Abstract
Background.
How personality traits and anxiety and depressive disorders relate longitudinally has implications for etiologic research and prevention. We sought to determine how neuroticism and extraversion relate to first-onset anxiety and depressive disorders in young adults.
Design.
An inception cohort of 489 university freshmen was followed for 6 years.
Method.
Participants self-reported personality traits using the Eysenck Personality Questionnaire, and anxiety and depressive disorders were assessed using the Diagnostic Interview Schedule.
Results.
Baseline neuroticism predicted first-onset panic disorder, agoraphobia, generalized anxiety disorder (GAD), and major depressive disorder (MDD), while introversion predicted first-onset agoraphobia. Participants who developed panic disorder, agoraphobia, GAD, or MDD had increases in neuroticism if the disorder was current at follow-up. These effects were moderate to large. Participants who developed MDD but were in remission by follow-up had a moderate increase in neuroticism.
Conclusions.
High neuroticism in young adulthood is either a true risk factor, or a marker of risk, for first-onset anxiety and depressive disorders, as is low extraversion for later agoraphobia. Results suggest large neuroticism “state” effects for panic disorder, agoraphobia, and MDD, and a moderate “scar” effect from MDD. Although many clinicians and researchers regard personality traits simply as “vulnerability” factors, longitudinal analyses suggest additional complexity.
Keywords: Longitudinal study, personality, anxiety disorders, panic disorder, agoraphobia, major depressive disorder
Introduction
Personality trait variation appears relevant to risk for anxiety and depressive disorders (Jeronimus et al., 2016). However, the onset of anxiety and depressive disorders also appears to alter personality traits temporarily (“state” effects) (Fanous et al., 2007; Karsten et al., 2012; Ormel et al., 2004), or perhaps more permanently (“scar” effects), though results regarding the latter are conflicting in the case of major depressive disorder (Fanous et al., 2007; Ormel et al., 2004). A better understanding of the longitudinal relations between personality traits and disorders could enhance etiologic research and facilitate prevention (Andersen & Bienvenu, 2011).
Prior prospective studies suggest that high neuroticism is a risk factor for future development of depressive and anxiety symptoms and disorders. A large meta-analysis of 59 longitudinal and prospective studies (443,313 participants) showed large associations between neuroticism and anxiety and depressive symptoms and disorders, though this association was attenuated after adjustment for baseline symptoms and psychiatric history (Jeronimus et al., 2016). Prospective studies of adolescents and young adults may more accurately assess premorbid personality (i.e., before first onset of some anxiety and depressive disorders). In a sample of 900 14-year-olds in New Zealand, higher neuroticism at 14 predicted depression and anxiety by age 30 (Newton-Howes et al., 2015). In studies of high school students followed for shorter periods (18 months to 6 years), higher baseline neuroticism was associated with subsequent first-onset DSM-IV depressive and anxiety disorders (Goldstein et al., 2018; Kendall et al., 2015; Zinbarg et al., 2016).
Anxiety and depressive disorders also have the potential to confound personality assessment. “State” effects could occur if having a current disorder changes a person’s sense of his or her personality traits, and such effects have been demonstrated clearly in persons with current major depressive episodes (Fanous et al., 2007; Kendler et al., 1993). Karsten et al. (2012) examined state effects of depressive and anxiety disorders on big-five personality traits in adults. They reported evidence of small state effects for both depressive and anxiety disorders on neuroticism (increase), as well as small state effects for depressive disorders on extraversion and conscientiousness (decreases). Similarly, Reich et al. (1986) reported that patients whose panic disorder and agoraphobia symptoms improved with treatment had concomitant changes in personality, including greater emotional strength (an inverse neuroticism analog). In contrast, Perna et al. (1992) reported that patients with panic disorder had high levels of harm avoidance (another neuroticism analog), but that the level of harm avoidance was unrelated to the patients’ current anxiety state, suggesting that state-trait confounding was not an issue. Nevertheless, little research has assessed possible state-trait effects of individual anxiety disorders other than panic disorder.
Anxiety and depressive disorders may result in more permanent changes to personality traits. With this “scar” effect, the changes in personality that occur with the onset of a disorder remain even after recovery. For example, in 2-wave studies at least 1 year apart, Kendler and colleagues (Fanous et al., 2007; Kendler et al., 1993) reported that neuroticism remained elevated, compared to baseline, after onset and remission of a major depressive episode. Alternately, in a 3-wave study over 2 years, Ormel et al. (2004) reported no evidence of a change in personality traits after a depressive episode, concluding that elevated neuroticism after a depressive episode reflected premorbid vulnerability. While these studies suggest that personality may be altered by depression, at least in the short-term (1–2 years), to our knowledge little research has been done on possible scar effects after recovery from anxiety disorders.
This Study
The objective of the current study was to assess longitudinal relationships between the personality traits neuroticism and extraversion and first-onset anxiety and depressive disorders in young adults. We sought to determine the extent to which personality traits act as risk factors for anxiety and depressive disorders, and the extent to which onset of a disorder was associated with personality “state” and/or “scar” effects.
Methods
Sample and Procedure
As described previously by Sher et al. (1991), in the 1987–1988 academic year, 3,156 out of 3,944 first-time freshmen in a large Midwestern university participated in a screening for a longitudinal study on alcoholism. These students were screened with measures of personality traits, alcohol and drug use, and parental alcoholism. The longitudinal sample comprised 489 participants, 237 controls without first- or second-degree relatives with alcohol or drug use disorders and 253 participants with a biological father who met criteria for a diagnosis of alcoholism. Participants provided written informed consent after the nature of the study was explained. At year 1 (baseline) the average age was 18.6 years; the sample was 47% male and 94% white; and 99.8% had never married. By year 7, the number of retained participants was 457, with an average age of 25.5 years; 65.2% had never married. Participants who did not complete the study were slightly older at year 1, but there was no other significant difference in demographic characteristics compared to participants retained throughout the study.
Measures
The Eysenck Personality Questionnaire (EPQ) and the Diagnostic Interview Schedule (DIS) were administered over a 6-year period (Sher et al., 2000). The EPQ is a 90-item self-report measure of neuroticism (23 items, α = 0.85), extraversion (21 items, α = 0.83), and psychoticism (Eysenck & Eysenck, 1975), alphas from current sample (Gershuny & Sher, 1998). In the current study, the correlation between neuroticism and extraversion was −.11. The EPQ was administered at years 1 and 7. We focused on the dimensions neuroticism (the tendency to experience negative emotions like nervousness, sadness, and anger) and extraversion (the tendency to be venturesome, energetic, assertive, and sociable and to experience positive emotions), because these two traits have been more consistently associated with anxiety and depressive disorders in cross-sectional studies than psychoticism (Kotov et al., 2010).
Trained non-clinician interviewers administered the DIS Version III-A (L. N. Robins et al., 1981) in years 1 and 2, and the DIS Version III-Revised (L. N. Robins et al., 1989) in years 3, 4, and 7. For the sake of consistency, all diagnoses for the current study were made using Diagnostic and Statistical Manual of Mental Disorders, Third Edition (DSM-III) criteria (1980). We limited our focus to anxiety and depressive disorders that tend to begin in young adulthood: panic disorder, agoraphobia, generalized anxiety disorder (GAD), and major depressive disorder (MDD) (Kessler et al., 2005). Although we had aggregate data on simple (specific) phobia, which can have onset after childhood, and data on social phobia, which can have onset after early adolescence, we chose not to include these disorders for the sake of simplicity of analytic interpretation. Specifically, most of the participants should have passed through the age period of greatest risk, so the results may not typify personality–simple/social phobia relations; younger samples would be preferable to address this research question. We decided not to include dysthymia because it is less common, and we anticipated limited statistical power.
Statistical Analyses
We completed all analyses using IBM SPSS (v25). All statistical tests were 2-tailed, and a p-value of .05 was considered statistically significant. For each analysis, we standardized personality traits using z-scores, excluded participants with a year-1 (baseline) lifetime history of the disorder in question, and compared participants with first onset of disorder during the 6-year follow-up period to participants at risk who did not develop the disorder in question.
We used logistic regression to analyze baseline personality traits (standardized as z-scores) as risk factors for first-onset anxiety and depressive disorders. These analyses produced odds ratios (OR) for first-onset disorder given a standard deviation higher personality trait score. Though survival analysis (e.g., Cox regression) also would have been appropriate, we chose logistic regression because of its relative simplicity (i.e., simple to interpret, less assumptions). We first performed unadjusted logistic regression analyses, then multivariable logistic regressions to adjust for potential confounder variables including age, sex, and family history of alcoholism (if those variables were also associated with incident disorder, p < .15). We present only unadjusted results because adjustment did not have a substantial effect on the variables of interest. For statistically significant associations, we calculated Cohen’s d effect sizes, to facilitate effect size comparisons with “state” and “scar” effect analyses described below.
We used linear regression to assess the effect of first-onset disorders on personality traits at follow-up, adjusting for baseline personality traits. To assess “state” effects, we compared participants with disorder present in the last 12 months to participants without onset of that disorder. To assess “scar” effects, we compared participants with disorder remitted for 12 months to participants without onset of that disorder. As with logistic regressions, we first performed unadjusted linear regression analyses (i.e., only including the baseline personality score and condition of interest as predictor variables). We then conducted additional analyses to adjust for potential confounder variables including age, sex, and family history of alcoholism (if these variables were associated with personality traits at follow-up, p < .15). Again, we present only unadjusted results because adjustment did not have a substantial effect on the variables of interest. Since personality trait scores were standardized, these analyses produced regression coefficients equivalent to Cohen’s d for the effect of present or past disorder.
Results
At year 1 (baseline), 111 participants met criteria for a lifetime history of at least one of the four target DSM-III diagnoses: 4 with panic disorder, 19 with agoraphobia, 91 with GAD, and 36 with MDD. By year 7, 112 participants had first onset of at least one of the DSM-III diagnoses: 18 with panic disorder, 42 with agoraphobia, 77 with GAD, and 47 with MDD (Table 1). Comorbidity was common with both baseline and first-onset disorders. Note that not all participants with first-onset disorders during the follow-up period had complete data for state and scar effect analyses. Baseline disorders were not associated with retention in the study, but lower baseline neuroticism and extraversion were associated with retention (mean z-score differences in participants lost to follow-up vs. retained were −0.19 and −0.09, respectively).
Table 1.
Descriptive data
| Year 1 | Year 7 | |
|---|---|---|
| Participants, n | 489 | 457 |
| Mean neuroticism (SD) | 9.41 (5.02) | 8.07 (5.29) |
| Mean extraversion (SD) | 15.86 (4.05) | 14.60 (4.45) |
| First-onset panic disorder, n | - | 18 (−5)* |
| First-onset agoraphobia, n | - | 42 (−20)* |
| First-onset generalized anxiety disorder, n | - | 77 (−1)* |
| First-onset major depressive disorder, n | - | 47 (−3)* |
Note.
Participants with first-onset disorder who had incomplete data at year 7
Baseline Personality Traits as Predictors of First-Onset Disorders
Higher baseline neuroticism was a risk factor for incident panic disorder (d = 0.9), agoraphobia (d = 0.9), GAD (d = 0.6), and MDD (d = 0.8) by year 7 (Table 2). Furthermore, baseline low extraversion was a risk factor for incident agoraphobia (d = −0.5). Controlling for age, sex, and family history of alcoholism did not substantially affect these findings (results not shown). Figure 1 illustrates the relationship between baseline neuroticism scores and the cumulative incidence of particular disorders over the 6-year follow-up period.
Table 2.
Baseline personality traits as predictors of first-onset DSM-III disorders during 6-year follow-up
| Beta | SE | Odds ratio* (95% CI) | p | R2 | ||
|---|---|---|---|---|---|---|
| Panic disordera | Neuroticism | 1.06 | .31 | 2.88 [1.56, 5.31] | .001 | .12 |
| Extraversion | −0.39 | .28 | 0.68 [0.39, 1.16] | .152 | .02 | |
| Agoraphobiab | Neuroticism | 1.14 | .25 | 3.12 [1.92, 5.07] | <.0005 | .16 |
| Extraversion | −0.56 | .21 | 0.57 [0.38, 0.87] | .008 | .05 | |
| Generalized anxiety disorderc | Neuroticism | 0.71 | .15 | 2.04 [1.52, 2.75] | <.0005 | .10 |
| Extraversion | 0.02 | .14 | 1.02 [0.78, 1.34] | .897 | <.001 | |
| Major depressive disorderd | Neuroticism | 0.87 | .18 | 2.39 [1.67, 3.42] | <.0005 | .12 |
| Extraversion | −0.17 | .17 | 0.84 [0.60, 1.18] | .317 | .005 |
Note. R2 = Nagelkerke R-squared.
odds ratio for a standard deviation higher personality trait score.
18 participants with first onset, 435 at risk but without onset.
42 participants with first onset, 411 at risk but without onset.
77 participants with first onset, 292 at risk but without onset.
47 participants with first onset, 371 at risk but without onset.
Figure 1.
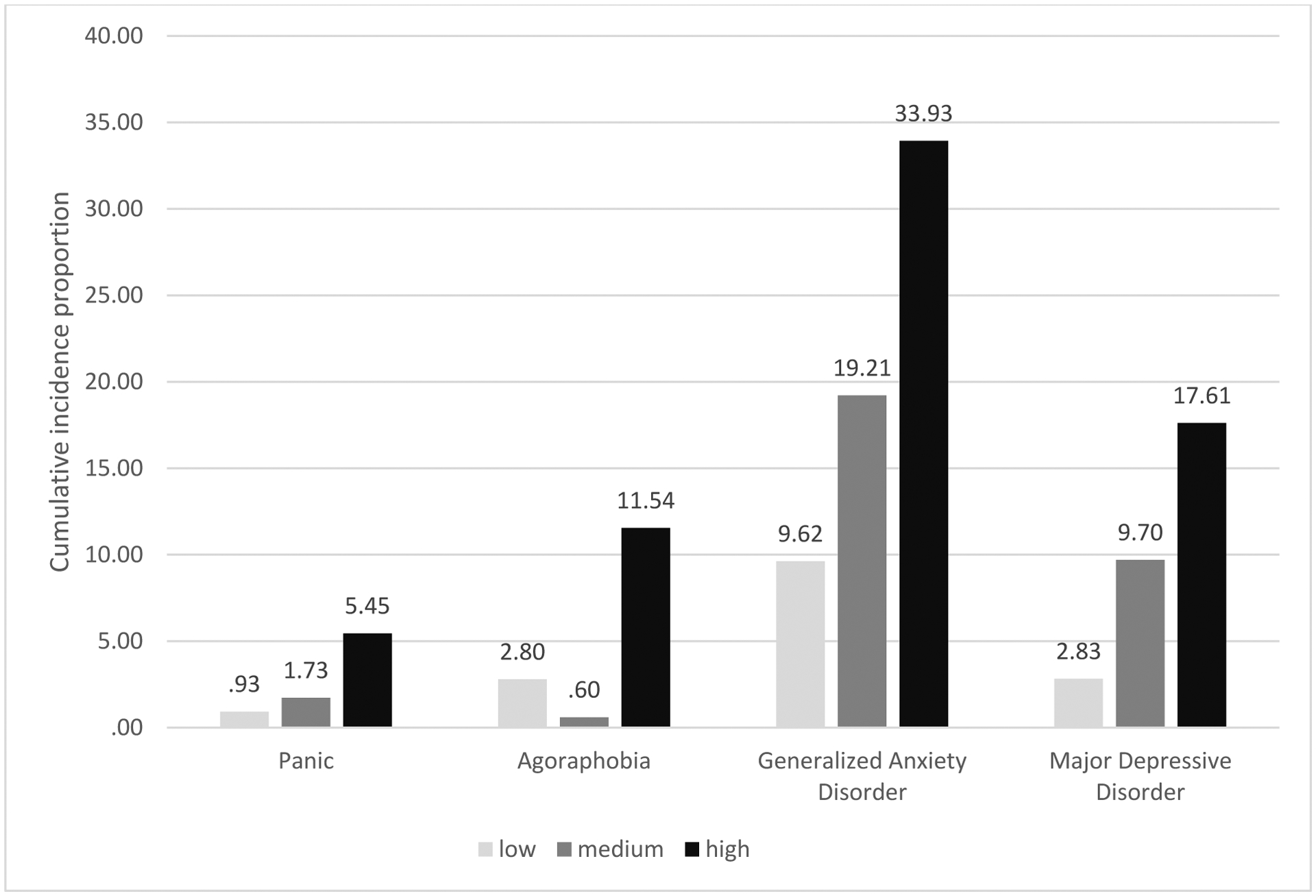
Cumulative incidence proportion of DSM-III disorders by baseline neuroticism score
low = baseline neuroticism z-score range −3 to −.5, medium = −.49 to .49, high = .5 to 3
Effect of First-Onset Disorders on Personality Traits
Having panic disorder, agoraphobia, GAD, or MDD in the last 12 months was associated with an elevation in participants’ neuroticism scores (Table 3). The effect sizes for these statistically significant findings were moderate (GAD) to large (panic disorder, agoraphobia, and MDD). Unexpectedly, having agoraphobia in the last 12 months was associated with a large elevation in extraversion. Having remitted MDD was also associated with a moderate “scar” effect; i.e., neuroticism remained moderately elevated in participants in whom MDD had remitted for at least 12 months. Controlling for age, sex, and family history of alcoholism did not substantially affect these findings (results not shown).
Table 3.
Effect of first-onset DSM-III disorders during 6-year follow-up on personality traits at year 7, controlling for baseline personality traits
| Disorder | Trait | Present (state effects) | Remitted (scar effects) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Beta | SE | [95% CI] | p | R2 | Beta* | SE | [95% CI] | p | R2 | ||
| Panic disordera | Neuroticism | 1.40 | .46 | [0.50, 2.31] | .003 | .35 | .01 | .26 | [−.50, .52] | .98 | .32 |
| Extraversion | −0.18 | −49 | [−1.15, 0.78] | .71 | .29 | −.22 | .27 | [−.75, .32] | .43 | .29 | |
| Agoraphobiab | Neuroticism | 1.07 | .47 | [0.16, 1.99] | .022 | .32 | −.03 | .19 | [−.41, .35] | .86 | .33 |
| Extraversion | 1.13 | .48 | [0.18, 2.08] | .020 | .30 | −.01 | .20 | [−.41, .38] | .94 | .30 | |
| Generalized anxiety disorderc | Neuroticism | 0.50 | .06 | [0.11, 0.89] | .013 | .35 | .21 | .12 | [−.02, .43] | .077 | .35 |
| Extraversion | 0.03 | .22 | [−0.40, 0.46] | .90 | .30 | .01 | .12 | [−.23, .25] | .94 | .32 | |
| Major depressive disorderd | Neuroticism | 1.77 | .34 | [1.10, 2.40] | <.0005 | .36 | .40 | .13 | [.14, .67] | .003 | .35 |
| Extraversion | −0.29 | .38 | [−1.03, 0.45] | .44 | .30 | −.25 | .14 | [−.53, .03] | .075 | .30 | |
Note.
Beta coefficients represent standardized differences in personality traits for participants with current or remitted disorder at year 7, compared to participants at risk for first onset of the disorder who did not have onset during 6-year follow-up, controlling for baseline personality traits.
3 participants with disorder present during last 12 months, 10 with remitted disorder, 435 at risk without onset.
3 participants with disorder present during last 12 months, 19 with remitted disorder, 411 at risk without onset.
18 participants with disorder present during last 12 months, 58 with remitted disorder, 292 at risk without onset.
5 participants with disorder present during last 12 months, 39 with remitted disorder, 371 at risk without onse.
Discussion
We found that baseline higher neuroticism was a risk factor for subsequent first-onset panic disorder, agoraphobia, GAD, and MDD, and baseline low extraversion was a risk factor for subsequent first-onset agoraphobia during the follow-up period. Neuroticism effect sizes were large for panic disorder, agoraphobia, and MDD and moderate for GAD; the extraversion effect size was moderate for agoraphobia. Participants who developed first-onset panic disorder, agoraphobia, GAD, or MDD during the follow-up period had increases in neuroticism if the disorder was current at follow-up. These “state” effects were large for panic disorder, agoraphobia, and MDD, and moderate for GAD. There was also evidence for a moderate scar effect in participants who developed MDD during the follow-up period, but remitted for at least 12 months by follow-up.
This study helps elucidate how personality traits and anxiety and depressive disorders relate in young adulthood. Information on personality traits could be useful for prevention of anxiety disorders in this vulnerable age group (Bienvenu & Ginsburg, 2007). The current study also shows that “state” effects, in particular, should be considered when measuring personality traits for use in genetic (Nagel et al., 2018) and other studies. Though many clinicians and researchers regard personality traits simply as “vulnerability” factors, longitudinal analyses suggest additional complexity.
Other recent longitudinal studies using complementary methods and samples from different age groups are useful in elucidating how personality traits relate to anxiety and depressive disorders from adolescence through adulthood. In a community sample of 550 adolescent girls aged 13.5 to 15.5, higher baseline neuroticism was associated with subsequent first onset of DSM-IV MDD and GAD over 18 months, even controlling for other baseline variables, including baseline subthreshold symptoms (Goldstein et al., 2018). In a sample of 547 11th-graders enriched for high neuroticism (mean age 16.9 years), baseline neuroticism was strongly associated with subsequent first onset of DSM-IV MDD and anxiety disorders over the following 3 years; baseline neuroticism was more strongly associated with MDD and anxiety disorders than substance use disorders (Zinbarg et al., 2016). In a study of 2,596 18- to 65-year-old participants (mean age 42 years) recruited from the general population, primary care, and mental health clinics and followed for 2 years, small neuroticism “state” effects were evident for DSM-IV depressive and anxiety disorders, and small extraversion state effects (reduced extraversion) were evident for depressive disorders (Karsten et al., 2012). Notably, this last study had a very large number of participants with current anxiety and depressive disorders contributing to estimation of “state” effects in adulthood (Karsten et al., 2012), so the effect sizes should have been estimated more precisely than in the current study. We found large “state” effects of panic disorder, agoraphobia, and MDD in a younger sample, but our estimates are based on a relatively small number of participants with disorder in the last year.
Strengths and Limitations
Strengths of the current study include relatively high participant retention and inclusion of a variety of analyses regarding potential personality–psychopathology relations in young adulthood. However, several potential limitations exist beyond those discussed previously.
First, participants were mostly white young adults, all of whom were able to attend college in the Midwest in the 1980s, potentially limiting generalizability. Additionally, approximately half of the sample was selected based on high familial risk for alcoholism. On the one hand, we see the last factor as advantageous, as family members of alcoholics are at increased risk of high neuroticism and anxiety and depressive disorders, not just substance use disorders (Merikangas & Avenevoli, 2000; Sher et al., 1991); i.e., this is an enriched sample. In addition, we found no evidence of confounding by family history of alcoholism. On the other hand, family members of alcoholics are at increased risk for substance use disorders, though neuroticism and extraversion appear less relevant to this risk than other (putatively orthogonal) personality characteristics (Sher et al., 2000).
Second, for purposes of continuity over time, we employed DSM-III criteria. Importantly, the DSM-III diagnosis of panic disorder was substantially more restrictive than later versions of the DSM; specifically, it required 3 panic attacks within a 3-week period, not just recurrent spontaneous panic attacks. Thus, DSM-III panic disorder was both less common and potentially more severe than later definitions of panic disorder. On the other hand, the DSM-III diagnosis of agoraphobia was less restrictive than DSM-III-R and DSM-IV agoraphobia, and in fact more similar to the modern (DSM-5) conception of agoraphobia, in which the diagnosis is not as restricted to fear of panic attacks. Thus, we consider the measurement of DSM-III agoraphobia a relative strength. The DSM-III conception of GAD was substantially less restrictive than later versions of the DSM, only requiring a month of anxious mood and allowing autonomic anxiety symptoms as part of its definition. GAD was the most common baseline and first-onset diagnosis in the current study, and it is important to acknowledge that DSM-III GAD could be a less severe, pervasive condition than modern GAD. The conceptualization of MDD has not changed substantially since DSM-III.
Third, for the sake of simplicity, we did not address potential subthreshold symptoms of anxiety and depressive disorders; instead we treated diagnoses as binary phenomena (i.e., DSM-III disorder present or absent). Since it would be unclear how baseline personality traits might relate to baseline subthreshold symptoms cross-sectionally, this seems reasonable; however, subthreshold “state” effects could inflate our effect sizes in risk factor analyses. Our “state” and “scar” analyses could also be affected by subthreshold disorder symptoms; specifically, subthreshold symptoms at follow-up would enhance apparent “scar” effects. In fact, results from a large longitudinal epidemiologic study suggest no neuroticism “scar” effect when controlling for residual depressive symptoms (Ormel et al., 2004).
Fourth, we did not control for multiple testing in our analyses; thus, we may have detected spurious differences. For example, we unexpectedly found higher extraversion in participants with current agoraphobia. We have limited confidence in this result, which appears questionable based on prior literature (Karsten et al., 2012).
Fifth, our study does not inform whether high neuroticism is a causal factor for anxiety and depressive disorders, or a marker of vulnerability [e.g., genetic vulnerability (Bienvenu et al., 2007; Hettema et al., 2006)]. Whether or not high neuroticism and low extraversion are causal risk factors, they remain valuable for targeted prevention efforts.
Conclusions
High neuroticism in young adulthood is either a true risk factor, or a marker of risk, for later anxiety and depressive disorders, as is low extraversion for later agoraphobia. However, the current results suggest prominent “state” effects on neuroticism from panic disorder, agoraphobia, and MDD, moderate state effects on neuroticism from GAD, and a moderate scar effects on neuroticism from MDD.
Acknowledgements:
We gratefully acknowledge the contributions of Dr. Everett Siegel as well as the comments of 2 anonymous reviewers that greatly helped shape the manuscript.
Source of Funding: This work was supported by National Institute of Health grants K23MH64543, K05 AA017242, and R37AA7231.
Footnotes
Disclosure of interest: The authors report no conflicts of interest.
IRB: The Institutional Review Board of the University of Missouri approved this study; a Certificate of Confidentiality protected the data.
References
- American Psychiatric Association. Task Force on Nomenclature and Statistics., & American Psychiatric Association. Committee on Nomenclature and Statistics. (1980). Diagnostic and statistical manual of mental disorders (3d ed.). American Psychiatric Association. [Google Scholar]
- Andersen AM, & Bienvenu OJ (2011). Personality and psychopathology. International Review of Psychiatry, 23(3), 234–247. 10.3109/09540261.2011.588692 [DOI] [PubMed] [Google Scholar]
- Bienvenu OJ, & Ginsburg GS (2007). Prevention of anxiety disorders. International Review of Psychiatry, 19(6), 647–654. 10.1080/09540260701797837 [DOI] [PubMed] [Google Scholar]
- Bienvenu OJ, Hettema JM, Neale MC, Prescott CA, & Kendler KS (2007). Low extraversion and high neuroticism as indices of genetic and environmental risk for social phobia, agoraphobia, and animal phobia. American Journal of Psychiatry, 164(11), 1714–1721. 10.1176/appi.ajp.2007.06101667 [DOI] [PubMed] [Google Scholar]
- Eysenck HJ, & Eysenck SBG (1975). Manual of the Eysenck Personality Questionnaire. Educational and Industrial Testing Services. [Google Scholar]
- Fanous AH, Neale MC, Aggen SH, & Kendler KS (2007). A longitudinal study of personality and major depression in a population-based sample of male twins. Psychological Medicine, 37(8), 1163–1172. 10.1017/S0033291707000244 [DOI] [PubMed] [Google Scholar]
- Gershuny BS, & Sher KJ (1998). The relation between personality and anxiety: Findings from a 3-year prospective study. Journal of Abnormal Psychology, 107(2), 252–262. 10.1037//0021-843x.107.2.252 [DOI] [PubMed] [Google Scholar]
- Goldstein BL, Kotov R, Perlman G, Watson D, & Klein DN (2018). Trait and facet-level predictors of first-onset depressive and anxiety disorders in a community sample of adolescent girls. Psychological Medicine, 48(8), 1282–1290. 10.1017/S0033291717002719 [DOI] [PubMed] [Google Scholar]
- Hettema JM, Neale MC, Myers JM, Prescott CA, & Kendler KS (2006). A population-based twin study of the relationship between neuroticism and internalizing disorders. American Journal of Psychiatry, 163(5), 857–864. 10.1176/ajp.2006.163.5.857 [DOI] [PubMed] [Google Scholar]
- Jeronimus BF, Kotov R, Riese H, & Ormel J (2016). Neuroticism’s prospective association with mental disorders halves after adjustment for baseline symptoms and psychiatric history, but the adjusted association hardly decays with time: a meta-analysis on 59 longitudinal/prospective studies with 443 313 participants. Psychol Med, 46(14), 2883–2906. 10.1017/S0033291716001653 [DOI] [PubMed] [Google Scholar]
- Karsten J, Penninx BWJH, Riese H, Ormel J, Nolen WA, & Hartman CA (2012). The state effect of depressive and anxiety disorders on big five personality traits. Journal of Psychiatric Research, 46(5), 644–650. 10.1016/j.jpsychires.2012.01.024 [DOI] [PubMed] [Google Scholar]
- Kendall AD, Zinbarg RE, Mineka S, Bobova L, Prenoveau JM, Revelle W, & Craske MG (2015). Prospective associations of low positive emotionality with first onsets of depressive and anxiety disorders: Results from a 10-wave latent trait-state modeling study. Journal of Abnormal Psychology, 124(4), 933–943. 10.1037/abn0000105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendler KS, Neale MC, Kessler RC, Heath AC, & Eaves LJ (1993). A Longitudinal Twin Study of Personality and Major Depression in Women. Archives of General Psychiatry, 50(11), 853–862. 10.1001/archpsyc.1993.01820230023002 [DOI] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, & Walters EE (2005). Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry, 62(6), 593–602. 10.1001/archpsyc.62.6.593 [DOI] [PubMed] [Google Scholar]
- Kotov R, Gamez W, Schmidt F, & Watson D (2010). Linking “Big” Personality Traits to Anxiety, Depressive, and Substance Use Disorders: A Meta-Analysis. Psychological Bulletin, 136(5), 768–821. 10.1037/a0020327 [DOI] [PubMed] [Google Scholar]
- Merikangas KR, & Avenevoli S (2000). Implications of genetic epidemiology for the prevention of substance use disorders. Addictive Behaviors, 25(6), 807–820. 10.1016/s0306-4603(00)00129-5 [DOI] [PubMed] [Google Scholar]
- Nagel M, Jansen PR, Stringer S, Watanabe K, de Leeuw CA, Bryois J, Savage JE, Hammerschlag AR, Skene NG, Muñoz-Manchado AB, 23 and Me, White, Tiemeier H, Linnarsson S, Hjerling-Leffler J, Polderman TJC, Sullivan PF, van der Sluis S, & Posthuma (2018). Meta-analysis of genome-wide association studies for neuroticism in 449,484 individuals identifies novel genetic loci and pathways. Nature Genetics, 50(7), 920–927. 10.1038/s41588-018-0151-7 [DOI] [PubMed] [Google Scholar]
- Newton-Howes G, Horwood J, & Mulder R (2015). Personality characteristics in childhood and outcomes in adulthood: findings from a 30 year longitudinal study. Aust N Z J Psychiatry, 49(4), 377–386. 10.1177/0004867415569796 [DOI] [PubMed] [Google Scholar]
- Ormel J, Oldehinkel AJ, & Vollebergh W (2004). Vulnerability before, during, and after a major depressive episode - A 3-wave population-based study. Archives of General Psychiatry, 61(10), 990–996. 10.1001/archpsyc.61.10.990 [DOI] [PubMed] [Google Scholar]
- Perna G, Bernardeschi L, Caldirola D, Garberi A, Draisci A, & Battaglia M (1992). Personality dimensions in panic disorder: state versus trait issues. New Trends in Experimental and Clinical Psychiatry, 8, 49–54. [Google Scholar]
- Reich J, Noyes R, Coryell W, & Ogorman TW (1986). The Effect of State Anxiety on Personality Measurement. American Journal of Psychiatry, 143(6), 760–763. 10.1176/ajp.143.6.760 [DOI] [PubMed] [Google Scholar]
- Robins LN, Helzer JE, Cottler L, & Goldring E (1989). Diagnostic Interview Schedule, Version III-R. Washington University. [Google Scholar]
- Robins LN, Helzer JE, Croughan J, & Ratcliff KS (1981). National Institute of Mental Health Diagnostic Interview Schedule - Its History, Characteristics, and Validity. Archives of General Psychiatry, 38(4), 381–389. 10.1007/BF01788437 [DOI] [PubMed] [Google Scholar]
- Sher KJ, Bartholow BD, & Wood MD (2000). Personality and substance use disorders: A prospective study. Journal of Consulting and Clinical Psychology, 68(5), 818–829. 10.1037/0022-006x.68.5.818 [DOI] [PubMed] [Google Scholar]
- Sher KJ, Walitzer KS, Wood PK, & Brent EE (1991). Characteristics of Children of Alcoholics - Putative Risk-Factors, Substance Use and Abuse, and Psychopathology. Journal of Abnormal Psychology, 100(4), 427–448. 10.1037//0021-843x.100.4.427 [DOI] [PubMed] [Google Scholar]
- Zinbarg RE, Mineka S, Bobova L, Craske MG, Vrshek-Schallhorn S, Griffith JW, Wolitzky-Taylor K, Waters AM, Sumner JA, & Anand D (2016). Testing a Hierarchical Model of Neuroticism and Its Cognitive Facets: Latent Structure and Prospective Prediction of First Onsets of Anxiety and Unipolar Mood Disorders During 3 Years in Late Adolescence. Clinical Psychological Science, 4(5), 805–824. 10.1177/2167702615618162 [DOI] [Google Scholar]


