004623-199509000-00016. [DOI] [PubMed] [Google Scholar]
- 8.Heaton K.M., El-Naggar A., Ensign L.G., Ross M.I., Balch C.M. Surgical Management and Prognostic Factors in Patients with Subungual Melanoma. Ann. Surg. 1994;219:197–204. doi: 10.1097/00000658-199402000-00012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Goydos J.S., Shoen S.L. Acral Lentiginous Melanoma. Cancer Treat. Res. 2016;167:321–329. doi: 10.1007/978-3-319-22539-5_14. [DOI] [PubMed] [Google Scholar]
- 10.Elder D.E., Massi D., Scolyer R.A., Willemze R. WHO Classification of Skin Tumours. 4th ed. Volume 11. IARC; Lyon, France: 2018. [Google Scholar]
- 11.Bradford P.T., Goldstein A.M., McMaster M.L., Tucker M.A. Acral Lentiginous Melanoma. Arch. Dermatol. 2009;145:427–434. doi: 10.1001/archdermatol.2008.609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Desai A., Ugorji R., Khachemoune A. Acral melanoma foot lesions. Part 1: Epidemiology, aetiology, and molecular pathology. Clin. Exp. Dermatol. 2017;42:845–848. doi: 10.1111/ced.13243. [DOI] [PubMed] [Google Scholar]
- 13.Piliang M.P. Acral Lentiginous Melanoma. Clin. Lab. Med. 2011;31:281–288. doi: 10.1016/j.cll.2011.03.005. [DOI] [PubMed] [Google Scholar]
- 14.Basurto-Lozada P., Molina-Aguilar C., Castaneda-Garcia C., Vázquez-Cruz M.E., Garcia-Salinas O.I., Álvarez-Cano A., Martínez-Said H., Roldán-Marín R., Adams D.J., Possik P.A., et al. Acral lentiginous melanoma: Basic facts, biological characteristics and research perspectives of an understudied disease. Pigment. Cell Melanoma Res. 2021;34:59–71. doi: 10.1111/pcmr.12885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Newell F., Wilmott J.S., Johansson P.A., Nones K., Addala V., Mukhopadhyay P., Broit N., Amato C.M., Van Gulick R., Kazakoff S.H., et al. Whole-genome sequencing of acral melanoma reveals genomic complexity and diversity. Nat. Commun. 2020;11:1–14. doi: 10.1038/s41467-020-18988-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yeh I., Jorgenson E., Shen L., Xu M., North J.P., Shain A.H., Reuss D., Wu H., A Robinson W., Olshen A., et al. Targeted Genomic Profiling of Acral Melanoma. J. Natl. Cancer Inst. 2019;111:1068–1077. doi: 10.1093/jnci/djz005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Vazquez V.D.L., Vicente A.L., Carloni A.C., Berardinelli G., Soares P., Scapulatempo-Neto C., Martinho O., Reis R.M. Molecular profiling, including TERT promoter mutations, of acral lentiginous melanomas. Melanoma Res. 2016;26:93–99. doi: 10.1097/CMR.0000000000000222. [DOI] [PubMed] [Google Scholar]
- 18.Curtin J.A., Fridlyand J., Kageshita T., Patel H.N., Busam K.J., Kutzner H., Cho K.-H., Aiba S., Bröcker E.-B., LeBoit P.E., et al. Distinct Sets of Genetic Alterations in Melanoma. N. Engl. J. Med. 2005;353:2135–2147. doi: 10.1056/NEJMoa050092. [DOI] [PubMed] [Google Scholar]
- 19.Hayward N.K., Wilmott J.S., Waddell N., Johansson P.A., Field M.A., Nones K., Patch A.-M., Kakavand H., Alexandrov L.B., Burke H., et al. Whole-genome landscapes of major melanoma subtypes. Nat. Cell Biol. 2017;545:175–180. doi: 10.1038/nature22071. [DOI] [PubMed] [Google Scholar]
- 20.Liang W.S., Hendricks W., Kiefer J., Schmidt J., Sekar S., Carpten J., Craig D.W., Adkins J., Cuyugan L., Manojlovic Z., et al. Integrated genomic analyses reveal frequentTERTaberrations in acral melanoma. Genome Res. 2017;27:524–532. doi: 10.1101/gr.213348.116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Berger M.F., Hodis E., Heffernan T.P., Deribe Y.L., Lawrence M.S., Protopopov A., Ivanova E., Watson I.R., Nickerson E., Ghosh P., et al. Melanoma genome sequencing reveals frequent PREX2 mutations. Nat. Cell Biol. 2012;485:502–506. doi: 10.1038/nature11071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Shi K., Zhang B., Kong B.Y., Zhang Y., Igartua C., Mohan L.S., Quan V.L., Panah E., Isales M.C., Beaubier N., et al. Distinct Genomic Features in a Retrospective Cohort of Mucosal, Acral and Vulvovaginal Melanomas. J. Am. Acad. Dermatol. 2019:0190. doi: 10.1016/j.jaad.2019.07.017. [DOI] [PubMed] [Google Scholar]
- 23.Zaremba A., Murali R., Jansen P., Möller I., Sucker A., Paschen A., Zimmer L., Livingstone E., Brinker T.J., Hadaschik E., et al. Clinical and genetic analysis of melanomas arising in acral sites. Eur. J. Cancer. 2019;119:66–76. doi: 10.1016/j.ejca.2019.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dika E., Lambertini M., Pellegrini C., Veronesi G., Melotti B., Riefolo M., Sperandi F., Patrizi A., Ricci C., Mussi M., et al. Cutaneous and Mucosal Melanomas of Uncommon Sites: Where Do We Stand Now? J. Clin. Med. 2021;10:478. doi: 10.3390/jcm10030478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zebary A., Omholt K., Vassilaki I., Höiom V., Lindén D., Viberg L., Kanter-Lewensohn L., Johansson C.H., Hansson J. KIT, NRAS, BRAF and PTEN mutations in a sample of Swedish patients with acral lentiginous melanoma. J. Dermatol. Sci. 2013;72:284–289. doi: 10.1016/j.jdermsci.2013.07.013. [DOI] [PubMed] [Google Scholar]
- 26.Borkowska A., Szumera-Ciećkiewicz A., Spałek M., Teterycz P., Czarnecka A., Kowalik A., Rutkowski P. Mutation profile of primary subungual melanomas in Caucasians. Oncotarget. 2020;11:2404–2413. doi: 10.18632/oncotarget.27642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Holman B.N., Van Gulick R.J., Amato C.M., Macbeth M.L., Davies K.D., Aisner D.L., Robinson W.A., Couts K.L. Clinical and molecular features of subungual melanomas are site-specific and distinct from acral melanomas. Melanoma Res. 2020;30:562–573. doi: 10.1097/CMR.0000000000000688. [DOI] [PubMed] [Google Scholar]
- 28.Hodi F.S., Corless C.L., Giobbie-Hurder A., Fletcher J.A., Zhu M., Marino-Enriquez A., Friedlander P., Gonzalez R., Weber J.S., Gajewski T.F., et al. Imatinib for Melanomas Harboring Mutationally Activated or Amplified KIT Arising on Mucosal, Acral, and Chronically Sun-Damaged Skin. J. Clin. Oncol. 2013;31:3182–3190. doi: 10.1200/JCO.2012.47.7836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zou Z., Ou Q., Ren Y., Lv Q., Qin L., Zhao L., Su S., Wu X., Bao H., Wang A., et al. Distinct genomic traits of acral and mucosal melanomas revealed by targeted mutational profiling. Pigment. Cell Melanoma Res. 2020;33:601–611. doi: 10.1111/pcmr.12865. [DOI] [PubMed] [Google Scholar]
- 30.Dumaz N., Jouenne F., Delyon J., Mourah S., Bensussan A., Lebbé C. Atypical BRAF and NRAS Mutations in Mucosal Melanoma. Cancers. 2019;11:1133. doi: 10.3390/cancers11081133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Nissan M.H., Pratilas C.A., Jones A.M., Ramirez R., Won H., Liu C., Tiwari S., Kong L., Hanrahan A.J., Yao Z., et al. Loss of NF1 in Cutaneous Melanoma Is Associated with RAS Activation and MEK Dependence. Cancer Res. 2014;74:2340–2350. doi: 10.1158/0008-5472.CAN-13-2625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pavlidou E.N., Balis V. Diagnostic significance and prognostic role of the ARID1A gene in cancer outcomes (Review) World Acad. Sci. J. 2020;2:49–64. doi: 10.3892/wasj.2020.37. [DOI] [Google Scholar]
- 33.Váraljai R., Horn S., Sucker A., Piercianek D., Schmitt V., Carpinteiro A., Becker K., Reifenberger J., Roesch A., Felsberg J., et al. Integrative Genomic Analyses of Patient-Matched Intracranial and Extracranial Metastases Reveal a Novel Brain-Specific Landscape of Genetic Variants in Driver Genes of Malignant Melanoma. Cancers. 2021;13:731. doi: 10.3390/cancers13040731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ticha I., Hojny J., Michalkova R., Kodet O., Krkavcova E., Hajkova N., Nemejcova K., Bartu M., Jaksa R., Dura M., et al. A comprehensive evaluation of pathogenic mutations in primary cutaneous melanomas, including the identification of novel loss-of-function variants. Sci. Rep. 2019;9:1–15. doi: 10.1038/s41598-019-53636-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Furney S.J., Turajlic S., Stamp G., Thomas J.M., Hayes A., Strauss D., Gavrielides M., Xing W., Gore M., Larkin J., et al. The mutational burden of acral melanoma revealed by whole-genome sequencing and comparative analysis. Pigment. Cell Melanoma Res. 2014;27:835–838. doi: 10.1111/pcmr.12279. [DOI] [PubMed] [Google Scholar]
- 36.Shain A.H., Yeh I., Kovalyshyn I., Sriharan A., Talevich E., Gagnon A., Dummer R., North J.P., Pincus L.B., Ruben B.S., et al. The Genetic Evolution of Melanoma from Precursor Lesions. N. Engl. J. Med. 2015;373:1926–1936. doi: 10.1056/NEJMoa1502583. [DOI] [PubMed] [Google Scholar]
- 37.Li J., Wang W., Zhang Y., Cieślik M., Guo J., Tan M., Green M.D., Wang W., Lin H., Li W., et al. Epigenetic driver mutations in ARID1A shape cancer immune phenotype and immunotherapy. J. Clin. Investig. 2020;130:2712–2726. doi: 10.1172/JCI134402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Horn S., Figl A., Rachakonda P.S., Fischer C., Sucker A., Gast A., Kadel S., Moll I., Nagore E., Hemminki K., et al. TERT Promoter Mutations in Familial and Sporadic Melanoma. Science. 2013;339:959–961. doi: 10.1126/science.1230062. [DOI] [PubMed] [Google Scholar]
- 39.Huang F.W., Hodis E., Xu M.J., Kryukov G.V., Chin L., Garraway L.A. Highly Recurrent TERT Promoter Mutations in Human Melanoma. Science. 2013;339:957–959. doi: 10.1126/science.1229259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Liau J.-Y., Tsai J.-H., Jeng Y.-M., Chu C.-Y., Kuo K.-T., Liang C.-W. TERT promoter mutation is uncommon in acral lentiginous melanoma. J. Cutan. Pathol. 2014;41:504–508. doi: 10.1111/cup.12323. [DOI] [PubMed] [Google Scholar]
- 41.Ekedahl H., Lauss M., Olsson H., Griewank K.G., Schadendorf D., Ingvar C., Jönsson G.B. HighTERTpromoter mutation frequency in non-acral cutaneous metastatic melanoma. Pigment. Cell Melanoma Res. 2016;29:598–600. doi: 10.1111/pcmr.12500. [DOI] [PubMed] [Google Scholar]
- 42.Tate J.G., Bamford S., Jubb H.C., Sondka Z., Beare D.M., Bindal N., Boutselakis H., Cole C.G., Creatore C., Dawson E., et al. COSMIC: The Catalogue Of Somatic Mutations In Cancer. Nucleic Acids Res. 2018;47:D941–D947. doi: 10.1093/nar/gky1015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Palmieri G., Italian Melanoma Intergroup for the Italian Melanoma Intergroup (IMI) Colombino M., Casula M., Manca A., Mandalà M., Cossu A. Molecular Pathways in Melanomagenesis: What We Learned from Next-Generation Sequencing Approaches. Curr. Oncol. Rep. 2018;20:1–16. doi: 10.1007/s11912-018-0733-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Siroy A.E., Boland G.M., Milton D.R., Roszik J., Frankian S., Malke J., E Haydu L., Prieto V.G., Tetzlaff M.T., Ivan D., et al. Beyond BRAF V600: Clinical Mutation Panel Testing by Next-Generation Sequencing in Advanced Melanoma. J. Investig. Dermatol. 2015;135:508–515. doi: 10.1038/jid.2014.366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hodis E., Watson I.R., Kryukov G.V., Arold S.T., Imielinski M., Theurillat J.-P., Nickerson E., Auclair D., Li L., Place C., et al. A Landscape of Driver Mutations in Melanoma. Cell. 2012;150:251–263. doi: 10.1016/j.cell.2012.06.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lissanu Deribe Y. Interplay between PREX2 mutations and the PI3K pathway and its effect on epigenetic regulation of gene expression in NRAS-mutant melanoma. Small GTPases. 2016;7:178–185. doi: 10.1080/21541248.2016.1178366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Fine B., Hodakoski C., Koujak S., Su T., Saal L.H., Maurer M., Hopkins B., Keniry M., Sulis M.L., Mense S., et al. Activation of the PI3K Pathway in Cancer Through Inhibition of PTEN by Exchange Factor P-REX2a. Science. 2009;325:1261–1265. doi: 10.1126/science.1173569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Srijakotre N., Man J., Ooms L.M., Lucato C.M., Ellisdon A.M., Mitchell C.A. P-Rex1 and P-Rex2 RacGEFs and cancer. Biochem. Soc. Trans. 2017;45:963–977. doi: 10.1042/BST20160269. [DOI] [PubMed] [Google Scholar]
- 49.O’Sullivan B., Brierley J., Byrd D., Bosman F., Kehoe S., Kossary C., Piñeros M., Van Eycken E., Weir H.K., Gospodarowicz M. The TNM classification of malignant tumours—towards common understanding and reasonable expectations. Lancet Oncol. 2017;18:849–851. doi: 10.1016/S1470-2045(17)30438-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Akbani R., Akdemir K.C., Aksoy B.A., Albert M., Ally A., Amin S.B., Arachchi H., Arora A., Auman J.T., Ayala B., et al. Genomic Classification of Cutaneous Melanoma. Cell. 2015;161:1681–1696. doi: 10.1016/j.cell.2015.05.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Zhang T., Dutton-Regester K., Brown K.M., Hayward N.K. The genomic landscape of cutaneous melanoma. Pigment. Cell Melanoma Res. 2016;29:266–283. doi: 10.1111/pcmr.12459. [DOI] [PubMed] [Google Scholar]
- 52.RCore Team . A Language and Environment for Statistical Computing. R Foundation for Statistical Computing; Vienna, Austria: 2020. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data will be available upon request.