INTRODUCTION
Cigarette smoking remains a major cause of premature death and nicotine dependence is a major barrier to smoking cessation.1,2 The DSM-5 is the primary guide to psychiatric diagnoses in the U.S. The 5th revision, released in 2013, replaced the term “nicotine dependence” and instead assigns the diagnosis “Tobacco Use Disorder” (TUD) to individuals experiencing clinically significant impairment, as indicated by meeting at least 2 of 11 specified criteria.3 Clinical practice guidelines encourage clinicians to routinely assess and treat tobacco use and dependence.4 Patient’s self-reported smoking rate is often used to guide clinical decision making, but surprisingly no previous report has described the proportion of cigarette smokers who meet DSM-5 TUD criteria across the full range of cigarette use patterns in a representative sample of the U.S. population. Lighter smoking is frequently perceived as less harmful. Consequently, such smokers may be less likely to be identified by medical providers and less likely to receive appropriate treatment.5 Information on the true prevalence of TUD in this population can directly inform clinical practice.
METHODS
The authors analyzed data from the National Epidemiological Study of Alcohol and Related Conditions–III, a nationally representative study of the non-institutionalized adult civilian population in the U.S. conducted from 2012 to 2013. Analyses were conducted in 2020. A total of 36,309 individuals (60.1% response rate) participated. The present analysis included individuals who reported past-year cigarette use, no use of other tobacco products, and had smoking rate information available (n=6,793). In-person interviews were conducted to assess the presence and severity of DSM-5 TUD among smokers. A detailed description of study procedures and interviews is available elsewhere.6–8 Details on individual symptom coding and the analytic approach are available in the Appendix. This project was deemed exempt by the Duke University Health System IRB.
RESULTS
Figure 1 illustrates the proportion of cigarette smokers at each level of cigarette consumption who met TUD criteria, and the mean number of criteria (of 11) met at each level of cigarette consumption. A clear relationship between the number of cigarettes smoked on a typical smoking day and the probability of meeting TUD criteria was also evident for non-daily smokers. Even among those who smoked less than weekly, 18.3% (95% CI=13.7, 24.2) of those who typically smoked 1–2 cigarettes on a smoking day met TUD criteria, whereas 44.6% (95% CI=36.8, 52.6) of those who smoked ≥3 cigarettes on a smoking day met TUD criteria. The Appendix provides additional details.
Figure 1.
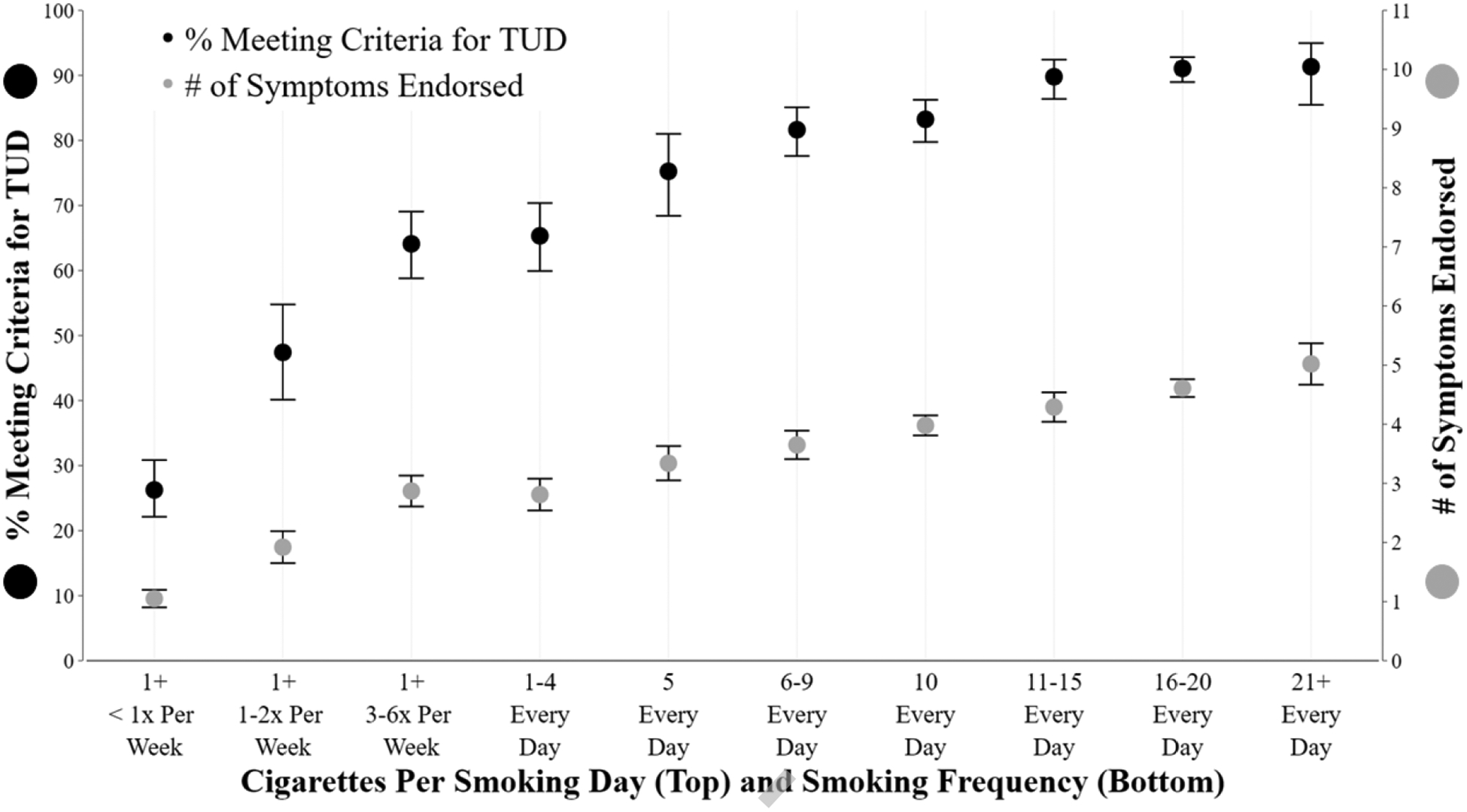
Relationship of cigarette smoking frequency with tobacco use disorder and mean symptoms endorsed.
Notes: Bars represent 95% CIs.
TUD, tobacco use disorder.
DISCUSSION
Results reveal a clear relationship between frequency of cigarette smoking and the proportion of cigarette smokers meeting DSM-5 TUD criteria, which becomes relatively flat above 10 cigarettes per day (CPD), at around 90%. Notably, almost two thirds of those smoking only 1–4 CPD met TUD criteria, as did the majority (64.1%) of those smoking 3–6 days per week and a substantial minority (26.3%) of individuals who smoke less than once per week. DSM-5 states that TUD is considered of “moderate” severity when ≥4 criteria are met, and these data show this is typical at ≥10 CPD. The proportion of smokers meeting diagnostic criteria at specific levels of cigarette consumption appears greater than in prior studies using DSM-4 criteria for nicotine dependence.9,10 This may be related to numerous factors, including changes in diagnostic criteria to encompass a dimensional approach that includes mild TUD (meeting 2–3 of 11 criteria), as well as the substantial (42%) increase in average nicotine intake per cigarette in recent decades.11 The present study highlights the high prevalence of TUD even among those considered light smokers and potential need for treatment within this population. Previous research has found that low-rate smokers report greater motivation to quit and are more likely than daily smokers to make a quit attempt.12,13 However, it is unclear the extent to which existing interventions are effective for light smokers. Continued efforts to identify optimal cessation approaches for this population remain an important direction for future research. Strengths of this study include the large representative sample spanning the full range of smoking patterns, and the use of a validated diagnostic assessment.
Limitations
Limitations include reliance on self-report and the exclusion of individuals who use multiple tobacco products, who represent a rapidly growing segment of the population of smokers.
CONCLUSIONS
The overwhelming majority (85.0%) of daily cigarette smokers and a sizable minority of non-daily smokers (44.0%) meet DSM-5 diagnostic criteria for TUD. Clinicians should ask about all smoking behavior, including non-daily smoking, as such smokers may still require treatment to successfully quit smoking.
Supplementary Material
ACKNOWLEDGMENTS
This manuscript was prepared using a limited access dataset obtained from the National Institute on Alcohol Abuse and Alcoholism (NIAAA). It does not reflect the opinions or views of NIAAA or the U.S. government. Additional support was provided by a career development award provided to JAO by the National Institute on Drug Abuse (K23 DA042898). JF is supported by NIH grants (R01 DA048428, U01 DA045517). The funders had no role in the design and conduct of the study; collection, management, analysis, or interpretation of the data; preparation, review, or approval of the manuscript; or decision to submit the manuscript for publication.
JF conceived the project. JAO and JF jointly designed the project. JAO conducted the statistical analysis. JF wrote the initial draft of the manuscript. Both JAO and JF reviewed the manuscript for important intellectual content and approved the submitted version.
JAO is co-inventor on a provisional patent of a system using machine learning to identify smoking environments from visual images that is unrelated to the submitted work. JF has received grants from the NIH; has previously received a grant, personal fees, and nonfinancial support from Pfizer Inc. unrelated to the submitted work; in the past (>3 years ago) has done paid consulting for pharmaceutical companies involved in manufacturing smoking-cessation medications (e.g., GlaxoSmithKline, Johnson & Johnson); and has acted as a deposed and compensated expert witness on behalf of plaintiffs suing cigarette manufacturers.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.WHO report on the global tobacco epidemic, 2017: monitoring tobacco use and prevention policies. WHO; 2017. https://www.who.int/tobacco/global_report/2017/en/. Accessed November 12, 2020. [Google Scholar]
- 2.The health consequences of smoking—50 years of progress: a report of the Surgeon General. Atlanta, GA: HHS, Centers for Disease Control; 2014. https://www.cdc.gov/tobacco/data_statistics/sgr/50th-anniversary/index.htm. Accessed November 12, 2020. [Google Scholar]
- 3.American Psychiatric Association. Diagnostic and statistical manual of mental disorders (DSM-5®). American Psychiatric Publishing; 2013. 10.1007/springerreference_179660. [DOI] [Google Scholar]
- 4.Fiore MC, Jaén CR, Baker TB, et al. Treating tobacco use and dependence: 2008 update. Rockville, MD: HHS; 2008. https://www.ahrq.gov/prevention/guidelines/tobacco/index.html. Accessed November 12, 2020. [Google Scholar]
- 5.Schane RE, Glantz SA, Ling PM. Nondaily and social smoking: an increasingly prevalent pattern. Arch Intern Med. 2009;169(19):1742–1744. 10.1001/archinternmed.2009.315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Grant BF, Goldstein RB, Smith SM, et al. The Alcohol Use Disorder and Associated Disabilities Interview Schedule-5 (AUDADIS-5): reliability of substance use and psychiatric disorder modules in a general population sample. Drug Alcohol Depend. 2015;148:27–33. 10.1016/j.drugalcdep.2014.11.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Oliver JA, Pacek LR, Locey EN, Fish LM, Hendricks PS, Pollak KI. Lack of utility of cigarettes per day cutoffs for clinical and laboratory smoking research. Addict Behav. 2019;98:106066. 10.1016/j.addbeh.2019.106066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hasin DS, Greenstein E, Aivadyan C, et al. The Alcohol Use Disorder and Associated Disabilities Interview Schedule-5 (AUDADIS-5): procedural validity of substance use disorders modules through clinical re-appraisal in a general population sample. Drug Alcohol Depend. 2015;148:40–46. 10.1016/j.drugalcdep.2014.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Donny EC, Dierker LC. The absence of DSM-IV nicotine dependence in moderate-to-heavy daily smokers. Drug Alcohol Depend. 2007;89(1):93–96. 10.1016/j.drugalcdep.2006.11.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Grant BF, Shmulewitz D, Compton WM. Nicotine use and DSM-IV nicotine dependence in the United States, 2001–2002 and 2012–2013. Am J Psychiatry. 2020;177(11):1082–1090. 10.1176/appi.ajp.2020.19090900. [DOI] [PubMed] [Google Scholar]
- 11.Jarvis MJ, Giovino GA, O’Connor RJ, Kozlowski LT, Bernert JT. Variation in nicotine intake among US cigarette smokers during the past 25 years: evidence from NHANES surveys. Nicotine Tob Res. 2014;16(12):1620–1628. 10.1093/ntr/ntu120. [DOI] [PubMed] [Google Scholar]
- 12.Tindle HA, Shiffman S. Smoking cessation behavior among intermittent smokers versus daily smokers. Am J Public Health. 2011;101(7):e1–e3. 10.2105/ajph.2011.300186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kotz D, Fidler J, West R. Very low rate and light smokers: smoking patterns and cessation-related behaviour in England, 2006–11. Addiction. 2012;107(5):995–1002. 10.1111/j.1360-0443.2011.03739.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


