Abstract
Objective
The study sought to provide physicians, informaticians, and institutional policymakers with an introductory tutorial about the history of medical documentation, sources of clinician burnout, and opportunities to improve electronic health records (EHRs). We now have unprecedented opportunities in health care, with the promise of new cures, improved equity, greater sensitivity to social and behavioral determinants of health, and data-driven precision medicine all on the horizon. EHRs have succeeded in making many aspects of care safer and more reliable. Unfortunately, current limitations in EHR usability and problems with clinician burnout distract from these successes. A complex interplay of technology, policy, and healthcare delivery has contributed to our current frustrations with EHRs. Fortunately, there are opportunities to improve the EHR and health system. A stronger emphasis on improving the clinician’s experience through close collaboration by informaticians, clinicians, and vendors can combine with specific policy changes to address the causes of burnout.
Target audience
This tutorial is intended for clinicians, informaticians, policymakers, and regulators, who are essential participants in discussions focused on improving clinician burnout. Learners in biomedicine, regardless of clinical discipline, also may benefit from this primer and review.
Scope
We include (1) an overview of medical documentation from a historical perspective; (2) a summary of the forces converging over the past 20 years to develop and disseminate the modern EHR; and (3) future opportunities to improve EHR structure, function, user base, and time required to collect and extract information.
Keywords: electronic health records, health policy, history of medicine, population health, burnout, professional
INTRODUCTION
By every measure, the transition away from paper-based records is completed. Greater than 95% of acute care and 85% of outpatient practices use a basic or certified electronic health record (EHR).1,2 The transition was fueled by concern about variable healthcare quality in the United States and computer technology’s potential to stave off an epidemic of medical errors, which drove decades of work by world-renowned informaticians and led to federal incentives to encourage adoption and meaningful use. In the period following the creation of the Meaningful Use criteria,3 EHR use accelerated at a remarkable pace; office-based physician adoption of EHRs rose from 18% in 2001 to 85.9% in 2017. As a result, patients have better access to their providers and their data through secure messaging and patient portal access.4 Physician satisfaction with current HER technology is favorable in scattered practices. A recent study from Williams et al5 found generally positive overall satisfaction, with perceived efficiency gains most associated with EHR satisfaction.
Unfortunately, this transition has been negatively associated with clinician wellness, standing in stark contrast to the anticipated positive effects of electronic medical records.6–8 Much of what we experience today is the result of the rapid adoption by physicians unfamiliar with this technology before its adoption was incentivized. For a time, this obscured any appetite for future innovation, although hints of the changes that may lie ahead are now becoming apparent.
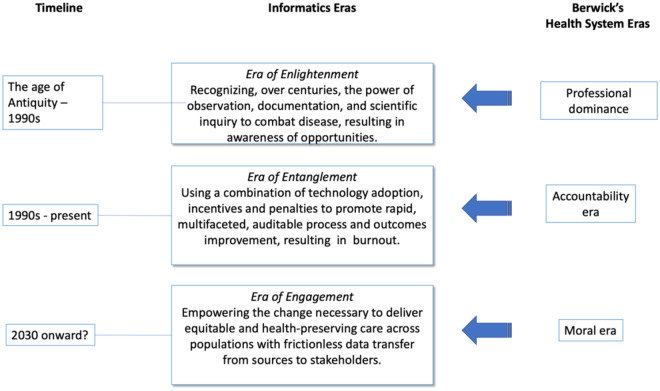
Don Berwick has organized the past, present, and future of health care into 3 eras: an era of professional dominance, an era of accountability and market theory, and a moral era in which there is greater transparency, civility, and the rejection of greed.9 As summarized in Figure 1, the state of EHR development follows a similar course to that of health care in Berwick’s eras, with the recent imposition of technology onto clinical workflows affecting physicians, nurses, pharmacists, and others, for whom clinical data entry expends effort with what appears to them to be little impact on clinical care. By situating the current moment within 3 eras covering centuries of medical information management and changing dimensions of disease and dis-ease, we draw attention to the dynamism of our current state and the criteria for meaningful reform.
Figure 1.
Timeline for electronic health record development and documentation, aligned with Berwick’s health system eras.9
THE ERA OF ENLIGHTENMENT
The modern EHR—including its form, content, and application to myriad research questions—draws on a variety of important historical antecedents. Medical documentation played a pivotal role in our current understanding of health and disease, evolving from a primarily educational tool to a document essential to patient care and clinical research. These possibilities developed first in Antiquity, with the transition from oral to written medical education traditions. For Hippocrates (ca. 460-370 BCE) and his disciples, reporting on individual patients promoted knowledge of diseases and their natural history. This kind of knowledge became an important part of Hippocratic practitioners’ claims to authority over the diverse array of barbers and surgeons patients encountered in the marketplace, where medicine was often practiced in public view.10 Centuries later, Galen (130-210 CE) extolled the virtue of closely studying masters and their books, linking knowledge of their texts to the competency of healers.11
The growth of the university heralded the expansion and formalization of documentation on patients. By the late medieval period, medical consilia emerged as a more standardized way of documenting individual consultations on patients.12 The typical consilium was a brief case report, consisting of some statement about the patient, perhaps including their name, sex, age, occupation, or residence, before the author described the patient’s diagnosis. Treatments were commonly offered, including recipes for therapies. Consilia became an important part of curricula at universities, as when Michele Savonarola (ca. 1385-1466) emphasized their use in mastering the practice of medicine.13 For Savonarola and his contemporaries, consilia made knowledge practical by adding detail to the traditionally theoretical curriculum emphasizing the works of authorities like Hippocrates, Aristotle (383-323 BCE), Galen, Al-Rhazes (854-932 CE), and others.
By the 18th and 19th centuries, the growth of hospitals ushered in an era of systematized patient data review, fully endorsed by medical professionals. Hospitals delivered more comprehensive care, allowing a new epidemiological perspective on disease.14 New forms of notetaking about—and thus thinking about—patients flourished. Autopsy records adhered to a standardized form, allowing seminal work by luminaries such as Xavier Bichat (1771-1802) to establish linkages between the effects of therapies on patients. Although still grounded in handwritten hospital admission registers and postmortem diagnoses, the perspective of physicians now telescoped from macroscopic to microscopic, and from hospital epidemiology to individual patient stories and course. Documentation led to new kinds of questions about health and disease.
By the 20th century, complexity became a defining characteristic of medical records, eventually outstripping the ability of traditional paper charts to meet the demands of day-to-day clinical work, let alone the needs of clinical researchers. For much of the early to mid-20th century, patients’ charts filled increasingly with consultants’ notes, diagnostic reports, and various forms, all usually organized by the document’s source or type. Toward the latter third of the 20th century, Lawrence Weed recognized the difficulty of understanding the patient’s story with the current source-based approach and recommended a move toward a problem-oriented medical record.15 Weed viewed a problem-based organization of the patient’s chart as instrumental to producing clearer thinking about the patient’s diagnoses and care. In his view, this reorganization was, in turn, better suited to computerizing the patient’s record.
Early electronic systems appeared in the 1960s. These systems showed promise, but unlike the transition from oral to written records, the shift from written to digital documentation created an easily extensible platform for data collection through forms, required text fields, and interrupting workflow to ensure data were accurate and complete. A diverse cast of stakeholders saw this potential, with professional societies including the American Medical Association, the American Association of Medical Record Librarians, and the Institute of Medicine contributing important criticisms and recommendations. Home-grown systems, developed primarily by physician engineers, carefully integrated some of these recommendations, with attention to their impact on physicians and nurses. Large hospital systems such as the Veterans Health Administration garnered praise for bringing electronic records into wide (mostly inpatient) clinical use.
The rationale for present-day EHRs was coming into focus. Companies including TDS, Epic, and Cerner successfully created commercial versions of these systems.16 As summarized in the Institute of Medicine report The Computer-Based Patient Record: An Essential Technology for Health Care (CPR Report),17 paper records suffered from problems with legibility, record loss, missing data, and volatility. Physicians, pharmacists, researchers, and nurses were among those often overlooking valuable clinical data because of the paper chart’s organization. The report stressed that a focus on data sources rather than patients (eg, physicians, nurses, monitors) limited the usefulness of the chart as a tool of clinical decision-making and research. As Morris Collen noted, there was now an emerging need, not for a computerized medical record but rather for computer-based patient records capable of supporting individual care while adding sequentially to the knowledge base for population health management.18 For Collen, the shift to this kind of system held enough promise for modern health care as to render its technology essential. The Institute’s subsequent research also summarized primary and secondary uses of the EHR (shown in Table 1), capturing the enormous potential for use beyond clinical care that an electronic system had in comparison with a written record.
Table 1.
Primary and secondary uses of an electronic health record system
| Primary uses | Secondary uses |
|---|---|
| ● Patient care delivery | ● Education |
| ● Patient care management | ● Regulation |
| ● Patient care support processes | ● Research |
| ● Financial and administrative | ● Public health and homeland security |
| ● Processes | ● Policy support |
| ● Patient self-management |
Adapted, with permission, from the Institute of Medicine Committee on Data Standards for Patient Safety.19
By the close of the 20th century, the first hints of a cost to frontline clinicians resulting from the shift toward electronic records was beginning to show. Limited computational power at that time basically prioritized critical clinical functions over a “simple-to-use, or a nearly intuitive, human interface.”20 As computational power increased, the focus stayed on technical and clinical quality and safety dimensions, rather than more seriously addressing challenges related to usability and workflow integration. This focus assumed that the time demands and additional stresses on physicians were offset by benefits, but as Ted Hughes noted, “Nothing is free.”21
Where clinicians originally designed their written records during Berwick’s era of professional dominance, EHRs were designed by committee, and were not constrained by the limitations of paper. Even when records were historically put to other uses—as was the case in Bichat’s morbid pathology—the impact on clinicians was minimal, especially compared with the shift toward data entry that the EHR imposed.22
The result decoupled the process of clinical record keeping from patient care. Combined with a shift toward lengthier documentation attributable to requirements in billing23 and defensive documentation due to legal concerns,24 updating patient charts began to feel irrelevant to clinical needs, which was “off-putting” to physicians.
Notably, despite the preponderance of encouraging EHR research, at least 1 meta-analysis challenged the notion of EHRs being ready for widespread dissemination by recognizing that the most compelling literature supporting EHR adoption came from a small number of benchmark institutions with homegrown EHRs, with little evidence available on the effect of commercially developed systems.25 The reluctance of physicians at the University of Virginia to comply initially with an institutional decision to adopt an inpatient EHR provided a glimpse into what was to come.26
THE ERA OF ENTANGLEMENT
Two other forcing functions led to present-day concerns. First, several reports from the Institute of Medicine provided EHR-enhancing recommendations. To Err is Human noted, “As health care and the system that delivers it become more complex, the opportunities for errors abound. We must systematically design safety into processes of care.”27Crossing the Quality Chasm proclaimed the central role of the EHR as the effector arm of quality initiatives by stating that “We must foster disseminating and applying knowledge to practice, the use of information technology in clinical care, and payment policies that reward performance.”28 The authors of Patient Safety, Achieving a New Standard for Care similarly stressed that “We describe a vision of patient safety systems integrated with clinical information systems and recommend strategies to create data standards that support that vision.”29 Finally, in Preventing Medication Errors, safety again figured prominently: “We must create a climate and infrastructure to continuously learn about and improve the safety of the medication-use process.”30 The authors of these reports, which included biomedical informatics experts, all sought to improve health care by collecting and using data to guide decision making and quality improvement.
Second, these federal government recommendations catalyzed the formation of the Office of the National Coordinator for Health Information Technology (ONC) and, later, the American Recovery and Reinvestment Act/Health Information Technology for Economic and Clinical Health Act of 2009. Additional policies and regulations relied on EHR functionality to create physician accountability for services delivered and for quality of care. These polices included the creation of Evaluation and Management coding guidelines in 1995, the Physician Quality Reporting System in 2006, and the Primary Care Incentive Program in 2011. Later, the Merit-based Incentive Payment System and the Medicare Access and CHIP Reauthorization Act added additional documentation requirements that annealed themselves to EHR-centric physician and nursing workflow.31 The effects have been startling; recent data show a 3- to 5-fold increase in U.S. progress note length as compared with other countries.23 Considerable administrative costs are now devoted to billing and insurance-related activities.32 Data also suggest that two-thirds of physician office time is spent on EHR work,33,34 quantifying clinical workforce effort in response to these new mandates. As EHR technology became widespread and computational power increased, biomedical informatics researchers could demonstrate the power of EHR data and realize the secondary uses such as education,35 research,36–38 and public health39 outlined in Table 1. The birth of data science as a discipline and the resurgence of artificial intelligence in medicine also depended on EHR technology.
Meaningful use of the EHR was double-edged sword—incentivizing the rapid adoption of EHR technology1 while also creating, through EHR certification mandates, an environment in which newly required features were entangled into an already complex and highly-regulated industry.23,40 Pressure to conform to new requirements and implementation timelines forced many successful homegrown EHRs to be replaced with commercial EHR products.41 The well-described phenomenon of cut and paste and “note bloat” that began in this century23 originated with the concern that visit summaries submitted to payers and regulators needed to include all byproducts of care completed and documented by other providers.
A careful inspection of the minor points in the same Institute of Medicine books that recommended EHRs reveals some insight into this conundrum. For example, the To Err is Human report notes that safety was compromised by an over-reliance on technology. Likewise, Crossing the Quality Chasm addressed many challenges to the quality framework but briefly acknowledged the quality risks associated with EHR. Other literature of the time, including Koppel’s seminal article about errors caused by EHR technology,42 foretold a less optimistic possible outcome. As EHRs became more widespread, clinicians often circumvented their limitations to deliver quality care.43,44
Likely causes of the challenges with today’s EHR can readily be mapped to the characteristics of the time according to Berwick, with its emphasis on measurement of quality metrics, incentives to improve quality, doubt about the truth of claims, and scrutiny about the content of the visit. Programs like Meaningful Use and their reliance on measurement and incentives have been described previously. Doubt and scrutiny were typically manifest by payers. Vogel and Goldberg remind us that the False Claims Act (a Civil War–era Act incentivizing the reporting of undelivered claims) was available to penalize practices committing healthcare fraud.45,46 The desire to implement quality improvement led to additional scrutiny, manifest as checkboxes in EHR forms to denote what was or was not done. For example, as pay-for-performance programs emerged, documentation about performance of screening tests became important. For example, a woman seen in primary care might be a candidate for a screening mammogram. This test might not be ordered for many reasons, some of which are substandard care, others of which are due to some contraindication (eg, having had a bilateral mastectomy). In response to the variability, EHR forms began including metadata checkboxes to help physicians document the rationale for the decision not to screen, which pop up when a mammogram is not ordered as indicated. As Robert Wachter noted, these “clicks” have accumulated and lengthened the time to complete many common tasks.47
A third area of entanglement includes what Atul Gawande called “revenge of the ancillaries.”48 The local implementation of an EHR required design sessions with local stakeholders. When physicians were unable to attend these meetings, the meetings continued in their absence, and often exacerbated the “click” burden by shifting some of regulatory requirements imposed on the laboratory, the radiology suite, and even the registration and scheduling system, back to the ordering provider.48
These numerous causes resulted in widespread misalignment of the technology and the typical clinical workflow. Our path forward begins with untangling the myriad roles being played by physicians, patients, and data in our healthcare system.
THE ERA OF ENGAGEMENT
Berwick noted changes that will be necessary to shape a future era driven by morality in health care. We can draw from his framework actions that we believe will chart a path forward.
Listen. Really Listen, while protecting civility. In these 2 actions, we recognize the need for a trusted partnership, with awareness of the rights, wishes, and concerns of all involved. As noted previously, the evolution from the Eras of Enlightenment to Entanglement involved various stakeholders who responded to regulation and legislation by impacting EHR design and implementation choices. The temptation might be to gravitate toward a technological solution—especially because technology historically carries a special allure for people inside and outside the informatics specialty—but as Wachter noted, our focus must remain on reforming precisely those problems that gave rise to clinician burnout.47 Communication by groups such as American Medical Informatics Association and the Blue Ridge Academic Health Group49 will lead to further understanding by all stakeholders of the role that informaticians, policymakers, and clinical care teams must play in aligning needs with workable solutions. Engagement, including a renewed interest in understanding clinicians’ experience using the modern EHR, will be critical to successfully introducing well-designed clinical information management technology. This partnership should look forward, while reflecting on the work leading up to the CPR Report, when authors noted the importance of creating a computer-based record, rather than electronic version of our paper-based chart, out of concerns for a future very much like the one in which we now live.
Stop excessive measurements. Fundamentally, the challenge with both excessive measuring and any focus on finance is related to the “what,” “who,” and “when” of these tasks. Already, ONC is addressing the “what” of measurement through discussions about balancing metadata elements with the needs of users generating those data.50
In terms of the “who” and “when,” technical innovations may automate some manual documentation requirements. Experiments by Johnson have demonstrated how EHR audit logs can be used to code visit activities.51 Finally, thoughtful shifting of some documentation activities to patients could alleviate the burden placed on the primary care giver in areas such as family history,52 social and behavioral determinants,53 and patient-reported outcomes measures.54
Decrease focus on finance. Decreasing the focus on finance is perhaps better stated as increasing the focus on patient well-being through actions that promote interoperability, as ONC is now doing.50 The 21st Century Cures Act stands out as an example of where policy appears to contribute positively, as it includes provisions that catalyze change in our digital landscape, including the challenges of information access imposed by a global, mobile society.55 This legislation is leading to more aggressive strategies to improve data interoperability through data models and application programming interfaces while simultaneously requiring that patients be given electronic access to EHR-based information.55–58
Abandon complex incentives. Many incentive models are complex because they aim to measure and change a behavior that is often counter to what is intrinsically of value to clinicians. Our attempts to engineer the execution of these incentives have failed to demonstrate improvement and have generated more ill will from physicians.
Avoid professional prerogative at the expense of the whole. Because modern medicine relies heavily on team and multispecialty-based care, the design and implementation of EHRs must attend to the capabilities and shortcomings of all team members, and not solely the needs of one group. Perhaps there are activities that can be safely shifted away from physicians with safeguards in place within the EHR, in favor of other work that should only be executed and documented by physicians.
Recommit to improvement science. A thorough commitment to improvement science—learning from data, applying what we learn, and learning from what we do—should permeate the way we think and talk about systems that impact clinical care.
The notion of the learning health system, made visible through Institute of Medicine in 2011,59 is becoming appreciated as a fulcrum for health system change.60,61 We also are beginning to appreciate how data science and informatics can personalize care and prediction using social, environmental, and behavioral health characteristics.62
The National Academy of Medicine had envisioned a role for the EHR in improving public health. In fact, public health (surveillance and detection) and population health (overall improvement of health status for a population over time) have become increasingly important in the era of obesity, child trafficking, and COVID-19.63–65 All of these activities require the use of the EHR and a commitment to iterative improvement in health care which are enabled through data analysis, alerts and reminders to improve compliance with new recommendations, and data collection to assess whether and how these proposed changes in the way we practice improve patient outcomes.
Improvement science must include a re-recruitment of clinical informatics experts into the academic settings. One area of collateral damage in the wake of the Era of Entanglement was the exodus of clinical informatics researchers who did not believe they could engage in EHR development, or who did not perceive their findings would result in change. There is increasing evidence that this concern has not been realized. It will be critical to reestablish this partnership66 so that they can refocus their efforts on improving the EHR itself. As we move forward with precision medicine, we face the conundrum of who should be responsible for entering and managing social and behavioral data that can impact decision making. While we recognize the value of including computable social and behavior determinants of health data in the EHR,67 the addition of this documentation burden to an already overburdened workforce could be overwhelming. Rather, this should be an opportunity for clinical informatics experts to develop innovative strategies to either support patient-reported social and behavioral determinants or to improve the integration of interdisciplinary team member’s work into the EHR.
Embrace transparency. Concomitant with streamlining mandated measures is rethinking the notion of privacy. The Health Insurance Portability and Accountability Act (HIPAA) stands out as a major obstacle to supporting learning health systems.68 Originally developed in response to the CPR Report, HIPAA has impinged on the ability of researchers to conduct legitimate health research. HIPAA’s implementation began prior to the widespread use of the Internet and the availability of global datasets and is now in need of significant reform.69 A regulatory reset of the balance point assuring “frictionless” access to healthcare data—especially around data liquidity and privacy—will inextricably impact the future of the EHR and the world.70 Contention between what we can learn from data vs who has the right to disclose it will likely be characterized by struggles to achieve increasingly sophisticated methods of disclosure and reuse, which will, in turn, lead to reengineering how we collect, store, retrieve, and reuse clinical data to avoid further burden on physicians. Perhaps the cleanest approach to liquidity will allow Americans to choose as a matter of explicit federal policy to opt out of HIPAA (eg, allowing people to share personal health data with everyone). In the meantime, prioritization of datasets that may (or may not) promote excellent outcomes in patient care should be considered. Datasets for public health, climate and health, employment and health, domestic security, food availability, and shelter need to be developed and made available within the EHR (perhaps using Web services such as FHIR [Fast Healthcare Interoperability Resources]) but not added to the clinician’s direct responsibility except where evidence warrants inclusion. If financing for health care shifts to universal access, documentation related to managing the system, such as the number of elements addressed during a review of systems, needs to be removed from the clinician’s workload.
Herbert Simon noted that a growth in information creates a scarcity of attention.71 There are some computer-based systems that are exploring how to combine external and EHR data, to minimize redundant data collection.72–74 The engagement of active clinicians with informaticians and other data scientists should make this next chapter for EHRs both more successful and more enjoyable for all who use them.
Reject greed. The healthcare system has become highly engineered to maximize time clinicians practice at the top of their license.48 Role-based workflows are engrained in many EHR systems, where each role within the care delivery team sees entirely different screens, coupled with opacity between workflows. While this activity ensures compliance, Gawande and others have observed that it comes at the expense of “taking one for the team.”48 We have yet to see a publication describing the contribution of this engineering to burnout but would submit that as the other aspects of engagement are executed, we do so with attention to where pleasure is found in the course of daily health care. Perhaps it is what makes each provider a unique human being that needs to be balanced against the risk of lower reimbursement or less efficiency. Eric Topol has pointed out that advances in artificial intelligence (AI) will provide our healthcare system with a choice: to use AI-enabled care to increase revenue per hour or to use AI-enabled care to give time and capacity back to clinicians to provide more thorough and thoughtful patient care.75
CONCLUSION
Like the consilia of the late medieval era or the autopsy reports of Bichat’s fledgling morbid pathology, the EHR is as promising a tool as it is dynamic. Against the backdrop of centuries of efforts at refining (if not reinventing) the medical record, the fundamental newness of the EHR is even more apparent, its successes and limitations all the more stark when considered against a long history of concerns in documenting patients’ health and disease that are distinct to our own. The current limitations of the electronic record distract from the way it has succeeded in expanding the boundaries of clinical care and research, making many aspects of care safer and more reliable. History is not always a perfect guide to the future, but it does suggest the possibility for growth and adaptation of electronic systems in areas such as clinical decision support, interoperability, and usability. Perhaps the only constant in the history of medical records is their dynamism—in time, the frustration at clinical alerts or mandated points of data entry will give way to new successes and challenges. Just as the limitations of paper records once motivated the adoption of electronic systems, today’s imposition of data entry onto clinicians has given discussions about the limitations of our EHRs a deep urgency. With new policy prescriptions and the careful collaboration of informaticians and clinicians, we see the Era of Engagement as holding the potential to remove much of that burden from clinical workflows, returning clinicians to the bedside without dissolving the positive qualities of the EHR.
AUTHOR CONTRIBUTIONS
KBJ provided the initial conception and design of the manuscript, collaborated on the drafting and revising of the manuscript, and provided final approval of this submitted version to be published. MJN provided substantial contributions to the entire manuscript, primarily drafted the history of medical documentation section, and collaborated on the drafting and revising of the manuscript. He provided final approval of this submitted version. DED provided the initial conception and design of the manuscript, collaborated on the drafting and revising of the manuscript, and provided final approval of this submitted version to be published. All authors agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
CONFLICT OF INTEREST STATEMENT
The authors have no competing interests to declare.
REFERENCES
- 1. Myrick K, Ogburn D, Ward B. National Electronic Health Records Survey, 2017. Hyattsville, MD: National Center for Health Statistics; 2019.
- 2. Adler-Milstein J, Holmgren AJ, Kralovec P, Worzala C, Searcy T, Patel V.. Electronic health record adoption in US hospitals: the emergence of a digital “advanced use” divide. J Am Med Inform Assoc 2017; 24 (6): 1142–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Blumenthal D, Tavenner M.. The “meaningful use” regulation for electronic health records. N Engl J Med 2010; 363 (6): 501–4. [DOI] [PubMed] [Google Scholar]
- 4. Goldzweig CL, Orshansky G, Paige NM, et al. Electronic patient portals: evidence on health outcomes, satisfaction, efficiency, and attitudes: a systematic review. Ann Intern Med 2013; 159 (10): 677–87. [DOI] [PubMed] [Google Scholar]
- 5. Williams DC, Warren RW, Ebeling M, Andrews AL, Teufel Ii RJ.. Physician use of electronic health records: survey study assessing factors associated with provider reported satisfaction and perceived patient impact. JMIR Med Inform 2019; 7 (2): e10949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Kroth PJ, Morioka-Douglas N, Veres S, et al. The electronic elephant in the room: physicians and the electronic health record. JAMIA Open 2018; 1 (1): 49–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Marmor RA, Clay B, Millen M, Savides TJ, Longhurst CA.. The impact of physician EHR usage on patient satisfaction. Appl Clin Inform 2018; 9 (1): 11–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Del Carmen MG, Herman J, Rao S, et al. Trends and factors associated with physician burnout at a multispecialty academic faculty practice organization. JAMA Netw Open 2019; 2 (3): e190554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Berwick DM. Era 3 for medicine and health care. JAMA 2016; 315 (13): 1329–30. [DOI] [PubMed] [Google Scholar]
- 10. Temkin O. Hippocrates in a World of Pagans and Christians. Baltimore, MD: Johns Hopkins University Press; 1991. [Google Scholar]
- 11. Horstmanshoff HFJ. Hippocrates and Medical Education: Selected Papers Read at the XIIth International Hippocrates Colloquium Universiteit Leiden, 24–26 August 2005. Leiden, the Netherlands–Boston, MA: Brill; 2010. [Google Scholar]
- 12. Agrimi J, Crisciani C.. Les “consilia” médicaux [Caroline Viola, trans.]. In: Typologie des sources duMoyen Age Occidental. Vol. 69. Turnhout, Belgium: Brepols; 1994. [Google Scholar]
- 13. Jacquart D. Theory, everyday practice, and three fifteenth-century physicians. Osiris 1990; 6: 140–60. [DOI] [PubMed] [Google Scholar]
- 14. Maulitz RC. Morbid Appearances: The Anatomy of Pathology in the Early Nineteenth Century. New York, NY: Cambridge University Press; 1987. [Google Scholar]
- 15. Weed LL. Medical Records, Medical Education, and Patient Care: The Problem-Oriented Record as a Basic Tool. Cleveland, OH: Press of Case Western Reserve University; 1969. [Google Scholar]
- 16. Brown SH, Lincoln MJ, Groen PJ, Kolodner RM.. VistA–U.S. Department of Veterans Affairs national-scale HIS. Int J Med Inform 2003; 69 (2–3): 135–56. [DOI] [PubMed] [Google Scholar]
- 17. Detmer DE, Steen EB.. The computer-based record: patient moving from concept toward reality. Int J Biomed Comput 1996; 42 (1–2): 9–19. [DOI] [PubMed] [Google Scholar]
- 18. Davis LS, Collen MF, Rubin L, Van Brunt EE.. Computer-stored medical record. Comput Biomed Res 1968; 1 (5): 452–69. [DOI] [PubMed] [Google Scholar]
- 19.Institute of Medicine Committee on Data Standards for Patient Safety. Key Capabilities of an Electronic Health Record System: Letter Report. Washington, DC: National Academy Press; 2003. [PubMed] [Google Scholar]
- 20. Dick RS, Steen EB, Detmer DE, eds. Institute of Medicine Committee on Improving the Patient Record. The Computer-Based Patient Record: An Essential Technology for Health Care, rev. ed. Washington, DC: National Academy Press; 1997. [PubMed] [Google Scholar]
- 21. Hughes Ted. Tiger'sbones, and other plays for children. Illustrated by AlanE. Cober. New York: Viking Press; 1974. [Google Scholar]
- 22. Nancarrow SA, Borthwick AM.. Dynamic professional boundaries in the healthcare workforce. Sociol Health Illness 2005; 27 (7): 897–919. [DOI] [PubMed] [Google Scholar]
- 23. Downing NL, Bates DW, Longhurst CA.. Physician burnout in the electronic health record era: are we ignoring the real cause? Ann Intern Med 2018; 169 (1): 50–1. [DOI] [PubMed] [Google Scholar]
- 24. Teichman PG. Documentation tips for reducing malpractice risk. Fam Pract Manag 2000; 7 (3): 29–33. [PubMed] [Google Scholar]
- 25. Chaudhry B, Wang J, Wu S, et al. Systematic review: impact of health information technology on quality, efficiency, and costs of medical care. Ann Intern Med 2006; 144 (10): 742–52. [DOI] [PubMed] [Google Scholar]
- 26. Massaro TA. Introducing physician order entry at a major academic medical center: I. Impact on organizational culture and behavior. Acad Med 1993; 68 (1): 20–5. [DOI] [PubMed] [Google Scholar]
- 27. Kohn LT, Corrigan J, Donaldson MS.. To Err is Human: building a Safer Health System. Washington, DC: National Academy Press; 2000. [PubMed] [Google Scholar]
- 28.Institute of Medicine Committee on Quality of Health Care in America. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academy Press; 2001. [Google Scholar]
- 29. Aspden P, Corrigan JM, Wolcott J, Erickson SM, eds. Institute of Medicine Committee on Data Standards for Patient Safety. Patient Safety: Achieving a New Standard for Care. Washington, DC: National Academies Press; 2004. [PubMed] [Google Scholar]
- 30. Aspden P, Wolcott J, Bootman JL, Cronenwelt LR, eds. Institute of Medicine Committee on Identifying and Preventing Medication Errors. Preventing Medication Errors. Washington, DC: National Academies Press; 2007. [Google Scholar]
- 31. Gillen E, Berzin O, Vincent A, Johnston D.. Certified electronic health record technology under the quality payment program. RTI Press Policy Brief. Research Triangle Park, NC: RTI Press; 2010. [PubMed] [Google Scholar]
- 32. Tseng P, Kaplan RS, Richman BD, Shah MA, Schulman KA.. Administrative costs associated with physician billing and insurance-related activities at an academic health care system. JAMA 2018; 319 (7): 691–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Sinsky C, Colligan L, Li L, et al. Allocation of physician time in ambulatory practice: a time and motion study in 4 specialties. Ann Intern Med 2016; 165 (11): 753–60. [DOI] [PubMed] [Google Scholar]
- 34. Overhage JM, McCallie D Jr.. Physician time spent using the electronic health record during outpatient encounters: a descriptive study. Ann Intern Med 2020; 172 (3): 169–74. [DOI] [PubMed] [Google Scholar]
- 35. Spickard A, Ridinger H, Wrenn J, et al. Automatic scoring of medical students' clinical notes to monitor learning in the workplace. Med Teach 2014; 36 (1): 68–72. [DOI] [PubMed] [Google Scholar]
- 36. Hripcsak G, Duke JD, Shah NH, et al. Observational Health Data Sciences and Informatics (OHDSI): opportunities for observational researchers. Stud Health Technol Inform 2015; 216: 574–8. [PMC free article] [PubMed] [Google Scholar]
- 37. Friedlin J, Grannis S, Overhage JM.. Using natural language processing to improve accuracy of automated notifiable disease reporting. AMIA Annu Symp Proc 2008; 2008: 207–11. [PMC free article] [PubMed] [Google Scholar]
- 38. Pletcher MJ, Forrest CB, Carton TW.. PCORnet's collaborative research groups. Patient Relat Outcome Meas 2018; 9: 91–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Johnson KB, Unertl KM, Chen Q, et al. Health information exchange usage in emergency departments and clinics: the who, what, and why. J Am Med Inform Assoc 2011; 18 (5): 690–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Bowes WA 3rd. Progress and challenge in meeting meaningful use at an integrated delivery network. AMIA Annu Symp Proc 2011; 2011: 144–51. [PMC free article] [PubMed] [Google Scholar]
- 41. Johnson KB, Ehrenfeld JM.. An EPIC switch: preparing for an electronic health record transition at Vanderbilt University Medical Center. J Med Syst 2018; 42 (1): 6. [DOI] [PubMed] [Google Scholar]
- 42. Koppel R, Metlay JP, Cohen A, et al. Role of computerized physician order entry systems in facilitating medication errors. JAMA 2005; 293 (10): 1197–203. [DOI] [PubMed] [Google Scholar]
- 43. Unertl KM, Weinger MB, Johnson KB.. Applying direct observation to model workflow and assess adoption. AMIA Annu Symp Proc 2006; 2006: 794–8. [PMC free article] [PubMed] [Google Scholar]
- 44. Friedman A, Crosson JC, Howard J, et al. A typology of electronic health record workarounds in small-to-medium size primary care practices. J Am Med Inform Assoc 2014; 21 (e1): e78–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Vogel RL. The false claims act and its impact on medical practices. J Med Pract Manage 2010; 26 (1): 21–4. [PubMed] [Google Scholar]
- 46. Goldberg MK. Are you committing health care fraud under the False Claims Act? The answer may not be as simple as you think. J Med Pract Manage 2002; 17 (4): 206–9. [PubMed] [Google Scholar]
- 47. Wachter RM. The Digital Doctor: Hope, Hype, and Harm at the Dawn of Medicine's Computer Age. New York, NY: McGraw-Hill Education; 2017. [Google Scholar]
- 48. Gawande A. Why doctors hate their computers. The New Yorker. November 12, 2018. https://www.newyorker.com/magazine/2018/11/12/why-doctors-hate-their-computers. Accessed November 29, 2020. [Google Scholar]
- 49.The Blue Ridge Academic Health Group. The Hidden Epidemic: The Moral Imperative for Academic Health Centers to Address Health Professionals’ Well-Being. Winter 2017–2018, Report 22. http://whsc.emory.edu/blueridge/publications/archive/blue-ridge-winter2017-2018.pdf. Accessed November 29, 2020.
- 50. Zayas-Caban T, Chaney KJ, Rucker DW.. National health information technology priorities for research: a policy and development agenda. J Am Med Inform Assoc 2020; 27 (4): 652–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Tang LA, Johnson KB, Kumah-Crystal YA.. Breadcrumbs: assessing the feasibility of automating provider documentation using electronic health record activity. AMIA Annu Symp Proc 2018; 2018: 1008–17. [PMC free article] [PubMed] [Google Scholar]
- 52. Wu RR, Myers RA, McCarty CA, et al. Protocol for the “Implementation, adoption, and utility of family history in diverse care settings” study. Implement Sci 2015; 10: 163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Sorondo B, Allen A, Bayleran J, et al. Using a patient portal to transmit patient reported health information into the electronic record: workflow implications and user experience. eGEMs (Wash DC). 2016; 4 (3): 1237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Blum D, Raj SX, Oberholzer R, et al. ; EURO IMPACT, European Intersectorial Multidisciplinary Palliative Care Research Training. Computer-based clinical decision support systems and patient-reported outcomes: a systematic review. Patient 2015; 8 (5): 397–409. [DOI] [PubMed] [Google Scholar]
- 55. Hudson KL, Collins FS.. The 21st century cures act - a view from the NIH. N Engl J Med 2017; 376 (2): 111–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Holmes DR Jr., Hance R, Syrek Jensen TS, et al. The 21st century cures act and early feasibility studies for cardiovascular devices: what have we learned, where do we need to go? J Am Coll Cardiol Intv 2018; 11 (21): 2220–5. [DOI] [PubMed] [Google Scholar]
- 57. Gabay M. 21st Century Cures Act. Hosp Pharm 2017; 52 (4): 264–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. DesRoches CM, Leveille S, Bell SK, et al. The views and experiences of clinicians sharing medical record notes with patients. JAMA Netw Open 2020; 3 (3): e201753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Institute of Medicine Roundtable on Value & Science-Driven Health Care, Grossmann C, Powers B, McGinnis JM.. Digital Infrastructure for the Learning Health System: The Foundation for Continuous Improvement in Health and Health Care: workshop Series Summary. Washington, DC: National Academies Press; 2011. [PubMed] [Google Scholar]
- 60. Grossmann C, Sanders J, English RA, Institute of Medicine Roundtable on Value & Science-Driven Health Care.Large Simple Trials and Knowledge Generation in a Learning Health System: Workshop Summary. Washington, DC: The National Academies Press; 2013. [PubMed] [Google Scholar]
- 61. Myburgh J. Patient-centered outcomes and resuscitation fluids. N Engl J Med 2018; 378 (9): 862–3. [DOI] [PubMed] [Google Scholar]
- 62. Prather AA, Gottlieb LM, Giuse NB, et al. National academy of medicine social and behavioral measures: associations with self-reported health. Am J Prev Med 2017; 53 (4): 449–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Bonander J, Gates S.. Public health in an era of personal health records: opportunities for innovation and new partnerships. J Med Internet Res 2010; 12 (3): e33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Detmer DE. Activating a full architectural model: improving health through robust population health records. J Am Med Inform Assoc 2010; 17 (4): 367–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Todres J, Clayton EW.. Responding to the sexual exploitation of minors. N Engl J Med 2014; 370 (14): 1282–3. [DOI] [PubMed] [Google Scholar]
- 66. Johnson KB, Patel NR.. Biomedical informatics and health information technology: a critical, pragmatic collaboration for clinical transformation. J Gen Intern Med 2020. Apr 22 [E-pub ahead of print]. doi: 10.1007/s11606-020-05833-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Adler NE, Stead WW.. Patients in context–EHR capture of social and behavioral determinants of health. N Engl J Med 2015; 372 (8): 698–701. [DOI] [PubMed] [Google Scholar]
- 68. Price WN, Cohen IG.. Privacy in the age of medical big data. Nat Med 2019; 25 (1): 37–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Peddicord D, Waldo AB, Boutin M, et al. A proposal to protect privacy of health information while accelerating comparative effectiveness research. Health Aff (Millwood) 2010; 29 (11): 2082–90. [DOI] [PubMed] [Google Scholar]
- 70. Detmer DE. Your privacy or your health–will medical privacy legislation stop quality health care? Int J Qual Health Care 2000; 12 (1): 1–3. [DOI] [PubMed] [Google Scholar]
- 71. Herbert A. Simon Quotes. https://www.brainyquote.com/quotes/herbert_a_simon_181919. Accessed November 29, 2020.
- 72. Ainsworth J, Buchan I.. Combining health data uses to ignite health system learning. Methods Inf Med 2015; 54 (6): 479–87. [DOI] [PubMed] [Google Scholar]
- 73. Detmer DE. At last! A working model of a data ecosystem for continuous learning in the evolving health noosphere. Methods Inf Med 2015; 54 (6): 477–8. [DOI] [PubMed] [Google Scholar]
- 74. Hosseini M, Faiola A, Jones J, Vreeman DJ, Wu H, Dixon BE.. Impact of document consolidation on healthcare providers' perceived workload and information reconciliation tasks: a mixed methods study. J Am Med Inform Assoc 2019; 26 (2): 134–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Topol EJ. High-performance medicine: the convergence of human and artificial intelligence. Nat Med 2019; 25 (1): 44–56. [DOI] [PubMed] [Google Scholar]