Abstract
In 2017, 43.9% of US physicians reported symptoms of burnout. Poor electronic health record (EHR) usability and time-consuming data entry contribute to burnout. However, less is known about how modifiable dimensions of EHR use relate to burnout and how these associations vary by medical specialty. Using the KLAS Arch Collaborative’s large-scale nationwide physician (MD/DO) data, we used ordinal logistic regression to analyze associations between self-reported burnout and after-hours charting and organizational EHR support. We examined how these relationships differ by medical specialty, adjusting for confounders. Physicians reporting ≤ 5 hours weekly of after-hours charting were twice as likely to report lower burnout scores compared to those charting ≥6 hours (aOR: 2.43, 95% CI: 2.30, 2.57). Physicians who agree that their organization has done a great job with EHR implementation, training, and support (aOR: 2.14, 95% CI: 2.01, 2.28) were also twice as likely to report lower scores on the burnout survey question compared to those who disagree. Efforts to reduce after-hours charting and improve organizational EHR support could help address physician burnout.
Keywords: electronic medical record, health information technology, emotional exhaustion, Pajama time, usability, optimization
INTRODUCTION
Burnout, a syndrome of emotional exhaustion, depersonalization, and a low sense of personal accomplishment, is a common problem among US physicians.1 The prevalence of US physician burnout was 43.9% in 2017, which was higher than among other working adults.2–4 Physician burnout is recognized as a significant problem with associated morbidity and mortality, including poor clinical care, medical mistakes, physicians leaving medicine, and suicide.5,6 The US economic burden of turnover and reduced clinical hours attributable to physician burnout is estimated to be $4.6 billion each year.7
A national report quantified top contributors to burnout based on the frequency with which each answer choice was selected. Too many bureaucratic tasks (55%) and the increasing computerization of practice (30%) were among the top responses.5 Specifically, evidence suggests that poor electronic health record (EHR) usability, high volume of patient call messages, and time-consuming data entry contribute to professional dissatisfaction.8–11 The amount of time spent on EHRs doing nonclinical work and documentation outside regular clinic hours are also associated with physician burnout.12–16
Existing literature examining the associations between burnout and the EHR is limited to specific medical specialties or select healthcare organizations. The narrow scope of these studies limits their generalizability and precludes the possibility of examining the impact of individual organizations. The effect of EHRs on physicians could vary depending on how the EHR is implemented and supported within an organization, but there is little data to support this idea.
Using KLAS Arch Collaborative survey responses from 25 018 physicians (MD/DO) at 213 organizations throughout the United States, we aimed to quantify the extent to which EHR satisfaction factors, namely after-hours charting and organizational EHR support, are associated with self-reported burnout overall and by physician specialty. Better understanding these measures will allow healthcare organizations to more effectively focus efforts to mitigate physician burnout.
MATERIALS AND METHODS
KLAS, an independent health information technology firm, began the Arch Collaborative in 2017 to measure and establish a benchmark for the clinician EHR experience. KLAS partnered with health systems to pilot research surveys. Since then, more than 200 separate health organizations (comprised primarily of community health systems, large health systems, and academic health systems) have participated in the Arch Collaborative, and most areas of medical practice are represented. The Collaborative’s main data-collection instrument is a web-based survey that is available for public use. Additional benchmarking data are available to organizations with a paid subscription to the Arch Collaborative. The core survey contains 35 questions.17 Participating organizations can make minor edits for clarity, add additional questions, or exclude irrelevant or sensitive questions. The survey is distributed to clinicians by healthcare organization leadership. The Arch Collaborative collects and analyzes the data and generates a report that includes national benchmarking. The database includes responses from over 46 000 physicians. A single-question burnout measure was added to the survey in 2018, and more than 25 000 burnout responses from over 200 healthcare organizations have been collected through June 2020.
Measures
The dependent variable of this study is represented by the single-question taken from the AMA mini-Z measurement for burnout.18 “Using your own definition of burnout, select 1 of the answers below: 1. I enjoy my work. I have no symptoms of burnout. 2. I am under stress and don’t always have as much energy as I did, but I don’t feel burned out. 3. I am definitely burning out and have 1 or more symptoms of burnout (eg, emotional exhaustion). 4. The symptoms of burnout that I am experiencing won’t go away. I think about work frustrations a lot. 5. I feel completely burned out. I am at the point where I may need to seek help.” Similar self-reported single questions have been validated and used in studies as a representation of burnout, though this single measure likely underrepresents burnout.19–21 We combined responses from options 3, 4, and 5 to calculate the percentage of physicians burned out for each specialty.
The focus of the Arch survey is to measure the EHR end-user experience. Accordingly, several questions are used to measure aspects of the EHR experience. Preliminary analyses indicated that 1 of our main independent variables, organizational EHR support, was among the survey measures most highly correlated with burnout. Other similar variables were excluded from our analysis due to collinearity. The Arch survey assesses the provider’s impression of organizational support of their use of the EHR with the prompt: “Our organization has done a great job of implementing, training on, and supporting the EHR.” The respondents could then answer on a 5-point Likert scale from strongly disagree to strongly agree. Consequently, rather than assessing each individual component, this question collectively assesses EHR implementation, training, and support.
Our other main independent variable is after-hours charting. Prior research has highlighted the effect that after-hours work has on burnout among much smaller populations than in the current study.13,15,16 The Arch Collaborative measures after-hours charting with the following question: “How many hours per week do you spend completing your charting outside of your normal business hours (evenings, weekends, after your shift, etc.)?” Respondents then selected banded answers under the following ranges: 0–5 hours, 6–15 hours, 16–25 hours, and 25+ hours. The likelihood of experiencing symptoms of burnout became more common with each increase in time spent on after-hours charting (see Table 1), with the largest jump occurring between 0–5 hours and 6–15 hours.
Table 1.
Demographic variables
| Demographic Variables | Organizations n = 213 | Organization % | Respondents n = 25 018 | Respondent % |
|---|---|---|---|---|
| Organization Type | — | — | — | — |
| Community Health System | 45 | 21.00% | 3267 | 13.00% |
| Large Health System | 44 | 20.60% | 7180 | 28.60% |
| Academic Health System | 40 | 18.70% | 8941 | 35.60% |
| Community Hospital | 29 | 13.60% | 695 | 2.80% |
| Midsize Health System | 22 | 10.30% | 2592 | 10.30% |
| Children’s Hospital | 17 | 7.90% | 1324 | 5.30% |
| Ambulatory Care Group | 19 | 8.90% | 1132 | 4.50% |
| Geographic Region | — | — | — | — |
| West | 100 | 47% | 4460 | 18% |
| Midwest | 94 | 44% | 7135 | 29% |
| Northeast | 88 | 41% | 6543 | 26% |
| South | 113 | 53% | 6880 | 28% |
| EHR Vendor b | — | — | — | — |
| Epic | 148 | 69.20% | 17 204 | 68.50% |
| Other | 81 | 37.90% | 1060 | 4.20% |
| Cerner | 43 | 20.10% | 3976 | 15.80% |
| MEDITECH | 32 | 15.00% | 525 | 2.10% |
| Allscripts | 23 | 10.70% | 1083 | 4.30% |
| eClinicalWorks | 22 | 10.30% | 1075 | 4.30% |
| NextGen Healthcare | 11 | 5.10% | 39 | 0.20% |
| Years Practicing Medicine | — | — | — | — |
| 0–4 years | — | — | 1343 | 5.30% |
| 5–14 years | — | — | 7789 | 31.00% |
| 15–24 years | — | — | 7196 | 28.60% |
| 25+ years | — | — | 8315 | 33.10% |
| Years Using the EHR | — | — | — | — |
| 1 year | — | — | 2274 | 9.00% |
| 2 years | — | — | 1818 | 7.20% |
| 3 years | — | — | 1861 | 7.40% |
| 4 years | — | — | 2284 | 9.10% |
| 5+ years | — | — | 13 012 | 51.80% |
| Self-Reported After-hours Charting | — | — | ||
| 0-5 hours | — | — | 20 912 | 57% |
| 6-15 hours | — | — | 12 829 | 35% |
| 16-25 hours | — | — | 2473 | 7% |
| 25+ hours | — | — | 752 | 2% |
| Organizational EHR Support c | — | — | ||
| Strongly Agree | — | — | 4038 | 9% |
| Agree | — | — | 15 586 | 35% |
| Indifferent | — | — | 11 134 | 25% |
| Disagree | — | — | 8511 | 19% |
| Strongly Disagree | — | — | 5359 | 12% |
| Self-Reported Burnout | — | — | ||
| Completely burned out | — | — | 340 | 1% |
| Symptoms of burnout won't go away | — | — | 1859 | 7% |
| Definitely burning out | — | — | 5417 | 22% |
| Under stress | — | — | 11 328 | 45% |
| No burnout | — | — | 6074 | 24% |
Healthcare organizations that have locations in more than 1 region are included multiple times in the geographic region counts.
Healthcare organizations that use more than 1 EHR vendor are included multiple times in the EHR vendor counts.
Agreement that organization has done a great job with EHR implementation, training, and support.
Confounding variables (see Table 1) were also taken from the Arch Collaborative survey, including healthcare organization, geographic region (taken from the longitude and latitude using the respondent’s IP address and converted into census regions), the EHR vendor used, years of practicing medicine, and years using the EHR (0–4 years and 5+ years). Physicians with missing responses for any of the included variables were excluded from the study.
Analyses
Ordinal logistic regression was used to analyze the association between burnout and after-hours charting and organizational EHR support. Individual burnout was measured on an ordinal scale from completely burned out to no burnout. Organizational EHR support was measured using the question: “Do you agree with the following statement? Our organization has done a great job of implementing, training on, and supporting the EHR.” Responses ranging from “strongly disagree” to “neither agree nor disagree” were coded as “disagree.” Responses ranging from “agree” to “strongly agree” were coded as “agree.” For after-hours charting, physicians were grouped by those who reported 0–5 hours of after-hours charting per week and those who reported 6+ hours of charting.
The final model included burnout on a 5-point Likert scale as the main outcome variable with the dichotomized variables for after-hours charting and organizational EHR support as the main explanatory variables, and controlling for organization using clustering, census region, EHR vendor, years practicing medicine, and years using the EHR. The physician specialty model replicated the original model but was limited to specialties with 300 or more respondents. Each specialty was mutually exclusive, meaning they were only able to select 1 self-identified specialty.
RESULTS
The demographic characteristics of the study population are presented in Table 1. Of the 25 018 respondents, 35.6% were from academic health systems, followed by 28.6% from large health systems (those with over 1500 beds). About 29% of respondents were in the Midwest and 28% in the South. Over 68% of respondents use Epic as their primary EHR vendor, followed by Cerner (15.8%). About 33% of participating physicians had been practicing medicine for 25+ years at the time of the survey. Almost 52% had been using the EHR for at least 5 years when surveyed.
Table 2 presents descriptive data for burnout, after-hours charting, and organizational EHR support. The level of burnout in our study ranged from 22% to 34% by specialty. The specialties with the highest levels of burnout in our study were family medicine (34%) and hematology/oncology (33%). The specialties with the lowest levels of burnout were psychiatry (22%) and anesthesiology (24%).
Table 2.
Physician burnout, after-hours charting, and organizational EHR support descriptive statistics
| Specialtya | Physician n | Organization n | % Of Physicians Burned Outc | % of Physicians with 6 or More Hours of Weekly After-hours Charting | Organizational EHR Supportb |
|---|---|---|---|---|---|
| All Organizations | 25 018 | 213 | 30% | 43% | 44% |
| Family Medicine | 3010 | 181 | 34% | 53% | 47% |
| Hematology/Oncology | 455 | 129 | 33% | 60% | 35% |
| Internal Medicine | 2164 | 170 | 32% | 53% | 47% |
| Neurology | 459 | 142 | 31% | 52% | 44% |
| Cardiology | 726 | 164 | 30% | 50% | 38% |
| Radiology | 349 | 128 | 29% | 12% | 35% |
| Gynecology and Obstetrics | 1126 | 166 | 29% | 41% | 43% |
| Pediatrics | 1684 | 176 | 28% | 43% | 50% |
| Pulmonology | 322 | 135 | 28% | 56% | 39% |
| Emergency Medicine | 1391 | 171 | 27% | 31% | 46% |
| General Surgery | 895 | 166 | 27% | 40% | 43% |
| Gastroenterology | 328 | 147 | 26% | 49% | 42% |
| Hospital Medicine | 973 | 141 | 25% | 34% | 54% |
| Orthopedics | 751 | 165 | 25% | 42% | 37% |
| Anesthesiology | 959 | 163 | 24% | 14% | 49% |
| Psychiatry | 465 | 148 | 22% | 37% | 47% |
Physician specialties with <300 respondents and physicians who did not indicate a specialty were included in the overall analysis but excluded from specialty analyses.
Percent that agree organization has done a great job with EHR implementation, training, and support.
Percent Burned Out is the percent who responded “I am definitely burning out and have 1 or more symptoms of burnout (eg, emotional exhaustion),” “The symptoms of burnout that I am experiencing won’t go away. I think about work frustrations a lot,” or “I feel completely burned out. I am at the point where I may need to seek help.”
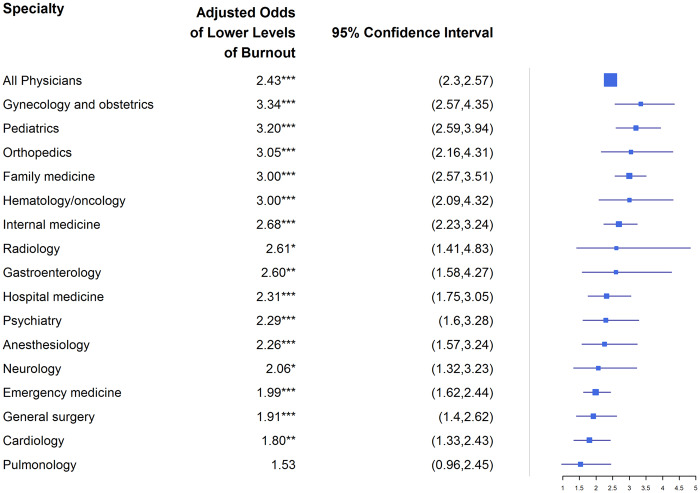
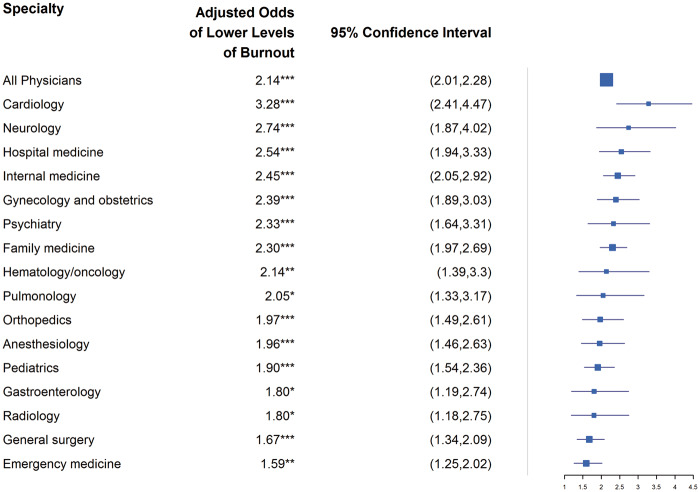
The associations between physician burnout and after-hours charting are presented in Figure 1. After adjusting for confounding variables, physicians with 5 or fewer hours of weekly after-hours charting (aOR: 2.43, 95% CI: 2.30, 2.57) were twice as likely to report lower levels of burnout than those with 6 or more hours. Figure 2 presents the associations between physician burnout and organizational EHR support. Those who agree that their organization has done a great job with EHR implementation, training, and support (aOR: 2.14, 95% CI: 2.01, 2.28) were also twice as likely to report lower levels of burnout than those who disagreed.
Figure 1.
Associations between 5 hours or fewer of weekly after-hours charting and lower levels of self-reported physician burnout.†*Significant at P < .05 **Significant at P < .001 ***Significant at P < .0001 † Self-reported burnout was measured using a 5-point scale from completely burned out to no burnout with a positive odds ratio indicating lower levels of burnout. Note: Physician specialties with <300 respondents and physicians who did not indicate a specialty were included in the overall analysis but excluded from specialty analyses.
Figure 2.
Associations between perceived organizational EHR support and lower levels of self-reported physician burnout.† *Significant at P < .05 **Significant at P < .001 ***Significant at P < .0001 † Self-reported burnout was measured using a 5-point scale from completely burned out to no burnout with a positive odds ratio indicating lower levels of burnout. Note: Physician specialties with <300 respondents and physicians who did not indicate a specialty were included in the overall analysis but excluded from specialty analyses.
Physicians with 5 or fewer hours of weekly after-hours charting were significantly more likely to report lower levels of burnout for most physician specialties, with the highest odds ratios for gynecology and obstetrics (aOR: 3.34, 95% CI: 2.57, 4.35) and pediatrics (aOR: 3.20, 95% CI: 2.59, 3.94). Physicians who agreed that their organization has done a great job with EHR implementation, training, and support were significantly more likely to report lower levels of burnout for all physician specialties, with the highest odds ratios for cardiology (aOR: 3.28, 95% CI: 2.41, 4.47) and neurology (aOR: 2.74, 95% CI: 1.87, 4.02).
DISCUSSION
In our study, after-hours charting was significantly associated with physician burnout. Physicians who reported spending 5 or fewer hours on weekly after-hours charting were significantly more likely to report lower levels of burnout overall and for most included specialties. Several other smaller-scale studies also found an association between after-hours charting and symptoms of burnout.13,15,16 However, the etiology of after-hours charting is multifactorial—clinical work volume and complexity, workflows, staffing, provider EHR mastery, the EHR build, and other factors can all contribute. EHR factors are not solely responsible for after-hours charting, and other efforts besides EHR improvements, such as team documentation and new approaches to care team models for clinical support,22,23 may reduce after-hours charting.
Satisfaction with organizational EHR support was significantly associated with lower levels of burnout overall and for all specialties included in our study, independent of the after-hours charting variable. While the organizational EHR support measurement has not been used in prior literature, previous studies have reported that organizational IT improvements can reduce burnout symptoms.24–27 Our findings suggest that EHR interventions focused on improving organizational EHR support could help reduce physician burnout regardless of the time physicians spend on after-hours charting.
Furthermore, variation in burnout by specialty in this study was notable. The specialties with the highest levels of burnout in our study were family medicine, hematology/oncology, internal medicine, pulmonology, neurology, and cardiology. A nationally representative study also reported that neurology and family medicine were among the specialties with the highest levels of burnout, in addition to urology, nephrology, and diabetes and endocrinology, which were not included in our analyses.5 The specialties with the lowest levels of burnout in our study were psychiatry, anesthesiology, orthopedics, hospital medicine, and gastroenterology. Similarly, a prior study reported that psychiatry, orthopedic, and gastroenterology specialists were among those physicians with the lowest levels of burnout.5 However, we found much lower levels of burnout compared to the prior study which was also on a national scale.5 The difference in the findings for the level of burnout could be related to differences in the burnout measurement and study design.19–21 The overall self-reported burnout in our study is similar to what was found in previous smaller-scale studies examining the relationship between after-hours charting and self-reported burnout.13,15
We acknowledge that there are limitations to this study. The response rate for some of the participating organizations is not known, which precludes reporting the overall response rate. Our sample methodology includes a risk of selection and nonresponse bias at both the organization and individual level of unknown direction and magnitude. We were also unable to control for sociodemographic variables such as sex, race, and age because they were not included in data collection. However, we used years practicing medicine as a proxy for age. In addition, while our data include physicians in all 50 states, they are a nonrandom sample and not nationally representative. Our sample disproportionately comes from health systems, with less representation of hospitals that remain independent of health systems.28 We have an oversampling of organizations using Epic. In our sample, 69% use the Epic EHR, while nationally, 29% of acute-care multispecialty hospitals use Epic.29 We also likely have an oversample of physicians from the northeast and midwest regions.30 We included these demographic variables as covariates to help account for these differences. Our study uses self-reported after-hours work which may reflect various inaccuracies, as opposed to objective measures of EHR use outside of scheduled hours. In addition, we collectively assessed EHR implementation, training, and support rather than assessing each individual component. Despite these limitations, this study provides new insights into factors associated with physician burnout and highlights areas for future research. The large sample of organizations and individual participants allowed us to analyze factors associated with burnout by specialty.
Using the Arch Collaborative database, we found that organizational EHR support and time spent on after-hours charting are independently associated with physician burnout. In addition, these associations and the level of burnout differed by physician specialty. Family medicine had the highest levels of burnout. Gynecology and obstetrics had the highest odds of not being burned out in association with 5 or fewer hours of after-hours charting. Cardiology had the highest odds of not being burned out in association with reporting adequate organizational EHR support. Organizational efforts to reduce after-hours charting and actively support physician mastery of the EHR could mitigate physician burnout. These findings, if verified by other research, may help healthcare organizations allocate and focus time and resources more effectively.
FUNDING
This research was supported in part by KLAS, a healthcare information technology research firm. The healthcare organizations who participated in this survey purchased an Arch Collaborative membership. The Arch Collaborative survey is available to the public domain. Arch Collaborative members subscribe to access benchmarked data and summarized content through KLAS. Funds from these memberships also helped sponsor this article.
AUTHOR CONTRIBUTIONS
Conceived study concept: CB, HCE, RC. Conceived study design: CD, JAM, JJ, LCM, RC. Contributed to data analysis and visualization: CD, CL, HCE, JJ. Wrote the manuscript: CB and LCM. All authors reviewed and edited manuscript. All authors approved the final manuscript.
ACKNOWLEDGMENTS
We would like to acknowledge Taylor Davis and Jenifer Gordon for the constructive feedback they provided throughout the analysis and writing processes.
AVAILABILITY OF DATA
The data underlying this article were provided by KLAS Research by permission. Data will be shared on request to the corresponding author with permission of KLAS Research.
CONFLICT OF INTEREST STATEMENT
KLAS works with most major healthcare IT vendors and consulting firms. Funds from these firms are used to conduct market research and to provide consulting engagements. These funds do not directly support the research presented in this article but are a major source of revenue for KLAS. In addition to these funds, HIT vendors can be members of the Arch Collaborative. Those that are paying members of the collaborative have received consulting engagements and data that are related to this research. Dr. Christopher Longhurst is an uncompensated KLAS advisory board member. Dr. Craig Joseph works for the consulting firm Nordic and formerly worked for the consulting company Avaap.
REFERENCES
- 1. Maslach C, Jackson S, Leiter M.. Maslach Burnout Inventory Manual. 3rd ed. Palo Alto, CA: Consulting Psychologists Press; 1996. [Google Scholar]
- 2. Shanafelt TD, Boone S, Tan L, et al. Burnout and satisfaction with work-life balance among US physicians relative to the general US Population. Arch Intern Med 2012; 172 (18): 1377–85. [DOI] [PubMed] [Google Scholar]
- 3. Shanafelt TD, West CP, Sinsky C, et al. Changes in burnout and satisfaction with work-life integration in physicians and the general US working population between 2011 and 2017. Mayo Clin Proc 2019; 94 (9): 1681–94. [DOI] [PubMed] [Google Scholar]
- 4.Medscape National Physician Burnout, Depression & Suicide Report 2019. Medscape. //www.medscape.com/slideshow/2019-lifestyle-burnout-depression-6011056 Accessed October 2, 2020.
- 5.Medscape National Physician Burnout & Suicide Report 2020: The Generational Divide. Medscape. 2020. www.medscape.com/slideshow/2020-lifestyle-burnout-6012460 Accessed May 21, 2020.
- 6. Stehman CR, Testo Z, Gershaw RS, Kellogg AR.. Burnout, drop out, suicide: physician loss in emergency medicine, part I. West J Emerg Med 2019; 20 (3): 485–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Han S, Shanafelt TD, Sinsky CA, et al. Estimating the attributable cost of physician burnout in the United States. Ann Intern Med 2019; 170 (11): 784–90. [DOI] [PubMed] [Google Scholar]
- 8. Friedberg MW, Chen PG, Van Busum KR, et al. Factors affecting physician professional satisfaction and their implications for patient care, health systems, and health policy. Rand Health Q 2014; 3 (4): 1. [PMC free article] [PubMed] [Google Scholar]
- 9. Hilliard RW, Haskell J, Gardner RL.. Are specific elements of electronic health record use associated with clinician burnout more than others? J Am Med Inform Assoc 2020; 27 (9): 1401–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Longhurst CA, Davis T, Maneker A, et al. ; Arch Collaborative. Local investment in training drives electronic health record user satisfaction. Appl Clin Inform 2019; 10 (2): 331–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Downing NL, Bates DW, Longhurst CA.. Physician burnout in the electronic health record era: are we ignoring the real cause? Ann Intern Med 2018; 169 (1): 50–1. [DOI] [PubMed] [Google Scholar]
- 12. Shanafelt TD, Dyrbye LN, Sinsky C, et al. Relationship between clerical burden and characteristics of the electronic environment with physician burnout and professional satisfaction. Mayo Clin Proc 2016; 91 (7): 836–48. [DOI] [PubMed] [Google Scholar]
- 13. Gardner RL, Cooper E, Haskell J, et al. Physician stress and burnout: the impact of health information technology. J Am Med Inform Assoc 2019; 26 (2): 106–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Marckini DN, Samuel BP, Parker JL, Cook SC.. Electronic health record associated stress: a survey study of adult congenital heart disease specialists. Congenit Heart Dis 2019; 14 (3): 356–61. [DOI] [PubMed] [Google Scholar]
- 15. Robertson SL, Robinson MD, Reid A.. electronic health record effects on work-life balance and burnout within the I3 population collaborative. J Grad Med Educ 2017; 9 (4): 479–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Adler-Milstein J, Zhao W, Willard-Grace R, Knox M, Grumbach K.. Electronic health records and burnout: time spent on the electronic health record after hours and message volume associated with exhaustion but not with cynicism among primary care clinicians. J Am Med Inform Assoc 2020; 27 (4): 531–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.KLAS Research. Arch Collaborative Example Survey [Internet]. Available from: https://klasresearch.com/images/pages/usability-studies/base-emr-experience-survey.pdf Accessed June 11, 2020.
- 18.American Medical Association. Physician Burnout: Improve Physician Satisfaction and Patient Outcomes [Internet]. Ed Hub. [cited 2020. Jun 16]. https://edhub.ama-assn.org/steps-forward/module/2702509
- 19. Rohland BM, Kruse GR, Rohrer JE.. Validation of a single-item measure of burnout against the Maslach Burnout Inventory among physicians. Stress Health 2004; 20 (2): 75–9. [Google Scholar]
- 20. Lewis SE, Nocon RS, Tang H, et al. Patient-centered medical home characteristics and staff morale in safety net clinics. Arch Intern Med 2012; 172 (1): 23–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Knox M, Willard-Grace R, Huang B, Grumbach K. Maslach burnout inventory and a self-defined, single-item burnout measure produce different clinician and staff burnout estimates. - Abstract - Europe PMC. 2020. https://europepmc.org/article/PMC/6082224 Accessed May 22, 2020. [DOI] [PMC free article] [PubMed]
- 22. Sinsky CA, Bodenheimer T.. Powering-up primary care teams: advanced team care with in-room support. Ann Fam Med 2019; 17 (4): 367–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Team Documentation [Internet]. 2020. https://edhub.ama-assn.org/steps-forward/module/2702598 Accessed October 2, 2020.
- 24. Guo U, Chen L, Mehta PH.. Electronic health record innovations: helping physicians – one less click at a time. Health Inf Manag J 2017; 46 (3): 140–4. [DOI] [PubMed] [Google Scholar]
- 25. Panagioti M, Panagopoulou E, Bower P, et al. Controlled interventions to reduce burnout in physicians: a systematic review and meta-analysis. JAMA Intern Med 2017; 177 (2): 195–205. [DOI] [PubMed] [Google Scholar]
- 26. West CP, Dyrbye LN, Erwin PJ, Shanafelt TD.. Interventions to prevent and reduce physician burnout: a systematic review and meta-analysis. Lancet 2016; 388 (10057): 2272–81. [DOI] [PubMed] [Google Scholar]
- 27. Sieja A, Markley K, Pell J, et al. Optimization sprints: improving clinician satisfaction and teamwork by rapidly reducing electronic health record burden. Mayo Clin Proc 2019; 94 (5): 793–802. [DOI] [PubMed] [Google Scholar]
- 28.Fast Facts Infographics AHA. 2020. https://www.aha.org/infographics/2020-07-24-fast-facts-infographics Accessed October 2, 2020.
- 29.US Hospital EMR Market Share 2020 Shifting Perspectives Among Large and Small Hospitals–KLAS Report. 2020. https://klasresearch.com/report/us-hospital-emr-market-share-2020/1616 Accessed October 2, 2020.
- 30. Young A, Chaudhry HJ, Pei X, Arnhart K, Dugan M, Snyder GB. A Census of Actively Licensed Physicians in the United States, 2016. 2017;15. https://meridian.allenpress.com/jmr/article/103/2/7/80882/A-Census-of-Actively-Licensed-Physicians-in-the Accessed October 2, 2020.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data underlying this article were provided by KLAS Research by permission. Data will be shared on request to the corresponding author with permission of KLAS Research.