Abstract
Objective
Stress and burnout due to electronic health record (EHR) technology has become a focus for burnout intervention. The aim of this study is to systematically review the relationship between EHR use and provider burnout.
Materials and Methods
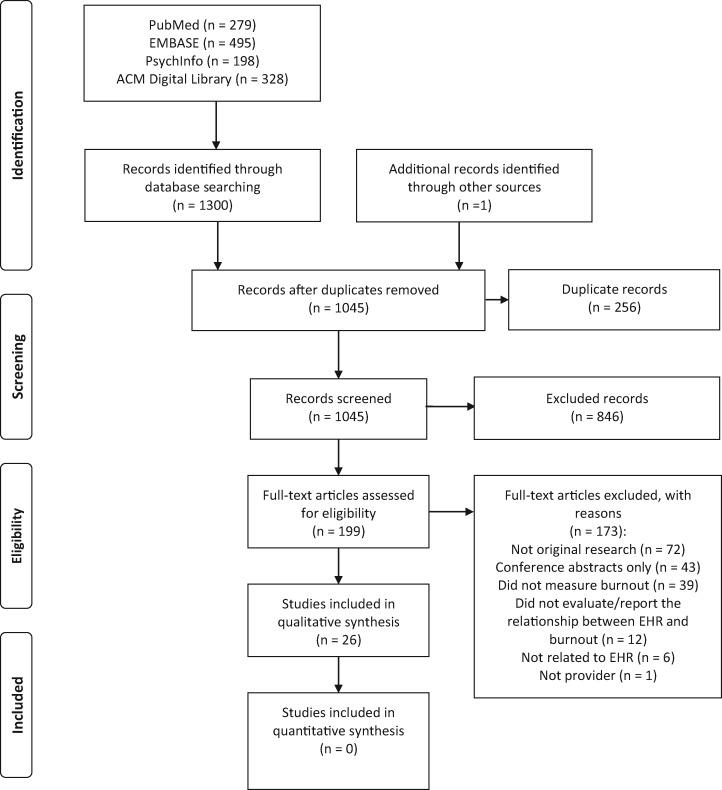
A systematic literature search was performed on PubMed, EMBASE, PsychInfo, ACM Digital Library in accordance with the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) statement. Inclusion criterion was original research investigating the association between EHR and provider burnout. Studies that did not measure the association objectively were excluded. Study quality was assessed using the Medical Education Research Study Quality Instrument. Qualitative synthesis was also performed.
Results
Twenty-six studies met inclusion criteria. The median sample size of providers was 810 (total 20 885; 44% male; mean age 53 [range, 34-56] years). Twenty-three (88%) studies were cross-sectional studies and 3 were single-arm cohort studies measuring pre- and postintervention burnout prevalence. Burnout was assessed objectively with various validated instruments. Insufficient time for documentation (odds ratio [OR], 1.40-5.83), high inbox or patient call message volumes (OR, 2.06-6.17), and negative perceptions of EHR by providers (OR, 2.17-2.44) were the 3 most cited EHR-related factors associated with higher rates of provider burnout that was assessed objectively.
Conclusions
The included studies were mostly observational studies; thus, we were not able to determine a causal relationship. Currently, there are few studies that objectively assessed the relationship between EHR use and provider burnout. The 3 most cited EHR factors associated with burnout were confirmed and should be the focus of efforts to improve EHR-related provider burnout.
Keywords: electronic health records, health information technology, provider burnout, systematic review
INTRODUCTION
Provider burnout is a major concern in health care.1 Burnout is defined by symptoms in 3 dimensions—feelings of energy depletion or exhaustion, increased mental distance from one’s job or feelings of cynicism or negativism about one’s job, and reduced professional efficacy.2 Over 40% of U.S. physicians across all specialties have reported at least 1 symptom of burnout.3,4 Similar burnout rates (35%-45%) have been reported among U.S. nurses.5 Provider burnout negatively influences patient care, increases medical errors, and decreases patient satisfaction.5–9 For providers, burnout is associated with increased risk of depression, substance abuse, and suicide.1,9–11 Last, physicians and nurses with burnout are likely to reduce work hours or change careers, which would further aggravate the problem of the growing physician shortage that is estimated to be between 42 900 to 121 900 providers by the year 2032.12–14
With the implementation of the Health Information Technology for Economic and Clinical Health Act in 2009, there has been widespread adoption of electronic health records (EHRs) in health care.15 In a 2017 survey, 96% of nonfederal acute care hospitals and 80% of office-based physicians had adopted certified EHRs.16 Seventy percent of EHR users reported health information technology (HIT)–related stress, which is highly associated with burnout.17 In addition, there have been numerous commentaries discussing the role of EHRs and their potential contribution to an increase in provider burnout.18–20 There is a small corpus of studies that have objectively evaluated the association between EHR usage and burnout, but none have synthesized the current data into a systemic review.
The presence and needed interactions with an EHR can detract from direct patient care when providers spend a significant portion of their clinical time completing EHR tasks.21 While prior studies have found mixed results regarding satisfaction with EHR implementation, studies that measured stress (defined as stress, psychological strain, and job stress) found increased stress among providers associated with EHR implementation.22 Pressure to document, the stress associated with documentation, and the lack of time allocated for documentation were all aspects of EHR usage linked to poor job satisfaction and increased levels of provider burnout.23 Two solutions to reduce burnout have been proposed to rectify provider stress and burnout: (1) clerical and scribe support to assist physicians with the documentation burden and (2) optimizing EHR workflows through education, workflow improvements, and technical enhancements.23 However, while clerical and scribe support and optimizing EHR workflow have been associated with increased provider efficiency and improved user satisfaction, their implementation has not clearly demonstrated decreased rates of provider burnout.23 Additionally, objective data exploring factors related to EHR component processes, such as order entry system, alert intrusions, total time spent on EHR, and percent of work time spent on EHR, have not been reviewed with regard to their association with objective measures of burnout. The aim of this study is to systematically search and review the literature on the relationship between the use of EHR and provider burnout and seeks to answer the following question: What is the relationship between EHR usage and provider burnout?
MATERIALS AND METHODS
Study identification and inclusion
A systematic literature review was performed on 4 databases (PubMed, EMBASE, PsychInfo, ACM Digital Library), from database inception to September 5, 2020, in accordance with PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines on systematic reviews (the PRISMA checklist can be seen in Supplementary Appendix 1).24 There was no review protocol for this study. The search strategy was developed with the help of a librarian using a Boolean strategy. A combination of terms electronic; computerized; health; medical; record; records, and “decision support system; medical order entry system; CPOE; computerized physician order entry; medical record system, computerized” were used to capture EHR-related articles. A combination of “work”, “workplace”, “job”, “occupational” and “stress”, “frustration”, “exhaustion” in addition to terms burnout, emotional exhaustion, depersonalization, and burnout, professional were used to capture burnout. MeSH (Medical Subject Heading) terms in PubMed were translated to corresponding subject headings in EMBASE and PsychInfo. MeSH terms were removed for the search in the ACM Digital Library because the ACM Digital Library does not perform indexing with subject heading. The detailed search strategies are presented in Supplementary Appendix 2. Publications for analysis met the following criterion—original research investigating the association between EHR and provider burnout. A provider was defined as anyone who provides direct patient care, including physicians, physician assistants, nurse practitioners, allied professionals, and nurses. Exclusion criteria included (1) not original research, (2) studies that did not use a well-described method to measure burnout, (3) conference abstracts only, (4) studies that did not objectively evaluate the relationship between EHR usage and burnout (eg, cross-sectional studies that only provided the prevalence of burnout and participant opinions of EHR, intervention studies that did not report pre- and postintervention burnout), (5) studies unrelated to EHR, and (6) studies not focused on providers. The review was limited to studies that objectively measured burnout because burnout, stress, and dissatisfaction, although closely related, are not interchangeable concepts.2,25 The following definitions were adopted: stress is a very general concept that is poorly defined but is driven mainly by job stressors, satisfaction is driven by a sense of belonging and successful completion of a healing mission, burnout is a triad of symptoms caused by a mismatch of high efforts with poor satisfaction in addition to workplace stress.25–27 Burnout is considered to be measured objective if the study used a well-described methodology or tool. We excluded conference abstracts due to the limited information provided and inability to perform quality assessments. We excluded studies that only provided descriptive data on provider opinions of EHR and burnout rate or provider subjective attribution of burnout to EHR; thus, qualitative studies were excluded from this review. The evaluation of the association between EHR variable (including provider opinion of EHR) and burnout was considered objective if 1 or more statistical tests were used to evaluate the relationship or if the study reported preintervention and postintervention burnout rate when an EHR related intervention was present. Two independent reviewers, Z.H. and P.H.T., performed title and abstract screening. Full-text screening was then performed also by 2 independent reviewers (Q.Y. and Z.H. or Q.Y. and P.H.T.) on studies that were not unanimously excluded during title and abstract screening. Disagreement during full text screening were resolved by discussion between the 2 raters and M.G.D. until consensus was reached. Reference lists of included articles were also screened manually as a secondary search strategy.
Study outcomes
Data collection was performed by 2 reviewers (Q.Y. and J.Z.) independently with discrepancies resolved by consensus with a third person (M.G.D.). Data variables collected included sample size, response rate, study design, gender, age, specialty, practice model, provider practice setting, provider type, EHR measures, burnout measures, prevalence of burnout, and type of statistical analysis performed evaluating the relationship between EHR and burnout, including results and P values (for multivariate analysis, other predictors included in the model were also collected). Effective sample size was defined as the number of respondents or the number of participants included in the analysis. Family medicine, general medicine, and general pediatrics in outpatient settings were grouped as primary care physicians (PCPs) in our review if the percentage of PCP was not reported. The primary study outcome was objectively measured burnout linked to EHR usage as determined by correlation between 1 or more EHR measures and burnout, odds ratio (OR) for logistics regression, regression coefficient for linear regression, and burnout prevalence before and after intervention or in the control group and the intervention group. Burnout prevalence in the study population was the total number of participants determined to be burned out divided by the total number of participants and was limited to the studies reporting such outcome. The secondary study outcomes included the prevalence of provider burnout and other predictors of burnout including HIT-related stress, which is defined as presence of 1 of the following: poor or marginal time for documentation, moderately high or excessive time spent on EHR at home, and agreement that EHR adds to daily frustration.17 Meta-analysis was not performed because there was significant heterogeneity between studies in terms of method of analysis, predictor used, and outcome used. To summarize categorical data such as the percentage of males or provider type, summing of the denominator and numerator was performed to calculate the overall percentage. To summarize continuous data such as age of the participants, the combined mean was calculated by dividing the sum of individual study mean multiplied by sample size, by the sum of the sample sizes. If the mean was not reported, the median was used as an alternative.
Study quality and bias
The qualities of the included studies were assessed using a validated tool—Medical Education Research Study Quality Instrument (MERSQI).28 MERSQI evaluates the methodology of a study in 6 domains—study design, sampling, type of data, validity of evaluation instrument, data analysis, and outcomes—with possible maximum score of 3 for each domain for a total possible score of 18.28 The total MERSQI score was calculated as the percentage of the total achievable score (accounting for “not applicable” responses) and then adjusted to a standard denominator of 18 to allow for comparison.28 For those studies that utilized a survey instrument to measure EHR usage or impression, an additional validity of evaluation instrument was added. Selective reporting was assessed in addition to MERSQI. Selective reporting is considered present if some predictors of the statistical model were not reported or if specific P values were not reported.
Interrater reliability
Absolute percentage agreement and weighted kappa coefficient was calculated to measure interrater reliability for MERSQI scoring between 2 raters.29 The reliability between raters was high, with 88% absolute agreement and weighted kappa of 0.88.
RESULTS
Study description
A total of 26 studies met inclusion criteria (Figure 1) with a total effective sample size of 20 885 participants (median 810 [range, 6-35 922] participants). Response rates in these studies ranged from 3.8% to 100%. Characteristics of included studies are described in Table 1.
Figure 1.
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flow diagram for search and selection process.
Table 1.
Characteristics of included studies
| Author | N | RR | Study design | Male | Age | Specialty | Practice Model | Provider Type | Practice setting | MERSQI |
|---|---|---|---|---|---|---|---|---|---|---|
|
Babbott, 201430 |
379 | 50.3% | Cross-sectional | 55.9% | Mean 43 y | PCP | Mixed | Physicians | Outpatient | 13.7 |
| Gilleland, 201431 | 139 | NR | Cross-sectional | NR | NR | Non-PCP | Academic | Physicians (trainees only) | Outpatient | 10.7 |
| Shanafelt, 20164 | 6560 | 18.3% | Cross-sectional | 31.6% (3% NS) | Median 56 y | 23.3% PCP, 3.3% NS |
24.9% Academic 17.5% NS |
Physicians | Unselected | 11.4 |
| Contratto, 201732 | 7 | 100% | Pre- and postintervention survey | NR | NR | PCP | Academic | Physicians (attendings only) | Outpatient | 13.2 |
| Gregory, 201733 | 16 | NR | Cross-sectional | NR | NR | PCP | Nonacademic | Physicians, NP, PA | Unselected | 11.8 |
| Rassolian, 201734 | 1752 | 91.1% | Cross-sectional | 58.3%c | NR | PCP | Mixed | Physicians (attendings) | Unselected | 14.2 |
| Robertson, 201735 | 585 | 67.6% | Cross-sectional | 45.2% | 34 | PCP | 34.5% academic | Physicians (41.9% attendings) | Unselected | 11.8 |
| Tawfik, 201736 | 1934 | 70.0% | Cross-sectional | 18.1% | NR | Non-PCP | 29% academic hospitals |
Physicians (trainees and attendings): 11.5%, NP: 1.7%, Nurses: 72.2% Other: 14.7% |
Inpatient | 11.8 |
| Domaney, 20188 | 52 | 61.2% | Cross-sectional | NR | NR | Non-PCP | Academic | Physicians (23.1% attendings) |
Outpatient: 46%, ED/consult: 26%, Inpatient: 30% |
11.8 |
| Harris, 201837 | 371 | 31.0% | Cross-sectional | 11.6% |
24-40 y: 29.1% 41-60 y: 47.7% 61-80 y: 23.2% |
32.3% PCP, 30.5% NS | Mixed | NP |
Outpatient: 38.0% inpatient: 62.0% |
13.3 |
| Pozdnyakova, 201838 | 6 | 100% | Pre- and postintervention survey | 50% | NR | PCP | Academic | Physicians (attendings only) | Outpatient | 13.2 |
| Privitera, 201839 | 1048 | 3.8% | Cross-sectional | 63.0% | Mean 55.1 y (SD = 11.3 y) | Mixed | 40.4% academic | Physicians (attendings only) | Unselected | 11.4 |
| Gardner, 201917 | 1792 | 42.7% | Cross-sectional | 64.3% |
30-50 y: 42.5%, 51-64 y: 39%, 65-90 y: 18.5% |
29.4% PCP | Mixed | Physicians (attendings only) | Outpatient: 67.6%, inpatient: 32.3% | 13.3 |
| Kroth, 201940 | 282 | 44.1% | Cross-sectional | 36.4% (14% NS) | Mean 50 y (SD = 11 y) | 68.4% PCP, 1.1% NS | Mixed |
Physicians (attendings only): 85.5%, NP: 5%, PA: 7.1%, NS: 0.4% |
Outpatient | 13.3 |
| Marckini, 201941 | 110 | 28.7% | Cross-sectional | 71.8% | <55 y: 70% | Non-PCP | 80.7% academic | Physicians | Unselected | 11.4 |
| Mehta, 201942 | 2274 | 21.1% | Cross-sectional | 58.1% | NR | Non-PCP | Mixed | Physicians (trainees and attendings) | Unselected | 13.3 |
| Olson, 201943 | 475 | 37.9% | Cross-sectional | 59.2% (4.4% NS) |
25-34 y: 6.7%, 35-44 y: 26.1%, 45-54 y: 24.4%, 55-65 y: 16.0%, >65 y: 8.4% NS: 18.3% |
17.1% PCP, 4.4% NS | 72% academic | Physicians (attendings only) |
Outpatient: 42.1%, inpatient: 21.9%, both: 35.4%, NS: 0.6% |
12.8 |
| Sieja, 201944 | 113 | 55.1% | Pre- and postintervention survey | NR | NR | Non-PCP | Mixed |
Physicians: 73%, NP/PA: 27% |
Outpatient | 13.8 |
| Tai-Seale, 201945 | 934 | 72.3% | Cross-sectional | 45.0% | Mean 50 y (SD = 11 y) | Mixed | Nonacademic | Physicians | Unselected | 14.1 |
|
Tran, 201946 |
107 | 56.3% | Cross-sectional | 29.0% (6% NS) | NR | PCP | Academic |
Physicians (attendings only): 80.4% NP/PA: 17.8%, NS: 1.8% |
Outpatient | 14.1 |
| Adler-Milstein, 202047 | 87 | 66.9% | Cross-sectional | 15.6% (3.9% NS) | NR | PCP | Academic |
Physicians (attendings only): 90% NP or PA: 10% |
Outpatient | 12.9 |
| Giess, 202048 | 159 | 77.9% | Cross-sectional | 51.6% |
<40 y: 22.8% 40-49 y: 29.1% ≥50 y: 27.2% Other: 20.9% |
Non-PCP | 96.8% academic | Physicians (attendings only) | NR | 13.3 |
| Hilliard, 202049 | 422 | 7.2% | Cross-sectional | 45.0% |
<40 y: 27.7% 40-60 y: 56.6% >60 y: 15.6% |
25.8% PCP | Mixed |
Physicians (attendings only): 84.8% NP: 11.1% PA: 4.0% |
Outpatient | 14.1 |
| Melnick, 202050 | 870 | 69.9% | Cross-sectional | 58.5% (0.8% NS) |
Median 53 (interquartile range, 42-61) y |
25.5% PCP, 0.1% NS | 32.2% academic, 19.1% NS | Physicians | Unselected | 13.3 |
| Somerson, 202051 | 203 | 5.8% | Cross-sectional | 79.8% | NR | Non-PCP | Mixed | Physicians (trainees only) | Unselected | 11.4 |
| Tajirian, 202052 | 208 | 44.5% | Cross-sectional | 50.5%, (4.3% NS) |
<30 y: 8.2% 31-40 y: 38.9% 41-50 y: 28.4% 51-60 y: 11.1% ≥61 y: 13.5% |
Non-PCP | Academic | Physicians (84.6% attendings) | Outpatient: 76.4%, inpatient: 39.4%, ED: 19.2%, other: 16.8% | 12.3 |
The percentage of males in the group of providers that were given the survey, not the respondents.
ED: emergency department; MERSQI: Medical Education Research Study Quality Instrument; NA: not applicable; NP: nurse practitioner; NR: not reported; NS: not specified; PCP: primary care provider; PA: physician assistant; RR: response rate.
Forty-four percent of the participants (9 093/20 590 in 21 studies) were male. The estimated mean age of the participants was 53 (range, 34-56) years across 7 studies. A total of 34.4% (6 768/19 661 in 24 studies) of the participants were PCPs, 32.9% (3 659/11 115 in 16 studies) practiced in an academic setting, and 89.2% (18 030/20 213 in 24 studies) were physicians, 2.6% were advanced practitioners, 6.8% were nurses, and 1.4% were allied professionals. Of 15 studies that specified the rank of the physicians (trainee vs faculty), only 10.5% (754/7 195) were trainees. Twenty-three studies were cross-sectional studies, and 3 were prospective studies that had a pre- and postinterventional design.
Study quality
Study quality was acceptable, with a median of 13.2 of 18 on MERSQI (Supplementary Appendix 3). No study scored <50% on the MERSQI scale. Most studies had low response rates for usable data, with only 4 studies reporting participation above 75%. Within the MERSQI scale, the validity of evaluation instruments for burnout employed was high with 96.2% of the studies scoring a 3 out of 3. The validity of evaluation instruments for EHR-associated variables was lower, with 61.1% (11/18) scoring a 3 out of 3. Most studies (96.2%) used appropriate statistical analysis, with only 2 (7.7%) studies being purely descriptive. Selective reporting was present in 15 (57.7%) of 26 studies.
Electronic health record
There were multiple approaches to assess EHR usage by providers. Most studies (n = 18) used subjective EHR data, 5 studies used EHR-derived data, and 3 studies used EHR-related interventions. The types of EHR data assessed included: general EHR use factors (14 studies), opinions of EHR (5 studies), EHR usability (4 studies), EHR user proficiency or efficiency (4 studies), messaging or communication within EHR (5 studies), EHR chart review (2 studies), EHR documentation (10 studies), and last, EHR order entry function (2 studies). Some studies (n = 12) evaluated various panels of these aforementioned measurements (Table 2).
Table 2.
Aspects of EHR assessed, type of burnout survey used, and statistical method utilized.
| Author, Year | EHR Use Measure | Burnout Measure | Statistical Analysis |
|---|---|---|---|
| Babbott, 201430 |
|
The single-item measure | Cohen's d family effect size |
| Gilleland, 201431 |
EHR derived data on:
|
Internally developed 5-point burnout survey | Spearman correlation |
| Shanafelt, 20164 |
|
Maslach Burnout Inventory | Logistic regression |
| Contratto, 201732 | Intervention:
|
2 questions (1 burnout, 1 depersonalization) adapted from Maslach Burnout Inventory | Descriptive |
| Gregory, 201733 |
|
Adapted Shirom-Melamed Burnout Measure | Linear regression |
| Rassolian, 201734 |
|
Mini-Z Survey | Logistic regression |
| Robertson, 201735 |
|
The single-item measure | Logistic regression |
| Tawfik, 201736 |
|
Maslach Burnout Inventory (emotional exhaustion subset) | Linear regression |
| Domaney, 20188 |
|
Maslach Burnout Inventory Human Services Survey | Spearman correlation |
| Harris, 201837 |
HIT-related stress:
|
The single-item measure | Logistic regression |
| Pozdnyakova, 201838 |
Intervention
|
The single-item measure | Descriptive |
| Privitera, 201839 |
|
Mini-Z Survey | Logistic regression |
| Gardner, 201917 |
HIT- related stress:
|
The single-item measure | Logistic regression |
| Kroth, 201940 |
|
The single-item measure | Logistic regression |
| Marckini, 201941 |
|
Maslach Burnout Inventory | Wilcoxon |
| Mehta, 201942 |
|
Mini Z Burnout Survey | Logistic regression |
| Olson, 201943 |
|
Maslach Burnout Inventory, Mini Z Burnout Survey |
Logistic regression |
| Sieja, 201944 |
Intervention
|
Maslach Burnout Inventory (emotional exhaustion subscale) | Chi-square |
| Tai-Seale, 201945 |
|
The single-item measure | Logistic regression |
| Tran, 201946 |
EHR derived data on:
|
Mini Z Burnout Survey | Logistic regression (outcome = EHR) |
| Adler-Milstein, 202047 |
EHR derived data:
Subjective data:
|
Maslach Burnout Inventory survey (emotional exhaustion and cynicism subscale) | Logistic regression |
| Giess, 202048 | The Stanford Physician Wellness Survey—EHR experience:
|
The single-item measure | Logistic regression |
| Hilliard, 202049 |
EHR-derived data: Workload variables
Efficiency variables
|
The single-item measure | Logistic regression |
| Melnick, 202050 |
|
Maslach Burnout Inventory | Logistic regression |
| Somerson, 202051 |
|
Maslach Burnout Inventory Human Services Survey | Logistic regression |
| Tajirian, 202052 | Perceived Usefulness of EHR
|
The single-item measure | Chi-square/Fisher |
Only EHR measures used to assess its relationship with burnout were included in the table.
CPOE: computerized provider order entry; EHR: electronic health record; EMR: electronic medical record; HIT: health information technology.
Burnout
Burnout was assessed using various validated instruments. Nine studies used instruments based on the Maslach Burnout Inventory (MBI), 9 used the single-item measure, 5 used the Mini-Z survey, 1 used an adapted Shirom-Melamed Burnout Measure (SMBM), 1 used both the MBI and the single-item measure, and 1 used an internally developed single item measure (Table 2). The MBI is a 22-item questionnaire that is divided into 3 subscales: emotional exhaustion (9 items), depersonalization (5 items), and personal accomplishment (8 items).53 It is internationally recognized as the standard measure of burnout.8 The single-item measure of burnout is based on a 5-point Likert-type scale and has been validated against MBI, providing good correlation with emotional exhaustion and depersonalization subscales of the MBI.54,55 However, while the single-item measure has a high specificity of over 90%, the sensitivity was only 50% for clinicians, and thus it may yield a more conservative result.56 The adapted SMBM also contains 3 subscales, each containing 3 items: physical fatigue, cognitive weariness, and emotional exhaustion.33 The SMBM was validated by the creator against MBI.57 The full Mini-Z assesses burnout based on 2 single-item measures similar to the previously mentioned single-item measure.58 The additional components of Mini-Z assess other factors associated with provider burnout such as satisfaction, stress, work control, chaos, etc.58 The burnout prevalence among study participants was between 16.7% and 63.5%, with a mean of 39.7% (8 679/21 867 in 22 studies).
Statistical design
Fifteen studies treated burnout as a binary variable and reported the ORs of burnout associated with EHR characteristics after adjusting for covariates. Two studies treated burnout as a continuous variable and reported beta coefficients associated with EHR characteristics from linear regression after adjusting for covariates. Six studies assessed the association between burnout and EHR without adjustment for covariates using various statistical methods (Table 2). Two studies reported purely descriptive data. Last, 1 study used burnout as a predictor to evaluate the time spent on the EHR and the percentage of EHR tasks completion.
Factors associated with burnout
General use of EHR, EHR usability, user proficiency and efficiency
The amount of time spent on EHR and time spent at home or after work hour were a popular focus of investigation; however, the results across the studies were equivocal (Table 3). Five studies found that time on EHR at home or after work was associated with burnout—self-reported high or excessive time on EHR (OR, 1.46-2.90) and17,35,39,43 objective EHR data highest quartile vs lowest quartile (OR, 12.52).47 In contrast, 4 studies did not find a statistically significant association.31,34,37,42 Gilleland et al31 found a positive correlation (r = 0.2, P =.02) between burnout and the percentage of hours spent on EHR after 5 pm out of total time spent on EHR daily, although this was a very weak association. General user proficiency34,43,47 and efficiency47 measures were not associated with burnout. Melnick et al50 found that the more user friendly an EHR was considered, as measured by a system usability scale, the lower the risk of burnout was. However, another study, which evaluated provider user difficulty with various EHR functions and its association with burnout, did not find any association.40 The number of EHR features available also was not associated with burnout.30
Table 3.
Association of EHR variables and burnout
| Reference number |
|||
|---|---|---|---|
| Positive Association | Negative Association | Not Significant | |
| General EHR use factors | |||
| EHR use | 36 a | 4 , 36 b | |
| Remote EHR use | 17 , 37 | ||
| Time spent on EHR | 51 | 31 | |
| EHR at home | 17 , 39 , 43 c | 34 d , 37 , 42 | |
| EHR after work hour | 35 , 47 | 31 | |
| Time spent on EHR on unscheduled days | 47 | ||
| Average # of logons after work hour | 31 | ||
| High % of time spent on EHR after work hour/total time logged on | 31 | ||
| Negative health consequences from EHR use | 40 | ||
| Intervention—EHR training, workflow redesign, and addition of specialty-specific EHR functions | 44 | ||
| Opinions of EHR | |||
| General opinions of EHR | 48 | ||
| Belief that EHR adds frustration | 17 , 37 , 52 | ||
| Disagree that EHR keeps patient safe | 52 | ||
| Disagree that EHR communications are efficient | 52 | ||
| Disagree that EHR improved efficiency | 41 | ||
| Dissatisfaction with EHR | 52 | ||
| Dissatisfaction with patient care related clerical tasks on EHR | 41 | ||
| Dissatisfaction with patient care unrelated clerical tasks on EHR | 41 | ||
| EHR usability | |||
| # of EHR features available | 30 | ||
| High EHR usability | 50 | ||
| EHR user proficiency/efficiency | |||
| EHR proficiency | 34 d 43 c 47 | ||
| EHR efficiency | 42 , 47 | ||
| Greater # of different EHR system used | 35 | ||
| Longer experience with any specific EHR | 35 | ||
| Length of current EHR in place | 35 | ||
| Messaging or communication within EHR | |||
| Time spent on inbox alert messages | 33 | ||
| High # of inbox messages | 45 , 47 | ||
| High # of patient call messages | 49 e f | ||
| High # of result messages | 49 e f | ||
| Insufficient time to deal with inbox alert messages | 33 | ||
| Patient portal use | 4 | ||
| Disagree that patient portal has improved efficiency | 41 | ||
| EHR chart review | |||
| Time spent on chart review | 49 e f | ||
| Use of Chart Search function | 49 e f | ||
| EHR documentation | |||
| Insufficient time for documentation | 17 , 34 d 37 , 39 , 42 , 43 c | ||
| Note length in EHR | 49 e f | ||
| Precharting of visit notes | 49 e f | ||
| High % of note entered using copy and paste | 49 b | ||
| High % of note entered using SmartTools | 49 f | ||
| High # of user SmartPhrases | 49 e f | ||
| Use of transcription or voice recognition for notes | 49 f | ||
| Uses scribes | 17 , 37 , 47 , 49 ef | ||
| EHR order function | |||
| High # of medication orders authorized | 49 e f | ||
| High # of nonmedication orders authorized | 49 e f | ||
| CPOE use | 4 | ||
| % of orders placed from preference list or SmartSet | 49 e f | ||
Statistically significant results on bivariate analysis but not significant on multivariate analysis were considered not significant. Not significant results from bivariate analysis not included in multivariate analysis are included in this table as not significant. For studies reporting each subdomains of burnout as outcome separately, statistically significant outcome in any one domain is considered significant result for the study. P value<.05 is considered significant.
CPOE: computerized provider order entry; EHR: electronic health record.
Multivariate modal with prevalence of burnout on neonatal intensive care unit level as outcome.
Mixed effect modal with neonatal intensive care unit as random effect and individual burnout as outcome.
Multivariate modal with burnout as outcome measured by Maslach Burnout Inventory and multivariate modal with burnout as outcome measured by Mini-Z showed consistent results thus were not reported separately in this table.
The modal with demographic, practice characteristics, and other variables of the survey all included in the model is used.
Multivariate modal with complete sample without note composition data.
Multivariate modal with subset of clinicians with note composition data.
Messaging or communication volumes within EHR
A high number of inbox messages (above average vs below average: OR, 2.06; physical exhaustion subscale, highest quartile vs lowest quartile: OR, 6.17),45,47 patient call messages (highest quartile vs lowest quartile, without note composition variables: OR, 3.81; highest quartile vs lowest quartile, with note composition variables in a subset of clinicians: OR 6.59),49 and insufficient time to deal with the volume of inbox alert messages (physical fatigue: β = 0.58, t = 2.56; cognitive weariness: β = 0.53, t = 2.23)33 have been associated with increased burnout. However, time spent on inbox alert messages,33 number of result messages,49 and patient portal usage4 were not associated with burnout.
EHR chart review and documentation
Time spent on EHR documentation (emotional exhaustion: r = 0.4 in residents, r = 0.38 in attendings)8 and insufficient time for documentation (OR, 1.40-5.83; 6 studies)17,34,37,39,42,43 were associated with increased burnout. However, results on time spent on chart review was inconclusive.8,49 A large percentage of notes entered by “copy and paste” was associated with a lower rate of burnout (highest quartile vs lowest quartile: OR, 0.22).49 Other specific EHR use habits such as methods of EHR documentation, such as dictation,49 use of a scribe,17,37,47,49 or use of SmartTools49; length of EHR note49; precharting49; writing EHR notes while with patients8,49; and use of the ChartSearch function, were not associated with burnout.49
EHR order function
Shanafelt et al4 associated computerized provider order entry use with increased burnout. However in contrast, Hilliard et al49 did not find any association between burnout and the number of medication or nonmedication orders authorized or the percentage of order placed from preference lists or SmartSets. Contratto et al32 found that the number of physicians with significant burnout decreased from 3 to 1 (of 7) physicians after a physician order entry clerical support staff member was hired; however, the study was only descriptive.
Provider opinion of EHR
Tajirian et al52 found that 88.2% of burned out providers believed that EHR usage adds frustration compared with 56.8% of providers not burned out believed that EHR usage adds frustration (P <.001). Providers that believed the EHR contribute to feelings of frustration had 2.17 to 2.44 odds of being burned out in 2 other studies.17,37 Higher burnout rates were also seen in providers with other negative perceptions of EHR: disagreed that EHR kept patients safe,52 disagreed that EHR communications were effective,52 disagreed that EHR improved efficiency,41 and dissatisfied with clerical tasks on EHR related or unrelated to patient care.41
Other factors such as provider, work environment, workflow, and workload factors related with burnout are summarized in Supplementary Appendices 4 and 5.
DISCUSSION
This analysis has shown that there are few studies that have objectively evaluated the relationship between EHR and provider burnout. Insufficient time for documentation, high volumes of inbox or patient call messages, and negative perceptions of EHR were the 3 most cited EHR related factors associated with increased measures of burnout among providers.
The presence of an EHR can generate significant clerical and cognitive burdens. A previous study has shown that for every hour of direct patient care, 2 hours were spent on the EHR and associated clerical work.59 Almost half of the providers using an EHR (46%) believe that they have insufficient time for documentation, vs only 13.6% among those without an EHR.17 This high demand of EHR documentation carries over to providers’ personal time, leading to over a third of providers reporting excessive amount of time spent on the EHR at home, contributing to dissatisfaction and poor work-life balance, which contributes to a higher incidence of burnout.17,35,39,47 While the use of an EHR at home or after work is a frequently cited factor associated with burnout, a review of evidence from the available literature was equivocal and did strongly support this contention.
The burden of a high inbox message volume was isolated as a contributor to burnout by several studies.33,45,47 Providers spent approximately 20 to 42 minutes per clinic day managing their inbox during their “free time.”46 Inbox messages includes communications from patients, other providers, and alert messages generated from EHR algorithms. EHR-generated alerts can account for almost half of the inbox messages.45 Studies have reported that providers desire protected time to manage alert messages as well as seeking improvements in EHR features to decrease alert burden and to assist with the management of inbox alert messages.33 Of note, Gregory et al33 did not find an association between the reported number of hours spent on managing inbox alert messages and burnout but found that a perceived excess of alerts was associated with increased burnout. Gregory et al33 did not evaluate the quantity of alerts received by providers, which was positively associated with higher burnout in all 3 studies that utilized EHR-based objective data.45,47,49
Current recommendations to reduce provider burden include medical scribes, team approach to care, EHR improvement, and EHR proficiency training.35,47 A systematic review of the use of scribes in healthcare settings suggested that it improved clinician satisfaction, productivity, time-related efficiency, revenue, and patient-clinician interactions.60 However, scribe use has not been associated with burnout in our review.17,37,47,49 Another strategy to decrease physician burnout is the team approach to care. This approach focused on offloading clerical burden (including documentation, nonphysician order entry, inbox management, health coaching, and care coordination) to nurses, medical assistants, or specialty technicians.4 Sieja et al44 reported a series of EHR improvement interventions performed by an 11-member team that led to a decrease of reported burnout from 39% to 34%, although statistical significance was not achieved. Forty-three percent of clinicians agreed that documentation time decreased after the intervention.44 EHR proficiency training was also proposed as a method to prevent burnout; however, in our review, EHR proficiency and efficiency measures were not linked to burnout.
Through our review, we have identified several deficiencies in the research on EHR and burnout. There is a paucity of research in the nursing and advanced practitioners user groups. This is especially important for nurses due to their heavy use of EHR and different workflow from physicians and advanced practitioners. Only Melnick et al50 evaluated EHR usability and found that EHR usability was very poor compared with other sectors indicating that this topic deserves more attention. Additionally, while Gregory assessed EHR generated inbox alerts, there were very few studies that evaluated4,33,49 COPE and associated synchronous alerts. Providers, on average, received over 4000 best practice advisories and 1000 drug alerts per year.61 Most of these alerts were overridden, and most alert overrides were appropriate.62 Whether this significant alert burden contributed to provider burnout would be worthy of further exploration.4 Only 5 studies used EHR-generated objective data, whereas most studies used provider-reported EHR use or workload. Providers’ self-reported time spent on EHR was only weakly correlated with objective data and tend to be overestimated thus more using EHR-derived objective data may provide more insights.31,47,52
The novelty of this review is that the search strategy only selected articles that used an objective measure of burnout. This process confirmed that insufficient documentation time, high inbox or patient call messages, and negative perception of EHR were associated with burnout. While the use of EHR at home or after work was also a frequently cited factor associated with burnout, evidence from available literature does not support this contention. The current study extends the level of knowledge on burnout by concentrating on objective measures of burnout and synthesizing the current quantitative literature on burnout. This study reenforces that the cumulative findings in the literature continued to support the 3 factors identified from prior research but demonstrates that the literature is too heterogeneous to allow a meta-analysis, which would increase the level of evidence supporting these factors. As such, we recommend more uniform methodology and standardized reporting of these factors in the future literature.
The quality of this review is governed by the quality of the included studies. Some degree of selective reporting was present in over half of the studies. A high number of studies used subjective EHR data introducing recall bias and most studies had poor response rates leading to selection bias. Owing to the observational nature of the included studies, we were not able to determine any causal relationships. There were only 3 interventional studies, and all had very small samples sizes. In addition, we were not able to perform a meta-analysis due to significant heterogeneity between studies. Some studies analyzed burnout as a continuous variable, while others as a binary variable, making it difficult to compare the results between these studies. Last, studies adjusted for various covariate factors; however, not all studies adjusted for provider or work-related factors that may affect burnout.
CONCLUSION
There are few studies that objectively evaluated the relationship between EHR usage and provider burnout. Insufficient time for documentation, high inbox or patient call message volume, and provider negative perceptions of EHR were the 3 most reported EHR-related factors associated with increased burnout in providers. The current data in the literature are insufficiently robust to allow a meta-analysis of the data. Future studies should use objective EHR measures, investigate computerized provider order entry system and synchronous alerts, and explore burnout in advanced practitioners and nursing population.
FUNDING
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
AUTHOR CONTRIBUTIONS
QY and MGD contributed to substantial contributions to the conception or design of the work.
QY, ZJ, ZH, PHT, and MGD made substantial contributions to the acquisition, analysis, or interpretation of data for the work.
QY drafted the work.
ZJ, ZH, PHT, and MGD revised it critically for important intellectual content.
QY, ZJ, ZH, PHT, and MGD Gave final approval of the version to be published.
QY, ZJ, ZH, PHT, and MGD gave agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
SUPPLEMENTARY MATERIAL
Supplementary material is available at Journal of the American Medical Informatics Association online.
DATA AVAILABILITY STATEMENT
The data underlying this article are available in the article and in its online supplementary material.
Supplementary Material
ACKNOWLEDGMENTS
We thank the librarians at University of Texas Health Science Center at San Antonio for their help with the literature search.
CONLICT OF INTEREST STATEMENT
The authors have no competing interests to declare.
References
- 1. Williams ES, Rathert C, Buttigieg SC.. The personal and professional consequences of physician burnout: a systematic review of the literature. Med Care Res Rev 2020; 77 (5): 371–86. [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization. Burn-out an “occupational phenomenon”: International Classification of Diseases. https://www.who.int/mental_health/evidence/burn-out/en/ Accessed June 15, 2020.
- 3. Shanafelt TD, West CP, Sinsky C, et al. Changes in burnout and satisfaction with work-life integration in physicians and the general US working population between 2011 and 2017. Mayo Clin Proc 2019; 94 (9): 1681–94. [DOI] [PubMed] [Google Scholar]
- 4. Shanafelt TD, Dyrbye LN, Sinsky C, et al. Relationship between clerical burden and characteristics of the electronic environment with physician burnout and professional satisfaction. Mayo Clin Proc 2016; 91 (7): 836–48. [DOI] [PubMed] [Google Scholar]
- 5. Dyrbye LN, Shanafelt TD, Johnson PO, et al. A cross-sectional study exploring the relationship between burnout, absenteeism, and job performance among American nurses. BMC Nurs 2019; 18 (1): 57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. West CP, Tan AD, Habermann TM, et al. Association of resident fatigue and distress with perceived medical errors. JAMA 2009; 302 (12): 1294–300. [DOI] [PubMed] [Google Scholar]
- 7. Grol R, Mokkink H, Smits A, et al. Work satisfaction of general practitioners and the quality of patient care. Fam Pract 1985; 2 (3): 128–35. [DOI] [PubMed] [Google Scholar]
- 8. Domaney NM, Torous J, Greenberg WE.. Exploring the association between electronic health record use and burnout among psychiatry residents and faculty: a pilot survey study. Acad Psychiatry 2018; 42 (5): 648–52. [DOI] [PubMed] [Google Scholar]
- 9. Shanafelt TD, Bradley KA, Wipf JE, et al. Burnout and self-reported patient care in an internal medicine residency program. Ann Intern Med 2002; 136 (5): 358–67. [DOI] [PubMed] [Google Scholar]
- 10. Soler JK, Yaman H, Esteva M, et al. ; European General Practice Research Network Burnout Study Group. Burnout in European family doctors: the EGPRN study. Fam Pract 2008; 25 (4): 245–65. [DOI] [PubMed] [Google Scholar]
- 11. van der Heijden F, Dillingh G, Bakker A, et al. Suicidal thoughts among medical residents with burnout. Arch Suicide Res 2008; 12 (4): 344–6. [DOI] [PubMed] [Google Scholar]
- 12. Sinsky CA, Dyrbye LN, West CP, et al. Professional satisfaction and the career plans of US physicians. Mayo Clin Proc 2017; 92 (11): 1625–35. [DOI] [PubMed] [Google Scholar]
- 13. Shanafelt T, Goh J, Sinsky C.. The business case for investing in physician well-being. JAMA Intern Med 2017;177(12):1826–32 [DOI] [PubMed] [Google Scholar]
- 14. Dall Tim RR, Jones K, Chakrabarti R, Lacobucci W.. 2019. Update The Complexities of Physician Supply and Demand Projections from 2017 to 2032. https://www.aamc.org/system/files/c/2/31-2019_update_-_the_complexities_of_physician_supply_and_demand_-_projections_from_2017-2032.pdf Accessed June 16, 2020.
- 15.U.S. Department of Health and Human Services. HITECH Act Enforcement Interim Final Rule. https://www.hhs.gov/hipaa/for-professionals/special-topics/hitech-act-enforcement-interim-final-rule/index.html#:∼:text=HITECH%20Act%20Enforcement%20Interim%20Final%20Rule,use%20of%20health%20information%20technology Accessed June 15, 2020.
- 16.Office of the National Coordinator for Health Information Technology. Health IT Data Summaries. https://dashboard.healthit.gov/apps/health-information-technology-data-summaries.php?state=National&cat9=all+data&cat1=ehr+adoption#summary-data Accessed September 15, 2020.
- 17. Gardner RL, Cooper E, Haskell J, et al. Physician stress and burnout: the impact of health information technology. J Am Med Inform Assoc 2019; 26 (2): 106–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Ehrenfeld JM, Wanderer JP.. Technology as friend or foe? Do electronic health records increase burnout? Curr Opin Anaesthesiol 2018; 31 (3): 357–60. [DOI] [PubMed] [Google Scholar]
- 19. Downing NL, Bates DW, Longhurst CA.. Physician burnout in the electronic health record era: are we ignoring the real cause? Ann Intern Med 2018; 169 (1): 50–1. [DOI] [PubMed] [Google Scholar]
- 20. Collier R. Rethinking EHR interfaces to reduce click fatigue and physician burnout. CMAJ 2018; 190 (33): E994–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Kataria S, Ravindran V.. Electronic health records: a critical appraisal of strengths and limitations. J R Coll Physicians Edinb 2020; 50 (3): 262–8. [DOI] [PubMed] [Google Scholar]
- 22. DeChant PF, Acs A, Rhee KB, et al. Effect of organization-directed workplace interventions on physician burnout: a systematic review. Mayo Clin Proc 2019; 3 (4): 384–408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Gesner E, Gazarian P, Dykes P.. The burden and burnout in documenting patient care: an integrative literature review. Stud Health Technol Inform 2019; 264: 1194–8. [DOI] [PubMed] [Google Scholar]
- 24. Moher D, Liberati A, Tetzlaff J, Altman DG; the PRISMA Group. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: the PRISMA statement. PLoS Med 2009; 6 (7): e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Stan VA, Correa R, Deslauriers JR, Faynboym S, Shah T, Widge AS; AMA-RFS Task Force on Resident/Fellow Physician Satisfaction. Support, technology and mental health: correlates of trainee workplace satisfaction. Perspect Med Educ 2020; 9 (1): 31–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Pines AM, Keinan G.. Stress and burnout: The significant difference. Pers Individ Dif 2005; 39 (3): 625–35. [Google Scholar]
- 27. Iacovides A, Fountoulakis KN, Kaprinis S, Kaprinis G.. The relationship between job stress, burnout and clinical depression. J Affect Disord 2003; 75 (3): 209–21. [DOI] [PubMed] [Google Scholar]
- 28. Reed DA, Cook DA, Beckman TJ, Levine RB, Kern DE, Wright SM.. Association between funding and quality of published medical education research. JAMA 2007; 298 (9): 1002–9. [DOI] [PubMed] [Google Scholar]
- 29. McHugh ML. Interrater reliability: the kappa statistic. Biochem Med 2012; 22 (3): 276–82. [PMC free article] [PubMed] [Google Scholar]
- 30. Babbott S, Manwell LB, Brown R, et al. Electronic medical records and physician stress in primary care: results from the MEMO Study. J Am Med Inform Assoc 2014; 21 (e1): e100–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Gilleland M, Komis K, Chawla S, Fernandez S, Fishman M, Adams M.. Resident duty hours in the outpatient electronic health record era: inaccuracies and implications. J Grad Med Educ 2014; 6 (1): 151–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Contratto E, Romp K, Estrada CA, Agne A, Willett LL.. Physician order entry clerical support improves physician satisfaction and productivity. South Med J 2017; 110 (5): 363–8. [DOI] [PubMed] [Google Scholar]
- 33. Gregory ME, Russo E, Singh H.. Electronic health record alert-related workload as a predictor of burnout in primary care providers. Appl Clin Inform 2017; 8 (3): 686–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Rassolian M, Peterson LE, Fang B, et al. Workplace factors associated with burnout of family physicians. JAMA Intern Med 2017; 177 (7): 1036–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Robertson SL, Robinson MD, Reid A.. Electronic health record effects on work-life balance and burnout within the I(3) population collaborative. J Grad Med Educ 2017; 9 (4): 479–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Tawfik DS, Phibbs CS, Sexton JB, et al. Factors associated with provider burnout in the NICU. Pediatrics 2017; 139 (5): e20164134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Harris DA, Haskell J, Cooper E, Crouse N, Gardner R.. Estimating the association between burnout and electronic health record-related stress among advanced practice registered nurses. Appl Nurs Res 2018; 43: 36–41. [DOI] [PubMed] [Google Scholar]
- 38. Pozdnyakova A, Laiteerapong N, Volerman A, et al. Impact of medical scribes on physician and patient satisfaction in primary care. J Gen Intern Med 2018; 33 (7): 1109–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Privitera MR, Atallah F, Dowling F, et al. Physicians’ electronic health records use at home, job satisfaction, job stress and burnout. J Hosp Adm 2018; 7 (4): 52–9. [Google Scholar]
- 40. Kroth PJ, Morioka-Douglas N, Veres S, et al. Association of electronic health record design and use factors with clinician stress and burnout. JAMA Netw Open 2019; 2 (8): e199609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Marckini DN, Samuel BP, Parker JL, et al. Electronic health record associated stress: a survey study of adult congenital heart disease specialists. Congenit Heart Dis 2019; 14 (3): 356–61. [DOI] [PubMed] [Google Scholar]
- 42. Mehta LS, Lewis SJ, Duvernoy CS, et al. Burnout and career satisfaction among U.S. cardiologists. J Am Coll Cardiol 2019; 73 (25): 3345–8. [DOI] [PubMed] [Google Scholar]
- 43. Olson K, Sinsky C, Rinne ST, et al. Cross-sectional survey of workplace stressors associated with physician burnout measured by the Mini-Z and the Maslach Burnout Inventory. Stress Health 2019; 35 (2): 157–75. [DOI] [PubMed] [Google Scholar]
- 44. Sieja A, Markley K, Pell J, et al. Optimization sprints: improving clinician satisfaction and teamwork by rapidly reducing electronic health record burden. Mayo Clin Proc 2019; 94 (5): 793–802. [DOI] [PubMed] [Google Scholar]
- 45. Tai-Seale M, Dillon EC, Yang Y, et al. Physicians' well-being linked to in-basket messages generated by algorithms in electronic health records. Health Aff (Millwood) 2019; 38 (7): 1073–8. [DOI] [PubMed] [Google Scholar]
- 46. Tran B, Lenhart A, Ross R, et al. Burnout and EHR use among academic primary care physicians with varied clinical workloads. AMIA Jt Summits Transl Sci Proc 2019; 2019: 136–44. [PMC free article] [PubMed] [Google Scholar]
- 47. Adler-Milstein J, Zhao W, Willard-Grace R, et al. Electronic health records and burnout: Time spent on the electronic health record after hours and message volume associated with exhaustion but not with cynicism among primary care clinicians. J Am Med Inform Assoc 2020; 27 (4): 531–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Giess CS, Ip IK, Cochon LR, et al. Predictors of self-reported burnout among radiology faculty at a large academic medical center. J Am Coll Radiol 2020; 17 (12): 1684–91. doi: 10.1016/j.jacr.2020.01.047 [DOI] [PubMed] [Google Scholar]
- 49. Hilliard RW, Haskell J, Gardner RL.. Are specific elements of electronic health record use associated with clinician burnout more than others? J Am Med Inform Assoc 2020; 27 (9): 1401–10. doi: 10.1093/jamia/ocaa092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Melnick ER, Dyrbye LN, Sinsky CA, et al. The association between perceived electronic health record usability and professional burnout among US physicians. Mayo Clin Proc 2020; 95 (3): 476–87. [DOI] [PubMed] [Google Scholar]
- 51. Somerson JS, Patton A, Ahmed AA, et al. Burnout among United States orthopaedic surgery residents. J Surg Educ 2020; 77 (4): 961–8. [DOI] [PubMed] [Google Scholar]
- 52. Tajirian T, Stergiopoulos V, Strudwick G, et al. The influence of electronic health record use on physician burnout: cross-sectional survey. J Med Internet Res 2020; 22 (7): e19274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Maslach C, Jackson S, Leiter M.. The Maslach Burnout Inventory Manual. 3rd ed. Palo Alto, CA: Consulting Psychologists Press; 1996.
- 54. Rohland BM, Kruse GR, Rohrer JE.. Validation of a single-item measure of burnout against the Maslach Burnout Inventory among physicians. Stress Health 2004; 20 (2): 75–9. [Google Scholar]
- 55. West CP, Dyrbye LN, Satele DV, et al. Concurrent validity of single-item measures of emotional exhaustion and depersonalization in burnout assessment. J Gen Intern Med 2012; 27 (11): 1445–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Knox M, Willard-Grace R, Huang B, et al. Maslach burnout inventory and a self-defined, single-item burnout measure produce different clinician and staff burnout estimates. J Gen Intern Med 2018; 33 (8): 1344–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Shirom A, Melamed S.. A comparison of the construct validity of two burnout measures in two groups of professionals. Int J Stress Manag 2006; 13 (2): 176–200. [Google Scholar]
- 58. Linzer M, Poplau S, Babbott S, et al. Worklife and wellness in academic general internal medicine: results from a national survey. J Gen Intern Med 2016; 31 (9): 1004–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Sinsky C, Colligan L, Li L, et al. Allocation of physician time in ambulatory practice: a time and motion study in 4 specialties. Ann Intern Med 2016; 165 (11): 753–60. [DOI] [PubMed] [Google Scholar]
- 60. Shultz CG, Holmstrom HL.. The use of medical scribes in health care settings: a systematic review and future directions. J Am Board Fam Med 2015; 28 (3): 371–81. [DOI] [PubMed] [Google Scholar]
- 61. Ancker JS, Edwards A, Nosal S, et al. ; HITEC Investigators. Effects of workload, work complexity, and repeated alerts on alert fatigue in a clinical decision support system. BMC Med Inform Decis Mak 2017; 17 (1): 36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Poly TN, Islam MM, Yang HC, et al. Appropriateness of overridden alerts in computerized physician order entry: systematic review. JMIR Med Inform 2020; 8 (7): e15653. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data underlying this article are available in the article and in its online supplementary material.