Abstract
Background:
Emergency General Surgery (EGS) encompasses a spectrum of time-sensitive and resource-intensive conditions which require adequate and timely access to surgical care. Developing metrics to accurately quantify spatial access to care is critical for this field. We sought to evaluate the ability of the Spatial Access Ratio (SPAR) which incorporates travel-time, hospital capacity and population demand in its ability to measure spatial access to EGS care and delineate disparities.
Methods:
We constructed a Geographic Information Science (GIS) platform for EGS-capable hospitals in California and mapped population location, race and socioeconomic characteristics. We compared the SPAR to the shortest travel time model in its ability to identify disparities in spatial access overall, and for vulnerable populations. Reduced spatial access was defined as >60 minutes travel time, or lowest three classes of SPAR.
Results:
283 EGS-capable hospitals identified, of which 142 (50%) had advanced resources. Using shortest travel time, only 166,950 persons (0.4% of total population) experienced prolonged (>60 minutes) travel time to any EGS-capable hospital, which increased to 1.05M (2.7%) for advanced-resource centers. Using SPAR, 11.5M (29.5%) had reduced spatial access to any EGS hospital, and 13.9M (35.7%) for advanced-resource centers. Rural residents had significantly decreased access for both overall and advanced EGS services when assessed by SPAR despite travel times within the 60-minute threshold.
Conclusions:
While travel time and SPAR showed similar overall geographic patterns of spatial access to EGS hospitals, SPAR identified a greater a greater proportion of the population as having limited access to care. Nearly one-third of California residents experience reduced spatial access to EGS hospitals when assessed by SPAR. Metrics that incorporate measures of population demand and hospital capacity in addition to travel time may be useful when assessing spatial access to surgical services.
Study type:
Observational
Level of Evidence:
Not applicable
Keywords: Emergency General Surgery, GIS, Spatial Access, Spatial Access Ratio
INTRODUCTION
Emergency general surgery (EGS) conditions constitute a significant public health burden in the United States, accounting for 3 million admissions annually with disproportionately higher morbidity and mortality compared to elective procedures.1–3 While EGS conditions span a wide range of severity, data suggests that up to 44% of admissions are high-acuity and pose an imminent threat to life without emergent surgical intervention.4,5 Timely access to surgical care is therefore critical to optimizing outcomes for this high-risk population.
Unfortunately, hospitals with surgical capabilities are unequally distributed across the United States, leading to considerable disparities in spatial access to care. Limitations in county-level availability of EGS services has been shown to extend beyond rurality and also affect minority and low socioeconomic status (SES) populations.6 Consequently, there is growing concern that reduced spatial access to care may be an important contributor to the elevated morbidity and mortality of these vulnerable populations. Developing methods to accurately and meaningfully quantify spatial access to surgical care is critical to evaluating its contribution to clinical outcomes, yet our understanding of spatial access to surgical services has been largely based on metrics such as travel distance or regional availability that capture only one aspect of accessibility.
Geographic Information Science (GIS) offers unique opportunities by which to study disparities in spatial access to surgical care. Spatial access to healthcare is defined as the ability of individuals to access healthcare services based on the locations of populations and healthcare providers, and involves both travel cost (e.g. distance, time) and supply-demand relationships (e.g. population demand, hospital capacity, resources). EGS conditions, with their time-sensitive and resource-intensive nature may therefore be particularly sensitive to disparities in spatial access to care. While commonly-used measures of travel cost or regional availability are straightforward and easy to understand, they do not capture the effect of supply and demand. Models that reflect both aspects are needed to understand spatial access to surgical care, but have not been widely studied in this field.
To address this gap, we sought to evaluate the ability of the Spatial Access Ratio (SPAR) to measure spatial access to EGS care. Using California as a sample state due to its large size and diverse population, we compared the SPAR, a gravity-based model that accounts for travel cost and supply-demand relationships (see below for more detail), to travel-time alone in its ability to discern patterns of spatial access to EGS-capable hospitals, and secondly, its ability to meaningfully identify disparities in spatial access. We hypothesized that the SPAR model would show a greater ability to identify disparities for the population as a whole, as well as for rural and vulnerable groups.
METHODS
Geospatial Data
We first constructed a GIS platform for EGS-capable hospitals in California. Geospatial data for the state of California including census units, zip code, city boundaries and transportation networks was obtained from the Census Topologically Integrated Geographic Encoding and Referencing file and the StreetMap North America network data set from the Environmental Systems Research Institute.7,8
Hospital Identification
We used the American Hospital Association 2015 Annual Survey Database to obtain information on precise geographic location, clinical resources and measures of utilization. We first identified all non-federal general service hospitals (n=317). We then excluded limited service hospitals (n=7) and any remaining hospital that performed fewer than 10 inpatient surgical cases over the year 2015 (n=9). From this cohort, we then excluded any hospital without an emergency department or general surgery service (n=18). Hospitals were classified as having “advanced” resources if they had at least 5 general ICU beds, at least one full time intensivist, the presence of a CT scanner, ultrasound and advanced gastroenterology services (identified by Endoscopic Retrograde Cholangiopancreatography (ERCP)). These resources were selected for their relevance to management of EGS diseases and signal a basic ability to care for patients with complex or severe illness. Presence of these services was obtained from the AHA database, and if missing or unavailable, review of hospital websites or email communication. We evaluated spatial access first to any EGS hospital, as all hospitals should be capable of managing basic or uncomplicated disease processes, then subsequently to advanced hospitals only, as management of complicated or severe disease would necessitate resources only available at these centers.
Socio-demographic Data
Socio-demographic characteristics examined included population size (overall population and population by race/ethnicity), poverty rate, health insurance coverage rate, and rural/urban status at the census block group (CBG) level. CBGs are the smallest geographical unit for which the census bureau publishes sample data. Population, poverty, and health insurance data were collected from the American Community Survey 2014–2018 five-year average dataset through the IPUMS National Historical Geographic Information System9. The population was categorized into five mutually exclusive groups: non-Hispanic White (NHW), non-Hispanic Blacks (NHB), Hispanic (H), Asian (A) and Native American/American Indian (NA). CBGs were classified into racial/ethnic composition categories based on predominant patterns of residential segregation, including white majority, black majority, and Hispanic majority. Majority was defined as >50% of residents identifying with the racial/ethnic composition category. There were no American Indian majority CBGs. Poverty rate was reported as proportion of homes in the CBG with median annual household income <200% of the federal poverty level. The health insurance coverage rate was calculated as the percentage of those age 18–64 who have at least one type of health insurance (e.g., employer based, privately purchased, Medicaid, Tricare or military-based, and Veterans Administration-based).
Rural/urban status of CBGs were derived from the census tract (i.e. a higher level of census units aggregated from CBGs) level 2010 Rural Urban Commuting Area (RUCA) codes10 and categorized into four groups: metropolitan, micropolitan, small rural, and isolated rural. For each CBG, the rural/urban status was determined by that of the census tract it falls in. Disparities in spatial access were assessed using both Shortest Travel Time Model and the Spatial Access Ratio, described below.
Shortest Travel Time Model
Travel time between a population site and an EGS site was calculated using the ArcMap software (version 10.5)11. Each CBG is considered as a population site and generally contains between 600 and 3,000 people. A population-weighted centroid based on lower level (i.e., census block) population was generated for each CBG to represent the population site’s location. Then, the travel time from a population site to an EGS hospital was calculated by the Network Analyst in ArcMap based on street network data and speed limit information12. This method uses the a priori assumption that all individuals within a CBG would have the same travel time to the nearest EGS hospital. After calculating travel times from a population site to all EGS hospitals, the shortest travel times to any EGS hospital and advanced EGS hospitals was selected. Categories of travel time were set at 10 minute intervals up to 30 minutes, then from 30.1–60 minutes, 60.1–120 minutes and >120 minutes. Short travel time was defined a priori as <20 minutes, while prolonged travel time was defined as >60 minutes.
Spatial Access Ratio Model
Gravity models of spatial access account for complicated interactions among healthcare supply, population demand, and travel cost between population locations and healthcare sites12–18. The Spatial Access Ratio uses an enhanced 2-step floating catchment area (E2SFCA) model, a commonly used and widely validated gravity model, to obtain an assessment of spatial access to health care services for a given population site15–19. Full details of this methodology are provided in supplementary material (Supplemental information 1).
To calculate the Spatial Access Ratio to EGS services in California, we used measures of supply, demand and travel cost. Supply, or surgical capacity, was measured using the annual volume of inpatient surgical operations. Demand was approximated by the population of each CBG. Distance and travel time from CBG population site to hospital site was calculated using ArcMap software as above. To account for the ‘edge effect’ (i.e., individuals living in boundary areas could go to the neighboring state for medical care) in spatial access modeling, a 50-mile buffer zone was extended from the boundary of California. Both California and the buffer zone were included in the spatial access calculation, however only California CBGs are presented in our results.
SPAR is presented as a ratio of the spatial access for the specific CBG relative to a set mean - in this case, the state of California. Greater values of SPAR denote better spatial access. SPAR values greater than one mean better-than-state-average spatial access, and vice versa. Categories of SPAR were identified using Jenk’s natural breaks classification method, which seeks to reduce the variance within classes, while maximizing the variance between classes. Reduced access was defined as the lowest 3 categories of spatial access. For the analysis of all EGS hospitals, this corresponded to an SPAR of <0.75, and for advanced hospitals, an SPAR of <0.81.
Statistical Analysis
We analyzed sociodemographic disparities in spatial access to EGS capable hospitals using both shortest travel time method and SPAR. We assessed differences in access within sociodemographic categories by comparing CBGs with majority (>50%) racial/ethnic minority to CBGs where a majority of residents identified as white. Poverty and insurance were assessed by comparing the respective highest quartile of CBGs to the lower quartile of CBGs. All comparisons were performed using 2-sided t-test, with significance assessed at p<0.05. All analyses were performed with SAS version 9.4 Cary, NC. The study was reviewed by the University of Utah Institutional Review Board and received exempt status.
RESULTS
EGS Capable Hospitals
The process identified a total of 283 hospitals with EGS capability, among which 142 were advanced-resource hospitals. Figure 1 shows the spatial distribution of all EGS hospitals and advanced EGS hospitals in California. Basic characteristics of hospitals are shown in Table 1. Advanced EGS hospitals were primarily located in the urban centers of San Francisco, Los Angeles and Sacramento. Only 8 (5.6%) were located in non-metropolitan areas.
Figure 1.
EGS-capable hospitals in California, 2015
Table 1.
Hospital characteristics of Basic and Advanced EGS hospitals*
| Basic resource hospitals N=141 |
Advanced resource hospitals N=142 |
p-value | |
|---|---|---|---|
| Total bed number | 139 [90–223] | 381 [249–381] | <0.01 |
| Medical/Surgical Intensive Care Unit Beds † | 5 [4–10] | 18.5 [12–30] | <0.01 |
|
Trauma Level | |||
| 1 or 2 | 0 | 42 (29.5%) | p<0.01 |
| 3 or 4 | 8 (5.7%) | 10 (8.0%) | |
| Coronary Intensive Care Unit † | 6 (4.3%) | 77 (54.2%) | p<0.01 |
| Hemodialysis† | 15 (10.6%) | 80 (56.3%) | p<0.01 |
| Emergency Department visits | 21,194 [12,249–42,886] | 51,233.5 [34,299 – 74,985] | <0.01 |
| Number of Operating Rooms† | 4 [3–7] | 11 [7–18] | <0.01 |
| Number of annual inpatient surgeries | 1304 [735 – 1970] | 2897.5 [ 1677 – 5166] | <0.01 |
| Teaching hospital† | 36 (25.5%) | 61 (43.0%) | <0.01 |
All values shown are Median [Interquartile Range] unless otherwise noted
N=184
ICU=Intensive Care Unit
Spatial Access using Shortest Travel Time
Figure 2 displays the geographic patterns of shortest travel time to all EGS-capable hospitals (Figure 2a) and advanced EGS hospitals (Figure 2b). 36.98 million (94.8%) of 39 million people in California live within a radius of 20 minutes driving time to an EGS-capable hospital and are primarily located in metropolitan areas or major cities. In contrast, only 0.17 million persons (0.44%) live outside a 60-minute radius of any EGS-capable hospital. Travel time to advanced EGS hospitals (Figure 2b) showed an increase in the proportion of the population with limited access. Fewer residents were within a 20-minute radius of advanced-resource center (33.49 million, 85.8%), and over one million California residents live outside a 60-minute radius of the nearest advanced-resource EGS hospital (1.05 million, 2.69%).
Figure 2.
Shortest travel time to (a) all EGS hospitals and (b) advanced EGS hospitals in California, 2015 (Note: travel times were first calculated for census block group centroids and then interpolated to the entire state using an inverse distance weighting method)
Spatial Access using Spatial Accessibility Ratio
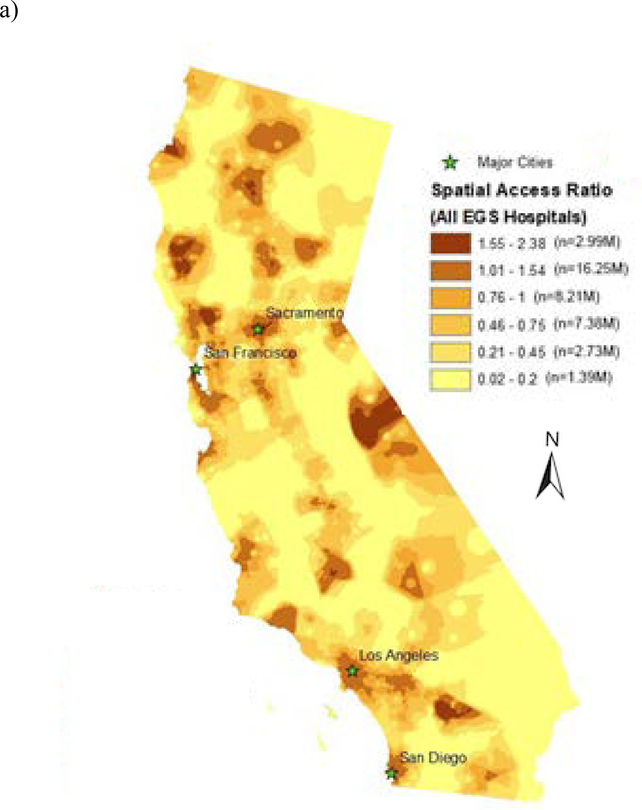
Spatial access measured by SPAR to any EGS-capable hospital, and advanced-resource hospitals is shown in Figure 3a and b, respectively. While the overall geographic pattern of spatial access is similar to that of travel time, SPAR revealed a greater degree of disparity and greater population distribution across all levels of access. Using this metric 2.99 million (7.67%) people were in the category of greatest spatial access, while 11.5 million (29.5%) of people had reduced spatial access (corresponding to SPAR <0.75) to any EGS hospital, with 1.39 million (3.56%) in the lowest category of access (SPAR <0.2). When considering access to advanced-resource hospitals, there is again lower spatial access overall, with 13.93 million (35.7%) with reduced spatial access (SPAR<0.81) and 3.47 million (8.89%) in the lowest category (SPAR<0.15).
Figure 3.
Spatial Access Ratio to (a) all EGS hospitals and (b) advanced EGS hospitals in California, 2015 (Note: SPAR values were first calculated for census block group centroids and then interpolated to the entire state using an inverse distance weighting method; SPAR values were categorized using the Jenk’s Natural Breaks method with minor revisions).
Patterns of Disparities in Spatial Access
Population-level analysis of spatial access to EGS hospitals by race/ethnicity, SES, health insurance coverage and rurality are shown in Table 2. Residents living in rural (non-metropolitan) regions had marked reductions in spatial access, with micropolitan, small rural and isolated rural residents meeting criteria for reduced spatial access to EGS hospitals by SPAR, but not travel time. For example, residents in isolated rural areas had an overall median SPAR of 0.05 [IQR 0.02–0.32] indicating spatial access only 5% of the state average, yet their median travel time remained within the 60-minute threshold at 37.4 minutes [IQR 20.6 – 57.8]. Patterns of spatial access to advanced EGS services follows a similar trend, with all non-metropolitan categories demonstrating significantly restricted access to SPAR, but median travel time less than 60 minutes. Of minority groups, only Native American/American Indians demonstrated reduced spatial access to EGS services using the predefined criteria for advanced EGS hospitals, with median SPAR 0.70 (IQR 0.08, 1.19), despite a median travel time of 11.31 minutes (IQR 5.83, 39.18).
Table 2.
Spatial access to EGS services in California by race/ethnicity, socioeconomic status, health insurance coverage, and rurality
| All EGS hospitals | Advanced EGS hospitals | |||
|---|---|---|---|---|
| Shortest travel time in minutes (median, (IQR)) | Spatial Access Ratio (median, (IQR)) | Shortest travel time in minutes (median, (IQR)) | Spatial Access Ratio (median, (IQR)) | |
| Race/Ethnicity | ||||
| Non-Hispanic White (n=14,760,407) | 6.36 (3.86, 10.39) | 0.92 (0.61, 1.24) | 8.38 (4.98, 15.33) | 0.90 (0.46, 1.31) |
| Non-Hispanic Black (n=2,160,157) | 5.37 (3.61, 7.84) | 1.10 (0.80, 1.34) | 7.76 (4.74, 11.30) | 1.20 (0.73, 1.47) |
| Hispanic (n=15,101,689) | 5.19 (3.40, 8.32) | 1.02 (0.70, 1.28) | 7.43 (4.80, 12.31) | 1.06 (0.62, 1.39) |
| Asian (n=5,425,238) | 5.29 (3.40, 8.01) | 1.05 (0.81, 1.31) | 7.10 (4.53, 10.86) | 1.11 (0.79, 1.46) |
| Native American/American Indian (n=137,710) | 7.16 (4.07, 15.24) | 0.84 (0.47, 1.20) | 11.31 (5.83, 39.18) | 0.70 (0.08, 1.19) |
| Poverty Rate | ||||
| Quartile 1 (Low poverty) (n=9,030,489) | 6.56 (4.16, 9.97) | 0.91 (0.64, 1.19) | 8.40 (5.27, 13.06) | 0.92 (0.60, 1.26) |
| Quartile 2 (n=10,021,864) | 6.05 (3.81, 9.75) | 0.95 (0.67, 1.23) | 7.95 (5.10, 13.13) | 0.97 (0.61, 1.33) |
| Quartile 3 (n=10,052,938) | 5.26 (3.38, 8.53) | 1.02 (0.71, 1.29) | 7.25 (4.59, 12.82) | 1.05 (0.62, 1.42) |
| Quartile 4 (High Poverty) (n=9,850,484) | 4.94 (3.14, 7.72) | 1.08 (0.71, 1.37) | 7.31 (4.43, 12.74) | 1.13 (0.54, 1.49) |
| Health Insurance Coverage | ||||
| Quartile1 (Low Uninsurance) (n=8,960,075) | 6.51 (4.00, 10.10) | 0.93 (0.65, 1.22) | 8.49 (5.09, 13.60) | 0.91 (0.58, 1.32) |
| Quartile 2 (n=10,039,293) | 6.06 (3.83, 9.55) | 0.96 (0.66, 1.23) | 8.11 (4.94, 13.46) | 0.95 (0.56, 1.33) |
| Quartile 3 (n=9,991,152) | 5.44 (3.50, 8.60) | 0.99 (0.69, 1.27) | 7.39 (4.73, 12.94) | 1.01 (0.59, 1.38) |
| Quartile 4 (High Uninsurance) (n=9,965,255) | 4.87 (3.20, 7.54) | 1.09 (0.76, 1.35) | 7.21 (4.61, 11.48) | 1.17 (0.70, 1.46) |
| Rurality | ||||
| Metropolitan (n=36,738,421) | 5.48 (3.52, 8.56) | 1.02 (0.72, 1.29) | 7.41 (4.70, 11.77) | 1.04 (0.68, 1.42) |
| Micropolitan (n=1,450,640) | 12.16 (4.59, 26.68) | 0.45 (0.13, 0.81) | 33.88 (20.18, 58.09) | 0.10 (0.01, 0.52) |
| Small Rural (n=369,726) | 21.52 (12.60, 37.91) | 0.20 (0.06, 0.89) | 53.42 (34.16, 111.03) | 0.04 (0.00, 0.07) |
| Isolated Rural (n=396,988) | 37.39 (20.64, 57.76) | 0.05 (0.02, 0.32) | 59.05 (35.40, 84.05) | 0.02 (0.00, 0.08) |
(note: a larger spatial access ratio (SPAR>1) represents better spatial access, and vice versa); SES=Socioeconomic status
Bolded values denote access below threshold: <60 minutes, or SPAR<0.75 (all EGS hospitals) / SPAR <0.81 (advanced EGS hospitals)
CBG-level analysis of spatial access across racial/ethnicity majority census blocks showed small, clinically insignificant differences in travel time and SPAR in favor of Hispanic, non-Hispanic black and Asian-majority compared to white-majority CBGs, with median travel time and SPAR within the acceptable threshold for reduced access for all groups (Supplemental Table 1a). This was similarly true for high-poverty and high-uninsurance CBGs. Subgroup analysis of metropolitan CBGs yielded similar results (Supplemental Table 1b). When rural CBGs were analyzed independently, Hispanic-majority CBGs had significantly lower SPAR for EGS hospitals overall (0.25 [IQR 0.07–0.51] vs white-majority 0.41 [0.05–0.91] p<0.001) whereas there was no difference in travel time (20.68 min [7.94–36.56] vs 16.05 min [6.05–39.36], p=0.31) (Table 3). Highest quartile poverty and uninsured CBGs had reduced access compared to reference groups by both SPAR and travel time.
Table 3.
Spatial Access in Rural Census Block Groups*
| Race/Ethnicity | Majority White n=1166 | Majority Hispanic n=361 | p-value | |
| All Hospitals | SPAR | 0.41 [0.05, 0.91] | 0.25 [0.07, 0.51] | <0.001 |
| Time (minutes) | 16.05 [6.05, 39.36] | 20.68 [7.94, 36.56] | 0.31 | |
| Advanced Resources | SPAR | 0.06 [0, 0.46] | 0.06 [0.03, 0.37] | <0.001 |
| Time | 48.62 [23.71, 76.2] | 34.58 [24.28, 55.35] | <0.001 | |
| Poverty | Lowest Poverty Quartile n=413 | Highest Poverty Quartile n=414 | p-value | |
| All Hospitals | SPAR | 0.45 [0.11, 0.84] | 0.3 [0.04, 0.70] | 0.02 |
| Time | 13.39 [5.87, 29.69] | 19.64 [5.46, 41.5] | 0.01 | |
| Advanced Resources | SPAR | 0.10 [0, 0.52] | 0.04 [0, 0.34] | 0.67 |
| Time | 38.56 [19.80, 70.37] | 43.59 [25.24, 72.48] | 0.63 | |
| Insurance coverage | Lowest Uninsured Insured n=414 | Highest Uninsured Quartile n=416 | p-value | |
| All Hospitals | SPAR | 0.48 [0.08, 0.93] | 0.23 [0.04, 0.6] | <0.001 |
| Time | 14.54 [5.40, 35.90] | 22.16 [9.19, 42.48] | <0.01 | |
| Advanced Resources | SPAR | 0.06 [0, 0.52] | 0.06 [0, 0.52] | 0.29 |
| Time | 46.76 [23.28, 75.20] | 41.69 [23.31, 71.55] | 0.83 | |
All values reported as median [interquartile range], n denotes number of census block groups analyzed. No rural majority Non-Hispanic Black or majority Asian CBGs were identified.
DISCUSSION
Emergency general surgery encompasses a wide spectrum of diseases that are often both time-sensitive and resource-intensive. Models of spatial access that incorporate not only travel time, but also population demand and hospital capacity are particularly relevant for this surgical specialty. In this study, we demonstrate use of the Spatial Access Ratio to measure geospatial access to EGS services in California using the commonly-used metric of travel time as a comparator. We found the metrics showed similar overall geographic patterns, however SPAR identified a greater degree of disparity in spatial access with a 29% absolute increase in the proportion of the population classified as having limited access to care. SPAR also identified disparities in access for minorities in rural areas that were not apparent using travel time alone.
Measurement of spatial access to surgical care has garnered increasing attention over the past decade, with important implications for health systems planning and resource allocation. Geospatial access involves both components of accessibility (i.e. proximity of patients to health services) and availability (i.e. adequacy of the type and supply of services relative to population needs). The use of time or distance metrics captures only accessibility, and can be problematic for emergency surgical care where specialized services such as intensive care capabilities and timely operating room availability may be critical to patient outcomes. An individual patient might be within close geographic proximity to a surgical hospital, but should the hospital have inadequate surgical capacity or be overwhelmed by patient demand, the patient’s overall spatial access to surgical care remains poor. Metrics such as SPAR capture both the accessibility and availability dimensions of spatial access. This is not to say that one metric is universally better; accessibility metrics such as travel time are certainly important – they are easily measured and understood, and readily available to patients. However, metrics such as SPAR that incorporate both accessibility and availability may be more useful for health systems planning that require consideration of health care capacity and population demand.
Prior studies of spatial access to EGS services in the United States have found large variations across geographic regions and revealed significant disparities in access for minority and socioeconomically vulnerable populations. Diaz et al in their study of geospatial access to inpatient surgery found that in 2015, 6.2 million people (3.9%) lived outside a 60-minute radius from any surgical hospital (an 82% increase over the previous decade), and 25.9 million (8.4%) from a major surgical hospital.20 Similarly, a county-level analysis of EGS availability by Khubchandani et al demonstrated that counties with higher proportions of rural, black, Hispanic, poor and uninsured patients had significantly higher odds of not having an EGS hospital.6 Together, these studies strongly indicate limitations and disparities in access to EGS services affect millions of U.S residents. However, purely travel-time or regional-availability measures are limited in their ability to account for health-seeking behaviors, such as the common event of crossing county borders, and cannot account for complex interactions with resource supply and demand.
To our knowledge, this is the first study to examine spatial access to surgical services using a metric that incorporates measures of hospital capacity and population demand. Our results for spatial access to EGS in California align with the travel time-based assessment of Diaz et al., but give greater granularity with regards to levels of access.20 SPAR offers an improved distribution of the population across the range of the metric, with substantial proportions of residents in each category, as compared to travel time, where a large degree of clustering occurs at the extremes of the scale. Moreover, SPAR identified distinct disparities in EGS access for rural regions with high proportion of Hispanic residents compared to predominantly white regions, a difference not readily apparent using travel time alone. This discrepancy between metrics may be explained by high demand with inadequate EGS resources in these regions. Adding resources and surgical capacity in these areas might help to address known disparities in access and clinical outcomes for minority communities. SPAR has been previously used to assess spatial access to medical oncologists for colorectal and breast cancer patients, with limited spatial access associated with decreased survival for rural patients.16,21–23 Our study results suggest that this metric can successfully be extended to surgical populations by incorporating simple measures of inpatient surgical capacity. This is directly relevant for health systems planning, with implications for other time and resource-dependent surgical specialties, including trauma and burn care.24, 25
A central finding in our analysis of disparities is the magnitude of limitations to EGS care for rural residents. In addition to longer travel times to reach surgical care, the overall spatial access for small rural community residents was a SPAR of 20% of the state average for EGS hospitals overall, and only 4% for advanced level care – a disparity which appears to be compounded for minority communities in rural areas. The rate of rural hospital closures in the United States has been increasing over the past decade, with 128 rural hospitals with inpatient capabilities closed since 2010 and over 1.7 million Americans were affected by rural hospital closures from 2010–2014.26, 27 The marked disparity we observed in spatial access to emergency surgical care is particularly worrisome for rural residents – and in particular, rural minority communities, placing them at risk for worse clinical outcomes due to delayed surgical intervention.
Our results must be interpreted in the context of several limitations. First, while we attempted to verify hospital EGS capabilities using multiple sources of information, misclassification of hospitals – either as “EGS-capable” or “advanced” is possible due to missing data in the selected data sources or inaccurate information during manual hospital review. Studies using similar methods have overall found a low rate of misclassification of EGS-capable hospitals and should not significantly affect our ability to compare the travel cost and gravity-based models.6 As formalized resource levels for EGS care have not been established, we used a broad definition of advanced resources, which focused on critical care and advanced GI services, two common reasons EGS patients undergo transfer to higher-level care centers. Further differentiation of advanced-resource centers based on more specialized resources (eg. continuous renal replacement therapy, interventional radiology, extracorporeal membrane oxygenation) and processes (eg. continuous in-house presence of general surgeons, designated acute care surgery operating rooms, 24-hour availability of interventional radiology) is needed, and will be best accomplished through guidance and consensus from governing bodies such as the American College of Surgeons, as has been done for trauma. Our assessment of spatial access also focuses only on initial hospital presentation, and does not account for the complexities of inter-hospital transfer and use of air-medial transport in this process.
With respect to construction of the SPAR metric, we did not have EGS specific case-volume of EGS surgeons for each hospital, and therefore used overall inpatient surgical case volume as a proxy measure for hospital capacity. This metric also represents only potential spatial access to care, and does not account for individual patient characteristics such as insurance status or behavior based on preferences. Insurance coverage is an important consideration that may influence patient decisions on where to seek care, but under the Emergency Medical Treatment and Labor Act should not restrict them from receiving emergency care at any hospital. Finally, the SPAR is a ratio, and as such, the values we present are relative to the California state mean. Without clear benchmarks on what constitutes “adequate” spatial access to care, it is therefore difficult to delineate exactly what level of SPAR demands improvement. Nevertheless, this ratio does work well for identifying the magnitude of disparities amongst vulnerable populations in a manner that is not easily communicated by travel time or distance alone.
There is considerable potential for SPAR to influence the equitable allocation of surgical resources. Modeling the effects of adding EGS-capable hospitals to low-SPAR regions, or simply adding specific resources (e.g. operating rooms, critical care capacity) where augmenting number of hospitals is not an option, will allow for estimations of how these efforts will affect the overall population, and reduce known disparities in access to care.28–31 In addition to evaluating how potential spatial access compares to realized access to care, further work is needed to examine the contribution of spatial access to clinical outcomes, and the influence of sociodemographic factors on this relationship. This understanding will be critical to developing coordinated care strategies that optimize outcomes for all EGS patients, including those who experience the greatest challenges reaching the hospital in the first place.
CONCLUSIONS
Models of spatial access that incorporate measures of hospital capacity and population demand in addition to travel cost are relevant to surgical fields such as EGS that require physical resources to treat patients. Nearly one-third of California residents experience reduced access to EGS hospitals when assessed by SPAR While travel time and SPAR showed similar overall patterns of spatial access to EGS-capable hospitals in California, SPAR showed greater differentiation of access across the state, and may be particularly useful in evaluating disparities and directing allocation of resources.
Supplementary Material
Acknowledgments
FUNDING
Dr McCrum was supported by funding from the American Association for the Surgery of Trauma Research and Education Scholarship and the National Institute of Minority and Health Disparities R21MD012657.
Footnotes
CONFLICT OF INTEREST
None of the authors have relevant conflicts of interest to report
REFERENCES
- 1.Ogola GO, Gale SC, Haider A, Shafi S. The financial burden of emergency general surgery: National estimates 2010 to 2060. J Trauma Acute Care Surg. 2015;79(3):444–448. [DOI] [PubMed] [Google Scholar]
- 2.Havens JM, Peetz AB, Do WS, Cooper Z, Kelly E, Askari R, Reznor G, Salim A. The excess morbidity and mortality of emergency general surgery. J Trauma Acute Care Surg. 2015;78(2):306–311. [DOI] [PubMed] [Google Scholar]
- 3.Gale SC, Shafi S, Dombrovskiy VY, Arumugam D, Crystal JS. The public health burden of emergency general surgery in the United States: A 10-year analysis of the Nationwide Inpatient Sample−−2001 to 2010. J Trauma Acute Care Surg. 2014;77(2):202–208. [DOI] [PubMed] [Google Scholar]
- 4.Shafi S, Aboutanos MB, Agarwal S, Brown CVR, Crandall M, Feliciano DV, Guillamondegui O, Haider A, Inaba K, Osler TM et al. Emergency general surgery: definition and estimated burden of disease. J Trauma Acute Care Surg. 2013;74(4):1092–1097. [DOI] [PubMed] [Google Scholar]
- 5.Scott JW, Olufajo OA, Brat GA, Rose JA, Zogg CK, Haider AH, Salim A, Havens JM. Use of National Burden to Define Operative Emergency General Surgery. JAMA Surg. 2016;151(6):e160480. [DOI] [PubMed] [Google Scholar]
- 6.Khubchandani JA, Shen C, Ayturk D, Kiefe CI, Santry HP. Disparities in access to emergency general surgery care in the United States. Surgery. 2018;163(2):243–250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.TIGER. Topologically Integrated Geographic Encoding and Referencing system. 2017; https://www.census.gov/geo/maps-data/data/tiger.html. Accessed May 19, 2017.
- 8.ESR I. StreetMap North America. 2010.
- 9.Manson S, Schroeder J, Van Riper D, Ruggles S. Ipums national historical geographic information system: Version 14.0. Minneapolis, MN: IPUMS. In:2019. [Google Scholar]
- 10.USDA. Rural-urban commuting areas codes, version 2.0. http://www.ers.usda.gov/data-products/rural-urban-commuting-area-codes.aspx#.U9lO7GPDWHo Last accessed 18 August 2019. In:2019.
- 11.ArcGIS Desktop: Release 10.5 [computer program]. Redlands, CA: Environmental Systems Research Institute; 2017. [Google Scholar]
- 12.Wan N, Zou B, Sternberg T. A three-step floating catchment area method for analyzing spatial access to health services. Int. J. of Geogr. Inf. Sci. 2012;26(6):1073–1089. [Google Scholar]
- 13.Guagliardo MF. Spatial accessibility of primary care: concepts, methods and challenges. Int. J. Health Geogr. 2004;3(1):3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Luo W Using a GIS-based floating catchment method to assess areas with shortage of physicians. Health Place. 2004;10(1):1–11. [DOI] [PubMed] [Google Scholar]
- 15.Luo W, Qi Y. An enhanced two-step floating catchment area (E2SFCA) method for measuring spatial accessibility to primary care physicians. Health Place. 2009;15(4):1100–1107. [DOI] [PubMed] [Google Scholar]
- 16.Wan N, Zhan FB, Zou B, Chow E. A relative spatial access assessment approach for analyzing potential spatial access to colorectal cancer services in Texas. Appl. Geogr. 2012;32(2):291–299. [Google Scholar]
- 17.Joseph AE, Bantock PR. Measuring potential physical accessibility to general practitioners in rural areas: a method and case study. Soc. Sci. Med. 1982;16(1):85–90. [DOI] [PubMed] [Google Scholar]
- 18.Lin Y, Wan N, Sheets S, Gong X, Davies A. A multi-modal relative spatial access assessment approach to measure spatial accessibility to primary care providers. Int. J. Health Geogr. 2018;17(1):33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Donohoe J, Marshall V, Tan X, Camacho FT, Anderson R, Balkrishnan R. Evaluating and comparing methods for measuring spatial access to mammography centers in Appalachia. Health Serv. Outcomes Res Methodol. 2016;16(1–2):22–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Diaz A, Schoenbrunner A, Pawlik TM. Trends in the Geospatial Distribution of Inpatient Adult Surgical Services across the United States. Ann Surg. 2019. [DOI] [PubMed] [Google Scholar]
- 21.Wan N, Zhan FB, Lu YM, Tiefenbacher JP. Access to healthcare and disparities in colorectal cancer survival in Texas. Health Place. 2012;18(2):321–329. [DOI] [PubMed] [Google Scholar]
- 22.Wang FH, McLafferty S, Escamilla V, Luo L. Late-stage breast cancer diagnosis and health care access in illinois. Prof Geogr. 2008;60(1):54–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wan N, Zhan FB, Zou B, Wilson JG. Spatial Access to Health Care Services and Disparities in Colorectal Cancer Stage at Diagnosis in Texas. Prof Geogr. 2013;65(3):527–541. [Google Scholar]
- 24.Dooley JH, Ozdenerol E, Sharpe JP, Magnotti LJ, Croce MA, Fischer PE. Location, location, location: Utilizing Needs-Based Assessment of Trauma Systems-2 in trauma system planning. J Trauma Acute Care Surg. 2020; 88(1):94–100. [DOI] [PubMed] [Google Scholar]
- 25.Carmichael H, Wiktor AJ, McInture RC, Wagner AL, Velopulos CG. Regional disparities in access to verified burn center care in the United States. J Trauma Acute Care Surg. 2019; 87(1): 111–116. [DOI] [PubMed] [Google Scholar]
- 26.Research TCGSCfHS. Rural Hospital Closures. 2020; shepcenter.unc.edu/programs-projects/rural-health/rural-hospital-closures Accessed April 6, 2020.
- 27.Kaufman BG, Thomas SR, Randolph RK, Perry JR, Thompson KW, Holmes GM, Pink GH. The Rising Rate of Rural Hospital Closures. J Rural Health. 2016;32(1):35–43. [DOI] [PubMed] [Google Scholar]
- 28.Lehaney B, Hlupic V. Simulation modelling for resource allocation and planning in the health sector. J R Soc Health. 1995;115(6):382–385. [DOI] [PubMed] [Google Scholar]
- 29.Santos A, Fallah N, Lewis R, Dvorak MF, Fehlings MG, Burns AS, Noonan VK, Cheng CL, Chan E, Singh A, et al. Methodology of the Access to Care and Timing Simulation Model for Traumatic Spinal Cord Injury Care. J Neurotrauma. 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Brown JB, Rosengart MR, Billiar TR, Peitzman AB, Sperry JL. Distance matters: Effect of geographic trauma system resource organization on fatal motor vehicle collisions. J Trauma Acute Care Surg. 2017;83(1):111–118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gomez D, Haas B, Doumouras AG, Zagorski B, Ray J, Rubenfel G, McLellan BA, Boyes DM, Natherns AB. A Population-Based Analysis of the Discrepancy Between Potential and Realized Access to Trauma Center Care. Ann. Surg. 2013;257(1):160–165. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.