Abstract
Objective
To identify specific thresholds of daily electronic health record (EHR) time after work and daily clerical time burden associated with burnout in clinical faculty.
Materials and Methods
We administered an institution-wide survey to faculty in all departments at Mount Sinai Health System from November 2018 to February 2019. The Maslach Burnout Inventory and Mayo Well-Being Index assessed burnout. Demographics, possible confounding variables, and time spent on EHR work/clerical burden were assessed.
Results
Of 4156 eligible faculty members, 1781(42.9%) participated in the survey. After adjustment for background factors, EHR frustration (odds ratio [OR]=1.64–1.66), spending >90 minutes on EHR-outside the workday by self-report (OR = 1.41–1.90) and >1 hour of self-reported clerical work/day (OR = 1.39) were associated with burnout. Reporting that one’s practice unloads clerical burden (OR = 0.50–0.66) and higher resilience scores (OR = 0.77–0.84) were negatively associated with burnout.
Spending >90 minutes/day on EHR-outside work (OR = 0.66–0.67) and >60 minutes/day on clerical work (OR = 0.54–0.58) was associated with decreased likelihood of satisfactory work–life integration (WLI) and professional satisfaction (PS). Greater meaning in work was associated with an increased
likelihood
of achieving WLI (OR = 2.51) and PS (OR = 21.67).
Conclusion
Results suggest there are thresholds of excessive time on the EHR-outside the workday (>90 minutes) and overall clerical tasks (>60 minutes), above which clinical faculty may be at increased risk for burnout, as well as reduced WLI and PS, independent of demographic characteristics and clinical work hours. These thresholds of EHR and clerical burden may inform interventions aimed at mitigating this burden to reduce physician burnout.
Keywords: well-being, burnout, clinical faculty, clerical burden, electronic health record
INTRODUCTION
Burnout is prevalent in physicians and other clinical faculty and associated with numerous negative consequences, including depression, substance abuse,1 suboptimal patient care,2 and an increased likelihood to leave clinical practice.3,4 A large national effort is currently underway to identify and address drivers of physician burnout with considerable focus on system-level solutions.5,6 To date, system factors that have been linked to burnout include greater number of hours worked per week,7–11 team-based care inefficiencies,12,13 and excessive time spent on clerical tasks.14
The electronic health record (EHR) is a major contributor to excess clerical burden, in large part due to disproportionate time spent on documentation, order entry, billing, and general inbox management.7,15 Most physicians report that the EHR negatively affects their work–life balance,16 and there is widespread frustration with current health information technology usability as well as time spent on clerical tasks.14,16–18 Additionally, physicians using EHRs have a higher prevalence of burnout than those using other documentation methods, such as paper, and an association between increased EHR time and burnout has been documented.7,14,16,17,19 Furthermore, some ambulatory care physicians spend roughly 50% of their workday on EHR and clerical work, 1–2 hours of which is often completed outside of work.4,15 As such, interventions to decrease burnout have targeted efficiency and clerical burden, such as enhancing team-based care, increasing communication, and hiring scribes or utilizing voice recognition software for documentation. While many teamwork-based interventions may help decrease burnout and stress,20–23 other studies have observed no effect or even an increase in burnout with workflow changes.20,24,25 Further, there is limited information on how a physician’s perception of their practice’s effort to unload clerical work may impact burnout.
In order to more fully understand the relationship between burnout, EHR burden, administrative tasks, and efforts to unload clerical burden, we conducted a faculty-wide survey across all departments at the Mount Sinai Health System in New York City. We sought to identify thresholds of time spent on the EHR outside the workday and daily clerical work associated with burnout to identify target goals for interventions designed to decrease that burden. We hypothesized that specific thresholds (60 and 90 minutes) of time spent on EHR outside of the workday and clerical work throughout the day would be positively associated with burnout, and that one’s practice unloading clerical work would be negatively associated with burnout.
MATERIALS AND METHODS
Between November 2018 and February 2019, we administered an anonymous, institution-wide cross-sectional survey to clinical faculty within the Mount Sinai Health System, a large academic medical center with 7 hospital sites in New York City. Eligible participants included any of the 4156 individuals (MD, DO, PhDs) with a faculty appointment at the time of survey administration identified via the Dean’s Office faculty records. Individuals were eligible for entry into a raffle for 4 Apple watches as an incentive for participation. The survey was disseminated electronically via e-mail using the RedCap survey platform and was approved by the institutional review board at the Icahn School of Medicine at Mount Sinai.
Survey design
Participants provided demographic data including gender, age, specialty, faculty rank, full-time status, department, hours worked per week, and percent of time spent on clinical work. We grouped departments into the following categories: Primary Care (general internal medicine, family medicine, general and adolescent pediatrics, and geriatric medicine); General Hospital Based Medicine (emergency medicine and hospital medicine); Subspecialty Medicine/Pediatrics (all nongeneralist medicine and pediatric subspecialties); Surgery (general and specialty surgery); Anesthesia/Radiology/Pathology; Other Specialties (neurology, psychiatry, ophthalmology, genetics, environmental medicine, physiatry, dermatology, dentistry), and Other Department (“Other Department” survey choice, basic science respondents with clinical responsibilities, and those who left department blank). The vast majority of the physicians in the specialties above used the same EHR-EPIC; however, the Anesthesia, Radiology, Pathology departments each used different EHRs during the time of this study, and Radiology and Pathology relied heavily on dictation software/transcription for documentation.
Assessments
Burnout
We utilized 2 validated instruments to measure burnout in order to assess its multiple dimensions and timeframes: the Mayo Well-Being Index (WBI) and the Maslach Burnout Inventory (MBI) 2 item scale.26,27 The MBI-2 assesses the traditional dimensions of burnout including emotional exhaustion and depersonalization over the past year (Cronbach’s α = 0.74, all reported Cronbach’s α were calculated from our data). A high score (≥4) on either subscale is consistent with job-related burnout. The 2-item MBI correlates highly with the 22-item MBI, for which there is an extensive literature supporting its validity.26 The WBI captures additional well-being dimensions relevant to burnout, including emotional and physical health over the past month. The WBI includes 7 yes/no items: burnout from work, emotional exhaustion, fatigue, overwhelmed feelings, emotional problems, depression, and physical health.28 A high score (≥4) on the WBI is consistent with burnout; α = 0.71. For burnout outcomes, we utilized burnout score thresholds as well as average overall scores in analyses to understand how predictor variables relate to positive screens for burnout and overall severity of burnout. For our secondary outcomes, we asked questions to assess professional satisfaction (PS)17,21 from the Mini-Z and work–life integration (WLI) measure from Sinksy and colleagues’ paper in 2017.4
EHR and clerical work
To assess burden of the EHR and clerical work, we administered questions modified from the Mini-Z.17,21 Specifically, respondents were asked to indicate their level of agreement with the statement: “The EHR adds to the frustration of my day” (5-point Likert scale from 0 = Strongly Disagree to 5 = Strongly Agree). They were also asked to report their daily time spent on clerical work (How much time per work day do you spend engaged in clerical or nonphysician work, such as calling for appointments, doing prior authorizations, faxing forms, requesting records, etc?) and daily time spent on the EHR outside of the workday measured in 30-minute intervals. In addition, we asked about the extent to which their patient care setting made an effort to unload clerical/administrative burden: “My practice makes an effort to unload clerical burden” with 4 response options from “Not at all” to “A lot.”
Clinical covariates
Depressive symptoms were assessed using the validated Patient Health Questionnaire-2 item (PHQ-2)29; α = 0.77. Though not a diagnostic tool,30 the PHQ-2 performs well against longer diagnostic instruments for depression.31 Perceived resilience was assessed using the 2-item Connor-Davidson Resilience Scale (CD-RISC),32 α = 0.66, (“I am able to adapt to change,” “I tend to bounce back after illness or hardship,” with 4 responses from “rarely true” to “true nearly all of the time”); and meaning derived from work using the statement, “The work I do is meaningful to me,” using a 5- point Likert scale from 0 = Strongly Disagree to 5 = Strongly Agree.33
Statistical analysis
Data analyses proceeded in 7 steps. First, we computed descriptive analyses for all variables. Second, we examined associations between independent variables and measures of burnout using independent-samples t-tests for parametric continuous data, Mann-Whitney U tests for nonparametric continuous data, and chi-square tests for categorical variables. Third, for categorical variables with 4 or more answer choices, we di- or trichotomized responses for the correlation analyses. For the daily time-based questions, we first conducted chi-square analysis with all answer choices to determine if there was a clear cutoff point for dichotomization (using the Bonferroni-corrected difference for both burnout measures separately). Fourth, for variables with 3 or more response options, we conducted posthoc analyses utilizing residuals to compute chi-square P values, corrected using the Bonferroni method for multiple comparisons. Fifth, for bivariate analyses of continuous MBI and WBI scores, we conducted independent-samples t-tests for dichotomous predictors (using the Levene’s test for the equal variance P value assessment). Sixth, we conducted analyses of variance (ANOVAs) for independent variables with more than 2 groups and used Tukey’s HSD (equal variances) and Dunnett’s T3 (equal variance not assumed) tests, with a Bonferroni correction for multiple comparisons. Seventh, for the multivariable analyses, we conducted logistic regressions for binary outcomes and linear regressions for continuous outcomes; interaction terms were incorporated into these analyses to evaluate the potential role of rank in moderating associations between EHR and clerical burden on measures of burnout. Finally, we conducted relative importance analyses using the R package relampo to assess the unique proportion of variance in burnout that was explained by significant independent variables in the multivariable models; this analysis partitioned the explained variance (R2) in burnout that was explained by each independent variable after accounting for intercorrelations among these variables.34
RESULTS
Descriptives
Of the 4156 eligible employed faculty, 1781 (42.9%) participated in the survey. In the current study, we focused on 1346 (75.6%) faculty who spent some time on patient care duties; faculty who responded that their clinical time during the work week was more than 0% time.
Table 1 shows the demographic composition of the sample. While we did not ask about degree, the vast majority of our faculty are physician MDs/DOs, with approximately 110 doctoral-level clinical psychologists across the system. Our sample contained an equal distribution of men (44.2%) and women (43.8%). About a third screened positive for burnout (MBI-2: 30.0%, WBI: 34.8%), with 37.7% reporting that they experienced WLI, and 63.1% endorsing overall professional satisfaction. Half of the sample reported that the EHR adds frustration to their day and 40.4% reported spending over an hour on the EHR outside work per day. Additionally, 24.7% spent >60 minutes on daily clerical work time, while 52.0% reported that their practice unloads clerical burden. Correlations did not reveal any moderate-to-strong (r > 0.4) significant interactions between demographic/predictor variables, and thus we included all variables in the multivariable analysis except depression, which we excluded in regressions with WBI burnout due to a shared question between this scale and the PHQ-2.
Table 1.
Personal and professional characteristics of the 1346 clinical faculty
| Participant Demographics n (%) or mean [SD] | |
|---|---|
| Gender | |
| Female | 589 (43.8) |
| Male | 595 (44.2) |
| Nonbinary/third gender/other | 52 (3.9) |
| Missing | 110 (8.2) |
| Age | |
| 20–39 | 372 (27.6) |
| 40–59 | 639 (47.5) |
| 60+ | 219 (16.3) |
| Missing | 116 (8.6) |
| Professional characteristics | |
| Faculty level | |
| Instructor, other | 153 (11.4) |
| Assistant professor | 639 (47.5) |
| Associate professor/professor | 429 (31.9) |
| Missing | 125 (9.3) |
| Full-time status | |
| Full-time | 1093 (81.2) |
| Part-time >60 | 113 (8.4) |
| Part-time <60 | 36 (2.6) |
| Missing | 105 (7.8) |
| % Time spent on clinical care | |
| 1–40% | 330 (24.5) |
| 41–60% | 277 (20.6) |
| >60% | 739 (54.9) |
| Hours worked per week | |
| <=40 | 199 (14.8) |
| 41–60 | 625 (46.4) |
| >60 | 416 (30.9) |
| Missing | 106 (7.9) |
| Department | |
| Primary Care | 170 (12.6) |
| Medicine/Pediatrics subspecialty | 226 (16.8) |
| Surgery (general and subspecialties) | 182 (13.5) |
| Hospital & EM | 146 (10.8) |
| Anesthesia/Radiology/Pathology | 205 (15.2) |
| Other specialties | 230 (17.1) |
| Other departments | 82 (6.1) |
| Depression, Resilience, and Meaning | |
| Depression (PHQ-2) | |
| Screen positive | 291 (21.6) |
| Work I do is meaningful to me | |
| Disagree/strongly disagree | 31 (2.3) |
| Neither agree nor disagree | 45 (3.3) |
| Agree/strongly agree | 1265 (93.8) |
| Missing | 7 (0.5) |
| Resilience (CD-RISC-2) a | 7.0 [1.3] |
| Electronic Health Record & Clerical Burden | |
| EHR adds frustration to my day | |
| Disagree/strongly disagree | 296 (22.0) |
| Neither agree nor disagree | 346 (25.7) |
| Agree/strongly agree | 683 (50.7) |
| Missing | 21 (1.6) |
| Time spent on EHR (outside work) per day (min) | |
| 0 | 180 (13.4) |
| <30 | 275 (20.4) |
| 30–60 | 320 (23.8) |
| 61–90 | 241 (17.9) |
| >90 | 303 (22.5) |
| Missing | 27 (2.0) |
| Time Spent on clerical work per day (min) | |
| 0 | 194 (14.4) |
| <30 | 416 (30.9) |
| 30–60 | 388 (28.8) |
| 61–90 | 192 (14.3) |
| > 90 | 141 (10.5) |
| Missing | 15 (1.1) |
| Practice makes an effort to unload clerical burden | |
| Not at all/a little | 624 (46.4) |
| Somewhat/a lot | 700 (52.0) |
| Missing | 22 (1.6) |
| Burnout, work–life integration, and professional satisfaction | |
| Maslach Burnout Inventory b | 2.8 [1.9] |
| Burned out | 390 (29.0) |
| Not burned out | 910 (67.6) |
| Missing | 46 (3.4) |
| Mayo Well-Being Index b | 4.0 [3.2] |
| Burned out | 453 (33.7) |
| Not burned out | 849 (63.1) |
| Missing | 44 (3.3) |
| Work leaves enough time for family (WLI) | |
| Disagree/strongly disagree | 553 (41.1) |
| Neither agree nor disagree | 279 (20.7) |
| Agree/strongly agree | 508 (37.7) |
| Missing | 6 (0.) |
| Overall I am satisfied with my job (PS) | |
| Disagree/strongly disagree | 239 (17.8) |
| Neither agree nor disagree | 251 (18.6) |
| Agree/strongly agree | 849 (63.1) |
| Missing | 7 (0.5) |
CD-RISC-2 = Conner-Davidson Resilience Scale 2 item; EHR = Electronic health record; EM = Emergency Medicine; MBI-2 = Maslach Burnout Inventory 2 item; min=minutes; PS = Professional Satisfaction (Overall I am satisfied with my job); Path = Pathology; PHQ-2 = Patient Health Questionnaire 2 item; WBI = Mayo Well-Being Index; WLI = Work–life integration (My work schedule leaves enough time for my personal/family life).
Continuous measures are described as mean [SD].
For both burnout measures, percentages represent the percentage of respondents who met the designated threshold for burnout on each scale (see Methods).
Burnout: MBI-2 and WBI
Table 2 shows results of bivariate analyses of dichotomous burnout for the MBI and WBI; bivariate analyses of continuous MBI and WBI scores are shown in Supplemental Table S1.
Table 2.
Prevalence of burnout, work–life integration, and professional satisfaction by personal and professional characteristics and EHR clerical burden (bivariate analyses)
| MBI-2 n (%) Burnout | P value | WBI n (%) Burnout | P value | WLI n (%) (strongly) agree | P value | PS n (%) (strongly) agree | P value | |
|---|---|---|---|---|---|---|---|---|
| Total | 390 (29.0) | 453 (34.8) | 508 (37.9) | 849 (63.4) | ||||
| Demographics and professional characteristics | ||||||||
| Gender | ||||||||
| Female | 192 (33.4) | P = .007a | 224 (39.1) | P = .001a | 195 (33.2) | P = .0007a | 357 (61.0) | P = .06 |
| Male | 143 (25.1) | P = .0007a | 163 (28.2) | P < .0001a | 264 (44.6) | P < .0001a | 403 (68.0) | P = .004a |
| Non-binary/third gender/other | 20 (40.0) | P = .11 | 26 (54.2) | P = .004a | 10 (19.2) | P = .004a | 25 (48.1) | P = .02 |
| Age | ||||||||
| 20–39 | 122 (33.5) | P = .05 | 148 (40.3) | P = .004a | 148 (40.0) | P = .37 | 224 (60.7) | P = .13 |
| 40–59 | 190 (30.5) | P = .48 | 221 (35.6) | P = .32 | 216 (33.9) | P = .001a | 392 (61.4) | P = .06 |
| 60+ | 40 (19.7) | P = .0007a | 42 (20.1) | P < .0001a | 104 (47.7) | P = .001a | 167 (76.6) | P < .0001a |
| Faculty level | ||||||||
| Instructor/other | 47 (32.2) | P = .42 | 55 (36.9) | P = .42 | 74 (48.7) | P = .005a | 97 (63.8) | P = 1.00 |
| Assistant prof | 198 (31.7) | P = .06 | 229 (36.8) | P = .04 | 229 (36.0) | P = .12 | 370 (58.2) | P < .0001a |
| Associate prof/professor | 101 (24.7) | P = .009 | 120 (28.9) | P = .007a | 161 (37.7) | P = .76 | 309 (72.4) | P < .001a |
| Full-time status | ||||||||
| Full-time | 327 (30.8) | P = .08 | 386 (36.3) | P < .001a | 386 (35.5) | P < .001a | 683 (62.8) | P = .08 |
| Part time | 32 (23.4) | 28 (19.7) | 84 (57.1) | 103 (70.1) | ||||
| % Time spent on clinical care | ||||||||
| 1%–40% | 79 (24.8) | P = .02 | 95 (29.8) | P = .03 | 133 (40.7) | 0.23 | 230 (70.1) | P = .004a |
| 41%–60% | 78 (28.8) | P = .62 | 103 (38.9) | P = .11 | 98 (35.5) | 0.37 | 178 (64.1) | P = .76 |
| 61%–100% | 233 (32.8) | P = .02 | 255 (35.5) | P = .55 | 277 (37.6) | 0.76 | 441 (60.1) | P = .005a |
| Hours worked/wk | ||||||||
| <40 | 55 (29.3) | P = .84 | 51 (26.2) | P = .009 | 132 (66.3) | P < .0001a | 126 (63.6) | P = 1.00 |
| 41–60 | 164 (27.1) | P = .04 | 188 (31.0) | P = .01 | 258 (41.6) | P = .009 | 413 (66.5) | P = .03 |
| >60 | 138 (34.0) | P = .02 | 175 (43.4) | P < .0001a | 79 (19.0) | P < .0001a | 245 (59.0) | P = .02 |
| Department | ||||||||
| Primary Care | 70 (41.9) | P < .001a | 66 (39.5) | P = .169 | 50 (29.6) | P = .02a | 85 (50.3) | P < .001a |
| All Others | 320 (28.2) | 387 (34.1) | 458 (39.1) | 764 (65.3) | ||||
| Medicine/Pediatric Subspecialty | 60 (27.5) | P = .38 | 80 (36.7) | P = .52 | 65 (28.9) | P = .002a | 145 (64.4) | P = .72 |
| All Others | 330 (30.5) | 373 (34.4) | 443 (39.7) | 704 (63.2) | ||||
| Surgery | 52 (29.7) | P = .93 | 67 (38.1) | P = .33 | 59 (32.4) | P = .10 | 114 (62.6) | P = .82 |
| All Others | 338 (30.0) | 386 (34.3) | 449 (38.8) | 735 (63.5) | ||||
| Hospital/EM | 52 (35.9) | P = .10 | 55 (38.2) | P = .36 | 73 (50.0) | P = .001a | 88 (60.3) | P = .40 |
| All others | 338 (29.3) | 398 (34.4) | 435 (36.4) | 761 (63.8) | ||||
| Anes/Rad/Path | 37 (19.4) | P = .001a | 44 (22.7) | P < 0.001a | 98 (48.0) | P = 0.001a | 153 (75.0) | P < .001a |
| All others | 353 (31.8) | 409 (36.9) | 410 (36.1) | 696 (61.3) | ||||
| Other specialty | 56 (25.0) | P = .07 | 66 (29.5) | P = 0.07 | 99 (43.3) | P = 0.06 | 161 (70.6) | P = .01a |
| All others | 334 (31.0) | 387 (35.9) | 409 (36.8) | 688 (61.9) | ||||
| Other depart | 22 (28.9) | P = .84 | 27 (32.9) | P = .71 | 34 (42.5) | P = .38 | 52 (65.0) | P = .76 |
| All others | 369 (30.1) | 426 (34.9) | 474 (37.6) | 797 (63.3) | ||||
| EHR and clerical work | ||||||||
| Daily clerical work time- min | ||||||||
| <=60 | 250 (26.0) | P < .001a | 295 (30.5) | P < .001a | 414 (41.7) | P < .001a | 683 (68.8) | P < .001a |
| >60 | 138 (42.5) | 155 (48.1) | 86 (25.9) | 155 (46.8) | ||||
| Daily EHR time outside work- min | ||||||||
| <=90 | 251 (25.6) | 302 (30.8) | P < .001a | 434 (43.0) | P < .001a | 677 (67.1) | P < .001a | |
| >90 | 134 (45.4) | P < .001a | 143 (48.3) | 61 (20.1) | 155 (51.2) | |||
| EHR frustration | ||||||||
| Agree | 250 (37.7) | P < .001a | 278 (41.9) | P < .001a | 212 (31.2) | P < .001a | 382 (56.2) | P < .001a |
| Disagree/neutral | 136 (22.0) | 171 (27.6) | 284 (44.4) | 452 (70.8) | ||||
| Practice unloads clerical work | ||||||||
| Agree | 153 (22.7) | P < .001a | 203 (29.9) | P < .001a | 286 (41.1) | P = .01a | 496 (71.1) | P < .001a |
| Disagree/neutral | 230 (38.0) | 245 (40.6) | 213 (34.2) | 338 (54.6) | ||||
| depression, meaning and resilience | ||||||||
| Depression | ||||||||
| Yes | 169 (58.7) | P < .001a | 235 (81.9) | P < .001a | 70 (24.1) | P < .001a | 103 (35.5) | P < .001a |
| No | 215 (21.5) | 217 (21.5) | 431 41.7) | 737 (71.4) | ||||
| Meaning in work | ||||||||
| Agree | 341 (28.0) | P < .001a | 415 (33.8) | P < .001a | 494 (39.2) | P < .001a | 843 (66.9) | P < .001a |
| Neutral/disagree | 47 (63.5) | 37 (52.9) | 14 (18.4) | 5 (6.6) | ||||
| Resilience- CD-RISC-2 Mean (std) | ||||||||
| Burned out/agree | 6.676 (1.403) | P < .001a | 6.696 (1.403) | P < .001a | 7.140 (1.281) | P = .002a | 7.173 (1.177) | P < .001a |
| Not burned out/neutral Disagree | 7.138 (1.189) | 7.166 (1.177) | 6.916 (1.278) | 6.711 (1.402) | ||||
Abbreviations: Anes/Rad/Path, Anesthesia/Radiology/Pathology; CD-RISC-2, Conner-Davidson Resilience Scale 2 item; EM: emergency medicine; EHR: electronic health record; MBI-2: Maslach Burnout Inventory 2 item; min: minutes; PS: Professional Satisfaction (Overall I am satisfied with my job); PHQ-2: patient health questionnaire 2 item; WBI: Mayo Well-Being Index; wk: week; WLI: Work-life integration (My work schedule leaves enough time for my personal/family life).
Note: Percentages were calculated as a proportion of each subgroup in the first column that were positive for burnout on the WBI, MBI, or agreed with the WLI or PS. See Table 1 for subgroup totals. Missing responses for burnout, WLI, and PS were not imputed.
P values for trichotomous variables represent posthoc residual analysis with converted Chi square P values with significance level of .008 based on the Bonferroni correction for multiple comparisons. P values for dichotomous variables represent the Pearson Chi-square 2 sided with a significant P value < .05.
Multivariable logistic and linear regression models explained 30% and 32% of the variance for the MBI and 19% and 20% of the variance for the WBI, respectively. Full-time work (MBI and WBI), age 20–39 (MBI and WBI), working >40% clinical (WBI), working >60% clinically (MBI), and being an assistant professor were associated with burnout. Female gender, nonbinary/other gender, working >60 hours/week and being younger than 60 were significantly associated with increased burnout and higher scores on the WBI. Respondents from Anesthesiology/Radiology/Pathology and Other Specialties were less likely to screen positive for burnout on the MBI and had lower scores on both scales. A positive depression screen was associated with positive screen and severity of burnout, while higher resilience scores were associated with lower likelihood of a positive screen for burnout and lower burnout scores. Meaning in work was associated with lower likelihood of screening positive for burnout on the MBI and lower average burnout scores on both scales. (Table 3, Supplemental Table S2).
Table 3.
Prevalence of burnout, work–life integration, and professional satisfaction by personal, professional characteristics and EHR clerical burden (multivariable analyses)
| MBI-2 Burnout R2 = 0.30 | WBI Burnout R2 = 0.19 | WLI R2 = 0.28 | PS R2 = 0.33 | |
|---|---|---|---|---|
| OR [95% CI]; P value | OR [95% CI]; P value | OR [95% CI]; P value | OR [95% CI]; P value | |
| Gender (ref: Male) | ||||
| Female | 1.29 [0.93–1.78]; P = .12 | 1.60 [1.20–2.14]; P = .001a | 0.48 [0.36–0.65]; P < 0.001a | 0.97 [0.71–1.32]; P = .83 |
| Non-binary/third gender/other | 1.01 [0.47–2.19]; P = .97 | 2.36 [1.16–4.81]; P = .02a | 0.28 [0.11–0.70]; P = 0.007a | 0.71 [0.33–1.52]; P = .38 |
| Age (ref: 20–39) | ||||
| 40–59 | 0.98 [0.68–1.42]; P =.93 | 0.82 [0.59–1.14]; P = .24 | 0.74 [0.53–1.05]; P = .09 | 0.89 [0.62–1.26]; P = .50 |
| 60+ | 0.65 [0.37–1.13]; P = .13 | 0.44 [0.26–0.73]; P = .002a | 0.97 [0.60–1.57]; P = .91 | 1.56 [0.92–2.63]; P = .10 |
| Part-time status (ref: full-time) | 0.76 [0.44–1.30]; P = .31 | 0.58 [0.35–0.97]; P = .04a | 1.35 [0.85–2.15]; P = .20 | 1.31 [0.78–2.20]; P = .30 |
| Time Spent Clinical Care (ref: 1%–40%) | ||||
| 41%–60% | 0.94 [0.58–1.51]; P = .79 | 1.51 [0.99–2.29]; P = .06 | 0.90 [0.59–1.36]; P = .62 | 0.80 [0.51–1.26]; P = .34 |
| 61%–100% | 1.38 [0.92–2.05]; P = .12 | 1.36 [0.978–2.009]; P = .09 | 0.75 [0.52–1.07]; P = .11 | 0.59 [0.40–0.86]; P = .007a |
| Hours worked/wk (ref: <=40) | ||||
| 41–60 | 0.96 [0.58–1.58]; P = .88 | 1.27 [0.81–2.00]; P = .30 | 0.37 [0.24–0.56]; P < .001a | 1.32 [0.82–2.11]; P = .25 |
| >60 | 1.17 [0.68–2.02]; P = .58 | 1.93 [1.18–3.16]; P = .009a | 0.12 [0.08–0.21]; P < .001a | 1.04 [0.62–1.75]; P = .88 |
| Level (ref: instructor/other) | ||||
| Assistant professor | 1.14 [0.71–1.82]; P = .60 | 1.00 [0.65–1.53]; P = 1.0 | 0.50 [0.32–0.76]; P = .002a | 0.60 [0.38–0.96]; P = .03a |
| Associate/full professor | 1.10 [0.63–1.82]; P =0.73 | 1.07 [0.65–1.77]; P = .79 | 0.55 [0.33–0.92]; P = .02a | 0.85 [0.49–1.45]; P = .55 |
| Department | ||||
| Primary care | 1.09 [0.60–1.97]; P = .77 | 0.83 [0.48–1.44]; P = .51 | 0.68 [0.37–1.22]; P = .19 | 0.76 [0.43–1.34]; P = .34 |
| Medicine/Pediatrics subspecialty | 0.59 [0.33–1.08]; P = .09 | 0.81 [0.47–1.38]; P = .43 | 0.77 [0.43–1.37]; P = .37 | 1.43 [0.81–2.53]; P = .22 |
| Surgery | 0.58 [0.313–1.083]; P = .09 | 0.84 [0.48–1.46]; P = .53 | 0.93 [0.52–1.67]; P = .80 | 1.59 [0.88–2.85]; P = .12 |
| Hospital/EM | 0.89 [0.498–1.749]; P = .73 | 1.04 [0.58–1.85]; P = .90 | 1.30 [0.71–2.38]; P = .39 | 1.68 [0.91–3.11]; P = .10 |
| Anes/Rad/Path | 0.50 [0.26–0.96]; P = .04a | 0.58 [0.32–1.04]; P = .07 | 1.21 [0.68–2.18]; P = .52 | 2.28 [1.23–4.20]; P = .009a |
| Other specialty | 0.53 [0.29–0.97]; P = .04a | 0.68 [0.40–1.16]; P = .16 | 1.08 [0.62–1.87]; P = .79 | 1.97 [1.12–3.48]; P = .02a |
| Depression, meaning, and resilience | ||||
| Depression (PHQ-2) | 4.41 [3.14–6.21]; P < .001a | – | 0.54 [0.37–0.78]; P = .001a | 0.27 [0.19–0.38]; P < .001a |
| Meaning in work (ref: disagree/neutral) | 0.36 [0.19–0.67]; P = .001a | 0.64 [0.36–1.14]; P = .13 | 2.51 [1.23–5.11]; P = .01a | 21.67 [8.17–57.47]; P < .001a |
| Resilience score (CD-RISC-2) | 0.84 [0.75–0.95]; P = .005a | 0.77 [0.69–0.85]; P < .001a | 1.12 [1.00–1.26]; P = .06 | 1.14 [1.02–1.28]; P = .02a |
| EHR and clerical burden | ||||
| Practice unloads clerical work (ref: disagree/neutral) | 0.50 [0.37–0.69]; P < .001a | 0.66 [0.50–0.87]; P = .003a | 1.32 [0.99–1.75]; P = .06 | 1.72 [1.28–2.32]; P < .001a |
| Frustration with EHR (ref: disagree/neutral) | 1.64 [1.19–2.26]; P = .003a | 1.66 [1.25–2.21]; P = .001a | 0.75 [0.56–1.01]; P = .06 | 0.81 [0.612–1.132]; P = .17 |
| EHR time outside work per Day >90 min (ref:<=90 min) | 1.90 [1.40–2.78]; P < .001a | 1.41 [1.01–1.95]; P = .04a | 0.67 [0.46–0.84]; P = .04a | 0.66 [0.46–0.94]; P = .02a |
| Time on clerical work/day (ref:<=60 min) | 1.24 [0.88–1.75]; P = .23 | 1.39 [1.01–1.91]; P = .04a | 0.58 [0.40–0.84]; P = .003a | 0.54 [0.39–0.76]; P < .001a |
Abbreviations: Anes/Rad/Path, Anesthesia/Radiology/Pathology; CD-RISC-2, Conner-Davidson Resilience Scale 2 item; EM, emergency medicine; EHR, electronic health record; MBI-2, Maslach Burnout Inventory 2 item; min, minutes; PS, professional satisfaction (Overall I am satisfied with my job); PHQ-2, patient health questionnaire 2 item; WBI, Mayo Well-Being Index; wk, week; WLI, work–life integration (My work schedule leaves enough time for my personal/family life).
Multivariable logistic regression, significant factors with P value < .05.
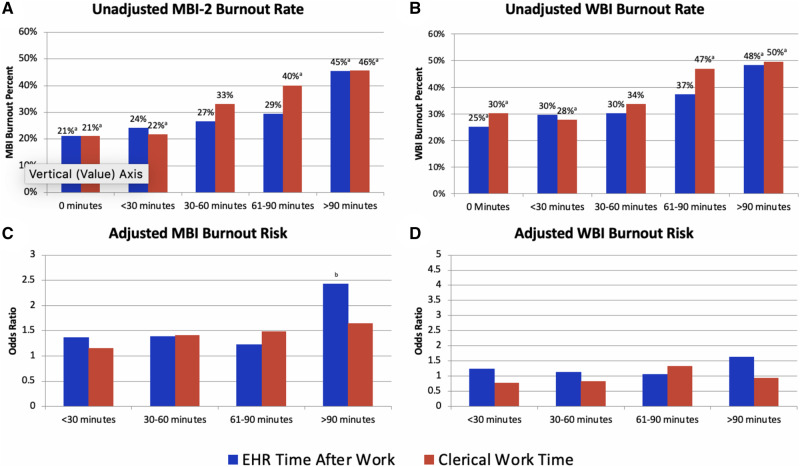
Figure 1 shows the unadjusted and adjusted relationship between spending increasing amounts of time on the EHR outside work and clerical tasks and overall burnout. As the thresholds for significantly increased likelihood of burnout in the unadjusted model were >90 minutes for EHR-outside work and >60 minutes for clerical time, we utilized these thresholds to dichotomize these variables for further analysis. In the multivariable analyses, EHR-outside work >90 minutes/day, frustration with EHR (MBI and WBI), and clerical work time >60 minutes (WBI) remained significantly associated with burnout. Agreeing that practice unloads clerical burden was associated with a lower likelihood of burnout and lower burnout scores (Table 3 and Supplemental Table S2). We also examined the interaction between faculty rank and hours worked and the EHR predictors and found that of those who spend >90 minutes EHR after work, associate and full professors were less likely than instructors/others to be burned out on the MBI (OR = 0.34, P = .007). Among faculty with >90 minutes EHR after work, assistant professors were more likely than the instructors/others to screen positive for burnout on the WBI (OR 3.5, P = .03). EHR > 90 minutes remained a significant predictor of burnout on the MBI but not the WBI when adjusting for the rank-EHR > 90 minutes interaction. Among those who spent >60 minutes on clerical work, those who worked 40–60 and >60 hours/week were more likely to be burned out (OR = 5.4, P = .002; OR = 2.3, P = .04). There were no other significant interactions with rank and hours worked and the EHR/clerical metrics.
Figure 1.
Relationship between daily time spent on the EHR after work and clerical work with burnout on the MBI-2 and WBI: a. Relationship between unadjusted burnout prevalence on the MBI-2 and daily time spent on the EHR after work and clerical time. b. Relationship between unadjusted burnout prevalence on the MBI-2 and daily time spent on the EHR after work and clerical time. c. Relationship between adjusted burnout odds on the MBI-2 and daily time spent on the EHR after work and clerical time. d. Relationship between adjusted burnout odds on the WBI and daily time spent on the EHR after work and clerical time.
*Represents significantly different results from the null hypotheses based on Bonferroni corrected p values for Chi-square analyses.
**Represents significantly associations on the multivariable logistic regression.
Abbreviations: EHR, electronic health record; MBI-2, Maslach Burnout Inventory 2 item; WBI, Mayo Well-Being Index.
Relative importance analyses of significant correlates of burnout from the multivariable logistic regression models revealed that depression (40% relative variance explained [RVE]), spending >90 minutes on the EHR after work (13% RVE), unloading clerical burden (12% RVE) and EHR frustration (10% RVE) accounted for the majority of explained variance in positive screen for burnout assessed by the MBI-2; while resilience (24% RVE), EHR frustration (14% RVE), age (13% RVE), and spending >90 minutes on the EHR after work (11% RVE) accounted for the majority of explained variance in WBI burnout.
Work–life integration (WLI) and professional satisfaction (PS)
Table 2 shows results of bivariate analyses of WLI and PS.
The multivariable regression models explained 28% of the variance for WLI and 33% of the variance for PS. As shown in Table 3, being female nonbinary/third gender, working 41–60 or >60 hours per week, and having higher academic rank were associated with lower likelihood of WLI. Assistant professors and those who spent >60% time on clinical care were significantly less likely to endorse overall PS, whereas those in Anesthesia/Radiology/Pathology and Other Specialties were nearly twice as likely to experience PS. Those who screened positively for depression were less likely to experience WLI and PS; and those endorsing meaning in work were over 2 and 21 times as likely as those who did not to have WLI and PS, respectively. Higher resilience scores were associated with PS. Given the strong relationship with meaning in work and PS, we conducted a sensitivity analysis without that variable and found similar results for the PS outcome (results not shown, available from the corresponding author upon request).
Spending >90 minutes/day on EHR-outside work and >60 minutes/day on clerical work were significantly associated with lower likelihood of WLI and PS. Agreement that one’s practice unloads clerical work was associated with a higher likelihood of WLI and PS.
Relative importance analyses revealed that hours worked (50% RVE), spending >90 minutes on the EHR after work (14% RVE), depression (12% RVE), and spending >60 minutes/day on clerical work (10% RVE) accounted for the majority of explained variance in WLI, while meaning in work (38% RVE), depression (24% RVE), and >60 minutes/day on clerical work (8% RVE) accounted for the majority of explained variance in PS.
DISCUSSION
Our study demonstrates a significant association between EHR time and clerical burden and burnout in clinical faculty. While previous studies have observed a link between EHR frustration and work after hours with burnout,7,14,16,17,19 our study suggests that specific time thresholds of EHR outside of work and clerical work may be linked to burnout, even after controlling for other key risk factors of burnout. Specifically, spending more than 90 minutes on the EHR outside of work was associated with 90% and 40% increased odds of burnout on the MBI and WBI, respectively, and accounted for >10% of the explained variance in multivariable models, while spending >60 minutes/day on clerical work was associated with a 40% increased odds of WBI burnout.
EHR and clerical burden were also negatively associated with WLI and professional satisfaction. Spending >90 minutes on the EHR outside work was associated with 33% lower odds of WLI and spending >60 minutes/day on clerical work with 42% and 46% lower odds of attaining WLI and PS, respectively. However, the perception of one’s practice unloading clerical burden was associated with half the odds of burnout on the MBI and a third lower odds of burnout on the WBI and with 70% higher odds of achieving professional satisfaction. As expected, depression and MBI burnout were closely associated, and screening positive for depression had the strongest association with MBI-assessed burnout in our multivariable model. These findings are consistent with prior work.35–41
Our study highlights a number of other notable findings. While perceiving greater meaning in work, being resilient, and not having depression are associated with a lower likelihood of burnout, one can still be burnt-out in the presence of these protective factors. There are clearly other unmeasured factors that may contribute to burnout risk in clinical faculty. It is also important to note the lower prevalence of burnout in the Anesthesia, Radiology, Pathology group. These departments used a different EMR than the others in our study and they also interact with that EMR in very different ways. Radiologists and pathologists use dictation software or a transcription service for documentation. While they must review and correct the documentation, the burden and type of documentation is distinct from those who type notes and navigate through a complex and redundant EHR system. In addition, while the group was small, we were able to gather data on nonbinary/third gender/other faculty members and showed that this group is at significantly higher risk for burnout and less likely to be professionally satisfied or have work–life integration. Finally, faculty rank seems to moderate the effect of the EHR on burnout in faculty. While it may not be a person’s rank itself that impacts burnout, it’s possible that those in the lower ranks may feel additional stress to be productive both clinically and academically.
In our study, the threshold of >90 minutes on the EHR outside of the workday was an important predictor of burnout in both bivariate and multivariable analyses. Interventions that focus on reducing documentation and EHR burden below this threshold may be effective in mitigating risk for burnout in clinical faculty. Scribes have been shown to decrease time spent on documentation, and improve the patient and provider experience, as well as decrease burnout and improve professional satisfaction.20,22,25 Other lower cost approaches, such as predesigned templates and phrases, and EHR efficiency trainings may also help decrease EHR burden, increase professional satisfaction, and decrease overall stress.20,41 Artificial intelligence-based solutions, such as voice recognition and automated dictation/note writing similar to what our Anesthesia, Radiology, and Pathology colleagues use,42,43 may also help reduce EHR and clerical burden. Studies on the impact of transcription and voice recognition software on physician well-being, while limited, show potential improvements in quality and efficiency of documentation and in satisfaction with the EHR.44,45 Moreover, as clerical burden was a significant predictor of WBI-assessed burnout, team-based interventions aimed at reducing overall clerical burden, such as trainings to improve teamwork, efficiency, and communication skills, as well as added clerical support for clinical faculty, can be considered as part of efforts to reduce burnout.20–23,46 Whatever the specific planned intervention, the association between a practice’s effort to unload clerical work and lower risk for burnout suggests that a practice’s effort to engage in the process of how to unload clerical burden—whether successful or not—may improve a provider’s sense of overall professional well-being and represents a meaningful touchpoint for organizational interventions on provider burnout.
There are a number of important potential limitations of this study. Our study was cross-sectional, so we were unable to determine directionality or causality for the observed associations. Our moderate response rate may indicate some degree of response bias. In our study, we did not assess advanced practice providers who are similarly burdened with the EHR and clerical burden. We were unable to assess other potential drivers of burnout as we had to keep the survey at a reasonable length. Notably, while the majority of the faculty in this survey population use the same EHR, three departments grouped together—Anesthesia, Radiology, and Pathology—use different electronic medical record systems, some of which have integrated dictation systems, which could have affected their EHR and clerical burden and ultimately impacted their level of burnout. Finally, to minimize participant burden, we utilized brief versions of the MBI and the CD-RISC, which have good validity but may not allow for a more nuanced examination of burnout and resilience that the longer versions offer.
CONCLUSION
Results of this study demonstrate a relationship between EHR/clerical burden and burnout in clinical faculty and suggest specific time spent thresholds associated with burnout. Data suggest that providers who work in a setting where there is a perceived effort to reduce this burden may experience a work culture benefit that buffers some of the negative impacts of clerical burden on physician and clinician well-being. As such, future studies should investigate novel ways of offloading such burdens, a process to involve and communicate with providers, and the impact of such interventions on burnout. In addition, future work should assess the relationship of EHR/clerical burden and burnout among other clinical providers, such as Nurse Practitioners and Physician’s Assistants. As we continue to tackle the challenge of physician and provider burnout, efforts designed to reduce EHR and clerical burden to less than an hour or so a day, while engaging clinicians in a process that visibly moves towards reducing such burden may help promote greater well-being and professional satisfaction in clinical faculty.
FUNDING AND ACKNOWLEDGMENTS
We acknowledge the Dean’s Office of the Icahn School of Medicine at Mount Sinai for its funding and support of this study. The funding was solely used for the incentive items for participants.
AUTHOR CONTRIBUTIONS
All authors listed have contributed sufficiently and meet all four criteria for authorship, and all who meet the four criteria are identified as authors in this manuscript.
SUPPLEMENTARY MATERIAL
Supplementary material is available at Journal of the American Medical Informatics Association online.
DATA AVAILABILITY
The data underlying this article cannot be shared publicly due to its confidential nature and the importance of protecting the privacy of our participants. The data will be shared on reasonable request to the corresponding author.
CONFLICT OF INTEREST STATEMENT
None declared.
Supplementary Material
REFERENCES
- 1. Oreskovich MR, Kaups KL, Balch CM, et al. Prevalence of alcohol use disorders among American surgeons. Arch Surg 2012; 147 (2): 168–74. [DOI] [PubMed] [Google Scholar]
- 2. Shanafelt TD, Balch CM, Bechamps G, et al. Burnout and medical errors among American surgeons. Ann Surg 2010; 251 (6): 995–1000. [DOI] [PubMed] [Google Scholar]
- 3. Hamidi MS, Bohman B, Sandborg C, et al. Estimating institutional physician turnover attributable to self-reported burnout and associated financial burden: a case study. BMC Health Serv Res 2018; 18 (1): 851.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Sinsky CA, Dyrbye LN, West CP, Satele D, Tutty M, Shanafelt TD.. Professional satisfaction and the career plans of US physicians. Mayo Clin Proc 2017; 92 (11): 1625–35. [DOI] [PubMed] [Google Scholar]
- 5. Taking Action against Clinician Burnout: A Systems Approach to Professional Well-Being. National Academies Press; ( US: ); 2019. [PubMed] [Google Scholar]
- 6. Kishore S, Ripp J, Shanafelt T, et al. Making the case for the chief wellness officer in America’s health systems: A call to action. Health Aff Blog 2018; [Google Scholar]
- 7. Kroth PJ, Morioka-Douglas N, Veres S, et al. Association of electronic health record design and use factors with clinician stress and burnout. JAMA Netw Open 2019; 2 (8): e199609.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. McMurray JE, Linzer M, Konrad TR, Douglas J, Shugerman R, Nelson K; for the SGIM Career Satisfaction Study Group. The work lives of women physicians. J Gen Intern Med 2000; 15 (6): 372–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Shanafelt TD, Boone S, Tan L, et al. Burnout and satisfaction with work-life balance among us physicians relative to the general us population. Arch Intern Med 2012; 172 (18): 1377–85. [DOI] [PubMed] [Google Scholar]
- 10. Shanafelt TD, Gradishar WJ, Kosty M, et al. Burnout and career satisfaction among US oncologists. JCO 2014; 32 (7): 678–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Shanafelt T, Balch C, Bechamps G, et al. Burnout and career satisfaction among American surgeons. Ann Surg 2009; 250 (3): 463–71. [DOI] [PubMed] [Google Scholar]
- 12. Smith CD, Balatbat C, Corbridge S, et al. Implementing optimal team-based care to reduce clinician burnout. NAM Perspect 2018. [Google Scholar]
- 13. Welp A, Manser T.. Integrating teamwork, clinician occupational well-being and patient safety – development of a conceptual framework based on a systematic review. BMC Health Serv Res 2016; 16 (1): 281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Shanafelt TD, Dyrbye LN, Sinsky C, et al. Relationship between clerical burden and characteristics of the electronic environment with physician burnout and professional satisfaction. Mayo Clin Proc 2016; 91 (7): 836–48. [DOI] [PubMed] [Google Scholar]
- 15. Arndt BG, Beasley JW, Watkinson MD, et al. Tethered to the EHR: primary care physician workload assessment using EHR event log data and time-motion observations. Ann Fam Med 2017; 15 (5): 419–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Robertson SL, Robinson MD, Reid A.. Electronic health record effects on work-life balance and burnout within the I3 population collaborative. J Grad Med Educ 2017; 9 (4): 479–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Gardner RL, Cooper E, Haskell J, et al. Physician stress and burnout: the impact of health information technology. J Am Med Inform Assoc JAMIA 2019; 26 (2): 106–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Melnick ER, Dyrbye LN, Sinsky CA, et al. The association between perceived electronic health record usability and professional burnout among US physicians. Mayo Clin Proc 2019; 95 (3): 476–87. [DOI] [PubMed] [Google Scholar]
- 19. Tran B, Lenhart A, Ross R, Dorr DA.. Burnout and EHR use among academic primary care physicians with varied clinical workloads. AMIA Jt Summits Transl Sci Proc 2019; 2019: 136–44. [PMC free article] [PubMed] [Google Scholar]
- 20. DeChant PF, Acs A, Rhee KB, et al. Effect of organization-directed workplace interventions on physician burnout: a systematic review. Mayo Clin Proc Innov Qual Outcomes 2019; 3 (4): 384–408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Linzer M, Poplau S, Grossman E, et al. A cluster randomized trial of interventions to improve work conditions and clinician burnout in primary care: results from the healthy work place (HWP) study. J Gen Intern Med 2015; 30 (8): 1105–11. doi:10.1007/s11606-015-3235-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Contratto E, Romp K, Estrada CA, Agne A, Willett LL.. Physician order entry clerical support improves physician satisfaction and productivity. South Med J 2017; 110 (5): 363–8. [DOI] [PubMed] [Google Scholar]
- 23. Linzer M, Poplau S, Brown R, et al. Do work condition interventions affect quality and errors in primary care? Results from the healthy work place study. J Gen Intern Med 2017; 32 (1): 56–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Hung DY, Harrison MI, Truong Q, Du X.. Experiences of primary care physicians and staff following lean workflow redesign. BMC Health Serv Res 2018; 18 (1): 274.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Pozdnyakova A, Laiteerapong N, Volerman A, et al. Impact of medical scribes on physician and patient satisfaction in primary care. J Gen Intern Med 2018; 33 (7): 1109–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. West CP, Dyrbye LN, Sloan JA, Shanafelt TD.. Single item measures of emotional exhaustion and depersonalization are useful for assessing burnout in medical professionals. J Gen Intern Med 2009; 24 (12): 1318–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. West CP, Tan AD, Shanafelt TD.. Association of resident fatigue and distress with occupational blood and body fluid exposures and motor vehicle incidents. Mayo Clin Proc 2012; 87 (12): 1138–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Dyrbye LN, Varkey P, Boone SL, Satele DV, Sloan JA, Shanafelt TD.. Physician satisfaction and burnout at different career stages. Mayo Clin Proc 2013; 88 (12): 1358–67. [DOI] [PubMed] [Google Scholar]
- 29. Spitzer RL. Utility of a new procedure for diagnosing mental disorders in primary care: the PRIME-MD 1000 study. JAMA 1994; 272 (22): 1749.. [PubMed] [Google Scholar]
- 30. Kroenke K, Spitzer RL, Williams JBW.. The patient health questionnaire-2: validity of a two-item depression screener. Med Care 2003; 41 (11): 1284–92. [DOI] [PubMed] [Google Scholar]
- 31. Whooley MA, Avins AL, Miranda J, Browner WS.. Case-finding instruments for depression. Two questions are as good as many. J Gen Intern Med 1997; 12 (7): 439–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Kuiper H, van Leeuwen CCM, Stolwijk-Swüste JM, Post MWM.. Measuring resilience with the Connor–Davidson Resilience Scale (CD-RISC): which version to choose? Spinal Cord 2019; 57 (5): 360–6. [DOI] [PubMed] [Google Scholar]
- 33. Likert R. A technique for the measurement of attitudes. Arch Psychol 1932. [Google Scholar]
- 34. Tonidandel S, LeBreton JM.. Determining the relative importance of predictors in logistic regression: an extension of relative weight analysis. Organ Res Methods 2010; 13 (4): 767–81. [Google Scholar]
- 35. Shanafelt T, Chung H, White H, Lyckholm LJ.. Shaping your career to maximize personal satisfaction in the practice of oncology. JCO 2006; 24 (24): 4020–6. [DOI] [PubMed] [Google Scholar]
- 36. Shanafelt TD, West CP, Sloan JA, et al. Career fit and burnout among academic faculty. Arch Intern Med 2009; 169 (10): 990–5. [DOI] [PubMed] [Google Scholar]
- 37. Reed S, Kemper KJ, Schwartz A, et al. Variability of burnout and stress measures in pediatric residents: an exploratory single-center study from the pediatric resident burnout–resilience study consortium. J Evid Based Complementary Altern Med 2018; 23: 2515690X1880477.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Simpkin AL, Khan A, West DC, et al. Stress from uncertainty and resilience among depressed and burned out residents: a cross-sectional study. Acad Pediatr 2018; 18 (6): 698–704. [DOI] [PubMed] [Google Scholar]
- 39. Dahn H, McGibbon A, Bowes D.. Burnout and resiliency in Canadian oncology residents: a nationwide resident and program director survey. Pract Radiat Oncol 2019; 9 (1): e118–e125. doi:10.1016/j.prro.2018.08.001 [DOI] [PubMed] [Google Scholar]
- 40. Bird A-N, Pincavage AT.. Initial characterization of internal medicine resident resilience and association with stress and burnout. J Biomed Educ 2016; 2016: 1–4. doi:10.1155/2016/3508638 [Google Scholar]
- 41. Menachemi N, Powers TL, Brooks RG.. The role of information technology usage in physician practice satisfaction. Health Care Manage Rev 2009; 34 (4): 364–71. [DOI] [PubMed] [Google Scholar]
- 42. Payne TH, Alonso WD, Markiel JA, et al. Using voice to create inpatient progress notes: effects on note timeliness, quality, and physician satisfaction. JAMIA Open 2018; 1 (2): 218–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Payne TH, Alonso WD, Markiel JA, Lybarger K, White AA.. Using voice to create hospital progress notes: Description of a mobile application and supporting system integrated with a commercial electronic health record. J Biomed Inform 2018; 77: 91–6. [DOI] [PubMed] [Google Scholar]
- 44. Blackley SV, Schubert VD, Goss FR, Al Assad W, Garabedian PM, Zhou L.. Physician use of speech recognition versus typing in clinical documentation: A controlled observational study. Int J Med Inform 2020; 141: 104178. [DOI] [PubMed] [Google Scholar]
- 45. Witt DJ. Transcription services in the ED. Am J Emerg Med 1995. Jan; 13 (1): 34–6. [DOI] [PubMed] [Google Scholar]
- 46. Dai M, Willard-Grace R, Knox M, et al. Team configurations, efficiency, and family physician burnout. J Am Board Fam Med 2020; 33 (3): 368–77. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data underlying this article cannot be shared publicly due to its confidential nature and the importance of protecting the privacy of our participants. The data will be shared on reasonable request to the corresponding author.