Microvascular alterations within and outside the central nervous system (CNS) in amyotrophic lateral sclerosis (ALS): ALS is a fatal neurodegenerative disease leading to paralysis and eventual death within 3 to 5 years of diagnosis due to respiratory dysfunction. Numerous pathogenic intrinsic and extrinsic effectors are involved in the diffuse motor neuron degeneration. Also, impairment of neurovascular unit components in the brain and spinal cord in ALS patients and in animal models of disease was noted and points to vascular pathology being a key factor in the recognition of ALS as a neurovascular disease (Garbuzova-Davis et al., 2011). Our original (Garbuzova-Davis and Sanberg, 2014) and other studies (Winkler et al., 2014; Kakaroubas et al., 2019) provide convincing evidence on structural and functional alterations of the blood-CNS barrier (B-CNS-B) in ALS, potentially representing an additional pathogenic disease mechanism. Degeneration of endothelial cells (ECs) and astrocyte end-feet processes, reduced pericyte capillary coverage, dysfunction of tight junction proteins, and impairment of endothelial transport system have been shown to compromise B-CNS-B integrity. Vascular leakage and microhemorrhages were also noted in the spinal cord. The weakened barrier function may allow detrimental factors from the systemic circulation to penetrate the CNS and escalate motor neuron degeneration. Additionally, vascular pathologies in ALS were determined not only within, but also outside of the CNS. Recently, we showed damaged microvasculature in the lungs ofG93A SOD1 mutant mice at the late stage of disease (Garbuzova-Davis et al., 2020). Numerous microhemorrhages, substantial capillary leakage and even capillary rupture resulting in lung petechiae, potentially via ECs damage, may represent essential effectors towards respiratory dysfunction in ALS. These findings are concurrent with noted capillary alterations within the CNS in both ALS patients and animal models of ALS. Since the damaged capillary endothelium in ALS does not properly maintain vascular homeostasis within and outside of the CNS, repairing the altered endothelium by cell administration may be a new therapeutic approach for this disease.
Stem cell therapy for restoring altered microvasculature within and outside the CNS in ALS: ALS is progressive disease with limited effective treatment and cell-based therapy is a promising approach. However, stem cell therapy has mainly prevented motor neurons from further degeneration via neuroprotective actions using various cellular sources and routes of cell administration. Despite these intensive investigations into developing a potential treatment for ALS, strategies to restore and/or re-establish microvascular integrity remain unaddressed. Our research team focused on repair of the damaged endothelium in ALS by intravenous cell delivery into symptomaticG93A SOD1 mutant mice, mimicking a clinical approach. In our initial study, human bone marrow-derived CD34+ cells (hBM34+) were intravenously administered at different doses into ALS mice at 13 weeks of age. Results showed beneficial effects of transplanted cells primarily at high dosage (1 × 106 cells/mouse) on restoration of barrier competence in the CNS and decreases in disease related effectors, leading to increased motor neuron survival (Garbuzova-Davis et al., 2017). Although some transplanted cells differentiated into ECs and engrafted within spinal cord capillaries, delayed effect on motor function and still severely damaged capillaries were determined in post-transplant ALS mice. Addressing this issue, administration of restricted-endothelial cell lineage may provide more benefits in B-CNS-B restoration. In our following study, human bone marrow-derived endothelial progenitor cells (hBMEPCs) at the same dose of hBM34+ were intravenously transplanted into symptomaticG93A SOD1 mutant mice. Transplanted cell effect was demonstrated by significant improvement of behavioral disease outcomes at 2–3 weeks after cell administration (versus 4 weeks with hBM34+ cell transplant) leading to delayed disease progression (Garbuzova-Davis et al., 2019b). This benefit likely occurred due to widespread distribution of transplanted cells and their engraftment into capillaries of the spinal cord and brain, resulting in substantial restoration of capillary ultrastructure, decreased capillary permeability, and enhancement of motor neuron survival. Thus, these results provide novel evidence that hBMEPCs administration effectively repairs the compromised CNS barrier, potentially by replacement of damaged ECs, and may be a promising therapeutic strategy for microvascular repair in ALS. Similar results on re-establishing vascular integrity were determined in the lungs ofG93A SOD1 mutant mice at the late disease stage, mostly after intravenous transplantation of hBMEPCs rather than hBM34+ cells (Garbuzova-Davis et al., 2020). Numerous administered hBMEPCs, expressing human anti-von Willibrand factor, were detected in the alveolus or bronchiolar walls. Together, these studies have shown efficacious effects of pervasively migrated transplanted hBMEPCs within and outside of the CNS by systemic delivery and may reveal intravenous cell administration as a minimally invasive route beneficially enhancing restorative processes on damaged microvessels in ALS. Also, in supporting hBMEPCs as an appropriate cell type for advanced repair of capillary impairment, Garbuzova-Davis et al. (2019a) showed that these cells release angiogenic factors in vitro and may maintain endogenous EC function and/or promote angiogenesis in vivo upon cell administration. In addition, transplanted hBMEPCs may release various nanosized vesicles assisting cell transplant effects.
Extracellular vesicles (EVs) as potential aids to cell therapy for restoring damaged microvasculature within and outside the CNS in ALS: EVs are important intermediaries in cell-to-cell communications regulating biological processes under physiological and pathological conditions. The EVs, composed of microvesicles (MVs), exosomes, and apoptotic bodies, can be distinguished by vesicle size, content, and different biogenesis pathways. These EV characteristics are comprehensively discussed in (EL Andaloussi et al., 2013; Tetta et al., 2013). It has been shown that MVs derived from endothelial progenitor cells isolated from human peripheral blood mononuclear cells enhanced endothelial cell survival and proliferation by incorporating into ECs in vitro and stimulated angiogenesis in vivo using immunodeficient SCID mice (Deregibus et al., 2007). Also, EVs derived from human bone marrow mesenchymal stromal cells reduced lung inflammation and lung ischemia/reperfusion injury in a mouse model, preventing lung edema by improving endothelial barrier integrity (Stone et al., 2017). The vesicles released from the cell of origin potentially delivered various bioactive molecules to target cells and act as intercellular mediators in communication networks (Tetta et al., 2013). Thus, EVs derived from transplanted cells may be a promising assistive element for repair of microvascular damage within and outside the CNS in ALS. Since transplantation of hBMEPCs into symptomaticG93A SOD1 mutant mice showed the most beneficial effects, we initiated studies on characteristics and therapeutic potential of EVs derived from hBMEPCs. The EVs were isolated from conditioned media of cultured hBMEPCs at different time points and total protein concentrations and sizes of isolated EVs were evaluated. Our preliminary results demonstrated similar protein amounts in EVs and vesicle sizes at all examined culture time points, confirming adequate isolation of hBMEPC-derived EVs. In our next study, cells from mouse brain endothelial cell line bEnd.3 (mBEC) were used to determine the effect of hBMEPC-derived EVs to mimic in vivo condition. The mBECs damage in vitro was substantially induced by adding plasma from early symptomaticG93A SOD1 mutant mice and EV dose-response effects were analyzed on cell viability using LIVE/DEAD viability/cytotoxicity assay. A significant decrease of dead mBECs and improved cell morphology were determined by culture media supplement mainly with 1 µg/mL of EVs. These initial results indicated that this EV dose was beneficial in alleviating mBEC damage by ALS mouse plasma. To determine the potential mechanism underlying hBM-EPC-derived EV actions leading to protection of endothelial cells from damage via pathological environment, the capability of mBECs to uptake EVs was investigated. For the purposes of this study, hBMEPCs were transfected with pMAX GFP using lipofectamine and GFP-labeled EVs were isolated from culture media. GFP-labeled hBM-EPCs were well apparent and GFP-labeled EVs were detected at appropriate vesicle sizes (Figure 1A and B). When GFP-labeled EVs at a concentration of 1 µg/mL were added to media supplemented with plasma derived fromG93A SOD1 mutant mice, numerous EVs were observed within cytosol of many cultured mBECs after just 24 hours of incubation (Figure 1C). GFP-labeled EVs were also seen in inner cell membrane at higher magnification (Figure 1D). Thus, our preliminary results demonstrated that hBMEPC-derived EVs were effectively isolated from cell culture media and considered as nanosized vesicles. Significant reductions of damaged ECs from the pathological environment in vitro by EVs internalization and probable release of various bioactive molecules into impaired mBECs may identify important underlying mechanisms of EV actions towards maintaining cell integrity.
Figure 1.
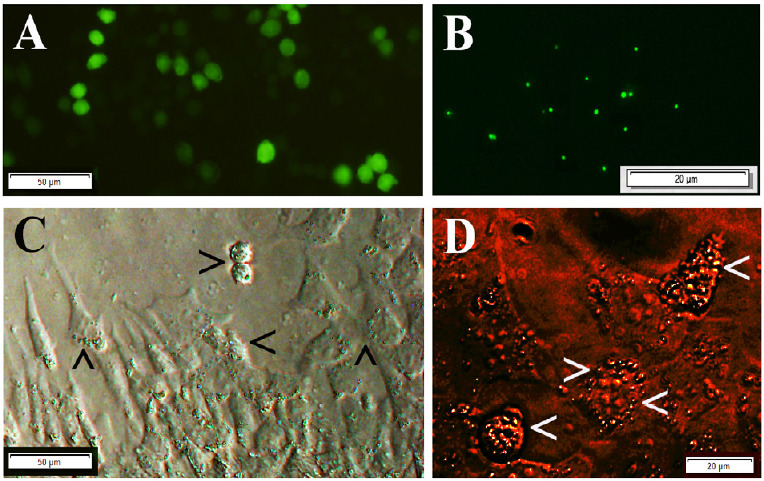
Transfection of hBM-EPCs with GFP and the uptake of GFP-labeled EVs by mouse brain endothelial cells in vitro.
(A) hBM-EPCs transfected with GFP using lipofectamine showed GFP-labeling (green). (B) Microscopic detection of GFP-labeled EVs demonstrated appropriate vesicle sizes (green). (C) Cytosolic GFP-labeled EV uptake (green, arrowheads) was detected in many mBECs exposed to ALS mouse plasma. (D) Cultured mBECs displayed at a higher magnification showed GFP-labeled EVs in inner cell membranes (green, arrowheads). Images in A, C, and D were obtained using live cells. Scale bar in A and C is 50 µm; in B and D is 20 µm. ALS: Amyotrophic lateral sclerosis; EVs: extracellular vesicles; GFP: green fluorescent proteins; hBM-EPCs: human bone marrow-derived endothelial progenitor cells; mBECs: mouse brain endothelial cell line bEnd.3. Images were sourced fromthe authors’ lab.
In summary, our EV studies represent a novel approach in understanding the role of stem cell-secreted factors in the therapeutic effects of cell therapy. Since we just initiated an investigation on EV’s contribution to ALS stem cell therapy, a number of areas still need elucidation in our perspective research: 1) EV molecular content, 2) specific EV component(s) involved in cell restoration, 3) mechanisms of EV uptake, 4) inhibitors of EV release or uptake, and 5) therapeutic effects of EV administration into SOD1 mutant mice. Also, determining specific protein(s) for mediating restoration of EC integrity via EV proteomics may provide important insights. These planned studies will further establish the mechanisms of stem cell-based microvascular repair in ALS.
This work was supported by the National Instites of Health, National Institute of Neurological Disorders and Stroke (1R01NS090962).
Footnotes
C-Editors: Zhao M, Li JY; T-Editor: Jia Y
Copyright license agreement: The Copyright License Agreement has been signed by both authors before publication.
Plagiarism check: Checked twice by iThenticate.
Peer review: Externally peer reviewed.
References
- 1.Deregibus MC, Cantaluppi V, Calogero R, Lo Iacono M, Tetta C, Biancone L, Bruno S, Bussolati B, Camussi G. Endothelial progenitor cell derived microvesicles activate an angiogenic program in endothelial cells by a horizontal transfer of mRNA. Blood. 2007;110:2440–2448. doi: 10.1182/blood-2007-03-078709. [DOI] [PubMed] [Google Scholar]
- 2.EL Andaloussi S, Mäger I, Breakefield XO, Wood MJ. Extracellular vesicles: Biology and emerging therapeutic opportunities. Nat Rev Drug Discov. 2013;12:347–357. doi: 10.1038/nrd3978. [DOI] [PubMed] [Google Scholar]
- 3.Garbuzova-Davis S, Ehrhart J, Mustafa H, Llauget A, Boccio KJ, Sanberg PR, Appel SH, Borlongan CV. Phenotypic characteristics of human bone marrow-derived endothelial progenitor cells in vitro support cell effectiveness for repair of the blood-spinal cord barrier in ALS. Brain Res. 2019a;1724:146428. doi: 10.1016/j.brainres.2019.146428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Garbuzova-Davis S, Kurien C, Haller E, Eve DJ, Navarro S, Steiner G, Mahendrasah A, Hailu S, Khatib M, Boccio KJ, Borlongan CV, Van Loveren HR, Appel SH, Sanberg PR. Human bone marrow endothelial progenitor cell transplantation into symptomatic ALS mice delays disease progression and increases motor neuron survival by repairing blood-spinal cord barrier. Sci Rep. 2019b;9:5280. doi: 10.1038/s41598-019-41747-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Garbuzova-Davis S, Kurien C, Thomson A, Falco D, Ahmad S, Staffetti J, Steiner G, Abraham S, James G, Mahendrasah A, Sanberg PR, Borlongan CV. Endothelial and astrocytic support by human bone marrow stem cell grafts into symptomatic ALS mice towards blood-spinal cord barrier repair. Sci Rep. 2017;7:884. doi: 10.1038/s41598-017-00993-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Garbuzova-Davis S, Rodrigues MC, Hernandez-Ontiveros DG, Louis MK, Willing AE, Borlongan CV, Sanberg PR. Amyotrophic lateral sclerosis: A neurovascular disease. Brain Res. 2011;1398:113–125. doi: 10.1016/j.brainres.2011.04.049. [DOI] [PubMed] [Google Scholar]
- 7.Garbuzova-Davis S, Sanberg PR. Blood-CNS barrier impairment in ALS patients versus an animal model. Front Cell Neurosci. 2014;8:21. doi: 10.3389/fncel.2014.00021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Garbuzova-Davis S, Shell R, Mustafa H, Hailu S, Willing AE, Sanberg PR, Borlongan CV. Advancing stem cell therapy for repair of damaged lung microvasculature in amyotrophic lateral sclerosis. Cell Transplant. 2020;29:963689720913494. doi: 10.1177/0963689720913494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kakaroubas N, Brennan S, Keon M, Saksena NK. Pathomechanisms of blood-brain barrier disruption in ALS. Neurosci J. 2019;2019:2537698. doi: 10.1155/2019/2537698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Stone ML, Zhao Y, Robert Smith J, Weiss ML, Kron IL, Laubach VE, Sharma AK. Mesenchymal stromal cell-derived extracellular vesicles attenuate lung ischemia-reperfusion injury and enhance reconditioning of donor lungs after circulatory death. Respir Res. 2017;18:212. doi: 10.1186/s12931-017-0704-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tetta C, Ghigo E, Silengo L, Deregibus MC, Camussi G. Extracellular vesicles as an emerging mechanism of cell-to-cell communication. Endocrine. 2013;44:11–19. doi: 10.1007/s12020-012-9839-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Winkler EA, Sengillo JD, Sagare AP, Zhao Z, Ma Q, Zuniga E, Wang Y, Zhong Z, Sullivan JS, Griffin JH, Cleveland DW, Zlokovic BV. Blood-spinal cord barrier disruption contributes to early motor-neuron degeneration in ALS-model mice. Proc Natl Acad Sci U S A. 2014;111:E1035–1042. doi: 10.1073/pnas.1401595111. [DOI] [PMC free article] [PubMed] [Google Scholar]


